- Department of Neurosurgery and Brain and Nerve Research Laboratory, The First Affiliated Hospital of Soochow University, Suzhou, China
Introduction: Post-stroke depression (PSD) is a common mental health problem after cerebrovascular accidents. There are several treatments that have been shown to be effective in treating post-stroke depression. However, it is not clear which treatment is more effective.
Methods: In this meta-analysis, an appropriate search strategy was used to search eligible randomized controlled trials (RCTs) on different treatments to treat patients with Post-stroke depression published up to December 2021 from the CNKI, PubMed, and Cochrane Library. We assessed the mean difference or odds ratio between each treatment and placebo and summarized them as the average and 95% confidence interval (CI) by conducting Bayesian network meta-analyses.
Results: By constructing a Bayesian network meta-analysis, we found that acupuncture combined with fluoxetine (vs placebo MD, −8.9; 95% CI, [−15, −2.9]) or paroxetine (vs placebo MD,—8.5; 95% CI, [−15, −2.5]) was the most effective for change in Hamilton depression scale (HAMD) at the end of the 4th week. For change in Hamilton depression scale at the end of the 8th week, rTMS combined with paroxetine (vs placebo MD, −13; 95% CI, [−17, −7.9]) had the greatest amount of change. The efficacy of medication combined with adjuvant therapy was also superior for the percentage of patients with Hamilton depression scale change over 50%.
Discussion: The combination of antidepressants with adjuvant therapy may enhance the efficacy of antidepressants and achieve better results than antidepressant monotherapy in both Hamilton depression scale changes at the end of week 4 or 8 and 50% Hamilton depression scale improvement rate. Acupuncture combined with fluoxetine treatment was more effective in the treatment of post-stroke depression at week 4, while rTMS combined with paroxetine was more effective at week 8. Further research is needed to determine whether acupuncture combined with fluoxetine is better than rTMS combined with paroxetine for post-stroke depression at week 8.
Background
Stroke is the third leading cause of death worldwide, accounting for approximately 5.9 million deaths each year. Stroke morbidity and mortality are rising rapidly with the growth of the elderly population (Villa et al., 2018). Cerebrovascular accidents and depression following are currently the two major causes of economic burden on society (Medeiros et al., 2020). Post-stroke depression (PSD) is the most common and burdensome neuropsychiatric complication after stroke. Some studies have shown that PSD is about one-third of the prevalence in stroke patients (Mitchell et al., 2017; Shi et al., 2017; Taylor-Rowan et al., 2019). Patients with PSD have higher mortality, more significant cognitive deficits, and lower quality of life than patients without PSD (Hilari et al., 2012; Blöchl et al., 2019; Starkstein and Hayhow, 2019). Therefore, it is extremely important to understand the pathogenesis of PSD and to find effective treatments.
The pathophysiology of PSD is complex and multifactorial, resulting from a combination of ischemia-induced neurobiological dysfunction and psychosocial distress (Robinson and Jorge, 2016). The pathology of PSD development may be related to alterations in the ascending monoamine pathway, excess of pro-inflammatory cytokines, dysfunction of the hypothalamic-pituitary-adrenal axis and altered neuroplasticity (Villa et al., 2018). The complexity of the pathogenesis of PSD makes its prevention and treatment on a biological basis a difficult task. Currently, selective 5-hydroxytryptamine reuptake inhibitors and tricyclic antidepressants have been clinically shown to have positive effects in the prevention and treatment of PSD, but the mechanisms by which they exert their therapeutic effects remain unclear and are associated with serious adverse events (Paolucci, 2017; Das, 2018). In recent years, with the continuous research on the pathology of PSD, many new effective treatment methods have emerged, such as acupuncture, herbal medicine, hyperbaric oxygen (HBO) and repetitive transcranial magnetic stimulation (rTMS), or even combined treatments (Lefaucheur et al., 2020; Liang et al., 2020; Gong et al., 2021). Treatments for PSD are longer restricted in medications alone.
There are currently a variety of treatments for PSD. There are also relevant studies describing the effectiveness of different treatments. But previous studies comparing the efficacy of these treatments are inadequate, especially there is no systematic assertion on the effectiveness of adjuvant therapy. Therefore, a Bayesian network meta-analysis was performed in order to analyze which of the treatments is more beneficial for the improvement of post-stroke depressed patients. The differences in the effectiveness of different treatments for PSD were analyzed in order to be able to provide an evidence-based medical reference for clinical treatment of PSD.
Materials and methods
Study protocol
Before starting this study, we prepared a draft study protocol following the format of the Cochrane Collaboration. The meta-analysis has not yet been registered.
Literature search
In our study, we used an appropriate search method to screen eligible randomized controlled trails on treatments to patients with PSD in 3 literature databases, PubMed, China National Knowledge Infrastructure (CNKI) and Cochrane library. The publication date of the included papers was up to December 2021. The search was performed in both databases following the keywords: “post-stroke depression” AND (“citalopram” OR “amitriptyline” OR “paroxetine” OR “fluoxetine” OR “venlafaxine” OR “sertraline” OR “mirtazapine” OR “escitalopram” OR “duloxetine” OR “antidepressant” OR “shuganjieyutang” OR “hyperbaric oxygen” OR “acupuncture” OR “repetitive transcranial magnetic stimulation” OR “rTMS” OR “HBO”) AND (“randomized controlled trail” OR “RCT” OR “random” OR “controlled”).
Inclusion and exclusion criteria
The criteria for study selection are described below. 1) Randomized controlled studies involving the treatment of post-stroke depressed patients. 2) Each included article must contain at least one outcome indicator, including Hamilton depression scale (HAMD) change at week 4, HAMD change at week 8, and HAMD 50% remission rate at end of treatment. 3) All data enrolled was assessed by HAMD-17. 4) Herbal medicine included was limited to traditional Chinese medicine, “shuganjieyutang”. 5) Each article must include at least two treatment modalities (including placebo) for each other. Studies that do not meet the 3 criteria above will be excluded.
Quality assessment and data extraction
Following the Cochrane Collaboration’s risk analysis assessment form, 2 authors were involved in collating and summarizing the quality of each article, including authorship, year of publication, and patient-based information. The potential risk of bias for each article was identified and the quality of the article was assessed, but in case of disagreement between the 2 authors, the other author was brought in for final determination.
Statistical analysis
After recording data from literatures that met the criteria, we used Gemtc R-package and R4.0.3 software to construct a Bayesian network model (van Valkenhoef et al., 2012; van Valkenhoef et al., 2016). We first tested the heterogeneity of the model, using chi-square q-tests and I2 statistics to assess heterogeneity between trials. If p < 0.05 or I2 > 50% showed significant heterogeneity, a random effects model was used. On the contrary, without significant heterogeneity, a fixed-effects model was used. Subsequently, we built the corresponding models based on the above results to integrate the treatment effects of drugs in different studies. The results were presented by constructing forest plots, league tables, and ranking plots. We then validated the consistency in the network model by comparing each node with the existence of direct, indirect, and pooled evidence using the node splitting method to assess the statistical differences between the different evidence determining the consistency of the indirect evidence with the direct evidence. Similarity was judged manually based on the quality control mitigation.
Result
Study charachteristics
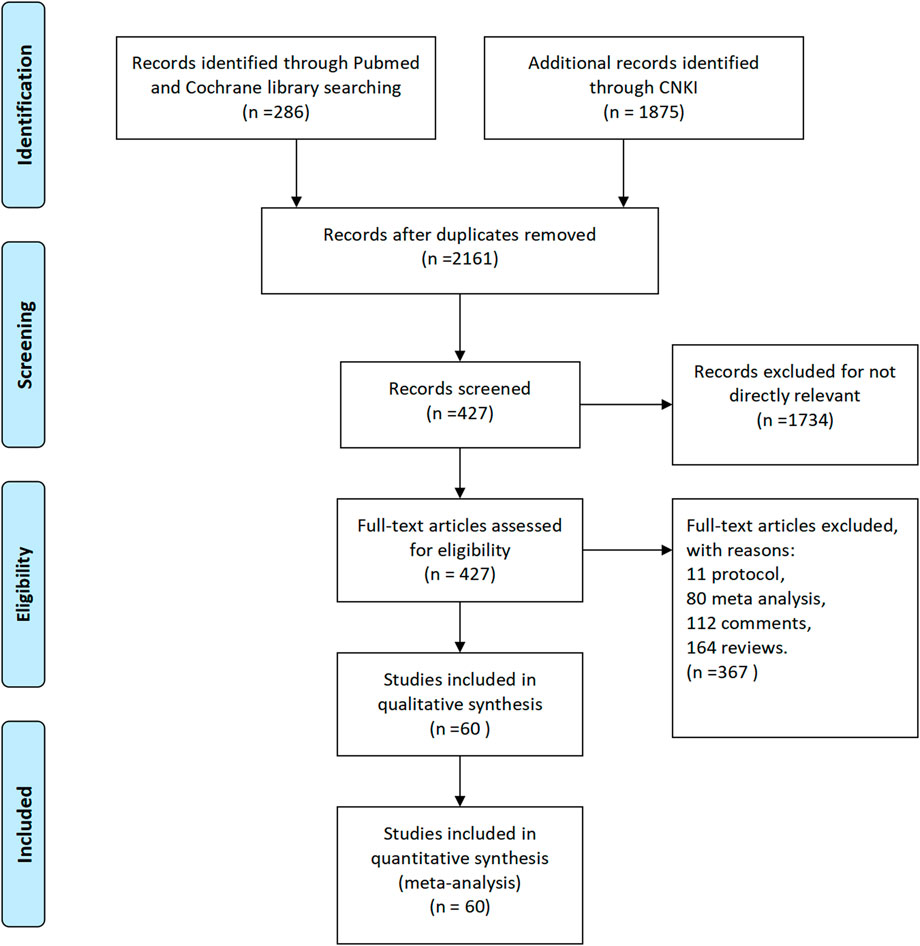
According to the above method, we searched 286 articles in Pubmed and Cochrane Library and 1875 articles in CNKI. By comparison, we removed the overlapping articles and obtained the final 427 articles by initial screening of abstracts. By reading the full text, 11 protocols, 80 meta-analyses, 112 comments and 164 reviews were finally removed (Figure 1). Finally, the characteristic information of the remaining 60 papers, which were included in this paper, is shown in supplementary material table one 17-76. This Table1 contains 16 different treatments include acupuncture, acupuncture combine with fluoxetine, acupuncture combine with paroxetine, amitriptyline, citalopram, duloxetine, escitalopram, fluoxetine, fluoxetine combine with HBO, HBO, mirtazapine, paroxetine, rTMS combine with paroxetine, sertraline, shuganjieyutang and venlafaxine.
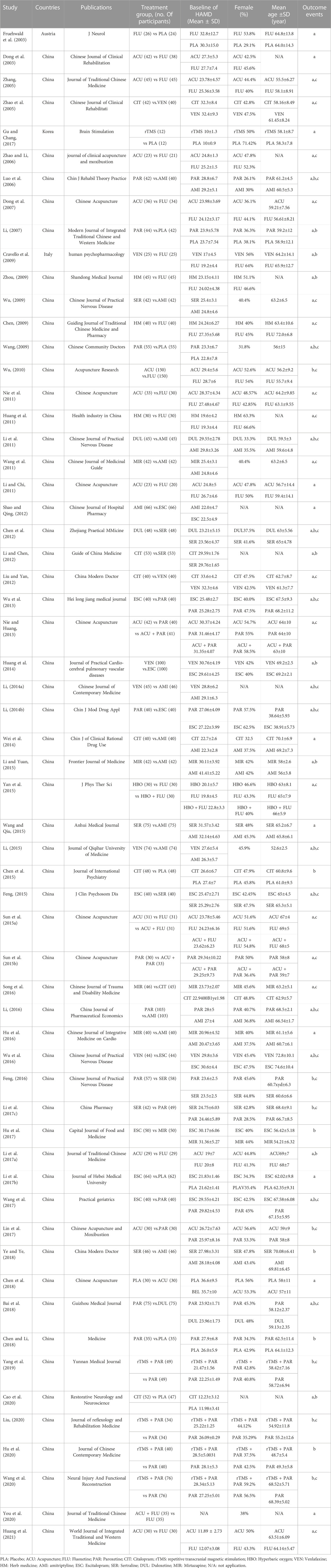
In addition, we conducted a detailed bias analysis of these 60 articles. The main bias focused on the possible blinding bias associated with acupuncture and its combination therapy, which could not be avoided during their implementation. The remaining factors that may have influenced the bias focused on the number of included populations, marked in the “other bias” item. All articles marked in yellow or red, present too small included populations, with less than 25 people included in each group in Li HJ’s literature, which may have had some impact on the results (Figure 2).
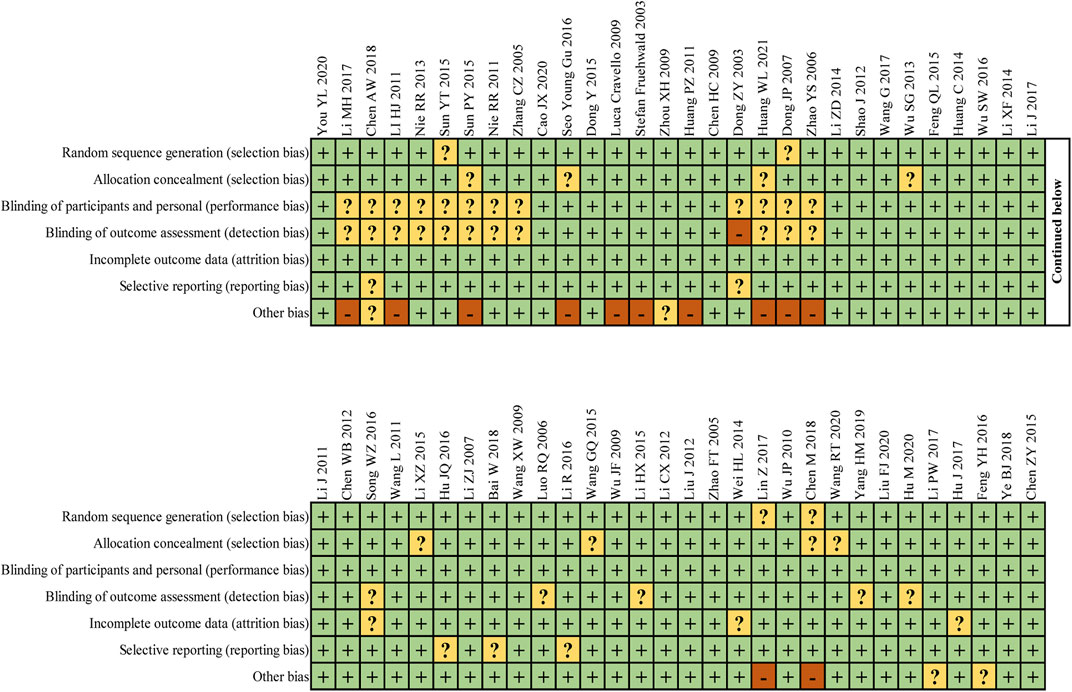
FIGURE 2. I Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
Heterogeneity examination
Before constructing the final network model, we verified the heterogeneity of the collected data, and we used a random-effects model for the two indicators of HAMD change at the end of week 4 and 8 with an overall I2 > 50%. Correspondingly, the proportion of patients with 50% improvement in HAMD, an indicator for which we used a fixed-effects model to construct the network because its overall I2 ≤ 50%. More detailed inter-article comparisons are shown in the supplementary materials (Supplementary Figure S1).
Network meta-analysis
We analyzed the efficacy of different treatments for PSD, including medications, traditional herbal treatments, and medications combined with acupuncture, HBO and rTMS, by means of a network meta-analysis. We selected two indicators, including the amount of HAMD changes (including results at the end of week 4 and 8 of treatment) and the percentage of patients with 50% improved HAMD.
Totally 17 treatments were enrolled in the analysis of the changes in HAMD score at the end of week 4 (Figure 3A). At the end of the 4th week of treatment, acupuncture (MD, −6.2; 95% CI, [−11, −1.6]), acupuncture combined with fluxetine (MD, −8.9; 95% CI, [−15, −2.9]), acupuncture combined with paroxetine (MD,—8.5; 95% CI, [−15, −2.5]), escitalopram (MD, −5.6; 95% CI, [−9.4, −1.8]), mirtazapine (MD, −6.6; 95% CI, [−12, −1.5]), paroxetine (MD, −5.2; 95% CI, [−8.7, −1.7]), and sertraline (MD, −4.7; 95% CI, [−9.3, −0.037]) were significantly superior compared to placebo (Figure 3B). Based on the evidence from the network, we drew line graphs showing the rank of probability for each treatment (Figure 3C). The results of the line graph suggest that acupuncture combined with fluoxetine was the most effective treatment at the end of the 4th week while the placebo was clearly the worst. More specific inter-treatment comparisons we show in the league table (Figure 3D). It can be found that acupuncture combined with fluoxetine is more effective to amitriptyline, venlafaxine, and placebo for PSD. Of interest is that the efficacy of fluoxetine after combined acupuncture is better than that of fluoxetine alone (MD, −5.4; 95% CI, [−9.51, −1.32]), which is statistically significant.
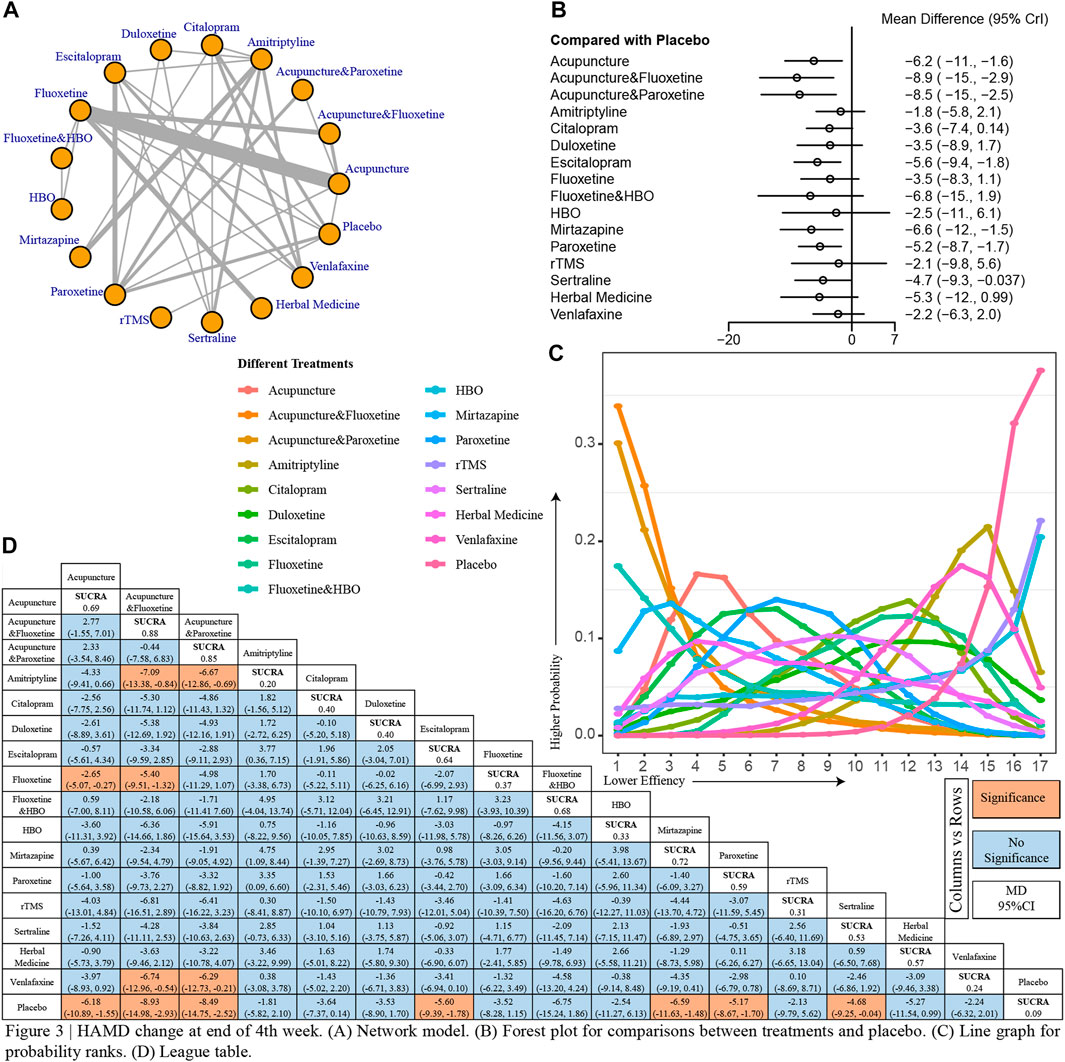
FIGURE 3. I HAMD change at end of 4th week. (A) Network model. (B) Forest plot for comparisons between treatments and placebo. (C) Line graph for probability ranks. (D) League table.
When the course of treatment was extended to 8 months, 13 modalities were included in our analysis (Figure 4A). All treatments showed better improvement compared to placebo, except amitriptyline (MD, −4.4; 95% CI, [−8.9, −0.2]), venlafaxine (MD, −5; 95% CI, [−10, −0.082]) (Figure 4B). Also, by inspection of the line graph of probability rank, we found that paroxetine treatment in combination with rTMS was the most effective in improving PSD at the end of the 8th week (Figure 4C). There is no doubt that the placebo group had the worst effect. Using the detailed data from the league table, we found that acupuncture is still an effective treatment modality, compared to placebo. Similarly, we found that paroxetine treatment in combination with rTMS was superior to paroxetine (rTMs and paroxetine vs paroxetine MD, −5.27; 95% CI, [−2.2, −8.3]) treatment alone (Figure 4D).
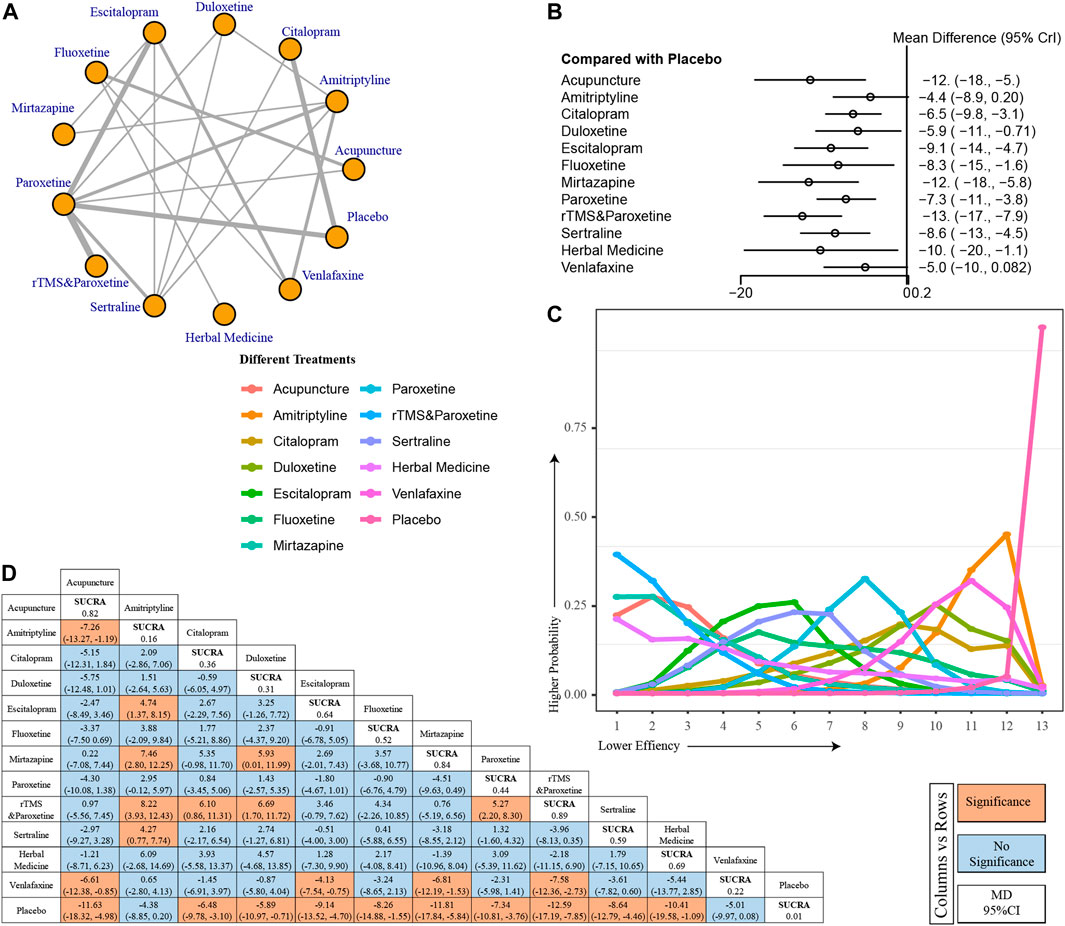
FIGURE 4. I HAMD change at end of 8th week. (A) Network model. (B) Forest plot for comparisons between treatments and placebo. (C) Line graph for probability ranks. (D) League table.
Seventeen treatments were included for comparison to assess the impact of different treatments on the percentage of patients with 50% improvement in HAMD (Figure 5A). All included treatment modalities demonstrated a better 50% improvement rate than placebo. Several combination treatment modalities, acupuncture combined with fluoxetine (OR, 1.0e+02; 95% CI, [25, 4.9e+02]), acupuncture combined with paroxetine (OR, 67; 95% CI, [21, 2.5e+02]), HBO combined with fluoxetine (OR, 44; 95% CI, [9, 2.5e+02]), and rTMS combined with paroxetine (OR, 55; 95% CI, [19, 1.9e+02]) showed good efficacy compared to placebo (Figure 5B). The efficacy of acupuncture combined with fluoxetine was the best in the line chart, and the efficacy of acupuncture combined with paroxetine and rTMS combined with paroxetine also ranked high (Figure 5C). Data from the league table also suggest that acupuncture combined with fluoxetine and rTMS combined with paroxetine is more effective than traditional antidepressants such as citalopram, amitriptyline, and duloxetine alone (Figure 5D).
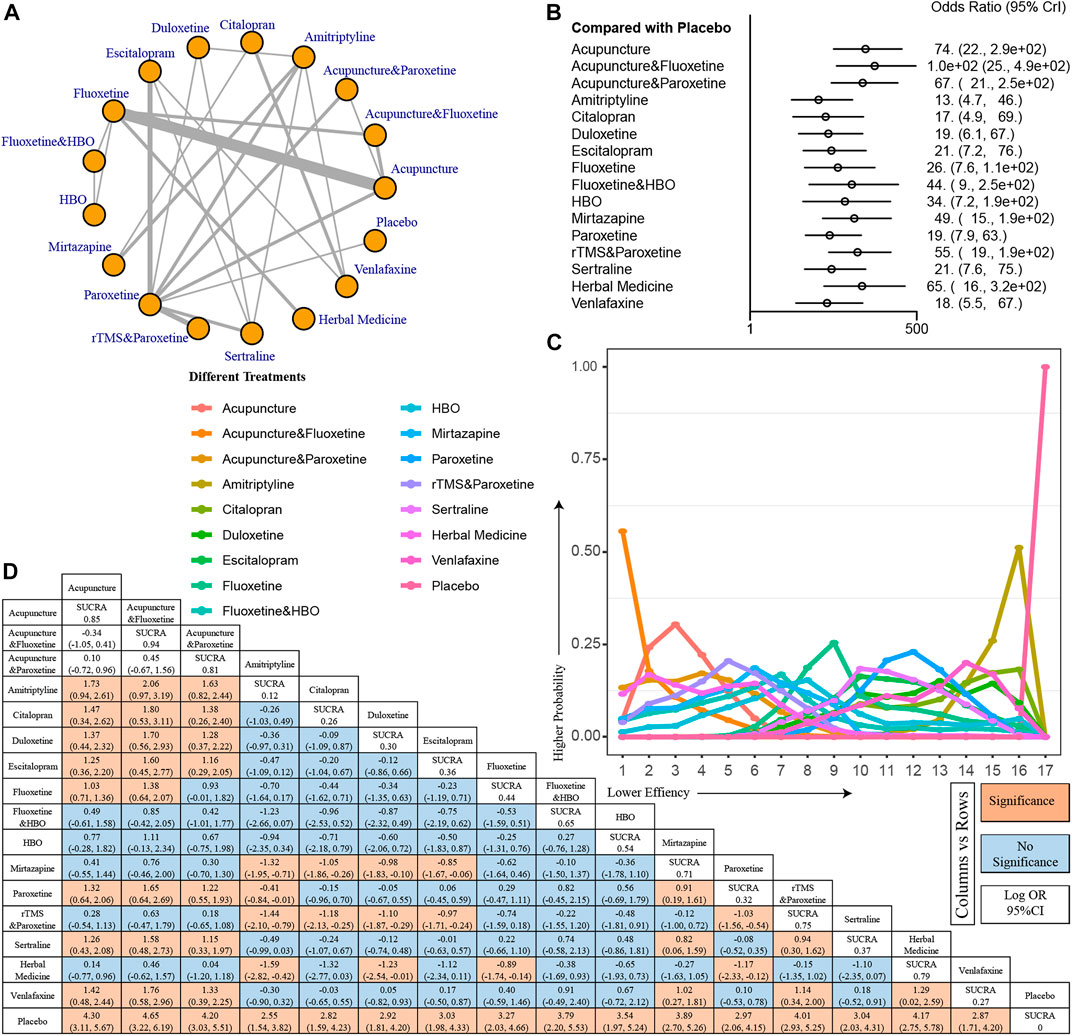
FIGURE 5. I Percentage of patients with 50% improvement in HAMD. (A) Network model. (B) Forest plot for comparisons between treatments and placebo. (C) Line graph for probability ranks. (D) League table.
Consistency and similarity examinations
Direct, indirect, and pooling evidence are available in the network for all indicators. Therefore, for each indicator, we used the node-splitting method to perform consistency tests. All 3 indicators were not tested for inconsistency between indirect and direct evidence, with all p-values >0.05, suggesting that our model was constructed reasonably correctly (Supplementary Figure S2). Similarity tests were performed by the bias analysis and quality control of the included articles. There was no significant bias in similarity between data, as previously described.
Discussion
PSD is the most common mental health problem, afflicting approximately 33% of stroke survivors, and PSD affects the recovery and quality of life of post-stroke patients (Robinson and Jorge, 2016). A growing amount of research suggests a strong association between PSD and stroke, and that both physiology and psychology play an important role in PSD (Zhou et al., 2022). Despite extensive efforts to study PSD, its pathogenesis is still unclear. Currently, selective 5-hydroxytryptamine reuptake inhibitors and tricyclic antidepressants are the main treatments in clinical practice (Paolucci, 2017). In recent years, there are more and more new treatment strategy for PSD, such as acupuncture, herbal medicine, HBO and rTMS (Hadidi et al., 2017). However, it is not clear which of the different treatments is more effective. In our study, we performed a Bayesian network meta-analysis of the 60 included articles to compare the effectiveness of different treatment methods. Our study found that the combination of antidepressants with adjuvant therapy enhanced the efficacy of antidepressants and was superior to antidepressant monotherapy. This provides some theoretical basis for future clinical work.
In this paper, we constructed an appropriate network meta-analysis model by collecting data from more than a dozen treatment modalities from previous works to analyze 3 indicators of effectiveness of PSD. The treatments we enrolled included commonly used antidepressant medications, herbal medicine, HBO, acupuncture, and medications combined with adjuvant therapy, covering almost all current clinical applications for the treatment of PSD. All 3 analyzed indicators were related to the HAMD score, the most widely used scale to evaluate the degree of depression in patients. The HAMD is a 17-item clinical assessment instrument used to quantify the severity of depression in subjects who have been diagnosed with depression (Hamilton, 1967). It became one of the most widely used prognostic indicators in depression and was used in many trials of new antidepressant drugs submitted to the Food and Drug Administration (FDA) (Leucht et al., 2013). We studied here only the amount of HAMD change at the 4th and 8th week end, and the percentage of patients with 50% improvement in HAMD, with the intention of analyzing which treatment modality is the most efficacious now.
Our analysis pointed out that at the end of the 4th week, not all classical antidepressants produced an effect, with only escitalopram, paroxetine, mirtazapine, and sertraline having significant efficacy. Antidepressants, including selective 5-hydroxytryptamine reuptake inhibitors and tricyclic antidepressants, have been shown to be effective in PSD. Although there are no studies showing that selective 5-hydroxytryptamine reuptake inhibitors are more effective than tricyclic antidepressants, selective 5-hydroxytryptamine reuptake inhibitors are currently used as the first line of treatment. This may be due to the fact that selective 5-hydroxytryptamine reuptake inhibitors is more effective in treating depression and generalized anxiety disorder and has fewer long-term side effects (Qin et al., 2014; Villa et al., 2018). In previous studies, tricyclic antidepressants, such as amitriptyline, were found to take 2–3 weeks to exert their effects and selective 5-hydroxytryptamine reuptake inhibitors took 3–4 weeks to work (Gillman, 2007). Therefore, the amount of change in HAMD scores at the fourth week after treatment may not be significant. And the treatments combined with acupuncture greatly enhanced the therapeutic effect of antidepressants. Among them, fluoxetine combined with acupuncture treatment has the greatest possibility to produce the best efficacy, according to our calculations. It was significantly superior compared to fluoxetine alone, initially demonstrating the effect of the combination treatment. The possible mechanism of acupuncture for the treatment of PSD is achieved by stimulating specific acupoints to induce the restoration of brain nerve cells, including noradrenergic, dopamine, 5-hydroxytryptamine neurons and their axons, while accelerating the repair of damaged brain tissue and promoting the release of 5-hydroxytryptamine in the brain and noradrenaline in the spinal cord (Zhang et al., 2010; Li et al., 2020) The mechanism by which herbs and rTMS exert their antidepressant effects is not fully understood. However, studies have shown that they can increase blood flow to local lesions, improve cortical metabolism, promote neuronal protein expression, and thus improve depressive symptoms (Liu et al., 2012; Liu et al., 2015). Therefore, drug treatment combined with acupuncture, rTMS and herbal medicine can have better therapeutic effect to a certain extent.
When the time window of treatment was stretched to 8 weeks, all treatment modalities except amitriptyline and griseofulvin achieved good efficacy. Notably, rTMS combined with paroxetine was most likely to achieve the most excellent treatment results at this time. Once again, the efficacy of the combination therapy exceeded that of paroxetine monotherapy. The better treatment outcome may be due to the longer treatment period compared to 4 weeks of treatment.
For overall effectiveness, the metric we chose was the percentage of patients with 50% improvement in HAMD. Our results continue to point to a preference for the use of combination therapy that can improve the depressive status of patients. Both acupuncture combined with fluoxetine and acupuncture combined with paroxetine, which performed well at the end of 4 weekends, and rTMS combined with paroxetine, which performed well at the end of 8 weekends, were in the top 5 most effective. This further confirms the good effect of the combined treatment. In contrast, we noted that while amitriptyline and venlafaxine had a higher percentage of patients with HAMD improvements of more than 50% than placebo. However, neither antidepressant showed better improvement than the placebo group at the end of 4 and 8 weeks. This may have a negative impact on their continued use as PSD medication in the future. Previous studies have shown that amitriptyline and venlafaxine have better treatment effects than placebo when used to treat depression. This result is inconsistent with the results of our study (Rampello et al., 1995; Furukawa et al., 2019). This may be since PSD has a different pathogenesis than common depression. For example, the PSD-related potentials are different from common depression-related potentials (Hajcak et al., 2010). This differences leads to the poor therapeutic effect of amitriptyline and venlafaxine in the treatment of PSD. The differences in their clinical effects need to be further investigated.
Although we concluded the above results, there are some limitations in the paper that may have an impact on our results. First, we have only conducted a limited analysis of the effectiveness of these treatments and lack relevant comparisons in terms of safety and other aspects. Although many treatments showed significant improvements in PSD, their side effects may cause adverse events in patients beyond depression. Second, the article included a limited population and a large sample of Chinese patients was included in the article, which may have introduced bias to the included population. The third point is that the included articles do not strictly distinguish between hemorrhagic or ischemic stroke. Both may have an impact on the way and severity of PSD. In addition, inconsistencies in the treatment modalities included at the end of week 4 and 8 are due to problems inherent in the data sources. Some treatment modalities were missing, making it impossible to compare the efficacy of the same treatment modality at different times. The fifth point is that only the HAMD score was used as the primary outcome indicator in this study, which would have missed some of the articles using other outcome indicators, such as geriatric depression scale and hospital anxiety and depression scale. Finally, there are many traditional Chinese medicines for the treatment of post-stroke depression, such as xiaoyaosan, shuganjieyutang and sinisan. However, in this study, only shuganjieyutang was included for meta-analysis because other medication outcome indicators were inconsistent or did not meet the inclusion criteria of this study.
Conclusion
In conclusion, for HAMD change effects at the end of the 4th and 8th week of PSD treatment, the combination of antidepressants with adjuvant therapy may enhance the efficacy of antidepressants and achieve better results than antidepressant monotherapy. According to our findings, acupuncture combined with fluoxetine treatment was more effective in the treatment of post-stroke depression at week 4 and had higher 50% HAMD improvement rate, while rTMS combined with paroxetine was more effective at week 8. Further research is needed to determine whether acupuncture combined with fluoxetine is better than rTMS combined with paroxetine for post-stroke depression at week 8. All conclusions still need to be justified by further clinical data.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding authors.
Author contributions
ZW and WY were the principal investigators. JZ designed the study and developed the analysis plan; JZ, GJ, and ZS analyzed the data and performed the meta-analysis; JZ, ZS, CG, and GJ contributed to the writing of the article. JZ, GC, and WC revised the manuscript and polished the language. All authors read and approved the final submitted paper.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fphar.2022.1035895/full#supplementary-material
Abbreviations
RCT, randomized controlled trial; OR, odds ratio; MD, mean difference; SUCRA, surface under the cumulative ranking curve; CI, confidence interval.
References
Bai, W., Liu, Y., and Li, Y. (2018). Efficacy of paroxetine and duloxetine in the treatment of post-stroke depression. Guizhou Med. J. 42 (4), 441–442. doi:10.3969/j.issn.1000-744X.2018.04.023
Blöchl, M., Meissner, S., and Nestler, S. (2019). Does depression after stroke negatively influence physical disability? A systematic review and meta-analysis of longitudinal studies. J. Affect. Disord. 247, 45–56. doi:10.1016/j.jad.2018.12.082
Cao, J., Liu, L., Sun, Y., Zeng, Q. H., Yang, Z. D., and Chen, J. C. (2020). Escitalopram improves neural functional prognosis and endothelial dysfunction in patients with acute cerebral infarction. Restor. Neurol. Neurosci. 38 (5), 385–393. doi:10.3233/RNN-201041
Chen, A., Gao, H., Wang, G., Li, J., and Shen, W. (2018). Effect of early acupuncture intervention on post-stroke depression: A randomized controlled trial. Chin. Acupunct. 38 (11), 1141–1144. doi:10.13703/j.0255-2930.2018.11.001
Chen, H. (2009). Clinical observation on 40 cases of post-stroke depression treated with shuganjieyutang. Guid. J. Traditional Chin. Med. Pharm. 15 (3), 23–25. doi:10.3969/j.issn.1672-951X.2009.03.011
Chen, M., and Li, P. Effectiveness of paroxetine in the treatment of poststroke depression. Med. Baltim. 2018; 97(29): e11496. DOI: doi: doi:10.1097/MD.0000000000011496
Chen, W., Tang, Y., and Zhao, Q. (2012). Clinical observation of duloxetine in the treatment of 48 cases of post-stroke depression. Zhejiang Praetical Med. 17 (6), 419–420. doi:10.3969/j.issn.1007-3299.2012.06.012
Chen, Z., Xu, X., and Wu, Y. (2015). Clinical effect of drug intervention in patients with post-stroke acute depression. J. Int. Psychiatry 42 (5), 97–100.
Cravello, L., Caltagirone, C., and Spalletta, G. (2009). The SNRI venlafaxine improves emotional unawareness in patients with post-stroke depression. Hum. Psychopharmacol. 24 (4), 331–336. doi:10.1002/hup.1021
Das, J., and Rajanikant, G. K. (2018). Post stroke depression: The sequelae of cerebral stroke. Neurosci. Biobehav. Rev. 90, 104–114. doi:10.1016/j.neubiorev.2018.04.005
Dong, J., Sun, W., Wang, S., Wu, Z. Q., and Liu, F. (2007). Clinical observation on head point-through-point electroacupuncture for treatment of poststroke depression. Chin. Acupunct. 27 (4), 241–244.
Dong, Z., Dai, Q., and Wang, F. (2003). Comparison of acupuncture and medicine in the treatment of post-stroke depression. Chin. Joumal Clin. Rehabilitation 7 (25), 3516. doi:10.3321/j.issn:1673-8225.2003.25.060
Feng, Q. (2015). A comparative study of escitalopram and sertraline in the treatment of post-stroke depression in the elderly. J. Clin. Psychosom. Dis. 3, 60–62. doi:10.3969/j.issn.1672-187X.2015.03.020-0060-03
Feng, Y. (2016). A randomized controlled study of paroxetine and sertraline in the treatment of post-stroke depression. Chin. J. Pract. Nerv. Dis. 19 (6), 114–115. doi:10.3969/j.issn.1673-5110.2016.06.078
Fruehwald, S., Gatterbauer, E., Rehak, P., and Baumhackl, U. (2003). Early fluoxetine treatment of post-stroke depression--a three-month double-blind placebo-controlled study with an open-label long-term follow up. J. Neurol. 250 (3), 347–351. doi:10.1007/s00415-003-1014-3
Furukawa, T. A., Cipriani, A., Cowen, P. J., Leucht, S., Egger, M., and Salanti, G. (2019). Optimal dose of selective serotonin reuptake inhibitors, venlafaxine, and mirtazapine in major depression: A systematic review and dose-response meta-analysis. Lancet. Psychiatry 6, 601–609. doi:10.1016/S2215-0366(19)30217-2
Gillman, P. K. (2007). Tricyclic antidepressant pharmacology and therapeutic drug interactions updated. Br. J. Pharmacol. 151, 737–748. doi:10.1038/sj.bjp.0707253
Gong, P., Ma, X., Gao, L., and Bi, J. (2021). Simple acupuncture combined with fluoxetine in the treatment of poststroke depression: A protocol for systematic review and meta-analysis. Med. Baltim. 100, e24968. doi:10.1097/MD.0000000000024968
Gu, S., and Chang, M. (2017). The effects of 10-hz repetitive transcranial magnetic stimulation on depression in chronic stroke patients. Brain Stimul. 10 (2), 270–274. doi:10.1016/j.brs.2016.10.010
Hadidi, N. N., Huna Wagner, R. L., and Lindquist, R. (2017). Nonpharmacological treatments for post-stroke depression: An integrative review of the literature. Res. Gerontol. Nurs. 10, 182–195. doi:10.3928/19404921-20170524-02
Hajcak, G., MacNamara, A., and Olvet, D. M. (2010). Event-related potentials, emotion, and emotion regulation: An integrative review. Dev. Neuropsychol. 35, 129–155. doi:10.1080/87565640903526504
Hamilton, M. (1967). Development of a rating scale for primary depressive illness. Br. J. Soc. Clin. Psychol. 6, 278–296. doi:10.1111/j.2044-8260.1967.tb00530.x
Hilari, K., Needle, J. J., and Harrison, K. L. (2012). What are the important factors in health-related quality of life for people with aphasia? A systematic review. Arch. Phys. Med. Rehabil. 93, S86–S95. doi:10.1016/j.apmr.2011.05.028
Hu, J., Li, C., and Yuan, L. (2017). A comparative study of the effects of escitalopram and mirtazapine on the quality of life in patients with post-stroke depression. Cap. J. Food Med. 24 (18), 69–70.
Hu, J., Li, Z., and Liu, Y. (2016). Efficacy of mirtazapine in the treatment of post-stroke depression. Chin. J. Integr. Med. Cardio 14 (23), 2822–2824. doi:10.3969/j.issn.1672-1349.2016.23.033
Hu, M., Li, M., and Chen, S. (2020). Application of repetitive transcranial magnetic stimulation combined with paroxetine hydrochloride in patients with post-stroke depression. J. Chin. Contemp. Med. 27 (18), 63–65. doi:10.3969/j.issn.1674-4721.2020.18.018
Huang, C., Pang, G., and Liang, H. (2014). Comparative study on the efficacy of escitalopram and venlafaxine sustained release in the treatment of post-stroke depression in the elderly. J. Pract. Cardio-cerebral Pulm. Vasc. Dis. 22 (4), 36–37. doi:10.3969/j.issn.1008-5971.2014.04.016
Huang, P., Chi, X., and Liu, R. (2011). Clinical study of shuganjieyutang in the treatment of post-stroke depression. Health industry China 31, 75.
Huang, W., Chen, W., and Wu, X. (2021). Observation on the therapeutic effect of acupuncture with visceral pentatonic tone method on post-stroke depression. World J. Integr. Traditional West. Med. 16 (12), 2334–2337. doi:10.13935/j.cnki.sjzx.211235
Lefaucheur, J-P., Aleman, A., Baeken, C., Benninger, D. H., Brunelin, J., Di Lazzaro, V., et al. (2020). Evidence-based guidelines on the therapeutic use of repetitive transcranial magnetic stimulation (rTMS): An update (2014-2018). Clin. Neurophysiol. 131, 474–528. doi:10.1016/j.clinph.2019.11.002
Leucht, S., Fennema, H., Engel, R., Kaspers-Janssen, M., Lepping, P., and Szegedi, A. (2013). What does the HAMD mean? J. Affect. Disord. 148, 243–248. doi:10.1016/j.jad.2012.12.001
Li, C., and Chen, J. (2012). Clinical efficacy and safety of citalopram and sertraline in the treatment of post-stroke depression. Guide China Med. 10 (36), 546–547. doi:10.15912/j.cnki.gocm.2012.36.782
Li, H. (2015). Clinical effect of venlafaxine in the treatment of post-stroke depression. Joumal Qiqihar Univ. Med. 36 (17), 2548–2549.
Li, H., Zhong, B., Fan, Y., and Hu, H. T. (2011). Acupuncture for post-stroke depression: A randomized controlled trial. Chin. Acupunct. 31 (01), 3–6. doi:10.13703/j.0255-2930.2011.01.002
Li, J., and Chi, L. (2011). A comparative study of duloxetine and amitriptyline in the treatment of post-stroke depression. Chin. J. Pract. Nerv. Dis. 14 (12), 30–31. doi:10.3969/j.issn.1673-5110.2011.12.016
Li, J., Wang, J., and Li, Y. (2017). Effects of escitalopram oxalate on post-stroke depression, cognition and neurological function. J. Hebei Med. Univ. 38 (5), 589–592. doi:10.3969/j.issn.1007-3205.2017.05.021
Li, M., Niu, J., Yan, P., Yao, L., He, W., Wang, M., et al. (2020). The effectiveness and safety of acupuncture for depression: An overview of meta-analyses. Complement. Ther. Med. 50, 102202. doi:10.1016/j.ctim.2019.102202
Li, M., Zhang, B., Meng, Z., Sha, T., Han, Y., Zhao, H., et al. (2017). Effect of Tiaoshen Kaiqiao acupuncture in the treatment of ischemic post-stroke depression:a randomized controlled trial. J. Traditional Chin. Med. 37 (02), 171–178. doi:10.1016/s0254-6272(17)30041-9
Li, P., Wang, H., and Sun, L. (2017). Comparison of efficacy and safety between sertraline and paroxetine in the treatment of post-stroke depression. China Pharm. 28 (36), 5098–5101. doi:10.6039/j.issn.1001-0408.2017.36.16
Li, R. (2016). Clinical efficacy of paroxetine in the treatment of stroke depression. China J. Pharm. Econ. 11 (3), 75–77. doi:10.12010/j.issn.1673-5846.2016.03.035
Li, X. (2014). A comparative study of escitalopram in the treatment of post-stroke depression and anxiety comorbidity. Chin. J. Mod. Drug Appl. 14, 151–152.
Li, X., and Yuan, G. (2015). Clinical observation of mirtazapine in the treatment of post-stroke depression. Front. J. Med. 5 (9), 45–47. doi:10.3969/j.issn.2095-1752.2015.09.024
Li, Z. (2007). Clinical observation of paroxetine tablets in the treatment of post-stroke depression. Mod. J. Integr. Traditional Chin. West. Med. 16 (34), 5103–5104.
Li, Z. (2014). Efficacy and safety of venlafaxine hydrochloride sustained release tablets in the treatment of post-stroke depression. Chin. J. Contemp. Med. 21 (9), 78–79.
Liang, X-X., Hao, Y-G., Duan, X-M., Han, X. L., and Cai, X. X. (2020). Hyperbaric oxygen therapy for post-stroke depression: A systematic review and meta-analysis. Clin. Neurol. Neurosurg. 195, 105910. doi:10.1016/j.clineuro.2020.105910
Lin, Z., Zhong, Y., and Quan, S. (2017). Acupuncture for post-stroke depression: A randomized controlled study. Chin. Acupunct. 37 (6), 581–585. doi:10.13703/j.0255-2930.2017.06.003
Liu, F. (2020). Effect of repeated transcranial magnetic stimulation combined with paroxetine hydrochloride on the efficacy and complications of patients with post-stroke depression. J. reflexology Rehabilitation Med. 1 (24), 133–135.
Liu, J., and Yan, X. P. (2012). Competitive aptamer bioassay for selective detection of adenosine triphosphate based on metal-paired molecular conformational switch and fluorescent gold nanoclusters. Biosens. Bioelectron. 50 (14), 135–141. doi:10.1016/j.bios.2012.04.015
Liu, L., Liu, C., Wang, Y., Wang, P., Li, Y., and Li, B. (2015). Herbal medicine for anxiety, depression and insomnia. Curr. Neuropharmacol. 13, 481–493. doi:10.2174/1570159x1304150831122734
Liu, X., Tian, W., Qiu, X., Li, J., Thomson, S., Li, L., et al. (2012). Correlation analysis of quantitative diffusion parameters in ipsilateral cerebral peduncle during Wallerian degeneration with motor function outcome after cerebral ischemic stroke. J. Neuroimaging 22, 255–260. doi:10.1111/j.1552-6569.2011.00617.x
Luo, R., Hu, C., and Chen, R. (2006). Effect of paroxetine on post-stroke depression. Chin. J. Rehabil. Theory Pract. 12 (7), 597–598.
Medeiros, G. C., Roy, D., Kontos, N., and Beach, S. R. (2020). Post-stroke depression: A 2020 updated review. Gen. Hosp. Psychiatry 66, 70–80. doi:10.1016/j.genhosppsych.2020.06.011
Mitchell, A. J., Sheth, B., Gill, J., Yadegarfar, M., Stubbs, B., Yadegarfar, M., et al. (2017). Prevalence and predictors of post-stroke mood disorders: A meta-analysis and meta-regression of depression, anxiety and adjustment disorder. Gen. Hosp. Psychiatry 47, 48–60. doi:10.1016/j.genhosppsych.2017.04.001
Nie, R., Huang, C., and Fu, W. (2011). [Observation of therapeutic effect on post stroke depression treated by differentiation of spleen and stomach]. Chin. Acupunct. 31 (4), 325–328.
Nie, R., and Huang, C. (2013). [Post-stroke depression treated with acupuncture and moxibustion: An evaluation of therapeutic effect and safety]. Chin. Acupunct. 33 (06), 490–494. doi:10.13703/j.0255-2930.2013.06.006
Paolucci, S. (2017). Advances in antidepressants for treating post-stroke depression. Expert Opin. Pharmacother. 18, 1011–1017. doi:10.1080/14656566.2017.1334765
Qin, B., Zhang, Y., Zhou, X., Cheng, P., Liu, Y., Chen, J., et al. (2014). Selective serotonin reuptake inhibitors versus tricyclic antidepressants in young patients: A meta-analysis of efficacy and acceptability. Clin. Ther. 36, 1087–1095. doi:10.1016/j.clinthera.2014.06.001
Rampello, L., Nicoletti, G., Raffaele, R., and DragoF., (1995). Comparative effects of amitriptyline and amineptine in patients affected by anxious depression. Neuropsychobiology 31, 130–134. doi:10.1159/000119183
Robinson, R. G., and Jorge, R. E. (2016). Post-stroke depression: A review. Am. J. Psychiatry 173, 221–231. doi:10.1176/appi.ajp.2015.15030363
Shao, J., and Qing, X. (2012). Effects of escitalopram on psychological status and quality of life in patients with post-stroke depression. Chin. J. Hosp. Pharm. 32 (13), 1047–1050.
Shi, Y., Yang, D., Zeng, Y., and Wu, W. (2017). Risk factors for post-stroke depression: A meta-analysis. Front. Aging Neurosci. 9, 218. doi:10.3389/fnagi.2017.00218
Song, W., Liu, Y. y., Peng, J. j., Liang, H. h., Chen, H. y., Chen, J. h., et al. (2016). Identification of differentially expressed signatures of long non-coding RNAs associated with different metastatic potentials in gastric cancer. J. Gastroenterol. 24 (5), 119–129. doi:10.1007/s00535-015-1091-y
Starkstein, S. E., and Hayhow, B. D. (2019). Treatment of post-stroke depression. Curr. Treat. Options Neurol. 21, 31. doi:10.1007/s11940-019-0570-5
Sun, P., Chu, H., Li, P., Wang, T., Pu, F., Wu, J., et al. (2015). [The effect of the acupuncture intervention of dredging Governor Vessel and regulating mentality for the medication treatment of post-stroke depression]. Chin. Acupunct. 35 (8), 753–757. doi:10.13703/j.0255-2930.2015.08.001
Sun, Y., Bao, Y., Wang, S., Chu, J., and Li, L. (2015). Efficacy on post-stroke depression treated with acupuncture at the acupoints based on ziwuliuzhu and prozac. Chin. Acupunct. 35 (2), 119–122. doi:10.13703/j.0255-2930.2015.02.004
Taylor-Rowan, M., Momoh, O., Ayerbe, L., Evans, J. J., Stott, D. J., and Quinn, T. J. (2019). Prevalence of pre-stroke depression and its association with post-stroke depression: A systematic review and meta-analysis. Psychol. Med. 49, 685–696. doi:10.1017/S0033291718002003
van Valkenhoef, G., Dias, S., Ades, A. E., and Welton, N. J. (2016). Automated generation of node-splitting models for assessment of inconsistency in network meta-analysis. Res. Synth. Methods 7, 80–93. doi:10.1002/jrsm.1167
van Valkenhoef, G., Lu, G., de Brock, B., Hillege, H., Ades, A. E., and Welton, N. J. (2012). Automating network meta-analysis. Res. Synth. Methods 3, 285–299. doi:10.1002/jrsm.1054
Villa, R. F., Ferrari, F., and Moretti, A. (2018). Post-stroke depression: Mechanisms and pharmacological treatment. Pharmacol. Ther. 184, 131–144. doi:10.1016/j.pharmthera.2017.11.005
Wang, G., and Qiu, G. (2015). Efficacy of sertraline on depression and effect on IL-6 IL-1β TNF-α in stroke patients. Anhui Med. J. 11, 1384–1386. doi:10.3969/j.issn.1000-0399.2015.11.021
Wang, G., Zhen, L., and Zhang, S. (2017). Comparison of efficacy between escitalopram and paroxetine in the treatment of elderly patients with chronic cerebral infarction depression. Pract. Geriatr. 31 (6), 578–581.
Wang, L., Yu, X., Wang, H., Lu, Y. Z., de Ruiter, M., Prins, M., et al. (2011). A novel class of heat-responsive small RNAs derived from the chloroplast genome of Chinese cabbage (Brassica rapa). BMC Genomics 13 (2), 289–291. doi:10.1186/1471-2164-12-289
Wang, R., Zhao, C., and Qin, X. (2020). Clinical efficacy and mechanism of low frequency repetitive transcranial magnetic stimulation combined with paroxetine in the treatment of post-stroke depression. Neural Inj. Funct. Reconstr. 15 (6), 349–351. doi:10.16780/j.cnki.sjssgncj.20190548
Wang, X. (2009). Effect of paroxetine on 55 cases of post-stroke depression. Chin. Community Dr. 11 (7), 11. doi:10.3969/j.issn.1007-614x.2009.07.008
Wei, H., Wu, Z., and Gao, Y. (2014). Efficacy of citalopram in the treatment of depression after cerebral infarction in the elderly. Chin J Clin. Ration. Drug Use 17, 59–60.
Wu, J. (2009). Clinical observation of sertraline in the treatment of post-stroke depression. Chin. J. Pract. Nerv. Dis. 12 (19), 33–34. doi:10.3969/j.issn.1673-5110.2009.19.019
Wu, J. (2010). [Clinical observation on acupuncture treatment of 150 cases of post-stroke depression according to syndrome differentiation]. Acupunct. Res. 35 (4), 303–306.
Wu, S., Chen, X. Q., Kong, X., Yin, P. L., Dong, L., Liao, P. Y., et al. (2016). Characteristics of respiratory syncytial virus-induced bronchiolitis co-infection with Mycoplasma pneumoniae and add-on therapy with montelukast. World J. Pediatr. 3, 88–95. doi:10.1007/s12519-015-0024-4
Wu, S., Xu, J., and Guo, H. (2013). A comparative study of escitalopram and paroxetine in the treatment of post-stroke depression in the elderly. Hei long jiang Med. J. 37 (1), 8–10. doi:10.3969/j.issn.1004-5775.2013.01.003
Yan, D., Shan, J., Ze, Y., Xiao-Yan, Z., and Xiao-Hua, H. (2015). The effects of combined hyperbaric oxygen therapy on patients with post-stroke depression. J. Phys. Ther. Sci. 27 (5), 1295–1297. doi:10.1589/jpts.27.1295
Yang, H., Zhang, Y., and Xu, Y. (2019). Efficacy of high frequency rTMS combined with paroxetine in the treatment of post-stroke depression. Yunnan Med. J. 40 (6), 552–554.
Ye, B., and Ye, D. (2018). Effects of sertraline on hypothalamic-pituitary-adrenergic axis and cognitive function in depressed patients after ischemic stroke. China Mod. Dr. 56 (25), 38–41.
You, Y., Zhang, T., Shu, S., Qian, X., Zhou, S., and Yao, F. (2020). Wrist-ankle acupuncture and fluoxetine in the treatment of post-stroke depression: A randomized controlled clinical trial. J. Traditional Chin. Med. 40 (3), 455–460. doi:10.19852/j.cnki.jtcm.2020.03.014
Zhang, C. (2005). The brain-resuscitation acupuncture method for treatment of post wind-stroke mental depression--a report of 45 cases. J. Tradit. Chin. Med. 25 (4), 243–246.
Zhang, Z-J., Chen, H-Y., Yip, K., Ng, R., and Wong, V. T. (2010). The effectiveness and safety of acupuncture therapy in depressive disorders: Systematic review and meta-analysis. J. Affect. Disord. 124, 9–21. doi:10.1016/j.jad.2009.07.005
Zhao, F., Xu, S., and Zhang, Q. (2005). Comparison of citalopram and venlafaxine in improving post-stroke depression. Chin. J. Clin. Rehabilitation 9 (12), 12–13. doi:10.3321/j.issn:1673-8225.2005.12.014
Zhao, Y., and Li, H. (2006). Clinical observation on 23 cases of post-stroke depression treated by acupuncture. J. Clin. Acupunct. moxibustion 22 (7), 19–20. doi:10.3969/j.issn.1005-779.2006.07.008
Zhou, L., Wang, T., Yu, Y., Li, M., Sun, X., Song, W., et al. (2022). The etiology of poststroke-depression: A hypothesis involving HPA axis. Biomed. Pharmacother. 151, 113146. doi:10.1016/j.biopha.2022.113146
Keywords: post-stroke depression, antidepressant, adjuvant therapy, meta-analysis, Hamilton depression scale (HAMD)
Citation: Zhang J, Song Z, Gui C, Jiang G, Cheng W, You W, Wang Z and Chen G (2022) Treatments to post-stroke depression, which is more effective to HAMD improvement? A network meta-analysis. Front. Pharmacol. 13:1035895. doi: 10.3389/fphar.2022.1035895
Received: 03 September 2022; Accepted: 02 December 2022;
Published: 19 December 2022.
Edited by:
Ying Xu, University at Buffalo, United StatesReviewed by:
Bun Tsoi, Hong Kong Polytechnic University, Hong Kong SAR, ChinaLena Kaethe Linda Oestreich, The University of Queensland, Australia
Copyright © 2022 Zhang, Song, Gui, Jiang, Cheng, You, Wang and Chen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zhong Wang, d2FuZ3pob25nNzYxQDE2My5jb20=; Wanchun You, d2N5b3VAc3VkYS5lZHUuY24=
†These authors have contributed equally to this work
 Jie Zhang†
Jie Zhang† Wanchun You
Wanchun You Zhong Wang
Zhong Wang Gang Chen
Gang Chen