
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Pharmacol., 07 December 2022
Sec. Drugs Outcomes Research and Policies
Volume 13 - 2022 | https://doi.org/10.3389/fphar.2022.1041400
This article is part of the Research TopicEmerging Talents in Pharmacology: Drugs Outcomes Research and Policies 2022View all 8 articles
A commentary has been posted on this article:
Commentary: Effect of aspirin in patients with established asymptomatic carotid atherosclerosis: a systematic review and meta-analysis
Background: Aspirin is widely used as an antiplatelet agent for secondary prevention in patients with atherosclerotic cardiovascular disease. However, it remains unclear whether aspirin can prevent the progression of carotid atherosclerosis or reduce vascular events and all-cause death.
Methods: We performed a meta-analysis of the effect of aspirin in asymptomatic carotid atherosclerotic patients. Electronic databases including Pubmed, EMBase, ISI Web, Medline, Cochrane, and clinicaltrial.gov were searched for relevant randomized controlled trials. A total of five studies (841 individuals, 2,145 person-years) were included in this study. Two reviewers independently performed the study assessment and data extraction. Forest plots were used to assess the efficacy of aspirin. Egger’s test was used to evaluate publication bias.
Results: Aspirin did not alleviate the progression of carotid intima-media thickness (cIMT) compared with control patients (WMD: −0.05 mm, 95% confidence interval 95%CI: −0.12, 0.03). In subset analysis, aspirin was only associated with regression of cIMT when compared with the empty/placebo group (WMD: −0.10 mm, 95%CI: −0.18, −0.02). In type 2 diabetes mellitus, there were no statistical significance between groups (WMD: 0.10 mm, 95%CI: −0.31, 0.50). For the main vascular events and all-cause death, there were no differences between the aspirin group (RR: 0.73, 95%CI: 0.41, 1.31) and the control group (RR: 0.88, 95%CI: 0.41, 1.90). For outcome events, similar results were observed when patients were classified by different cIMT value (p > 0.05). The risk of gastrointestinal bleeding was similar between participants receiving and not receiving aspirin therapy (RR: 1.04, 95%CI: 0.07, 16.46).
Conclusion: In patients with asymptomatic carotid atherosclerosis, low-dose aspirin may slightly alleviate the progression of cIMT, but does not reduce vascular events and all-cause death.
Systematic Review Registration: https://www.crd.york.ac.uk/PROSPERO/, identifier PROSPERO
Atherosclerosis is a vital part of the chronic inflammatory reaction in the body, which involves a secondary autoimmune component (Egger et al., 2001; Kobiyama and Ley, 2018; Xu et al., 2018) that deteriorates over time. The normal artery wall has a triple-layer structure, with atherosclerotic plaques forming in the intima layer. Pathologically, atherosclerotic plaques show deposition of low-density lipoprotein particles, oxidative modification, monocyte migration, foam cell formation, smooth muscle migration, extracellular matrix molecule production, and necrotic core formation (Libby et al., 2019).
Previous studies have reported that carotid atherosclerosis is a surrogate biomarker for predicting further coronary heart disease risk (Geroulakos et al., 1994; Polak et al., 2011; Baldassarre et al., 2012; Bos et al., 2021). The global prevalence of elevated carotid intima-media thickness (cIMT), carotid plaques, and carotid stenosis in people aged 30–79 years in 2020 was 27.62%, 21.13%, and 1.5%, respectively (equivalent to 1066.70 million, 815.75 million, and 57.79 million people, respectively) (Song et al., 2020). Lipid-lowering agents and antiplatelet agents remain an integral part of atherosclerosis treatment. Numerous studies have demonstrated the efficacy of lipid-lowering agents (e.g., statins, Ezetimibe, and PSCK9 inhibitors), antiplatelet agents, and blood pressure and diabetes mellitus control in secondary prevention of atherosclerotic cardiovascular disease (Chapman, 2007; Baigent et al., 2009; Hackam, 2021). As for antiplatelet agents, it is important to assess the bleeding risk before using these treatments.
In 1828, willow was refined into yellow crystals and labeled salicin by a professor of pharmacy—this was the first report of identification and synthesis of the active ingredient of these ubiquitous trees (Fuster and Sweeny, 2011). Aspirin, a type of salicylic acid, is one of the most common antiplatelet pharmaceuticals in current clinical practice. Aspirin covalently and irreversibly inhibits cyclooxygenase and platelet thromboxane A2 biosynthesis (Maree and Fitzgerald, 2004; Kalra et al., 2013). Aspirin is widely used in the secondary prevention of coronary heart disease. In patients with transient ischemic attack or ischemic stroke, the employment of aspirin substantially reduces the risk of early recurrent stroke (Rothwell et al., 2016). Nevertheless, there was no apparent benefit for patients without prior ischemic events (Bavry et al., 2017). Furthermore, the benefit of aspirin in asymptomatic carotid atherosclerosis remains controversial (Paciaroni and Bogousslavsky, 2015). Bleeding events, including fatal or non-fatal gastrointestinal bleeding and intracranial hemorrhage, are a side effect of long-term aspirin use. Thus, considering the balance between antiplatelet and bleeding risk is important when administering this medicine to certain populations.
The aim of the present meta-analysis was to determine whether aspirin is beneficial in patients with asymptomatic carotid atherosclerosis, we assessed the efficacy of aspirin in cIMT regression, prevention of vascular events, and all-cause death, as well as the associated bleeding risk.
This meta-analysis was initiated on 12 May 2022. After searching for studies in electronic databases, five randomized controlled trials involving 841 patients (mean duration: 2.55 years; 2,145 person-years) were included. Registration of the study protocol was done in advance in PROSPERO (No. CRD42022331783). PRISMA 2020 checklist was completed (Supplementary Material S1).
Randomized controlled trials were eligible if they involved a comparison of an aspirin group versus an empty/placebo/other antiplatelet group in patients with asymptomatic carotid atherosclerotic diseases. We also examined reviews and meta-analyses of antiplatelet agents and carotid atherosclerosis as additional resources. Exclusion criteria included 1) Laboratory studies, cohort studies, cross-sectional studies, case-control studies, case reports, letters, commentaries, and summaries, 2) Studies performed on patients with acute myocardial infarction, coronary artery disease, angina pectoris, stroke, lower extremities atherosclerotic occlusive disease, or other complications that involved antiplatelet therapy, 3) Studies that did not report the change in cIMT, carotid plaques, vascular events, deaths, or hemorrhagic events, and 4) Studies where data could not be extracted.
Electronic databases including Pubmed, EMBase, ISI Web, Medline, Cochrane, and clinicaltrial.gov were searched by using the Mesh or Title/Abstract of (“Aspirin” OR “Antiplatelet”) AND (“CIMT” OR “Carotid Intima-Media Thickness” OR “Carotid plaques” OR “Carotid atherosclerosis”) from inception to May 2022. Reviews, meta-analyses, and the references of the identified studies were examined to search for additional resources. There were no restrictions in languages and regions.
Primary outcomes in this meta-analysis were 1) The change in cIMT or carotid plaques, 2) Cardiovascular events (e.g., acute myocardial infarction, unstable angina, and progression of coronary artery disease), 3) Cerebrovascular events (e.g., transient ischemic attacks, ischemic stroke, and hemorrhagic stroke), and 4) All-cause death. The secondary outcomes were gastrointestinal bleeding events.
All studies collected through electronic databases were imported into EndNote X9 and duplicate records were removed. Two reviewers (Xianjin Hu and Yao Hu) separately examined the title, abstract, and entire text of each study. Discrepancies were resolved by consensus or a third author adjudication (Xiankun Sun). These procedures are shown in Figure 1.
Based on a predetermined form, data were separately retrieved by two reviewers. Conflicts were settled by consensus or adjudication by a third author. The following data were collected from each study: first author, publication date, participants’ characteristics (male proportion, age), country of study, sample sizes of the various groups, interventions and duration in each group, and the main outcomes (cIMT, cardio-cerebrovascular events, deaths, and hemorrhagic events).
We determined the change in the mean cIMT between baseline and the study end by multiplying the mean cIMT value (per year change) by the length of the follow-up period, which was reported in one study (Kodama et al., 2000). A similar calculation was used to compute the standard deviation (SD). The Excel spreadsheet provided by the Cochrane website was used to calculate the SD using the p-value or standard error, allowing us to extract SD from other studies that did not disclose the SD of changes in cIMT values.
Two reviewers independently evaluated the risk of bias in the included trials using the Cochrane Collaboration tool (random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data, selective reporting, and other bias). Conflicts were settled by consensus or adjudication by a third author.
All analyses were performed with Review Manager (v5.4.1; RevMan, the Cochrane collaboration, Oxford, United Kingdom) and Stata 17. For continuous variables, data are presented as weighted mean difference (WMD) with 95% confidence intervals (95%CI). For binary variables, data are presented as relative risk (RR) and 95%CI. A random effects model was used for statistical analysis because of the clinical and methodological variability across the trials. Heterogeneity across trials was assessed using the standard Chi-square test (significance set at p < 0.05) and the I2 statistic (significance set at I2 > 50%) Egger’s test was performed to assess the potential for publication bias.
Our meta-analysis included five randomized controlled trials with 841 patients. A flow diagram of the selection procedure is shown in Figure 1. After the initial search, a total of 4,905 articles were included (148 from Pubmed, 3,192 from EMBase, 1016 from ISI Web, 387 from Medline, 161 from Cochrane, and one from clinicaltrial.gov). Only one eligible study was obtained from the reference lists. After eliminating duplicates and screening the title and abstract, full text assessments were performed in 20 trials. Of these, five studies were included in the final quantitative analysis.
Detailed information from the five studies is shown in Table 1. All studies were designed as a randomized conthrolled trial. Four of the studies used a 1:1 allocation for the aspirin group and control group, while one study used a 1:2 allocation. Two studies enrolled participants with type 2 diabetes mellitus, and one study enrolled patients with hypertension. There were two studies eliminating the patients treated with anticoagulation. The rest of trials did not mention the information of using anticoagulation or not. All interventional groups received aspirin therapy, although the doses were different (75–325 mg daily). Two studies used an empty group for comparisons (one with cilostazol and one with placebo), and one study used a standard management group (including diet and exercise). Four of the studies were followed up for 2.3–3 years, while one study was followed up for 6 months. All included patients had asymptomatic increased cIMT, carotid stenosis, or carotid plaques.
In pooled analysis, aspirin therapy was not associated with changes in cIMT values compared with the control group (WMD: −0.05 mm, 95%CI: −0.12, 0.03). In subset analysis, aspirin alleviated the progression of cIMT when compared with the empty/placebo group (WMD: −0.10 mm, 95%CI: −0.18, −0.02), while the efficacy of cilostazol might be better that of aspirin (WMD: 0.31 mm, 95%CI: 0.15, 0.47) (Figure 2).
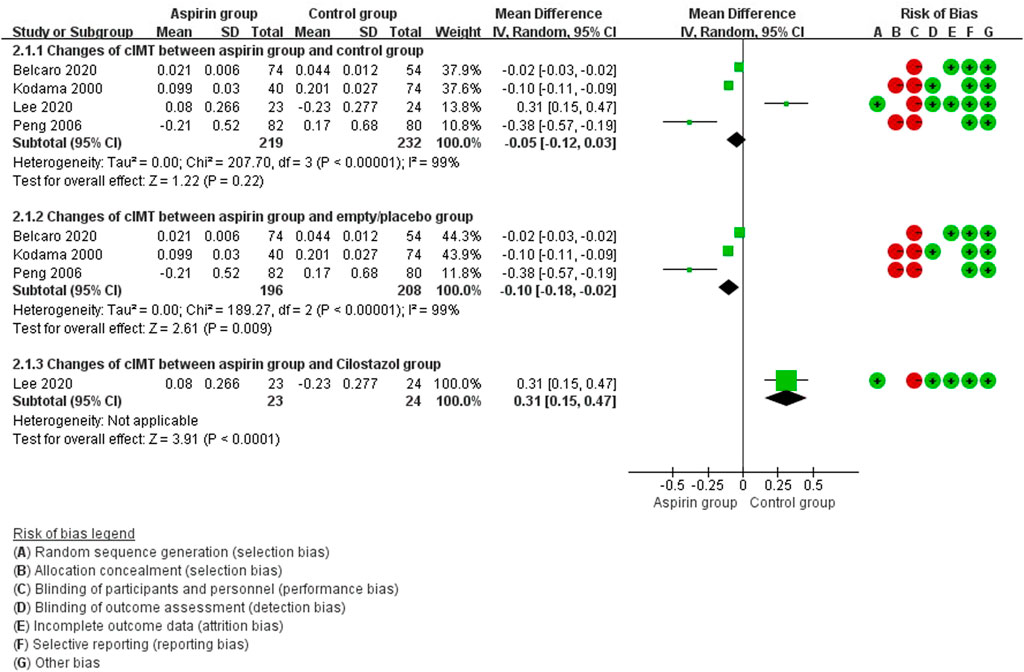
FIGURE 2. Forest plot of changes in carotid intima-media thickness (cIMT) between the aspirin group and the control group.
There were no differences in vascular events between the aspirin group and the control group (RR: 0.73, 95%CI: 0.41, 1.31) (Figure 3). Separate analysis of cardiovascular events (Figure 4) and cerebrovascular events (Figure 5) also showed no difference between the aspirin and control groups. Aspirin did not reduce all-cause death (RR: 0.88, 95%CI: 0.41, 1.90) (Figure 6) in one study that reported mortality. Finally, there were no differences in gastrointestinal bleeding events between patients receiving or not receiving aspirin therapy (RR: 1.04, 95%CI: 0.07, 16.46) (Figure 7).
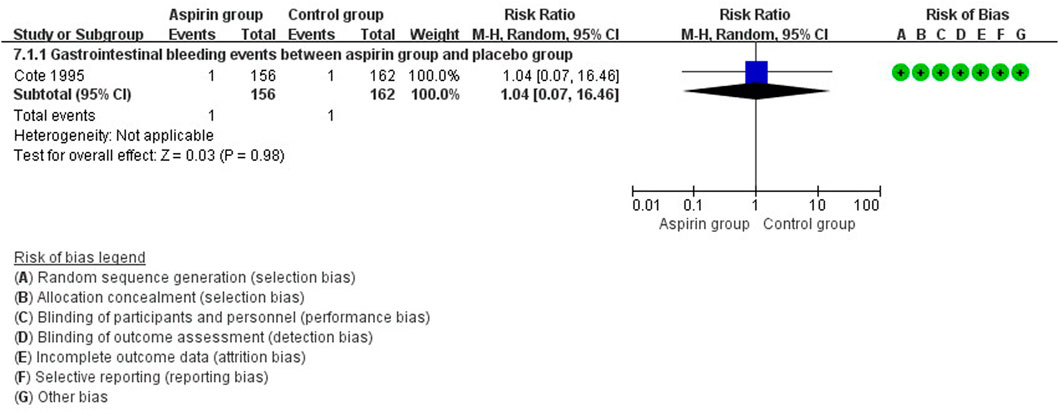
FIGURE 7. Forest plot of gastrointestinal bleeding events between the aspirin group and the control group.
In the subset analysis of type 2 diabetes mellitus, there were no statistical significance between groups (WMD: 0.10 mm, 95%CI: −0.31, 0.50) (Figure 8). In patients with cIMT ≥ 1.0 mm, cIMT reduced slightly but no statistical significance (WMD: −0.22 mm, 95%CI: −0.50, 0.05) (Figure 9). Similar results were observed in patients with cIMT ≥ 1.5 mm or asymptomatic carotid stenosis >50% (WMD: −0.02 mm, 95%CI: −0.03, −0.02) (Figure 9). For the outcome events, including cardiovascular events, cerebrovascular events and all-cause death, there were no statistical significance between aspirin group and control group when patients classified by different cIMT (Figure 10).
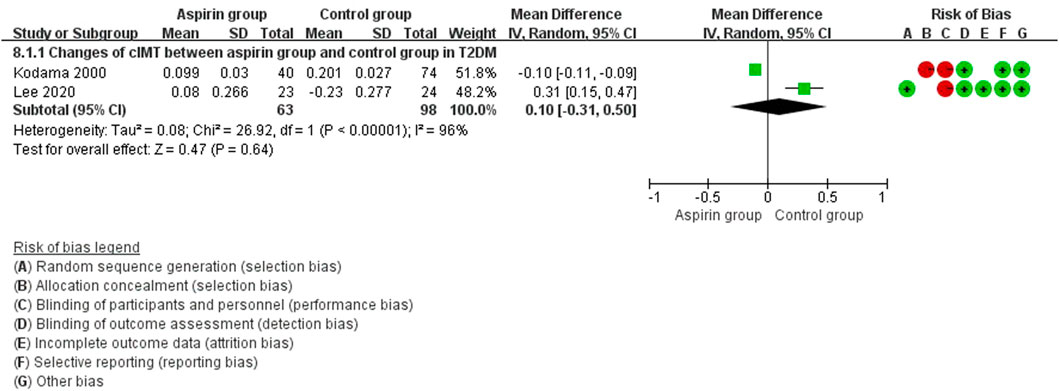
FIGURE 8. Forest plot of changes in carotid intima-media thickness (cIMT) between the aspirin group and the control group in type 2 diabetes mellitus.
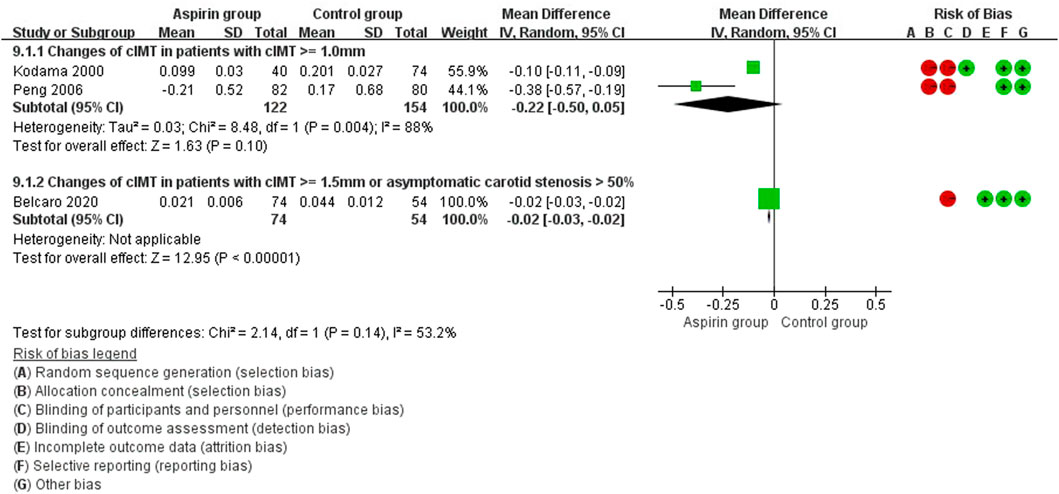
FIGURE 9. Forest plot of changes in carotid intima-media thickness (cIMT) in patients with cIMT ≥ 1.0 mm.
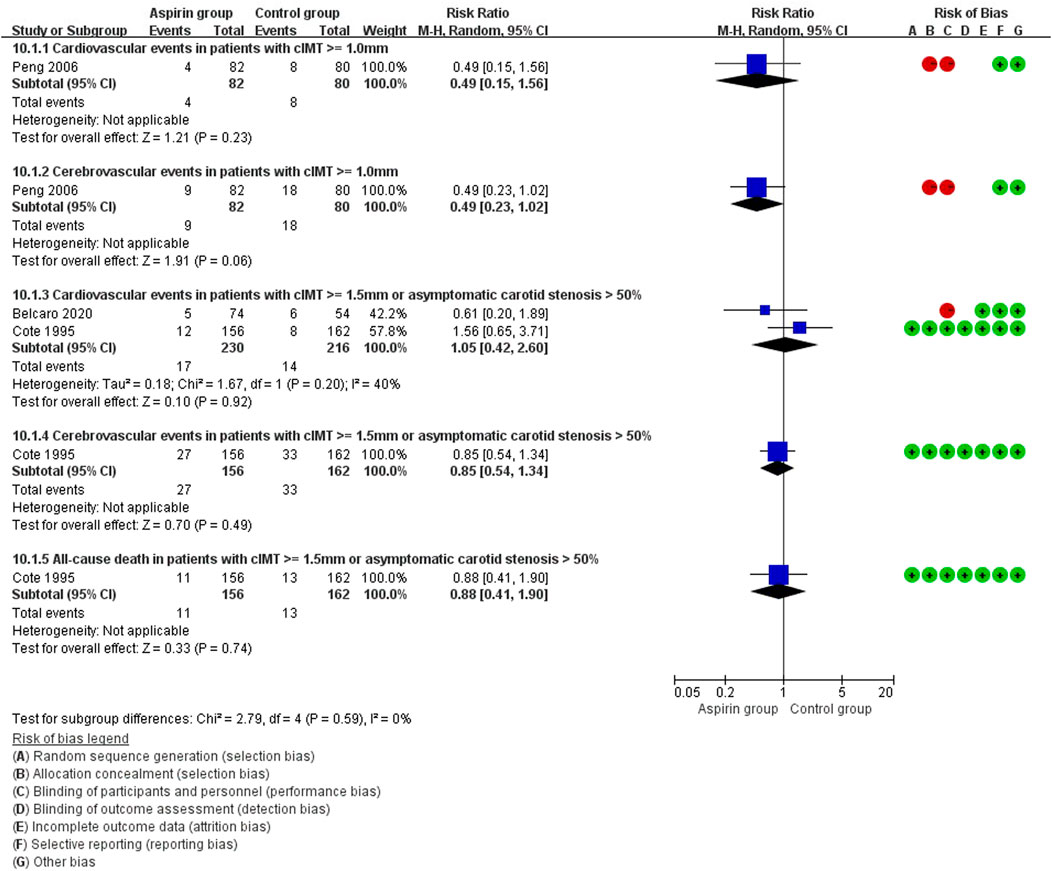
FIGURE 10. Forest plot of outcome events in patients with different carotid intima-media thickness (cIMT) or carotid stenosis.
Because of the small number of trials involved in this meta-analysis, it was difficult to assess publication bias using a funnel plot. Thus, we utilized the Egger’s test (Figures 11, 12). There was no significant publication bias in the continuous (p = 0.744) and binary (p = 0.483) variables.
The aim of this meta-analysis was to determine the efficacy of antiplatelet agents in patients with asymptomatic carotid atherosclerosis. Our main finding was that aspirin did not reduce the incidence of vascular events and all-cause death in patients with asymptomatic carotid atherosclerosis. Nevertheless, compared with an empty/placebo group, aspirin marginally reduced the progression of carotid atherosclerosis. Furthermore, during the follow-up period, there was no effect of aspirin on gastrointestinal bleeding risk.
The therapeutic strategies used in the included studies were based on the presence of symptoms caused by cerebral circulation insufficiency. According to the European Stroke Organization’s guidelines (Bonati et al., 2021), carotid endarterectomy is recommended for patients with moderate–severe symptomatic carotid artery stenosis (50%–99%). By contrast, patients with mild symptomatic stenosis (<50%) are not advised to accept endarterectomy. The European Society of Cardiology guidelines for diagnosis and treatment of peripheral arterial disease (Aboyans et al., 2018) suggest that medical therapy is better than surgery in patients with asymptomatic carotid stenosis (<60%), symptomatic carotid stenosis (<50%), and near occlusion or occlusion. Indeed, the 1-year risk of stroke or death was often lower with intensive medical therapy (approximately 0.5%) than with either carotid endarterectomy or stenting in asymptomatic carotid stenosis patients (Spence, 2020). Thus, most of patients with asymptomatic carotid stenosis should accept medical therapy to reduce vascular events morbidity and mortality. According to our meta-analysis, however, aspirin might not be necessary for these patients when no complication proposed to accept antiplatelet agents.
According to the pathological process of atherosclerosis, lipid deposition, oxidation, and platelet accumulation are critical events during plaque formation and the onset of complications (Reininger et al., 2010). These are also therapeutic targets in clinical practice. For example, aspirin acts as an antiplatelet agent by reducing thromboxane A2 synthesis, and has anti-inflammatory properties involving inhibition of cyclooxygenase activity (Vane and Botting, 2003; Yasuda et al., 2008). In a recent network meta-analysis evaluating the efficacies of several medications on cIMT progression (Huang et al., 2019), phosphodiesterase III inhibitors were the most efficient in reducing the annual mean cIMT, followed by calcium channel blockers, platelet ADP inhibitors, and cyclooxygenase inhibitors (WMD: −0.033 mm per year). However, the network analysis only included two studies of aspirin. In the present meta-analysis, we found that aspirin may slightly reduce the progression of carotid atherosclerosis. The efficacy of aspirin on cIMT may relate to its anti-inflammatory properties (Feldman et al., 2001; Arazi and Badimon, 2012). Other common antiplatelet agents (e.g., cilostazol and clopidogrel) were also reported to be beneficial in preventing carotid atherosclerosis progression (Geng et al., 2012; Takeda et al., 2012). Indeed, the development of symptoms caused by carotid atherosclerosis differed from the progression of carotid atherosclerosis (Park et al., 2016). Nevertheless, previous meta-analyses did not report whether small changes in cIMT were associated with reversal of endpoint events.
The key outcome assessed in the present study was reversal of the endpoints. However, aspirin had no effect on the incidence of vascular events and all-cause death in asymptomatic carotid atherosclerosis patients. Furthermore, the endpoints were not reversed regardless of whether the cIMT value was higher than 1.0 mm or 1.5 mm. Similar outcomes were reported in randomized controlled trials. For example, in a large primary-prevention trial of cardiovascular disease and cancer in women, aspirin reduced the risk of stroke, but had no effect on risk of myocardial infarction or death from cardiovascular causes (Ridker et al., 2005). Comparable results were also reported in patients with type 2 diabetes mellitus (Ogawa et al., 2008), older adults (McNeil et al., 2018), and in Japanese patients >60 years old with atherosclerotic risk factors (Ikeda et al., 2014). Furthermore, in asymptomatic atherosclerotic patients with a low ankle brachial index, aspirin administration had no effect on vascular events compared with placebo (Fowkes et al., 2010). Thus, there is no strong evidence for routine aspirin administration in asymptomatic carotid atherosclerosis patients. Long-term aspirin therapy is also associated with risk of bleeding (Zheng and Roddick, 2019; Gresele et al., 2020). For example, in a recent randomized controlled trial of patients with diabetes without evident cardiovascular disease, although aspirin prevented serious vascular events, this was largely counterbalanced by the bleeding hazard (Bowman et al., 2018). Use of other antithrombotic treatments (e.g., vitamin K antagonists and salicylates) was also suggested to cause intra-plaque hemorrhage that may induce vascular events (Mujaj et al., 2018). As such, it is necessary to identify vulnerable plaques and classify the risk of bleeding, especially in patients with a low-risk of cardiovascular disease (Faggiano et al., 2017; Gaziano et al., 2018). In the present study, there was no difference in the risk of gastrointestinal bleeding between patients receiving short-term aspirin and those not.
There are several limitations of our meta-analysis. The first was the lack of relevant randomized controlled trials, which reduces the accuracy and extrapolation of our findings. Second, because carotid atherosclerosis was detected via Doppler ultrasound in all included trials, it was difficult to identify and classify the vulnerable plaques. Thus, our conclusions may not be appropriate for patients with a high risk of future vascular events, even if they show no ischemia symptoms. Third, the I2 value was >50% in part of our study, suggestive of partial heterogeneity. Fourth, the aspirin doses ranged from 75 to 325 mg daily, which may change the antiplatelet properties and risk of bleeding. Finally, the short follow-up duration of the trials included in this study may underestimate the efficacy of aspirin in asymptomatic carotid atherosclerosis patients. Thus, large and long-term cohort studies and randomized controlled trials are required to confirm the effects of aspirin in this population.
Low-dose aspirin was unable to reduce vascular events and all-cause death in patients with asymptomatic carotid atherosclerosis, with only a minor improvement in the progression of cIMT. Nevertheless, the risk of gastrointestinal bleeding was not increased after short-term aspirin treatment. However, the long-term efficacy of antiplatelet agents remains unclear in patients with asymptomatic carotid atherosclerosis. For patients with vulnerable plaques or a high risk of future cardiovascular events, treatment with antiplatelet agents can be considered for patients with a low risk of bleeding.
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
XH and YL searched articles. XH selected articles, extracted data, performed analyses, and wrote the manuscript. YH selected the articles and extracted the data. XS made a decision when there was a divergence on article selection and data extraction. YZ and XH designed the research and contributed to data interpretation. All authors approved the final manuscript.
We thank Liwen Bianji (Edanz) (www.liwenbianji.cn) for editing the English text of a draft of this manuscript.
The Author XH declared his involvement in the manuscript as a scientist in training.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fphar.2022.1041400/full#supplementary-material
CI, confidence intervals; CIMT, carotid intima-media thickness; RR, relative risk; SD, standard deviation; WMD, weighted mean difference.
Aboyans, V., Ricco, J. B., Bartelink, M. E. L., Björck, M., Brodmann, M., Cohnert, T., et al. (2018). 2017 ESC guidelines on the diagnosis and treatment of peripheral arterial diseases, in collaboration with the European society for vascular surgery (ESVS): Document covering atherosclerotic disease of extracranial carotid and vertebral, mesenteric, renal, upper and lower extremity arteriesEndorsed by: The European stroke organization (ESO)the task force for the diagnosis and treatment of peripheral arterial diseases of the European society of Cardiology (ESC) and of the European society for vascular surgery (ESVS). Eur. Heart J. 39 (9), 763–816. doi:10.1093/eurheartj/ehx095
Arazi, H. C., and Badimon, J. J. (2012). Anti-inflammatory effects of anti-platelet treatment in atherosclerosis. Curr. Pharm. Des. 18 (28), 4311–4325. doi:10.2174/138161212802481264
Baigent, C., Blackwell, L., Collins, R., Emberson, J., Godwin, J., Peto, R., et al. (2009). Aspirin in the primary and secondary prevention of vascular disease: Collaborative meta-analysis of individual participant data from randomised trials. Lancet 373 (9678), 1849–1860. doi:10.1016/s0140-6736(09)60503-1
Baldassarre, D., Hamsten, A., Veglia, F., de Faire, U., Humphries, S. E., Smit, A. J., et al. (2012). Measurements of carotid intima-media thickness and of interadventitia common carotid diameter improve prediction of cardiovascular events: Results of the IMPROVE (carotid intima media thickness [IMT] and IMT-progression as predictors of vascular events in a high risk European population) study. J. Am. Coll. Cardiol. 60 (16), 1489–1499. doi:10.1016/j.jacc.2012.06.034
Bavry, A. A., Elgendy, I. Y., Elbez, Y., Mahmoud, A. N., Sorbets, E., Steg, P. G., et al. (2017). Aspirin and the risk of cardiovascular events in atherosclerosis patients with and without prior ischemic events. Clin. Cardiol. 40 (9), 732–739. doi:10.1002/clc.22724
Belcaro, G., Cesarone, M. R., Scipione, C., Scipione, V., Dugall, M., Shu, H., et al. (2020). Delayed progression of atherosclerosis and cardiovascular events in asymptomatic patients with atherosclerotic plaques: 3-year prevention with the supplementation with Pycnogenol®+Centellicum®. Minerva Cardioangiol. 68 (1), 15–21. doi:10.23736/s0026-4725.19.05051-5
Bonati, L. H., Kakkos, S., Berkefeld, J., de Borst, G. J., Bulbulia, R., Halliday, A., et al. (2021). European Stroke Organisation guideline on endarterectomy and stenting for carotid artery stenosis. Eur. Stroke J. 6 (2), I–xlvii. doi:10.1177/23969873211012121
Bos, D., Arshi, B., van den Bouwhuijsen, Q. J. A., Ikram, M. K., Selwaness, M., Vernooij, M. W., et al. (2021). Atherosclerotic carotid plaque composition and incident stroke and coronary events. J. Am. Coll. Cardiol. 77 (11), 1426–1435. doi:10.1016/j.jacc.2021.01.038
Bowman, L., Mafham, M., Wallendszus, K., Stevens, W., Buck, G., Barton, J., et al. (2018). Effects of aspirin for primary prevention in persons with diabetes mellitus. N. Engl. J. Med. 379 (16), 1529–1539. doi:10.1056/NEJMoa1804988
Chapman, M. J. (2007). From pathophysiology to targeted therapy for atherothrombosis: A role for the combination of statin and aspirin in secondary prevention. Pharmacol. Ther. 113 (1), 184–196. doi:10.1016/j.pharmthera.2006.08.005
Côté, R., Battista, R. N., Abrahamowicz, M., Langlois, Y., Bourque, F., and Mackey, A. (1995). Lack of effect of aspirin in asymptomatic patients with carotid bruits and substantial carotid narrowing. The Asymptomatic Cervical Bruit Study Group. Ann. Intern. Med. 123 (9), 649–655. doi:10.7326/0003-4819-123-9-199511010-00002
Egger, G., Burda, A., Obernosterer, A., Mitterhammer, H., Kager, G., Jürgens, G., et al. (2001). Blood polymorphonuclear leukocyte activation in atherosclerosis: Effects of aspirin. Inflammation 25 (2), 129–135. doi:10.1023/a:1007174723608
Faggiano, P., Gaibazzi, N., Faden, G., and Guidetti, F. (2017). Is anti-platelet therapy always necessary in asymptomatic 30-40% carotid stenosis? J. Cardiovasc. Med. 18 Suppl 1: Special Issue on The State of the Art for the Practicing Cardiologist: The 2016 Conoscere E Curare Il Cuore (CCC) Proceedings from the CLI Foundation, e112–e116. doi:10.2459/jcm.0000000000000474
Feldman, M., Jialal, I., Devaraj, S., and Cryer, B. (2001). Effects of low-dose aspirin on serum C-reactive protein and thromboxane B2 concentrations: A placebo-controlled study using a highly sensitive C-reactive protein assay. J. Am. Coll. Cardiol. 37 (8), 2036–2041. doi:10.1016/s0735-1097(01)01289-x
Fowkes, F. G., Price, J. F., Stewart, M. C., Butcher, I., Leng, G. C., Pell, A. C., et al. (2010). Aspirin for prevention of cardiovascular events in a general population screened for a low ankle brachial index: A randomized controlled trial. Jama 303 (9), 841–848. doi:10.1001/jama.2010.221
Fuster, V., and Sweeny, J. M. (2011). Aspirin: A historical and contemporary therapeutic overview. Circulation 123 (7), 768–778. doi:10.1161/circulationaha.110.963843
Gaziano, J. M., Brotons, C., Coppolecchia, R., Cricelli, C., Darius, H., Gorelick, P. B., et al. (2018). Use of aspirin to reduce risk of initial vascular events in patients at moderate risk of cardiovascular disease (ARRIVE): A randomised, double-blind, placebo-controlled trial. Lancet 392 (10152), 1036–1046. doi:10.1016/s0140-6736(18)31924-x
Geng, D. F., Deng, J., Jin, D. M., Wu, W., and Wang, J. F. (2012). Effect of cilostazol on the progression of carotid intima-media thickness: A meta-analysis of randomized controlled trials. Atherosclerosis 220 (1), 177–183. doi:10.1016/j.atherosclerosis.2011.09.048
Geroulakos, G., O’Gorman, D. J., Kalodiki, E., Sheridan, D. J., and Nicolaides, A. N. (1994). The carotid intima-media thickness as a marker of the presence of severe symptomatic coronary artery disease. Eur. Heart J. 15 (6), 781–785. doi:10.1093/oxfordjournals.eurheartj.a060585
Gresele, P., Paciullo, F., and Migliacci, R. (2020). Antithrombotic treatment of asymptomatic carotid atherosclerosis: A medical dilemma. Intern. Emerg. Med. 15 (7), 1169–1181. doi:10.1007/s11739-020-02347-7
Hackam, D. G. (2021). Optimal medical management of asymptomatic carotid stenosis. Stroke 52 (6), 2191–2198. doi:10.1161/strokeaha.120.033994
Huang, R., Mills, K., Romero, J., Li, Y., Hu, Z., Cao, Y., et al. (2019). Comparative effects of lipid lowering, hypoglycemic, antihypertensive and antiplatelet medications on carotid artery intima-media thickness progression: A network meta-analysis. Cardiovasc. Diabetol. 18 (1), 14. doi:10.1186/s12933-019-0817-1
Ikeda, Y., Shimada, K., Teramoto, T., Uchiyama, S., Yamazaki, T., Oikawa, S., et al. (2014). Low-dose aspirin for primary prevention of cardiovascular events in Japanese patients 60 years or older with atherosclerotic risk factors: A randomized clinical trial. JAMA 312 (23), 2510–2520. doi:10.1001/jama.2014.15690
Kalra, K., Franzese, C. J., Gesheff, M. G., Lev, E. I., Pandya, S., Bliden, K. P., et al. (2013). Pharmacology of antiplatelet agents. Curr. Atheroscler. Rep. 15 (12), 371. doi:10.1007/s11883-013-0371-3
Kobiyama, K., and Ley, K. (2018). Atherosclerosis. Circ. Res. 123 (10), 1118–1120. doi:10.1161/circresaha.118.313816
Kodama, M., Yamasaki, Y., Sakamoto, K., Yoshioka, R., Matsuhisa, M., Kajimoto, Y., et al. (2000). Antiplatelet drugs attenuate progression of carotid intima-media thickness in subjects with type 2 diabetes. Thromb. Res. 97 (4), 239–245. doi:10.1016/s0049-3848(99)00168-1
Lee, D. H., Chun, E. J., Moon, J. H., Yun, H. M., and Lim, S. (2020). Effect of cilostazol on carotid plaque volume measured by three-dimensional ultrasonography in patients with type 2 diabetes: The FANCY study. Diabetes Obes. Metab. 22 (12), 2257–2266. doi:10.1111/dom.14147
Libby, P., Buring, J. E., Badimon, L., Hansson, G. K., Deanfield, J., Bittencourt, M. S., et al. (2019). Atherosclerosis. Nat. Rev. Dis. Prim. 5 (1), 56. doi:10.1038/s41572-019-0106-z
Maree, A. O., and Fitzgerald, D. J. (2004). Aspirin and coronary artery disease. Thromb. Haemost. 92 (6), 1175–1181. doi:10.1160/th04-02-0127
McNeil, J. J., Wolfe, R., Woods, R. L., Tonkin, A. M., Donnan, G. A., Nelson, M. R., et al. (2018). Effect of aspirin on cardiovascular events and bleeding in the healthy elderly. N. Engl. J. Med. 379 (16), 1509–1518. doi:10.1056/NEJMoa1805819
Mujaj, B., Bos, D., Muka, T., Lugt, A. V., Ikram, M. A., Vernooij, M. W., et al. (2018). Antithrombotic treatment is associated with intraplaque haemorrhage in the atherosclerotic carotid artery: A cross-sectional analysis of the rotterdam study. Eur. Heart J. 39 (36), 3369–3376. doi:10.1093/eurheartj/ehy433
Ogawa, H., Nakayama, M., Morimoto, T., Uemura, S., Kanauchi, M., Doi, N., et al. (2008). Low-dose aspirin for primary prevention of atherosclerotic events in patients with type 2 diabetes: A randomized controlled trial. Jama 300 (18), 2134–2141. doi:10.1001/jama.2008.623
Paciaroni, M., and Bogousslavsky, J. (2015). Antithrombotic therapy in carotid artery stenosis: An update. Eur. Neurol. 73 (1-2), 51–56. doi:10.1159/000367988
Park, Y. J., Kim, D. I., Kim, G. M., Kim, D. K., and Kim, Y. W. (2016). Natural history of asymptomatic moderate carotid artery stenosis in the era of medical therapy. World Neurosurg. 91, 247–253. doi:10.1016/j.wneu.2016.04.037
Peng, H. S., Sun, C. Y., and Lv, H. X. (2006). Efficacy of intervention with simvastatin and aspirin for carotid arteriosclerosis in patients with hypertension. [Chinese]. Chin. J. Cerebrovasc. Dis. 3 (1), 15–18.
Polak, J. F., Pencina, M. J., Pencina, K. M., O’Donnell, C. J., Wolf, P. A., D’Agostino, R. B., et al. (2011). Carotid-wall intima-media thickness and cardiovascular events. N. Engl. J. Med. 365 (3), 213–221. doi:10.1056/NEJMoa1012592
Reininger, A. J., Bernlochner, I., Penz, S. M., Ravanat, C., Smethurst, P., Farndale, R. W., et al. (2010). A 2-step mechanism of arterial thrombus formation induced by human atherosclerotic plaques. J. Am. Coll. Cardiol. 55 (11), 1147–1158. doi:10.1016/j.jacc.2009.11.051
Ridker, P. M., Cook, N. R., Lee, I. M., Gordon, D., Gaziano, J. M., Manson, J. E., et al. (2005). A randomized trial of low-dose aspirin in the primary prevention of cardiovascular disease in women. N. Engl. J. Med. 352 (13), 1293–1304. doi:10.1056/NEJMoa050613
Rothwell, P. M., Algra, A., Chen, Z., Diener, H.-C., Norrving, B., and Mehta, Z. (2016). Effects of aspirin on risk and severity of early recurrent stroke after transient ischaemic attack and ischaemic stroke: Time-course analysis of randomised trials. Lancet 388 (10042), 365–375. doi:10.1016/s0140-6736(16)30468-8
Song, P., Fang, Z., Wang, H., Cai, Y., Rahimi, K., Zhu, Y., et al. (2020). Global and regional prevalence, burden, and risk factors for carotid atherosclerosis: A systematic review, meta-analysis, and modelling study. Lancet. Glob. Health 8 (5), e721–e729. doi:10.1016/s2214-109x(20)30117-0
Spence, J. D. (2020). Management of asymptomatic carotid stenosis. Ann. Transl. Med. 8 (19), 1262. doi:10.21037/atm-20-975
Takeda, M., Yamashita, T., Shinohara, M., Sasaki, N., Tawa, H., Nakajima, K., et al. (2012). Beneficial effect of anti-platelet therapies on atherosclerotic lesion formation assessed by phase-contrast X-ray CT imaging. Int. J. Cardiovasc. Imaging 28 (5), 1181–1191. doi:10.1007/s10554-011-9910-6
Vane, J. R., and Botting, R. M. (2003). The mechanism of action of aspirin. Thromb. Res. 110 (5-6), 255–258. doi:10.1016/s0049-3848(03)00379-7
Xu, S., Pelisek, J., and Jin, Z. G. (2018). Atherosclerosis is an epigenetic disease. Trends Endocrinol. Metab. 29 (11), 739–742. doi:10.1016/j.tem.2018.04.007
Yasuda, O., Takemura, Y., Kawamoto, H., and Rakugi, H. (2008). Aspirin: Recent developments. Cell. Mol. Life Sci. 65 (3), 354–358. doi:10.1007/s00018-007-7449-4
Keywords: aspirin, asymptomatic carotid atherosclerosis, carotid intima-media thickness, gastrointestinal bleeding, meta-analysis
Citation: Hu X, Hu Y, Sun X, Li Y and Zhu Y (2022) Effect of aspirin in patients with established asymptomatic carotid atherosclerosis: A systematic review and meta-analysis. Front. Pharmacol. 13:1041400. doi: 10.3389/fphar.2022.1041400
Received: 10 September 2022; Accepted: 24 November 2022;
Published: 07 December 2022.
Edited by:
Lon J. Van Winkle, Rocky Vista University, United StatesReviewed by:
Francesco Paciullo, Centro Emostasi e Trombosi Perugia, ItalyCopyright © 2022 Hu, Hu, Sun, Li and Zhu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ye Zhu, NTEwODk0MzQyQHFxLmNvbQ==
†These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.