- 1Graduate School, Beijing University of Chinese Medicine, Beijing, China
- 2National Clinical Research Center for Chinese Medicine Cardiology, Xiyuan Hospital, China Academy of Chinese Medical Sciences, Beijing, China
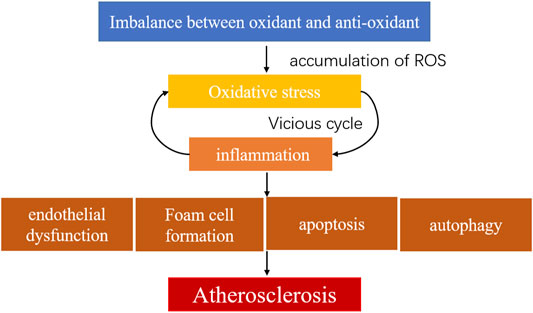
Atherosclerosis is a complex chronic disease that occurs in the arterial wall. Oxidative stress plays a crucial role in the occurrence and progression of atherosclerotic plaques. The dominance of oxidative stress over antioxidative capacity generates excess reactive oxygen species, leading to dysfunctions of the endothelium and accelerating atherosclerotic plaque progression. Studies showed that Chinese herbal medicines and traditional Chinese medicine (TCM) might regulate oxidative stress; they have already been used to treat diseases related to atherosclerosis, including stroke and myocardial infarction. This review will summarize the mechanisms of oxidative stress in atherosclerosis and discuss studies of Chinese herbal medicines and TCM preparations treating atherosclerosis, aiming to increase understanding of TCM and stimulate research for new drugs to treat diseases associated with oxidative stress.
Introduction
Atherosclerosis is one of the primary causes of death and is becoming one of the greatest threats to human health. Lancet Global Health reported that the number of patients with carotid plaques and stenosis worldwide increased significantly from 2000 to 2020 (Song et al., 2020). Atherosclerotic plaques cause vessel stenosis, which hinders the normal blood flow and leads to ischemia changes in tissues and organs (Willeit et al., 2003). Depending on the location of the atherosclerotic plaque, it may cause coronary artery disease, cerebrovascular disease (stroke), or peripheral arterial disease. Several factors induce atherosclerosis (Libby et al., 2019), including hypertension, hyperlipidemia, diabetes, long-term smoking, obesity; there are also non-disease factors such as gender and age (Gress et al., 2000; McClelland et al., 2006; Tyrrell and Goldstein, 2021). The pathogenesis of atherosclerosis is hypothesized to include inflammation, lipid infiltration, oxidative stress, platelet hyperfunction, immune dysfunction, and shear stress (Mury et al., 2018). Oxidative stress and inflammation are two primary factors in the progression of atherosclerosis (Hulsmans and Holvoet, 2010). When the antioxidant activity is insufficient to reduce reactive oxygen species (ROS), excess of the latter jeopardizes arterial endothelial function and threatens plaque stability (Davignon and Ganz, 2004; Laufs et al., 2005).
In this review, we collected the relevant clinical and experimental studies and reviews by searching papers published from January 2000 to February 2021 in Pubmed, Web of science, the China National Knowledge Internet (CNKI), and the China academic database, Wanfang, using “atherosclerosis”, “oxidative stress”, “TCM” or “TCM formula” or “TCM preparation” or “Chinese herbal medicine” or “herbal active compounds” or “herbal active ingredients” or “herbal monomer” as the term. We will first review the mechanism of atherosclerotic plaque formation and progression. Then we discuss oxidative stress in the development of atherosclerotic plaques. Finally, we summarize experimental and clinical research on Chinese herbal medicines, active metabolites, and TCM prescriptions to treat atherosclerosis. The purpose of our review is to summarize the efficacy and mechanism of the Chinese herbal medicines in treating atherosclerosis from the perspective of antioxidants and provide evidence and deeper insights for future drug exploration and application in this area.
Formation and Progression of Atherosclerosis
The structure of typical arterial walls includes vascular intima, media, and adventitia. Typical atherosclerotic are characterized by intimal thickening, excessive deposition of lipid, and infiltration of monocytes and lymphocytes. Endothelial injury dysfunction initiates atherosclerosis. Endothelial cells attach to the inner sides of arterial walls, where they help mediate immune functions by expressing adhesion molecules during inflammation that mediate the removal of swallowing foreign bodies (Libby et al., 2011). NO, prostacyclin, and bradykinin are generated by endothelial cells (Davignon and Ganz, 2004); these factors dilate blood vessels and prevent white blood cell adhesion and platelet aggregation. Endothelial cells also produce endothelin and angiotensin II that regulate vasoconstriction, promoting the proliferation of smooth muscle cells and affecting plaque progression.
Hypertension (Li et al., 2020a), hyperlipidemia (Drechsler et al., 2010), chronic smoking (Naya et al., 2011), and changes in shear stress (Chatzizisis et al., 2007) are risk factors for atherosclerosis; all result in inflammation and endothelial cell dysfunction, causing changes in permeability and expression of adhesion molecules such as vascular cell adhesion molecule-1 (VCAM-1) and E-selectin (Tabas et al., 2015). Adhesion molecules recruit inflammatory monocytes to adhere to endothelial cells and infiltrate the arterial intima (Tabas et al., 2007). Low-density lipoprotein (LDL) is transported to the arterial wall by recognizing guanine nucleotide exchange factor 4 (DOCK4) and scavenger receptor type B (SR-B1) in endothelial cells and modified to oxidized LDL (ox-LDL) (Huang et al., 2019). Leukocytes transform into macrophages and express SRs such as SR-A1, lipoxygenase 1 (Lox1), and CD36, recognizing the oxidized epitope of ox-LDL and internalizing ox-LDL to form foam cells (Canton et al., 2013; Chistiakov et al., 2017). Macrophages are the primary inflammatory cells in atherosclerotic plaques and are significant in plaque formation; they modulate plaque stability by polarizing into M1 and M2 macrophages (Canton et al., 2013).
M1 macrophages secrete pro-inflammatory factors TNF-α, IL-6, IL-1β, inducible nitric oxide synthesis (iNOS), and other effectors that promote early plaque formation, thinning fibrous caps, and enhancing immune response (Moore and Tabas, 2011; Barrett et al., 2019; Liao et al., 2020). Reverse cholesterol transport (RCT) is an important mechanism that maintains balanced lipid metabolism. High-density lipoprotein (HDL) transports cholesterol from extrahepatic tissue such as foam cells and atherosclerotic plaques to the liver for catabolism (Yu et al., 2019). HDL participates in RCT and exerts antioxidant and anti-inflammatory functions. In atherosclerosis, the structure and composition of HDL changes, hindering RCT and accelerating plaque progression (Ouimet et al., 2019). LXRα (liver X receptorα)/ABCA1 (ATP binding cassette subfamily A member 1) is a critical signal in RCT. Changes in this pathway promote the entry and retention of cholesterol-containing LDL particles in the arterial wall, causing early atherosclerosis lesions characterized by accumulation of macrophages, foam cells, and lipid droplets.
In atherogenesis, smooth muscle cells (SMCs) migrate to the inner membranes of the arterial walls and secrete extracellular matrix (ECM) components such as collagen and proteoglycan. Proteoglycan regulates ECM remodeling and cytokine function, interacting with apolipoprotein B, and retaining LDL under the endothelium (Stephens et al., 2011), forming a fibrous cap with proliferated SMCs covering the plaques. The fibrous cap covers macrophage derived foam cells. As the disease continues, these foam cells undergo apoptosis, causing the accumulation of extracellular lipids to form lipid-rich plaque cores, enlarged lipid or necrotic cores, that protrude into the artery. In advanced stages of atherosclerosis, the apoptosis of SMCs and the decomposition of collagen and elastin (exacerbated by the inflammatory process (Karunakaran et al., 2021)) cause rupture of the fibrous cap around the lipid core and incite coagulation factors to interact with tissue factors, leading to thrombus formation and associated complications (Figure 1).
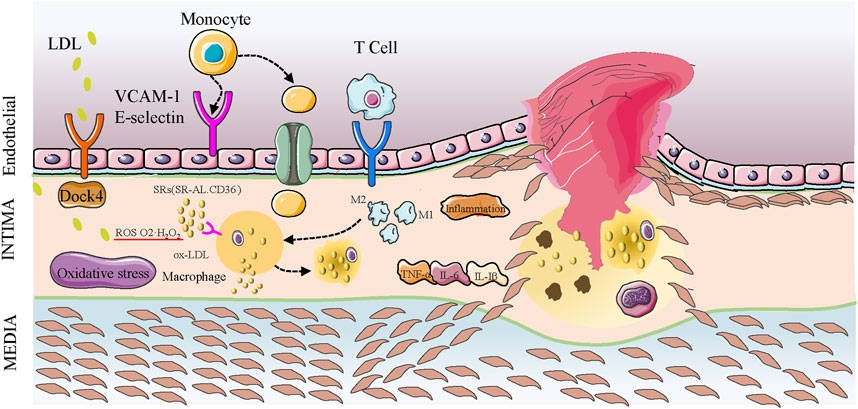
FIGURE 1. Development of atherosclerotic plaques. LDL enters the arterial intima via endothelial cells expressing SR-B1 receptors in combination with DOCK4 action. LDL particles are oxidized to ox-LDL, and the monocytes entering the intima are transformed into macrophages that phagocytize ox-LDL mediated by surface SR (SR-A1, CD36). They also phagocytize other cholesterols in the intima to form foam cells. Macrophages are polarized into M1 and M2 forms. M1 macrophages release pro-inflammatory factors such as IL-6 to promote plaque progression, and oxidative stress promotes inflammatory factors. SMCs enter the intima to form fibrous caps, and oxidative stress and inflammation promote apoptosis and cell death in the plaque, leading to the accumulation of lipid and lipid cores. The continuous inflammation and oxidative stress causes the lipid nuclei to enlarge, the fibrous cap dilutes and ruptures, and platelets accumulate to form thrombi.
Oxidative Stress and Atherosclerosis
Oxidative stress refers to the increased production of ROS in tissues or cells that weaken scavenging ability. Oxidative stress and inflammation are two major mechanisms of atherosclerosis. They interact with one another and form a vicious cycle in plaque progression. ROS include superoxide (compounds containing superoxide ion), hydrogen peroxide (H2O2), hydroxyl radicals, and nitric oxide radicals. These ROS participate in cell growth, proliferation, apoptosis, endothelial activation, mitochondrial damage, adhesion, and vascular inflammation process in atherosclerosis (Li and Shah, 2004; Madamanchi et al., 2005; Zhang et al., 2020a) (Figure 2). Major sources of ROS include nicotinamide adenine dinucleotide phosphate oxidase (NADPH oxidase or Nox), mitochondrial enzymes, Lox, uncoupled endothelial nitric oxide synthase (eNOS or NOS3), myeloperoxidases (MPO), cyclooxygenase (COX), mitochondria, and xanthine oxidase (XO). NADPH oxidase is the primary enzyme of ROS generation and has seven isoforms, namely Nox1-Nox5, Duox1, and Duox2, found in endothelial cells, vascular SMCs, fibroblasts, or perivascular adipocytes (Konior et al., 2014). Malondialdehyde (MDA), a lipid oxidation product, modifies LDL particles, leading to vascular endothelial cell structure changes and jeopardizing endothelial function. Superoxide dismutase (SOD), glutathione (GSH), catalase (CAT), paraoxonase (PON), and nitric oxide (NO) are antioxidants that degrade excessive ROS to maintain internal homeostasis. The dominance of oxidation over antioxidant capabilities leads to excess accumulation of oxygen free radicals and metabolites (Cadenas, 2018). This disequilibrium leads to oxidative stress in atherosclerotic diseases (Griendling and FitzGerald, 2003a; Griendling and FitzGerald, 2003b; Sies, 2015). ROS produced by macrophages and SMCs may participate in inflammation, endothelial dysfunction, apoptosis, autophagy, and increased plaque vulnerability (Channon, 2002; Lin et al., 2012). Over-activation of Nox increases superoxide formation and ROS generation, impairing the NO production in the arterial wall and causing vascular endothelial dysfunction. For example, eNOS is associated with arterial endothelial function. Tetrahydrobiopterin (BH4) and L-arginine are cofactors for eNOS production. Insufficient synthesis of either of these two factors cause eNOS reduction or uncoupling, impairs NO production, and accelerates superoxide accumulation, causing endothelial dysfunction and hastening atherosclerosis (Antoniades et al., 2006; Antoniades et al., 2007; Daiber and Chlopicki, 2020). However, the evidence also suggests that the endothelial isoform Nox4 produces protective H2O2, maintains endothelial function, reduces macrophage adhesion to endothelial surfaces, and provide anti-atherosclerotic functions (Schürmann et al., 2015; Langbein et al., 2016). XO produces ROS through molecular oxygen as an electron acceptor (Förstermann et al., 2017). After ROS accumulation in the arterial walls, the inhibition of xanthine dehydrogenase (XDH) and the activation of XO activity causes active oxygen production, creating a vicious cycle (McNally et al., 2003). XO also stimulates macrophages and vascular smooth muscle cells (VSMCs) to generate Lox-1 and increase ROS accumulation. Lox-1, a specific receptor for ox-LDL, activates ROS generation and NF-κB (Murdocca et al., 2021), impairing eNOS expression and causing endothelial dysfunction. ROS converts XDH into XO, causing mitochondrial damage (Zhang et al., 2020b). MPO is an oxidant highly expressed in neutrophils that produces hypochlorous acid (HOCI) from H2O2 and becomes a significant ROS generator in inflammatory response. In atherosclerosis-related diseases, MPO oxidizes apolipoprotein A1 (ApoA1) in high-density lipoprotein (HDL) (Huang et al., 2013) and impairs cholesterol acceptor function (Huang et al., 2014). Overproduction of HOCI, which MPO generates, can directly jeopardize macrophages, causing cell death and increasing plaque inflammation by recruiting neutrophils and accelerating plaque progression (Hickey, 2011; Duivenvoorden et al., 2013; Guo et al., 2020). The adhesion molecules expressed on endothelium recruit monocytes, and inflammatory cells stimulate monocytes to infiltrate into the intima, which mutually affects endothelial function. Oxidative stress occurring in plaques activates inflammatory pathways, such as NF-κB, and enhances adhesion molecule production, promoting plaque progression and thrombus formation via platelet activation (Liu et al., 2021). It also participates in macrophage polarization and increases M1 production, activating inflammation and reducing stability of vulnerable plaques (Yang et al., 2020a). ROS induces SRs in SMCs, leading to transformation into foam cells and promoting the release of matrix metalloproteinases, causing dilution of fibrous caps and plaque disruption (Kattoor et al., 2017).
Many studies examined ROS-stimulating arterial walls producing cytokines to activate signal pathways. The mechanism and critical targets of oxidative stress in the occurrence and development of atherosclerosis have also been further explored. Nrf2 eliminates ROS production, increasing the expression of antioxidant enzyme genes and maintaining oxidation/antioxidant balance in atherosclerosis (Zhu et al., 2019a). Sirtuin (Sirt) family proteins, the silent information regulators of deacetylase activity, are also crucial in the process of oxidative stress in atherosclerosis. Overexpression of Sirt1 up-regulates antioxidant-related expression, promotes the generation of transcription factor forkhead protein O subfamily 3a (FOXO3a)/PGC-1α complex, and up-regulates SOD secretion, exerting an antioxidant role against the progression of atherosclerosis (Olmos et al., 2013). Uncoupling proteins (UCPs), members of the mitochondrial transporter proteins family, act as proton transporters on the inner mitochondrial membrane related to ROS production, endothelial dysfunction, cell apoptosis, and proliferation; these also become target genes in atherosclerosis (Kim et al., 2007). An in-depth study of the specific mechanisms of oxidative stress in atherosclerosis would help identify new medications to treat atherosclerosis.
TCM for Treatment of Atherosclerosis, Targeting Oxidative Stress
Chinese Herbal Medicines and Active Metabolites of Herbs
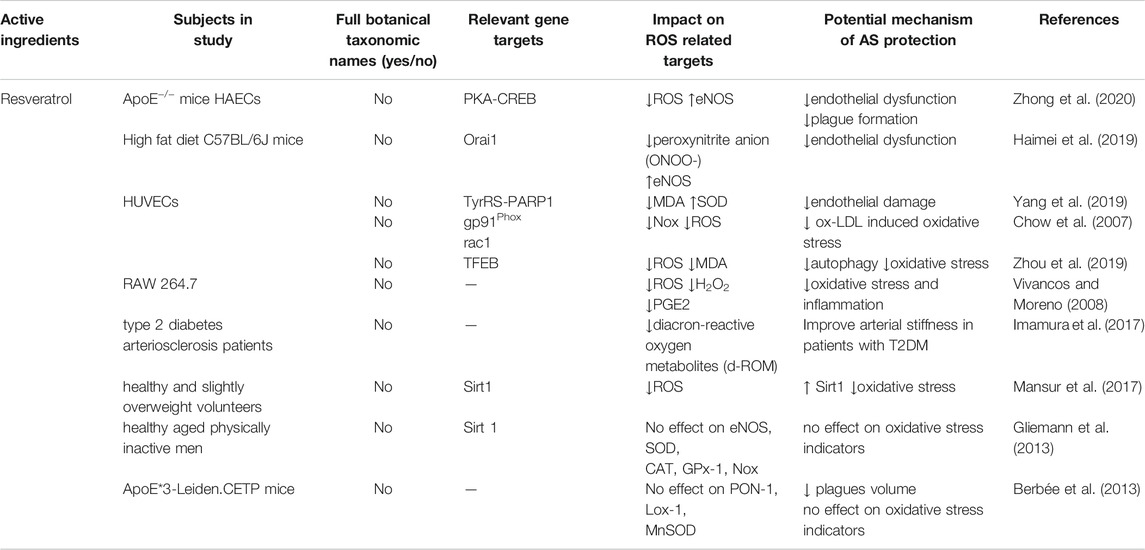
Resveratrol
Resveratrol is a natural phenolic compound found in varieties of plants, such as grapes and peanut, as well as Chinese herbal medicine, including Reynoutria japonica Houtt [Polygonaceae; Polygoni cuspidati rhizoma et radix] and Veratrum nigrum L. [Melanthiaceae]. Studies revealed that resveratrol mediates anti-atherosclerosis and heart protection. It protects endothelial cells from lipid damage, promotes vasodilation by regulating nitric oxide synthesis, and scavenges oxygen radicals and superoxide radicals by limiting lipid peroxidation, inhibiting platelet aggregation, and SMCs proliferation (Mohar and Malik, 2012; Bonnefont-Rousselot, 2016; Wiciński et al., 2018). Resveratrol reduces MDA, COX-1, and Nox production and activates SOD and GSH to balance the oxidation and antioxidant capacities, leading to eNOS generation to reduce endothelial dysfunction and pathological atherosclerotic changes (Szewczuk et al., 2004; Chow et al., 2007; Vivancos and Moreno, 2008; Bruedigam et al., 2011; Li et al., 2018a; Haimei et al., 2019; Li et al., 2019c; Yang et al., 2019). Transcription factor EB (TFEB) regulates homeostasis and maintains oxidant/antioxidant balance. Resveratrol promotes the translocation of TFEB from the cytoplasm to the nucleus in human umbilical vein endothelial cells (HUVECs) to activate TFEB and exert antioxidant effects, reducing autophagy and relieving endothelial dysfunction (Zhou et al., 2019). Similar results were found in clinical trials showing a beneficial effect of resveratrol in atherosclerosis by reducing oxidative stress (Imamura et al., 2017; Mansur et al., 2017). However, Gliemann et al. revealed that, instead of heart protection, supplementation of resveratrol did not affect Sirt 1, eNOS, or SOD expression and may impair the beneficial effects of physical exercise on cardiovascular health in older men (Gliemann et al., 2013). While affirming the effect of resveratrol on atherosclerosis, some researchers raised doubts. Berbée et al. compared resveratrol with statins in the treatment of ApoE*3-Leden CETP atherosclerotic mice, and showed that resveratrol alone reduced plaque volume (similar to use atorvastatin alone), but did not affect oxidative stress-related indicators PON1, COX-1, COX2, Lox-1, and MnSOD (Berbée et al., 2013). These findings suggest that more evidence is needed to confirm resveratrol’s antioxidant effects on atherosclerosis (Table 1).
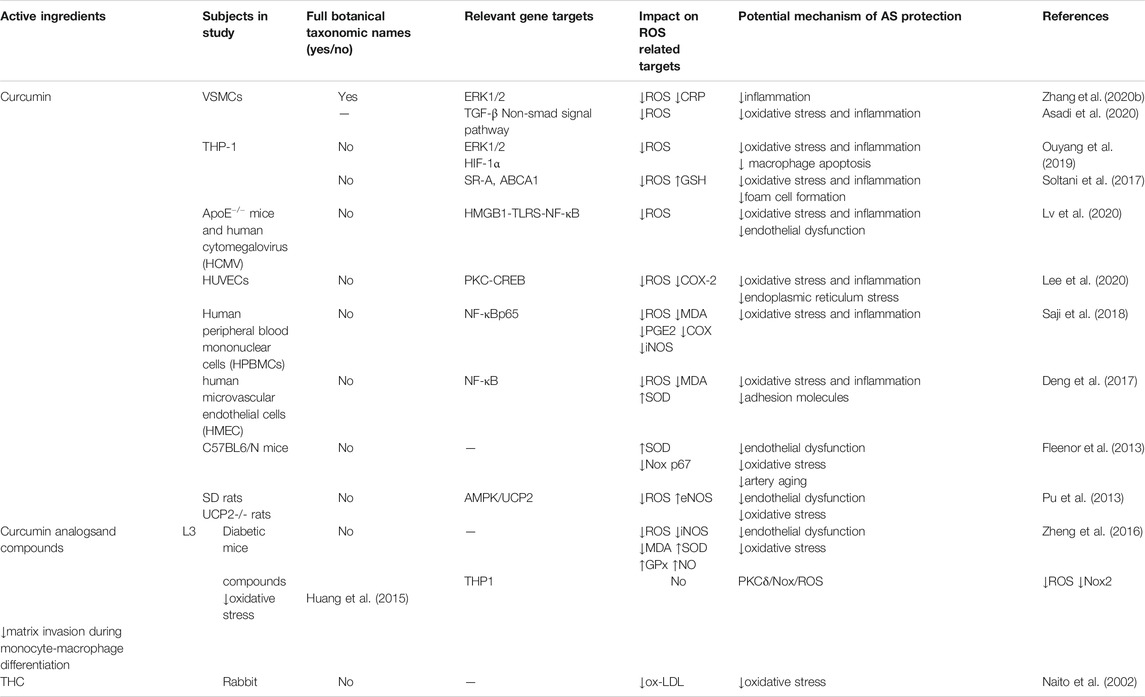
Curcumin and Its Analogues
Curcumin is the active ingredient of Curcuma longa L. [Zingiberaceae; Curcumae radix; Curcumae longae rhizoma]. It is a polyphenol demonstrated to act as a free radical scavenger and antioxidant that benefits in treating cardiovascular diseases (Zingg et al., 2013; Panahi et al., 2018; Li et al., 2019b; Li et al. 2020b). Curcumin inhibits ROS generation, limits lipid peroxidation (Panahi et al., 2018), and enhances NO bioavailability (Goel et al., 2008; Li et al., 2019a). Studies demonstrated that curcumin suppresses ROS production in both animal models and in vitro by inhibiting ROS-related inflammation pathways and cytokines (Zingg et al., 2013), such as ERK1/2 pathway (Ouyang et al., 2019; Zhang et al., 2020a), the high-mobility-group protein B1(HMGB1)- toll-like receptor (TLRS)-NF-κB pathway (Lv et al., 2020), COX-2 (Lee et al., 2020), and others (Shi et al., 2017; Saji et al., 2018; Asadi et al., 2020), preventing endothelial dysfunction and adhesion molecules secretion. Pu et al. found that curcumin alleviated ROS-induced endothelial dysfunction through UCP2 and increased eNOS activity (Pu et al., 2013; Treviño-Saldaña and García-Rivas, 2017). Arterial dysfunction and oxidative stress caused by vascular aging are vital factors in the development of atherosclerosis. Laboratory studies revealed some mechanisms of curcumin’s effect on aging arteries. Fleenor et al. (Fleenor et al., 2013) explored the effect of curcumin on carotid artery function and vascular oxidative stress in aged mice. They discovered that curcumin increased eNOS in the aged carotid artery, reversed endothelial-dependent dilation, reduced superoxide, and inhibited NADPH oxidase p67 subunit activity. After up-regulating ABCA1 expression and inhibiting SR-A and CD36 in macrophages, curcumin reduced ROS production and foam cell formation to stabilize vulnerable plaques (Soltani et al., 2017). Curcumin analogs, such as L3, tetrahydrocurcumin (THC), Cur-NPs(Meng et al., 2019), HASF (a dual ROS-sensitive and CD44 receptor targeting amphiphilic carrier) (Hou et al., 2020), and curcumin compounds, are synthetic compounds that have similar effects; for example, they elevate glutathione peroxidase (GPx) catalyze GSH, and have higher bioavailability than common curcumin, showing anti-oxidative stress in atherosclerosis through multiple gene targets (Naito et al., 2002; Huang et al., 2015; Zheng et al., 2016). In summary, the antioxidant effects of curcumin combat atherosclerosis by the following mechanisms: 1) Blocking enzymes that promote ROS generation; 2) increasing antioxidant enzyme activity; 3) reducing damage to endothelial cells by anti-inflammatory actions, enhancing eNOS, and reducing adhesion factors; and 4) reducing foam cell formation (more details in Table 2).
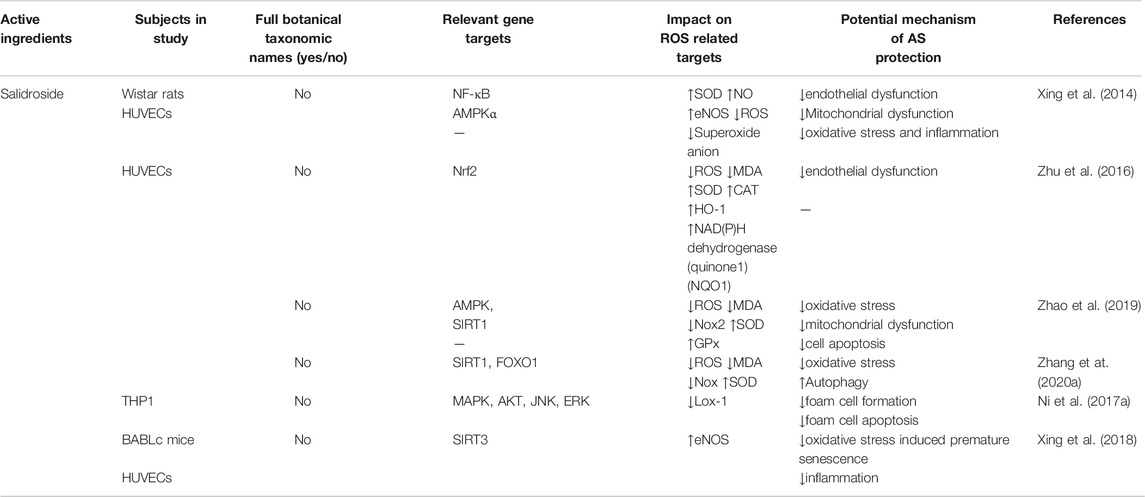
Salidroside
Salidroside is an active ingredient that exists in Chinese herbal medicine Hongjingtian (Rhodiola crenulata (Hook.f. & Thomson) H.Ohba [Crassulaceae; Rhodiolae crenulatae radix et rhizoma]); this agent reduces oxidative stress (Mao et al., 2010; Li et al., 2011a)and is used to treat atherosclerosis. In terms of relieving endothelial dysfunction after impaired ROS production, salidroside enhances eNOS production and activates several pathways, including Sirt1/Foxo1, AMPK, and Sirt3, regulating oxidative stress, inflammation, cell apoptosis, autophagy, and mitochondrial function (Xing et al., 2014; Xing et al., 2018; Zhao et al., 2019; Zhu et al., 2019b). Hemoxygenase 1(HO-1) is an important antioxidant enzyme in cell microsomes that mediates anti-inflammation and anti-oxidation and suppresses the activity of adhesion molecules (Zhang et al., 2018). Zhu et al. (Zhu et al., 2016) found that salidroside promotes the expression of HO-1 and NAD(P)H dehydrogenase-quinone oxidoreductase 1(NQO1), lowers MDA and ROS production by regulating Nrf2, and subsequently alleviates enthothelial dysfunction. Ni et al. believed that salidroside impaired the combination of ox-LDL with Lox-1 and affected foam cell formation and apoptosis in atherosclerosis by regulating Lox-1 content; during this process, there were no changes in HO-1 expression (Ni et al., 2017a). Although the anti-oxidation effect of salidroside has been determined, its specific mechanism still needs to be further explored (Table 3).
Active Ingredients of Danshen
The traditional Chinese herbal medicine Danshen (Salvia miltiorrhiza Bunge [Lamiaceae; Salviae miltiorrhizae radix et rhizoma]) has been widely applied in the treatment of atherosclerotic diseases in Asia with encouraging results (Li et al., 2018b; Ren et al., 2019). The chemical components in Salvia are divided into fat-soluble and water-soluble components. Salvianolic acids (A-G) are water-soluble components. Tanshinone I, tanshinone IIA, tanshinone IIB, methyl tanshinate, and danshendiol are fat-soluble components. Investigators discovered that salvianolic acids have a good therapeutic effect on atherosclerosis (Xiang et al., 2018; Ma et al., 2020; Yang et al., 2020b). In a diabetic rat model, salvianolic acid B (Ren et al., 2016) decreased Nox2 and Nox4 expression, limiting ROS that caused endothelial dysfunction. The vasoprotective factors eNOS and NO also improved in this process, preventing the occurrence of atherosclerosis. Tanshinone IIA is one of the pharmacologically active ingredients derived from Danshen that participates in maintaining vascular homeostasis; it is widely used to prevent and treat coronary heart disease (CHD) in Asia (Gao et al., 2012; Feng et al., 2021). Tanshinone IIA competes with LDL oxidation induced by diverse oxidizing systems, like copper-, peroxyl radical-, and peroxynitrite, scavenging peroxyl radicals and preventing atherosclerosis (Niu et al., 2000). In animal experiments (the ApoE−/− model and high fatty diet rabbit), tanshinone IIA exerted antioxidant and anti-inflammatory effects by reducing ox-LDL, ROS, MDA, and other pro-oxidative stress products to reduce lipid peroxidation and inhibit atherosclerosis progression via multiple targets (ERK, NF-κB, PPARγ, and miR) (Fang et al., 2008; Tang et al., 2011; Chen et al., 2012; Liu et al., 2015; Xuan et al., 2017). In vitro experiments showed that tanshinone IIA reduced the damage caused by H2O2, increased the production of antioxidant enzymes, and prevented endothelial cell injury from oxidative stress (Lin et al., 2006; Zhu et al., 2017a). Adjusting antioxidant enzyme GPx generation may be a critical step in reducing ROS-related functions like apoptosis, endothelial injury, and inflammation (Li et al., 2008; Fang et al., 2008; Zhu et al., 2017a). Tanshinone IIA also alleviates ROS-induced subsequent autophagy and apoptosis (Ni et al., 2017b; Chen et al., 2012; Huimin et al., 2017; Li et al., 2008), presenting potential anti-atherosclerosis effects (Table 4).
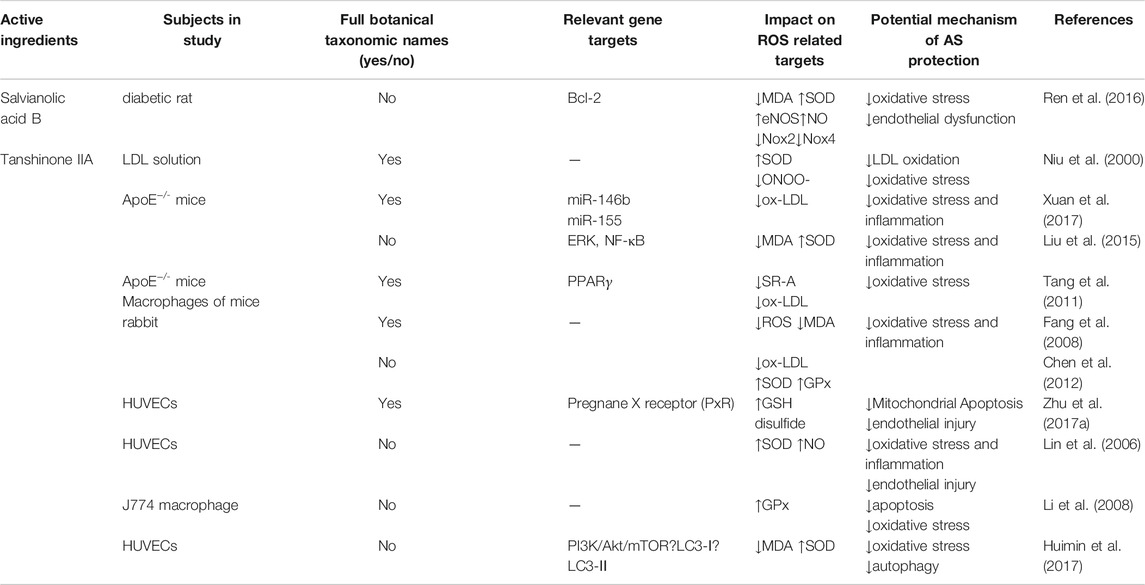
TABLE 4. Active ingredients in Danshen for treatment of atherosclerosis by regulating oxidative stress.
Berberine
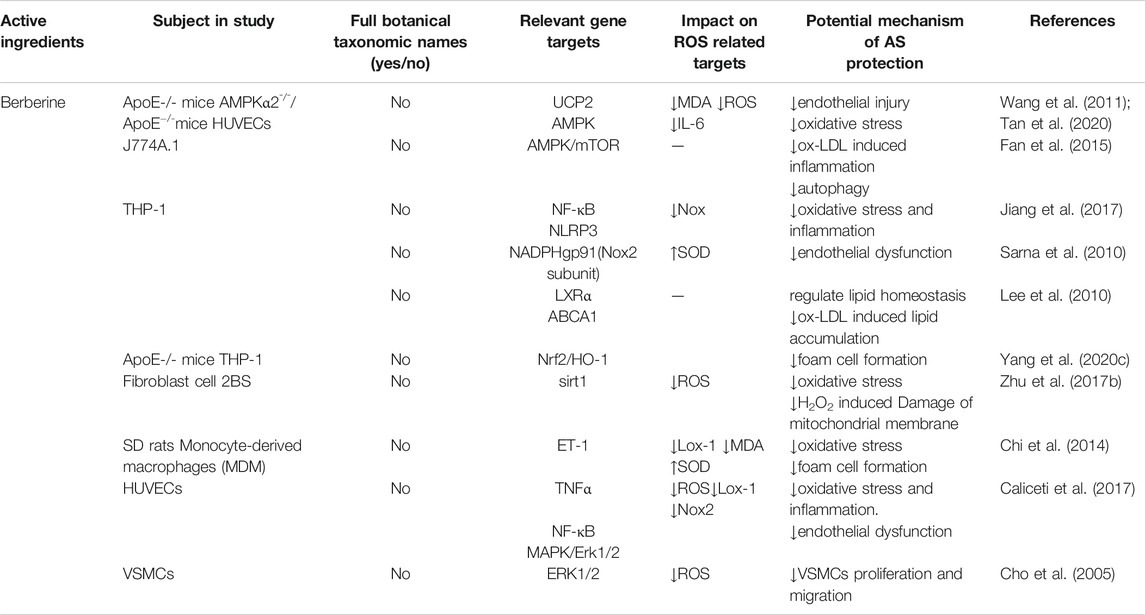
Berberine is an active ingredient derived from the Chinese herbal medicine Coptis chinensis Franch. [Ranunculaceae; Coptidis rhizoma] that helps to treat atherosclerosis-related cardiovascular diseases (Mulvihill and Huff, 2010; Wu et al., 2010). It inhibits endothelial cell dysfunction via multiple mechanisms (Fatahian et al., 2020). By regulating UCP2 and Nox2, berberine blocks MDA and enhances SOD production, inhibiting the AMPK pathway to relieve inflammation and autophagy; it also protects against endothelial cell dysfunction in atherosclerosis (Sarna et al., 2010; Wang et al., 2011; Fan et al., 2015; Caliceti et al., 2017; Tan et al., 2020). Accumulation of foam cells and apoptosis leads to increased lipid core volume and thinning of the fibrous caps, resulting in rupture of vulnerable plaques. Studies showed that berberine maintained lipid homeostasis and reduced foam cells formation via LXRα/ABCA1 and Nrf/HO-1, limiting macrophage ox-LDL uptake and cholesterol efflux and inhibiting macrophages superoxide anion production (Lee et al., 2010; Yang et al., 2020c). Berberine also decreased endothelin-1 (ET-1) induced Lox-1 expression in monocyte-derived macrophages, acting as an antioxidant and reducing foam cell formation (Chi et al., 2014; Caliceti et al., 2017). Zhu X et al. (Zhu et al., 2017b) established a premature aging model using low-concentration berberine to interfere with hydrogen peroxide; they found that berberine combated premature aging in human diploid fibroblasts via Sirt1-mediated ROS reduction, protecting loss of mitochondrial membrane potential and showing an antioxidant effect. Berberine may inhibit cell senescence caused by reducing oxidative stress associated with age-related diseases. Berberine also inhibited the proliferation and migration of VSMCs by suppressing Nox activity (Cho et al., 2005) and suppressed ROS-dependent NLRP3 inflammasomes in human peripheral blood mononuclear cells (PBMCs) (Jiang et al., 2017), providing research targets for berberine in treating atherosclerosis. (Table 5).
Quercetin
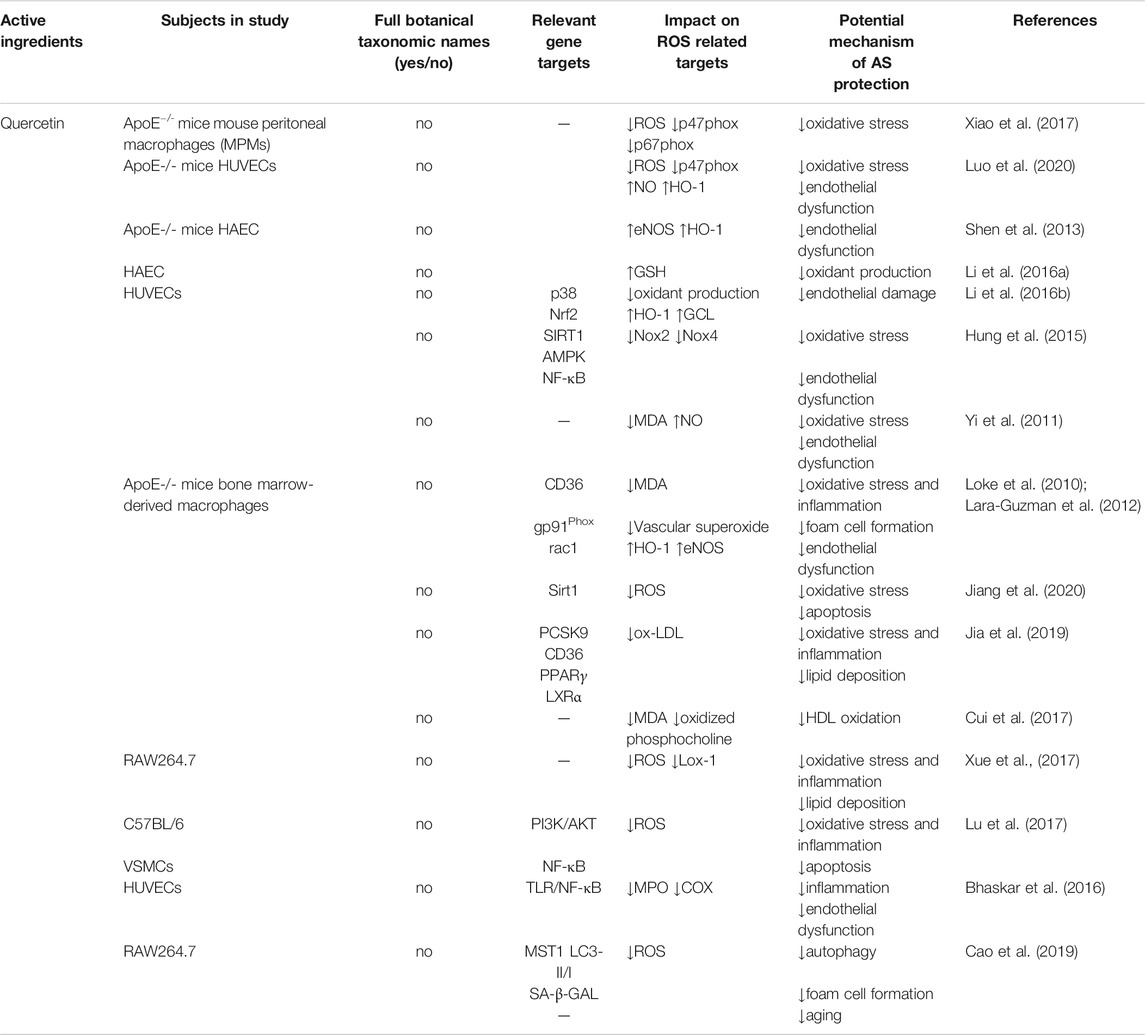
Quercetin is widely distributed in the plant kingdom. Chinese herbal medicines such as Styphnolobium japonicum (L.) Schott [Fabaceae; Sophorae flos], Platycladus orientalis (L.) Franco [Cupressaceae; Platycladi cacumen], Alpinia officinarum Hance [Zingiberaceae; Alpiniae officinarum rhizoma], Tussilago farfara L. [Asteraceae; Farfarae flos], Morus alba L. [Moraceae; Mori folium; Mori cortex], and Ginkgo biloba L. [Ginkgoaceae; Ginkgo folium; Ginkgo semen] (Zhanxia et al., 2019) are major sources of quercetin. Quercetin is also found in fruits, nuts, and vegetables (Stromsnes et al., 2020). Studies showed that quercetin has potential to treat atherosclerosis by reducing inflammation and resisting oxidative stress (Deng et al., 2020). The antioxidant effects of quercetin occur first by inhibition of p47phox and p67phox activity, reducing NADPH oxidase activation to decrease ROS production (Xiao et al., 2017). Sirt1 and AMPK may be potential key targets for reducing Nox2 and Nox4 expression (Hung et al., 2015) and regulating ROS, superoxide (Loke et al., 2010), and MDA production (Yi et al., 2011; Lara-Guzman et al., 2012). Quercetin also increases generation of antioxidants such as HO-1 (Shen et al. 2013; Luo et al., 2020), NAD(P)H dehydrogenase, and glutamate-cysteine ligase (GCL) by activating Nrf2 (Li et al., 2016b). Li et al. (Li et al., 2016a) studied the mechanism of quercetin restoring the expression of GSH in human aortic endothelial cells (HAEC) that was relevant to GCL. In this manner, quercetin inhibited oxidative stress. After balancing oxidation and anti-oxidation, NO and eNOS bioavailability improved, reducing inflammation (Lara-Guzman et al., 2012; Bhaskar et al., 2016; Lu et al., 2017; Xue et al., 2017; Jia et al., 2019), autophagy (Cao et al., 2019), and apoptosis (Lu et al., 2017; Jiang et al., 2020), and inhibiting the recruitment of monocytes by adhesion factors, thereby protecting endothelial cell function. By elevating HDL cholesterol absorption capacity, quercetin increased HDL anti-oxidation and reduced lipid accumulation (Lara-Guzman et al., 2012; Cui et al., 2017; Xue et al., 2017; Jia et al., 2019) (Table 6).
Other Active Ingredients of Herbs
The Chinese herbal medicine Sanqi (Panax notoginseng (Burkill) F.H.Chen [Araliaceae; Notoginseng radix et rhizoma]) is a traditional medicine widely used to treat CHD in China. It was shown to have good efficacy and safety in clinical practice (Sun et al., 2016; Duan et al., 2017). Panax notoginseng saponins, including ginsenoside Rb1, ginsenoside Rg1, and notoginsenoside R1, are the active ingredients extracted from Sanqi; they reduce ROS generation by inhibiting NOX4 activity and block recruitment of adhesion molecules to monocytes induced by multiple pathways (Dou et al., 2012; Qiao et al., 2015; Fan et al., 2016), protecting endothelial function and preventing atherosclerosis. Ginsenoside, derived from the Chinese herbal medicine Panax ginseng C.A.Mey. [Araliaceae; Ginseng radix et rhizoma], includes ginsenosides Rg1 and Rb1 (also abstracted from Sanqi), Rb2, Rb3, Rg2, Rg3, Rf, F1, F2, Rd, and Rh2 (Jin et al., 2019). Lü et al. (Lü et al., 2019) found that Rb1 competitively inhibited the expression of the estrogen receptor ER-β, reducing ROS generation in endothelial cells and increasing eNOS and SOD, thereby reducing endothelial dysfunction. Coupled with ROS reduction, the inflammatory response was also suppressed to alleviate atherosclerosis (Fan et al., 2016; Zhou et al., 2017). Similar results were also found in ginsenoside F1, which reduced LDL-induced endothelial dysfunction; it may be considered a new medication to treat atherosclerosis (Li et al., 2011b; Qin et al., 2017). Ginko biloba L. [Ginkgoaceae; Ginkgo folium; Ginkgo semen]is a dioecious tree species native to China. Flavonoids and terpenoids are the primary active compounds in Ginkgo biloba leaves. They have various pharmacological effects, including anti-oxidation, anti-platelet, and anti-apoptosis, preventing and treating cardiovascular and cerebrovascular diseases, Alzheimer’s disease, and atherosclerosis (Li et al., 2020c; Tian et al., 2017). Ginkgo biloba extract (GBE) is used in modern medicine. The standard GBE- EGB761 synthesized by Willmar Schwabe Pharmaceuticals includes terpenoids, flavonoids, alkylphenols, polypentanol, and organic acids (van Beek and Montoro, 2009). To reduce ROS, GBE inhibits NADPH oxidase subunits p47 (Phox) and rac-1; it also reduces gp91 and p22 (Phox) expression caused by ox-LDL induced AMPK and PKC activation (Ou et al., 2013). GBE also enhances HO-1 expression through the Akt/eNOS and p38/MAPK pathways (Tsai et al., 2013). It reduces the adhesion molecules such as monocyte chemokine-1 (MCP-1) and VCAM-1 mediated by ROS and prevents the adhesion of monocytes to endothelial cells, protecting endothelial cells’ function (Chen et al., 2003; Ou et al., 2009; Piazza et al., 2019). In terms of inhibiting the formation of foam cells, Li et al. (Tonghua, 2019) found that EGb761 inhibited the uptake of cholesterol by VSMC smooth muscle cells and enhanced the efflux of cholesterol by smooth muscle cells. EGb761 treatment inhibited the expression of SR-A1 and LOX-1, thereby inhibiting the uptake of ox-LDL by smooth muscle cells. Ginkgolide B, another active component abstracted from Ginkgo biloba leaves, presented similar mechanisms to EGB761 (Li et al., 2009; Ma et al., 2013; Feng et al., 2018; Wang et al., 2019). The antioxidant effect of GBE on atherosclerosis is mediated by reducing ROS generation, thereby preventing endothelial dysfunction caused by the adhesion of monocytes and endothelial cells (Jung et al., 2012) (Table 7).
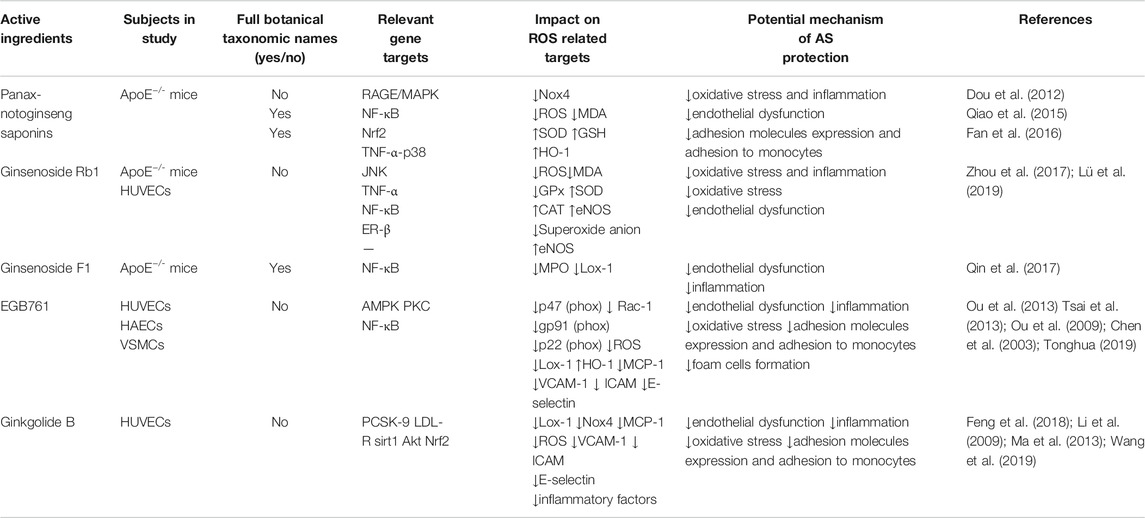
TABLE 7. Other active ingredients in herbs that treat atherosclerosis by regulating oxidative stress.
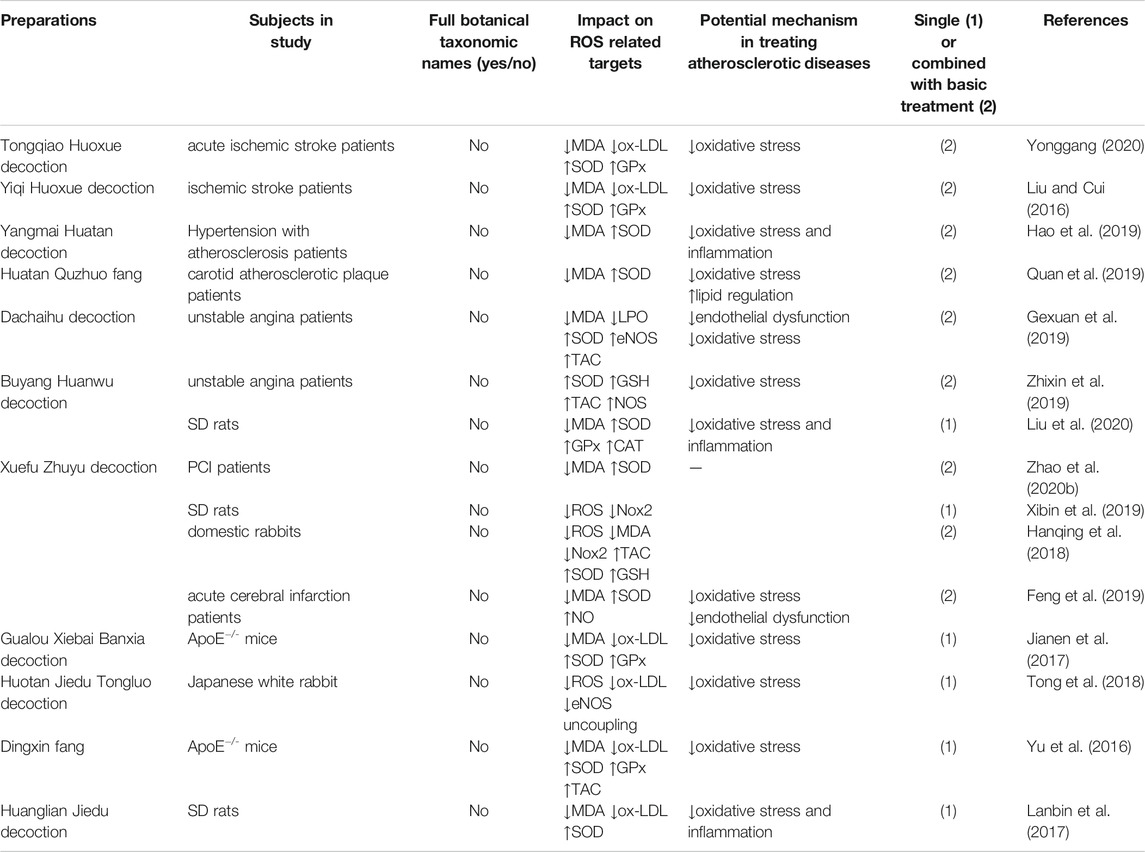
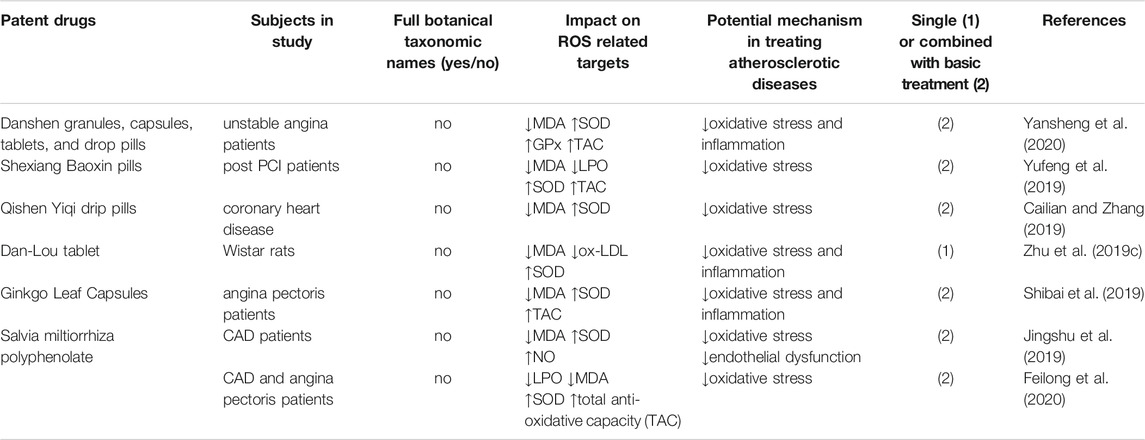
TCM Preparations and Related Drugs
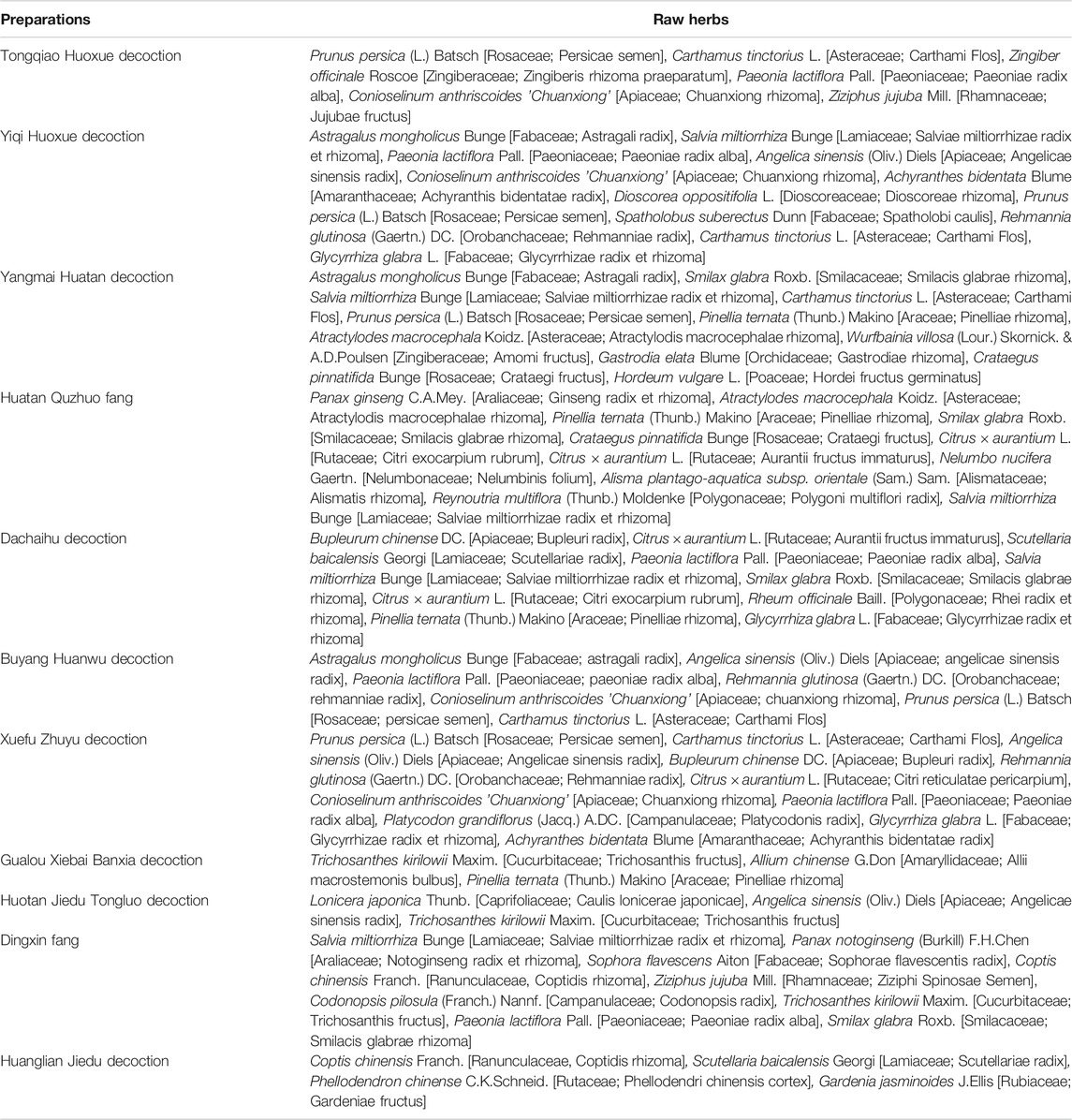
TCM preparations and its patent drugs include many Chinese herbs containing various ingredients. Clinical studies and laboratory research have shown positive effects on oxidative stress in atherosclerosis-related diseases (Hanqing et al., 2018; Feng et al., 2019; Xibin et al., 2019; Yonggang, 2020; Zhong et al., 2020). Tongqiao Huoxue decoction and Yiqi Huoxue decoction reduce MDA and ox-LDL production in ischemic stroke patients, relieve oxidative stress, and improve cerebral blood flow (Yonggang, 2020; Liu and Cui, 2016). Liang et al. (Hao et al., 2019) found that combined use of acupuncture and Dan-Lou tablets in patients with hypertension and atherosclerosis inhibited ROS production, enhanced SOD, and reduced inflammatory factors. Huatan Quzhuo fang exerted antioxidant effects in carotid atherosclerotic plaque patients (Quan et al., 2019). Dachaihu decoction (Gexuan et al., 2019) and Buyang Huanwu decoction (Zhixin et al., 2019) may reduce angina pectoris frequency in CHD patients through increasing SOD, total antioxidant capacity, and other antioxidant indicators. Xuefu Zhuyu decoction, which is frequently applied to treat blood stasis diseases in China, also shows alleviated atherosclerosis (Xibin et al., 2019; Feng et al., 2019; Zhao et al., 2020a), revealing a protective effect on oxidative stress (Table 8). According to Liu et al. (Liu et al., 2020), Buyang Huanwu decoction regulated oxidative stress and inflammation through TGF-β and NF-κB pathways, reducing MDA production and increasing CAT expression in a rat model of atherosclerosis. And the antioxidant effect achieved by Gualou Xiebai Banxia decoction was the inhibition of Lox-1 in aorta and enhancement of SOD and GPx generation (Jianen et al., 2017). Similar findings were also observed in Chinese medicine patent medications as well (Yu et al., 2016; Lanbin et al., 2017; Tong et al., 2018; Cailian and Zhang, 2019; Shibai et al., 2019; Yufeng et al., 2019; Zhu et al., 2019c; Yansheng et al., 2020). In CHD patients, clinical studies revealed that Salvia miltiorrhiza polyphenolate downregulated endothelin-1 expression, reducing the frequency of angina pectoris and improving heart function by protecting endothelial function and moderating oxidative stress (Jingshu et al., 2019; Feilong et al., 2020) (more details in Table 8 and Table 9, raw herbs of each preparation listed in Table 10).
Discussion
The application of antioxidants in the treatment of atherosclerosis are still under exploration. Clinical studies showed that natural antioxidants such as vitamin C and vitamin E did not reduce cardiovascular events (Libby et al., 2011). ACE inhibitors, ARB, aspirin, and statins reduce ROS generation and improve antioxidant effects (Kattoor et al., 2017). However, clear evidence of atherosclerotic antioxidant effects of these drugs remains insufficient. Probucol is a synthetic antioxidant used to regulate lipids and treat atherosclerosis. Kim et al. (Joon et al., 2018) found that combination use of aspirin or cilostazol with probucol can reduce vascular events in ischemic stroke at high risk of cerebral hemorrhage patients; however, they failed to demonstrate decreased risk of myocardial infarction. AGI-1067, an equivalent antioxidant and modifier of probucol, reduced restenosis after PCI without prolonging the QTc interval (Tardif et al., 2003). In a randomized double-blind placebo trial of acute coronary syndrome, AGI-1067 reduced composite secondary endpoint events such as primary outcome with all deaths, cardiovascular death, non-fatal myocardial infarction, or non-fatal stroke. Nevertheless, the agent insufficiently reduced the primary endpoint events, including cardiovascular death, myocardial infarction (non-fatal), stroke (non-fatal), and unstable angina, and was more likely to cause adverse events such as anemia and bleeding (Tardif et al., 2008). Further evaluation is required before the drug is officially used in the clinical treatment of atherosclerosis.
Chinese herbal medicine has a history spanning thousands of years and has been widely used to treat atherosclerosis in China. Based on our summary, current evidence from the studies illustrates that Chinese herbal medicines, herbal active metabolites, and TCM preparations have made progress in the antioxidant-mediated treatment of atherosclerosis. And the underlying mechanisms of these ingredients are also elucidated in a more specific manner, such as preventing plaque progression through protecting endothelial function, lipid metabolism, and foam cell formation. Researchers provided experimental bases for and clinical verifications of antioxidant targets of TCM. These ingredients may serve as alternatives for treatment of atherosclerosis via management of oxidative stress.
Nevertheless, there are limitations and controversies that hinder the promotion of these results. Most studies concluded in this review failed in stating the source plants of the active ingredients in appropriate botanical nomenclature (shown in Tables 1–8 and Table 10). Ambiguous or incorrect use of botanical nomenclature may hinder the accuracy and promotion of research results since readers may not recognize which plants are being referenced (Rivera et al., 2014).
Most clinical studies have an insufficient number of patients and a lack of large-scale multi-center clinical studies. TCM preparations consist of various Chinese herbs that may involve multiple chemical components. Their complexity and diversity creates challenges in determining the mechanisms of these compounds in treating atherosclerosis: are the therapeutic effects mediated by an active metabolite alone? Or do several ingredients work together? The questions remain open.
Choosing a suitable research model guarantees the accuracy of the TCM mechanism exploration and the reliability of the results. In vitro models, including mouse or human cell lines, are feasible tools to explore cellular functions and mechanisms, as well as gene targets and drug transport. Most of the atherosclerosis-related in vitro inflammation models used human or animal-derived macrophage cell lines, such as murine leukemia cell line RAW264.7 and J774 and human leukemia monocyte cell line THP-1. After intervening with phorbol-12-myristate-13- acetate (PMA), 1α, 25-dihydroxyvitamin D3 (vD3), or macrophage colony-stimulating factor (M-CSF), THP-1 could differentiate into macrophages (Chanput et al., 2014). Researchers analyzed the inflammation mechanisms in atherosclerosis by constructing a biology network model and found that HAECs expressed a richer mechanism map compared with immortalized endothelial cell lines (De Leon et al., 2014). Since the macrophages in human and mouse atherosclerotic lesions have been affected by microenvironmental factors, the results obtained from immortal cell lines may differ from the in vivo data. Primary macrophages, bone marrow-derived macrophages, and peritoneal macrophages, including large peritoneal macrophages (LPMs) and small peritoneal macrophages (SPMs), are also commonly used cell models in atherosclerosis. Both LPMs and SPMs can coordinate immune responses, but these two peritoneal macrophages subtypes show heterogeneous cellular markers (Lee and Choi, 2020). ApoE−/− mouse model, high-fat diet mouse, and rabbit model constitute the primary in vivo platforms for studying underlying pharmaceutical mechanisms in atherosclerosis. However, the location of atherosclerotic lesions in mice is different from that in humans. In the mouse model, plaques locate in the aortic sinus and innominate arteries, while the coronary arteries and carotid arteries are the primary lesions in human (Zhao et al., 2020b; Basu and Bornfeldt, 2020). The experimental models involved in this review can indeed explain the potential mechanisms of TCM in treating atherosclerosis via antioxidants. Nevertheless, due to the limitations of the in vitro and in vivo models, there is still a long way to go before basic research results can be transformed into the clinic.
In conclusion, translation from the bench to the bedside remains challenging. Oxidative stress is a critical component in the progression of atherosclerosis. Therefore, it is essential to develop medications or supplements to treat atherosclerosis from the perspective of enhancing antioxidant enzyme induction, inhibiting ROS generation, or blocking subsequent reactions, such as inhibition of inflammation process; all of these form vicious cycles in oxidative stress. Further exploration of the therapeutic effect of TCM on atherosclerosis from the perspective of oxidative stress and elucidating the mechanisms and targets will provide reliable evidence for the use of Chinese herbal medicine.
Author Contributions
LS searched the relevant literature and drafted the manuscript. HX and JJ provided helpful advice and organized the work. JZ, RL, and QL assisted in literature searching and revised the manuscript. All authors have read and approved the final version of the manuscript.
Funding
This article is supported by the National Natural Science Foundation of China (No. 81874412 and 82074215).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
The authors would like to thank the National Natural Science Foundation of China.
References
Antoniades, C., Shirodaria, C., Crabtree, M., Rinze, R., Alp, N., Cunnington, C., et al. (2007). Altered Plasma versus Vascular Biopterins in Human Atherosclerosis Reveal Relationships between Endothelial Nitric Oxide Synthase Coupling, Endothelial Function, and Inflammation. Circulation 116 (24), 2851–2859. doi:10.1161/circulationaha.107.704155
Antoniades, C., Shirodaria, C., Warrick, N., Cai, S., de Bono, J., Lee, J., et al. (2006). 5-methyltetrahydrofolate Rapidly Improves Endothelial Function and Decreases Superoxide Production in Human Vessels: Effects on Vascular Tetrahydrobiopterin Availability and Endothelial Nitric Oxide Synthase Coupling. Circulation 114 (11), 1193–201. doi:10.1161/circulationaha.106.612325
Asadi, A., Yaghobi Nezhad, D., Rafie Javazm, A., Khanicheragh, P., Mashouri, L., Shakeri, F., et al. (2020). In Vitro Effects of Curcumin on Transforming Growth Factor-β-Mediated Non-smad Signaling Pathway, Oxidative Stress, and Pro-inflammatory Cytokines Production with Human Vascular Smooth Muscle Cells. Iran J. Allergy Asthma Immunol. 19 (1), 84–93. doi:10.18502/ijaai.v19i1.2421
Barrett, T. J., Distel, E., Murphy, A. J., Hu, J., Garshick, M. S., Ogando, Y., et al. (2019). Apolipoprotein AI) Promotes Atherosclerosis Regression in Diabetic Mice by Suppressing Myelopoiesis and Plaque Inflammation. Circulation 140 (14), 1170–1184. doi:10.1161/circulationaha.119.039476
Basu, D., and Bornfeldt, K. E. (2020). Hypertriglyceridemia and Atherosclerosis: Using Human Research to Guide Mechanistic Studies in Animal Models. Front. Endocrinol. (Lausanne) 11, 504. doi:10.3389/fendo.2020.00504
Berbée, J. F., Wong, M. C., Wang, Y., van der Hoorn, J. W., Khedoe, P. P., van Klinken, J. B., et al. (2013). Resveratrol Protects against Atherosclerosis, but Does Not Add to the Antiatherogenic Effect of Atorvastatin, in APOE*3-Leiden.CETP Mice. J. Nutr. Biochem. 24 (8), 1423–1430. doi:10.1016/j.jnutbio.2012.11.009
Bhaskar, S., Sudhakaran, P. R., and Helen, A. (2016). Quercetin Attenuates Atherosclerotic Inflammation and Adhesion Molecule Expression by Modulating TLR-NF-Κb Signaling Pathway. Cell Immunol 310, 131–140. doi:10.1016/j.cellimm.2016.08.011
Bonnefont-Rousselot, D. (2016). Resveratrol and Cardiovascular Diseases. Nutrients 8 (5). doi:10.3390/nu8050250
Bruedigam, C., Eijken, M., Koedam, M., Chiba, H., and van Leeuwen, J. P. (2011). Opposing Actions of Rosiglitazone and Resveratrol on Mineralization in Human Vascular Smooth Muscle Cells. J. Mol. Cel Cardiol 51 (5), 862–871. doi:10.1016/j.yjmcc.2011.07.020
Cadenas, S. (2018). ROS and Redox Signaling in Myocardial Ischemia-Reperfusion Injury and Cardioprotection. Free Radic. Biol. Med. 117, 76–89. doi:10.1016/j.freeradbiomed.2018.01.024
Cailian, C., and Zhang, Lu. (2019). Effect of Qishen Yiqi Dripping Pills Combined with Ticagrelor on Plasma Visfatin Levels and Serum Oxidative Stress Markers in Patients with Coronary Heart Disease. Drug Eval. Res. 42 (05), 917–920. doi:10.7501/j.issn.1674-6376.2019.05.019
Caliceti, C., Rizzo, P., Ferrari, R., Fortini, F., Aquila, G., Leoncini, E., et al. (2017). Novel Role of the Nutraceutical Bioactive Compound Berberine in Lectin-like OxLDL Receptor 1-mediated Endothelial Dysfunction in Comparison to Lovastatin. Nutr. Metab. Cardiovasc. Dis. 27 (6), 552–563. doi:10.1016/j.numecd.2017.04.002
Canton, J., Neculai, D., and Grinstein, S. (2013). Scavenger Receptors in Homeostasis and Immunity. Nat. Rev. Immunol. 13 (9), 621–634. doi:10.1038/nri3515
Cao, H., Jia, Q., Yan, L., Chen, C., Xing, S., and Shen, D. (2019). Quercetin Suppresses the Progression of Atherosclerosis by Regulating MST1-Mediated Autophagy in Ox-LDL-Induced RAW264.7 Macrophage Foam Cells. Int. J. Mol. Sci. 20 (23). doi:10.3390/ijms20236093
Channon, K. M. (2002). Oxidative Stress and Coronary Plaque Stability. Arterioscler Thromb. Vasc. Biol. 22 (11), 1751–1752. doi:10.1161/01.atv.0000042203.08210.17
Chanput, W., Mes, J. J., and Wichers, H. J. (2014). THP-1 Cell Line: an In Vitro Cell Model for Immune Modulation Approach. Int. Immunopharmacol 23 (1), 37–45. doi:10.1016/j.intimp.2014.08.002
Chatzizisis, Y. S., Coskun, A. U., Jonas, M., Edelman, E. R., Feldman, C. L., and Stone, P. H. (2007). Role of Endothelial Shear Stress in the Natural History of Coronary Atherosclerosis and Vascular Remodeling: Molecular, Cellular, and Vascular Behavior. J. Am. Coll. Cardiol. 49 (25), 2379–2393. doi:10.1016/j.jacc.2007.02.059
Chen, J. W., Chen, Y. H., Lin, F. Y., Chen, Y. L., and Lin, S. J. (2003). Ginkgo Biloba Extract Inhibits Tumor Necrosis Factor-Alpha-Induced Reactive Oxygen Species Generation, Transcription Factor Activation, and Cell Adhesion Molecule Expression in Human Aortic Endothelial Cells. Arteriosclerosis, Thromb. Vasc. Biol. 23 (9), 1559–1566. doi:10.1161/01.atv.0000089012.73180.63
Chen, W., Tang, F., Xie, B., Chen, S., Huang, H., and Liu, P. (2012). Amelioration of Atherosclerosis by Tanshinone IIA in Hyperlipidemic Rabbits through Attenuation of Oxidative Stress. Eur. J. Pharmacol. 674 (2-3), 359–364. doi:10.1016/j.ejphar.2011.10.040
Chi, L., Peng, L., Hu, X., Pan, N., and Zhang, Y. (2014). Berberine Combined with Atorvastatin Downregulates LOX-1 Expression through the ET-1 Receptor in Monocyte/macrophages. Int. J. Mol. Med. 34 (1), 283–290. doi:10.3892/ijmm.2014.1748
Chistiakov, D. A., Melnichenko, A. A., Myasoedova, V. A., Grechko, A. V., and Orekhov, A. N. (2017). Mechanisms of Foam Cell Formation in Atherosclerosis. J. Mol. Med. (Berl) 95 (11), 1153–1165. doi:10.1007/s00109-017-1575-8
Cho, B. J., Im, E. K., Kwon, J. H., Lee, K. H., Shin, H. J., Oh, J., et al. (2005). Berberine Inhibits the Production of Lysophosphatidylcholine-Induced Reactive Oxygen Species and the ERK1/2 Pathway in Vascular Smooth Muscle Cells. Mol. Cell 20 (3), 429–434.
Chow, S. E., Hshu, Y. C., Wang, J. S., and Chen, J. K. (2007). Resveratrol Attenuates oxLDL-Stimulated NADPH Oxidase Activity and Protects Endothelial Cells from Oxidative Functional Damages. J. Appl. Physiol. 102 (4), 1520–1527. doi:10.1152/japplphysiol.00881.2006
Cui, Y., Hou, P., Li, F., Liu, Q., Qin, S., Zhou, G., et al. (2017). Quercetin Improves Macrophage Reverse Cholesterol Transport in Apolipoprotein E-Deficient Mice Fed a High-Fat Diet. Lipids Health Dis. 16 (1), 9. doi:10.1186/s12944-016-0393-2
Daiber, A., and Chlopicki, S. (2020). Revisiting Pharmacology of Oxidative Stress and Endothelial Dysfunction in Cardiovascular Disease: Evidence for Redox-Based Therapies. Free Radic. Biol. Med. 157, 15–37. doi:10.1016/j.freeradbiomed.2020.02.026
Davignon, J., and Ganz, P. (2004). Role of Endothelial Dysfunction in Atherosclerosis. Circulation 109 (23 Suppl. 1), Iii27–32. doi:10.1161/01.CIR.0000131515.03336.f8
De Leon, H., Boue, S., Schlage, W. K., Boukharov, N., Westra, J. W., Gebel, S., et al. (2014). A Vascular Biology Network Model Focused on Inflammatory Processes to Investigate Atherogenesis and Plaque Instability. J. Transl Med. 12, 185. doi:10.1186/1479-5876-12-185
Deng, Q., Li, X. X., Fang, Y., Chen, X., and Xue, J. (2020). Therapeutic Potential of Quercetin as an Antiatherosclerotic Agent in Atherosclerotic Cardiovascular Disease: A Review. Evid. Based Complement. Alternat Med. 2020, 5926381. doi:10.1155/2020/5926381
Dou, L., Lu, Y., Shen, T., Huang, X., Man, Y., Wang, S., et al. (2012). Panax Notogingseng Saponins Suppress RAGE/MAPK Signaling and NF-kappaB Activation in Apolipoprotein-E-Deficient Atherosclerosis-Prone Mice. Cell Physiol Biochem 29 (5-6), 875–882. doi:10.1159/000315061
Drechsler, M., Megens, R. T., van Zandvoort, M., Weber, C., and Soehnlein, O. (2010). Hyperlipidemia-triggered Neutrophilia Promotes Early Atherosclerosis. Circulation 122 (18), 1837–1845. doi:10.1161/circulationaha.110.961714
Duan, L., Xiong, X., Hu, J., Liu, Y., Li, J., and Wang, J. (2017). Panax Notoginseng Saponins for Treating Coronary Artery Disease: A Functional and Mechanistic Overview. Front. Pharmacol. 8, 702. doi:10.3389/fphar.2017.00702
Duivenvoorden, R., Mani, V., Woodward, M., Kallend, D., Suchankova, G., Fuster, V., et al. (2013). Relationship of Serum Inflammatory Biomarkers with Plaque Inflammation Assessed by FDG PET/CT: the Dal-PLAQUE Study. JACC Cardiovasc. Imaging 6 (10), 1087–1094. doi:10.1016/j.jcmg.2013.03.009
Fan, J., Liu, D., He, C., Li, X., and He, F. (2016). Inhibiting Adhesion Events by Panax Notoginseng Saponins and Ginsenoside Rb1 Protecting Arteries via Activation of Nrf2 and Suppression of P38 - VCAM-1 Signal Pathway. J. ethnopharmacology 192, 423–430. doi:10.1016/j.jep.2016.09.022
Fan, X., Wang, J., Hou, J., Lin, C., Bensoussan, A., Chang, D., et al. (2015). Berberine Alleviates Ox-LDL Induced Inflammatory Factors by Up-Regulation of Autophagy via AMPK/mTOR Signaling Pathway. J. Transl Med. 13, 92. doi:10.1186/s12967-015-0450-z
Fang, Z. Y., Lin, R., Yuan, B. X., Yang, G. D., Liu, Y., and Zhang, H. (2008). Tanshinone IIA Downregulates the CD40 Expression and Decreases MMP-2 Activity on Atherosclerosis Induced by High Fatty Diet in Rabbit. J. Ethnopharmacol 115 (2), 217–222. doi:10.1016/j.jep.2007.09.025
Fatahian, A., Haftcheshmeh, S. M., Azhdari, S., Farshchi, H. K., Nikfar, B., and Momtazi-Borojeni, A. A. (2020). Promising Anti-atherosclerotic Effect of Berberine: Evidence from In Vitro, In Vivo, and Clinical Studies. Rev. Physiol. Biochem. Pharmacol. 178, 83–110. doi:10.1007/112_2020_42
Feilong, Chen., Wang, Xiuling., and Ma, Bin. (2020). Evaluation for the Treatment Effect of Salvianolate and its Influence on the Hemorheologyand Oxidative Stress in Angina Pectoris Patients. Chin. J. Disaster Med. 8 (03), 137–141. doi:10.13919/j.issn.2095-6274.2020.03.005
Feng, Chen., Wu, Xi., Mu, Yingtao., Xu, Taotao., and Liu, Renbin. (2019). Effects of Xuefu Zhuyu Decoction Combined with Conventional Treatment on Inflammatory Response, Oxidative Stress, Endothelium and Related Factors in Patients with Acute Cerebral Infarction. J. Hainan Med. Univ. 25 (10), 762–765. doi:10.13210/j.cnki.jhmu.20190327.001
Feng, J., Liu, L., Yao, F., Zhou, D., He, Y., and Wang, J. (2021). The Protective Effect of Tanshinone IIa on Endothelial Cells: a Generalist Among Clinical Therapeutics. Expert Rev. Clin. Pharmacol. 14 (2), 239–248. doi:10.1080/17512433.2021.1878877
Feng, Z., Yang, X., Zhang, L., Ansari, I. A., Khan, M. S., Han, S., et al. (2018). Ginkgolide B Ameliorates Oxidized Low-Density Lipoprotein-Induced Endothelial Dysfunction via Modulating Lectin-like Ox-LDL-Receptor-1 and NADPH Oxidase 4 Expression and Inflammatory Cascades. Phytotherapy Res. : PTR 32 (12), 2417–2427. doi:10.1002/ptr.6177
Fleenor, B. S., Sindler, A. L., Marvi, N. K., Howell, K. L., Zigler, M. L., Yoshizawa, M., et al. (2013). Curcumin Ameliorates Arterial Dysfunction and Oxidative Stress with Aging. Exp. Gerontol. 48 (2), 269–276. doi:10.1016/j.exger.2012.10.008
Förstermann, U., Xia, N., and Li, H. (2017). Roles of Vascular Oxidative Stress and Nitric Oxide in the Pathogenesis of Atherosclerosis. Circ. Res. 120 (4), 713–735. doi:10.1161/circresaha.116.309326
Gao, S., Liu, Z., Li, H., Little, P. J., Liu, P., and Xu, S. (2012). Cardiovascular Actions and Therapeutic Potential of Tanshinone IIA. Atherosclerosis 220 (1), 3–10. doi:10.1016/j.atherosclerosis.2011.06.041
Gexuan, R., Li, X., Tan, H., and Chen, J. (2019). A Multicenter, Randomized, Double-Blind Controlled Clinical Trial of Dachaihu Decoction for Unstable Angina Pectoris. World Chin. Med. 14 (04), 882–886. doi:10.3969/j.issn.1673-7202.2019.04.018
Gliemann, L., Schmidt, J. F., Olesen, J., Biensø, R. S., Peronard, S. L., Grandjean, S. U., et al. (2013). Resveratrol Blunts the Positive Effects of Exercise Training on Cardiovascular Health in Aged Men. J. Physiol. 591 (20), 5047–5059. doi:10.1113/jphysiol.2013.258061
Goel, A., Kunnumakkara, A. B., and Aggarwal, B. B. (2008). Curcumin as “Curecumin”: from Kitchen to Clinic. Biochem. Pharmacol. 75 (4), 787–809. doi:10.1016/j.bcp.2007.08.016
Gress, T. W., Nieto, F. J., Shahar, E., Wofford, M. R., and Brancati, F. L. (2000). Hypertension and Antihypertensive Therapy as Risk Factors for Type 2 Diabetes Mellitus. Atherosclerosis Risk in Communities Study. N. Engl. J. Med. 342 (13), 905–912. doi:10.1056/nejm200003303421301
Griendling, K. K., and FitzGerald, G. A. (2003a). Oxidative Stress and Cardiovascular Injury: Part I: Basic Mechanisms and In Vivo Monitoring of ROS. Circulation 108 (16), 1912–1916. doi:10.1161/01.Cir.0000093660.86242.Bb
Griendling, K. K., and FitzGerald, G. A. (2003b). Oxidative Stress and Cardiovascular Injury: Part II: Animal and Human Studies. Circulation 108 (17), 2034–2040. doi:10.1161/01.CIR.0000093661.90582.c4
Guo, C., Davies, M. J., and Hawkins, C. L. (2020). Role of Thiocyanate in the Modulation of Myeloperoxidase-Derived Oxidant Induced Damage to Macrophages. Redox Biol. 36, 101666. doi:10.1016/j.redox.2020.101666
Haimei, L., Xu, J., Guan, L., Lin, Y., and Yan, F. (2019). Mechanism of Resveratrol Regulating Orai1 Expression in Aorta of Mice and Inhibiting Oxidative Stress Injury in Atherosclerosis. Pharmacol. Clin. Chin. Materia Med. 35 (01), 71–76. doi:10.13412/j.cnki.zyyl.2019.01.016
Hanqing, T., Pang, L., Zhang, S., Yue, F., Ning, W., and Wang, L. (2018). Effects of Xuefu Zhuyu Decoction on Oxidative Stress in Rabbits with Blood Stasis Syndrome of Coronary Heart Disease. Prog. Vet. Med. 39 (08), 31–35. doi:10.16437/j.cnki.1007-5038.2018.08.007
Hao, L., Yu, Y., and Zhou, Z. (2019). Clinical Observation on Acupuncture and Medicine Combined Treatment of Hypertension with Atherosclerosis. China Med. Herald 16 (30), 147–150.
Hickey, M. J. (2011). MPO and Neutrophils: a Magnetic Attraction. Blood 117 (4), 1103–1104. doi:10.1182/blood-2010-11-317479
Hou, X., Lin, H., Zhou, X., Cheng, Z., Li, Y., Liu, X., et al. (2020). Novel Dual ROS-Sensitive and CD44 Receptor Targeting Nanomicelles Based on Oligomeric Hyaluronic Acid for the Efficient Therapy of Atherosclerosis. Carbohydr. Polym. 232, 115787. doi:10.1016/j.carbpol.2019.115787
Huang, L., Chambliss, K. L., Gao, X., Yuhanna, I. S., Behling-Kelly, E., Bergaya, S., et al. (2019). SR-B1 Drives Endothelial Cell LDL Transcytosis via DOCK4 to Promote Atherosclerosis. Nature 569 (7757), 565–569. doi:10.1038/s41586-019-1140-4
Huang, S. L., Chen, P. Y., Wu, M. J., Tai, M. H., Ho, C. T., and Yen, J. H. (2015). Curcuminoids Modulate the PKCδ/NADPH Oxidase/Reactive Oxygen Species Signaling Pathway and Suppress Matrix Invasion during Monocyte-Macrophage Differentiation. J. Agric. Food Chem. 63 (40), 8838–8848. doi:10.1021/acs.jafc.5b04083
Huang, Y., DiDonato, J. A., Levison, B. S., Schmitt, D., Li, L., Wu, Y., et al. (2014). An Abundant Dysfunctional Apolipoprotein A1 in Human Atheroma. Nat. Med. 20 (2), 193–203. doi:10.1038/nm.3459
Huang, Y., Wu, Z., Riwanto, M., Gao, S., Levison, B. S., Gu, X., et al. (2013). Myeloperoxidase, Paraoxonase-1, and HDL Form a Functional Ternary Complex. J. Clin. Invest. 123 (9), 3815–3828. doi:10.1172/jci67478
Huimin, Cao., Song, Nan., Zhang, Ni., Yang, Guanlin., Chen, Wenzhe., Zhang, Zhe., et al. (2017). Regulation on Autophagy with Tanshinone ⅡA for Anti-oxidative Stress Damage of Endothelial Cells through PI3K/Akt/mTOR Pathway. J. Beijing Univ. Traditional Chin. Med. 40 (11), 933–939. doi:10.3969/j.issn.1006-2157.2017.11.011
Hulsmans, M., and Holvoet, P. (2010). The Vicious Circle between Oxidative Stress and Inflammation in Atherosclerosis. J. Cel Mol Med 14 (1-2), 70–78. doi:10.1111/j.1582-4934.2009.00978.x
Hung, C. H., Chan, S. H., Chu, P. M., and Tsai, K. L. (2015). Quercetin Is a Potent Anti-atherosclerotic Compound by Activation of SIRT1 Signaling under oxLDL Stimulation. Mol. Nutr. Food Res. 59 (10), 1905–1917. doi:10.1002/mnfr.201500144
Imamura, H., Yamaguchi, T., Nagayama, D., Saiki, A., Shirai, K., and Tatsuno, I. (2017). Resveratrol Ameliorates Arterial Stiffness Assessed by Cardio-Ankle Vascular Index in Patients with Type 2 Diabetes Mellitus. Int. Heart J. 58 (4), 577–583. doi:10.1536/ihj.16-373
Jia, Q., Cao, H., Shen, D., Li, S., Yan, L., Chen, C., et al. (2019). Quercetin Protects against Atherosclerosis by Regulating the Expression of PCSK9, CD36, PPARγ, LXRα and ABCA1. Int. J. Mol. Med. 44 (3), 893–902. doi:10.3892/ijmm.2019.4263
Jianen, G., Shubin, M., Yan, X., Xin, S., Gao, F., Liang, G., et al. (2017). Effects of Gualou Xiebai Banxia Decoction on Blood Lipid Metabolism, Oxidative Stress and Aortic Lox-1 Expression in ApoE-/- Mice. Zhongguo Zhong yao za zhi 42 (04), 752–757. doi:10.19540/j.cnki.cjcmm.20161222.076
Jiang, Y. H., Jiang, L. Y., Wang, Y. C., Ma, D. F., and Li, X. (2020). Quercetin Attenuates Atherosclerosis via Modulating Oxidized LDL-Induced Endothelial Cellular Senescence. Front. Pharmacol. 11, 512. doi:10.3389/fphar.2020.00512
Jiang, Y., Huang, K., Lin, X., Chen, Q., Lin, S., Feng, X., et al. (2017). Berberine Attenuates NLRP3 Inflammasome Activation in Macrophages to Reduce the Secretion of Interleukin-1β. Ann. Clin. Lab. Sci. 47 (6), 720–728.
Jin, S., Jeon, J. H., Lee, S., Kang, W. Y., Seong, S. J., Yoon, Y. R., et al. (2019). Detection of 13 Ginsenosides (Rb1, Rb2, Rc, Rd, Re, Rf, Rg1, Rg3, Rh2, F1, Compound K, 20 (S)-Protopanaxadiol, and 20 (S)-Protopanaxatriol) in Human Plasma and Application of the Analytical Method to Human Pharmacokinetic Studies Following Two Week-Repeated Administration of Red Ginseng Extract. Molecules 24 (14). doi:10.3390/molecules24142618
Jingshu, G., Zhou, Y., Miao, Z., Gao, S., and Jia, C. (2019). Effect of Salvianolate on Endothelial Function and Oxidative Stress in Patients with Coronary Heart. China Pharmaceuticals 28 (24), 75–77. doi:10.3969/j.issn.1006-4931.2019.24.024
Joon, K. B., Lee, E-J., Kwon Sun, U., Park Jong-Ho, S., Kim, Y-J., Hong, K-S., et al. (2018). Prevention of Cardiovascular Events in Asian Patients with Ischaemic Stroke at High Risk of Cerebral Haemorrhage (PICASSO): a Multicentre, Randomised Controlled Trial. Lancet Neurol. 17 (6).
Jung, I. H., Lee, Y. H., Yoo, J. Y., Jeong, S. J., Sonn, S. K., Park, J. G., et al. (2012). Ginkgo Biloba Extract (GbE) Enhances the Anti-atherogenic Effect of Cilostazol by Inhibiting ROS Generation. Exp. Mol. Med. 44 (5), 311–318. doi:10.3858/emm.2012.44.5.035
Karunakaran, D., Nguyen, M. A., Geoffrion, M., Vreeken, D., Lister, Z., Cheng, H. S., et al. (2021). RIPK1 Expression Associates with Inflammation in Early Atherosclerosis in Humans and Can Be Therapeutically Silenced to Reduce NF-Κb Activation and Atherogenesis in Mice. Circulation 143 (2), 163–177. doi:10.1161/circulationaha.118.038379
Kattoor, A. J., Pothineni, N. V. K., Palagiri, D., and Mehta, J. L. (2017). Oxidative Stress in Atherosclerosis. Curr. Atheroscler. Rep. 19 (11), 42. doi:10.1007/s11883-017-0678-6
Kim, H. S., Park, K. G., Koo, T. B., Huh, S., and Lee, I. K. (2007). The Modulating Effects of the Overexpression of Uncoupling Protein 2 on the Formation of Reactive Oxygen Species in Vascular Cells. Diabetes Res. Clin. Pract. 77 (Suppl. 1), S46–S48. doi:10.1016/j.diabres.2007.01.032
Konior, A., Schramm, A., Czesnikiewicz-Guzik, M., and Guzik, T. J. (2014). NADPH Oxidases in Vascular Pathology. Antioxid. Redox Signal. 20 (17), 2794–2814. doi:10.1089/ars.2013.5607
Lanbin, Y., Chen, Y., Xu, G., Yang, L., Hu, J., Duan, J., et al. (2017). Study on the Mechanism of Huanglian Jiedu Decoction on Atherosclerotic Rats Based on Anti-inflammatory and Oxidative Stress. Modernization Traditional Chin. Med. Materia Medica-World Sci. Techn. 19 (11), 1841–1845. doi:10.11842/wst.2017.11.013
Langbein, H., Brunssen, C., Hofmann, A., Cimalla, P., Brux, M., Bornstein, S. R., et al. (2016). NADPH Oxidase 4 Protects against Development of Endothelial Dysfunction and Atherosclerosis in LDL Receptor Deficient Mice. Eur. Heart J. 37 (22), 1753–1761. doi:10.1093/eurheartj/ehv564
Lara-Guzman, O. J., Tabares-Guevara, J. H., Leon-Varela, Y. M., Álvarez, R. M., Roldan, M., Sierra, J. A., et al. (2012). Proatherogenic Macrophage Activities Are Targeted by the Flavonoid Quercetin. J. Pharmacol. Exp. Ther. 343 (2), 296–306. doi:10.1124/jpet.112.196147
Laufs, U., Wassmann, S., Czech, T., Münzel, T., Eisenhauer, M., Böhm, M., et al. (2005). Physical Inactivity Increases Oxidative Stress, Endothelial Dysfunction, and Atherosclerosis. Arterioscler Thromb. Vasc. Biol. 25 (4), 809–814. doi:10.1161/01.ATV.0000158311.24443.af
Lee, J., and Choi, J. H. (2020). Deciphering Macrophage Phenotypes upon Lipid Uptake and Atherosclerosis. Immune Netw. 20 (3), e22. doi:10.4110/in.2020.20.e22
Lee, S. E., Park, H. R., Jeon, S., Han, D., and Park, Y. S. (2020). Curcumin Attenuates Acrolein-Induced COX-2 Expression and Prostaglandin Production in Human Umbilical Vein Endothelial Cells. J. Lipid Atheroscler. 9 (1), 184–194. doi:10.12997/jla.2020.9.1.184
Lee, T. S., Pan, C. C., Peng, C. C., Kou, Y. R., Chen, C. Y., Ching, L. C., et al. (2010). Anti-atherogenic Effect of Berberine on LXRalpha-ABCA1-dependent Cholesterol Efflux in Macrophages. J. Cel Biochem 111 (1), 104–10. doi:10.1002/jcb.22667
Li, C., Miao, X., Li, F., Adhikari, B. K., Liu, Y., Sun, J., et al. (2019a). Curcuminoids: Implication for Inflammation and Oxidative Stress in Cardiovascular Diseases. Phytother Res. 33 (5), 1302–1317. doi:10.1002/ptr.6324
Li, C., Zhang, W. J., Choi, J., and Frei, B. (2016a). Quercetin Affects Glutathione Levels and Redox Ratio in Human Aortic Endothelial Cells Not through Oxidation but Formation and Cellular Export of Quercetin-Glutathione Conjugates and Upregulation of Glutamate-Cysteine Ligase. Redox Biol. 9, 220–228. doi:10.1016/j.redox.2016.08.012
Li, C., Zhang, W. J., and Frei, B. (2016b). Quercetin Inhibits LPS-Induced Adhesion Molecule Expression and Oxidant Production in Human Aortic Endothelial Cells by P38-Mediated Nrf2 Activation and Antioxidant Enzyme Induction. Redox Biol. 9, 104–113. doi:10.1016/j.redox.2016.06.006
Li, F., Tang, H., Xiao, F., Gong, J., Peng, Y., and Meng, X. (2011a). Protective Effect of Salidroside from Rhodiolae Radix on Diabetes-Induced Oxidative Stress in Mice. Molecules 16 (12), 9912–9924. doi:10.3390/molecules16129912
Li, H., Sureda, A., Devkota, H. P., Pittalà, V., Barreca, D., Silva, A. S., et al. (2020a). Curcumin, the Golden Spice in Treating Cardiovascular Diseases. Biotechnol. Adv. 38, 107343. doi:10.1016/j.biotechadv.2019.01.010
Li, J. M., and Shah, A. M. (2004). Endothelial Cell Superoxide Generation: Regulation and Relevance for Cardiovascular Pathophysiology. Am. J. Physiol. Regul. Integr. Comp. Physiol. 287 (5), R1014–R1030. doi:10.1152/ajpregu.00124.2004
Li, J., Xie, Z. Z., Tang, Y. B., Zhou, J. G., and Guan, Y. Y. (2011b). Ginsenoside-Rd, a Purified Component from Panax Notoginseng Saponins, Prevents Atherosclerosis in apoE Knockout Mice. Eur. J. Pharmacol. 652 (1-3), 104–10. doi:10.1016/j.ejphar.2010.11.017
Li, J., Zhong, Z., Yuan, J., Chen, X., Huang, Z., and Wu, Z. (2019b). Resveratrol Improves Endothelial Dysfunction and Attenuates Atherogenesis in Apolipoprotein E-Deficient Mice. J. Nutr. Biochem. 67, 63–71. doi:10.1016/j.jnutbio.2019.01.022
Li, R., Chen, B. W. Wu., Bao, L., Li, J., and Qi, R. (2009). Ginkgolide B Suppresses Intercellular Adhesion Molecule-1 Expression via Blocking Nuclear Factor-kappaB Activation in Human Vascular Endothelial Cells Stimulated by Oxidized Low-Density Lipoprotein. J. Pharmacol. Sci. 110 (3), 362–369. doi:10.1254/jphs.08275fp
Li, X., Lu, L., Chen, J., Zhang, C., Chen, H., and Huang, H. (2020b). Ginkgo BilobaNew Insight into the Mechanisms of Extract in Vascular Aging Prevention. Curr. Vasc. Pharmacol. 18 (4), 334–345. doi:10.2174/1570161117666190621150725
Li, Y., Aziz, Q., Anderson, N., Ojake, L., and Tinker, A. (2020c). Endothelial ATP-Sensitive Potassium Channel Protects against the Development of Hypertension and Atherosclerosis. Hypertension 76 (3), 776–784. doi:10.1161/hypertensionaha.120.15355
Li, Y. I., Elmer, G., and Leboeuf, R. C. (2008). Tanshinone IIA Reduces Macrophage Death Induced by Hydrogen Peroxide by Upregulating Glutathione Peroxidase. Life Sci. 83 (15-16), 557–562. doi:10.1016/j.lfs.2008.08.003
Li, Y. R., Li, S., and Lin, C. C. (2018a). Effect of Resveratrol and Pterostilbene on Aging and Longevity. Biofactors 44 (1), 69–82. doi:10.1002/biof.1400
Li, Y., Tian, L., Sun, D., and Yin, D. (2019c). Curcumin Ameliorates Atherosclerosis through Upregulation of miR-126. J. Cel Physiol 234 (11), 21049–21059. doi:10.1002/jcp.28708
Li, Z. M., Xu, S. W., and Liu, P. Q. (2018b). Salvia miltiorrhizaBurge (Danshen): a Golden Herbal Medicine in Cardiovascular Therapeutics. Acta Pharmacol. Sin 39 (5), 802–824. doi:10.1038/aps.2017.193
Liao, J., An, X., Yang, X., Lin, Q. Y., Liu, S., Xie, Y., et al. (2020). Deficiency of LMP10 Attenuates Diet-Induced Atherosclerosis by Inhibiting Macrophage Polarization and Inflammation in Apolipoprotein E Deficient Mice. Front Cel Dev Biol 8, 592048. doi:10.3389/fcell.2020.592048
Libby, P., Buring, J. E., Badimon, L., Hansson, G. K., Deanfield, J., Bittencourt, M. S., et al. (2019). Atherosclerosis. Nat. Rev. Dis. Primers 5 (1), 56. doi:10.1038/s41572-019-0106-z
Libby, P., Ridker, P. M., and Hansson, G. K. (2011). Progress and Challenges in Translating the Biology of Atherosclerosis. Nature 473 (7347), 317–325. doi:10.1038/nature10146
Lin, C. J., Lee, C. C., Shih, Y. L., Lin, T. Y., Wang, S. H., Lin, Y. F., et al. (2012). Resveratrol Enhances the Therapeutic Effect of Temozolomide against Malignant Glioma In Vitro and In Vivo by Inhibiting Autophagy. Free Radic. Biol. Med. 52 (2), 377–391. doi:10.1016/j.freeradbiomed.2011.10.487
Lin, R., Wang, W. R., Liu, J. T., Yang, G. D., and Han, C. J. (2006). Protective Effect of Tanshinone IIA on Human Umbilical Vein Endothelial Cell Injured by Hydrogen Peroxide and its Mechanism. J. Ethnopharmacol 108 (2), 217–222. doi:10.1016/j.jep.2006.05.004
Liu, B., Song, Z., Yu, J., Li, P., Tang, Y., and Ge, J. (2020). The Atherosclerosis-Ameliorating Effects and Molecular Mechanisms of BuYangHuanWu Decoction. Biomed. Pharmacother. 123, 109664. doi:10.1016/j.biopha.2019.109664
Liu, X., Lu, B., Fu, J., Zhu, X., Song, E., and Song, Y. (2021). Amorphous Silica Nanoparticles Induce Inflammation via Activation of NLRP3 Inflammasome and HMGB1/TLR4/MYD88/NF-Kb Signaling Pathway in HUVEC Cells. J. Hazard. Mater. 404, 124050. doi:10.1016/j.jhazmat.2020.124050
Liu, X., Guo, C. Y., Ma, X. J., Wu, C. F., Zhang, Y., Sun, M. Y., et al. (2015). Anti-inflammatory Effects of Tanshinone IIA on Atherosclerostic Vessels of Ovariectomized ApoE Mice Are Mediated by Estrogen Receptor Activation and through the ERK Signaling Pathway. Cel Physiol Biochem 35 (5), 1744–1755. doi:10.1159/000373986
Liu, X., and Cui, Y. (2016). Effect of Yiqi Huoxue Decoction on Oxidative Stress Response and Neurologic Deficit in Patients with Ischemic Stroke. Mod. J. Integrated Traditional Chin. West. Med. 25 (22), 2422–2424. doi:10.3969/j.issn.1008-8849.2016.22.009
Loke, W. M., Proudfoot, J. M., Hodgson, J. M., McKinley, A. J., Hime, N., Magat, M., et al. (2010). Specific Dietary Polyphenols Attenuate Atherosclerosis in Apolipoprotein E-Knockout Mice by Alleviating Inflammation and Endothelial Dysfunction. Arterioscler Thromb. Vasc. Biol. 30 (4), 749–757. doi:10.1161/atvbaha.109.199687
Lü, J. M., Jiang, J., Jamaluddin, M. S., Liang, Z., Yao, Q., and Chen, C. (2019). Ginsenoside Rb1 Blocks Ritonavir-Induced Oxidative Stress and eNOS Downregulation through Activation of Estrogen Receptor-Beta and Upregulation of SOD in Human Endothelial Cells. Int. J. Mol. Sci. 20 (2). doi:10.3390/ijms20020294
Lu, X. L., Zhao, C. H., Yao, X. L., and Zhang, H. (2017). Quercetin Attenuates High Fructose Feeding-Induced Atherosclerosis by Suppressing Inflammation and Apoptosis via ROS-Regulated PI3K/AKT Signaling Pathway. Biomed. Pharmacother. 85, 658–671. doi:10.1016/j.biopha.2016.11.077
Luo, M., Tian, R., and Lu, N. (2020). Quercetin Inhibited Endothelial Dysfunction and Atherosclerosis in Apolipoprotein E-Deficient Mice: Critical Roles for NADPH Oxidase and Heme Oxygenase-1. J. Agric. Food Chem. 68 (39), 10875–10883. doi:10.1021/acs.jafc.0c03907
Lv, Y. L., Jia, Y., Wan, Z., An, Z. L., Yang, S., Han, F. F., et al. (2020). Curcumin Inhibits the Formation of Atherosclerosis in ApoE(-/-) Mice by Suppressing Cytomegalovirus Activity in Endothelial Cells. Life Sci. 257, 117658. doi:10.1016/j.lfs.2020.117658
Ma, L., Liu, X., Zhao, Y., Chen, B., Li, X., and Qi, R. (2013). Ginkgolide B Reduces LOX-1 Expression by Inhibiting Akt Phosphorylation and Increasing Sirt1 Expression in Oxidized LDL-Stimulated Human Umbilical Vein Endothelial Cells. PloS one 8 (9), e74769. doi:10.1371/journal.pone.0074769
Ma, Q., Yang, Q., Chen, J., Yu, C., Zhang, L., Zhou, W., et al. (2020). Salvianolic Acid A Ameliorates Early-Stage Atherosclerosis Development by Inhibiting NLRP3 Inflammasome Activation in Zucker Diabetic Fatty Rats. Molecules 25 (5). doi:10.3390/molecules25051089
Madamanchi, N. R., Vendrov, A., and Runge, M. S. (2005). Oxidative Stress and Vascular Disease. Arterioscler Thromb. Vasc. Biol. 25 (1), 29–38. doi:10.1161/01.Atv.0000150649.39934.13
Mansur, A. P., Roggerio, A., Goes, M. F. S., Avakian, S. D., Leal, D. P., Maranhão, R. C., et al. (2017). Serum Concentrations and Gene Expression of Sirtuin 1 in Healthy and Slightly Overweight Subjects after Caloric Restriction or Resveratrol Supplementation: A Randomized Trial. Int. J. Cardiol. 227, 788–794. doi:10.1016/j.ijcard.2016.10.058
Mao, G. X., Wang, Y., Qiu, Q., Deng, H. B., Yuan, L. G., Li, R. G., et al. (2010). Salidroside Protects Human Fibroblast Cells from Premature Senescence Induced by H(2)O(2) Partly through Modulating Oxidative Status. Mech. Ageing Dev. 131 (11-12), 723–731. doi:10.1016/j.mad.2010.10.003
McClelland, R. L., Chung, H., Detrano, R., Post, W., and Kronmal, R. A. (2006). Distribution of Coronary Artery Calcium by Race, Gender, and Age: Results from the Multi-Ethnic Study of Atherosclerosis (MESA). Circulation 113 (1), 30–37. doi:10.1161/circulationaha.105.580696
McNally, J. S., Davis, M. E., Giddens, D. P., Saha, A., Hwang, J., Dikalov, S., et al. (2003). Role of Xanthine Oxidoreductase and NAD(P)H Oxidase in Endothelial Superoxide Production in Response to Oscillatory Shear Stress. Am. J. Physiol. Heart Circ. Physiol. 285 (6), H2290–H2297. doi:10.1152/ajpheart.00515.2003
Meng, N., Gong, Y., Zhang, J., Mu, X., Song, Z., Feng, R., et al. (2019). A Novel Curcumin-Loaded Nanoparticle Restricts Atherosclerosis Development and Promotes Plaques Stability in Apolipoprotein E Deficient Mice. J. Biomater. Appl. 33 (7), 946–954. doi:10.1177/0885328218815328
Mohar, D. S., and Malik, S. (2012). The Sirtuin System: The Holy Grail of Resveratrol? J. Clin. Exp. Cardiolog 3 (11). doi:10.4172/2155-9880.1000216
Moore, K. J., and Tabas, I. (2011). Macrophages in the Pathogenesis of Atherosclerosis. Cell 145 (3), 341–355. doi:10.1016/j.cell.2011.04.005
Mulvihill, E. E., and Huff, M. W. (2010). Antiatherogenic Properties of Flavonoids: Implications for Cardiovascular Health. Can. J. Cardiol. 26 (Suppl. l), 17a–21a. doi:10.1016/s0828-282x(10)71056-4
Murdocca, M., C De Masi, S., Pucci, R. M., Novelli, G., Di Natale, C., and Sangiuolo, F. (2021). LOX-1 and Cancer: an Indissoluble Liaison. Cancer Gene Ther. doi:10.1038/s41417-020-00279-0
Mury, P., Chirico, E. N., Mura, M., Millon, A., Canet-Soulas, E., and Pialoux, V. (2018). Oxidative Stress and Inflammation, Key Targets of Atherosclerotic Plaque Progression and Vulnerability: Potential Impact of Physical Activity. Sports Med. 48 (12), 2725–2741. doi:10.1007/s40279-018-0996-z
Naito, M., Wu, X., Nomura, H., Kodama, M., Kato, Y., Kato, Y., et al. (2002). The Protective Effects of Tetrahydrocurcumin on Oxidative Stress in Cholesterol-Fed Rabbits. J. Atheroscler. Thromb. 9 (5), 243–250. doi:10.5551/jat.9.243
Naya, M., Morita, K., Yoshinaga, K., Manabe, O., Goto, D., Hirata, K., et al. (2011). Long-term Smoking Causes More Advanced Coronary Endothelial Dysfunction in Middle-Aged Smokers Compared to Young Smokers. Eur. J. Nucl. Med. Mol. Imaging 38 (3), 491–498. doi:10.1007/s00259-010-1647-2
Ni, J., Li, Y., Li, W., and Guo, R. (2017a). Salidroside Protects against Foam Cell Formation and Apoptosis, Possibly via the MAPK and AKT Signaling Pathways. Lipids Health Dis. 16 (1), 198. doi:10.1186/s12944-017-0582-7
Ni, Z., Cao, H., Song, N., Yang, G., Jia, L., and Zhang, Z. (2017b). The Protective Effect of Tanshinone ⅡA on Ox-LDL Induced Endothelial Cell Oxidative Stress Injury through Regulating Autophagosome. Chin. J. Arteriosclerosis 25 (03), 244–249.
Niu, X. L., Ichimori, K., Yang, X., Hirota, Y., Hoshiai, K., Li, M., et al. (2000). Tanshinone II-A Inhibits Low Density Lipoprotein Oxidation In Vitro. Free Radic. Res. 33 (3), 305–312. doi:10.1080/10715760000301471
Olmos, Y., Sánchez-Gómez, F. J., Wild, B., García-Quintans, N., Cabezudo, S., Lamas, S., et al. (2013). SirT1 Regulation of Antioxidant Genes Is Dependent on the Formation of a FoxO3a/PGC-1α Complex. Antioxid. Redox Signal. 19 (13), 1507–1521. doi:10.1089/ars.2012.4713
Ou, H. C., Hsieh, Y. L., Yang, N. C., Tsai, K. L., Chen, K. L., Tsai, C. S., et al. (2013). Ginkgo Biloba Extract Attenuates oxLDL-Induced Endothelial Dysfunction via an AMPK-dependent Mechanism. J. Appl. Physiol. 114 (2), 274–285. doi:10.1152/japplphysiol.00367.2012
Ou, H. C., Lee, W. J., Lee, I. T., Chiu, T. H., Tsai, K. L., Lin, C. Y., et al. (2009). Ginkgo Biloba Extract Attenuates oxLDL-Induced Oxidative Functional Damages in Endothelial Cells. J. Appl. Physiol. 106 (5), 1674–1685. doi:10.1152/japplphysiol.91415.2008
Ouimet, M., Barrett, T. J., and Fisher, E. A. (2019). HDL and Reverse Cholesterol Transport. Circ. Res. 124 (10), 1505–1518. doi:10.1161/circresaha.119.312617
Ouyang, S., Yao, Y. H., Zhang, Z. M., Liu, J. S., and Xiang, H. (2019). Curcumin Inhibits Hypoxia Inducible Factor-1α-Induced Inflammation and Apoptosis in Macrophages through an ERK Dependent Pathway. Eur. Rev. Med. Pharmacol. Sci. 23 (4), 1816–1825. doi:10.26355/eurrev_201902_17145
Panahi, Y., Ahmadi, Y., Teymouri, M., Johnston, T. P., and Sahebkar, A. (2018). Curcumin as a Potential Candidate for Treating Hyperlipidemia: A Review of Cellular and Metabolic Mechanisms. J. Cel Physiol 233 (1), 141–152. doi:10.1002/jcp.25756
Piazza, S., Pacchetti, B., Fumagalli, M., Bonacina, F., Dell'Agli, M., and Sangiovanni, E. (2019). Comparison of Two Ginkgo Biloba L. Extracts on Oxidative Stress and Inflammation Markers in Human Endothelial Cells. Mediators Inflamm., 6173893. doi:10.1155/2019/6173893
Pu, Y., Zhang, H., Wang, P., Zhao, Y., Li, Q., Wei, X., et al. (2013). Dietary Curcumin Ameliorates Aging-Related Cerebrovascular Dysfunction through the AMPK/uncoupling Protein 2 Pathway. Cel Physiol Biochem 32 (5), 1167–1177. doi:10.1159/000354516
Qiao, Y., Zhang, P. J., Lu, X. T., Sun, W. W., Liu, G. L., Ren, M., et al. (2015). Panax Notoginseng Saponins Inhibits Atherosclerotic Plaque Angiogenesis by Down-Regulating Vascular Endothelial Growth Factor and Nicotinamide Adenine Dinucleotide Phosphate Oxidase Subunit 4 Expression. Chin. J. Integr. Med. 21 (4), 259–265. doi:10.1007/s11655-014-1832-4
Qin, M., Luo, Y., Lu, S., Sun, J., Yang, K., Sun, G., et al. (2017). Ginsenoside F1 Ameliorates Endothelial Cell Inflammatory Injury and Prevents Atherosclerosis in Mice through A20-Mediated Suppression of NF-kB Signaling. Front. Pharmacol. 8, 953. doi:10.3389/fphar.2017.00953
Quan, Li., Zhang, Xuexin., and Liu, Yanjun. (2019). Clinical Observation of Huatan Quzhuo Prescription in the Treatment of Carotid Atherosclerosis Plaque with Spleen Deficiency and Phlegm Turbidity Repression Type. Hebei J. Traditional Chin. Med. 41 (01), 42–46. doi:10.3969/j.issn.1002-2619.2019.01.009
Ren, J., Fu, L., Nile, S. H., Zhang, J., and Kai, G. (2019). Salvia Miltiorrhiza in Treating Cardiovascular Diseases: A Review on its Pharmacological and Clinical Applications. Front. Pharmacol. 10, 753. doi:10.3389/fphar.2019.00753
Ren, Y., Tao, S., Zheng, S., Zhao, M., Zhu, Y., Yang, J., et al. (2016). Salvianolic Acid B Improves Vascular Endothelial Function in Diabetic Rats with Blood Glucose Fluctuations via Suppression of Endothelial Cell Apoptosis. Eur. J. Pharmacol. 791, 308–315. doi:10.1016/j.ejphar.2016.09.014
Rivera, D., Allkin, R., Obon, C., Alcaraz, F., Verpoorte, R., and Heinrich, M. (2014). What Is in a Name? the Need for Accurate Scientific Nomenclature for Plants. J. Ethnopharmacol 152 (3), 393–402. doi:10.1016/j.jep.2013.12.022
Saji, S., Asha, S., Svenia, P. J., Ratheesh, M., Sheethal, S., Sandya, S., et al. (2018). Curcumin-galactomannoside Complex Inhibits Pathogenesis in Ox-LDL-Challenged Human Peripheral Blood Mononuclear Cells. Inflammopharmacology 26 (5), 1273–1282. doi:10.1007/s10787-018-0474-0
Sarna, L. K., Wu, N., Hwang, S. Y., Siow, Y. L., and O, K. (2010). Berberine Inhibits NADPH Oxidase Mediated Superoxide Anion Production in Macrophages. Can. J. Physiol. Pharmacol. 88 (3), 369–378. doi:10.1139/y09-136
Schürmann, C., Rezende, F., Kruse, C., Yasar, Y., Löwe, O., Fork, C., et al. (2015). The NADPH Oxidase Nox4 Has Anti-atherosclerotic Functions. Eur. Heart J. 36 (48), 3447–3456. doi:10.1093/eurheartj/ehv460
Shen, Y., Ward, N. C., Hodgson, J. M., Puddey, I. B., Wang, Y., Zhang, D., et al. (2013). Dietary Quercetin Attenuates Oxidant-Induced Endothelial Dysfunction and Atherosclerosis in Apolipoprotein E Knockout Mice Fed a High-Fat Diet: a Critical Role for Heme Oxygenase-1. Free Radic. Biol. Med. 65, 908–915. doi:10.1016/j.freeradbiomed.2013.08.185
Shi, J., Deng, H., and Zhang, M. (2017). Curcumin Pretreatment Protects against PM2.5-induced Oxidized Low-Density Lipoprotein-Mediated Oxidative Stress and Inflammation in Human Microvascular Endothelial Cells. Mol. Med. Rep. 16 (3), 2588–2594. doi:10.3892/mmr.2017.6935
Shibai, Li., Liu, Jun., and Wu, Zhisheng. (2019). Clinical Evaluation on Ginkgo Leaf Capsules Combined with Nicorandil in the Treatment of Angina Pectoris of Coronary Heart Disease. China Pharmaceuticals 28 (11), 77–80. doi:10.3969/j.issn.1006-4931.2019.11.024
Sies, H. (2015). Oxidative Stress: a Concept in Redox Biology and Medicine. Redox Biol. 4, 180–183. doi:10.1016/j.redox.2015.01.002
Soltani, B., Bodaghabadi, N., Ghaemi, N., and Sadeghizadeh, M. (2017). Radiation-induced Surge of Macrophage Foam Cell Formation, Oxidative Damage, and Cytokine Release Is Attenuated by a Nanoformulation of Curcumin. Int. J. Radiat. Biol. 93 (3), 303–314. doi:10.1080/09553002.2016.1242817
Song, P., Fang, Z., Wang, H., Cai, Y., Rahimi, K., Zhu, Y., et al. (2020). Global and Regional Prevalence, Burden, and Risk Factors for Carotid Atherosclerosis: a Systematic Review, Meta-Analysis, and Modelling Study. Lancet Glob. Health 8 (5), e721–e729. doi:10.1016/s2214-109x(20)30117-0
Stephens, E. H., Saltarrelli, J. G., Baggett, L. S., Nandi, I., Kuo, J. J., Davis, A. R., et al. (2011). Differential Proteoglycan and Hyaluronan Distribution in Calcified Aortic Valves. Cardiovasc. Pathol. 20 (6), 334–342. doi:10.1016/j.carpath.2010.10.002
Stromsnes, K., Mas-Bargues, C., Gambini, J., and Gimeno-Mallench, L. (2020). Protective Effects of Polyphenols Present in Mediterranean Diet on Endothelial Dysfunction. Oxid Med. Cel Longev 2020, 2097096. doi:10.1155/2020/2097096
Sun, Y., Liu, Y., and Chen, K. (2016). Roles and Mechanisms of Ginsenoside in Cardiovascular Diseases: Progress and Perspectives. Sci. China Life Sci. 59 (3), 292–298. doi:10.1007/s11427-016-5007-8
Szewczuk, L. M., Forti, L., Stivala, L. A., and Penning, T. M. (2004). Resveratrol Is a Peroxidase-Mediated Inactivator of COX-1 but Not COX-2: a Mechanistic Approach to the Design of COX-1 Selective Agents. J. Biol. Chem. 279 (21), 22727–22737. doi:10.1074/jbc.M314302200
Tabas, I., García-Cardeña, G., and Owens, G. K. (2015). Recent Insights into the Cellular Biology of Atherosclerosis. J. Cel Biol 209 (1), 13–22. doi:10.1083/jcb.201412052
Tabas, I., Williams, K. J., and Borén, J. (2007). Subendothelial Lipoprotein Retention as the Initiating Process in Atherosclerosis: Update and Therapeutic Implications. Circulation 116 (16), 1832–1844. doi:10.1161/circulationaha.106.676890
Tan, W., Wang, Y., Wang, K., Wang, S., Liu, J., Qin, X., et al. (2020). Improvement of Endothelial Dysfunction of Berberine in Atherosclerotic Mice and Mechanism Exploring through TMT-Based Proteomics. Oxidative Med. Cell. longevity 2020, 8683404. doi:10.1155/2020/8683404
Tang, F. T., Cao, Y., Wang, T. Q., Wang, L. J., Guo, J., Zhou, X. S., et al. (2011). Tanshinone IIA Attenuates Atherosclerosis in ApoE(-/-) Mice through Down-Regulation of Scavenger Receptor Expression. Eur. J. Pharmacol. 650 (1), 275–284. doi:10.1016/j.ejphar.2010.07.038
Tardif, J. C., Grégoire, J., Schwartz, L., Title, L., Laramée, L., Reeves, F., et al. (2003). Effects of AGI-1067 and Probucol after Percutaneous Coronary Interventions. Circulation 107 (4), 552–558. doi:10.1161/01.cir.0000047525.58618.3c
Tardif, J. C., McMurray, J. J., Klug, E., Small, R., Schumi, J., Choi, J., et al. (2008). Effects of Succinobucol (AGI-1067) after an Acute Coronary Syndrome: a Randomised, Double-Blind, Placebo-Controlled Trial. Lancet 371 (9626), 1761–1768. doi:10.1016/s0140-6736(08)60763-1
Tian, J., Liu, Y., and Chen, K. (2017). Ginkgo Biloba Extract in Vascular Protection: Molecular Mechanisms and Clinical Applications. Curr. Vasc. Pharmacol. 15 (6), 532–548. doi:10.2174/1570161115666170713095545
Tong, L., Zhao, M. J., Han, X. W., Deng, Y., Zhao, Y. Z., Yang, T., et al. (2018). [Huotan Jiedu Tongluo Decoction Alleviates Early Atherosclerosis of Rabbits by Inhibiting eNOS Uncoupling Pathway]. Zhongguo Zhong yao Za Zhi = Zhongguo zhongyao zazhi = China J. Chin. materia Med. 43 (21).
Tonghua, Li. (2019). “Ginkgo Biloba Extract (EGb761) Inhibiting Smoothmuscle Foam Cell Formation and the Underlyingmechanisms,” in Doctoral Dissertation (Cnki: PLA Air Force Military Medical University).
Treviño-Saldaña, N., and García-Rivas, G. (2017). Regulation of Sirtuin-Mediated Protein Deacetylation by Cardioprotective Phytochemicals. Oxid Med. Cel Longev 2017, 1750306. doi:10.1155/2017/1750306
Tsai, H. Y., Huang, P. H., Lin, F. Y., Chen, J. S., Lin, S. J., and Chen, J. W. (2013). Ginkgo Biloba Extract Reduces High-Glucose-Induced Endothelial Reactive Oxygen Species Generation and Cell Adhesion Molecule Expression by Enhancing HO-1 Expression via Akt/eNOS and P38 MAP Kinase Pathways. Eur. J. Pharm. Sci. : official J. Eur. Fed. Pharm. Sci. 48, 803–811. doi:10.1016/j.ejps.2013.01.002
Tyrrell, D. J., and Goldstein, D. R. (2021). Ageing and Atherosclerosis: Vascular Intrinsic and Extrinsic Factors and Potential Role of IL-6. Nat. Rev. Cardiol. 18 (1), 58–68. doi:10.1038/s41569-020-0431-7
van Beek, T. A., and Montoro, P. (2009). Chemical Analysis and Quality Control of Ginkgo Biloba Leaves, Extracts, and Phytopharmaceuticals. J. Chromatogr. A 1216 (11), 2002–2032. doi:10.1016/j.chroma.2009.01.013
Vivancos, M., and Moreno, J. J. (2008). Effect of Resveratrol, Tyrosol and Beta-Sitosterol on Oxidised Low-Density Lipoprotein-Stimulated Oxidative Stress, Arachidonic Acid Release and Prostaglandin E2 Synthesis by RAW 264.7 Macrophages. Br. J. Nutr. 99 (6), 1199–207. doi:10.1017/s0007114507876203
Wang, G., Liu, Z., Li, M., Li, Y., Alvi, S. S., Ansari, I. A., et al. (2019). Ginkgolide B Mediated Alleviation of Inflammatory Cascades and Altered Lipid Metabolism in HUVECs via Targeting PCSK-9 Expression and Functionality. Biomed. Research International 2019, 7284767. doi:10.1155/2019/7284767
Wang, Q., Zhang, M., Liang, B., Shirwany, N., Zhu, Y., and Zou, M. H. (2011). Activation of AMP-Activated Protein Kinase Is Required for Berberine-Induced Reduction of Atherosclerosis in Mice: the Role of Uncoupling Protein 2. PLoS One 6 (9), e25436. doi:10.1371/journal.pone.0025436
Wiciński, M., Socha, M., Walczak, M., Wódkiewicz, E., Malinowski, B., Rewerski, S., et al. (2018). Beneficial Effects of Resveratrol Administration-Focus on Potential Biochemical Mechanisms in Cardiovascular Conditions. Nutrients 10 (11). doi:10.3390/nu10111813
Willeit, J., Kiechl, S., Weimer, T., Mair, A., Santer, P., Wiedermann, C. J., et al. (2003). Marburg I Polymorphism of Factor VII-Aactivating Protease: a Prominent Risk Predictor of Carotid Stenosis. Circulation 107 (5), 667–670. doi:10.1161/01.cir.0000055189.18831.b1
Wu, M., Wang, J., and Liu, L. T. (2010). Advance of Studies on Anti-atherosclerosis Mechanism of Berberine. Chin. J. Integr. Med. 16 (2), 188–92. doi:10.1007/s11655-010-0188-7
Xiang, Y., Ye, S., Cai, C., Chen, J., Zhao, X., Zhu, N., et al. (2018). Salvianolic Acid a Attenuates Limb Ischemia/reperfusion Injury in Skeletal Muscle of Rats. Biomed. Pharmacother. 97, 551–556. doi:10.1016/j.biopha.2017.10.094
Xiao, L., Liu, L., Guo, X., Zhang, S., Wang, J., Zhou, F., et al. (2017). Quercetin Attenuates High Fat Diet-Induced Atherosclerosis in Apolipoprotein E Knockout Mice: A Critical Role of NADPH Oxidase. Food Chem. Toxicol. 105, 22–33. doi:10.1016/j.fct.2017.03.048
Xibin, Dou., Tang, Hanqing., Zhao, Yufeng., Zhao, Qiuhua., Li, Keming., and Wang, Luyao. (2019). Effects of Xuefuzhuyu Decoction on Blood Fat and Myocardial Enzymes in the Coronary Heart Disease Rat Model. Guangdong Med. J. 40 (06), 767–771. doi:10.13820/j.cnki.gdyx.20185097
Xing, S. S., Li, J., Chen, L., Yang, Y. F., He, P. L., Li, J., et al. (2018). Salidroside Attenuates Endothelial Cellular Senescence via Decreasing the Expression of Inflammatory Cytokines and Increasing the Expression of SIRT3. Mech. Ageing Dev. 175, 1–6. doi:10.1016/j.mad.2017.12.005
Xing, S., Yang, X., Li, W., Bian, F., Wu, D., Chi, J., et al. (2014). Salidroside Stimulates Mitochondrial Biogenesis and Protects against H₂O₂-induced Endothelial Dysfunction. Oxid Med. Cel Longev 2014, 904834. doi:10.1155/2014/904834
Xuan, Y., Gao, Y., Huang, H., Wang, X., Cai, Y., and Luan, Q. X. (2017). Tanshinone IIA Attenuates Atherosclerosis in Apolipoprotein E Knockout Mice Infected with Porphyromonas Gingivalis. Inflammation 40 (5), 1631–1642. doi:10.1007/s10753-017-0603-8
Xue, F., Nie, X., Shi, J., Liu, Q., Wang, Z., Li, X., et al. (2017). Quercetin Inhibits LPS-Induced Inflammation and Ox-LDL-Induced Lipid Deposition. Front. Pharmacol. 8, 40. doi:10.3389/fphar.2017.00040
Yang, J., Zhou, X., Zeng, X., Hu, O., Yi, L., and Mi, M. (2019). Resveratrol Attenuates Oxidative Injury in Human Umbilical Vein Endothelial Cells through Regulating Mitochondrial Fusion via TyrRS-PARP1 Pathway. Nutr. Metab. (Lond) 16, 9. doi:10.1186/s12986-019-0338-7
Yang, X. J., Liu, F., Feng, N., Ding, X. S., Chen, Y., Zhu, S. X., et al. (2020a). Berberine Attenuates Cholesterol Accumulation in Macrophage Foam Cells by Suppressing AP-1 Activity and Activation of the Nrf2/HO-1 Pathway. J. Cardiovasc. Pharmacol. 75 (1), 45–53. doi:10.1097/fjc.0000000000000769
Yang, Y., Wang, J., Guo, S., Pourteymour, S., Xu, Q., Gong, J., et al. (2020b). Non-lethal Sonodynamic Therapy Facilitates the M1-To-M2 Transition in Advanced Atherosclerotic Plaques via Activating the ROS-AMPK-mTORC1-Autophagy Pathway. Redox Biol. 32, 101501. doi:10.1016/j.redox.2020.101501
Yang, Y., Pei, K., Zhang, Q., Wang, D., Feng, H., Du, Z., et al. (2020c). Salvianolic Acid B Ameliorates Atherosclerosis via Inhibiting YAP/TAZ/JNK Signaling Pathway in Endothelial Cells and Pericytes. Biochim. Biophys. Acta Mol. Cel Biol Lipids 1865 (10), 158779. doi:10.1016/j.bbalip.2020.158779
Yansheng, K., Liu, J., Zhang, W., Wang, T., Wang, X., Wen, L., et al. (2020). Effect of Compound Danshen Granules, Capsules, Tablets, and Drop Pills on Curative Effect, Inflammatory Factors, and Oxidative Stress Indexes of Angina Pectoris Patients with Coronary Heart Disease. Drug Eval. Res. 43 (02), 287–292. doi:10.7501/j.issn.1674-6376.2020.02.021
Yi, L., Jin, X., Chen, C. Y., Fu, Y. J., Zhang, T., Chang, H., et al. (2011). Chemical Structures of 4-Oxo-Flavonoids in Relation to Inhibition of Oxidized Low-Density Lipoprotein (LDL)-induced Vascular Endothelial Dysfunction. Int. J. Mol. Sci. 12 (9), 5471–5489. doi:10.3390/ijms12095471
Yonggang, Li. (2020). Effects of Tongqiao Huoxue Decoction on Oxidative Stress and Cerebral Blood Flow in Patients with Acute Ischemic Stroke. Hunan J. Traditional Chin. Med. 36 (03), 36–37. doi:10.16808/j.cnki.issn1003-7705.2020.03.014
Yu, X. H., Zhang, D. W., Zheng, X. L., and Tang, C. K. (2019). Cholesterol Transport System: An Integrated Cholesterol Transport Model Involved in Atherosclerosis. Prog. lipid Res. 73, 65–91. doi:10.1016/j.plipres.2018.12.002
Yu, Zhang., Cheng, Saibo., Zhao, Dandan., Su, Zhijie., Zhang, Lei., Xu, Yuling., et al. (2016). Dingxin Recipe Attenuates Atherosclerosis by Up-Regulating PTEN Expression in Apo E Knockout Mice. Chin. J. Exp. Traditional Med. Formulae 22 (24), 111–115. doi:10.13422/j.cnki.syfjx.2016240111
Yufeng, Qian., Fang, Cunming., and Chen, Guoyou. (2019). Effects of Shexiang Baoxin Pills on Serum Cyclophilin A and Oxidative Stress in Patients with Coronary Heart Disease after PCI. Mod. J. Integrated Traditional Chin. West. Med. 28 (25), 2822–2825. doi:10.3969/j.issn.1008-8849.2019.25.024
Zhang, M, K. Nakamura. S. Kageyama., AO, Lawal., Gong, K. W., Bhetraratana, M., Fujii, T., Sulaiman, D., et al. (2018). Myeloid HO-1 Modulates Macrophage Polarization and Protects against Ischemia-Reperfusion Injury. JCI insight 3 (19). doi:10.1172/jci.insight.120596
Zhang, X., Liu, J., Pang, X., Zhao, J., and Xu, S. (2020a). Curcumin Suppresses Aldosterone-Induced CRP Generation in Rat Vascular Smooth Muscle Cells via Interfering with the ROS-Erk1/2 Signaling Pathway. Evid. Based Complement. Alternat Med. 2020, 3245653. doi:10.1155/2020/3245653
Zhang, Y., Murugesan, P., Huang, K., and Cai, H. (2020b). NADPH Oxidases and Oxidase Crosstalk in Cardiovascular Diseases: Novel Therapeutic Targets. Nat. Rev. Cardiol. 17 (3), 170–194. doi:10.1038/s41569-019-0260-8
Zhanxia, H., Liang, S., Lu, B., and Ji, L. (2019). Effect of PI3K-Mediated Nrf2 Phosphorylated Activation in Quercetin in Inhibiting Clivorine-Induced Hepatotoxicity. Chin. J. Exp. Traditional Med. Formulae 25 (05), 112–118. doi:10.13422/j.cnki.syfjx.20190423
Zhao, D., Sun, X., Lv, S., Sun, M., Guo, H., Zhai, Y., et al. (2019). Salidroside Attenuates Oxidized Low-Density Lipoprotein-Induced Endothelial Cell Injury via Promotion of the AMPK/SIRT1 Pathway. Int. J. Mol. Med. 43 (6), 2279–2290. doi:10.3892/ijmm.2019.4153
Zhao, J., Liu, H., Xu, B., Peng, J., Xing, Y., Tang, W., et al. (2020a). The Role of Xuefu Zhuyu Decoction in Prevention of Contrast-Induced Nephropathy after Percutaneous Coronary Intervention. Evid. Based Complement. Alternat Med. 2020, 5419016. doi:10.1155/2020/5419016
Zhao, Y., Qu, H., Wang, Y., Xiao, W., Zhang, Y., and Shi, D. (2020b). Small Rodent Models of Atherosclerosis. Biomed. Pharmacother. 129, 110426. doi:10.1016/j.biopha.2020.110426
Zheng, B., Yang, L., Wen, C., Huang, X., Xu, C., Lee, K. H., et al. (2016). Curcumin Analog L3 Alleviates Diabetic Atherosclerosis by Multiple Effects. Eur. J. Pharmacol. 775, 22–34. doi:10.1016/j.ejphar.2016.02.016
Zhixin, D., Gu, X., and Li, J. (2019). Clinical Study on Modified Buyang Huanwu Tang Combined with Routine Western Medicine Therapy for Angina Pectoris. Xin Zhong Yi 51 (06), 93–97. doi:10.13457/j.cnki.jncm.2019.06.028
Zhong, D-y., Li, H-y., Lan, L., Ma, R-m., Jiang, C-t., Ding-xiang, L., et al. (2020). Effect of Tongqiao Huoxue Decoction Combined with Western Medicine on Ischemic Stroke: A Systematic Review. Evidence-Based Complement. Altern. Med. 2020, 8877998. doi:10.1155/2020/8877998
Zhou, P., Lu, S., Luo, Y., Wang, S., Yang, K., Zhai, Y., et al. (2017). Attenuation of TNF-α-Induced Inflammatory Injury in Endothelial Cells by Ginsenoside Rb1 via Inhibiting NF-Κb, JNK and P38 Signaling Pathways. Front. Pharmacol. 8, 464. doi:10.3389/fphar.2017.00464
Zhou, X., Yang, J., Zhou, M., Zhang, Y., Liu, Y., Hou, P., et al. (2019). Resveratrol Attenuates Endothelial Oxidative Injury by Inducing Autophagy via the Activation of Transcription Factor EB. Nutr. Metab. (Lond) 16, 42. doi:10.1186/s12986-019-0371-6
Zhu, H., Chen, Z., Ma, Z., Tan, H., Xiao, C., Tang, X., et al. (2017a). Tanshinone IIA Protects Endothelial Cells from H₂O₂-Induced Injuries via PXR Activation. Biomol. Ther. (Seoul) 25 (6), 599–608. doi:10.4062/biomolther.2016.179
Zhu, L., Liu, Y., Liu, Y., Xu, H., Wang, S., Liu, Y., et al. (2019a). Anti-inflammatory and Antioxidative Effects of Dan-Lou Tablets in the Treatment of Coronary Heart Disease Revealed by Metabolomics Integrated with Molecular Mechanism Studies. J. ethnopharmacology 240, 111911. doi:10.1016/j.jep.2019.111911
Zhu, X., Yue, H., Guo, X., Yang, J., Liu, J., Liu, J., et al. (2017b). The Preconditioning of Berberine Suppresses Hydrogen Peroxide-Induced Premature Senescence via Regulation of Sirtuin 1. Oxid Med. Cel Longev 2017, 2391820. doi:10.1155/2017/2391820
Zhu, Y., Zhang, Y., Huang, X., Xie, Y., Qu, Y., Long, H., et al. (2019b). Z-ligustilide Protects Vascular Endothelial Cells from Oxidative Stress and Rescues High Fat Diet-Induced Atherosclerosis by Activating Multiple NRF2 Downstream Genes. Atherosclerosis 284, 110–120. doi:10.1016/j.atherosclerosis.2019.02.010
Zhu, Y., Zhang, Y. J., Liu, W. W., Shi, A. W., and Gu, N. (2016). Salidroside Suppresses HUVECs Cell Injury Induced by Oxidative Stress through Activating the Nrf2 Signaling Pathway. Molecules 21 (8). doi:10.3390/molecules21081033
Zhu, Z., Li, J., and Zhang, X. (2019c). Salidroside Protects against Ox-LDL-Induced Endothelial Injury by Enhancing Autophagy Mediated by SIRT1-FoxO1 Pathway. BMC Complement. Altern. Med. 19 (1), 111. doi:10.1186/s12906-019-2526-4
Keywords: oxidative stress, atherosclerosis, anti-oxidant treatment, traditional Chinese medicine, Chinese herbal medicines
Citation: Song L, Zhang J, Lai R, Li Q, Ju J and Xu H (2021) Chinese Herbal Medicines and Active Metabolites: Potential Antioxidant Treatments for Atherosclerosis. Front. Pharmacol. 12:675999. doi: 10.3389/fphar.2021.675999
Received: 04 March 2021; Accepted: 16 April 2021;
Published: 13 May 2021.
Edited by:
Ling Zhang, Zhejiang Chinese Medical University, ChinaReviewed by:
Mingbao Lin, Chinese Academy of Medical Sciences and Peking Union Medical College, ChinaZhenzhong Yang, Zhejiang University, China
Copyright © 2021 Song, Zhang, Lai, Li, Ju and Xu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hao Xu, eHVoYW90Y21AaG90bWFpbC5jb20=
 Luxia Song
Luxia Song Jie Zhang
Jie Zhang Runmin Lai
Runmin Lai Qiuyi Li
Qiuyi Li Jianqing Ju
Jianqing Ju Hao Xu
Hao Xu