
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Pharmacol., 31 August 2021
Sec. Ethnopharmacology
Volume 12 - 2021 | https://doi.org/10.3389/fphar.2021.707394
This article is part of the Research TopicAnti-Inflammatory Agents in the Context of Age-related Cardiometabolic Disease: Ethnopharmacological PerspectivesView all 5 articles
Objectives: We intend to conduct a meta-analysis on the systematic evaluation of traditional Chinese medicine (TCM) in the treatment of ventricular remodeling following acute myocardial infarction (AMI). Our findings may provide certain references for the clinical treatment of ventricular remodeling.
Methods: A systematic literature search was conducted in PubMed, Web of Science, Cochrane Library, Embase, CNKI, Wanfang Data, CQVIP, and CBM before 20 July 2020. Data were analyzed using a random/fixed-effect model. Primary outcomes included the effectiveness and TCM syndrome score (TCMSS). Secondary outcomes included 1) echocardiography data, including the left ventricular end-diastolic diameter (LVEDD), left ventricular end-systolic diameter (LVESD), left ventricular end-diastolic volume index (LVEDVi), left ventricular end-systolic volume index (LVESVi), left ventricular end-diastolic volume (LVEDV), left ventricular end-systolic volume (LVESV), interventricular septum thickness (IVST), left ventricular posterior wall thickness (LVPWT), left ventricular ejection fraction (LVEF), E/A, stroke volume (SV), and wall motion score (WMS); 2) serum indicators, including the B-type natriuretic peptide (BNP) or N-terminal pro-B-type natriuretic peptide (NT-proBNP), and C-reactive protein (CRP) or high sensitivity CRP (hs-CRP); (3) major adverse cardiovascular events (MACE) and other adverse events
Results: Forty RCTs involving 3,659 subjects were recruited. Our findings proved that a combination of TCM or TCM preparations with conventional Western medicine for preventing and reversing ventricular remodeling at post-AMI could remarkably enhance the total effectiveness and reduced TCMSS. Moreover, myocardial functions (LVEF, E/A, and SV), ventricular remodeling (LVEDVi, LVESVi, LVEDV, LVESV, LVEDD, LVESD, LVPWT, and WMS), serum levels of BNP and CRP, and MACE were significantly improved by the combination of TCM or TCM preparations with conventional Western medicine. Nevertheless, IVST and the incidence of other adverse events were comparable between control and experimental groups
Conclusion: The combination of TCM or TCM preparations and conventional Western medicine can alleviate the process of ventricular remodeling, enhance cardiac function, and reduce the incidence of MACE in AMI patients.
With the emergence and gradual application of percutaneous coronary intervention, the mortality due to acute myocardial infarction (AMI) has sharply declined (Bajaj et al., 2015). The hospitalization rate of AMI shows a decreasing trend in recent years. Nevertheless, there are 550,000 new onsets and 200,000 recurrent cases of AMI annually in the United States (Dariush et al., 2016). More seriously, the global burden of cardiovascular diseases and AMI mainly concentrates on low- and middle-income countries. At present, more than 80% of deaths from cardiovascular diseases occur in these countries (Murray et al., 2012; Murray et al., 2015). After AMI, due to oxidative stress, inflammatory response, neuroendocrine regulation, and other reasons, the morphological structure of the myocardium and cardiac fibroblasts changed significantly (Zhang et al., 2021). A series of pathological changes, in turn, affect ventricular size, structure, and function, that is, ventricular remodeling (Liang et al., 2020b). In fact, reduced cardiomyocytes and poor development of viable cardiomyocytes and extracellular matrix are the chief criminals of ventricular remodeling. They not only trigger adverse cardiac events but also activate multiple-system functions like the neurohormonal pathway due to the declined systolic function (McMurray, 2005). As a consequence, a vicious circle following AMI further aggravates ventricular remodeling, thereafter leading to the deterioration of cardiac function, heart failure, malignant arrhythmia, and even cardiac death.
Most drugs that delay ventricular remodeling exert their functions by antagonizing the renin-angiotensin-aldosterone system (RAAS) or cross-talking with it, including angiotensin-converting enzyme inhibitors (ACEIs), angiotensin II receptor blockers (ARBs) and aldosterone antagonists, and β-adrenergic receptor antagonists. Long-term combination therapy can improve clinical symptoms, hemodynamic status, and clinical outcomes of ventricular remodeling. However, ACEIs and ARBs can increase plasma renin activity, which only temporarily reduces plasma aldosterone levels, but cannot block mineralocorticoid receptors. The DREAM trial found that the inhibitory effect of ACEIs alone on the RAAS is far from enough. About 50% of patients with chronic heart failure would suffer from the escape of ACE inhibition (Roig et al., 2000). Although ARBs block the effect of AngII on AT1R, a large dose of ARBs can cause AngII accumulation in the body, which can directly activate AT2R. Although AT2R can antagonize some adverse effects of AT1R, overactivation of AT2R can also increase the risk of cardiovascular events by activating inflammatory factors or other pathological conditions. Mineralocorticoid receptor antagonists are not effective on some non-gene cardiovascular effects of aldosterone. Novel drugs for more effectively regulating the RAAS are under development, including the direct renin inhibitors, ACE2 agonists, AT2R agonists, and aldosterone synthase inhibitors. The direct renin inhibitor aliskiren has been clinically applied, the additional use of which with conventional drugs of ACEIs/ARBs and β-blockers in high-risk myocardial infarction with low left ventricular function cannot improve ventricular remodeling but even induce more adverse events like hypotension and increased serum creatinine and hyperkalemia. Therefore, aliskiren is not recommended to be additionally used in these patients (Solomon et al., 2011). Data of the ASTRONAUT trial demonstrated that the use of aliskiren in patients with chronic heart failure cannot reduce cardiovascular mortality and rehospitalization rate due to heart failure (Gheorghiade et al., 2013). Therefore, searching for effective adjuvant therapy for the current treatment of ventricular remodeling after myocardial infarction has become a new insight.
Compound medicine is superb in achieving a comprehensive outcome, rather than a single target. It contains multiple compounds or compound groups, aiming to obtain a better therapeutic efficacy through several pharmacological mechanisms (Luo et al., 2009). In particular, compound medicine has been extensively applied in the adjuvant treatment of cardiovascular diseases alongside Western medicine, which is featured by satisfactory outcomes and fewer adverse events (Liang et al., 2020a; Liang et al., 2020d). To our knowledge, compound medicine targeting ventricular remodeling lacks in the market. Traditional Chinese medicine (TCM) is natural and has a long history, which is becoming popular throughout the world. Most TCMs are compound preparations. Even a single substance drug has complex ingredients, rather than a single chemical composition. Under the guidance of TCM theory, TCM preparations (such as tablets, injections, aerosols, pills, powders, and pastes) have been widely used in the prevention and health management of human diseases owing to their unique advantages of multi-target involvement.
There is abundant in vitro and in vivo evidence on TCM treatment of ventricular remodeling following AMI. Chen et al. suggested that the Tongguan capsule obviously ameliorates ventricular remodeling and cardiac function in AMI rats, which is superior to captopril (Chen et al., 2010). In a Sprague-Dawley rat model of myocardial infarction, Danhong injection induces upregulation of fibrosis-associated genes (MMP-2 and MMP-9) and VEGF, as well as downregulation of caspase-3. In addition, vascular density in the infarct margin increased in rats administrated with Danhong injection, proving that Danhong injection effectively protects ventricular remodeling and cardiac function (Chen et al., 2016). Liang et al. demonstrated that the Qiliqiangxin capsule improves cardiac function and ventricular remodeling in heart failure rats at post-AMI via upregulating VEGF and phosphorylating Akt (Liang et al., 2016). However, it is noteworthy that a systematic evaluation of the clinical safety and efficacy of TCM compounds in the treatment of ventricular remodeling is lacked because of the deficiency of multi-center, large sample data, which significantly limits their reliability and popularization in clinical practice. In the present study, we intend to conduct a meta-analysis on the systematic evaluation of TCM compounds in the treatment of ventricular remodeling following AMI. Our findings may provide certain references for the clinical treatment of ventricular remodeling.
Relevant literature published before July 20, 2020, was searched in PubMed, Web of Science, Cochrane Library, Embase, CNKI, Wanfang Data, CQVIP, and CBM. The following MeSH (medical subject headings) and free words were searched in the combination: myocardial infarction/acute myocardial infarction + ventricular remodeling/myocardial remodeling/left ventricular remodeling + traditional Chinese medicine/TCM/combination of Chinese and Western medicine/Chinese patent drug/natural medicine + randomized controlled trial/random distribution/random. In addition, relevant data in the Chinese Clinical Trial Registry (ChiCTR) and ClinicalTrails were manually searched to avoid any missing information.
Inclusion and exclusion criteria of random controlled trials (RCTs) about oral administrations of TCM and TCM preparations for intervening AMI were developed according to the Cochrane Handbook for Systematic Reviews of Interventions (version 5.0). Relevant clinical RCTs conducted by either blinding, allocation concealment, or comparison with negative control or placebo were not limited by languages. Research elements should be complete, including research objective, study design, and statistical processing. Recruited AMI patients were not limited by age, gender, time of onset, and case origin. Control subjects were treated by conventional Western medication, including reperfusion treatment, nitrates, anticoagulants, β-receptor blockers, ACEI, and lipid-regulating drugs, and placebos were also included. Meanwhile, TCM or TCM preparations were additionally supplied in the experimental group. General treatments like recumbent and oxygen inhalation were applied in both groups.
The following literature was excluded: 1) unclear diagnostic criteria or non-AMI patients; 2) subjects who had severe primary diseases like brain, liver, or kidney diseases; 3) repeated studies; 4) animal experiments, case reports, reviews, summarize experiences, or ineligible studies lacking the rigorism, main indicators, texts or pathological data; and 5) subjects in the control group who were treated with TCM or TCM preparations.
The quality of recruited literature was independently assessed by two investigators using a risk bias assessment tool as the Cochrane Handbook for Systematic Reviews of Interventions (version 5.0) suggested. Six items were considered, including the method of randomized allocation, allocation concealment, blinding, the integrity of results, selective reporting results, and other resources of biases.
Study selection and data extraction were independently conducted by two investigators based on the searching strategy. At first, searched literature was initially screened for titles and abstracts and re-screened for texts. The following items were extracted from eligible studies, including authors, year, interventions, length of time, sex composition, average age, results, and adverse events. Any disagreement was solved by the third investigator.
Primary outcomes included the effectiveness and TCM syndrome score (TCMSS). Secondary outcomes included 1) echocardiography data, including the left ventricular end-diastolic diameter (LVEDD), left ventricular end-systolic diameter (LVESD), left ventricular end-diastolic volume index (LVEDVi), left ventricular end-systolic volume index (LVESVi), left ventricular end-diastolic volume (LVEDV), left ventricular end-systolic volume (LVESV), interventricular septum thickness (IVST), left ventricular posterior wall thickness (LVPWT), left ventricular ejection fraction (LVEF), E/A, stroke volume (SV), and wall motion score (WMS); 2) serum indicators, including the B-type natriuretic peptide (BNP) or N-terminal pro-B-type natriuretic peptide (NT-proBNP), and C-reactive protein (CRP) or high sensitivity CRP (hs-CRP); and 3) major adverse cardiovascular events (MACE) and other adverse events.
Data processing was conducted using Revman (version 5.3) and Stata (version 14.0). Relative risk (RR) was presented as the effect of binary data, while mean deviation (MD) or standard mean deviation (SMD) were used as that of continuous data. 95% confidence interval (CI) was calculated. The heterogeneity was assessed by the Chi-square test (Liang et al., 2019). I2 < 50% and p > 0.1 were considered no heterogeneity and a fixed-effect model was adopted; otherwise, a random-effect model was introduced (Liang et al., 2021). Potential causes of the heterogeneity were analyzed through subgroup analyses, L’Abbe graph, or radial plots. Sensitivity analysis was performed for assessing the result reliability, and a descriptive analysis was replaced if the heterogeneity was considered high. Funnel plots were depicted for assessing publication biases. A significant difference was set at p < 0.05.
At first, a total of 669 studies were initially searched. Endnote was used to manage the searched studies. After excluding repeated studies, 413 records were screened. 253 other-type studies were excluded, 160 eligible studies were recruited. Later, 101 studies were further excluded because of ineligible research contents or interventions. By reviewing texts in detail, 19 studies were excluded because they were not RCTs or the experiment was not rigorous. At last, 40 studies were recruited for meta-analysis (Figure 1).
Among 40 recruited RCTs (Zhang et al., 2002a; Zhang et al., 2002b; Huang and Hong, 2004; Tang et al., 2004; Zhao et al., 2005; Chen et al., 2006; Dong, 2006; Feng et al., 2006; Zhang, 2006; Chao et al., 2007; Deng et al., 2007; Du et al., 2007; Li et al., 2007; Du et al., 2008; Zhang, 2008; Zhao, 2008; Lin, 2011; Ruan et al., 2011; Ruan, 2012; Yang et al., 2012; Fan, 2014; Li, 2014; Yang et al., 2014; Liu et al., 2016; Shuai et al., 2016; Gong et al., 2017; Jiang et al., 2017; Li, 2017; Wu, 2017; Fan, 2018; Huang et al., 2018; Kai et al., 2018; Li, 2018; Wang et al., 2018; Xiang et al., 2019; Xu et al., 2019; Fang, 2020; Jiang, 2020; Mao et al., 2020; Yang et al., 2020), there were 3,659 subjects, including 1,845 controls treated with conventional Western medicine and 1,814 subjects treated with Western medicine combined with TCM or TCM preparations. Their baseline characteristics are listed in Supplementary Table S1. The details of conventional Western medication are shown in Supplementary Table S2, and details of TCM are shown in Supplementary Table S3.
A total of 25/40 studies reported the method of randomized allocation by random number table or software. The remaining only mentioned that subjects were randomly assigned. One study described allocation concealment in detail. There were four double-blinded studies, and others did not point out blinding or non-blinding (Supplementary Figure S1).
The heterogeneity of the selected 17 studies (Dong, 2006; Du et al., 2007; Fan, 2014; Fan, 2018; Fang, 2020; Feng et al., 2006; Huang et al., 2018; Jiang, 2020; Jiang et al., 2017; Li, 2018; Li, 2017; Li, 2014; Liu et al., 2016; Wang et al., 2018; Xu et al., 2019; Zhang, 2008; Zhao, 2008) reporting the effectiveness of TCM interventions was considered high (I2 = 80%, p = 0.00001 < 0.1), which could be attributed to studies conducted by Zhang 2008 (Zhang, 2008) and Wang 2018 (Wang et al., 2018) via the analysis of the L'Abbe plot (Supplementary Figure S2), radial plot (Supplementary Figure S3A), and sensitivity analysis (Supplementary Figure S4). After removing them, there was no heterogeneity in the remaining 15 studies (I2 = 18%, p = 0.25), and thus, a fixed-effect model was adopted. RR of the 15 studies was 1.25 (95% CI = 1.18–1.32, Z = 7.41, p < 0.05), suggesting that the effectiveness of a combination of TCM or TCM preparations was superb than that of conventional Western medicine (Figure 2A).
Funnel plots were depicted aiming to assess publication biases, and an asymmetric funnel graph suggested the absence of publication bias (Figure 3A). As Begg’s test shown, a certain publication bias existed in the 15 studies (p = 0.003). We thereafter processed the non-symmetric funnel plots through trim and filling. The four points of the square indicated the effectiveness of studies that should be recruited in the future. Taken into consideration of funnel plots, similar studies to Dong 2006 (Dong, 2006), Fan 2014 (Fan, 2014), Li 2018 (Wang et al., 2018), and Fan 2018 (Fan, 2018) are required to be recruited, aiming to eliminate the publication bias (Figure 3B). There was no heterogeneity in the eight studies (Du et al., 2008; Zhao, 2008; Lin, 2011; Huang et al., 2018; Xiang et al., 2019; Xu et al., 2019; Fang, 2020; Jiang, 2020) reporting TCMSS of TCM interventions (I2 = 31%, p = 0.18), and as a result, a fixed-effect model was adopted. SMD of the eight studies was -0.85 (95% CI = -1.01 ∼ -0.69, Z = 10.28, p < 0.05), suggesting that a combination of TCM or TCM preparations was superb in reducing TCMSS than that of conventional Western medicine (Figure 2B). Since the sample size was less than 10, and we did not identify any heterogeneity, publication bias and sensitivity were unnecessary to be examined.
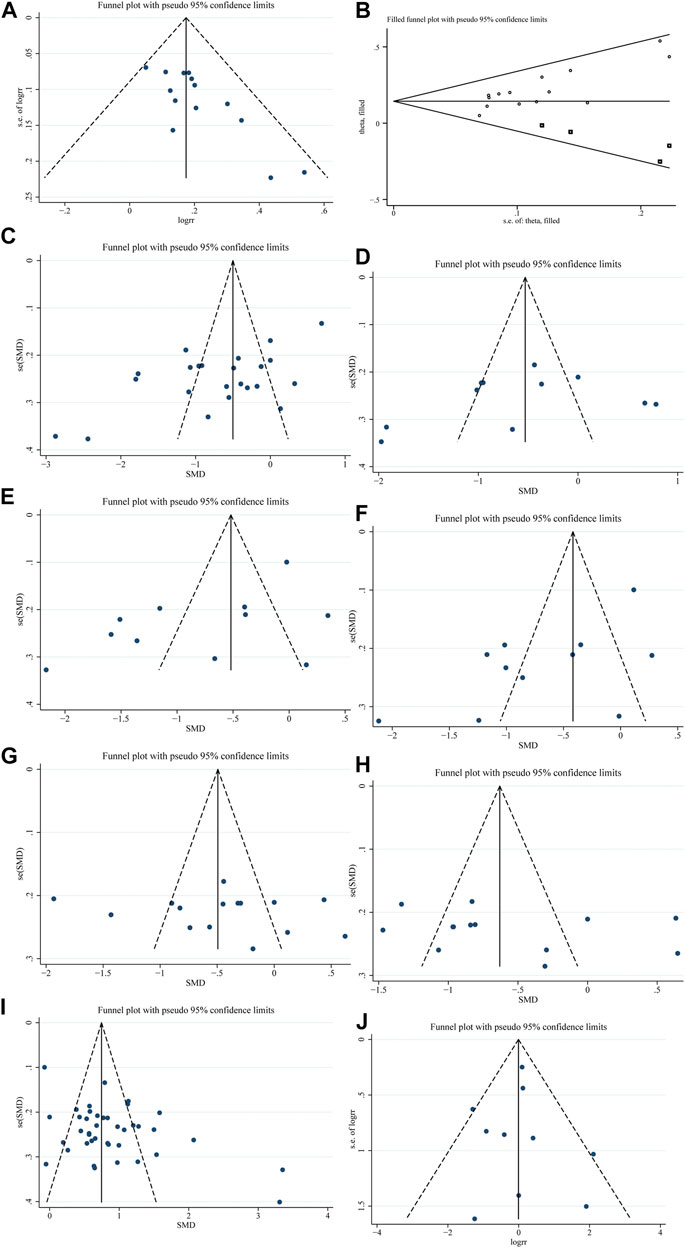
FIGURE 3. Funnel plots. (A). Effectiveness. (B). Effectiveness after trim. (C). LVEDD. (D). LVESD. (E). LVEDVi. (F). LVESVi. (G). LVEDV. (H). LVESV. (I). LVEF. (J). Other adverse events.
There was a significant heterogeneity among 23 studies (Huang and Hong, 2004; Zhao et al., 2005; Dong, 2006; Li et al., 2007; Du et al., 2008; Zhao, 2008; Ruan, 2012; Yang et al., 2012; Fan, 2014; Li, 2014; Liu et al., 2016; Gong et al., 2017; Jiang et al., 2017; Li, 2017; Wu, 2017; Fan, 2018; Huang et al., 2018; Kai et al., 2018; Li, 2018; Wang et al., 2018; Xu et al., 2019; Fang, 2020; Jiang, 2020) (I2 = 92%, p < 0.1), and its source was analyzed by conducting radial plots and sensitivity analysis. Nevertheless, we failed to identify the source of the heterogeneity, which may be explained by differences in the course of interventions, examination instruments, and individualized experiences. As a result, a random-effect model was introduced for meta-analysis. SMD of the 23 studies was -0.72 (95% CI = -1.06 ∼ -0.37, Z = 4.07, p < 0.05), suggesting that a combination of TCM or TCM preparations was superb in reducing LVEDD than that of conventional Western medicine (Figure 4A). The funnel plots were symmetrically distributed (Begg’s test, p = 0.113), indicating the absence of a publication bias (Figure 3C).
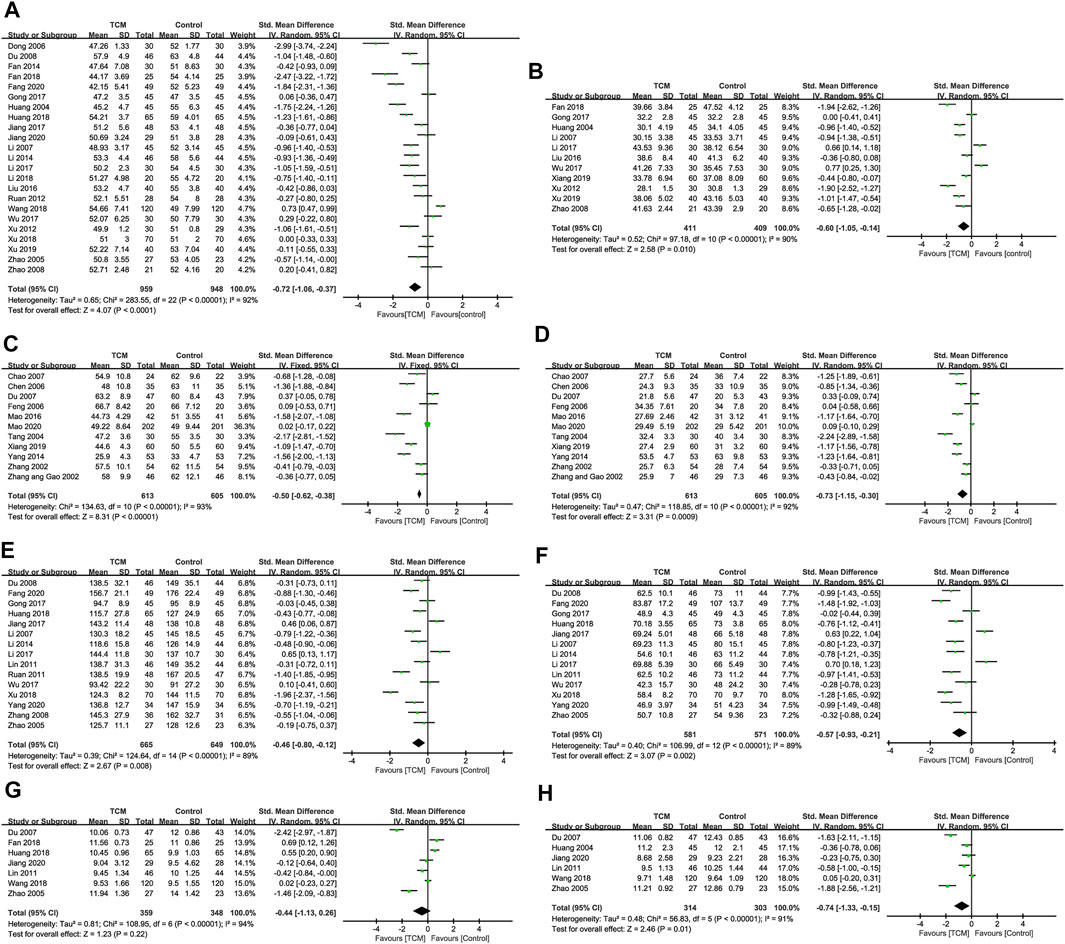
FIGURE 4. Indicators for improving ventricular remodeling. (A). LVEDD. (B). LVESD. (C). LVEDVi. (D). LVESVi. (E). LVEDV. (F). LVESV. (G). IVST. (H). LVPWT.
There was a significant heterogeneity among 11 studies (I2 = 90%, p < 0.1) (Huang and Hong, 2004; Li et al., 2007; Zhao, 2008; Yang et al., 2012; Liu et al., 2016; Gong et al., 2017; Li, 2017; Wu, 2017; Fan, 2018; Xiang et al., 2019; Xu et al., 2019), and we failed to identify the source of the heterogeneity. Therefore, a random-effect model was introduced for meta-analysis. SMD of the 11 studies was -0.60 (95% CI = -1.05 ∼ -0.14, Z = 2.58, p = 0.010 < 0.05), suggesting that a combination of TCM or TCM preparations was superb in reducing LVESD than that of conventional Western medicine (Figure 4B). The funnel plots were symmetrically distributed (Begg’s test, p = 0.436 > 0.05), indicating the absence of a publication bias (Figure 3D).
There was a significant heterogeneity among 11 studies (I2 = 93%, p < 0.1) (Zhang et al., 2002a; Zhang et al., 2002b; Tang et al., 2004; Chen et al., 2006; Dong, 2006; Feng et al., 2006; Chao et al., 2007; Du et al., 2007; Yang et al., 2014; Shuai et al., 2016; Xiang et al., 2019; Mao et al., 2020), and we failed to identify the source of the heterogeneity. Therefore, a random-effect model was introduced for meta-analysis. SMD of the 11 studies was -0.78 (95% CI = −1.24 ∼ −0.32, Z = 3.32, p = 0.0009 < 0.05), suggesting that a combination of TCM or TCM preparations was superb in reducing LVEDVi than that of conventional Western medicine (Figure 4C). The funnel plots were symmetrically distributed (Begg’s test, p = 0.213 > 0.05), indicating the absence of a publication bias (Figure 3E).
There was a significant heterogeneity among 11 studies (I2 = 92%, p < 0.1) (Zhang et al., 2002a; Zhang et al., 2002b; Tang et al., 2004; Chen et al., 2006; Dong, 2006; Feng et al., 2006; Chao et al., 2007; Du et al., 2007; Yang et al., 2014; Shuai et al., 2016; Xiang et al., 2019; Mao et al., 2020), and we failed to identify the source of the heterogeneity. Therefore, a random-effect model was introduced for meta-analysis. SMD of the 11 studies was -0.73 (95% CI = −1.15 ∼ −0.30, Z = 3.31, p = 0.0009 < 0.05), suggesting that a combination of TCM or TCM preparations was superb in reducing LVESVi than that of conventional Western medicine (Figure 4D). The funnel plots were symmetrically distributed (Begg’s test, p = 0.276 > 0.05), indicating the absence of a publication bias (Figure 3F).
There was a significant heterogeneity among 15 studies (I2 = 89%, p < 0.1) (Zhao et al., 2005; Li et al., 2007; Du et al., 2008; Zhang, 2008; Lin, 2011; Ruan et al., 2011; Li, 2014; Gong et al., 2017; Jiang et al., 2017; Li, 2017; Wu, 2017; Huang et al., 2018; Kai et al., 2018; Fang, 2020; Yang et al., 2020), and we failed to identify the source of the heterogeneity. Therefore, a random-effect model was introduced for meta-analysis. SMD of the 15 studies was -0.46 (95% CI = −0.80 ∼ −0.12, Z = 2.67, p = 0.008), suggesting that a combination of TCM or TCM preparations was superb in reducing LVEDV than that of conventional Western medicine (Figure 4E). The funnel plots were symmetrically distributed (Begg’s test, p = 0.843), indicating the absence of a publication bias (Figure 3G).
There was a significant heterogeneity among 13 studies (I2 = 89%, p < 0.1) (Zhao et al., 2005; Li et al., 2007; Du et al., 2008; Lin, 2011; Li, 2014; Gong et al., 2017; Jiang et al., 2017; Li, 2017; Wu, 2017; Huang et al., 2018; Kai et al., 2018; Fang, 2020; Yang et al., 2020), and we failed to identify the source of the heterogeneity. Therefore, a random-effect model was introduced for meta-analysis. SMD of the 13 studies was -0.57 (95% CI = −0.93 ∼ −0.21, Z = 3.07, p = 0.002 < 0.05), suggesting that a combination of TCM or TCM preparations was superb in reducing LVESV than that of conventional Western medicine (Figure 4F). The funnel plots were symmetrically distributed (Begg’s test, p = 0.951), indicating the absence of a publication bias (Figure 3H).
There was a significant heterogeneity among seven studies (I2 = 89%, p < 0.1) (Zhao et al., 2005; Du et al., 2007; Lin, 2011; Fan, 2018; Huang et al., 2018; Wang et al., 2018; Jiang, 2020), and we failed to identify the source of the heterogeneity. Therefore, a random-effect model was introduced for meta-analysis. SMD of the seven studies was -0.44 (95% CI = −1.13–0.26, Z = 1.23, p = 0.22 > 0.05), suggesting that there was no significant difference in IVST between a combination of TCM or TCM preparations with conventional Western medicine (Figure 4G).
There was a significant heterogeneity among six studies (I2 = 91%, p < 0.1) (Huang and Hong, 2004; Zhao et al., 2005; Du et al., 2007; Lin, 2011; Wang et al., 2018; Jiang, 2020), and we failed to identify the source of the heterogeneity. Therefore, a random-effect model was introduced for meta-analysis. SMD of the six studies was -0.74 (95% CI = −1.33 ∼ −0.15, Z = 2.46, p = 0.01), suggesting that a combination of TCM or TCM preparations was superb in reducing LVPWT than that of conventional Western medicine (Figure 4H).
There was a significant heterogeneity among all 40 studies (I2 = 86%, p < 0.1), and we failed to identify the source of the heterogeneity. Therefore, a random-effect model was introduced for meta-analysis. SMD of the 40 studies was 0.87 (95% CI = 0.68–1.05, Z = 9.00, p < 0.05), suggesting that a combination of TCM or TCM preparations was superb in LVEF than that of conventional Western medicine (Figure 5A). The funnel plots were symmetrically distributed (Begg’s test, p = 0.213), indicating the absence of a publication bias (Figure 3I).
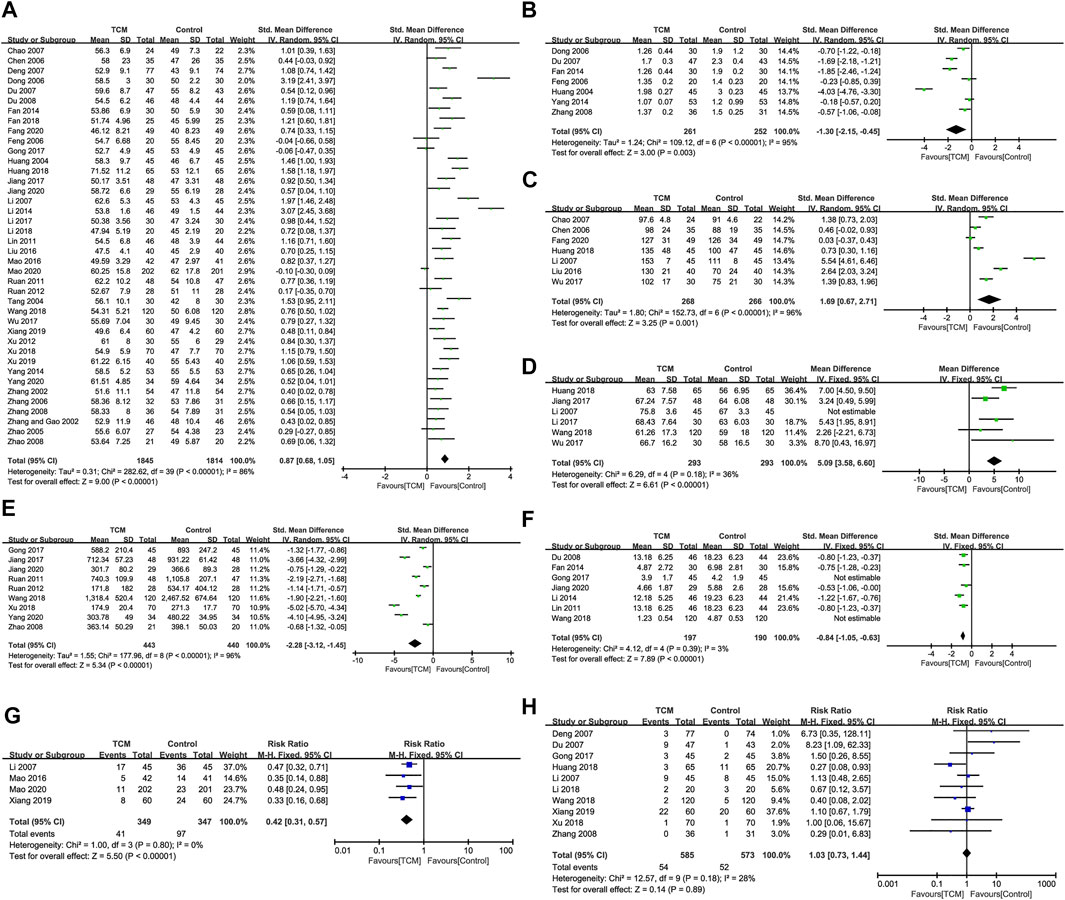
FIGURE 5. Indicators for improving cardiac function, serum indicators, and MACE. (A). LVEF. (B). WMS. (C). E/A. (D). SV. (E). BNP/NT-pro BNP. (F). CRP/hs-CRP. (G). MACE. (H). Other adverse events.
There was a significant heterogeneity among seven studies (I2 = 95%, p < 0.1) (Huang and Hong, 2004; Dong, 2006; Feng et al., 2006; Du et al., 2007; Zhang, 2008; Fan, 2014; Yang et al., 2014), and we failed to identify the source of the heterogeneity. Therefore, a random-effect model was introduced for meta-analysis. SMD of the seven studies was -1.30 (95% CI = −1.06 ∼ −0.08, Z = 3.00, p = 0.003 < 0.05), suggesting that a combination of TCM or TCM preparations was superb in reducing WMS than that of conventional Western medicine (Figure 5B).
There was a significant heterogeneity among seven studies (I2 = 96%, p < 0.1) (Feng et al., 2006; Chao et al., 2007; Deng et al., 2007; Li et al., 2007; Liu et al., 2016; Wu, 2017; Huang et al., 2018), and we failed to identify the source of the heterogeneity. Therefore, a random-effect model was introduced for meta-analysis. SMD of the seven studies was 1.69 (95% CI = 0.83–1.96, Z = 3.25, p = 0.001 < 0.05), suggesting that a combination of TCM or TCM preparations was superb in E/A than that of conventional Western medicine (Figure 5C).
The heterogeneity of the selected six studies reporting the SV of TCM interventions was considered high (I2 = 73%, p = 0.002) (Li et al., 2007; Jiang et al., 2017; Li, 2017; Wu, 2017; Huang et al., 2018; Wang et al., 2018), which could be attributed to studies conducted by Li 2007 (Li et al., 2007) (Supplementary Figure S3, S18D). After removing it, there was no heterogeneity in the remaining five studies (I2 = 36%, p = 0.18), and thus a fixed-effect model was adopted. MD of the five studies was 5.09 (95% CI = 3.58–6.60, Z = 6.61, p < 0.05), suggesting that the effectiveness of a combination of TCM or TCM preparations was superb in SV than that of conventional Western medicine (Figure 5D).
There was a significant heterogeneity among nine studies (I2 = 96%, p < 0.1) (Gong et al., 2017; Jiang, 2020; Jiang et al., 2017; Kai et al., 2018; Ruan et al., 2011; Ruan, 2012; Wang et al., 2018; Yang et al., 2020; Zhao, 2008), and its source was analyzed by conducting radial plots, sensitivity analysis, and subgroup analysis. Nevertheless, we failed to identify the source of the heterogeneity, which may be explained by differences in age, gender, course, and commercial kits. As a result, a random-effect model was introduced for meta-analysis. SMD of the nine studies was -2.28 (95% CI = −1.32 ∼ −0.05, Z = 5.34, p < 0.05), suggesting that a combination of TCM or TCM preparations was superb in reducing BNP/NT-pro BNP than that of conventional Western medicine (Figure 5E). There was a significant heterogeneity among seven studies (I2 = 98%, p < 0.1) (Du et al., 2008; Lin, 2011; Fan, 2014; Li, 2014; Gong et al., 2017; Wang et al., 2018; Jiang, 2020), which could be attributed to studies conducted by Wang 2018 (Wang et al., 2018) and Gong 2017 (Gong et al., 2017) (Supplementary Figure S3C). After removing them, there was no heterogeneity in the remaining five studies (I2 = 3%, p = 0.39), and thus a fixed-effect model was adopted. SMD of the five studies was −0.84 (95% CI = −1.05 ∼ −0.63, Z = 7.89, p < 0.05), suggesting that a combination of TCM or TCM preparations was superb in reducing CRP/hs-CRP than that of conventional Western medicine (Figure 5F).
There was no heterogeneity in the four studies (Li et al., 2007; Mao et al., 2020; Shuai et al., 2016; Xiang et al., 2019) reporting MACE of TCM interventions (I2 = 0, p = 0.80 > 0.1), and as a result, a fixed-effect model was adopted. RR of the four studies was 0.42 (95% CI = 0.31–0.57, Z = 5.50, p < 0.05), suggesting that a combination of TCM or TCM preparations was superb in MACE than that of conventional Western medicine (Figure 5G). There was no heterogeneity among the 10 studies (I2 = 28%, p = 0.18 > 0.1) (Deng et al., 2007; Du et al., 2007; Li et al., 2007; Zhang, 2008; Gong et al., 2017; Huang et al., 2018; Kai et al., 2018; Li, 2018; Wang et al., 2018; Xiang et al., 2019). Therefore, a fixed-effect model was introduced for meta-analysis. RR of the 10 studies was 1.03 (95% CI = 0.73–1.44, Z = 0.14, p = 0.89 > 0.05), suggesting that there was no significant difference in other adverse events between a combination of TCM or TCM preparations with conventional Western medicine (Figure 5H). The funnel plots were symmetrically distributed (Begg’s test, p = 0.721), indicating the absence of a publication bias (Figure 3J).
The heterogeneity of relevant studies reporting the effectiveness was remarkably improved after removing studies conducted by Zhang 2008 (Zhang, 2008) and Wang 2018 (Wang et al., 2018). Echocardiography data (LVEDSi, LVEDVi, LVEDV, LVESD, LVEDD, LVESE, IVST, LVPWT, LVEF, E/A, and WMS) presented a high heterogeneity and its source was unable to be identified after a series of analyses, which may be attributed to differences in age, gender, course, instrument, and experience of the operator. In particular, the heterogeneity of relevant studies reporting SV was markedly improved after removing the study conducted by Li 2007 (Li et al., 2007). The heterogeneity source of BNP, however, was unknown, and we believed that age, gender, course, and commercial kits may cause the source. Studies conducted by Gong 2017 (Gong et al., 2017) and Wang 2018 (Wang et al., 2018) were the sources of the heterogeneity of CRP. Fixed-effect models were introduced for analyzing TCMSS, MACE, and adverse events since they did not have any heterogeneity.
Sensitivity analysis was performed for assessing the result reliability. Removal of any study did not obviously affect the general results, suggesting the robust results we obtained, except for effectiveness results of Zhang 2008 (Zhang, 2008) and Wang 2018 (Wang et al., 2018), SV results of Li 2007 (Li et al., 2007), and CRP/hs-CRP results of Gong 2017 (Gong et al., 2017) and Wang 2018 (Wang et al., 2018) (Supplementary Figures S4–S6). And the 4 RCTs were considered as the source analysis of heterogeneity of effectiveness, SV, and CRP/hs-CRP. We did not identify any heterogeneity about TCMSS, MACE, and other adverse events; therefore, sensitivity was unnecessary to be examined.
The subgroup analysis was carried out when we try to find the heterogeneity of BNP/NT-proBNP and CRP/hs-CRP. However, there was nothing that could be found. We did not perform the subgroup analysis about other outcomes. In addition, we found that the duration of studies also varies, from weeks to months, so we conducted subgroup analysis according to the intervention duration. According to the results of intervention duration subgroup analysis (Supplementary Table S4), we found that in some outcome indicators, the heterogeneity was not completely eliminated after grouping, indicating that the difference of intervention duration may not be the potential source of heterogeneity.
At present, Western medicine is widely applied in the treatment and reverse of ventricular remodeling at post-AMI. For instance, imidapril, a type of ACEI, is able to suppress the remodeling of the left ventricle by inhibiting MMP activity in the plasma of AMI patients (Yokota et al., 2014). ARBs exert a similar function to that of ACEIs (Yokota et al., 2010). Statins like atorvastatin are demonstrated to defend inflammatory response via downregulating IL-1, IkBα, and NF-κB p50, thus preventing ventricular remodeling in rats (Karla et al., 2016). Besides, statin treatments are capable of alleviating ventricular remodeling in AMI patients through recovering the coronary endothelial function through endogenous nitric oxide (Ishida et al., 2012). The guidelines recommend that ACEI should be applied to all AMI patients as soon as possible, and ARB is recommended for patients who cannot tolerate ACEI. ACEI/ARB doses need to be titrated to the target dose or maximum tolerable dose. In the past 2 years, sacubitril/valsartan has been proven to be superior to ACEI/ARB in improving cardiac outcomes and reversing ventricular remodeling (Hajra et al., 2019). Besides, sacubitril/valsartan could improve exercise tolerance (Malfatto et al., 2020; Piepoli et al., 2021), showing promising applications in the treatment of AMI and reducing all-cause deaths. The TCM theory considers that blood stasis syndrome, phlegm-dampness syndrome, Qi-deficiency syndrome, Yang-deficiency syndrome, deficiency in origin, and excess in superficiality or deficiency-excess mixing occur following AMI. Therefore, TCM treatment mainly focuses on the holistic and individualized treatment of AMI patients. In clinical practice, Pinellia ternata, Carthamus tinctorius, Peach Kernel, Salvia miltiorrhiza, Trichosanthes kirilowii, Scutellaria baicalensis, Codonopsis, and Monkey Grass are usually used in the treatment of AMI. TCM compounds or preparations are composed of a single or multiple TCM under the guidance of the TCM principle and method, which are adjusted based on ancient, classical, and modern prescriptions (Luo et al., 2009). Generally speaking, Western medicine is featured by a direct function on the lesion and target, while TCM highlights the balance of the whole body (Liang et al., 2020c). It is considered that a combination of Western medicine and TCM is capable of enhancing the therapeutic efficacy through taking both of their advantages, thus achieving the goal of the simultaneous treatment of root and tip, rather than a single target/organ/system (Liang et al., 2020d). Recent evidence underlying the mechanisms of TCM in treating ventricular remodeling at post-AMI has emerged. It is reported that the Heart-Protecting Musk Pill treatment remarkably declines the collagen-positive area and improves the left ventricular function by downregulating IL-6 and TNF-α in rats following AMI (Cen et al., 2017). A combination of Tanshinone IIA and puerarin effectively inhibits infiltration of inflammatory cells, myocardial fibrosis, and ventricular fibrosis, therefore protecting the hemodynamics of AMI mice (Gao et al., 2019). As a result, the application of TCM or TCM preparations in the treatment of ventricular remodeling at post-AMI should be well concerned.
Once myocardial ischemia occurs, inflammatory factors (IL-1, caspase-1) immediately trigger the strong infiltration of neutrophils, and lymphocytes and macrophages are also involved in, that is, the inflammation phase (Mezzaroma et al., 2011; Yan et al., 2013). Later, the enlarged ischemia lesion acutely expands the ventricle and the infarcted ventricular wall. Meanwhile, extracellular matrixes are degraded and cardiac fibroblasts are rapidly proliferated, leading to the synthesis of collagens, that is, the proliferation phase. With the pathological process, the newly formed scar becomes mature which maintains the shape of the heart and prevents the formation of an aneurysm, that is, the mature phase (Frangogiannis, 2014; Seropian et al., 2014). In the initial phase, the heart is able to compensatively maintains the cardiac output through ventricular dilation. However, the compensatory mechanism eventually causes cardiac dysfunction and heart failure over time (Seropian et al., 2014). In clinical practice, echocardiography is generally applied to effectively reflect the degree of ventricular remodeling by quantifying the diameter, volume, and wall thickness of the left ventricle. In the present study, we comprehensively analyzed echocardiography data from 40 RCTs and demonstrated that a combination of TCM or TCM preparations with conventional Western medicine more pronouncedly reduced LVEDSI, LVEDVI, LVEDV, LVESV, LVEDD, LVESD, and LVPWT in AMI patients in comparison to controls (p < 0.05). IVST was comparable between groups (p > 0.05). BNP or NT-proBNP is a quantified biomarker of heart failure that refers to the diastolic and systolic functions of the left ventricle. It is usually utilized for assessing the prognosis of AMI (Alvin et al., 2013). Here, we assessed the prognosis of ventricular remodeling at post-AMI and MACE by detecting cardiac functions. It is shown that a combination of TCM or TCM preparations with conventional Western medicine was superb in elevating LVEF, E/A, and SV and reducing wall motion score, serum level of BNP, and MACE rate than controls (p < 0.05). In addition, the results of SV were robust after removing a single study conducted by Li 2007 (Li et al., 2007). Publication bias about LVEF was absent as well. CRP is an acute-phase protein that is produced by the stimulation of pro-inflammatory cytokines, which is considered a risk factor for cardiovascular diseases. Excessive inflammation will aggravate the occurrence of fibrosis and lead to pathological remodeling (Kaneko et al., 2011; Anzai, 2018; Rita et al., 2018) Our results revealed that combining treatment of TCM or TCM preparations with Western medicine more obviously reduced serum level of CRP in AMI patients than those who solely treated with Western medicine (p < 0.05). After removing studies of Gong 2017 (Gong et al., 2017) and Wang 2018 (Wang et al., 2018), the results remained robust. We did not obtain a significant difference in the rate of adverse events between groups (p > 0.05). The determination of the effectiveness and TCMSS was in accordance with the Guiding Principles for Clinical Research of New Chinese Medicines (Trial) in 2002, the Diagnostic Criteria of TCM Syndrome Differentiation for Coronary Heart disease revised by the Chinese Association of Integrative Medicine in October 1990 (Zhao, 2008), and Guidelines for the Diagnosis and Treatment of Acute Coronary Heart disease (CHD Myocardial Infarction) (Zhao, 2008). Compared with controls, TCM or TCM preparation combined with Western medicine markedly elevated the total effectiveness and reduced TCMSS (p < 0.05). After removing studies of Zhang 2008 (Zhang, 2008) and Wang 2018 (Wang et al., 2018), the single study posed few impacts on the total effectiveness. In addition, recruitment of similar studies to Dong 2006 (Dong, 2006), Fan 2014 (Fan, 2014), Li 2018 (Li, 2018), and Fan 2018 (Fan, 2018) in the future is able to eliminate the current publication bias.
Taken together, this study systematically assesses the function of TCM or TCM preparations in the treatment of vascular remodeling at post-AMI. A total of 40 RCTs, involving 3,659 AMI patients, were recruited. Our findings proved that a combination of TCM or TCM preparations with conventional Western medicine for preventing and reversing ventricular remodeling at post-AMI could remarkably enhance the total effectiveness and myocardial function (LVEF, E/A, SV, and WMS), manifesting as reduced TCMSS, the diameter, volume and wall thickness of the left ventricle (LVEDSi, LVEDVi, LVEDV, LVESV, LVEDD, LVESD, and LVPWT), serum levels of BNP and CRP, and MACE rate. Nevertheless, IVST and the incidence of other adverse events were comparable between control and experimental groups. Because of differences in age, sex, course, instruments, and individualized experiences, the heterogeneity of echocardiography data and serum levels of CRP and BNP are considered high, and its source should be further determined by subgroup analyses. Although TCM is considered to be safe because of no significant difference in the incidence of other adverse events between groups, only 10 studies mentioned adverse events during the treatment. Therefore, the safety of TCM or TCM preparation in the treatment of ventricular remodeling at post-AMI requires to be further validated in clinical trials. This study for the first time assessed that the additional use of TCM or TCM preparations based on conventional Western medicine significantly improved ventricular remodeling at post-AMI, which were conductive to make clinical decisions.
Nevertheless, the present study has some limitations. First of all, TCM is mainly applied in China. As a result, relevant clinical data abroad are lacked. Secondly, the quality of recruited literature should be concerned as the specific randomized method and blinding are not mentioned in some studies. Thirdly, mortality is rarely reported in the recruited studies. Hence, we are unable to determine the long-term efficacy of TCM and its further clinical application. Fourthly, the heterogeneity source is difficult to be searched. Fifthly, there are multiple TCM syndrome types at post-AMI. In the present meta-analysis, we only analyzed whether an additional use of TCM or TCM preparation can enhance the therapeutic efficacy of Western medicine solely at post-AMI, while the potential function of different TCMs in AMI with the same syndromes was failed to be analyzed. Analyzing the therapeutic effect of TCM preparations containing multiple traditional Chinese herbals could be more complicated or general than that of a single TCM or monomer, which may result in heterogeneity. Moreover, only some of the recruited studies described the detailed chemical components and quality evaluation measures of TCM, which should be further verified (Supplementary Table S3). Finally, several RCTs did not mention the baseline characteristics of subjects and specific drugs used in control groups. As a result, we only analyzed whether TCM or TCM preparations could yield a better efficacy on AMI patients compared with controls, which may result in heterogeneity. The accuracy of the results we obtained needs to be further validated.
This study concluded that a combination of TCM or TCM preparations with conventional Western medicine can effectively enhance the efficacy on preventing and reversing ventricular remodeling at post-AMI, which also significantly reduces TCMSS, serum levels of BNP and CRP, and the incidence of MACE, as well as improving ventricular remodeling and cardiac function. In addition, no significant differences in adverse events and IVST are detected by additionally applying TCM or TCM preparations on the basis of conventional Western medicine for the treatment of AMI. Our results should be validated in double-blinded, multi-center studies with a large sample in the future because of the relatively high heterogeneity. In addition, in future studies, we will analyze the chemical composition, safety, and efficacy of a series of TCM preparations to further validate their potentials in clinical application.
The original contributions presented in the study are included in the article/Supplementary Material; further inquiries can be directed to the corresponding author.
XZ and BL contributed to this work equally. XZ, BL, and NG proposed the subject and designed the protocol for this systematic review. XZ, BL, and CS conducted literature screening and data extraction. XZ and BL performed the statistical analysis. All authors interpreted the results. XZ and BL drafted the manuscript. NG coordinated and inspected all aspects of the research design. All authors contributed to the revision of the manuscript and approved the final manuscript for submission.
This study was partly funded by the National Natural Science Foundation of China (81774229), Research and Practice Innovation Plan for Postgraduates of Jiangsu, China (KYCX21_1641), Jiangsu Leading Talent Project of Traditional Chinese Medicine (Jiangsu TCM 2018 No.4), and Jiangsu Universities Nursing Advantage Discipline Project (2019YSHL095).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
We thank all relevant published studies and individuals involved in TCM and ventricular remodeling.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fphar.2021.707394/full#supplementary-material
Alvin, N., Marzuki, S., and Marulam, P. (2013). Potential Clinical Application of Novel Cardiac Biomarkers for Acute Myocardial Infarction. Acta Med. Indones. 45 (3), 240–250.
Anzai, T. (2018). Inflammatory Mechanisms of Cardiovascular Remodeling. Circ. J. 82 (3), 629–635. doi:10.1253/circj.cj-18-0063
Bajaj, A., Sethi, A., Rathor, P., Suppogu, N., and Sethi, A. (2015). Acute Complications of Myocardial Infarction in the Current Era. J. Invest. Med. 63 (7), 844–855. doi:10.1097/jim.0000000000000232
Cen, W., Chen, Z.-L., Gu, N., and Hoppe, R. (2017). Prevention of AMI Induced Ventricular Remodeling: Inhibitory Effects of Heart-Protecting Musk Pill on IL-6 and TNF-Alpha. Evid. Based Complement. Alternat. Med. 2017, 3217395. doi:10.1155/2017/3217395
Chen, B.-J., Feng, J.-X., Su, X.-X., Meng, L.-Q., Li, Z.-S., Gao, Y.-L., et al. (2010). Effects of Tongguan Capsule (通冠胶囊) on post-myocardial Infarction Ventricular Remodeling and Cardiac Function in Rats. Chin. J. Integr. Med. 16 (2), 157–161. doi:10.1007/s11655-010-0157-1
Chen, B.-J., Su, X.-X., and Pan, Z.-Q. (2006). Clinical Study of Tongguan Capsule on Inhibiting Left Ventricular Remodeling after Acute Myocardial Infarction. Jiangsu Traditional Chin. Med. 27 (2), 23–24. doi:10.3389/fphys.2018.00589
Chen, J., Cao, W., Asare, P. F., Lv, M., Zhu, Y., Li, L., et al. (2016). Amelioration of Cardiac Dysfunction and Ventricular Remodeling after Myocardial Infarction by Danhong Injection Are Critically Contributed by Anti-TGF-β-mediated Fibrosis and Angiogenesis Mechanisms. J. Ethnopharmacology 194, 559–570. doi:10.1016/j.jep.2016.10.025
Dariush, M., Mozaffarian, D., Benjamin, E. J., Go, A. S., Arnett, D. K., Blaha, M. J., et al. (2016). Executive Summary: Heart Disease and Stroke Statistics--2016 Update: A Report from the American Heart Association. Circulation 133 (4), 447–454. doi:10.1161/CIR.0000000000000366
Deng, S.-L., Lin, H.-J., and Zhong, C.-M. (2007). Study on Improvement of Left Ventricular Function in Patients with Acute Myocardial Infarction by Wenyang Buqi Decoction. Chin. West. Med. J. cardio Cerebrovasc. Dis. 5 (1), 3–4. doi:10.1007/s10557-018-6804-z
Dong, X.-R. (2006). “Research on the Effects of Reversing Left Ventricular Remodeling after Acute Myocardial Infarction by Yiqihuoxue Prescription,” in Henan Coll. Traditional Chin. Med. Editor D. Xiaorui, 4, 787–795. doi:10.1007/s10554-012-0159-5
Du, W.-X., Zhu, M.-D., Feng, L.-M., Song, Q.-G., Wei, Y., Ma, P., et al. (2008). Intervention Effect of Qishenyiqi Gutta Pill on Early Ventricular Remodeling after Acute Myocardial Infarction. Chin. J. Evidence-Based Cardiovasc. Med. 1 (1), 41–43.
Fan, Y.-Y. (2014). “The Clinic Investigation about the Effect of Shenzao Yangxintang on the Left Ventricular Remodeling of Acute Myocardial Infarction Who Had Treated by Percutaneous Coronary Intervention, and Were Belong to Qi Stagnation and Blood Stasis in the Traditional Chinese Medicine,” in Guangzhou Univ. Chin. Med. Editor F. Yanyan, 4, 391–397. doi:10.4103/0253-7613.135950
Fan, Y. (2018). Effect of Xingengjiuni Decoction on Ventricular Remodeling and Cardiac Function in Patients with Acute Myocardial Infarction. Henan Med. Res. 27 (12), 2230–2231. doi:10.4103/0253-7613.135950
Fang, K.-Y. (2020). Effect of Yugeng Tongyu Decoction on miRNA-21,GDF-15 Expression and Ventricular Remodling in Patients with Myocardial Infarction. J. Huaihai Med. 38 (2), 117–119. doi:10.1136/thoraxjnl-2014-206225
Feng, Q.-M., Dong, Y.-R., and Yang, Z.-F. (2006). Effect of Yiqihuoxue Recipe on Left Ventricular Remodeling after Acute Myocardial Infarction. Chin. J. Rehabil. Theor. Pract. 12 (6), 475–477. doi:10.1155/2014/745919
Frangogiannis, N. G. (2014). The Immune System and the Remodeling Infarcted Heart. J. Cardiovasc. Pharmacol. 63 (3), 185–195. doi:10.1097/fjc.0000000000000003
Gao, S., Li, L., Li, L., Ni, J., Guo, R., Mao, J., et al. (2019). Effects of the Combination of Tanshinone IIA and Puerarin on Cardiac Function and Inflammatory Response in Myocardial Ischemia Mice. J. Mol. Cell Cardiol. 137, 59–70. doi:10.1016/j.yjmcc.2019.09.012
Gheorghiade, M., Böhm, M., Greene, S. J., Fonarow, G. C., Lewis, E. F., Zannad, F., et al. (2013). Effect of Aliskiren on Postdischarge Mortality and Heart Failure Readmissions Among Patients Hospitalized for Heart Failure. JAMA 309 (11), 1125–1135. doi:10.1001/jama.2013.1954
Gong, J., Jiang, W.-B., and Gu, N. (2017). Clinical Efficacy of Guanxin Ⅴ Mixture in Treating Ventricular Remodeling after Acute Myocardial Infarction and its Mechanism. China Pharmaceuticals 26 (22), 30–33. doi:10.1186/s12906-021-03211-7
Hajra, A., Ujjawal, A., Sud, K., Chakraborty, S., and Bandyopadhyay, D. (2019). Sacubitril/valsartan Averts post-myocardial Infarction Ventricular Remodeling and Preserves Heart Function. IJC Heart & Vasculature 22, 218–219. doi:10.1016/j.ijcha.2019.02.005
Huang, X.-L., Luan, Y.-H., Shi, H.-Y., and Li, L. (2018). Clinical Study on Buyang Huanwu Decoction on Cardiac Remodeling and Cardiac Function in Patients with Myocardial Infarction. Shaanxi J. Traditional Chin. Med. 39 (10), 1360–1362. doi:10.1155/2012/385247
Huang, X.-P., and Hong, R.-R. (2004). Clinical Observation of Yiqi Huoxue Capsule against Early Left Ventricular Remodeling after Myocardial Infarction. J. Guangzhou Univ. Traditional Chin. Med. 21 (3), 185–187. doi:10.1161/01.cir.101.25.2981
Ishida, K., Geshi, T., Nakano, A., Uzui, H., Mitsuke, Y., Okazawa, H., et al. (2012). Beneficial Effects of Statin Treatment on Coronary Microvascular Dysfunction and Left Ventricular Remodeling in Patients with Acute Myocardial Infarction. Int. J. Cardiol. 155 (3), 442–447. doi:10.1016/j.ijcard.2011.11.015
Jiang, T. (2020). in Study of Shenjie Granules on Cardiac Function in Patients with Qi Deficiency and Blood Stasis after PCI of Acute Myocardial Infarction. J. Ting (Nanjing, China: Nanjing University of Chinese Medicine).
Jiang, X.-X., Qian, M., Leng, J., and Lu, J.-Y. (2017). Effect of Xuanbi Tongmai Decoction Combined with Metoprolol on Early Ventricular Remodeling and Cardiac Function after Acute Myocardial Infarction. Liaoning J. Traditional Chin. Med. 44 (9), 1917–1920. doi:10.1067/mhj.2001.117966
Kai, X., Cun-Rui, Z., Hong, G., Mu, S., Zong-Xing, X., Ru-Fei, C., et al. (2018). The Effect of Shenxiong Injection Combined with Captopril on Ventricular Remodeling and Serum Brain Natriuretic Peptide in Patients with Myocardial Infarction. China Med. Herald 15 (3), 130–133.
Kaneko, H., Anzai, T., Takahashi, T., Kohno, T., Shimoda, M., Sasaki, A., et al. (2011). Role of Vascular Endothelial Growth Factor-A in Development of Abdominal Aortic Aneurysm. Cardiovasc. Res. 91 (2), 358–367. doi:10.1093/cvr/cvr080
Karla, R., Rafael, P. d. C. H., Anali, G. T., Daniela, D. d. C., Andrei, C. S., Alexandre, d. S. V. K., et al. (2016). Atorvastatin Improves Ventricular Remodeling after Myocardial Infarction by Interfering with Collagen Metabolism. PLoS One 11 (11), e0166845. doi:10.1371/journal.pone.0166845
Li, B. (2018). Effect of Shuxuetong Injection in the Treatment of Acute Myocardial Infarction with Conventional Western Medicine and its Influence on Left Ventricular Remodeling and Cardiac Function. Inner Mongolia J. Traditional Chin. Med. 37 (11), 61–63. doi:10.16040/j.cnki.cn15-1101.2018.11.044
Li, J. (2017). Effect of Combined Chinese and Western Medicine on Early Ventricular Remodeling and Cardiac Function after AMI. J. Pract. Gynecol. Endocrinol. 4 (30), 107–108. doi:10.16484/j.cnki.issn2095-8803.2017.30.074
Li, Q.-H. (2014). Clinical Study on Early Ventricular Remodeling after Acute Myocardial Infarction Treatment of Yiqi Huayu Capsule. Editor L. Qiuhong (Tangshan: Hebei United University).
Li, Z., Zheng, W.-L., and Wu, H. (2007). Influence of Guanxinning Injection on Left Ventricular Remodeling after Acute Myocardial Infarction. Chin. J. Integrated Traditional West. Med. Intensive Crit. Care 14 (4), 227–230.
Liang, B., Liang, Y., Zhao, L.-Z., Zhao, Y.-X., and Gu, N. (2021). Rivaroxaban for Cancer-Associated Venous Thromboembolism. Sci. Prog. 104 (2), 368504211012160. doi:10.1177/00368504211012160
Liang, B., Qu, Y., Zhao, Q.-F., and Gu, N. (2020a). Guanxin V for Coronary Artery Disease: A Retrospective Study. Biomed. Pharmacother. 128, 110280. doi:10.1016/j.biopha.2020.110280
Liang, B., Zhang, X.-X., and Gu, N. (2020b). Virtual Screening and Network Pharmacology-Based Synergistic Mechanism Identification of Multiple Components Contained in Guanxin V against Coronary Artery Disease. BMC Complement. Med. Ther. 20 (1), 345. doi:10.1186/s12906-020-03133-w
Liang, B., Zhao, L.-Z., Liao, H.-L., and Gu, N. (2019). Rivaroxaban for Cancer-Associated Venous Thromboembolism: A Systematic Review and Meta-Analysis Protocol. Medicine 98 (48), e18087. doi:10.1097/md.0000000000018087
Liang, B., Zhou, Y., Fu, L., and Liao, H.-L. (2020c). Antiarrhythmic Mechanisms of Chinese Herbal Medicine Dingji Fumai Decoction. Evid. Based Complement. Alternat. Med. 2020, 9185707. doi:10.1155/2020/9185707
Liang, B., Zou, F.-H., Fu, L., and Liao, H.-L. (2020d). Chinese Herbal Medicine Dingji Fumai Decoction for Ventricular Premature Contraction: A Real-World Trial. Biomed. Res. Int. 2020, 5358467. doi:10.1155/2020/5358467
Liang, T., Zhang, Y., Yin, S., Gan, T., An, T., Zhang, R., et al. (2016). Cardio-protecteffect of Qiliqiangxin Capsule on Left Ventricular Remodeling, Dysfunction and Apoptosis in Heart Failure Rats after Chronic Myocardial Infarction. Am. J. Transl Res. 8 (5), 2047–2058.
Lin, X.-D. (2011). Clinical Trial of Compound Danshen Dripping Pill on Ventricular Remodeling after Acute Myocardial Infarction. World Chin. Med. 6 (2), 111–112.
Liu, C.-X., Wan, g. Y.-T., and Gu, C.-Y. (2016). Effects of Shuxuetong Injection on Left Ventricular Remodeling and Cardiac Function in Patients with Acute Myocardial Infarction. Mod. J. Integrated Traditional Chin. West. Med. 25 (16), 1758–1760. doi:10.3969/j.issn.1008-8849.2016.16.015
Luo, G.-A., Liang, Q.-L., Liu, Q.-F., Li, X., and Wang, Y.-M. (2009). Prospect on the Composite Drugs Innovation System. World Sci. Technology 11 (1), 3–10. doi:10.1016/S1876-3553(10)60006-3
Malfatto, G., Ravaro, S., Caravita, S., Baratto, C., Sorropago, A., Giglio, A., et al. (2020). Improvement of Functional Capacity in Sacubitril-Valsartan Treated Patients Assessed by Cardiopulmonary Exercise Test. Acta Cardiologica 75 (8), 732–736. doi:10.1080/00015385.2019.1669317
Mao, S., Ouyang, W., Zhou, Y., Zeng, R., Zhao, X., Chen, Q., et al. (2020). Addition of Chinese Herbal Remedy, Tongguan Capsules, to the Standard Treatment in Patients with Myocardial Infarction Improve the Ventricular Reperfusion and Remodeling: Proteomic Analysis of Possible Signaling Pathways. J. Ethnopharmacology 257, 112794. doi:10.1016/j.jep.2020.112794
McMurray, J. J., and Pfeffer, M. A. (2005). Heart Failure. The Lancet 365, 1877–1889. doi:10.1016/s0140-6736(05)66621-4
Mezzaroma, E., Toldo, S., Farkas, D., Seropian, I. M., Van Tassell, B. W., Salloum, F. N., et al. (2011). The Inflammasome Promotes Adverse Cardiac Remodeling Following Acute Myocardial Infarction in the Mouse. Proc. Natl. Acad. Sci. 108 (49), 19725–19730. doi:10.1073/pnas.1108586108
Murray, C. J., Vos, T., Lozano, R., Naghavi, M., Flaxman, A. D., Michaud, C., et al. (2012). Disability-adjusted Life Years (DALYs) for 291 Diseases and Injuries in 21 Regions, 1990-2010: a Systematic Analysis for the Global Burden of Disease Study 2010. Lancet 380 (9859), 2197–2223. doi:10.1016/S0140-6736(12)61689-4
Murray, C. J. L., Barber, R. M., Foreman, K. J., Ozgoren, A. A., Abd-Allah, F., Abera, S. F., et al. (2015). Global, Regional, and National Disability-Adjusted Life Years (DALYs) for 306 Diseases and Injuries and Healthy Life Expectancy (HALE) for 188 Countries. quantifying epidemiological Transit. Lancet, 386(10009), 2145–2191. doi:10.1016/S0140-6736(15)61340-X
Piepoli, M. F., Hussain, R. I., Comin‐Colet, J., Dosantos, R., Ferber, P., Jaarsma, T., et al. (2021). OUTSTEP‐HF: Randomised Controlled Trial Comparing Short‐term Effects of Sacubitril/valsartan versus Enalapril on Daily Physical Activity in Patients with Chronic Heart Failure with Reduced Ejection Fraction. Eur. J. Heart Fail. 23 (1), 127–135. doi:10.1002/ejhf.2076
Rita, C. A., Oliveira, S. S., and Clara, S. S. (2018). The Use of High Sensitivity C-Reactive Protein in Cardiovascular Disease Detection. J. Pharm. Pharm. Sci. 21 (1), 496–503. doi:10.18433/jpps29872
Roig, E., Perez-Villa, F., Morales, M., Jiménez, W., Orús, J., Heras, M., et al. (2000). Clinical Implications of Increased Plasma Angiotensin II Despite ACE Inhibitor Therapy in Patients with Congestive Heart Failure. Eur. Heart J. 21 (1), 53–57. doi:10.1053/euhj.1999.1740
Ruan, L., Qin, F., Fu, L., Tang, Y.-R., Wang, J., Zheng, Q., et al. (2011). Reperfusion in Acute Myocardial Infarction Left Ventricular Remodeling and Cardiac Function of Xuemaikang. J. Pract. Cardio-Cerebral Pulm. Vasc. Dis. 19 (4), 573–574.
Ruan, X.-F. (2012). Influence of Kangxin Decoction on Cardiac Function and Ventricular Remodeling of Acute Myocardial Infarction. J. Emerg. traditional Chin. Med. 21 (7), 1033–1034.1036
Seropian, I. M., Toldo, S., Van Tassell, B. W., and Abbate, A. (2014). Anti-Inflammatory Strategies for Ventricular Remodeling Following ST-Segment Elevation Acute Myocardial Infarction. J. Am. Coll. Cardiol. 63 (16), 1593–1603. doi:10.1016/j.jacc.2014.01.014
Shuai, M., Lei, W., Wen-Wei, O., Yuan-Shen, Z., Jian-Yong, Q., Li-Heng, G., et al. (2016). Traditional Chinese Medicine, Danlou Tablets Alleviate Adverse Left Ventricular Remodeling after Myocardial Infarction: Results of a Double-Blind, Randomized, Placebo-Controlled, Pilot Study. BMC Complement. Altern. Med. 16 (1), 447. doi:10.1186/s12906-016-1406-4
Solomon, S. D., Hee Shin, S., Shah, A., Skali, H., Desai, A., Kober, L., et al. (2011). Effect of the Direct Renin Inhibitor Aliskiren on Left Ventricular Remodelling Following Myocardial Infarction with Systolic Dysfunction. Eur. Heart J. 32 (10), 1227–1234. doi:10.1093/eurheartj/ehq522
Tang, Y.-P., Liu, Y., and Liang, P. (2004). Clinical Study on Preventing and Treating Left Ventricle Remodeling after Acute Myocardial Infarction with Integrative Chinese and Western Medicine Chin. J. Integr. Med. 10 (1), 25–28. doi:10.1007/BF02836553
Wang, Y.-P., Li, H.-Y., Su, C.-G., Ma, Q.-N., and Zang, Q. (2018). Study on the Protective Mechanism of Shensong Yangxin Capsule on Ventricular Remodeling after Myocardial Infarction. Hebei J. Traditional Chin. Med. 40 (12), 1788–1792. doi:10.3969/j.issn.1002-2619.2018.12.006
Wu, N. (2017). To Observe the Effect of Gualouxiebai Banxia Tang on Left Ventricular Function and Left Ventricular Remodeling in Myocardial Infarction Patients with Phlegm-Dampness Syndrome. Nanjing, China: Nanjing university of Chinese Medicine.
Xiang, Z.-X., Li, C.-G., Qiu, W.-F., Liu, J., Wang, A.-X., Liang, Z.-M., et al. (2019). Clinical Efficacy of Danlou Tablets in Improving Left Ventricular Adverse Remodeling after Myocardial Infarction: a Randomized Controlled Trial. Chin. J. Integr. Med. Cardio-Cerebrovascular Dis. 17 (24), 3864–3867. doi:10.12102/ji.ssn.1672-1349.2019.24.004
Xu, X.-J., Zhang, Y.-Y., Zhang, S.-J., Gong, J.-X., Lou, B., Ming-Lin, G., et al. (2019). Effect of Compound Danshen Dripping Pills Combined with Rosuvastatin on Left Ventricular Remodeling and Myocardial Fibrosis in Patients with Acute Myocardial Infarction after Percutaneous Coronary Intervention. China Med. Herald 16 (35), 61–64.77
Yan, X., Anzai, A., Katsumata, Y., Matsuhashi, T., Ito, K., Endo, J., et al. (2013). Temporal Dynamics of Cardiac Immune Cell Accumulation Following Acute Myocardial Infarction. J. Mol. Cell Cardiol. 62, 24–35. doi:10.1016/j.yjmcc.2013.04.023
Yang, G.-L., Yang, X.-Z., Liu, J.-H., Li, H.-Y., Liu, P., and Cao, X.-M. (2014). Ultrasonic Observation of Musk Heart-Protecting Pills on Left Ventricular Remodeling and Cardiac Function after Acute Myocardial Infarction. Henan Traditional Chin. Med. 34 (1), 58–59. doi:10.6367/j.issn.1003-5028.2014.01.080
Yang, Q., Lin, H., Lu, H.-T., Wu, G.-S., Guo, H.-Y., and Chi, J.-F. (2020). The Effect of Chinese Herbal Formula Gualou Xiebai Banxia Decoction on Ventricular Remodeling and Inflammatory Factors after Acute Myocardial Infarction. J. Electrocardiography Circ. 39 (02), 128–132. doi:10.2124/j.issn.2095-3933.2020.2.2020-3927
Yang, W., Xu, X., Wang, S., and Zhang, C. (2012). Effects of Tongxinluo Capsule on Serum Type III Procollagen Amino Terminus Peptide and Left Ventricular Remodeling in Patients with Acute Myocardial Infarction after Emergency PCI. Chin. J. Difficult Complicated Cases 11 (6), 452–453. doi:10.3969/j.issn.1671-6450.2012.06.021
Yokota, T., Osanai, T., Hanada, K., Kushibiki, M., Abe, N., Oikawa, K., et al. (2010). Effects of Telmisartan on Markers of Ventricular Remodeling in Patients with Acute Myocardial Infarction: Comparison with Enalapril. Heart Vessels 25 (6), 460–468. doi:10.1007/s00380-010-0013-4
Yokota, T., Tomita, H., Mori, Y., Kudo, T., Hiraga, H., Suto, N., et al. (2014). Imidapril and Enalapril Similarly Inhibit Plasma Matrix Metalloproteinase Activities and Attenuate Left Ventricular Remodeling in Patients with Acute Myocardial Infarction. J. Cardiovasc. Pharmacol. 63 (6), 528–532. doi:10.1097/fjc.0000000000000077
Zhang, J.-G., Gao, D.-S., Wei, G.-H., Shen, C.-Y., Wang, S.-C., Liu, Y.-J., et al. (2002a). Clinical Study on Effect of Astragalus Lnjection on Left Ventricular Remodeling and Left Ventricular Function in Patients with Acute Myocardial Infarction. Chin. J. Integr. Med. 22 (5), 346–348.
Zhang, J.-G., Gao, D.-S., Wei, G.-H., Wang, X.-Z., Shen, C.-Y., Liu, L.-X., et al. (2002b). Effect of Astragalus Injection on Left Ventricular Remodeling and Cardiac Function in Elderly Patients with Early Acute Myocardial Infarction. J. Jining Med. Coll. 25 (4), 23–25.
Zhang, L. (2006). Clinical Study on Left Ventricular Remodeling after AMI Treated with Yixintong. Shandong Med. J. 46 (34), 47–48.
Zhang, X.-X., Shao, C.-L., Cheng, S.-Y., Zhu, Y., Liang, B., and Gu, N. (2021). Effect of Guanxin V in Animal Model of Acute Myocardial Infarction. BMC Complement. Med. Ther. 21 (1), 72. doi:10.1186/s12906-021-03211-7
Zhang, X.-Z. (2008). Cilinical Study on Huixin Capsule Preventing LV Remodeling after Reperfusion in Acute Myocardial Infarction. Jinan: Shandong University of Chinese Medicine.
Zhao, J., Liu, N., Zuo, J.-L., Huang, X.-P., and Chen, J.-H. (2005). Clinical Study of Kaixin Capsule against Ventricular Remodeling after Myocardial Infarction. J. New Chin. Med. 37 (4), 31–32. doi:10.3969/j.issn.1671-6450.2012.06.021
Zhao, Q.-F. (2008). The Influence of Patient’s Heart Function after Acute Myocardial Infarction by Cuanxin V and the Experimental Study on Intervention of Ventricular Remodeling. Nanjing, China: Nanjing university of Chinese Medicine.
Chao, S.-W., Wang, L., Fan, J.-H., and Liu, H.-M., 2007. Recent clinical observation of tanshlnone II A on prevention of left ventricular remodeling in cases with acute myocardial infarction. Chin. J. Integrated Traditional West. Med. Intensive Crit. Care 14(3), 145-146. 10.1161/01.cir.81.4.1161
Keywords: traditional Chinese medicine, acute myocardial infarction, ventricular remodeling, meta-analysis, randomized controlled trial
Citation: Zhang X-X, Liang B, Shao C-L and Gu N (2021) Traditional Chinese Medicine Intervenes Ventricular Remodeling Following Acute Myocardial Infarction: Evidence From 40 Random Controlled Trials With 3,659 Subjects. Front. Pharmacol. 12:707394. doi: 10.3389/fphar.2021.707394
Received: 10 May 2021; Accepted: 26 July 2021;
Published: 31 August 2021.
Edited by:
Somasundaram Arumugam, National Institute of Pharmaceutical Education and Research, Kolkata, IndiaReviewed by:
Wawaimuli Arozal, University of Indonesia, IndonesiaCopyright © 2021 Zhang, Liang, Shao and Gu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ning Gu, Z3VuaW5nQG5qdWNtLmVkdS5jbg==
†These authors have contributed equally to this work
‡ORCID: Bo Liang, orcid.org/0000-0002-1749-6976; Ning Gu, orcid.org/0000-0003-0704-6768
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.