- 1Department of Global Health and Development, Graduate School, Hanyang University, Seoul, South Korea
- 2Institute of Health Services Management, Hanyang University, Seoul, South Korea
- 3Department of Obstetrics and Gynecology, College of Medicine, Hanyang University, Seoul, South Korea
- 4Department of Preventive Medicine, College of Medicine, Hanyang University, Seoul, South Korea
Background: There are limited data on the use of herbal medicines (HM) among breastfeeding mothers, despite the fact that knowledge of the possible benefits or harms of HM use has a direct relationship with the health of infants, especially in resource-limited countries. The study aims to determine the prevalence and factors associated with HM use among breastfeeding mothers in Tanzania.
Methods: The study followed a cross-sectional design using a structured survey questionnaire. Survey participants were recruited from the reproductive and child health clinic at Uhuru health center in Morogoro, Tanzania. The survey instrument comprised of 34 questions, including demographic information, the pattern of HM use during breastfeeding, and women’s perceptions of HM. Chi-square test and logistic regression were used for data analysis using SPSS ver. 24.0.
Results: The majority of the respondents (53.8%) used HM during breastfeeding. The most commonly used HM was black pepper (Piper nigrum L.; 80.0%), followed by pumpkin seeds (Cucurbita pepo L.; 18.0%). About one-third (27.5%) of HM users discussed their use with their healthcare providers. In addition, higher education levels and low breastmilk supply were identified as potential predictors of HM use.
Conclusion: The practice of HM use among breastfeeding mothers in Tanzania is popular to ease breastfeeding difficulties. However, the issue of the safety or effectiveness of HM is still an unknown agenda. This awakens the need to evaluate HM’s safety, efficacy, and quality through pharmacological studies for scientific evidence. Lastly, a clinical guideline should be developed in healthcare settings to promote open dialogues between the healthcare providers and mothers to ensure the safe use of HM.
Introduction
Globally, there is an increasing number of studies on women’s lifelong use of herbal medicines (HM). Several studies have documented women’s HM use in various life stages, starting from menstruation, pregnancy, childbirth, postpartum, and menopause (Ngoma and Siachapa, 2017; Wang J. et al., 2018; Moini Jazani et al., 2018; Zheng et al., 2019; Adane et al., 2020; Sumankuuro et al., 2020). Especially during some of these life stages, such as pregnancy, delivery, and the postpartum period, women’s HM use should be paid close attention to, as seemingly naive HM that has no negative impact on non-pregnant women can have a detrimental effect on the child and pregnant woman (Budzynska et al., 2012; Ahmed et al., 2017).
According to the World Health Organization, exclusive breastfeeding (EBF) is an essential practice during the postpartum period for maternal and child health (WHO, 2015), as it is one of the most effective ways to promote both mothers’ and newborns’ physiological and psychological health (Ebina and Kashiwakura, 2012; Antonakou et al., 2013; Al Sabati and Mousa, 2019; Mikšić et al., 2020). Breastmilk is more natural and cost-effective than bottle feeding and ensures ideal nutrition for newborns, thus promoting infant health, providing essential bioactive nutrients, and lowering the risks for various infections and hospitalizations (Oguchi et al., 1997; Butte et al., 2002; Hauck et al., 2011; Ajetunmobi et al., 2015). In addition, breastfeeding facilitates mother and child bonding by promoting physical intimacy between the mother and child (Johnson, 2013; Liu et al., 2013). However, up to 92% of nursing women encounter various difficulties during their breastfeeding journeys (Wagner et al., 2013). Some mothers seek an alternative mode of care, such as HM, to alleviate the problems due to the lack of access to conventional healthcare services and the belief that HM is more natural and safe to use than conventional medicine (Augustino and Gillah, 2005; Sim et al., 2013; Aleandri et al., 2014; Zheng et al., 2020). Some of the commonly used HM among breastfeeding mothers include fenugreek (Trigonella foenum-graecum L.), ginger (Zingiber officinale Roscoe), fennel (Foeniculum vulgare Mill.), shatavari (Asparagus racemosus Willd.), and aniseed (Pimpinella anisum L.). Moreover, various phytochemical compounds (e.g., glycosides, alkaloids, flavonoids, and minerals) found in medicinal plants modulate hormone levels and act as lactogenic agents (Bnouham, 2010; Dandotiya et al., 2013; Sim et al., 2013).
Nevertheless, there is much debate about whether the existing evidence related to breastfeeding mother’s HM use supports their safety and efficacy (Sim et al., 2013; Bettiol et al., 2018a) as previous studies show inconclusive evidence explaining the mechanism behind herbs as galactagogues, requiring further research to determine HM’s clinical efficacy (Anderson, 2017; Bowman, 2017; Wang S. et al., 2018; Sibeko et al., 2021). Furthermore, inappropriate use of certain HM during breastfeeding was found to cause allergic reactions and neurotoxic effects on newborns (Bnouham, 2010). Yet, irrespective of the lack of scientific evidence and potential harm to newborns, as large as 97% of breastfeeding women use HM to overcome challenges with breastfeeding, and concerns are rising about the level of knowledge among healthcare providers on breastfeeding women’s HM use (Sim et al., 2013; Bettiol et al., 2018b; James et al., 2019; Zheng et al., 2020).
Thus, several studies have examined breastfeeding mothers’ HM use in various cultural settings (Bnouham, 2010; Sim et al., 2013; Aleandri et al., 2014; Bettiol et al., 2018b; James et al., 2019; Orabi et al., 2020; Zheng et al., 2020). However, limited data is available regarding the HM use in East African countries like Tanzania even though HM use is widely practiced to treat various physical conditions such as women’s complications as well as infectious and chronic diseases (Augustino and Gillah, 2005; Moshi et al., 2009; Amri and Kisangau, 2012; Kacholi and Amir, 2022). Consequently, breastfeeding mothers’ self-care practices must be examined to establish appropriate policy measures and clinical protocols to ensure the health of the mother and the child. Therefore, this study aims to examine the pattern and factors associated with HM use among breastfeeding mothers in Tanzania. Furthermore, this study emphasizes the importance of informing policymakers for developing a clinical guideline that could improve the self-care behaviors of women during breastfeeding.
Materials and Methods
Study Design
A descriptive cross-sectional study was conducted to identify HM use among breastfeeding mothers in Morogoro, Tanzania.
Study Setting and Participants
The eligible participants included all breastfeeding women but are not limited to exclusive breastfeeding women between the ages of 18–49 years old with a child below 2 years who visited the reproductive and child health clinic at Uhuru health center in Morogoro, Tanzania. On average, approximately 160 pregnant women visit the Uhuru health center per month, and about 20% of those women visit the center for the reproductive and child health services. Exclusion criteria were those women attending the clinic for services apart from reproductive and child healthcare services and those who did not consent to participate in the survey.
Study Size
The sample size determination formula, based on the confidence interval (CI) was used to calculate the required sample size:
Data Collection
A face-to-face interview using a structured questionnaire was conducted from August 2017 to November 2017. The survey was conducted by three trained surveyors from Tanzania. All participants were informed about the confidentiality of the study and were given verbal information and instructions regarding the research. Participants who completed the IRB-approved consent form were able to participate in the study. A total of 400 questionnaires were distributed, 28 questionnaires were incomplete (response rate: 93.0%); therefore, the data of 372 respondents were included in the analysis.
Survey Instrument
The questionnaire was first developed in English based on previous studies investigating HM use among breastfeeding women (Sim et al., 2013). In order to measure the content and face validity of the survey instrument, the questionnaire was reviewed by three experts (two researchers who were maternal and child health experts in Korea and one researcher from Uhuru health center, Tanzania). The questionnaire was then translated into Swahili, which was translated back into English by a third party to confirm its accuracy. The questionnaire was pilot-tested on a sample of 20 participants to evaluate the clarity and reliability of the questions.
The final version of the questionnaire consisted of three sections with 34 items, including multiple-choice and open-ended questions. The first section included eight questions on the health-related characteristics of the breastfeeding mothers, such as general health status (1 = very good, 5 = very poor), number of children, age of the youngest child, duration of breastfeeding of the youngest child, uptake of counseling on breastfeeding, and problems/difficulties experienced during breastfeeding. The second section included 18 questions regarding HM use (i.e., types and frequency of HM used, age of the child when HM was first used, indications and reasons for HM use, source of information and recommendation of HM, the experience of side effects, perceived safety and efficacy of HM, intention to recommend HM to other women, and disclosure and non-disclosure of HM use to health physicians and its reasons). Lastly, the final section consisted of eight questions on the participants’ sociodemographic characteristics such as age, level of education, occupation, number of family members in the household, household income, health insurance status, and marital status.
Statistical Analysis
In this study, the collected data of 372 participants were analyzed using Statistical Package for Social Sciences (SPSS) version 24.0. The descriptive statistics were used to examine the sociodemographic characteristics of the participants (i.e., age, education level, family size, occupation, marital status, number of assets, health insurance status, perceived health status, number of children, exclusive breastfeeding, and the types of breastfeeding problems). A Chi-square test was used to analyze the differences in sociodemographic characteristics between the users of HM during breastfeeding and the non-users. Only the statistically significant variables (i.e., education level, number of children, and low breastmilk supply) from previous chi-square analysis were analyzed using multivariate logistic regression analysis to identify the potential predictors of HM use among breastfeeding mothers.
Ethical Clearance
The study was approved by the Institutional Review Board on Human Subjects Research and Ethics Committees at Hanyang University Seoul, Korea (HYI-17-134-2). Formal permission was also obtained from Morogoro Municipal Council in Tanzania to carry out the study (E10/MMC-138/VOLIV/100).
Results
Sociodemographic Characteristics of Study Participants
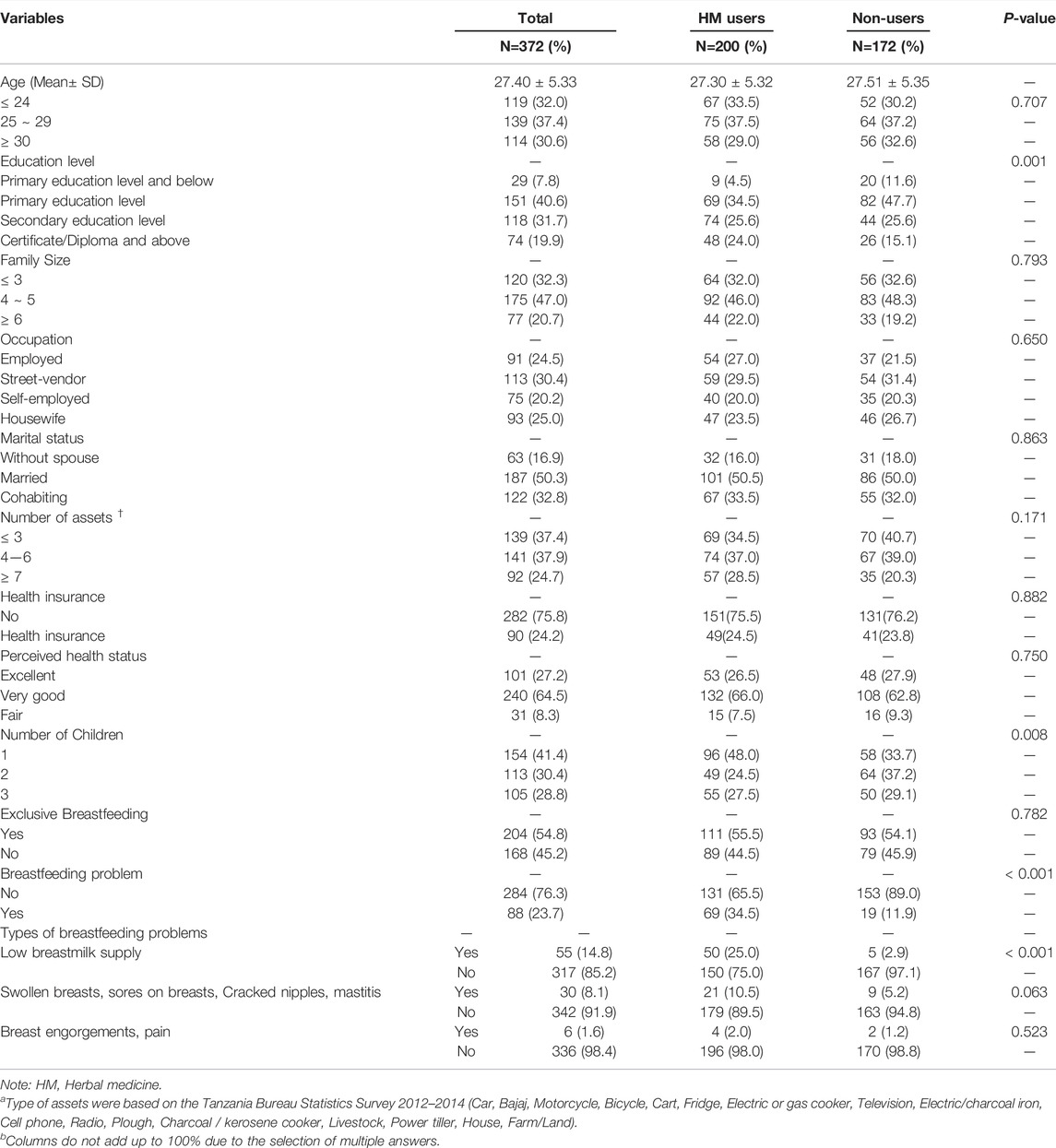
The details of the sociodemographic characteristics of respondents are shown in Table 1 The mean age of breastfeeding mothers was 27.4 ± 5.3 years. Most participants were secondary school graduates (31.7%), or had a certificate/diploma and above (19.9%), were married (50.3%), and did not have health insurance (75.8%). Mothers had one (41.4%) or two (30.4%) children, and 54.8% of respondents exclusively breastfed their children. Among the respondents, 23.7% reported having problems with breastfeeding, and low breastmilk supply (14.8%) was the most commonly reported problem. More than half (53.8%) of the respondents have used at least one of the HM modalities listed during breastfeeding. Significant differences found between HM users and non-users were education level (p = 0.001), number of children (p = 0.008), having breastfeeding problem (p < 0.001), and low breastmilk supply (p < 0.001).
Types of HM Modalities for Breastfeeding
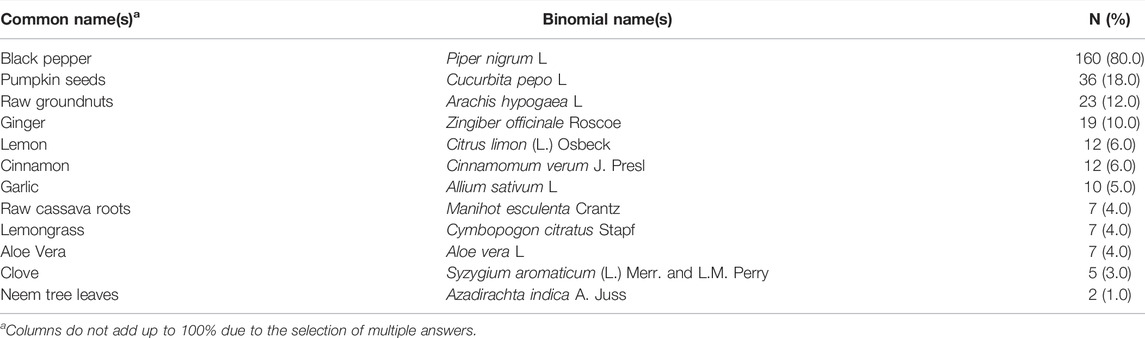
As presented in Table 2, the most commonly used HM modality was Piper nigrum L. (80.0%), followed by Cucurbita pepo L. (18.0%) and Arachis hypogaea L. (12.0%).
Source of Information on HM
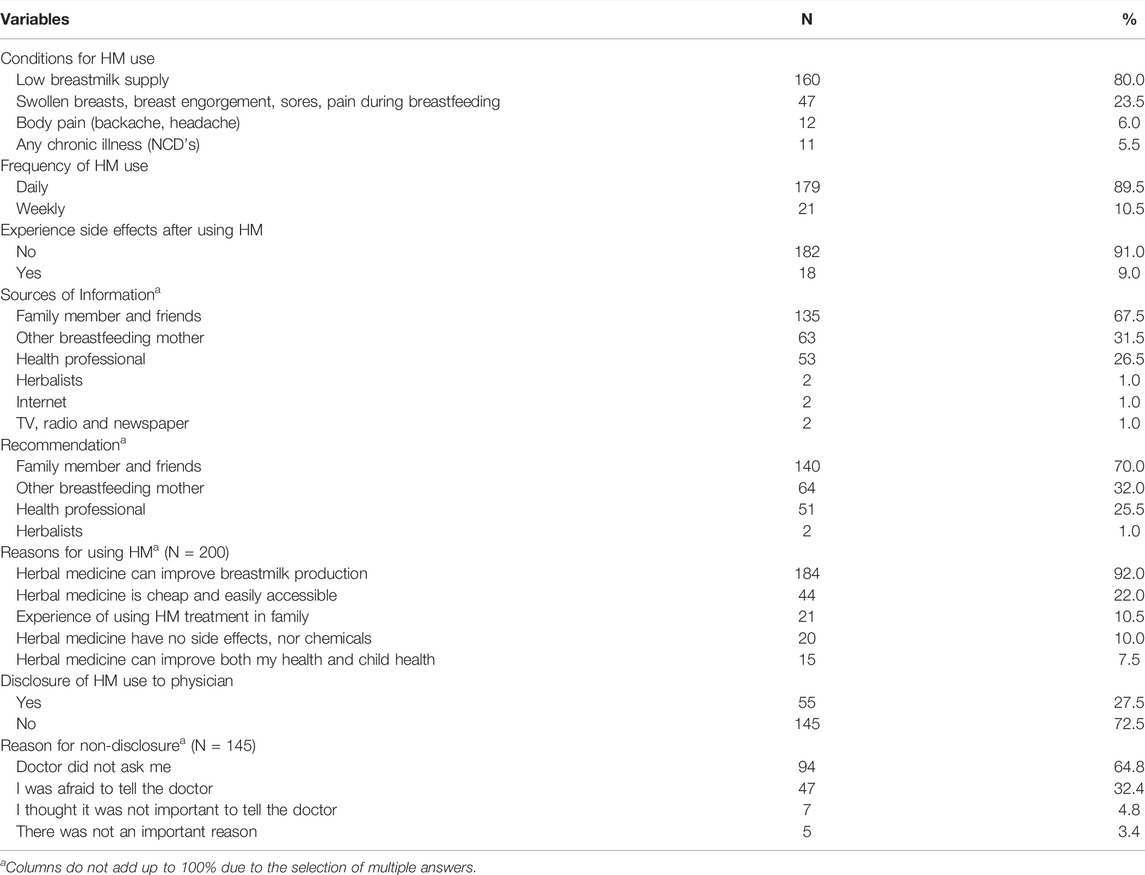
The primary information sources of HM use were family members and friends (67.5%) and other breastfeeding mothers (31.5%), 26.5% from healthcare professionals, and 1.0% from herbalists (Table 3).
Patterns of HM Use Among Participants
The experience and pattern of HM use during breastfeeding are presented in Table 3. The majority of HM users (89.5%) used the herbal products daily, and most women received recommendations on HM use from their family members and friends (70.0%). Among the HM users, 9.0% reported to have experienced side effects such as nausea, abdominal pain, and diarrhea. The most frequently reported reason for using HM during breastfeeding was the belief in improving low breastmilk supply (92.0%). A smaller proportion of HM users believed that HM does not cause side effects nor contains chemicals (10.0%). Among 200 participants using HM, 145 (72.5%) did not disclose their use to physicians, and the most common reasons for non-disclose were lack of physician inquiry (64.8%) and women’s fear of the doctor’s response (32.4%).
Potential Predictors of HM Use During Breastfeeding
The findings from multivariate logistic regression analysis are presented in Table 4. An education level of certificate/diploma and above (OR: 7.447, CI: 2.492–22.252, p < 0.001), secondary education level (OR: 5.524, CI: 1.943–15.711, p = 0.001), primary education level (OR: 3.348, CI: 1.197–9.361, p = 0.021), and having low breast milk supply (OR: 13.758, CI: 5.022–37.689, p < 0.001) were associated with HM use during breastfeeding.

TABLE 4. Potential predictors of HM use among breastfeeding mothers using multivariate logistic regression analysis.
Discussion
This study explored the prevalence and determinants of HM use among breastfeeding mothers in Tanzania, and our results revealed the high popularity of HM use among nursing mothers. As previous studies found, globally, 37.0–97.3% of mothers use HM to ease breastfeeding problems (Sim et al., 2013; Aleandri et al., 2014; Bettiol et al., 2018b; James et al., 2019; Zheng et al., 2020). Such variations in utilization rate can be attributed to differences in how HM is defined in each study, as well as the differences in the public acceptance and availability of HM due to cultural influences (Sim et al., 2013; James et al., 2019). Considering the low prevalence of exclusive breastfeeding and lack of appropriate breastfeeding knowledge among Tanzanian women (Hashim et al., 2016; Hasselberg et al., 2016; Kaaya et al., 2021) due to various individual, socio-cultural, and environmental barriers (Agho et al., 2019; Mundagowa et al., 2021), appropriate use of HM as galactagogues can potentially allow the mothers to engage in optimal breastfeeding practices and act as a safe alternative to synthetic galactagogues (Penagos-Tabares et al., 2014; Jyotsna and Sameet, 2020).
Similar to the broad range observed in the prevalence of HM use, wide varieties of HM were used by breastfeeding mothers in different countries. In Tanzania, the most commonly used herbal products were P. nigrum and C. pepo, whereas in Sierra Leone, Cassia sieberiana DC. and Luffa acutangula (L.) Roxb. were the most popular (James et al., 2019). T. foenum-graecum and Z. officinale use was the highest during lactation in Australia (Sim et al., 2013), while Tetrapanax papyrifer (Hook) K. Koch and Vaccaria segetalis (Neck.) Garcke consumption were most prevalent in Macau (Zheng et al., 2020). Such differences in preferred modalities can be due to different cultural traditions, as each traditional medicine is rooted in varying climate settings and religious backgrounds (Jaiswal and Williams, 2017; Tesfahuneygn and Gebreegziabher, 2019; Zhang and Dong, 2020). In addition, differences in the main indications for use reported among the studies may explain variations in HM modalities observed. For example, in our study, the most reported indication for HM was poor milk production, yet, in the Italian study, the main indications for HM use were dermatological conditions such as preventing stretch marks and preparing nipples for breastfeeding (Aleandri et al., 2014). Furthermore, among the Macau women, the primary indications for use were in relation to modulating the amount of breastmilk produced and managing breast and nipple pain (Zheng et al., 2020). These findings indicate that variations in the types of HM used can be expected depending on women’s cultural background and main indications for use (Forinash et al., 2012; Budzynska et al., 2013).
The procedures for preparing herbal remedies also vary by cultural background. P. nigrum, used by 80% of mothers in this study, is considered a medicinal plant in various cultures (Jamal et al., 2011; Takooree et al., 2019) and is specifically used to promote breastmilk production and postpartum care in India, Indonesia, and Morocco (Ramarao et al., 2000; Buragohain, 2008; Bnouham, 2010; Dandotiya et al., 2013; Chellappandian et al., 2014; Goyal, 2017; Muslichah et al., 2021). Depending on the cultural tradition, P. nigrum’s fruits are often mixed with other herbs (i.e., Terminalia chebula Retz., Piper longum L., Zingiber officinale Rosc., Curcuma aeruginosa Roxb., and Piper betel L.) and prepared as herbal concoctions to be consumed as galactagogue (Jyotsna and Sameet, 2020; Muslichah et al., 2021). Although not native to Africa, P. nigrum is also cultivated in East, Central, and West African regions and is often used as food condiments, insecticides, and cold-remedy (Kuete, 2017). It is also considered a galactagogue in places, and lactating mothers are recommended to consume a porridge with P. nigrum to promote breastmilk production (Hasselberg et al., 2016; Makwetta, 2021).
Nevertheless, despite women’s high dependency on HM to improve their breastfeeding due to the perception that HM is a natural and safe alternative to conventional medicine, HM’s clinical efficacy and safety as galactagogues still remain inconclusive and need further research (Sim et al., 2013; Zheng et al., 2020). For example, in the case of P. nigrum, its reputation as a lactogenic agent have received limited attention and relies on anecdotal evidence rather than clinical (Khare, 2007; Takooree et al., 2019). This may be because modalities such as P. nigrum are considered a food additive rather than a product with pharmacological value in many cultures, the importance of examining the effectiveness and potential dangers of such modalities can be neglected (Heinrich, 2016).
Although P. nigrum is better recognized for its anti-bacterial and anti-inflammatory effects in the existing literature, previous findings suggest its potential indirect effect as a galactagogue (Takooree et al., 2019). For instance, piperine, the active alkaloid contained in P. nigrum, improves the digestive capacity and enhances the bioavailability of drugs by increasing absorption activity in the intestines (Srinivasan, 2007; Goyal, 2017; Haq, et al., 2021) Piperine also possesses antioxidant properties which offer protection against oxidative stress by removing free radicals, reactive oxygen species, and chemical carcinogens (Srinivasan, 2007; Haq, et al., 2021). Managing postpartum oxidative stress is important as prolonged stress is involved in the pathogenesis of various maternal and neonatal diseases and can potentially alter the quality of breastmilk (Ozsurekci & Aykac, 2016; Kuramoto & Kitagawa, 2017). As consumption of balanced meals and proper nutrition is crucial for successful postpartum recovery and breastfeeding, piperine’s positive effect on the digestive tract, as well as the antioxidative effect may have helped the mothers to maintain good health and nutritional status to sustain optimal breastfeeding (Mistry & Williams, 2011; Goyal, 2017; Haq, et al., 2021). Nevertheless, as lactating mothers’ consumption of P. nigrum results in the transfer of piperine into the breastmilk, its potential effect on newborns warrants further investigation (N' Diaye et al., 2021).
Consumption of C. pepo was also prevalent among Tanzanian mothers. An animal study found that phytochemicals of C. pepo extract have a stimulatory effect on the pituitary gland, which stimulates prolactin secretion and increases the production of breast milk (Malgwi et al., 2013). However, further pharmacological research is required to ascertain their clinical efficacy in humans. As such, large-scale human clinical trials should be conducted for various traditional modalities to generate scientific evidence and demonstrate the safety and effectiveness of HM used among breastfeeding mothers (Jyotsna and Sameet, 2020).
In addition to the lack of scientific evidence to support HM’s effectiveness as galactagogues, the potential toxicity of HM due to heavy metal contamination is also a significant problem (Okem et al., 2014; Zhou et al., 2019; Luo et al., 2020). Because heavy metal components can pass through the breastmilk, inappropriate use of HM can expose infants to toxic substances (Palmieri et al., 2019). In fact, a study from Taiwan found that mothers’ consumption of Chinese herbal medicine was associated with the lead body burden in infants, posing potential health risks (Chien et al., 2006). The problems with contaminated HM have received considerable attention among academics and policymakers as HM is often obtained from unreliable sources such as local herbal shops and supermarkets; therefore, it is difficult to determine whether herbal products are manufactured and processed safely (Kunle et al., 2012; Sim et al., 2013; Aleandri et al., 2014). Thus, regulatory measures should be established to properly monitor the production of herbal products.
Lack of communication on HM use between the healthcare providers and nursing mothers is also a growing issue as poor communication can inhibit proper physician intervention when potential harm arises from inappropriate HM use (Foley et al., 2019). Congruent with previous findings, more than half of breastfeeding mothers in this study did not disclose their HM use to the doctors because the doctors did not ask and the women feared the doctors’ negative response (Foley et al., 2019; James et al., 2019). This implies that to prevent the potential risk of HM associated with inadequate patient-doctor communication, the physicians should actively inquire the nursing mothers about HM use and provide appropriate feedback to protect the health of the mothers and children.
Lastly, potential predictors of HM use identified in our sample include having low breastmilk supply and higher education attainment. Higher education level was frequently associated with the use of the non-conventional mode of care as people with higher education levels tend to have better health literacy, thus are more likely to practice patient autonomy and actively seek additional modes of care (Kemppainen et al., 2018; Fjær et al., 2020). Additionally, previous studies also found the age of the breastfeeding child, family income, ethnicity, previous use and positive attitudes towards non-conventional therapies, and the perceived accessibility of reliable information on HM use to be associated with HM use (Sim et al., 2013; Bettiol et al., 2018b; James et al., 2019; Zheng et al., 2020).
Several limitations can be found in this study. Because the study was conducted at a single health center, the views and opinions of study participants may not fully represent those of the other breastfeeding women. In addition, a recall bias can exist due to the retrospective design of the study. Lastly, cross-sectional data only provides information regarding the association between HM use and potential predictor variables. However, this is the first study to document the pattern of HM use among breastfeeding mothers in Tanzania and identify the factors that are significantly associated with HM use.
Conclusion
There is a high prevalence of HM use among breastfeeding mothers in Tanzania to overcome various problems with breastfeeding. Appropriate HM use can be used as one of the strategies to achieve EBF as it can help nursing mothers from resource-limited countries to tackle common breastfeeding challenges and practice optimal feeding behavior. However, the effectiveness and safety of the most commonly used HM among nursing mothers rely on anecdotal evidence rather than clinical, and this awakens the need to evaluate HM’s safety and efficacy through pharmacological studies for scientific evidence. In addition, despite the popular use of HM among nursing mothers, no guideline has been established in clinical settings to promote open dialogues between the healthcare providers and mothers to ensure the safe use of HM. This puts emphasis on the development of public awareness program to encourage active patient-physician communication and facilitate proper HM use.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by Institutional Review Board on Human Subjects Research and Ethics Committees, Hanyang University (HYI-17-134-2); Morogoro Municipal Council in Tanzania (E10/MMC-138/VOLIV/100). The patients/participants provided their written informed consent to participate in this study.
Author Contributions
VM, JH, and DH were responsible for the study concept and design. HI, JH, SC, and DH analyzed the data and drafted the manuscript. VM, JH, and DH contributed to the designing of data collection tools and data collection. VM, HI, JH, SC, and DH critically reviewed the manuscript and contributed intellectual content. All authors read and approved the final manuscript.
Funding
This study was funded by the 2015-2017 Korea International Cooperation Agency (KOICA) Scholarship Program and supported by the Hanyang Master’s Degree Program in the Department of Global Health and Development at Hanyang University (National Health Policy).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
The authors would like to express their sincere gratitude to all the participants for their cooperation and willingness to share their experiences.
Abbreviations
HM, herbal medicine; WHO, world health organization; EBF, exclusive breastfeeding.
References
Adane, F., Seyoum, G., Alamneh, Y. M., Abie, W., Desta, M., and Sisay, B. (2020). Herbal Medicine Use and Predictors Among Pregnant Women Attending Antenatal Care in Ethiopia: a Systematic Review and Meta-Analysis. BMC Pregnancy Childbirth 20 (1), 157. doi:10.1186/s12884-020-2856-8
Agho, K. E., Ezeh, O. K., Ghimire, P. R., Uchechukwu, O. L., Stevens, G. J., Tannous, W. K., et al. (2019). Exclusive Breastfeeding Rates and Associated Factors in 13 "Economic Community of West African States" (ECOWAS) Countries. Nutrients 11 (12). doi:10.3390/nu11123007
Ahmed, M., Hwang, J. H., Choi, S., and Han, D. (2017). Safety Classification of Herbal Medicines Used Among Pregnant Women in Asian Countries: a Systematic Review. BMC Complement. Altern. Med. 17 (1), 489. doi:10.1186/s12906-017-1995-6
Ajetunmobi, O. M., Whyte, B., Chalmers, J., Tappin, D. M., Wolfson, L., Fleming, M., et al. (2015). Breastfeeding Is Associated with Reduced Childhood Hospitalization: Evidence from a Scottish Birth Cohort (1997-2009). J. Pediatr. 166 (3), 620–e624. doi:10.1016/j.jpeds.2014.11.013
Al Sabati, S. Y., and Mousa, O. (2019). Effect of Early Initiation of Breastfeeding on the Uterine Consistency and the Amount of Vaginal Blood Loss during Early Postpartum Period. Nur Prim. Care 3 (3), 1–6. doi:10.33425/2639-9474.1108
Aleandri, V., Bertazzoni, G., Romanzi, D., Vetrano, G., Durazzi, F., Mazzanti, G., et al. (2014). The Use of Herbal Products during Breastfeeding: a Study from a Public Italian Hospital. J. Food Process. Technol. 05 (8), 1. doi:10.4172/2157-7110.1000354
Amri, E., and Kisangau, D. P. (2012). Ethnomedicinal Study of Plants Used in Villages Around Kimboza forest reserve in Morogoro, Tanzania. J. Ethnobiol. Ethnomed. 8, 1. doi:10.1186/1746-4269-8-1
Anderson, P. O. (2017). Herbal Use during Breastfeeding. Breastfeed. Med. 12 (9), 507–509. doi:10.1089/bfm.2017.0150
Antonakou, A., Papoutsis, D., Panou, I., Chiou, A., and Matalas, A. L. (2013). Role of Exclusive Breastfeeding in Energy Balance and Weight Loss during the First Six Months Postpartum. Clin. Exp. Obstet. Gynecol. 40 (4), 485–488.
Augustino, S., and Gillah, P. R. (2005). Medicinal Plants in Urban Districts of Tanzania: Plants, Gender Roles and Sustainable Use. Int. Forest. Rev. 7 (1), 44–58. doi:10.1505/ifor.7.1.44.64157
Bettiol, A., Lombardi, N., Marconi, E., Crescioli, G., Bonaiuti, R., Maggini, V., et al. (2018a). The Impact of Previous Pregnancy Loss on Lactating Behaviors and Use of Herbal Medicines during Breastfeeding: a Post Hoc Analysis of the Herbal Supplements in Breastfeeding InvesTigation (HaBIT). Evid. Based Complement. Alternat. Med. 2018, 1035875. doi:10.1155/2018/1035875
Bettiol, A., Lombardi, N., Marconi, E., Crescioli, G., Bonaiuti, R., Maggini, V., et al. (2018b). The Use of Complementary and Alternative Medicines during Breastfeeding: Results from the Herbal Supplements in Breastfeeding InvesTigation (HaBIT) Study. Br. J. Clin. Pharmacol. 84 (9), 2040–2047. doi:10.1111/bcp.13639
Bnouham, M. (2010). Medicinal Plants with Potential Galactagogue Activity Used in the Moroccan Pharmacopoeia. J. Complement. Integr. Med. 7 (1). doi:10.2202/1553-3840.1268
Bowman, D. (2017). Does Herbal Medicine Assist Breastfeeding Mothers with an Insufficient Milk Supply? Aust. J. Herbal Med. 29 (1), 2–4.
Budzynska, K., Gardner, Z. E., Dugoua, J. J., Low Dog, T., and Gardiner, P. (2012). Systematic Review of Breastfeeding and Herbs. Breastfeed. Med. 7 (6), 489–503. doi:10.1089/bfm.2011.0122
Budzynska, K., Gardner, Z. E., Low Dog, T., and Gardiner, P. (2013). Complementary, Holistic, and Integrative Medicine: Advice for Clinicians on Herbs and Breastfeeding. Pediatr. Rev. 34 (8), 343–3. doi:10.1542/pir.34-8-343
Buragohain, J. (2008). Folk Medicinal Plants Used in Gynecological Disorders in Tinsukia District, Assam, India. Fitoterapia 79 (5), 388–392. doi:10.1016/j.fitote.2008.03.004
Butte, N. F., Lopez-Alarcon, M. G., and Garza, C.Expert Consultation on theOptimal Duration of Exclusive (2002). Nutrient Adequacy of Exclusive Breastfeeding for the Term Infant during the First Six Months of Life / Nancy F. Butte, Mardia G. Lopez-Alarcon. Cutberto GarzaGeneva: World Health Organization.
Chellappandian, M., Pandikumar, P., Mutheeswaran, S., Gabriel Paulraj, M., Prabakaran, S., Duraipandiyan, V., et al. (2014). Documentation and Quantitative Analysis of Local Ethnozoological Knowledge Among Traditional Healers of Theni District, Tamil Nadu, India. J. Ethnopharmacol. 154 (1), 116–130. doi:10.1016/j.jep.2014.03.028
Chien, L. C., Yeh, C. Y., Lee, H. C., Jasmine Chao, H., Shieh, M. J., and Han, B. C. (2006). Effect of the Mother's Consumption of Traditional Chinese Herbs on Estimated Infant Daily Intake of lead from Breast Milk. Sci. Total Environ. 354 (2-3), 120–126. doi:10.1016/j.scitotenv.2005.01.033
Dandotiya, H., Singh, G., and Kashaw, S. (2013). The Galactagogues Used by Indian Tribal Communities to Overcome Poor Lactation. Int. J. Biotechnol. Bioeng. Res. 4 (3), 243–248.
Ebina, S., and Kashiwakura, I. (2012). Influence of Breastfeeding on Maternal Blood Pressure at One Month Postpartum. Int. J. Womens Health 4, 333–339. doi:10.2147/ijwh.S33379
Fjær, E. L., Landet, E. R., McNamara, C. L., and Eikemo, T. A. (2020). The Use of Complementary and Alternative Medicine (CAM) in Europe. BMC Complement. Med. Ther. 20 (1), 108. doi:10.1186/s12906-020-02903-w
Foley, H., Steel, A., Cramer, H., Wardle, J., and Adams, J. (2019). Disclosure of Complementary Medicine Use to Medical Providers: a Systematic Review and Meta-Analysis. Sci. Rep. 9 (1), 1573. doi:10.1038/s41598-018-38279-8
Forinash, A. B., Yancey, A. M., Barnes, K. N., and Myles, T. D. (2012). The Use of Galactogogues in the Breastfeeding Mother. Ann. Pharmacother. 46 (10), 1392–1404. doi:10.1345/aph.1R167
Goyal, M. (2017). Use of Ethnomedicinal Plants for Prophylaxis and Management of Postpartum Complications Among the Marwari Community of Jodhpur District of Rajasthan. Food Qual. Saf. 1 (3), 203–210. doi:10.1093/fqsafe/fyx013
Haq, I. U., Imran, M., Nadeem, M., Tufail, T., Gondal, T. A., and Mubarak, M. S. (2021). Piperine: A Review of its Biological Effects. Phytother. Res. 35 (2), 680–700. doi:10.1002/ptr.6855
Hashim, T. H., Mgongo, M., Katanga, J., Uriyo, J. G., Damian, D. J., Stray-Pedersen, B., et al. (2016). Predictors of Appropriate Breastfeeding Knowledge Among Pregnant Women in Moshi Urban, Tanzania: a Cross-Sectional Study. Int. Breastfeed. J. 12, 11. doi:10.1186/s13006-017-0102-4
Hasselberg, M., Huus, K., and Golsäter, M. (2016). Breastfeeding Preterm Infants at a Neonatal Care Unit in Rural Tanzania. J. Obstet. Gynecol. Neonatal. Nurs. 45 (6), 825–835. doi:10.1016/j.jogn.2016.07.010
Hauck, F. R., Thompson, J. M., Tanabe, K. O., Moon, R. Y., and Vennemann, M. M. (2011). Breastfeeding and Reduced Risk of Sudden Infant Death Syndrome: a Meta-Analysis. Pediatrics 128 (1), 103–110. doi:10.1542/peds.2010-3000
Heinrich, M. (2016). “Food-Herbal Medicine Interface,” in Encyclopedia of Food and Health. Editors B. Caballero, P. M. Finglas, and F. Toldrá (Oxford: Academic Press), 94–98. doi:10.1016/b978-0-12-384947-2.00772-8
Jaiswal, Y. S., and Williams, L. L. (2017). A Glimpse of Ayurveda - the Forgotten History and Principles of Indian Traditional Medicine. J. Tradit. Complement. Med. 7 (1), 50–53. doi:10.1016/j.jtcme.2016.02.002
Jamal, J. A., Ghafar, Z. A., and Husain, K. (2011). Medicinal Plants Used for Postnatal Care in Malay Traditional Medicine in the Peninsular Malaysia. Pharmacognosy J. 3 (24), 15–24. doi:10.5530/pj.2011.24.4
James, P. B., Kaikai, A. I., Bah, A. J., Steel, A., and Wardle, J. (2019). Herbal Medicine Use during Breastfeeding: a Cross-Sectional Study Among Mothers Visiting Public Health Facilities in the Western Area of Sierra Leone. BMC Complement. Altern. Med. 19 (1), 66. doi:10.1186/s12906-019-2479-7
Johnson, K. (2013). Maternal-Infant Bonding: A Review of Literature. Int. J. Childbirth Educ. 28 (3).
Jyotsna, T., and Sameet, M. (2020). An Ayurvedic and Contemprory Overveiw of Lactation Insufficiency and its Cure: a Conceptual Approach. World J. Phar. Res. 9 (6), 1185–1195. doi:10.20959/wjpr20206-17679
Kaaya, E. S., Ko, J., and Luhanga, E. (2021). Maternal Knowledge-Seeking Behavior Among Pregnant Women in Tanzania. Womens Health (Lond) 17, 17455065211038442. doi:10.1177/17455065211038442
Kacholi, D. S., and Amir, H. M. (2022). Ethnobotanical Survey of Medicinal Plants Used by Traditional Healers in Managing Gonorrhoea and Syphilis in Urambo District, Tabora Region, Tanzania. J. Herbs, Spices Med. Plants 28, 179–192. doi:10.1080/10496475.2022.2035476
Kemppainen, L. M., Kemppainen, T. T., Reippainen, J. A., Salmenniemi, S. T., and Vuolanto, P. H. (2018). Use of Complementary and Alternative Medicine in Europe: Health-Related and Sociodemographic Determinants. Scand. J. Public Health 46 (4), 448–455. doi:10.1177/1403494817733869
Kuete, V. (2017). Medicinal Spices and Vegetables from Africa: Therapeutic Potential against Metabolic, Inflammatory, Infectious and Systemic Diseases. Academic Press.
Kunle, O. F., Egharevba, H. O., and Ahmadu, P. O. (2012). Standardization of Herbal Medicines - A Review. Int. J. Biodvers. Conserv. 4 (3), 101–112. doi:10.5897/IJBC11.163
Kuramoto, N., and Kitagawa, M. (2017). Evaluation of Oxidative Stress, Antioxidant Power, and Antioxidant Potential of Breastmilk of Breast-Feeding Mothers. Health 9 (8), 1145–1158. doi:10.4236/health.2017.98083
Liu, J., Leung, P., and Yang, A. (2013). Breastfeeding and Active Bonding Protects against Children's Internalizing Behavior Problems. Nutrients 6 (1), 76–89. doi:10.3390/nu6010076
Luo, L., Wang, B., Jiang, J., Fitzgerald, M., Huang, Q., Yu, Z., et al. (2020). Heavy Metal Contaminations in Herbal Medicines: Determination, Comprehensive Risk Assessments, and Solutions. Front. Pharmacol. 11, 595335. doi:10.3389/fphar.2020.595335
Malgwi, I., Olorunshola, K., Hamman, W., and Eze, E. (2013). The Study of Effect of Aqueous Cucurbita Pepo Linn Seed Extract on Serum Prolactin Level of Lactating Female Albino Rats. Sci. J. Med. Sci. 2 (3), 21–26.
Mikšić, Š., Uglešić, B., Jakab, J., Holik, D., Milostić Srb, A., and Degmečić, D. (2020). Positive Effect of Breastfeeding on Child Development, Anxiety, and Postpartum Depression. Ijerph 17 (8), 2725. doi:10.3390/ijerph17082725
Mistry, H. D., and Williams, P. J. (2011). The Importance of Antioxidant Micronutrients in Pregnancy. Oxid. Med. Cel. Longev. 2011, 841749. doi:10.1155/2011/841749
Moini Jazani, A., Hamdi, K., Tansaz, M., Nazemiyeh, H., Sadeghi Bazargani, H., Fazljou, S. M. B., et al. (2018). Herbal Medicine for Oligomenorrhea and Amenorrhea: a Systematic Review of Ancient and Conventional Medicine. Biomed. Res. Int. 2018, 3052768. doi:10.1155/2018/3052768
Moshi, M. J., Otieno, D. F., Mbabazi, P. K., and Weisheit, A. (2009). The Ethnomedicine of the Haya People of Bugabo ward, Kagera Region, north Western Tanzania. J. Ethnobiol. Ethnomed. 5, 24. doi:10.1186/1746-4269-5-24
Mundagowa, P. T., Chadambuka, E. M., Chimberengwa, P. T., and Mukora-Mutseyekwa, F. N. (2021). Barriers and Facilitators to Exclusive Breastfeeding Practices in a Disadvantaged Community in Southern Zimbabwe: A Maternal Perspective. Wn 12 (1), 73–91. doi:10.26596/wn.202112173-91
Muslichah, S., Azrianingsih, R., Indriyani, S., and Arumingtyas, E. L. (2021). Ethnobotanical Study of Postnatal Medicinal Plants in the Ethnic Madurese in Bangkalan Regency, East Java, Indonesia. Ijfmt 15 (3), 4247–4255. doi:10.37506/ijfmt.v15i3.15960
Ngoma, C. M., and Siachapa, B. (2017). "Use of Herbal Medicines to Induce Labour by Pregnant Women: A Systematic Review of Literature". Jojnhc 2 (3), 1–5. doi:10.19080/JOJNHC.2017.02.555590
N´Diaye, K., Debong, M., Behr, J., Dirndorfer, S., Duggan, T., Beusch, A., et al. (2021). Dietary Piperine Is Transferred into the Milk of Nursing Mothers. Mol. Nutr. Food Res. 65 (23), 2100508. doi:10.1002/mnfr.202100508
Oguchi, S., Shinohara, K., Yamashiro, Y., Walker, W. A., and Sanderson, I. R. (1997). Growth Factors in Breast Milk and Their Effect on Gastrointestinal Development. Zhonghua Min Guo Xiao Er Ke Yi Xue Hui Za Zhi 38 (5), 332–337. doi:10.7097/APS.199710.0332
Okem, A., Southway, C., Stirk, W. A., Street, R. A., Finnie, J. F., and Van Staden, J. (2014). Heavy Metal Contamination in South African Medicinal Plants: A Cause for Concern. South Afr. J. Bot. 93, 125–130. doi:10.1016/j.sajb.2014.04.001
Orabi, A. M., Alharbi, R., and Abdulkhaleg, N. (2020). Exploring Awareness and Attitudes of Nurses towards Herbal Medicine Use during Pregnancy and Breastfeeding. Ajhse 1 (2), 52–65. doi:10.52417/ajhse.v1i2.82
Ozsurekci, Y., and Aykac, K. (2016). Oxidative Stress Related Diseases in Newborns. Oxid. Med. Cel. Longev. 2016, 2768365. doi:10.1155/2016/2768365
Palmieri, J. R., Meacham, S., Brunette, J., Miluski, T., Dhanju, S., and Stein, S. (2019). Effects Heavy Metal and Organic Contaminants during Pregnancy and Lactation on Child Health. JTO. Clin. Res. Rep. 2, 26–34.
Penagos Tabares, F., Bedoya Jaramillo, J. V., and Ruiz-Cortés, Z. T. (2014). Pharmacological Overview of Galactogogues. Vet. Med. Int. 2014, 1–20. doi:10.1155/2014/602894
Ramarao, N., Rajendran, A., and Henry, A. N. (2000). Increasing the Secretion of Breast Milk-Indigenous Practices in Andhra Pradesh. Anc. Sci. Life 19 (3-4), 176–178.
Sibeko, L., Johns, T., and Cordeiro, L. S. (2021). Traditional Plant Use during Lactation and Postpartum Recovery: Infant Development and Maternal Health Roles. J. Ethnopharmacol. 279, 114377. doi:10.1016/j.jep.2021.114377
Sim, T. F., Sherriff, J., Hattingh, H. L., Parsons, R., and Tee, L. B. (2013). The Use of Herbal Medicines during Breastfeeding: a Population-Based Survey in Western Australia. BMC Complement. Altern. Med. 13, 317. doi:10.1186/1472-6882-13-317
Srinivasan, K. (2007). Black Pepper and its Pungent Principle-Piperine: a Review of Diverse Physiological Effects. Crit. Rev. Food Sci. Nutr. 47 (8), 735–748. doi:10.1080/10408390601062054
Sumankuuro, J., Soyen, C., Crockett, J., Ibrahim, M., Ngmenkpieo, F., and Wulifan, J. K. (2020). Women's Motivation and Associated Factors for Herbal Medicine Use during Pregnancy and Childbirth: A Systematic Review. Health 12 (06), 572–597. doi:10.4236/health.2020.126044
Takooree, H., Aumeeruddy, M. Z., Rengasamy, K. R. R., Venugopala, K. N., Jeewon, R., Zengin, G., et al. (2019). A Systematic Review on Black Pepper (Piper Nigrum L.): from Folk Uses to Pharmacological Applications. Crit. Rev. Food Sci. Nutr. 59 (Suppl. 1), S210–s243. doi:10.1080/10408398.2019.1565489
Tesfahuneygn, G., and Gebreegziabher, G. (2019). Medicinal Plants Used in Traditional Medicine by Ethiopians: A Review Article. J. Respir. Med. Lung Dis. 4 (1), 1–3.
Wagner, E. A., Chantry, C. J., Dewey, K. G., and Nommsen-Rivers, L. A. (2013). Breastfeeding Concerns at 3 and 7 Days Postpartum and Feeding Status at 2 Months. Pediatrics 132 (4), e865–75. doi:10.1542/peds.2013-0724
Wang, J., Liu, J., Ni, X., Nie, G., Zeng, Y., Cao, X., et al. (2018a). Adjuvant Therapy of Oral Chinese Herbal Medicine for Menopausal Depression: a Systematic Review and Meta-Analysis. Evid. Based Complement. Alternat. Med. 2018, 7420394. doi:10.1155/2018/7420394
Wang, S., Zhang, C., Li, C., Li, D., He, P., Su, Z., et al. (2018b). Efficacy of Chinese Herbal Medicine Zengru Gao to Promote Breastfeeding: a Multicenter Randomized Controlled Trial. BMC Complement. Altern. Med. 18 (1), 53. doi:10.1186/s12906-018-2121-0
WHO (2015). Advocacy Strategy: Breastfeeding Advocacy Initiative, for the Best Start in Life. Geneva: World Health Organization.
Zhang, N., and Dong, M. (2020). Translation Strategies of Traditional Chinese Medicine Terms from the Perspective of Cross-Culture Communication. OALib 07 (10), 1–7. doi:10.4236/oalib.1106828
Zheng, T., Chen, W., Hu, H., Wang, Y., Harnett, J. E., and Ung, C. O. L. (2020). The Prevalence, Perceptions and Behaviors Associated with Traditional/complementary Medicine Use by Breastfeeding Women Living in Macau: a Cross-Sectional Survey Study. BMC Complement. Med. Ther. 20 (1), 122. doi:10.1186/s12906-020-02921-8
Zheng, T., Yao, D., Chen, W., Hu, H., Ung, C. O. L., and Harnett, J. E. (2019). Healthcare Providers' Role Regarding the Safe and Appropriate Use of Herbal Products by Breastfeeding Mothers: A Systematic Literature Review. Complement. Ther. Clin. Pract. 35, 131–147. doi:10.1016/j.ctcp.2019.01.011
Keywords: herbal medicine, breastfeeding, health behavior, tanzania, cross-sectional study
Citation: Millinga VP, Im HB, Hwang JH, Choi SJ and Han D (2022) Use of Herbal Medicines Among Breastfeeding Mothers in Tanzania: A Cross-Sectional Study. Front. Pharmacol. 13:751129. doi: 10.3389/fphar.2022.751129
Received: 31 July 2021; Accepted: 30 March 2022;
Published: 28 April 2022.
Edited by:
Titilayo Fakeye, University of Ibadan, NigeriaReviewed by:
Armando Caceres, Universidad de San Carlos de Guatemala, GuatemalaZohreh Mahmoodi, Alborz University of Medical Sciences, Iran
Copyright © 2022 Millinga, Im, Hwang, Choi and Han. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Dongwoon Han, ZHdoYW5AaGFueWFuZy5hYy5rcg==
 Valeria Phelician Millinga
Valeria Phelician Millinga Hyea Bin Im
Hyea Bin Im Jung Hye Hwang1,2,3
Jung Hye Hwang1,2,3 Soo Jeung Choi
Soo Jeung Choi Dongwoon Han
Dongwoon Han