- 1National Clinical Research Center of Geriatric Diseases, Chinese PLA General Hospital, Beijing, China
- 2Department of Hematology, Fifth Medical Center of Chinese PLA General Hospital, Beijing, China
- 3Department of Thoracic Surgery, First Medical Center, General Hospital of PLA, Beijing, China
- 4Department of Emergency, First Medical Center of Chinese PLA General Hospital, Beijing, China
- 5Department of Emergency, Hainan Hospital of Chinese PLA General Hospital, Sanya, China
- 6Department of General Medicine, First Medical Center of General Hospital of People’s Liberation Army, Beijing, China
- 7Hospital Management Institute, Medical innovation research department, Chinese PLA General Hospital, Beijing, China
- 8Department of General Medicine, Hainan Hospital of General Hospital of People’s Liberation Army, Beijing, China
- 9State Key Laboratory of Kidney Diseases, National Clinical Research Center of Kidney Diseases, General Hospital of People’s Liberation Army, Beijing, China
Objective: This study aimed to explore the effectiveness of sodium bicarbonate (SB) administration on mortality in septic patients with acute moderate lactic acidosis (MLA).
Methods: The large ICU database (MIMIC-IV) was retrospectively analyzed. Patients with sepsis and acute MLA were identified. Propensity score analysis (PSA) was performed to explain baseline differences in the probability of accepting or not accepting SB. The edge structured cox model (MSCM) was used to adjust for baseline and time-varying confounding variables. The primary outcome was the ICU and hospital mortality. The subgroup of septic shock was also investigated.
Results: A total of 512 septic patients with acute MLA were identified in this study, including 160 in the SB group and 352 in the non-SB group. In the PSA, SB administration was associated with reduced ICU (HR .58, 95% CI 0.38–.89; p <.05) and hospital (HR .67, 95% CI 0.47–.95; p <.05) mortality in septic patients with acute MLA. In the subgroup, the results were similar with septic patients. In the MSCM, SB administration could also improve the ICU (HR .35, 95% CI 0.16–.75; p <.01) and (HR .50, 95% CI 0.28–.88; p <.05) mortality on septic patients. However, In the subgroup, SB administration could only be found associated with improved hospital (HR .44, 95% CI 0.20–.97; p <.05) survival in septic shock.
Conclusion: SB administration treatment could reduce ICU and hospital mortality of septic patients with acute MLA. Meanwhile, it could also improve hospital survival in the subgroup of septic shock patients with acute MLA.
Introduction
Sepsis are major health care problems in the intensive care unit (ICU), affecting millions of people worldwide every year, of which one-third to one-sixth die (Fleischmann et al., 2016; Rhee et al., 2017; Fleischmann-Struzek et al., 2020). Lactic acidosis, as one of the most common types of moderate lactic acidosis, was also commonly observed in sepsis with a strikingly high mortality according to the different definitions (Luft et al., 1983; Fall and Szerlip, 2005). Early and appropriate treatment after sepsis and lactic acidosis could improve the prognosis.
Sodium bicarbonate solution (SB) is commonly applied in fluid resuscitation and correcing the disorders of acid and base in the early stage after sepsis. While SB therapy was widely investigated for its relationship with mortality in severe septic patients (Ganesh et al., 2016; Jaber et al., 2018; Zhang et al., 2018; Fujii et al., 2021; Yagi and Fujii, 2021), sepsis with lactic acidosis has been less well investigated. Only two small RCTs have compared the effects of sodium bicarbonate and equimolar saline in treating lactic acidosis and no difference was found in hemodynamic indicators or vasopressin consumption (Cooper et al., 1990; Mathieu et al., 1991). In the update of the Surviving Sepsis Campaign guidelines 2021, Evans et al. (2021) suggest against using SB treatment to make improvement in haemodynamics or to decrease the consumption of vasopressor for adults with septic shock and lactic acidemia induced by hypoperfusion (INVALID CITATION, 2018). However, the effect of SB therapy on death rate when used in most septic patients with moderate lactic acidosis (MLA) is still not known.
According to the aforementioned information, the purpose of our study was exploring the effects of SB administration on the death rate of the septic patients who had acute MLA and in the subgroup of septic shock. Since SB treatment is a time-weighted predictive factor which depends on bicarbonate concentration (BC), lactate, PaCO2 and pH in blood, the SB administration records, time-dependent covariates, and baseline data were explained by using the marginal structural cox model (MSCM) (Robins et al., 2000; de Keyser et al., 2014; Karim et al., 2014).
Materials and methods
The design of the research and database
A retrospective design and MIMIC-IV, v0.4 database were used., This research included 76540 critically ill patients from six ICUs in a single center institution (Beth Israel Deaconess Medical Center, bidmc; Boston, MA) between 2008 and 2019 (Johnson et al., 2016; Johnson et al., 2018; Johnson et al., 2020). Since the database we analyzed here has been approved for public use by the institutional review board (IRB), there is no need to additionally provide IRB approval.
Study cohort
All admissions in the MIMIC-IV database were included. Non-etheless, only the admissions to ICU recorded for the first time were used for the analysis (Zhang et al., 2018). Inclusion criteria: 1) sepsis was diagnosed on the admission to ICU; 2) onset of acute MMA (within a few days (Yagi and Fujii, 2021) with 7.2 ≤ pH < 7.3 and BC <20 mmol/L; 3) with lactate >2.2 mmol/L; 4) no respiratory acidosis (PaCO2 < 50 mmHg) (Zhang et al., 2018); 5) without stage 2 or 3 AKI (the diagnosis and staging of AKI was according to the level of serum creatinine following the Kidney Disease: Improving Global Outcomes) (Mathieu et al., 1991). Patients’ pH, BC, lactate, serum creatinine and PaCO2 were documented after admission to ICU within 48 h (Singer et al., 2016). The sepsis was defined as a condition with “life-threatening organ dysfunction caused by a dysregulated host response to infection” (Singer et al., 2016). If the results of various examination were documented, only the highest level of lactate and PaCO2, and the lowest level of pH and BC were utilized. We excluded the patients with cardiac arrest or ICU stay >100 days (Zhang et al., 2018).
Variables
The variables chosen from MIMIC-IV database were the data documented within 24 h after the patient was admitted to the ICU, including sex, body mass index (BMI), age, comorbidity after admission to ICU, mechanical ventilation, and vasopressor consumption. Acute kidney injury (AKI) was defined according to the Kidney Disease: Improving Global Outcomes (Kellum and Lameire, 2013). The shock index (shock index >1.0) was used to evaluate the degree of shock on the first day of admission to ICU (Allgöwer and Burri, 1946). Lactate solution treatment in the first 24 h was also taken into account. In the establishment of the mixed-effects model, the admission year was used as a random factor (SerpaNeto et al., 2018).
Laboratory indicators including pH, lactate, PaCO2, and BC were documented during the whole period of ICU stay. The result and examination time of the lab tests were extracted from the MIMIC-IV. If the test was conducted for more than one time, the highest PaCO2 and lactate values, and the lowest pH and BC values every day were used in the analysis.
Outcome measures
The primary outcome measure was the mortality of the patients during hospital stay. The survival rate when patients were discharged from the hospital were also an outcome measure.
Statistical analysis
The cohorts were assigned into intervention (SB) and control (non-SB) group based on SB treatment during the first 48 h after the admission to ICU. Continuous variables were presented as median value with interquartile range (IQR) or mean value with standard deviation. Mann-Whitney U test or Student’s t-test was utilized to make comparison between groups. Categorical data were presented as relative frequency (%) and absolute frequency (n). Fisher’s exact test or Chi-square test was employed to analyze the data.
The baseline differences in the possibility of applying SB treatment were explained by using the propensity score analysis (PSA) (Zhang, 2017). In PSA, the patients in SB group were given SB during the first 48 h of ICU stay. The data in PSA are presented in Table 1. The propensity scores of the two groups were matched by using the nearest neighbor method. The parameters (p < .05) were used to adjust the residual imbalance in Cox regression model. Clinical professionals were consulted to determine the possible confounders.
SB therapy during ICU stay was a time-weighted variable in MSCM. Sex, BMI, age, comorbidities, mechanical ventilation application and vasopressor were possible confounders at baseline. These data were documented during the first 24 h of ICU stay. BC, pH, lactate, and PaCO2 tested during ICU stay varied with time increased. The selection and confounding bias resulted from informative censoring were corrected by using “ipw” package (version 1.0-11) and Inverse probability weighting estimation in the R (version 4.0.0) (Robins et al., 2000). The variables used in MSCM were list in the Supplementary Tables S8–S10.
There were missing data on (<25%) pH, PaO2, BMI, PaCO2 and shock index (Supplementary Table S1). Various imputation procedures were used for these missing variables. Multiple imputation was carried out using the prediction mean matching method of continuous variables and the logistic regression method of categorical data, and 5 databases were established. After multiple imputation, the multivariate model was replicated in 5 databases and the pooled results were obtained (SerpaNeto et al., 2018).
MSCM and PSA analyses were used to conduct subgroup analysis by grouping patients into septic shock patients with acute moderate lactic acidosis.
The statistical analyses were all conducted by applying R package (version 4.0.0). p < .05 was regarded as statistically significant different.
Results
Study cohort
A total of 512 septic patients from the MIMIC-IV were selected who had acute moderate lactic acidosis during the first 48 h of ICU stay. Among them, 160 patients underwent SB therapy during the first 48 h, and 352 patients didn’t underwent the therapy (Figure 1).
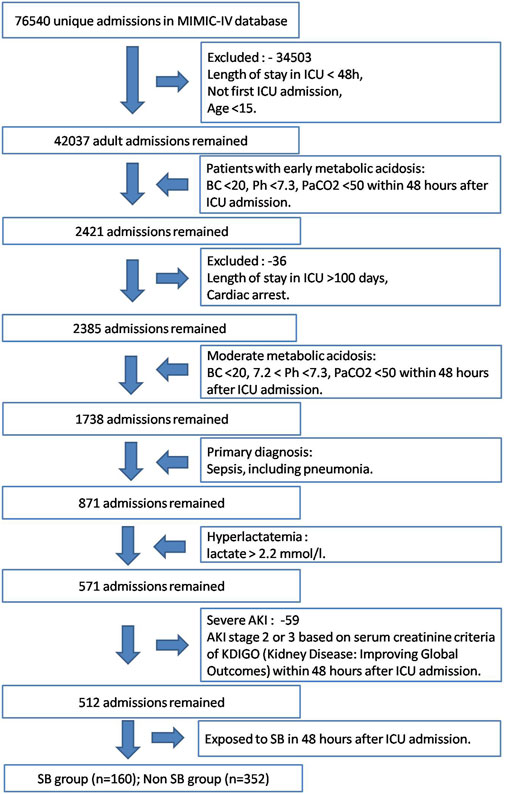
FIGURE 1. Study cohort selection workflow of MIMIC-IV database based on the designed inclusion and exclusion criteria.
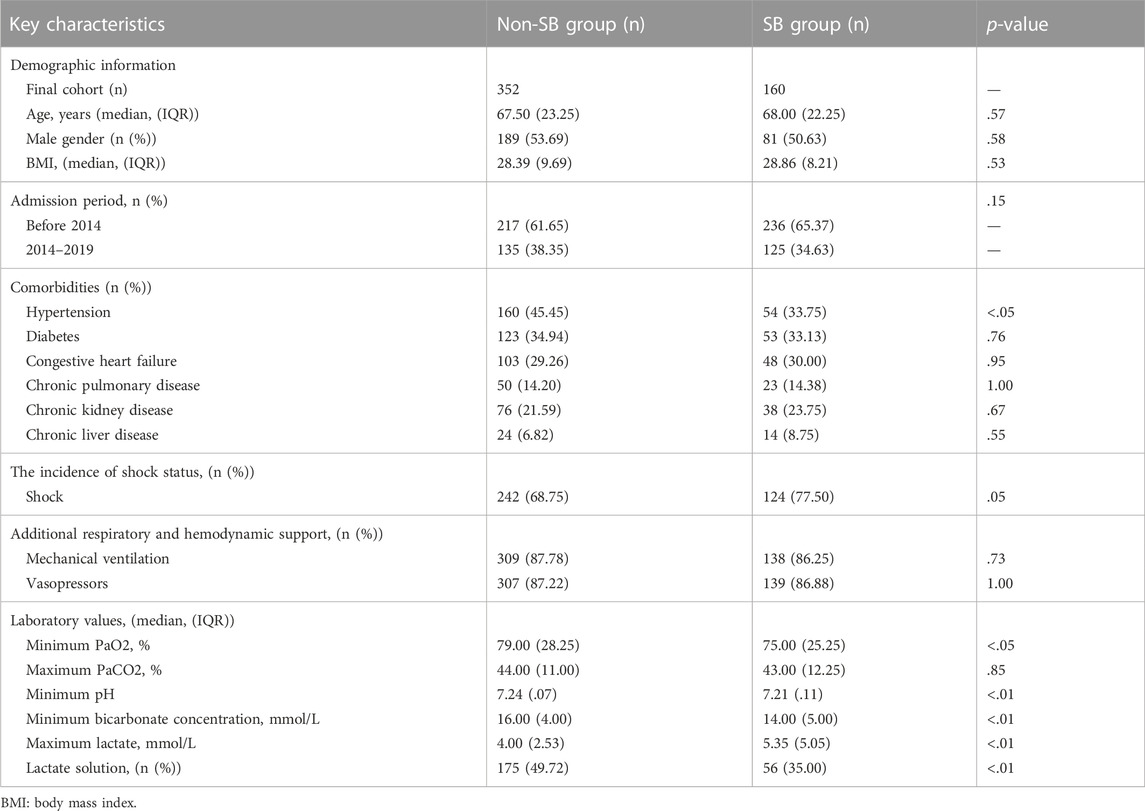
Table 1 presented the information in the two groups at baseline. The hypertension percentage was lower in SB group [54 (33.75%) vs. 160 (45.45%); p <.05] in comparison with non-SB group. In the first 24 h of ICU stay, the incidence of shock was higher in SB group [124 (77.50%) vs. 242 (68.75%); p = .05] compared with non-SB group. There was no statistically significant difference in mechanical ventilation application or vasopressors between SB and non-SB groups. The minimum pH [7.21 (.11) vs. 7.24 (.07), p <.01], PaO2 [75.00 (25.25) vs. 79.00 (28.25), p <.01] and BC [14.00 (5.00) vs. 16.00 (4.00), p <.01] were remarkably reduced, and lactate level was remarkably increased [5.35 (5.05) vs. 4.00 (2.53), p <.01] in SB group compared with the non-SB group. The application of lactate solution was markedly increased in the non-SB group [56 (35.00) vs. 175 (49.72); p <.01] in comparison with SB group. There was no statistically significant difference in admission period between the two groups. There was no participant having multiple times of admission in the cohort.
Propensity score analysis
In PSA, 160 patients from SB and 160 patients from non-SB groups were matched, and the imbalance between the two groups was largely improved (Supplementary Table S2). Cox proportional hazard model was applied due to the remaining imbalances. It was demonstrated that SB administration was highly related with decreased mortality of the septic patients with acute MLA in ICU (HR: .58; 95% CI: .38–.89; p <.05) and in hospital (HR: .67; 95% CI: .47–.95; p <.05) (Table 2; Table 3). In the subgroup of septic shock patients who had acute MLA, it was also presented that SB administration was in a close relationship with increased survival rate in ICU stay (HR: .53; 95% CI: .32–.89; p <.05) and hospital stay (HR: .58; 95% CI: .38–.89; p <.05) survival (Table 2; Table 3).

TABLE 2. Association of early sodium bicarbonate infusion and ICU mortality in the overall and subgroup by using propensity score analysis.

TABLE 3. Association of early SB infusion and hospital mortality in the overall and subgroups by using propensity score analysis.
Results of marginal structural cox model
SB administration and time-dependent confounding factors were analyzed by using MSCM. The results of MSCM demonstrated the relationships between SB administration and decreased mortality in ICU (HR: .35; 95% CI: .16–.75; p <.01) and hospital (HR: .50; 95% CI: .28–.88; p <.05) in the septic patients who had acute MLA (Figures 2, 3, Supplementary Table S3). In the subgroup (Figures 2, 3, Supplementary Table S4), significant association was only found between SB administration and reduced hospital mortality (HR: .44; 95% CI: .20–.97; p <.05), but not found with ICU mortality (HR: .50; 95% CI: .22–1.13; p = .10). The key factors of SB administration for predicting hospital and ICU mortality in septic patients with acute MLA, and for the mortality in hospital in septic patients who had acute MLA were showed in Supplementary Tables S5–S7. Meanwhile, the predictors of the use of sodium bicarbonate infusion at each time point during hospital and ICU stay in septic patients with acute MLA and during hospital stay in septic shock patients with acute MLA was showed in Supplementary Tables S8–S10.
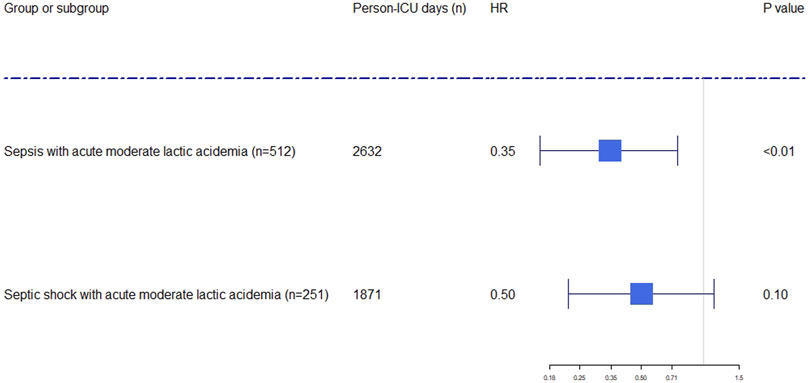
FIGURE 2. Forest plot showing the effect of sodium bicarbonate administration on ICU mortality in septic and septic shock patients with acute moderate lactic acidosis. The hazard ratios were estimated using the marginal structural cox model. Person-days were the days of ICU and hospital length of stay. The x-axis tick marks follow a logarithmic scale. HR: hazard ratio.
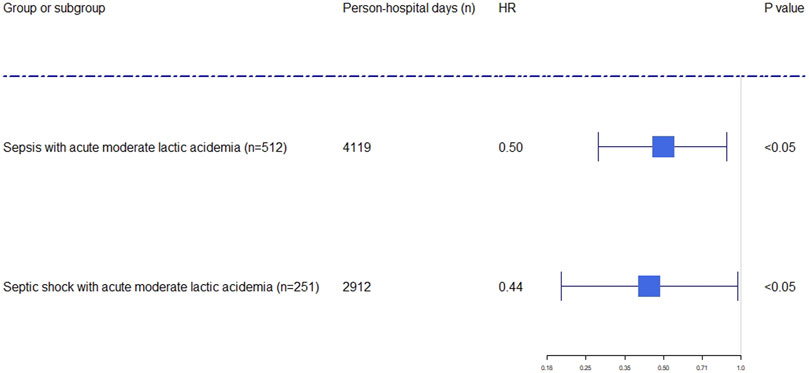
FIGURE 3. Forest plot showing the effect of sodium bicarbonate administration on hospital mortality in septic and septic shock patients with acute moderate lactic acidosis. The hazard ratios were estimated using the marginal structural cox model. Person-days were the days of ICU and hospital length of stay. The x-axis tick marks follow a logarithmic scale. HR: hazard ratio.
Discussion
According to our results, it was found that there was strong relationship between SB administration and decreased mortality during ICU and hospital stay in adult septic patients who had acute MLA. SB administration was also associated with reduced hospital mortality in septic shock patients who had acute MLA in the subgroup. Our research presented that lactic acidosis was commonly found in the patients at critically ill status who suffered from septic shock and sepsis, and SB administration was often employed in these patients, however, there was no sufficient evidence of the effect on mortality (Forsythe and Schmidt, 2000; Boyd and Walley, 2008; Evans et al., 2021). Hence, our study was the first proving that SB administration could improve the survival of septic patients who had acute MLA in both ICU and hospital, and also could reduce hospital mortality for septic shock patients who had acute MLA.
SB administration was extensively used in clinical practice for the treatment of severe moderate lactic acidosis in ICU(9). Nevertheless, no sufficient evidence was found to prove its effects on mortality in septic patients who had MLA. Cooper et al. (1990) presented that sodium bicarbonate therapy could elevate PCO2 and pH without benefits in cardiac output or blood pressure. Mathieu et al. (1991) could not found any change in hemodynamic parameters. In a retrospective observational study, Zhongheng Zhang et al. (2018) also did not find the significant improved effect on mortality rate for sepsis patients who had severe lactic acidosis. Current research showed that SB administration was not helpful to the sepsis patients who had acute MLA but was also related to improved clinical outcomes for septic shock patients. It was demonstrated by our study that SB therapy was advantageous for septic shock and sepsis patients who had acute MLA.
Based on the latest review, Kosuke Yagi and Tomoko Fujii concluded that the presence of moderate lactic acidosis was common in ICU, and the mortality was even higher in moderate lactic acidosis rather than severe sepsis (Yagi and Fujii, 2021). However, high quality evidence of SB administration for moderate lactic acidosis are still lacking. The standard practice of SB could be effective in both and moderate lactic acidosis. Our observations provided supportive proof that SB administration could be applied in sepsis patients who had acute MLA, especially in the patients suffering from septic shock.
There were some additional strengths in our study. Firstly, the data were extracted from the MIMIC-IV database which ensured high quality of the and a large cohort of patients. The possible relationship between SB therapy and mortality could be observed. Secondly, MSCM and PSA were used in this research to explain the data at baseline and the time-dependent confounders. Thirdly, the subgroup analysis was conducted and potent evidence was found in septic shock patients with acute MLA.
There were also limitations in this study. Firstly, the cohort in this study is only from one institution. Randomized controlled clinical trials could provide more persuasive evidence. Secondly, some data (liquid input and output, etc.) were missing due to the unavailability of data in the database. Thirdly, PSA and MSCM were applied to balance key confounding variables, however, residual confounding variables could not be completely avoided since the observational study design was adopted in this study. Fourth, the data collection time in MIMIC-IV was more than 10 years, during which there was a huge change in clinical care. Fifth, missing data was also a limitation. There was no difference in baseline data between the combined estimated and source datasets. Sixth, due to incorrect and missing data, sofa scores were not included in the evaluation variables. Other complete and correct variables, such as comorbidity, additional hemodynamic and respiratory support, which were closely related to the SOFA score evaluation, were used in the analysis. Seventh, the effect of SB treatment which as a time-weighted predictive factor was only observed focusing on the initial 48 h in this study, but not included other time windows that might also impact on mortality. Eighth, Multiple imputation can be quite different when it is applied to cross-sectional data or longitudinal data. Last, the findings of this research need to be further confirmed by rigorous clinical studies, such as randomized clinical trials.
Conclusion
SB therapy could decrease the mortality rate in hospital and ICU stay in septic patients who had acute MLA. Meanwhile, it could also improve hospital survival in the subgroup of septic shock patients with acute MLA. Randomized controlled clinical trials are further required to validate our findings.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding authors.
Ethics statement
Ethical review and approval was not required for the study on human participants in accordance with the local legislation and institutional requirements. The patients/participants provided their written informed consent to participate in this study.
Author contributions
SH and BY: Data curation, writing-original draft preparation. YP and QX: Visualization, investigation. LW, JW, and XZ: Software, validation. YY and LC: Supervision. CF: Conceptualization, methodology, software and writing-reviewing and editing.
Funding
We were grateful for the team of the Laboratory for Computational Physiology from the Massachusetts Institute of Technology (MIT-LCP) who kept the MIMIC databases. We also thank the support from the National Natural Science Fund (nos. 82072200, 82200169).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fphar.2022.1059285/full#supplementary-material
References
Allgöwer, M., and Burri, C. (1946). Shock index. Dtsch. Med. Wochenschr. 92 (43), 1947–1950. doi:10.1055/s-0028-1106070
Boyd, J. H., and Walley, K. R. (2008). Is there a role for sodium bicarbonate in treating lactic acidosis from shock? Curr. Opin. Crit. Care 14 (4), 379–383. doi:10.1097/MCC.0b013e3283069d5c
Cooper, D. J., Walley, K. R., Wiggs, B. R., and Russell, J. A. (1990). Bicarbonate does not improve hemodynamics in critically ill patients who have lactic acidosis. A prospective, controlled clinical study. Ann. Intern Med. 112 (7), 492–498. doi:10.7326/0003-4819-112-7-492
de Keyser, C. E., Leening, M. J., Romio, S. A., Jukema, J. W., Hofman, A., Ikram, M. A., et al. (2014). Comparing a marginal structural model with a cox proportional hazard model to estimate the effect of time-dependent drug use in observational studies: Statin use for primary prevention of cardiovascular disease as an example from the rotterdam study. Eur. J. Epidemiol. 29 (11), 841–850. doi:10.1007/s10654-014-9951-y
Evans, L., Rhodes, A., Alhazzani, W., Antonelli, M., Coopersmith, C. M., French, C., et al. (2021). Surviving sepsis campaign: International guidelines for management of sepsis and septic shock 2021. Intensive Care Med. 47 (11), 1181–1247. doi:10.1007/s00134-021-06506-y
Fall, P. J., and Szerlip, H. M. (2005). Lactic acidosis: From sour milk to septic shock. J. Intensive Care Med. 20 (5), 255–271. doi:10.1177/0885066605278644
Fleischmann, C., Scherag, A., Adhikari, N. K., Hartog, C. S., Tsaganos, T., Schlattmann, P., et al. (2016). Assessment of global incidence and mortality of hospital-treated sepsis. Current estimates and limitations. Am. J. Respir. Crit. Care Med. 193 (3), 259–272. doi:10.1164/rccm.201504-0781OC
Fleischmann-Struzek, C., Mellhammar, L., Rose, N., Cassini, A., Rudd, K. E., Schlattmann, P., et al. (2020). Incidence and mortality of hospital- and ICU-treated sepsis: Results from an updated and expanded systematic review and meta-analysis. Intensive Care Med. 46 (8), 1552–1562. doi:10.1007/s00134-020-06151-x
Forsythe, S. M., and Schmidt, G. A. (2000). Sodium bicarbonate for the treatment of lactic acidosis. Chest 117 (1), 260–267. doi:10.1378/chest.117.1.260
Fujii, T., Udy, A. A., Nichol, A., Bellomo, R., Deane, A. M., El-Khawas, K., et al. (2021). Incidence and management of metabolic acidosis with sodium bicarbonate in the ICU: An international observational study. Crit. Care 25 (1), 45. doi:10.1186/s13054-020-03431-2
Ganesh, K., Sharma, R. N., Varghese, J., and Pillai, M. G. (2016). A profile of metabolic acidosis in patients with sepsis in an Intensive Care Unit setting. Int. J. Crit. Illn. Inj. Sci. 6 (4), 178–181. doi:10.4103/2229-5151.195417
Jaber, S., Paugam, C., Futier, E., Lefrant, J. Y., Lasocki, S., Lescot, T., et al. (2018). Sodium bicarbonate therapy for patients with severe metabolic acidaemia in the intensive care unit (BICAR-ICU): A multicentre, open-label, randomised controlled, phase 3 trial. Lancet 392 (10141), 31–40. doi:10.1016/S0140-6736(18)31080-8
Johnson, A. B. L., Pollard, T., Horng, S., Celi, L. A., and Mark, R. MIMIC-IV. (ver- sion 0.4) 2020. Available at: https://www.physionet.org/.
Johnson, A. E., Pollard, T. J., Shen, L., Lehman, L. W., Feng, M., Ghassemi, M., et al. (2016). MIMIC-III, a freely accessible critical care database. Sci. Data 3, 160035. doi:10.1038/sdata.2016.35
Johnson, A. E., Stone, D. J., Celi, L. A., and Pollard, T. J. (2018). The MIMIC code repository: Enabling reproducibility in critical care research. J. Am. Med. Inf. Assoc. 25 (1), 32–39. doi:10.1093/jamia/ocx084
Karim, M. E., Gustafson, P., Petkau, J., Zhao, Y., Shirani, A., Kingwell, E., et al. (2014). Marginal structural Cox models for estimating the association between β-interferon exposure and disease progression in a multiple sclerosis cohort. Am. J. Epidemiol. 180 (2), 160–171. doi:10.1093/aje/kwu125
Kellum, J. A., and Lameire, N. (2013). Diagnosis, evaluation, and management of acute kidney injury: A KDIGO summary (Part 1). Crit. care (London, Engl. 17 (1), 204. doi:10.1186/cc11454
Luft, D., Deichsel, G., Schmülling, R. M., Stein, W., and Eggstein, M. (1983). Definition of clinically relevant lactic acidosis in patients with internal diseases. Am. J. Clin. Pathol. 80 (4), 484–489. doi:10.1093/ajcp/80.4.484
Mathieu, D., Neviere, R., Billard, V., Fleyfel, M., and Wattel, F. (1991). Effects of bicarbonate therapy on hemodynamics and tissue oxygenation in patients with lactic acidosis: A prospective, controlled clinical study. Crit. Care Med. 19 (11), 1352–1356. doi:10.1097/00003246-199111000-00008
Rhee, C., Dantes, R., Epstein, L., Murphy, D. J., Seymour, C. W., Iwashyna, T. J., et al. (2017). Incidence and trends of sepsis in US hospitals using clinical vs claims data, 2009-2014. Jama 318 (13), 1241–1249. doi:10.1001/jama.2017.13836
Robins, J. M., Hernán, M. A., and Brumback, B. (2000). Marginal structural models and causal inference in epidemiology. Epidemiology 11 (5), 550–560. doi:10.1097/00001648-200009000-00011
Serpa Neto, A., Deliberato, R. O., Johnson, A. E. W., Bos, L. D., Amorim, P., Pereira, S. M., et al. (2018). Mechanical power of ventilation is associated with mortality in critically ill patients: An analysis of patients in two observational cohorts. Intensive Care Med. 44 (11), 1914–1922. doi:10.1007/s00134-018-5375-6
Singer, M., Deutschman, C. S., Seymour, C. W., Shankar-Hari, M., Annane, D., Bauer, M., et al. (2016). The third international consensus definitions for sepsis and septic shock (Sepsis-3). Jama 315 (8), 801–810. doi:10.1001/jama.2016.0287
Yagi, K., and Fujii, T. (2021). Management of acute metabolic acidosis in the ICU: Sodium bicarbonate and renal replacement therapy. Crit. Care 25 (1), 314. doi:10.1186/s13054-021-03677-4
Zhang, Z. (2017). Propensity score method: A non-parametric technique to reduce model dependence. Ann. Transl. Med. 5 (1), 7. doi:10.21037/atm.2016.08.57
Keywords: acute moderate lactic acidosis, mortality, sodium bicarbonate administration, sepsis, septic shock
Citation: Huang S, Yang B, Peng Y, Xing Q, Wang L, Wang J, Zhou X, Yao Y, Chen L and Feng C (2023) Clinical effectiveness of sodium bicarbonate therapy on mortality for septic patients with acute moderate lactic acidosis. Front. Pharmacol. 13:1059285. doi: 10.3389/fphar.2022.1059285
Received: 01 October 2022; Accepted: 19 December 2022;
Published: 09 January 2023.
Edited by:
Hai Jin, Northern Theater General Hospital, ChinaReviewed by:
Zhongheng Zhang, Sir Run Run Shaw Hospital, ChinaMuaaz Alkhouli, Damascus University, Syria
Copyright © 2023 Huang, Yang, Peng, Xing, Wang, Wang, Zhou, Yao, Chen and Feng. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yuan Yao, eWFveXVhbjMwMUBzaW5hLmNu; Li Chen, Y2hlbmxpLWNoaW5hQDE2My5jb20=; Cong Feng, ZmMxOTRAMTYzLmNvbQ==
†These authors have contributed equally to this work and share first authorship
 Sai Huang
Sai Huang Bo Yang3†
Bo Yang3† Yaojun Peng
Yaojun Peng Cong Feng
Cong Feng