- 1The Second School of Clinical Medicine, Zhejiang Chinese Medical University, Hangzhou, China
- 2School of Life Sciences, Zhejiang Chinese Medical University, Hangzhou, China
- 3School of Pharmaceutical Sciences, Zhejiang Chinese Medical University, Hangzhou, China
Background: Keeping in view the high recurrence rate and risk of ischemic stroke, combinatorial therapy involving traditional Chinese medicine (TCM) with conventional Western medicine (WM) is receiving wider scientific attention. Thus, a systematical analysis was made to explore the efficacy of TCM+WM in the long-term secondary prevention for patients with ischemic stroke.
Methods: Qualified inclusion and exclusion criteria were set up beforehand, and two researchers independently read the articles, extracted data, and evaluated the quality of included articles according to Cochrane Reviewer’s Handbook 5.1 method. For the sake of comprehensive data acquisition, seven databases from the time of their establishment to May 5, 2021, have been searched completely. Additionally, pairwise meta-analysis was made to compare TCM+WM vs. WM, and network meta-analysis was conducted by frequentist random effects models for the comparison of different kinds of TCM+WM via indirect evidence. The primary outcomes defined were recurrent stroke and NIHSS. Secondary outcomes were fibrinogen (Fib) fasting blood glucose (FBG), triglycerides (TG), and total cholesterol (TC). Safety outcomes were outlined as all-cause mortality and adverse events (AEs). Furthermore, Stata16.0 software was used to accomplish the systematical analysis and cluster analysis.
Results: In total, 47 qualified randomized controlled trials (RCTs) including 10,732 patients were taken into consideration. Seven traditional Chinese medicines included in the study are Naoxintong capsule (NXT), Tongxinluo capsule (TXL), Buyang Huanwu decoction (BYHW), Naomaitai capsule (NMT), Dengzhan Shengmai capsule (DZSM), Naoshuantong capsule (NST), and Maixuekang capsule (MXK). With respect to their primary outcomes, all kinds of TCM+WM were significantly more effective than WM (e.g., NXT in recurrent stroke (OR=0.54, P<0.01), TXL in NIHSS (WM=−1.4, P<0.01)). Additionally, the outcomes of cluster analysis indicated that MXK+WM and NST+WM had relatively good preventive effects for recurrent stroke, NIHSS, and all-cause mortality. There was no significant difference in the comparisons of AEs; however, this may arise from the lack of sufficient data.
Conclusion: According to our systematical analysis, MXK+WM and NST+WM had relatively good secondary prevention effects for patients with ischemic stroke regarding recurrent stroke, NIHSS, and all-cause mortality. Nevertheless, better, high-quality, large-sample randomized clinical trials (RCTs) are required to verify our conclusions in the future.
Systematic Review Registration: [https://inplasy.com/inplasy-2021-5-0036/], identifier [INPLASY202150036].
Introduction
Stroke causes nearly 5% of all disabilities (Collaborators, 2017b) and about 10% of deaths around the world (Collaborators, 2017a). In addition, ischemic stroke accounts for about 70% of the total death caused by stroke (Feigin et al., 2018). Moreover, a good volume of research showed that the cumulative long-term risk of recurrence of stroke is 11.1% at 1 year and 26.4% at 5 years (Mohan et al., 2011). Besides, patients with ischemic stroke are faced with a higher risk of vascular events or death (Kernan et al., 2014; Amarenco et al., 2016). Furthermore, some researchers said that taking secondary prevention on time will decrease the risk of stroke recurrence by about 80% (Hackam and Spence, 2007; Rothwell et al., 2007). Therefore, it is essential to take appropriate measures to avoid the recurrence of stroke.
According to the American Heart Association/American Stroke Association guideline (AHA/ASA), conventional Western medicine for stroke treatment includes hypoglycemic drugs, antihypertensive drugs, antiplatelet drugs, hypolipidemic drugs, etc. (Kernan et al., 2014). However, the combination of clopidogrel and aspirin is not any more effective than either aspirin or clopidogrel monotherapy, and gives rise to a higher risk of bleeding (Diener et al., 2004; Bhatt et al., 2006; Bhatt et al., 2007). Some patients are resistant to antiplatelet drugs (Guo et al., 2019). Moreover, one study has shown that statins for the treatment of stroke can increase the relative risk of new onset diabetes by 9% (Gao, 2015). New treatment methods are thus warranted.
Traditional Chinese medicine (TCM) is attracting increasing attention on account of its exact curative effect and low toxicity (Bu et al., 2020). In addition, in pre-thrombotic conditions, TCM is a multi-link, multi-target which effectively prevents the recurrence of ischemic stroke (Kang and Li, 2012). Furthermore, TCM plays a significant role in the prevention of cerebrovascular disease and recovery of limb function (Zhang et al., 2012).
For example, a randomized controlled trial (RCT) showed that Naoxintong capsule (NXT) had a positive effect on the prevention of recurrence of stroke (Sun, 2020), and another RCT indicated that Tongxinluo capsule (TXL) promoted the recovery of nerve function (Bo et al., 2017). In this study, NXT, TXL, Buyang Huanwu decoction (BYHW), Naomaitai capsule (NMT), Dengzhan Shengmai capsule (DZSM), Naoshuantong capsule (NST), and Maixuekang capsule (MXK) were made a part of the systematical analysis.
At present, there are only a few reviews and meta-analyses on the long-term secondary prevention of cerebral infarction by the combination of Western medicine (WM) and traditional Chinese medicine (TCM). One of the few studies showed that Buyang Huanwu decoction has no statistical significance in reducing the recurrence rate of ischemic stroke (Xie, 2015), possibly because of the lack of any significant literature at that time. Different from traditional pairwise meta-analysis, network meta-analysis (NMA) allows various treatments to be compared and ranked through direct and indirect contrasts to select the best ones (De Laat, 2017). However, comparisons of efficacy across different types of TCM are still inconclusive, causing confusion among physicians and patients.
Therefore, this study is intended to use systematical analysis including pairwise and network meta-analysis to compare the long-term secondary prevention effects and safety of the addition of different kinds of traditional Chinese medicines against ischemic stroke. In addition, the stroke risk factors of different kinds of TCM were also compared to provide references for the study regarding the cause of recurrence. This article will help researchers to better understand the advantages of TCM in the treatment of stroke and offer better assistance for clinical applications.
Materials and Methods
Our systematical analysis was registered in the International Platform of Registered Systematic Review and Meta-Analysis Protocols (INPLASY) under the registration number INPLASY202150036. The analysis was carried out according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (Hutton et al., 2015) (Supplementary Material S1). The abbreviations used in this manuscript have been listed in Supplementary Material S2.
Eligibility and Exclusion Criteria
The (Patient/Intervention/Comparison/Outcome/Study design) PICOS framework was employed as our eligibility criteria, thus only randomized controlled trials (RCTs) consistent with the following requirements were taken into our consideration: (1) Participants: patients with the diagnosis of ischemic stroke with no limitation on nationality, race, gender, age, and disease duration; (2) Interventions and comparisons: the treatment group was given conventional WM plus TCM, and the control group adopted another kind of TCM plus WM or WM alone. In addition, the WM treatment must be the same between treatment and control groups. The common WM drugs were antiplatelet, statins, antihypertensive drugs, hypoglycemic drugs, etc. whereas TCM included NXT, TXL, BUHW, NMT, DZSM, NST, and MXK. Besides, there were no limitations on dosage and the follow-up time was defined as more than 2 months; (3) Outcomes: the primary outcomes of this systematical analysis were recurrent stroke and the National Institute of Health stroke scale (NIHSS). Additionally, the secondary outcomes were stroke risk factors including elevated fibrinogen (Fib), fasting blood glucose (FBG), triglycerides (TG), and total cholesterol (TC). Moreover, the safety outcomes were all-cause mortality and adverse events (AEs). In this systematical analysis, RCT which included one of the primary outcomes was sufficient. Furthermore, the reasons behind choosing these secondary outcomes are the fact that increases in Fib (Refaai et al., 2018), FBG (Lawes et al., 2004), TG (Yuan et al., 2020), and TC (Yuan et al., 2020) have a close association with ischemic stroke or cardiovascular events; and (4) Study design: Only RCTs were taken into consideration for the current investigation.
RCTs would be excluded if they were in accordance with the following criteria: (1) The follow-up time was less than 2 months; (2) the treatment methods include acupuncture or other kinds of TCM; (3) publications were duplicated; (4) data was incomplete; (5) there were no relevant outcomes; and (6) the patients had serious complications.
Search Strategy
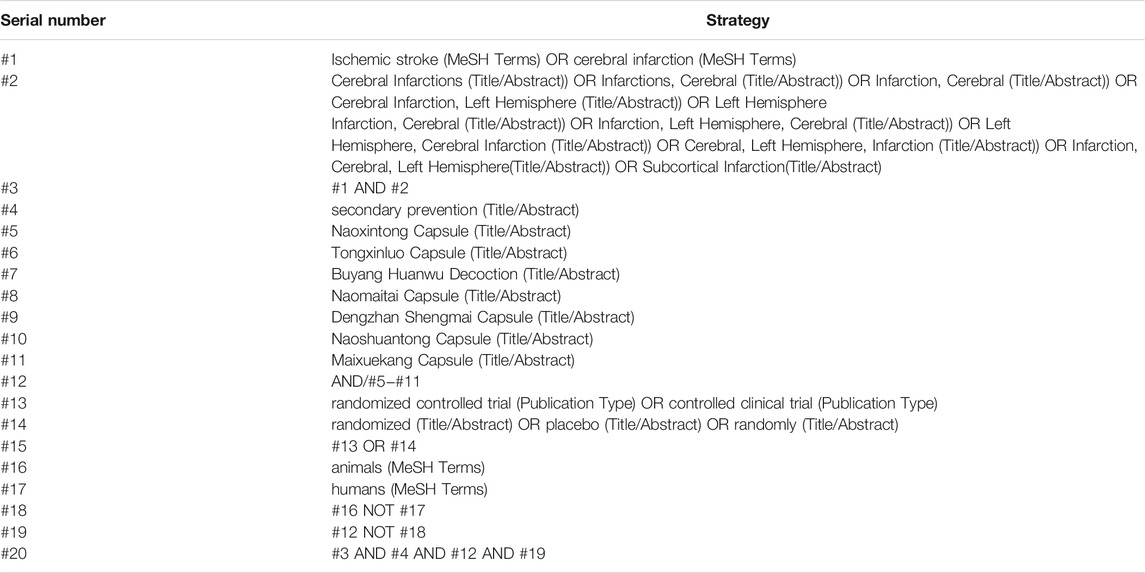
PubMed, Web of Science, embase, China National Knowledge Infrastructure (CNKI), Chinese Biological Medicine Literature Service System (CBM), China Science and Technology Journal database (VIP), and Wan−fang database (WF) were searched for this investigation. The included studies were published in the period starting from the foundation of each database to May 5, 2021. The topic search used was the combination of medical topic title terminology and free text terminology. Searched terms included “ischemic stroke,” “cerebral infarction,” “secondary prevention,” “Naoxintong Capsule,” “Tongxinluo Capsule,” “Buyang Huanwu Decoction,” “Naomaitai Capsule,” “Dengzhan Shengmai Capsule,” “Naoshuantong Capsule,” and “Maixuekang Capsule”. The detailed search process of PubMed is outlined in Table 1. Furthermore, references in the literature were searched manually.
Literature Inclusion and Data Extraction
Endnote 20.0 software was utilized for creating a library of the obtained articles and the literature inclusion was done by two researchers independently. Duplicated articles were excluded first. The titles and abstracts of articles were then thoroughly read for primary screening in accordance with the inclusion and exclusion criteria. The next step involved the re-screening of the articles via reading full-text content based on the inclusion and exclusion criteria. A third researcher would additionally participate in the discussion if at any stage the results were controversial. Moreover, relevant data were extracted which included publication date, author’s name, title, detailed characteristics of participants (sample capacity, age, sex), interventions (drug, dose, and follow-up time), outcomes (primary outcomes, secondary outcomes, and safety outcomes), and elements which were used to evaluate the risk of bias. Furthermore, since our research was related to ethnopharmacology, the compositions of included medicines were clearly recorded (Heinrich et al., 2020). In addition, all botanical plants were named according to the existing international standards in databases (Rivera et al., 2014).
Risk of Bias Assessment
According to the Cochrane risk of bias tool (Higgins et al., 2011), the quality assessment of all included RCTs was conducted by two researchers independently. Every RCT was classified as low, unclear, or high risk of bias based on seven quality evaluation items precisely: selection bias (random sequence generation and allocation concealment), performance bias (blinding of participants and personnel), detection bias (blinding of outcome assessment), attrition bias (incomplete outcome data), reporting bias (selective reporting), and other bias. In addition, when assessing outcomes, the objective outcomes (e.g., recurrent stroke) and subjective outcomes (e.g., NIHSS) were considered separately. When a discordance exists between two researchers, the ultimate outcomes would be resolved by consensus with a third researcher.
Statistical Analysis
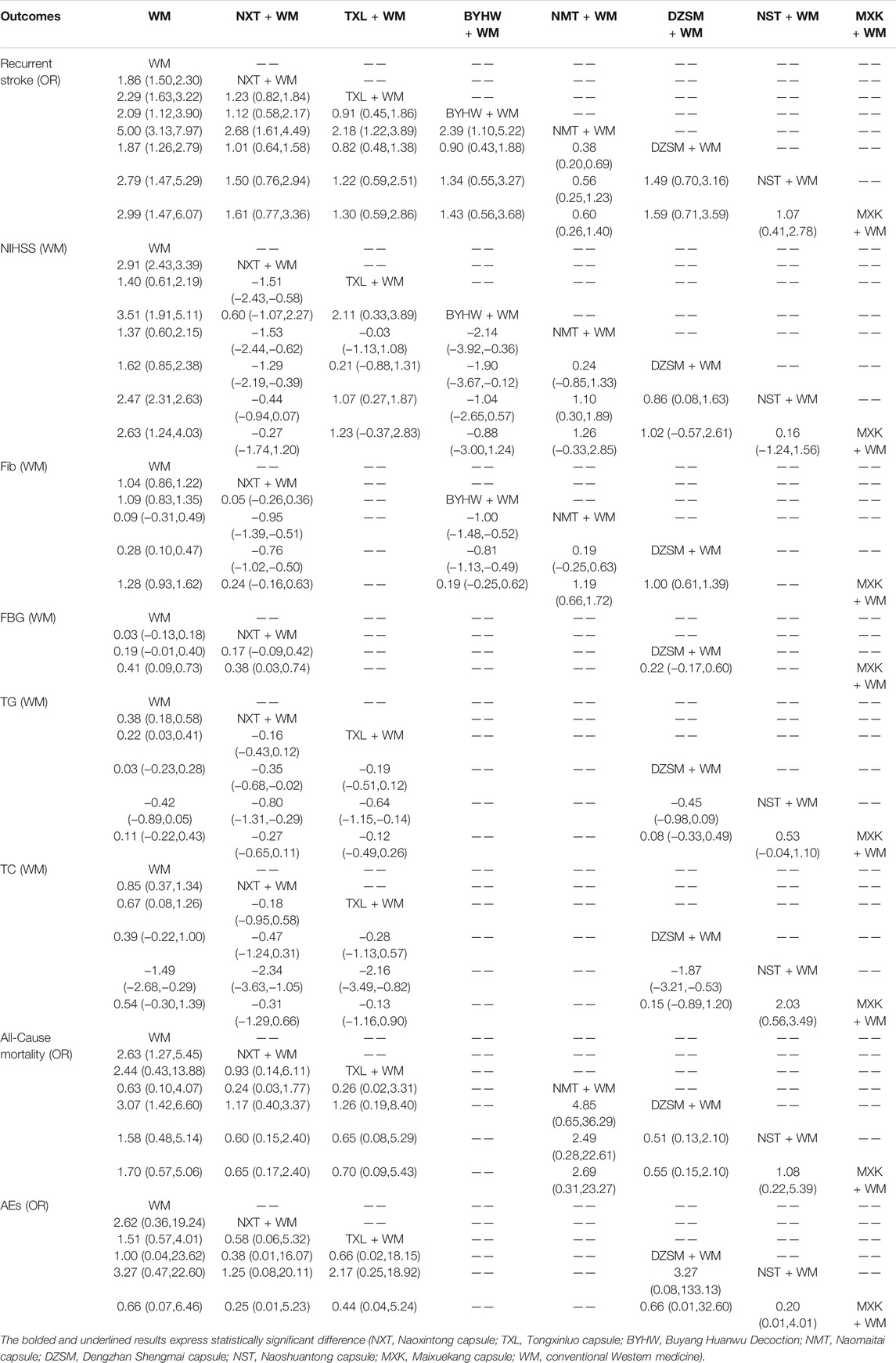
For binary variables, the outcomes were shown as odds ratios (ORs) as well as 95% confidence intervals (95% CIs). For continuous variables, the outcomes were presented as the mean differences (MDs) as well as 95% CIs. Moreover, the results were significantly different when 95% CIs of ORs did not contain 1 or 95% CIs of MDs did not include 0. In addition, if each outcome had at least two studies, the pairwise meta-analysis would be performed with a random effects model. Besides, different interventions would be compared by network meta-analysis under a frequentist framework with a random effects model. League tables were also utilized to display the findings of the systematical analysis. The chance of each treatment included in the systematical analysis being the best was evaluated using the surface under the cumulative ranking curve area (SUCRA) to obtain the best treatment (Salanti et al., 2011). In addition, cluster analysis was used to determine the optimum therapy for ischemic stroke.
In the standard pairwise meta-analysis, the statistical heterogeneity was tested by the calculation of I2 statistics and the clinical heterogeneity was assessed by comparisons of data on potential effect modifiers. If the I2 ≤ is 50%, the heterogeneity is not obvious (Higgins et al., 2003). Since each network graph was not looped, the incoherence (the statistical disagreement between direct and indirect results) could not be evaluated. In systematical analysis, we also assumed a consistent estimate for the heterogeneity variance. The distribution of putative effect modifiers was examined to determine transitivity between treatment comparisons (Turner et al., 2012).
If the number of studies was adequate, funnel plots were used to determine the presence of publication bias. Furthermore, the GRADE evaluation would serve as the foundation for the quality assessment, which would cover the five aspects of research restriction: study limitation, indirectness, inconsistency, imprecision, and publication bias (Salanti et al., 2014). A subgroup meta-analysis was also performed to evaluate the following possible effect modifiers (source of heterogeneity): 1. Treatment dosage (low dose, median dose, and high dose). 2. The age of patients (mean age less than 60 and mean age not less than 60). 3. The specific methods of WM (with statins and without statins). Finally, a post hoc sensitivity analysis was made: we used a leave−one−out meta-analysis to identify the independent impact of each study on the pooled estimates. We use Stata 16.0 software to get the statistical outcomes and statistical graphing of this systematical analysis.
Results
Literature Selection
A total of 2094 articles were obtained at first, including 541 articles from CNKI, 808 articles from WanFang data, 674 articles from CBM, 66 articles from VIP, 3 articles from PubMed, 0 and 2 articles, respectively, from the web of science and embase. After de-duplicating articles, a total of 1271 articles were taken into consideration. Then, following a thorough reading of the title and abstract of each publication, we excluded the publications that were not relevant to our systematical analysis. Furthermore, the full text of the remaining 196 articles was carefully read to find articles that met our PICOS principles. In the end, 47 articles were taken into consideration. In conclusion, only RCTs about the comparison between TCM + WM and WM were ultimately chosen. Furthermore, the conditions of patients and treatment methods must meet our pre-determined requisites. Moreover, the outcomes in the literature must have one of the primary outcomes. In addition, the follow-up time must be longer than 2 months. We show the PRISMA diagram about the further details of the article screening process in Figure 1.
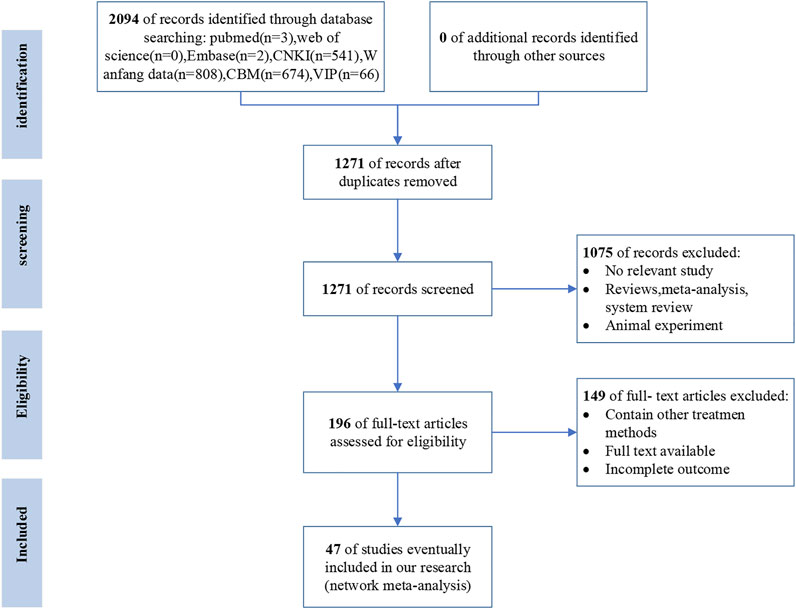
FIGURE 1. Flow diagram of literature screening (CNKI, National Knowledge Infrastructure; CBM, the Chinese Biological Medicine Literature Service System; VIP, the Chinese Scientific Journal Full−text database; WF, the Wan−fang database; n, number of articles).
Study Characteristics
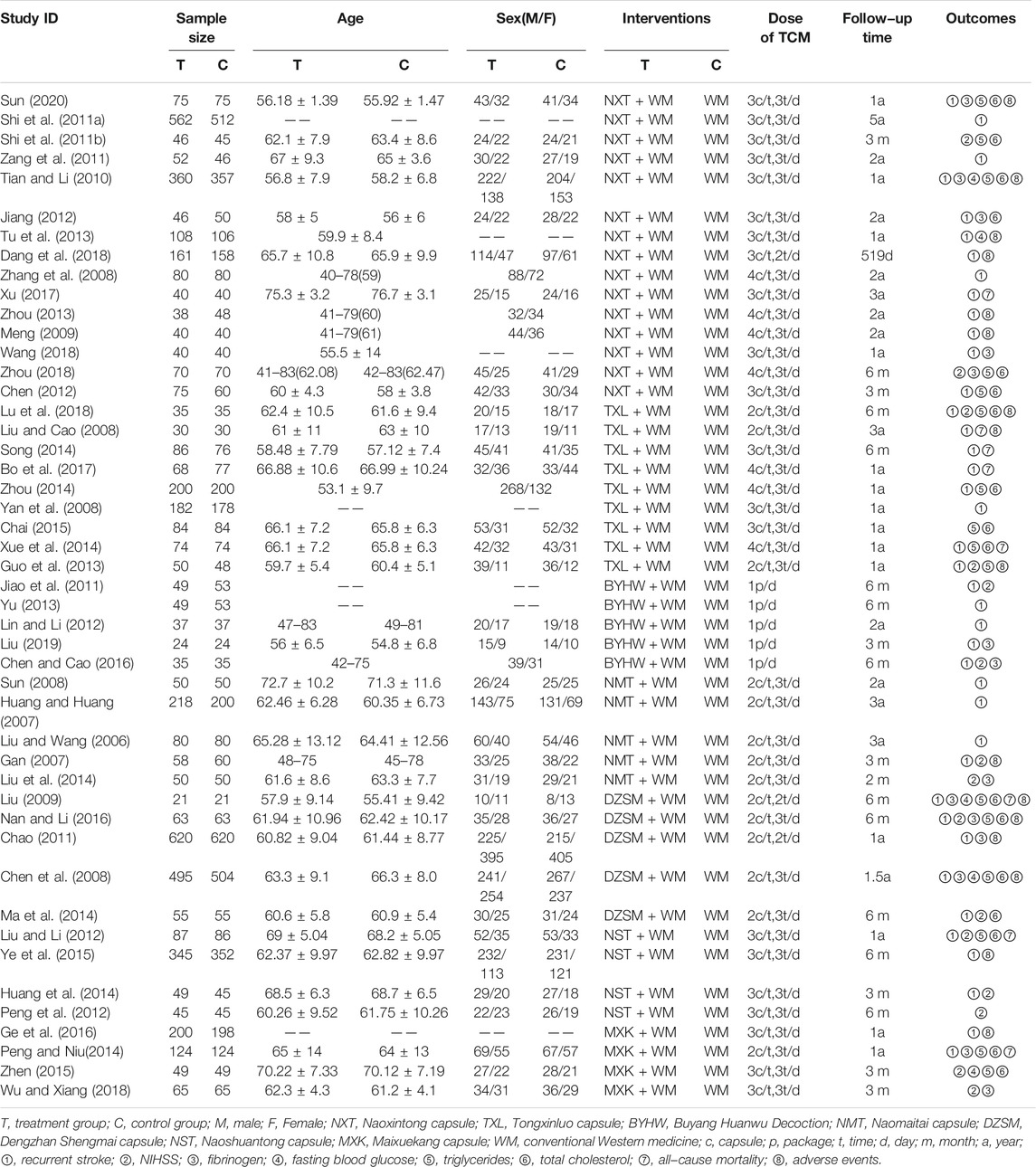
On the whole, there were 47 RCTs (Liu and Wang, 2006; Gan, 2007; Huang and Huang, 2007; Chen et al., 2008; Liu and Cao, 2008; Sun, 2008; Yan et al., 2008; Zhang et al., 2008; Liu, 2009; Meng, 2009; Tian and Li, 2010; Shi D. H. et al., 2011; Shi F. H. et al., 2011; Chao, 2011; Jiao et al., 2011; Zang et al., 2011; Chen, 2012; Jiang, 2012; Lin and Li, 2012; Peng et al., 2012; Guo et al., 2013; Tu et al., 2013; Yu, 2013; Zhou, 2013; Huang et al., 2014; Liu et al., 2014; Ma et al., 2014; Peng and Niu, 2014; Song, 2014; Xue et al., 2014; Zhou, 2014; Chai, 2015; Ye et al., 2015; Zhen, 2015; Chen and Cao, 2016; Ge et al., 2016; Nan and Li, 2016; Bo et al., 2017; Xu, 2017; Dang et al., 2018; Lu et al., 2018; Wang, 2018; Wu and Xiang, 2018; Zhou, 2018; Liu, 2019; Sun, 2020) involving 10,732 patients. Most of the patients involved in the trial were middle-aged and elder. All articles were about two-arm comparisons between TCM + WM and WM, and seven comparisons were made a part of our systematical analysis: NXT + WM vs. WM (n = 15), TXL + WM vs. WM (n = 9), BYHW + WM vs. WM (n = 5), NMT + WM vs. WM (n = 5), DZSM + WM vs. WM (n = 5), NST + WM vs. WM (n = 4), MXK + WM vs. WM (n = 4). Moreover, the most used drugs were aspirin, statins, and antihypertensive drugs. The median follow-up time was found to be 1 year (range, 2 months to 5 years). More details of the included articles are described in Table 2. Additionally, the specific intervention methods of TCM in each publication have been demonstrated in Supplementary material S3 Other detail information can be found in Supplementary material S4 which demonstrated indications and chemical analysis of each TCM and Supplementary material S5 which depicted compositions and extraction procedure of each TCM. Moreover, the network graphs of the above seven kinds of TCM + WM have been listed in Figure 2. About Figure 2, the size of the point is assigned by the total number of people in each study, and the width of the edge is assigned by the standard error.
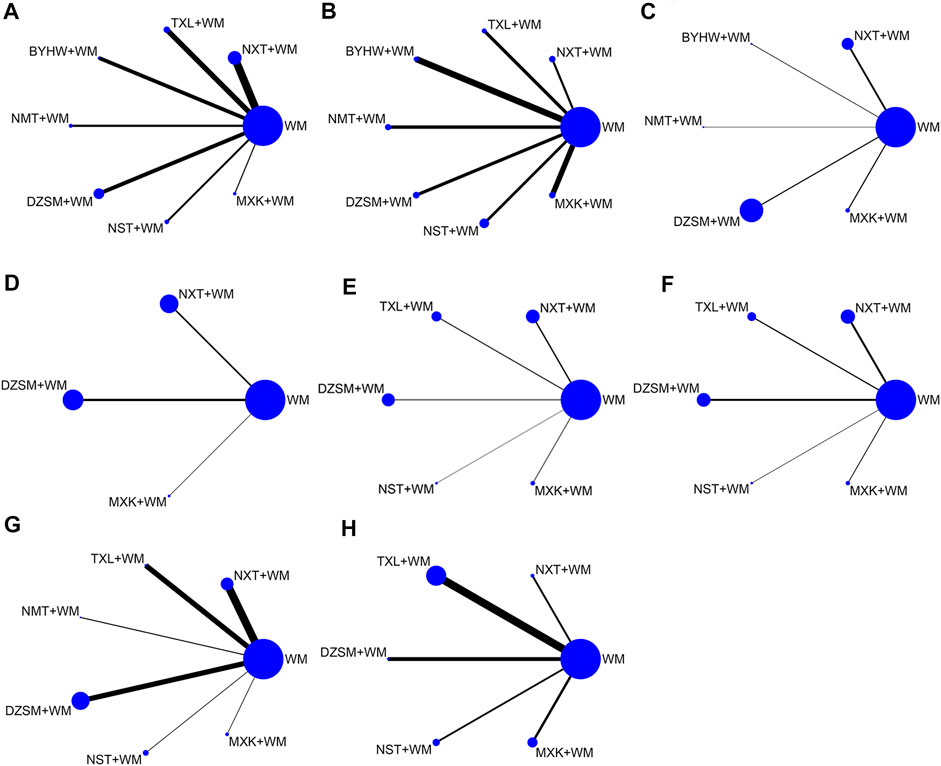
FIGURE 2. Network graphs for various outcomes. The size of the point is assigned by the total number of people in each study, and the width of the edge is assigned by standard error. (A) Recurrent stroke; (B) NIHSS; (C) Fib; (D) FBG; (E) TG; (F) TC; (G) all−cause mortality; (H) AEs (NXT, Naoxintong capsule; TXL, Tongxinluo capsule; BYHW, Buyang Huanwu Decoction; NMT, Naomaitai capsule; DZSM, Dengzhan Shengmai capsule; NST, Naoshuantong capsule; MXK, Maixuekang capsule; WM, conventional Western medicine; Fib, fibrinogen; FBG, fasting plasma glucose; TG, triglycerides; TC, cholesterol; AEs, adverse events).
Risk of Bias Assessment
When it comes to random sequence generation, 16 articles used random number tables or other random methods, therefore these articles were presumed to have a low risk of bias. On the contrary, two articles generated random sequences according to the admission time, which will lead to a high risk of bias. Regarding allocation concealment, three RCTs highlighted that random sequences would be kept by a third party; they were thus evaluated to have a low risk of bias. In terms of performance bias, two articles mentioned the performance of the double-blind method leading to a low risk of bias. Nevertheless, seven articles did not use a placebo, thus the evaluation was “high.” In terms of blinding of outcome assessment, two articles were assessed to have a low risk for using the double-blind method. Moreover, since all articles had no incomplete data, we classify them as low risk. Due to the lack of sufficient information, the biased entries of other aspects in each article were evaluated to be “unclear.” In conclusion, the quality of included articles was poor. Summary of the risk of bias is demonstrated in Figure 3 in which green indicates a low risk of bias, yellow indicates a medium risk of bias, and red indicates a high risk of bias.
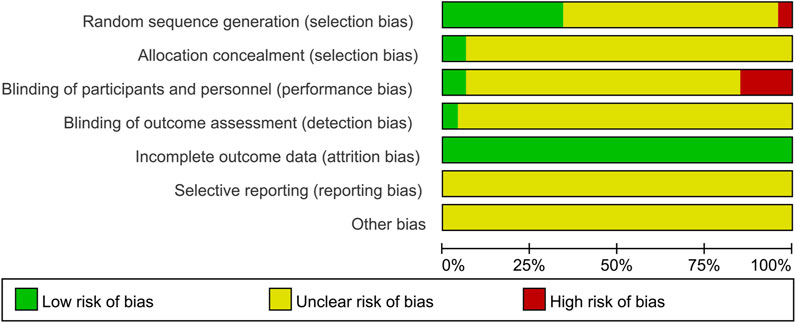
FIGURE 3. Summary of the risk of bias. The vertical axis represents the quality evaluation items, and the horizontal axis represents the number of randomized controlled trials. Herein green indicates low risk of bias, yellow indicates medium risk of bias, and red indicates high risk of bias.
Outcomes
Recurrent Stroke
In total, 40 studies involving 7 treatments regarding recurrent stroke were evaluated: NXT + WM vs. WM (n = 13), TXL + WM vs. WM (n = 8), BYHW + WM vs. WM (n = 5), NMT + WM vs. WM (n = 4), DZSM + WM vs. WM (n = 5), NST + WM vs. WM (n = 3), MXK + WM vs. WM (n = 2). All types of TCM + WM were superior to WM alone, and the results were significantly different. Table 3 shows the detailed information of comparisons: NXT + WM vs. WM (OR = 0.54, 95%CIs (0.43, 0.66)), TXL + WM vs. WM (OR = 0.44, 95%CIs (0.31, 0.61)), BYHW + WM vs. WM (OR = 0.48, 95%CIs (0.26, 0.89)), NMT + WM vs. WM (OR = 0.20, 95%CIs (0.13, 0.32)), DZSM + WM vs. WM (OR = 0.53, 95%CIs (0.36, 0.79)), NST + WM vs. WM (OR = 0.36, 95%CIs (0.19, 0.68)), MXK + WM vs. WM (OR = 0.33, 95%CIs (0.16, 0.68)). Furthermore, NMT + WM vs. NXT + WM (OR = 0.37, 95%CIs (0.22, 0.62)), NMT + WM vs. TXL + WM (OR = 0.46, 95%CIs (0.26, 0.82)), NMT + WM vs. BYHW + WM (OR = 0.42, 95%CIs (0.19, 0.91)), NMT + WM vs. DZSM + WM (OR = 0.38, 95%CIs (0.20, 0.69)) were related to significantly reduce recurrent stroke. Other comparisons did not have statistically significant differences.
Based on the outcomes of SUCRA probabilities (Table 4; Figure 4), NMT + WM was most likely to be the best choice. In addition, the detailed ranking results of those seven kinds of TCM + WM were depicted as follows: NMT + WM (97.0%) > MXK + WM (71.1%) > NST + WM (66.5%) > TXL + WM (54.1%) > BYHW + WM (44.6%) > DZSM + WM (34.5%) > NXT + WM (32.1%) > WM (0.2%).
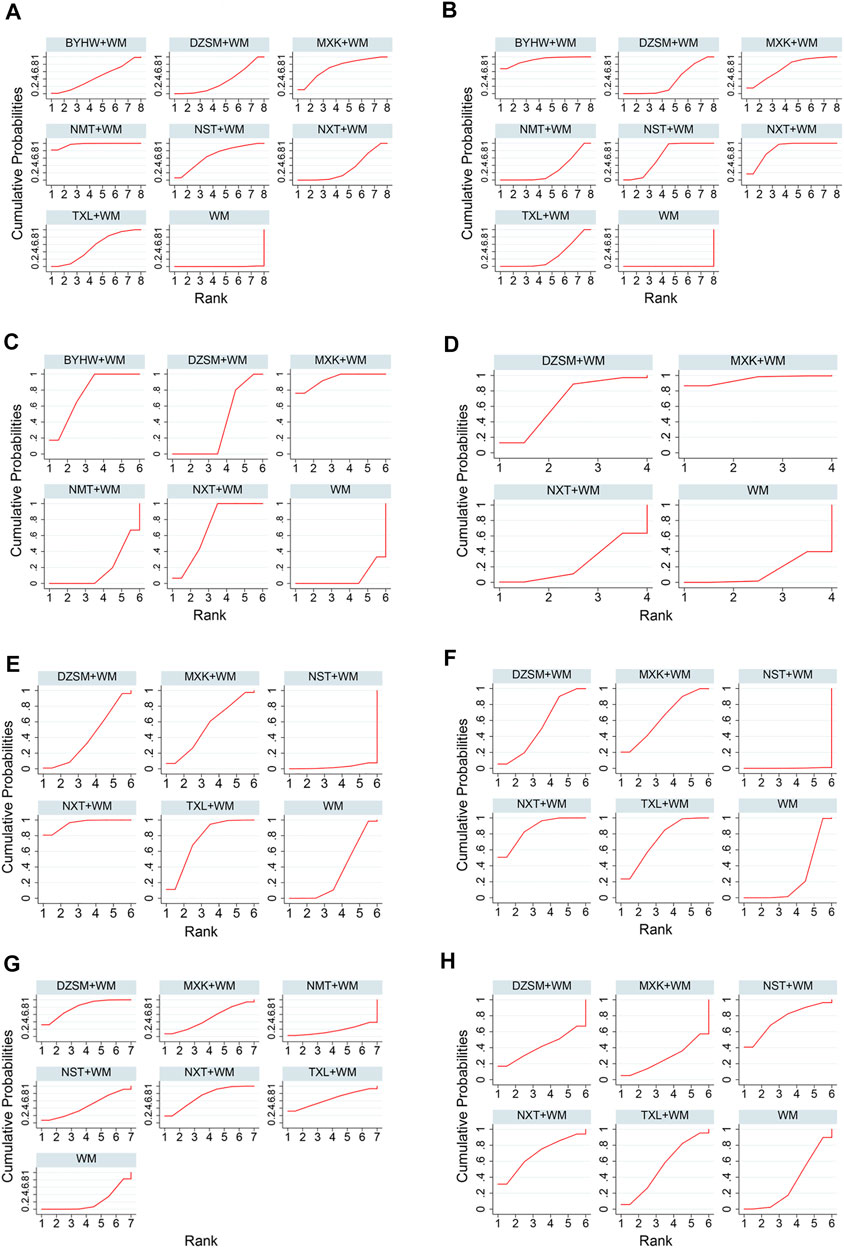
FIGURE 4. SUCRA for various outcomes. The vertical axis represents cumulative probabilities, and the horizontal axis represents ranking of the treatment. (A) Recurrent stroke; (B) NIHSS; (C) Fib; (D) FBG; (E) TG; (F) TC; (G) All-cause mortality; (H) AEs (NXT, Naoxintong capsule; TXL, Tongxinluo capsule; BYHW, Buyang Huanwu Decoction; NMT, Naomaitai capsule; DZSM, Dengzhan Shengmai capsule; NST, Naoshuantong capsule; MXK, Maixuekang capsule; WM, conventional Western medicine; Fib, fibrinogen; FBG, fasting blood glucose; TG, triglycerides; TC, cholesterol; AEs, adverse events).
NIHSS
A total of 15 researches including 7 interventions referred to NIHSS: NXT + WM vs. WM (n = 2), TXL + WM vs. WM (n = 2), BYHW + WM vs. WM (n = 2), NMT + WM vs. WM (n = 2), DZSM + WM vs. WM (n = 2), NST + WM vs. WM (n = 3), MXK + WM vs. WM (n = 2). Compared with WM alone, all TCM + WM had significant effectiveness regarding NIHSS. In addition, the specific results are listed in Table 3: NXT + WM vs. WM (MD = −2.91, 95%CIs (−3.39, −2.43)), TXL + WM vs. WM (MD = −1.40, 95%CIs (−2.19, −0.61)), BYHW + WM vs. WM (MD = −3.51, 95%CIs (−5.11, −1.91)), NMT + WM vs. WM (MD = −1.37, 95%CIs (−2.15, −0.60)), DZSM + WM vs. WM (MD = −1.62, 95%CIs (−2.38, −0.85)), NST + WM vs. WM (MD = −2.47, 95%CIs (−2.63, −2.31)), MXK + WM vs. WM (MD = −2.63, 95%CIs (−4.03, −1.24)). In addition, comparisons of any one of the three drugs (BYHW + WM, NXT + WM, NST + WM) with any one of the other three drugs (DZSM + WM, NMT + WM, TXL + WM) performed statistically significantly different. Moreover, no statistically significant difference was found between other treatments.
According to the ranking of SUCRA probabilities (Table 4; Figure 4), the order of 7 types of TCM + WM was: BYHW + WM (91.4%) > NXT + WM (83.4%) > MXK + WM (70.6%) > NST + WM (64.7%) > DZSM + WM (35.0%) > TXL + WM (27.9%) > NMT + WM (26.9%) > WM (0.0%).
Fib
A total of 14 RCTs involving 5 interventions investigated Fib: NXT + WM vs. WM (n = 5), BYHW + WM vs. WM (n = 2), NMT + WM vs. WM (n = 1), DZSM + WM vs. WM (n = 4), MXK + WM vs. WM (n = 2). Except for NMT + WM, each TCM + WM’s comparison with WM had significant difference. Table 3 specifically expresses the following difference: NXT + WM vs. WM (MD = −1.04, 95%CIs (−1.22, −0.86)), BYHW + WM vs. WM (MD = −1.09, 95%CIs (−1.35, −0.83)), DZSM + WM vs. WM (MD = −0.28, 95%CIs (−0.47, −0.10)), MXK + WM vs. WM (MD = −1.28, 95%CIs (−1.62, −0.93)). Other detailed results can be found in Table 3.
Based on the SUCRA value (Table 4; Figure 4), the ranking of 5 types of TCM + WM was as follows: MXK + WM(93.6%) > BYHW + WM(76.4%) > NXT + WM(70.0%) > DZSM + WM(36%) > NMT + WM(17.3%) > WM(6.7%).
FBG
In total, 5 RCTs with three treatments referred to FBG were found: NXT + WM vs. WM (n = 2) DZSM + WM vs. WM (n = 2) MXK + WM vs. WM (n = 1). Only two comparisons in Table 3 showed significant difference: MXK + WM vs. WM (MD = −0.41, 95%CIs (−0.73, −0.09)), MXK + WM vs. NXT + WM (MD = −0.38, 95%CIs: (−0.74, −0.03)). Other results showed no statistically significant difference.
Based on the ranking of SUCRA probabilities (Table 4; Figure 4), the ranking of the included three types of TCM + WM was as follows: MXK + WM (94.9%) > DZSM + WM (66.3%) > NXT + WM (25.0%) > WM (13.8%).
TG
A total of 16 articles with 5 interventions presented data about TG: NXT + WM vs. WM (n = 5), TXL + WM vs. WM (n = 5) DZSM + WM vs. WM (n = 3), NST + WM vs. WM (n = 1), MXK + WM vs. WM (n = 2). Compared with WM, only NXT + WM (MD = −0.80, 95%CIs (−1.31, −0.29)) and TXL + WM (MD = −0.64, 95%CIs (−1.15, −0.14)) significantly reduce TG. Also, the comparison results are demonstrated in Table 3.
According to the SUCRA values (Table 4; Figure 4), the order of 5 kinds of TCM + WM was: NXT + WM (95.4%) > TXL + WM (74.7%) > MXK + WM (54.1%) > DZSM + WM (40.4%) > WM (32.9%) > NST + WM (2.6%).
TC
The information of TC was available for 17 researches including 5 treatments: NXT + WM vs. WM (n = 6), TXL + WM vs. WM (n = 4) DZSM + WM vs. WM (n = 4), NST + WM vs. WM (n = 1), MXK + WM vs. WM (n = 2). As it is listed in Table 3 that NXT + WM and TXL + WM significantly reduced TC compared with WM alone: NXT + WM vs. WM (MD = −2.34, 95%CIs (−3.63, −1.05)) and TXL + WM vs. WM (MD = −2.16, 95%CIs (−3.49, −0.82)). However, it is interesting to find that compared to WM alone, NST + WM (MD = 1.49, 95%CIs (0.29, 2.68)) significantly improved TC.
According to the ranking of SCURA probabilities (Table 4; Figure 4), the results of ranking of 5 treatments were as follows: NXT + WM (85.9%) > TXL + WM (72.9%) > MXK + WM (63.7%) > DZSM + WM (53%) > WM (24.3%) > NST + WM (0.3%).
All-Cause Mortality
In total, 16 studies involving 6 kinds of medicines investigated all-cause mortality: NXT + WM vs. WM (n = 6), TXL + WM vs. WM (n = 3), NMT + WM vs. WM (n = 1), DZSM + WM vs. WM (n = 4), NST + WM vs. WM (n = 1), MXK + WM vs. WM (n = 1). Only two results in Table 3 demonstrate significant difference: DZSM + WM vs. WM (OR = 0.33, 95%CIs (0.15, 0.70)), NXT + WM vs. WM (OR = 0.38, 95%CIs (0.18, 0.79)).
It can be seen from SUCRA values (Table 4; Figure 4) that the six types of TCM + WM’s rankings in reducing all-cause mortality were: DZSM + WM (79.7%) > NXT + WM (72.5%) > TXL + WM (64.5%) > MXK + WM (49.5%) > NST + WM (46.5%) > WM (20.9%) > NMT + WM (16.4%).
AEs
Most of the adverse events were gastrointestinal reaction, nausea, and giddiness(Peng and Niu, 2014; Bo et al., 2017; Xu, 2017). Our research showed that patients were tolerable for adverse reactions of TCM + WM or WM. In addition, the information of AEs was available for 8 researches involving 5 treatments: NXT + WM vs. WM (n = 1), TXL + WM vs. WM (n = 4) DZSM + WM vs. WM (n = 1), NST + WM vs. WM (n = 1), MXK + WM vs. WM (n = 1). All results performed no significant differences, which are listed in Table 3.
Based on the ranking of SUCRA probabilities (Table 4; Figure 4), the 5 interventions’ rankings in reducing AEs were: NST + WM (75.7%) > NXT + WM (68.8%) > TXL + WM (53.6%) > DZSM + WM (42.0%) > WM (32.5%) > MXK + WM (27.5%).
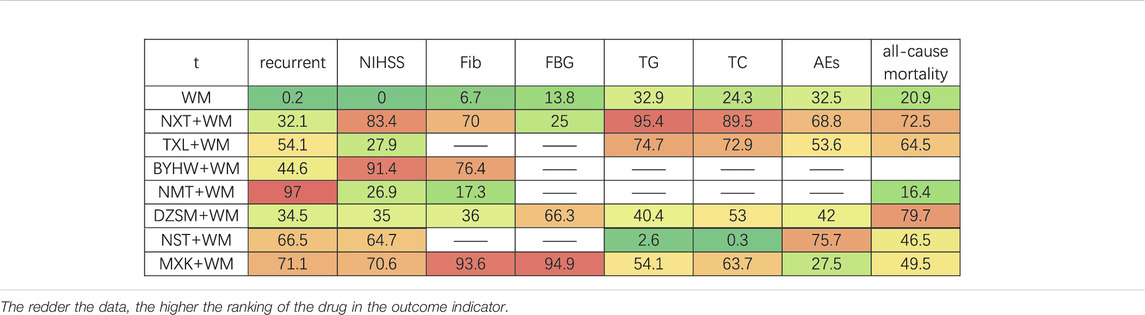
Cluster Analysis
Two-dimensional clustering was utilized to find the best TCM through different indicators of various drugs. Herein blue indicates the best choice considering both outcomes, red indicates the second choice considering both outcomes, green indicates the third choice considering both outcomes, and orange indicates the last choice considering both outcomes. When it comes to recurrent stroke and NIHSS, the cluster analysis depicted that BYHW + WM, NXT + WM, MXK + WM, NST + WM were dominant in comparison (Figure 5A). Furthermore, as cluster analysis related to recurrent stroke and al-cause mortality was made, we found that MXK + WM, NST + WM had relatively good curative effects (Figure 5B). In conclusion, the results of cluster analysis demonstrated that MXK + WM, NST + WM had relatively good secondary prevention effects with regard to recurrent stroke, NIHSS, and all-cause mortality.
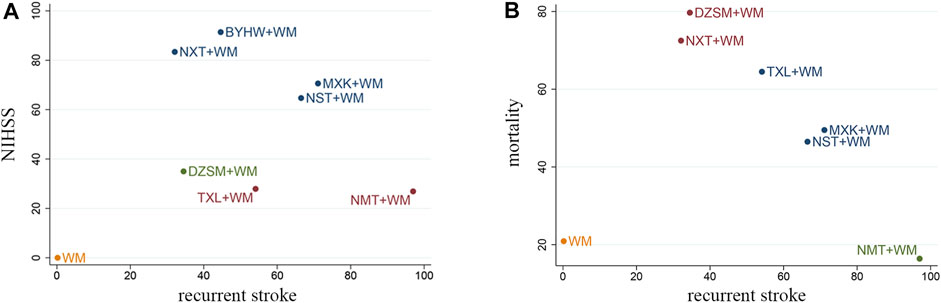
FIGURE 5. Cluster analysis plots for three outcomes. (A) Recurrent stroke (X axis), NIHSS (Y axis); (B) recurrent stroke (X axis), all-cause mortality (Y axis). Herein blue indicates the best choice considering both outcomes, red indicates the second choice considering both outcomes, green indicates the third choice considering both outcomes, orange indicates the last choice considering both outcomes (NXT, Naoxintong capsule; TXL, Tongxinluo capsule; BYHW, Buyang Huanwu Decoction; NMT, Naomaitai capsule; DZSM, Dengzhan Shengmai capsule; NST, Naoshuantong capsule; MXK, Maixuekang capsule; WM, conventional Western medicine).
Publication Bias
To test the publication bias, the comparison−adjusted funnel plots for recurrent stroke were plotted. As it is listed in Figure 6, we found the scatters were basically symmetrical along the center line and the angle between the center line and the adjusted auxiliary line was not large. The results indicated that there is little publication bias and the small sample effects were rare.
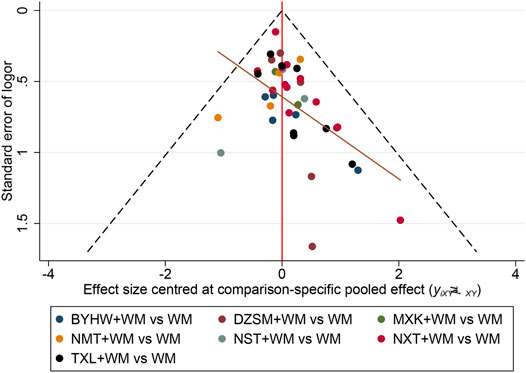
FIGURE 6. Funnel plot for recurrent stroke. The vertical axis represents “standard error of effect size” and horizontal axis represents “effect size centered at comparison-specific pooled effect.” (NXT, Naoxintong capsule; TXL, Tongxinluo capsule; BYHW, Buyang Huanwu Decoction; NMT, Naomaitai capsule; DZSM, Dengzhan Shengmai capsule; NST, Naoshuantong capsule; MXK, Maixuekang capsule; WM, conventional Western medicine).
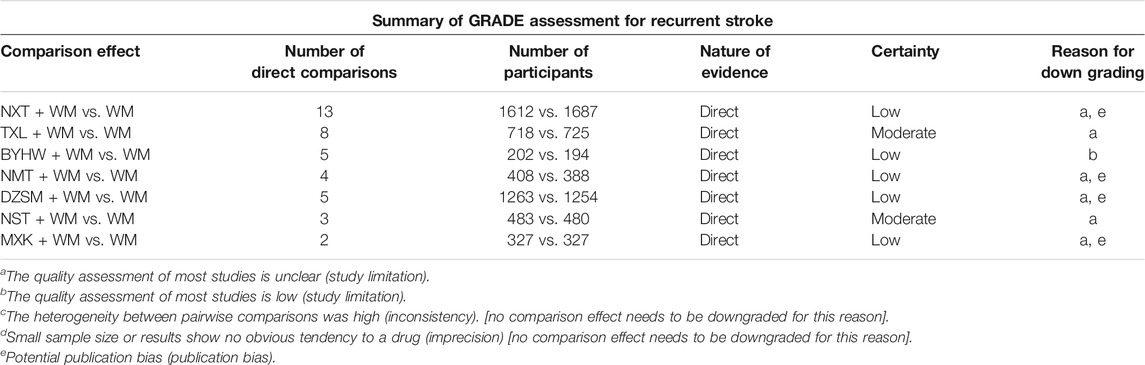
GRADE Assessment
Here, strength of evidence was evaluated through GRADE assessment which was about the comparisons between TCM + WM with WM on recurrent stroke. Except BYHW + WM had high risk of bias leading to low certainty evidence, other types of TCM + WM’s study limitation were uncertain. Furthermore, there was no inconsistency in this systematical analysis which meant no study needs to be downgraded. In addition, all researches had enough sample size and demonstrated obvious tendency to TCM giving rise to no imprecision. Thus, all study didn’t required to be downgraded. Moreover, some of the TCM + WM were downgraded for having publication bias. (Table 5).
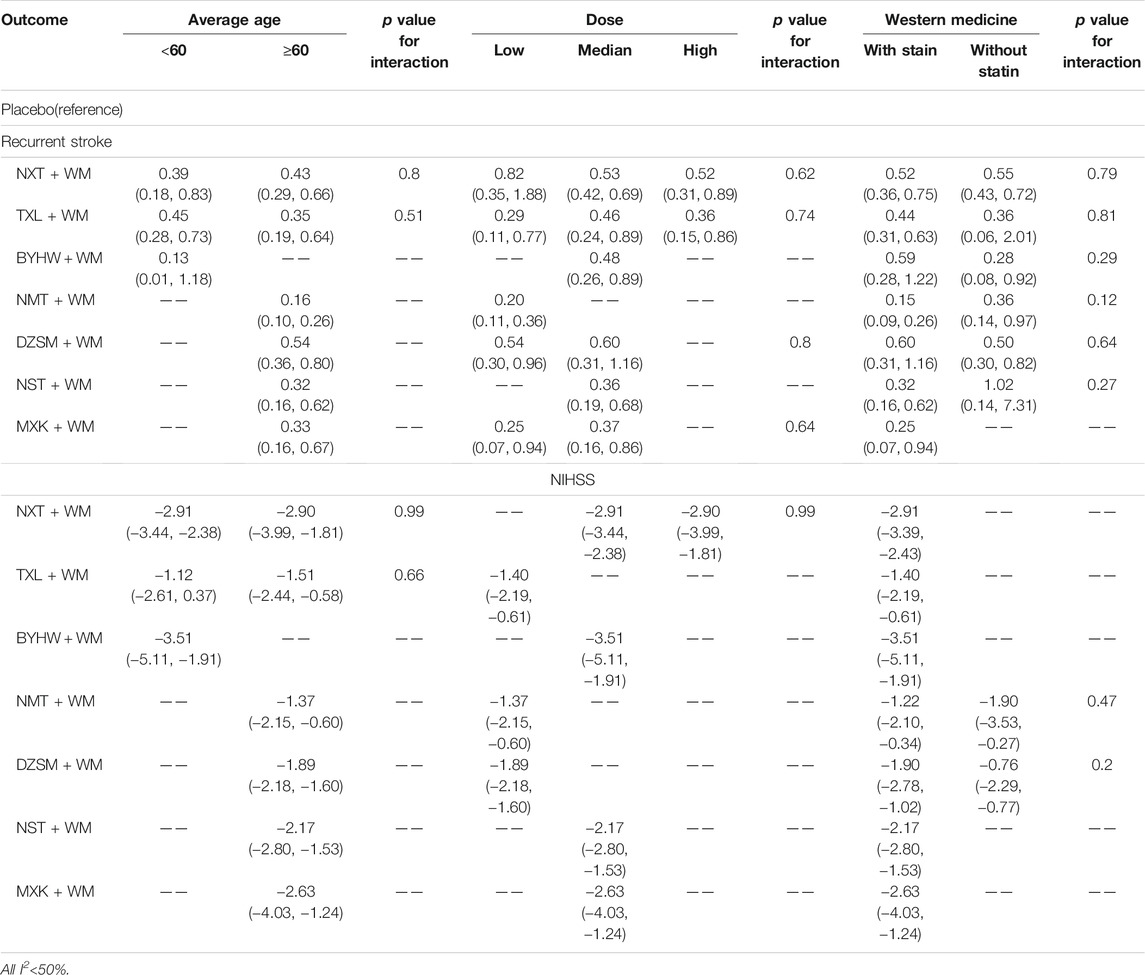
Subgroup Analysis
For recurrent stroke and NIHSS, all calculation of potential effect modifier (potential source of heterogeneity) including age of patients (average age <60 vs. average age ≥60), treatment dose (low does vs. medium dose vs. high dose), and the specific methods of WM (with statins vs. without statins) demonstrated no significant difference (Table 6). Thus, we believe that the age of patients and treatment dose had little effect on the transitivity of our systematical analysis.
Sensitivity Analysis
In the standard pairwise meta-analysis, statistical heterogeneity was tested by the calculation of I2 if the number of the study was at least 5 and we find all I2<50%. Additionally, a leave−one−out meta-analysis was used to evaluate the independent effect of every study on summary results. The results suggested that no study needed to be excluded, thus we thought each study produced little bias in the results.
Discussion
Unilateral weakness, unilateral sensory loss, speech disturbance, clumsiness or ataxia, and vertigo are all common stroke symptoms (Hankey and Blacker, 2015). Non-contrast CT is used to precisely diagnose the condition because of its sensitivity and rapidity. RI is also employed to refine the understanding of infarct location (Powers et al., 2019). In addition, most ischemic strokes originated from thromboembolism, the common source of embolism is atherosclerosis and heart disease, especially atrial fibrillation. Other causes of ischemic stroke involve small vessel disease, which has a close association with hypertension and diabetes, especially in Asia (Campbell et al., 2019).
The systematical analysis approach was taken to compare the secondary prevention effects and safety of TCM + WM in the treatment of stroke. In this study, a total of 47 RCTs including 10,732 patients were included in this work, and we evaluated 7 treatments in terms of 8 indicators involving recurrent stroke, NIHSS, Fib, FBG, TG, TC, all-cause mortality, and AEs. The results indicated that all kinds of TCM + WM were more effective on long-term secondary prevention of ischemic stroke than WM alone. Additionally, through cluster analysis, we concluded that MXK + WM and NST + WM had relatively good preventive effects.
In this systematical analysis, seven kinds of TCM were extracted from Astragali Radix, Radix, Chuanxiong Rhizoma, Persicae Semen, Carthami Flos, Pheretima, or other herbs through modern technological means (Bu et al., 2020). Guo et al. reported TCM has the effects of anti-oxidation, anti-inflammatory, anti-apoptosis, and protection of blood−brain barrier (Guo et al., 2017). Furthermore, Yan et al. found that the TCM can prevent stroke through a variety of signaling pathways (Yan et al., 2019), such as JAK2/STAT3 which regulates proinflammatory cytokine expression (Chen et al., 2017; Hu et al., 2017), NF−κB which is related to the inflammatory mechanism of brain tissue reperfusion injury (Fann et al., 2018; Fu et al., 2020), PI3K/Akt which participates in the pathological process of cerebral ischemia and plays a role in promoting survival and anti-apoptotic pathway (Samakova et al., 2019; Chen et al., 2020).
Nevertheless, there were few systematic reviews and meta-analyses to show the long-term secondary preventive effects of TCM on ischemic stroke. The comparisons between them were rather ambiguous leading to confusion in choosing the appropriate drugs. Thus, this study used pairwise meta-analysis as well as network meta-analysis thus better demonstrating the effects of different kinds of TCM. In addition, different types of TCM were quantitatively ranked to determine the best choice for treatment in clinical settings.
In terms of primary outcomes including recurrent stroke and NIHSS, the results suggested that all types of TCM + WM were better than WM, and results had a statistically significant difference. Some articles reported its origin from multi-channel and multi-target therapy of TCM (Li and Li, 2016; Wei, 2016). Wang et al. said NXT can decrease recurrent stroke and NIHSS, which also corroborates well with our study (Wang et al., 2019). Also, Ma et al. pointed out DZSM is beneficial for recurrent stroke and NIHSS (Ma et al., 2014). However, Xie found there was no significant difference in the recurrent stroke between the BYHW + WM and WM (Xie, 2015), and we guessed it was caused by a small sample size at that time. Moreover, according to the ranking of SUCRA probabilities, NMT + WM, MXK + WM were most likely to become the best treatments for recurrent stroke, and BYHW + WM and NXT + WM were most probably to be the best choices for NIHSS.
The secondary outcomes were stroke risk factors including Fib, FBG, TG, and TC (Diener and Hankey, 2020). The SCURA ranking of WM alone was very low, implying that the combination of TCM and WM was superior to WM. NST was lower in SUCRA values compared with WM when it comes to TC and TG. We believe that the reason behind NST reducing stroke recurrence was due to other stroke risk factors. Moreover, Chen and Yu showed that MXK can decrease Fib which agrees with our results (Chen and Yu, 2020). Our conclusion was also consistent with Wang et al. who proved that NXT is beneficial for reducing TC and TG (Wang et al., 2019). Furthermore, our results were favored by the outcome of the experiments utilizing TCM to reduce blood lipid and blood glucose in mice (Chen et al., 2018; Li et al., 2018). Based on SUCRA value, MXK + WM and BYHW + WM were most likely to be the best choice for reducing Fib. In terms of FBG, MXK had the highest probability to be the best treatment. In TC, the most effective choices were NXT + WM and TXL + WM. Moreover, NXT + WM and TXL + WM were most likely to be the best in TG. However, the samples of some secondary outcome indicators of TCM were less, thus more RCTs are warranted to test our results.
For all-cause mortality, only DZSM and NXT were found to significantly decrease all-cause mortality, all other comparisons have no statistically significant difference. As regards AEs, there was no significant difference in all contrasts. Thus, this implied that all kinds of TCM + WM were more or less tolerable for patients, however, it may be limited to lack of data. Moreover, the AEs predominantly include gastrointestinal reactions, nausea, and giddiness (Peng and Niu, 2014; Bo et al., 2017; Xu, 2017).
In conclusion, TCM + WM were more effective than WM in the long−term secondary prevention for patients with ischemic stroke, and there was no significant difference in the comparisons of AEs. Regarding recurrent stroke, NIHSS, and all-cause mortality, MXK + WM and NST + WM had relatively good preventive effects on long-term secondary prevention through cluster analysis. The basis for confirming the secondary preventive effect of MXK and NST on cerebral infarction is as follows.
The main component of MXK is Hirudo nipponica Whitman (Haemadipsidae, Hirudo) which is the strongest natural thrombin-specific inhibitor discovered yet (Junren et al., 2021). Hirudin inhibits thrombin activity by directly binding with thrombin and plays an anticoagulant role. Second, hirudin has a strong antiplatelet effect, which can inhibit thrombin-induced platelet thrombin binding, platelet activation as well as aggregation (Garcia et al., 2012; Han et al., 2020). Additionally, in comparison with heparin, hirudin has less bleeding and side effects, and it has no allergic reaction and no toxicity (Johnson, 1994; Markwardt, 1994). Furthermore, clinical trials (e.g., Peng, Zhen, Ge, and Wu) showed that MXK has a significant effect on the secondary prevention of ischemic stroke (Peng and Niu, 2014; Zhen, 2015; Ge et al., 2016; Wu and Xiang, 2018).
Typha orientalis C. Presl (Typhaceae, Typhae Pollen), Paeonia lactiflora Pall (Paeoniaceae, Paeoniae Radix Rubra), Curcuma phaeocaulis Valeton (Zingiberaceae, Curcumae Radix), Gastrodia elata Blume (Orchidaceae, Gastrodiae Rhizoma), Rha ponticum uniflorum (L.) DC (Compositae, Rhapontici Radix) make up NST, a Chinese medication (Luo et al., 2020). It is also extensively used for increasing blood circulation, eliminating blood stasis, and promoting nerve function recovery (Liu et al., 2014). Moreover, a meta-analysis showed that NST has the effect of increasing blood adiponectin, decreasing neurological deficits, and reducing the area of atherosclerotic plaque (Zhang et al., 2019). Since it has been widely used to treat ischemic stroke, Liu and Huang demonstrated that NST + WM is better than WM in recurrent stroke, and the results are significantly different (Liu and Li, 2012; Huang et al., 2014).
Innovations and Limitations of the Study
This is for the first time that the secondary prevention effects of various kinds of TCM on ischemic stroke as well as their safety were systematically evaluated. Moreover, this is the pioneer study, ranking seven kinds of TCM based on SUCRA value from different indicators, which furnishes the high-quality basis for clinical practice. Finally, strict inclusion and exclusion criteria were established, and the articles were thereby searched comprehensively.
Nevertheless, the risk of bias in most included articles was unclear and no direct comparison between TCM was found, giving rise to a lack of evidence, but we included 47 articles involving a large sample size and the subgroup analysis showed that the transitivity was good. All included RCTs were conducted in China, therefore more RCTs are needed to see whether the findings of this study applied to patients from other regions. Furthermore, clinical heterogeneity might appear because of the diversity and different courses of treatment of Western medicine. Despite these shortcomings, this is the first comparison of the long-term secondary prevention effects of various TCM on ischemic stroke from multiple indexes and provide some valuable suggestions for clinical practice.
Conclusion
In summary, our systematical analysis revealed that TCM had positive secondary prevention effects on patients with cerebral infarction, and there was no significant difference in the comparisons of AEs. Additionally, MXK + WM and NST + WM had relatively good preventive effects for recurrent stroke, NIHSS, and all-cause mortality. Nevertheless, on account of some limitations, more high-quality, and double-blinded multicenter RCTs with a larger sample size are needed to test and verify our results in the future.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material. Further inquiries can be directed to the corresponding authors.
Author Contributions
JL and LY conceived and designed the study. XZ, YZ and HW extracted and analyzed the data. JL, YH and WJ performed this systematical analysis. JL and XL wrote this manuscript. LY, WJ and XZ played an important role in the revision of the manuscript. All authors contributed to the article and approved the final version of manuscript.
Funding
This work was supported by the National Key R&D Program of China (Nos. 2019YFC1708600, 2019YFC1708604) the National Natural Science Foundation of China (Nos.81630105, 81904083, 81973560), and the Key Laboratory of TCM Encephalopathy of Zhejiang Province (grant no. 2020E10012).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors, and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fphar.2021.722975/full#supplementary-material
References
Amarenco, P., Lavallée, P. C., Labreuche, J., Albers, G. W., Bornstein, N. M., Canhão, P., et al. (2016). One−Year Risk of Stroke after Transient Ischemic Attack or Minor Stroke. N. Engl. J. Med. 374 (16), 1533–1542. doi:10.1056/NEJMoa1412981
Bhatt, D. L., Flather, M. D., Hacke, W., Berger, P. B., Black, H. R., Boden, W. E., et al. (2007). Patients with Prior Myocardial Infarction, Stroke, or Symptomatic Peripheral Arterial Disease in the CHARISMA Trial. J. Am. Coll. Cardiol. 49 (19), 1982–1988. doi:10.1016/j.jacc.2007.03.025
Bhatt, D. L., Fox, K. A., Hacke, W., Berger, P. B., Black, H. R., Boden, W. E., et al. (2006). Clopidogrel and Aspirin versus Aspirin Alone for the Prevention of Atherothrombotic Events. N. Engl. J. Med. 354 (16), 1706–1717. doi:10.1056/NEJMoa060989
Bo, G., Wan, Y., Wang, G. H., and Xiong, H. (2017). The Clinical Research of Tongxinluo Capsule in Treating Ischemic Stroke Patients. J. Chengdu Med. Coll. 12 (03), 277–279. doi:10.3969/j.issn.1674−2257.2017.03.008
Bu, L., Dai, O., Zhou, F., Liu, F., Chen, J. F., Peng, C., et al. (2020). Traditional Chinese Medicine Formulas, Extracts, and Compounds Promote Angiogenesis. Biomed. Pharmacother. 132, 110855. doi:10.1016/j.biopha.2020.110855
Campbell, B. C. V., De Silva, D. A., Macleod, M. R., Coutts, S. B., Schwamm, L. H., Davis, S. M., et al. (2019). Ischaemic Stroke. Nat. Rev. Dis. Primers 5 (1), 70. doi:10.1038/s41572−019−0118−8
Chai, X. B. (2015). Observation on the Curative Effect of Tongxinluo Capsule Combined with Statins and Aspirin in the Treatment of Cerebral Infarction. Inner Mongolia J. Traditional Chin. Med. (7), 70–71. doi:10.3969/j.issn.1006−0979.2015.07.071
Chao, J. F. (2011). A Multicenter, Randomized, Double−Blind Clinical Study on Secondary Prevention of Ischemic Stroke with Yiqi Huoxue Yangyin Herbs. Doctor. J. Chengdu Univ. Traditional Chin. Med.
Chen, B., Fang, X. H., Wu, Y. H., Jing, S. L., Sun, H. J., and Li, S. T. (2008). Acute Ischemic Stroke: Paradigm for Treatment. Chin. J. Neurol. 41 (3), 195–230. doi:10.3321/j.issn:1006−7876.2008.03.015
Chen, W. F., and Yu, T. (2020). Meta Analysis of the Clinical Effect of Maixuekang Capsule in the Treatment of Acute Cerebral Infarction. Hunan J. Traditional Chin. Med. 36 (08), 134–139. doi:10.16808/j.cnki.issn1003−7705.2020.08.055
Chen, X., Chen, H., He, Y., Fu, S., Liu, H., Wang, Q., et al. (2020). Proteomics−Guided Study on Buyang Huanwu Decoction for its Neuroprotective and Neurogenic Mechanisms for Transient Ischemic Stroke: Involvements of EGFR/PI3K/Akt/Bad/14−3−3 and Jak2/Stat3/Cyclin D1 Signaling Cascades. Mol. Neurobiol. 57 (10), 4305–4321. doi:10.1007/s12035−020−02016−y
Chen, X., Li, G. M., Zhou, L. H., Sun, J. B., Huang, Y., and Luo, E. L. (2018). Effect of Dengzhanshengmai (DZSM) on Cognition Function, Blood Glucose and Blood Lipid Level for Mouse Model of Transient Ischemic Attack. Anatomical Res. 40 (03), 161–164+181. doi:10.3969/j.issn.1671−0770.2018.03.001
Chen, Y., and Cao, J. (2016). Clinical Observation on 35 Cases of Cerebral Infarction in Convalescence Treated with Integrated Traditional Chinese and Western Medicine. Pract. Clin. J. Integrated Traditional Chin. West. Med. 16 (5), 16–18. doi:10.13638/j.issn.1671−4040.2016.05.007
Chen, Y. (2012). Effect of Naoxintong Capsule Combined with Atorvastatin on Secondary Prevention of Acute Cerebral Infarction. Chin. Manipulation Rehabil. Med. 3 (8), 26.
Chen, Y., Huang, X. S., Wu, H. J., Luo, Y. L., Wang, Y., and Tan, L. H. (2017). Effect of Puerarin on JAK2/STAT3 Signaling Pathway after Cerebral Ischemia−Reperfusion Injury in Rats. Hunan J. Traditional Chin. Med. 33 (04), 144–147+165. doi:10.16808/j.cnki.issn1003−7705.2017.04.070
Collaborators, G. D. a. H. (2017a). Global, Regional, and National Age−Sex Specific Mortality for 264 Causes of Death, 1980−2016: a Systematic Analysis for the Global Burden of Disease Study 2016. Lancet 390 (10100), 1151–1210. doi:10.1016/S0140−6736(17)32152−9
Collaborators, G. D. a. H. (2017b). Global, Regional, and National Disability−Adjusted Life−Years (DALYs) for 333 Diseases and Injuries and Healthy Life Expectancy (HALE) for 195 Countries and Territories, 1990−2016: a Systematic Analysis for the Global Burden of Disease Study 2016. Lancet 390 (10100), 1260–1344. doi:10.1016/S0140−6736(17)32130−X
Dang, C. J., Yu, X. F., Cai, D. F., Zhu, X. Y., Zhang, H. Z., Wang, M. Z., et al. (2018). Secondary Prevention Effect of Naoxintong Capsule on Ischemic Stroke of Blood Stasis Type. J. Traditional Chin. Med. 59 (13), 1121–1125. doi:10.13288/j.11−2166/r.2018.13.011
Diener, H. C., Bogousslavsky, J., Brass, L. M., Cimminiello, C., Csiba, L., Kaste, M., et al. (2004). Aspirin and Clopidogrel Compared with Clopidogrel Alone after Recent Ischaemic Stroke or Transient Ischaemic Attack in High−Risk Patients (MATCH): Randomised, Double−Blind, Placebo−Controlled Trial. Lancet 364 (9431), 331–337. doi:10.1016/S0140−6736(04)16721−4
Diener, H. C., and Hankey, G. J. (2020). Primary and Secondary Prevention of Ischemic Stroke and Cerebral Hemorrhage: JACC Focus Seminar. J. Am. Coll. Cardiol. 75 (15), 1804–1818. doi:10.1016/j.jacc.2019.12.072
Fann, D. Y., Lim, Y. A., Cheng, Y. L., Lok, K. Z., Chunduri, P., Baik, S. H., et al. (2018). Evidence that NF−Κb and MAPK Signaling Promotes NLRP Inflammasome Activation in Neurons Following Ischemic Stroke. Mol. Neurobiol. 55 (2), 1082–1096. doi:10.1007/s12035−017−0394−9
Feigin, V. L., Feigin, V. L., Nguyen, G., Cercy, K., Johnson, C. O., Alam, T., et al. (2018). Global, Regional, and Country−specific Lifetime Risks of Stroke, 1990 and 2016. N. Engl. J. Med. 379 (25), 2429–2437. doi:10.1056/NEJMoa1804492
Fu, C., Zhang, X., Zeng, Z., Tian, Y., Jin, X., Wang, F., et al. (2020). Neuroprotective Effects of Qingnao Dripping Pills against Cerebral Ischemia via Inhibiting NLRP3 Inflammasome Signaling Pathway: In Vivo and In Vitro. Front. Pharmacol. 11, 65. doi:10.3389/fphar.2020.00065
Gan, Z. R. (2007). Effect of Naomaitai Capsule on Serum C−Reactive Protein and Prognosis in Patients with Cerebral Infarction. Chin. Gen. Pract. 10 (24), 2040–2042. doi:10.3969/j.issn.1007−9572.2007.24.007
Gao, C. Y. (2015). Thinking of Integrated Traditional Chinese and Western Medicine on Secondary Prevention of Ischemic Stroke. Proc. 11th China Neurol. Conf. integrated traditional Chin. West. Med., 94.
Garcia, D. A., Baglin, T. P., Weitz, J. I., and Samama, M. M. (2012). Parenteral Anticoagulants: Antithrombotic Therapy and Prevention of Thrombosis, 9th Ed: American College of Chest Physicians Evidence−Based Clinical Practice Guidelines. Chest 141 (2 Suppl. l), e24S–e43S. doi:10.1378/chest.11−2291
Ge, Y. C., Zhao, H. Q., Shi, J., and Wu, Z. H. (2016). Value of Maixuekang Capsule in Secondary Prevention of Ischemic Stroke. China J. Mod. Med. 26 (21), 83–86. doi:10.3969/j.issn.1005−8982.2016.21.017
Guo, J. Q., Wang, X. J., Yao, B. L., Zhang, H., He, L. N., Lu, X., et al. (2013). Effect of Tongxinluo Capsule on Sequela of Cerebral Infarction. Chin. J. Coal Industry Med. 16 (2), 1972–1974.
Guo, L., Huang, G. L., Zhou, K., Zhou, D. W., and Lu, Y. (2017). Research Progress on the Mechanism of Traditional Chinese Medicine and its Effective Components in the Prevention and Treatment of Cerebral Apoplexy Ischemia−Reperfusion Injury. Heilongjiang J. Traditional Chin. Med. 46 (02), 69–71.
Guo, P. P., Chen, X. X., Wang, X. R., and Liu, Z. G. (2019). Progress in the Mechanism and Clinical Treatment of Antiplatelet Resistance of Aspirin and Clopidogrel. Chin. J. Clin. Neurosciences 27 (03), 321–328.
Hackam, D. G., and Spence, J. D. (2007). Combining Multiple Approaches for the Secondary Prevention of Vascular Events after Stroke: a Quantitative Modeling Study. Stroke 38 (6), 1881–1885. doi:10.1161/STROKEAHA.106.475525
Han, H. H., Zhang, H. T., Wang, R., Yan, Y., Liu, X., Wang, Y., et al. (2020). Improving Long Circulation and Procoagulant Platelet Targeting by Engineering of Hirudin Prodrug. Int. J. Pharm. 589, 119869. doi:10.1016/j.ijpharm.2020.119869
Heinrich, M., Appendino, G., Efferth, T., Fürst, R., Izzo, A. A., Kayser, O., et al. (2020). Best Practice in Research − Overcoming Common Challenges in Phytopharmacological Research. J. Ethnopharmacol 246, 112230. doi:10.1016/j.jep.2019.112230
Higgins, J. P., Altman, D. G., Gøtzsche, P. C., Jüni, P., Moher, D., Oxman, A. D., et al. (2011). The Cochrane Collaboration's Tool for Assessing Risk of Bias in Randomised Trials. BMJ 343, d5928. doi:10.1136/bmj.d5928
Higgins, J. P., Thompson, S. G., Deeks, J. J., and Altman, D. G. (2003). Measuring Inconsistency in Meta−Analyses. BMJ 327 (7414), 557–560. doi:10.1136/bmj.327.7414.557
Hu, G. Q., Du, X., Li, Y. J., Gao, X. Q., Chen, B. Q., and Yu, L. (2017). Inhibition of Cerebral Ischemia/reperfusion Injury−Induced Apoptosis: Nicotiflorin and JAK2/STAT3 Pathway. Neural Regen. Res. 12 (1), 96–102. doi:10.4103/1673−5374.198992
Huang, H. M., Ding, Y. B., Deng, W. H., and Pan, X. P. (2014). Application Research on Aspirin Resistance in Patients with Cerebral Infarction Treated by Naoshuantong. Guide China Med. (5), 19–20.
Huang, X. H., and Huang, X. B. (2007). Clinical Study on Naomaitai Capsule in Preventing Recurrence of strokeThe Third pan TCM Forum, TCM "preventive Treatment" and the First Fuyang Forum, 306–308.
Hutton, B., Salanti, G., Caldwell, D. M., Chaimani, A., Schmid, C. H., Cameron, C., et al. (2015). The PRISMA Extension Statement for Reporting of Systematic Reviews Incorporating Network Meta−Analyses of Health Care Interventions: Checklist and Explanations. Ann. Intern. Med. 162 (11), 777–784. doi:10.7326/M14−2385
Jiang, Y. X. (2012). Effect of Buchang Naoxintong Capsule on Secondary Prevention of Ischemic Cerebrovascular Disease. Chin. J. Pract. Med. 39 (12), 111–112. doi:10.3760/cma.j.issn.1674−4756.2012.12.056
Jiao, J., Niu, Y., and Wei, X. (2011). Clinical Effect of Buyang Huanwu Decoction on Secondary Prevention of Qi Deficiency Cerebral Infarction in Convalescence. J. Zhejiang Univ. Tradit. Chin. Med. 35 (6), 836–838. doi:10.3969/j.issn.1005−5509.2011.06.009
Johnson, P. H. (1994). Hirudin: Clinical Potential of a Thrombin Inhibitor. Annu. Rev. Med. 45, 165–177. doi:10.1146/annurev.med.45.1.165
Junren, C., Xiaofang, X., Huiqiong, Z., Gangmin, L., Yanpeng, Y., Xiaoyu, C., et al. (2021). Pharmacological Activities and Mechanisms of Hirudin and its Derivatives − A Review. Front. Pharmacol. 12, 660757. doi:10.3389/fphar.2021.660757
Kang, z., and Li, y. (2012). Application of Integrated Traditional Chinese and Western Medicine in Secondary Prevention of Cerebral Infarction. Acta Chin. Med. 27 (02), 220–222.
Kernan, W. N., Ovbiagele, B., Black, H. R., Bravata, D. M., Chimowitz, M. I., Ezekowitz, M. D., et al. (2014). Guidelines for the Prevention of Stroke in Patients with Stroke and Transient Ischemic Attack: a Guideline for Healthcare Professionals from the American Heart Association/American Stroke Association. Stroke 45 (7), 2160–2236. doi:10.1161/STR.0000000000000024
Lawes, C. M., Parag, V., Bennett, D. A., Suh, I., Lam, T. H., Whitlock, G., et al. (2004). Blood Glucose and Risk of Cardiovascular Disease in the Asia Pacific Region. Diabetes Care 27 (12), 2836–2842. doi:10.2337/diacare.27.12.2836
Li, S. S., and Li, G. Y. (2016). Research Progress on Prevention and Treatment of Ischemic Stroke with Traditional Chinese Medicine. Anat. Res. 38 (03), 200–202.
Li, T. M., Wu, Y., Xu, L. Y., and Zhong, P. (2018). Effect of Buyang Huanwu Decoction on Blood Lipid and Inflammatory Reaction of Atherosclerotic Plaque in ApoE Gene Deficient Mice. J. New Chin. Med. 50 (02), 5–8.
Lin, R. F., and Li, P. k. (2012). Observation on Cerebral Infarction of Qi Deficiency and Blood Deficiency Treated with Modified Buyang Huanwu Decoction. China Health Industry (4), 49–50.
Liu, F. (2019). Treatment of 24 Cases of Ischemic Stroke with Buyang Huanwu Decoction Combined with Aspirin. China Pract. Med. 14 (3), 119–120. doi:10.14163/j.cnki.11−5547/r.2019.03.072
Liu, H., Peng, Y. Y., Liang, F. Y., Chen, S., Li, P. B., Peng, W., et al. (2014). Protective Effects of Traditional Chinese Medicine Formula NaoShuanTong Capsule on Haemorheology and Cerebral Energy Metabolism Disorders in Rats with Blood Stasis. Biotechnol. Biotechnol. Equip 28 (1), 140–146. doi:10.1080/13102818.2014.901678
Liu, J. X., and Li, X. M. (2012). Therapeutic and Preventive Effects of Naoshuantong Capsule on Cerebral Infarction. Guide China Med. 10 (18), 5–6. doi:10.3969/j.issn.1671−8194.2012.18.003
Liu, S. R., and Cao, J. (2008). Effect of Tongxinluo Capsule on Secondary Prevention of Ischemic Stroke. The Fourth Int. Conf. collaterals, 252–255.
Liu, W. J., and Wang, S. X. (2006). Observation on the Effect of Naomaitai Capsule on 80 Cases of Cerebral Infarction. Henan Traditional Chin. Med. 26 (12), 71–72. doi:10.3969/j.issn.1003−5028.2006.12.053
Liu, W. W. (2009). Preliminary Study of Dengzhan Shengmai Capsule on Secondary Prevention of Ischemic Stroke (6 Months). [dissertation/master‘s thesis]. Wuhan, China: Hubei University of traditional Chinese Medicine.
Lu, Y. L., Qiao, X. D., and Ye, F. (2018). Effect of Tongxinluo Capsule Combined with Aspirin and Atorvastatin on Secondary Prevention of Ischemic Stroke. Guizhou Med. J. 42 (3), 318–320. doi:10.3969/j.issn.1000−744X.2018.03.024
Luo, L., Wu, S., Chen, R., Rao, H., Peng, W., and Su, W. (2020). The Study of Neuroprotective Effects and Underlying Mechanism of Naoshuantong Capsule on Ischemia Stroke Mice. Chin. Med. 15 (1), 119. doi:10.1186/s13020−020−00399−7
Ma, L. S., Chu, Z. H., and Zhao, S. C. (2014). Effect of Dengzhan Shengmai Capsule on Secondary Prevention of Atherosclerotic Cerebral Infarction. Chin. J. Clin. Pharmacol. Ther. 19 (04), 442–445.
Markwardt, F. (1994). The Development of Hirudin as an Antithrombotic Drug. Thromb. Res. 74 (1), 1–23. doi:10.1016/0049−3848(94)90032−9
Meng, X. Q. (2009). Effect of Buchang Naoxintong on Preventing Recurrence of Cerebral Infarction. Liaoning J. Traditional Chin. Med. 36 (11), 1942.
Mohan, K. M., Wolfe, C. D., Rudd, A. G., Heuschmann, P. U., Kolominsky−Rabas, P. L., and Grieve, A. P. (2011). Risk and Cumulative Risk of Stroke Recurrence: a Systematic Review and Meta−Analysis. Stroke 42 (5), 1489–1494. doi:10.1161/STROKEAHA.110.602615
Nan, M. Z., and Li, D. D. (2016). Application Effect of Dengzhan Shengmai Capsule in Secondary Prevention of Ischemic Stroke. China Foreign Med. Treat. 35 (9), 146–148. doi:10.16662/j.cnki.1674−0742.2016.09.146
Peng, R. Q., and Niu, J. P. (2014). Clinical Study of Maixuekang Capsule on Secondary Prevention of Ischemic Stroke. 17th Natl. Conf. Neurol. Chin. Med. Assoc. 1.
Peng, W., Zhou, J., and Yang, Y. (2012). Effect of Naoshuantong Capsule on Cerebral Blood Flow reserve in Patients with Cerebral Infarction. Clin. J. Chin. Med. 4 (24), 93–94.
Powers, W. J., Rabinstein, A. A., Ackerson, T., Adeoye, O. M., Bambakidis, N. C., Becker, K., et al. (2019). Guidelines for the Early Management of Patients with Acute Ischemic Stroke: 2019 Update to the 2018 Guidelines for the Early Management of Acute Ischemic Stroke: A Guideline for Healthcare Professionals from the American Heart Association/American Stroke Association. Stroke 50 (12), e344–e418. doi:10.1161/STR.0000000000000211
Refaai, M. A., Riley, P., Mardovina, T., and Bell, P. D. (2018). The Clinical Significance of Fibrin Monomers. Thromb. Haemost. 118 (11), 1856–1866. doi:10.1055/s−0038−1673684
Rivera, D., Allkin, R., Obón, C., Alcaraz, F., Verpoorte, R., and Heinrich, M. (2014). What Is in a Name? the Need for Accurate Scientific Nomenclature for Plants. J. Ethnopharmacol 152 (3), 393–402. doi:10.1016/j.jep.2013.12.022
Rothwell, P. M., Giles, M. F., Chandratheva, A., Marquardt, L., Geraghty, O., Redgrave, J. N., et al. (2007). Effect of Urgent Treatment of Transient Ischaemic Attack and Minor Stroke on Early Recurrent Stroke (EXPRESS Study): a Prospective Population−Based Sequential Comparison. Lancet 370 (9596), 1432–1442. doi:10.1016/S0140−6736(07)61448−2
Salanti, G., Ades, A. E., and Ioannidis, J. P. (2011). Graphical Methods and Numerical Summaries for Presenting Results from Multiple−Treatment Meta−Analysis: an Overview and Tutorial. J. Clin. Epidemiol. 64 (2), 163–171. doi:10.1016/j.jclinepi.2010.03.016
Salanti, G., Del Giovane, C., Chaimani, A., Caldwell, D. M., and Higgins, J. P. (2014). Evaluating the Quality of Evidence from a Network Meta−Analysis. PLoS One 9 (7), e99682. doi:10.1371/journal.pone.0099682
Samakova, A., Gazova, A., Sabova, N., Valaskova, S., Jurikova, M., and Kyselovic, J. (2019). The PI3k/Akt Pathway Is Associated with Angiogenesis, Oxidative Stress and Survival of Mesenchymal Stem Cells in Pathophysiologic Condition in Ischemia. Physiol. Res. 68 (Suppl. 2), S131–S138. doi:10.33549/physiolres.934345
Shi, D. H., Zhang, H. T., Zhao, M. Y., He, L., Sun, Q., Tan, J. W., et al. (2011a). Effect of Naoxintong Capsule Combined with Atorvastatin on Secondary Prevention of Acute Cerebral Infarction. Chin. Gen. Pract. 14 (23), 2699–2700. doi:10.3969/j.issn.1007−9572.2011.23.041
Shi, F. H., Wu, Q. Z., and Hu, Y. L. (2011b). Efficacy Analysis of Naoxintong Capsule Combined with Aspirin Tablets and Aspirin Tablets Alone in Secondary Prevention of Cerebral Infarction. Med. Innovation China 8 (22), 45–46. doi:10.3969/j.issn.1674−4985.2011.22.028
Song, H. Q. (2014). Neoclassicism in Art. Hebei J. Traditional Chin. Med. (6), 890–892. doi:10.1002/9781118351352.wbve1436
Sun, H. J. (2020). The Value of Naoxintong Capsule in Secondary Prevention of Ischemic Stroke. Sichuan J. Anat. 28 (01), 26–27. doi:10.3969/j.issn.1005−1457.2020.01.012
Sun, X. Y. (2008). Effect of Sanjin Naomaitai Capsule on Cerebral Infarction. Pract. J. Card. Cereb. Pneumal Vasc. Dis. 16 (7), 30–31. doi:10.3969/j.issn.1008−5971.2008.07.016
Tian, D. F., and Li, X. X. (2010). Clinical Observation of Naoxintong Capsule on Secondary Prevention of 360 Cases of Ischemic Stroke. Yunnan J. Traditional Chin. Med. Materia Med. 31 (12), 36–37. doi:10.3969/j.issn.1007−2349.2010.12.020
Tu, Y. F., Guo, J. C., and Zeng, K. J. (2013). Preventive Effect of Combination of Chinese and Western Medicine on 108 Patients with Cerebral Infarction. Guangming J. Chin. Med. 28 (7), 1412–1414. doi:10.3969/j.issn.1003−8914.2013.07.062
Turner, R. M., Davey, J., Clarke, M. J., Thompson, S. G., and Higgins, J. P. (2012). Predicting the Extent of Heterogeneity in Meta−Analysis, Using Empirical Data from the Cochrane Database of Systematic Reviews. Int. J. Epidemiol. 41 (3), 818–827. doi:10.1093/ije/dys041
Wang, P. P., Li, X. L., Li, X. C., Zhang, M. L., Liu, S. Y., Li, B., et al. (2019). Meta Analysis of Clinical Efficacy and Safety of Naoxintong Capsule Combined with Aspirin and Statins in the Treatment of Cerebral Infarction. Chin. J. Pharmacoepidemiol. 28 (10), 636–642.
Wang, S. H. (2018). Application Effect Evaluation of Buchang Naoxintong Capsule in Preventing Recurrence of Cerebral Infarction. Electron. J. Clin. Med. Lit. 5 (71), 153. doi:10.3877/j.issn.2095−8242.2018.71.141
Wei, J. J. (2016). Progress in Treatment of Cerebral Infarction with Traditional Chinese and Western Medicine. Tianjin Pharm. 28 (04), 56–58.
Wu, X. H., and Xiang, Z. (2018). Clinical Effect of Maixuekang Capsule on Patients with Cerebral Infarction in Convalescence. Chin. J. Mod. Drug Appl. 12 (23), 3–5. doi:10.14164/j.cnki.cn11−5581/r.2018.23.002
Xie, J. H. (2015). Buyang Huanwu Decoction In the Treatment of Ischemic Stroke in Convalescence: A Systematic Review. [dissertation/master‘s thesis]. Chengde, China: Chengde Medical College.
Xu, H. X. (2017). Application Effect of Buchang Naoxintong in Preventing Recurrence of Cerebral Infarction. Contemp. Med. Symp. 15 (05), 139–140.
Xue, M. Z., Mi, G. Q., Wang, L. H., Li, L., and Sun, L. C. (2014). Tongxinluo Capsule Combined with Atorvastatin and Aspirin in the Treatment of Ischemic Stroke with Cerebral Artery Stenosis. Mod. J. Integr. Tradit. Chin. West. Med. (35), 3920–3922. doi:10.3969/j.issn.1008−8849.2014.35.015
Yan, B., Zhou, D., Guo, F. Q., Rao, P., Gao, L., Liu, F. Y., et al. (2008). A Randomized, Prospective, Multicenter, Controlled Clinical Study of Tongxinluo in Patients with Ischemic Stroke (Acute and Subacute). West China Med. J. 23 (5), 945–946.
Yan, F. Q., Yao, C. m., Qin, Y. Q., Chen, Y., Liu, T. Q., and Zhang, Q. P. (2019). Research Progress of Effective Components of Traditional Chinese Medicine in Prevention and Treatment of Cerebral Ischemia−Reperfusion Injury. Acta Chin. Med. 34 (10), 2108–2112.
Ye, X. Q., Xie, Y. M., Zhou, Y. H., Zhao, X. Q., Han, J. H., Wagn, X. Z., et al. (2015). Effect of Naoshuantong Capsule on Change of SSQOL index in Patients with Ischemic Stroke in Six Mouths Follow−Up. Cjcmm 40 (21), 4297–4300. doi:10.4268/cjcmm20152132
Yu, F. S. (2013). Clinical Effect Analysis of Buyang Huanwu Decoction in the Treatment of Cerebral Infarction Recovery. Guide China Med. (22), 263–264.
Yuan, S., Tang, B., Zheng, J., and Larsson, S. C. (2020). Circulating Lipoprotein Lipids, Apolipoproteins and Ischemic Stroke. Ann. Neurol. 88 (6), 1229–1236. doi:10.1002/ana.25916
Zang, W. P., Feng, L. H., and Wang, R. A. (2011). Effect of Buchang Naoxintong Capsule on Secondary Prevention of Cerebral Infarction. Chin. J. Mod. Drug Appl. 5 (2), 166. doi:10.3969/j.issn.1673−9523.2011.02.146
Zhang, H., Xing, Y., Chang, J., Wang, L., An, N., Tian, C., et al. (2019). Efficacy and Safety of NaoShuanTong Capsule in the Treatment of Ischemic Stroke: A Meta−Analysis. Front. Pharmacol. 10, 1133. doi:10.3389/fphar.2019.01133
Zhang, X. C., Cai, Y. F., and Huang, Y. (2012). Discussion on the Clinical Breakthrough point and Advantages of Traditional Chinese Medicine in the Prevention and Treatment of Stroke. J. New Chin. Med. 44 (05), 1–3.
Zhang, X. Z., Zhang, D. X., and Xu, H. Y. (2008). Effect of Buchang Naoxintong on Secondary Prevention of Ischemic Cerebrovascular Disease. Pract. J. Card. Cereb. Pneumal Vasc. Dis. 16 (12), 37. doi:10.3969/j.issn.1008−5971.2008.12.022
Zhen, W. X. (2015). Clinical Effect of Maixuekang Capsule on Patients with Cerebral Infarction in Convalescence. Pharmacol. Clin. Chin. Mater. Med. 31 (4), 247–249.
Zhou, D. S. (2013). Effect of Buchang Naoxintong on Preventing Recurrence of Cerebral Infarction. Health Way 12 (2), 119. doi:10.3969/j.issn.1671−8801.2013.02.121
Zhou, X. L. (2014). Clinical Observation of Tongxinluo in Reducing the Recurrence Rate of Cerebral Infarction. Chin. J. Clin. Rational Drug Use 7 (7), 67–68.
Keywords: traditional Chinese medicine, ischemic stroke, long-term, secondary prevention, recurrent stroke, stroke risk factors, systematical analysis
Citation: Li J, Zhao X, Zhang Y, Wan H, He Y, Li X, Yu L and Jin W (2021) Comparison of Traditional Chinese Medicine in the Long-Term Secondary Prevention for Patients with Ischemic Stroke: A Systematical Analysis. Front. Pharmacol. 12:722975. doi: 10.3389/fphar.2021.722975
Received: 09 June 2021; Accepted: 05 October 2021;
Published: 18 November 2021.
Edited by:
Yi Wang, Zhejiang University, ChinaReviewed by:
You Yun, China Academy of Chinese Medical Sciences, ChinaLu Yan, Institute of Botany (CAS), China
Copyright © 2021 Li, Zhao, Zhang, Wan, He, Li, Yu and Jin. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Li Yu, eXVsaTkxMTlAMTI2LmNvbQ==; Weifeng Jin, amluX3dlaWZlbmdAMTI2LmNvbQ==
†These authors have contributed equally to this work
 Jiali Li
Jiali Li Xixi Zhao2†
Xixi Zhao2† Yangyang Zhang
Yangyang Zhang Haitong Wan
Haitong Wan Yu He
Yu He Xiaohong Li
Xiaohong Li Li Yu
Li Yu Weifeng Jin
Weifeng Jin