
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Pharmacol. , 26 May 2021
Sec. Drugs Outcomes Research and Policies
Volume 12 - 2021 | https://doi.org/10.3389/fphar.2021.655836
Background: Immunosuppressive medication (IM) nonadherence is associated with poor transplant outcomes. Therefore, it is of great importance to identify predictive factors with IM nonadherence. We aimed to improve the predicted capacity of the theory of planned behavior (TPB) by adding health belief model’s (HBM) variables in renal transplant patients (RTPs).
Methods: This cross-sectional study distributed questionnaires to patients who had undergone renal transplant and follow-up regularly in the transplant center of Third Xiangya Hospital in China. The self-developed questionnaire collected data in three aspects: general data questionnaire, TPB, HBM-specific questionnaire, and Basel Assessment of Adherence to Immunosuppressive Medications scale.
Results: A total of 1,357 of 1,480 patients completed the survey, with a participation rate of 91.69% and IM nonadherence rate of 33.53%. The marital status, household income, preoperative drinking history, the time after transplantation, and religion showed independent predictive factors with IM nonadherence (p < 0.05). Strikingly, adding HBM variables to the TPB theory model significantly increased its prediction ability to IM nonadherence (52%). Also, HBM manifested the highest coefficient of effect (−0.620). Particularly, perceived barriers and perceived seriousness, the variables of the HBM model, played a vital influence on medication nonadherence (−0.284 and 0.256).
Conclusion: Our study here reveals the first investigation of the combined effects of the TPB and HBM model on IM nonadherence in Chinese RTPs, which could significantly improve the predictive ability of any single model. Meanwhile, future interventions should be conducted to both increase perceived seriousness and reduce perceived barriers for taking IM, which will effectively decrease IM nonadherence rates and improve transplant outcomes.
Since 1954, when the first renal transplant was successfully conducted between twins, a series of sustainable progresses such as refined surgical techniques improved immunosuppressive protocols and optimized perioperative management of transplant patients have been utilized to improve patient and graft survival following the renal transplant (Tonelli et al., 2011). However, the renal transplant community has been now challenged by acute rejection and transplant graft loss because of IM nonadherence (Prihodova et al., 2014). A recent study showed that IM nonadherence could lead to increasing risk of cancer over the long term in renal transplant patients (RTPs) (Yadav et al., 2019). However, research reports indicated that the prevalence rate of IM nonadherence in China ranges from 23.2 to 54.9% in RTPs (Teng et al., 2015; Xia et al., 2019; Liu et al., 2021), which was almost consistent with a worldwide incidence of 20–50% (Germani et al., 2011). Therefore, identifying the predictive factors with IM nonadherence would allow us to evaluate patients’ need for interventions to improve adherence, which could reduce the acute rejection rate and transplant graft loss to improve transplant outcomes. Numerous studies about nonadherence to IM in RTPs have indicated that demographics such as age, gender, working and socioeconomic status, educational level, and marital status were often associated with nonadherence rates (Spivey et al., 2014; Kung et al., 2017).
Several postulated theories or models have been utilized to predict and intervene nonadherence to IM in RTPs. The health belief model (HBM) model consisted of perceived susceptibility, perceived seriousness, perceived benefits, and perceived barriers, which has been widely used in many health-related behaviors (cancer, heart disease, hypertension, and renal transplant recipients) (Brown et al., 2011; Horwood et al., 2015; Zhao et al., 2015; Quast et al., 2016; Yang et al., 2016; Kung et al., 2017). An effective application of the HBM model has been conducted to predict IM nonadherence among RTPs in our transplant center, and our results indicated that perceived seriousness and perceived barriers were closely associated with IM nonadherence (Xia et al., 2019). Also, a recent study indicated that beliefs about medications were more powerful predictors to nonadherence than clinical or sociodemographic factors among patients with multiple sclerosis (Neter et al., 2021). The theory of planned behavior (TPB), as a cognitive model, also exhibited several advantages to predict a wide range of health-related behaviors (Andrew et al., 2016; Li et al., 2019; Caru et al., 2020). The TPB model only consisted of several variables (attitudes, subjective norms, perceived behavioral control, and intentions), which were avoided to include and test so many demographic and clinical factors. The validity of the TPB has been supported by different behavior domains and populations within large samples and applied successfully to predict IM nonadherence into solid organ transplant recipients (Chisholm et al., 2007; Hugon et al., 2014). Nevertheless, so far, all the predicted behavior models were usually tested independently to predict health behaviors, and few models were well suited to identify all the factors that contributed to nonadherence to a prescribed medical regimen as crucial as immunosuppressive therapy and each model had its limitations. For example, Chisholm et al. (2007) reported that the predictive capacity of the TPB could be enhanced by adding other variables such as the past behavior. Our previous study has demonstrated that the HBM could be used to predict health-related behaviors (Xia et al., 2019); however, a combined theory model to predict medication nonadherence has received little attention in RTPs. Therefore, we attempted to add the HBM variable to the TPB model to enhance the predicted power of combining the TPB and HBM model on IM nonadherence in RTPs. To the best of our knowledge, this is the first study to explore the combined effects of the TPB and HBM model on IM nonadherence in Chinese RTPs, and we hope to increase the prediction of the models on IM nonadherence and suggest some interventions to improve the IM nonadherence.
This was a cross-sectional study and analyzed by structural equation modeling. The sample size should be more than 200 or 10 times of the observed variables. In our study, a total of 1,357 RTPs from transplant follow-up outpatient clinic of the Third Xiangya Hospital of Central South University were enrolled within one year from August 2019 to July 2020. The inclusion criteria were carried out as follows: 1. 18 years or older; 2. were able to communicate in Mandarin; 3. functioning renal transplant (not on dialysis); 4. qualified assessment from outpatient physician. The exclusion criteria were as follows: 1. multiple or other organ transplant recipients; 2. diagnosed with severe mental illness or cognitive impairment. All donors were derived from corresponding relatives or patients who died of cardiac diseases (Association Organ Transplantation Society of Chinese Medical, 2013).
When RTPs came for the follow-up visits in the Third Xiangya Hospital, the staff who work in the transplant follow-up outpatient clinic invited them to take part in this study. Patients who were interested in the research received an informed consent form during the consultation with the staff and completed the questionnaire in the lounge of the outpatient clinic under the supervision of the staff. Also, these four questionnaires were filled out in one time and the average time for completing these questionnaires was 25.6 min. After completing the questionnaires, all the participants received a gift (oral medicine box) to appreciate their participation. These completed questionnaires were kept by a special person to avoid information disclosure.
A written informed consent was obtained from all subjects, and this study was approved by the Ethics Committee of The Third Xiangya Hospital Central South University (No:2019-S61). At the same time, all methods were performed in accordance with the ethical guidelines and regulations of the 1975 Declaration of Helsinki.
A total of four questionnaires were used in this study.
Participants’ demographic characteristics were collected by this questionnaire, which included age, gender, BMI, marital status, work, religion, education, household income, transplant-related hospitalization, the time after transplantation, organ source, etc.
The BAASIS was a self-reported questionnaire developed by the Leuven Basel Adherence Research Group (Dobbels et al., 2010) and translated into Chinese in 2016. The previous study indicated that the BAASIS was reliable and valid to evaluate IM nonadherence in transplant recipients (Dobbels et al., 2010; De Bleser et al., 2011; Shemesh et al., 2017). We examined two dimensions of IM nonadherence in our questionnaire: implementation and discontinuation. Implementation was assessed by four questions (dose taking, drug holidays, timing deviation more than 2 h from the prescribed time, and dose reduction); overall IM nonadherence was defined as a “yes” to any of the five questions regarding to implementation or discontinuation in the last four weeks and data analysis was scored dichotomously. The BAASIS score was interpreted as acceptable in terms of reliability and validity, if the Cronbach’s α was greater than or equal to 0.78 (Dobbels et al., 2010; Shemesh et al., 2017).
The researcher developed this study questionnaire based on the Rosenstock’s health belief model and the Chinese version of HBM has been validated in Chinese hypertension patients (Zhao et al., 2015). It constructed perceived susceptibility regarding self-awareness of infection and adverse reactions of the medication (three items); perceived seriousness regarding individual awareness of impact of rejection, infection and other complications, and their survival (four items); perceived benefits of adherence to treatment with IM regarding subjective beliefs whether better adherence lowers the possibility of complications (four items); and perceived barriers to adherence regarding the adverse effects of medication and some living conflicts (four items). Each item on the IM belief questionnaire was structured using a 5-point Likert scale ranging from 1 (strongly disagree) to 5 (strongly agree). As for the perceived barriers, the scaling was opposite the other constructs. The reliability of each questionnaire was tested using Cronbach’s α. The range of Cronbach’s α among Chinese patients was 0.77–0.90 (Zhao et al., 2015).
We adapted the TPB questionnaire initially developed and validated in RTPs by Chisholm et al. (2007) and the Chinese version of TPB has been validated in Chinese RTPs and dialysis patients (Du et al., 2018; Li C. et al., 2019). The questionnaire explored attitudes (twelve items), subjective norms (five items), perceived behavioral control (two items), past behavior (two items), and intentions (two items). Evidence for the reliability and predictive validity of the TPB model have been supported by numerous studies (Andrew et al., 2016; Li A. S. W. et al., 2019; Caru et al., 2020). The reliability of each questionnaire was tested using Cronbach’s α, and the range of Cronbach’s α among the Chinese RTPs was 0.606–0.855 (Du et al., 2018).
All statistical analyses were performed using the SPSS version 20.0 (SPSS Inc., Chicago, IL, United States). The sociodemographic characteristics were analyzed using descriptive statistics. The categorical variables were summarized by numbers or percentages. Relationships among sociodemographic characteristics, IM beliefs, and IM nonadherence were analyzed using the chi-square test and binary logistic regression analysis. The TPB structural equation was run by Amos 21.0 (Analysis of Moment Structures, IBM, Armonk, NY, United States). Spearman’s rank correlation coefficient was employed to measure associations between categorical TPB and HBM variables and medication nonadherence. A p value <0.05 (two-tailed) was considered statistically significance.
In this study, a total of 1,480 RTPs in the follow-up outpatient clinic were invited and 1,357 valid questionnaires were enrolled for further study (Figure 1). The sociodemographic characteristics of the participants are summarized in Table 1. The mean age and BMI were 41.25 years and 22.75 kg/m2, respectively. 67.80% of the participants were male, 61.02% of them were married, 48.71% of them had a higher education level than undergraduate, and 93.81% of them lacked religion. Meanwhile, we found that only 42.08% of them were still working. Approximately 91.82% of patients received grafts from deceased donors. About half of the participants had preoperative drinking history and 56.67% of them were hospitalized after transplantation.
The overall IM nonadherence rate was 33.53% based on the BAASIS assessment. In detail, our results indicated that 31.10% of RTPs happened to the item of “In the last four weeks the IM was taken more than 2 h before or after the prescribed dosing time,” which was the most commonly occurred. Meanwhile, we found that 19.81% of RTPs missed one dose and 10.02% of RTPs skipped two or more doses. The percentage of RTPs who altered the prescribed amount and completely stopped the intake of IM was 7.15 and 1.47%, respectively (Table 2).
Table 3 showed the univariate analyses of the relationship between all sociodemographic variables and IM nonadherence. All sociodemographic variables, except for transplant-related hospitalization, manifested statistical significance. Furthermore, our logistic regression analysis revealed that a variety of variables, such as marital status, religion household income, preoperative drinking history, posttransplant time, each dimension of HBM, attitudes, past behavior, perceived behavioral control, and intentions, were independent predictive nonadherence factors to IM (Table 4).
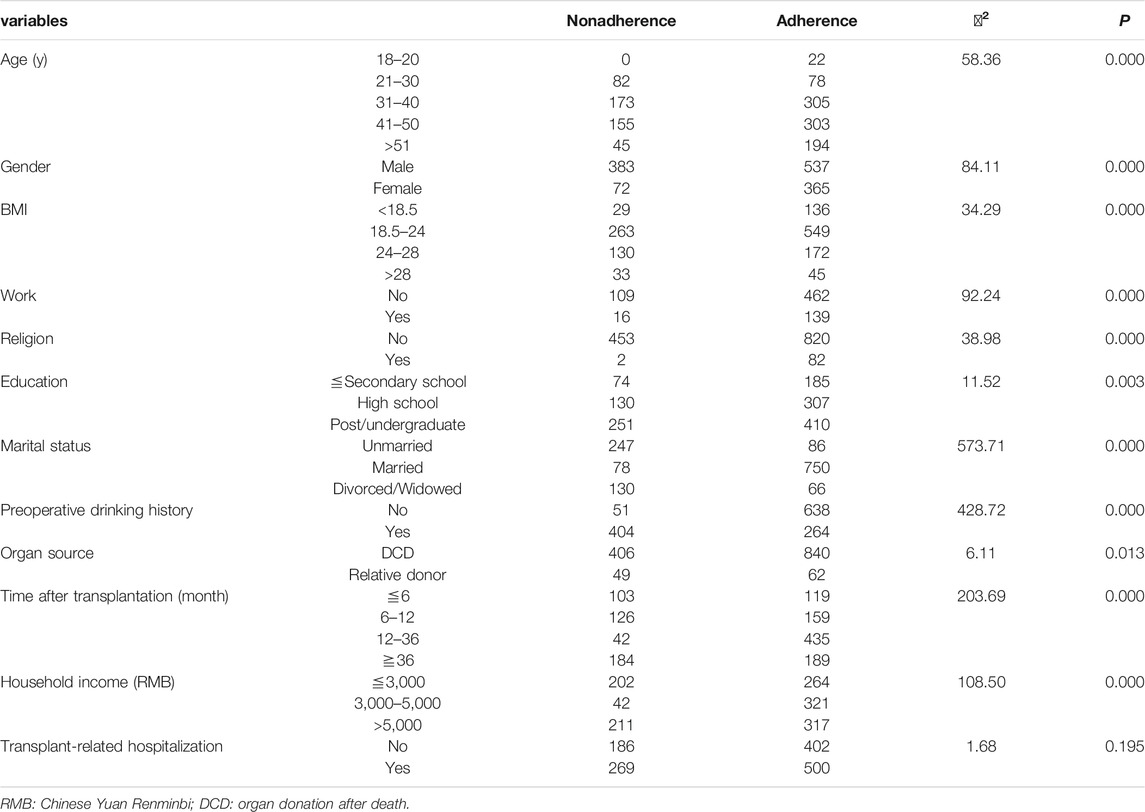
TABLE 3. Univariate analysis of the association between sociodemographic characteristics and IM adherence among RTPs.
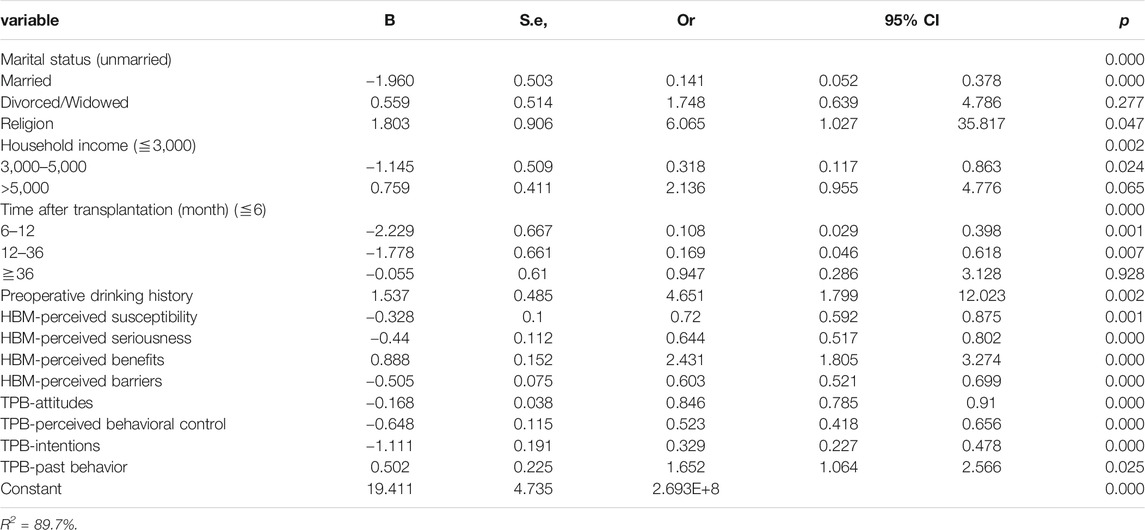
TABLE 4. Binary logistic regression analysis of the association between sociodemographic characteristics and IM adherence among RTPs.
In our study, each dimension of TPB and HBM questionnaires were significantly correlated with IM nonadherence (p < 0.05), but the dimension of HBM had a higher interrelationship to IM nonadherence than that of TPB (Table 5). In addition, perceived barriers to adherence exhibited significantly negative correlation with adherence (r = −0.743, p < 0.01).
In the current study, TPB alone, as a superior cognitive model, only explained 2% of variance in nonadherence to IM. However, combining the TPB and HBM model could explain 52% of variance in nonadherence to IM (Figure 2). Therefore, it was clear that incorporation of the HBM model was made it possible to improve the prediction capacity of the TPB model. In detail, perceived barriers, attitudes, and HBM contributed to the overall effect to IM nonadherence. HBM had the highest coefficient of effect (−0.620) and perceived barriers was second (0.284). Perceived seriousness and intentions influenced IM nonadherence directly with coefficient of effect 0.256 and −0.126. Past behavior (−0.044), subjective norms (−0.035), and perceived behavioral control (−0.009) influenced IM nonadherence indirectly via mediators of intentions (Table 6). Also, the model fitted the data well, and the CMIN/DF, RMSEA, GFI, CFI, and IFI values of the combined model were 2.469, 0.033, 0.995, 0.992, and 0.992, respectively.
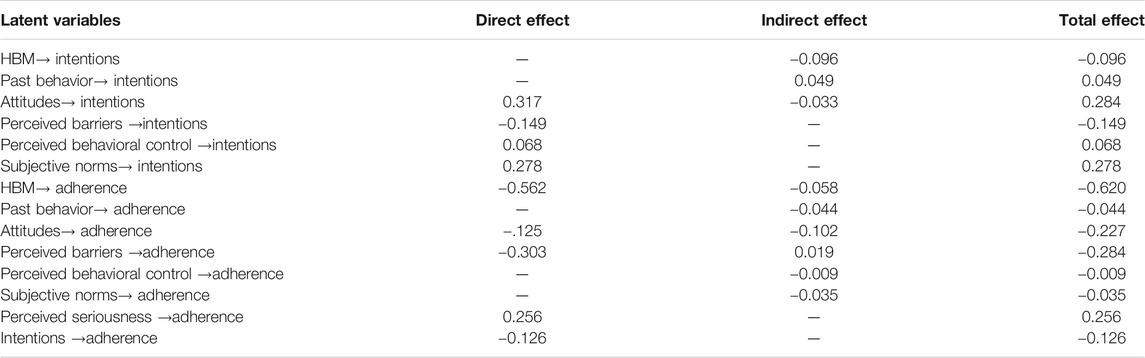
TABLE 6. Effect of each latent variable of the structural equation model on medication intentions and adherence.
Our article initiated the first study of the incorporation between TBP variables and the HBM model in IM nonadherence in Chinese RTPs. Also, the purpose of our work was to conduct the combined model to determine the barriers to IM nonadherence and provide some new insights on how to improve the IM adherence among the RTPs.
In the current study, the IM nonadherence of the patients was 33.53%, which was in accordance with previously reported 5–50% range of nonadherence rate in renal transplantation (Leendertse et al., 2008; Germani et al., 2011). Forgetfulness was one of the major reasons for nonadherence to medications in other clinical settings such as HIV (Morowatisharifabad et al., 2019). Better drug reminder also effectively reduced the rate of nonadherence.
The binary logistic regression analysis suggested that several sociodemographic characteristics such as marital status, household income, preoperative drinking history, the time after transplantation, and religion were independent predictive factors of IM nonadherence. Our study indicated that distinct marital statuses exhibit different capacity of IM nonadherence; married recipients were more likely to adhere to IM than to single or divorced recipients. Additionally, findings from other studies have revealed that the family member–based supervised therapy used in patients with hypertension and type 2 diabetes may have positive effects on patient IM nonadherence (Mayberry and Osborn, 2012; Huang et al., 2014; Shen et al., 2017).
Meanwhile, family income had negative effect on IM nonadherence. Although a Brazilian study reported that higher family income was the only factor that was associated with immunosuppressive nonadherence because of lower income recipients benefiting from better access to care and coverage of health-care costs after transplantation (Marsicano et al., 2015), higher family income could support transplant recipients to pay for their IM, check the IM concentration, and improve the quality of life in China. Also, the life quality manifested a direct effect on medication adherence in Asian RTPs (Ganjali et al., 2019). In addition, religion issues also displayed a considerable influence on positive attitudes toward transplantation (Messina, 2015; Kobus et al., 2016). Religions like Christianity, Islam, Judaism, Buddhism, or other denominations provided guidance and principles for their behavior and thinking in these areas. Therefore, the recipients with religions may have some special etiquettes to limit the use of IM.
Moreover, our result showed that the recipients within half to one year were more likely adherent to IM. Interestingly, the recipients with more than three years did not show significant correlation with adherence to IM. Many studies reported that RTPs believed their allografts would become relatively histocompatible over a longer time (Chisholm et al., 2007; Zhao et al., 2017). In the present study, one of the plausible reasons was that the patients were more appreciative of their allografts and cautious in the early postoperation. Also, the more the time passes, the less the appreciation they have. Meanwhile, doctor’s advices and patients’ positive attitudes about the usage of immunosuppressive drugs for allograft might be diluted when time passes.
Finally, RTPs with preoperative drinking history were prone to IM nonadherence and studies in alcoholism have highlighted the impairments of affecting episodic memory as well as semantic and cognitive procedural learning (Pitel et al., 2007; Le Berre et al., 2010; Noël et al., 2012; Le Berre et al., 2017). So patients with preoperative drinking history tend to forget to take IM. From the above results, important strategies for intervention are needed to be utilized to minimize the barriers and improve the adherence to IM.
In the present study, TPB only explained 2% of variance in adherence to IM. Based on our previous empirical and theoretical work (Xia et al., 2019), IM beliefs were closely associated with IM nonadherence in Chinese RTPs. Our result showed that combining the TPB and HBM model could explain 52% of variance in IM adherence as well as all variables except for the subjective norms were independent predictive factors of IM nonadherence according to the logistic analysis. Several studies have noted that due to variations in the behavior under investigation, it should not be expected that all TPB factors (attitudes, subjective norms, and perceived behavioral control) will always be significant and stronger support for some components of the TPB than others, with subjective norms often emerging as the weakest predictor (Chisholm et al., 2007). Our results indicated that though the small items of the TPB model showed some advantages in predicting a wide range of health-related behaviors, it did not exhibit superiority in our large sample study. Based on our previous empirical and theoretical work (Xia et al., 2019), we integrated the HBM variables into the TPB structural equation model and found that the combined model has the ability to improve the predictive capacity of IM nonadherence than that in any single model. Therefore, we proposed that the combination of TPB and HBM exhibits more advantages in predicting IM nonadherence in studies with large samples.
In the structural equation model, we discovered that attitudes act as a salient predictor to IM intentions (0.284), both directly and indirectly. Chisholm MA et al reported that those RTPs who were particularly at risk might have a history of nonadherence to medical advice, especially when they had negative attitude about IM adherence (Chisholm et al., 2007; Hugon et al., 2014). An individual's perception of the "benefits and harms" of the target behavior is crucial to the behavioral attitude. Thus, important interventions to improve and strengthen attitudes about IM benefits were needed to promote the IM adherence. Notably, subjective norms were second only to attitudes in predicting IM intentions (0.278). In other words, the greater the influence of other individual or group giving to RTPs in IM adherence, the stronger the intentions to take medication. Therefore, medical staff should not only provide positive psychological interventions and social support to RTPs but also enhance their family’s awareness of taking IM regularly and timely.
In our study, HBM contributed the overall effect to IM nonadherence with the highest coefficient of effect and perceived barriers could play a vital influence on IM nonadherence. Our result was consistent with some previous studies showing that perceived barriers tend to be the strongest predictor of compliance (Wang et al., 2006; Carpenter, 2010). However, a recent study provided some different evidence that perceived susceptibility to rejection and perceived benefits of treatment were identified as major predictors of IM nonadherence (Kung et al., 2017). This difference might be due to different sample sizes in these studies. Nevertheless, all studies confirmed that health-related beliefs measured by HBM is an effective predictor of IM nonadherence. Based on our results, future educational programs should focus on the seriousness of not taking IM for Chinese RTPs. Some perceiving barriers, such as forgetting to take medicine and conflicts with social events, were similar to other reports. A recent study about hypertension population reported that forgetting was the most common reason for causing difficulty in taking medication (Yang et al., 2016). Understanding the barriers to optimal adherence provided information that could be used to better target interventions by doctors or health-care professionals. According to the present results, some effective methods, such as electronic medication devices with reminder and record functions, could play important roles in enhancing RTPs’ adherence. Our study also found that all variables of the TPB model did not exhibit sufficient effects on IM nonadherence, which might be one explanation of why TPB only explained 2% of variance in IM nonadherence. Until now, IM nonadherence could be predicted by several models, each having advantages and disadvantages, but none was considered as the gold standard. So we hoped that combination of the TPB and HBM model could make up for their shortcomings and provide much more interventions to improve transplant outcomes in clinical applications.
The most important aspect of this study included using the combined model and representing the larger sample size. Admittedly, the present study still had some limitations. One limitation was the potential bias, which was considered as follows: 1) A prestudy sample size calculation was absent. Hence, the findings of this study should be interpreted with caution. This is because the absence of sample size calculation may lead to systematic errors. 2) The adherence questionnaire used in this study was based on self-report, hence there could be recall bias. 3) Randomization was not employed in the selection of participants, hence the way the sample was obtained could introduce selection bias. Another limitation was that our study lacked effective external validity at present because of the COVID-19. In the future, multicenter studies with larger samples of different age-groups and some objective measures of IM nonadherence are needed to confirm our conclusions.
Our study, to our knowledge, is the first to explore the combined effect of the TPB and HBM model on IM nonadherence in Chinese RTPs, which could significantly improve the predictive capacity of any single model in IM nonadherence. Important implications for intervention can be drawn from our results. The logistic regression analysis results suggested that medical staff should focus on the RTPs with single or divorced status, families with low income, long time course after renal transplantation, and preoperative drinking history. Moreover, the combined model implied that encouraging RTPs’ willingness toward IM and enhancing their families’ awareness of taking IM regularly and timely were great ways to improve IM adherence. Meanwhile, future interventions should be conducted to increase perceived seriousness and to reduce perceived barriers for taking IM, which will effectively increase IM adherence rates and reduce the rejection risk to improve transplant outcomes. Future multicenter validation about the prediction and prevention of IM nonadherence are needed to confirm our conclusions, which would make more RTPs benefit.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by the Ethics Committee of The Third Xiangya Hospital Central South University (No:2019-S61). The patients/participants provided their written informed consent to participate in this study.
PZ: investigation, data curation, and writing—original draft. XZ: software, investigation, and resources. JY: writing—review and methodology and visualization. JL: conceptualization, supervision, and methodology.
The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article. This work was supported by the National Natural Science Foundation of China (grant number 71904209) and National Natural Science Foundation of Changsha (grant number kq2007070).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The authors acknowledge the Third Xiangya Hospital’s accommodation of our research requests amidst the COVID-19 outbreak. Most importantly, we would like to thank Xiao Wang, Shaojun Ye, and Yan Wang for their assistance in participant recruitment, data collection, and data transcribing.
IM, immunosuppressive medication; TPB, theory of planned behavior; HBM, health belief model; RTPs, renal transplant patients; BAASIS, basal assessment of adherence to immunosuppressive medications scale.
Andrew, B. J., Mullan, B. A., De Wit, J. B. F., Monds, L. A., Todd, J., and Kothe, E. J. (2016). Does the Theory of Planned Behaviour Explain Condom Use Behaviour Among Men Who Have Sex with Men? A Meta-Analytic Review of the Literature. AIDS Behav. 20 (12), 2834–2844. doi:10.1007/s10461-016-1314-0
Association Organ Transplantation Society of Chinese Medical, (2013). Guidelines for Organ Donation for Cardiac Death in China. 2nd Edition. Beijing: Practical Journal of Organ Transplantation (Electronic Version), 1–4.
Brown, W., Ottney, A., and Nguyen, S. (2011). Breaking the Barrier: the Health Belief Model and Patient Perceptions Regarding Contraception. Contraception 83 (5), 453–458. doi:10.1016/j.contraception.2010.09.010
Carpenter, C. J. (2010). A Meta-Analysis of the Effectiveness of Health Belief Model Variables in Predicting Behavior. Health Commun. 25 (8), 661–669. doi:10.1080/10410236.2010.521906
Caru, M., Curnier, D., Levesque, A., Sultan, S., Marcil, V., Laverdière, C., et al. (2020). Children's Physical Activity Behavior Following a Supervised Physical Activity Program in Pediatric Oncology. J. Cancer Res. Clin. Oncol. 146 (11), 3037–3048. doi:10.1007/s00432-020-03294-8
Chisholm, M. A., Kwong, W. J., and Spivey, C. A. (2007). Associations of Characteristics of Renal Transplant Recipients with Clinicians' Perceptions of Adherence to Immunosuppressant Therapy. Transplantation 84 (9), 1145–1150. doi:10.1097/01.tp.0000287189.33074.c8
Chisholm, M. A., Williamson, G. M., Lance, C. E., and Mulloy, L. L. (2007). Predicting Adherence to Immunosuppressant Therapy: a Prospective Analysis of the Theory of Planned Behaviour. Nephrol. Dial. Transplant. 22 (8), 2339–2348. doi:10.1093/ndt/gfm149
De Bleser, L., Dobbels, F., Berben, L., Vanhaecke, J., Verleden, G., Nevens, F., et al. (2011). The Spectrum of Nonadherence with Medication in Heart, Liver, and Lung Tranplant Patients Assessed in Various Ways. Transpl. Int. 24 (9), 882–891. doi:10.1111/j.1432-2277.2011.01296.x
Dobbels, F., Berben, L., De Geest, S., Drent, G., Lennerling, A., Whittaker, C., et al. (2010). The Psychometric Properties and Practicability of Self-Report Instruments to Identify Medication Nonadherence in Adult Transplant Patients: A Systematic Review. Transplantation 90 (2), 205–219. doi:10.1097/tp.0b013e3181e346cd
Du, C., Wu, S., Liu, H., Hu, Y., and Li, J. (2018). Influencing Factors of the Intention of Taking Medicine Among Renal Transplant Recipients[J]. J. Nurs. Sci. 33 (7), 3. doi:10.3870/j.issn.1001-4152.2018.07.033
Ganjali, R., Ghorban Sabbagh, M., Nazemiyan, F., Mamdouhi, F., Badiee Aval, S., Taherzadeh, Z., et al. (2019). Factors Associated with Adherence to Immunosuppressive Therapy and Barriers in Asian Kidney Transplant Recipients. Immunotargets Ther. 8, 53–62. doi:10.2147/itt.s212760
Germani, G., Lazzaro, S., Gnoato, F., Senzolo, M., Borella, V., Rupolo, G., et al. (2011). Nonadherent Behaviors after Solid Organ Transplantation. Transplant. Proc. 43 (1), 318–323. doi:10.1016/j.transproceed.2010.09.103
Horwood, H., Williams, M. J. A., and Mandic, S. (2015). Examining Motivations and Barriers for Attending Maintenance Community-Based Cardiac Rehabilitation Using the Health-Belief Model. Heart Lung Circ. 24 (10), 980–987. doi:10.1016/j.hlc.2015.03.023
Huang, S., Chen, Y., Zhou, J., and Wang, J. (2014). Use of Family Member-Based Supervision in the Management of Patients with Hypertension in Rural China. Patient Prefer Adherence 8, 1035–1042. doi:10.2147/PPA.S66777
Hugon, A., Roustit, M., Lehmann, A., Saint-Raymond, C., Borrel, E., Hilleret, M.-N., et al. (2014). Influence of Intention to Adhere, Beliefs and Satisfaction about Medicines on Adherence in Solid Organ Transplant Recipients. Transplantation 98 (2), 222–228. doi:10.1097/tp.0000000000000221
Kobus, G., Malyszko, J. S., and Małyszko, J. (2016). Do Age and Religion Have an Impact on the Attitude to Organ Transplantation? Transplant. Proc. 48 (5), 1354–1359. doi:10.1016/j.transproceed.2016.02.055
Kung, P.-C., Yeh, M. C., Lai, M.-K., and Liu, H. E. (2017). Renal Transplant Recipients: The Factors Related to Immunosuppressive Medication Adherence Based on the Health Belief Model. J. Nurs. Res. 25 (5), 392–397. doi:10.1097/jnr.0000000000000181
Le Berre, A.-P., Fama, R., and Sullivan, E. V. (2017). Executive Functions, Memory, and Social Cognitive Deficits and Recovery in Chronic Alcoholism: A Critical Review to Inform Future Research. Alcohol. Clin. Exp. Res. 41 (8), 1432–1443. doi:10.1111/acer.13431
Le Berre, A.-P., Pinon, K., Vabret, F., Pitel, A.-L., Allain, P., Eustache, F., et al. (2010). Study of Metamemory in Patients with Chronic Alcoholism Using a Feeling-Of-Knowing Episodic Memory Task. Alcohol. Clin. Exp. Res. 34 (11), 1888–1898. doi:10.1111/j.1530-0277.2010.01277.x
Leendertse, A. J., Egberts, A. C., Stoker, L. J., and Van Den Bemt, P. M. (2008). Frequency of and Risk Factors for Preventable Medication-Related Hospital Admissions in the Netherlands. Arch. Intern. Med. 168 (17), 1890–1896. doi:10.1001/archinternmed.2008.3
Li, A. S. W., Figg, G., and Schüz, B. (2019). Socioeconomic Status and the Prediction of Health Promoting Dietary Behaviours: A Systematic Review and Meta‐Analysis Based on the Theory of Planned Behaviour. Appl. Psychol. Health Well‐being 11 (3), 382–406. doi:10.1111/aphw.12154
Li, C., Wang, C., Zhang, N., and Ding, J. (2019). Effects of Health Education Based on Theory of Planned Behavior on Treatment Compliance Among Maintenance Hemodialysis Patients[J]. Chin. J. Mod. Nurs. 25 (8), 4. doi:10.3760/cma.j.issn.1674-2907.2019.08.026
Liu, J., Zhu, X., Yan, J., Gong, L., Wu, X., Liu, M., et al. (2021). Association between Regulatory Emotional Self-Efficacy and Immunosuppressive Medication Adherence in Renal Transplant Recipients:Does Medication Belief Act as a Mediator?[J]. Front. Pharmacol. 12, 559368. doi:10.3389/fphar.2021.559368
Marsicano, E., Fernandes, N., Colugnati, F., Fernandes, N., De Geest, S., and Sanders-Pinheiro, H. (2015). Multilevel Correlates of Non-adherence in Kidney Transplant Patients Benefitting from Full Cost Coverage for Immunosuppressives: A Cross-Sectional Study[J]. PLoS ONE 10 (11), e0138869. doi:10.1371/journal.pone.0138869
Mayberry, L. S., and Osborn, C. Y. (2012). Family Support, Medication Adherence, and Glycemic Control Among Adults with Type 2 Diabetes. Diabetes care 35 (6), 1239–1245. doi:10.2337/dc11-2103
Messina, E. (2015). Beyond the Officially Sacred, Donor and Believer: Religion and Organ Transplantation. Transplant. Proc. 47 (7), 2092–2096. doi:10.1016/j.transproceed.2015.06.031
Morowatisharifabad, M., Movahed, E., Farokhzadian, J., Nikooie, R., Hosseinzadeh, M., Askarishahi, M., et al. (2019). Antiretroviral Therapy Adherence and its Determinant Factors Among People Living with HIV/AIDS: a Case Study in Iran[J]. BMC Res. Notes 12 (1), 162. doi:10.1186/s13104-019-4204-5
Neter, E., Glass-Marmor, L., Wolkowitz, A., Lavi, I., and Miller, A. (2021). Beliefs about Medication as Predictors of Medication Adherence in a Prospective Cohort Study Among Persons with Multiple Sclerosis[J]. BMC Neurol. 21 (1), 136. doi:10.1186/s12883-021-02149-0
Noël, X., Van Der Linden, M., Brevers, D., Campanella, S., Hanak, C., Kornreich, C., et al. (2012). The Contribution of Executive Functions Deficits to Impaired Episodic Memory in Individuals with Alcoholism. Psychiatry Res. 198 (1), 116–122. doi:10.1016/j.psychres.2011.10.007
Pitel, A. L., Beaunieux, H., Witkowski, T., Vabret, F., Guillery-Girard, B., Quinette, P., et al. (2007). Genuine Episodic Memory Deficits and Executive Dysfunctions in Alcoholic Subjects Early in Abstinence. Alcohol. Clin. Exp. Res. 31 (7), 1169–1178. doi:10.1111/j.1530-0277.2007.00418.x
Prihodova, L., Nagyova, I., Rosenberger, J., Majernikova, M., Roland, R., Groothoff, J. W., et al. (2014). Adherence in Patients in the First Year after Kidney Transplantation and its Impact on Graft Loss and Mortality: a Cross-Sectional and Prospective Study. J. Adv. Nurs. 70 (12), 2871–2883. doi:10.1111/jan.12447
Quast, J., Knobloch, M. J., Patterson, E., Purvis, S., Shirley, D., and Safdar, N. (2016). Understanding Inpatient Perceptions of Indwelling Urinary Catheters Using the Health Belief Model. Infect. Control. Hosp. Epidemiol. 37 (9), 1098–1100. doi:10.1017/ice.2016.120
Shemesh, Y., Peles-Bortz, A., Peled, Y., Harzahav, Y., Lavee, J., Freimark, D., et al. (2017). Feelings of Indebtedness and Guilt toward Donor and Immunosuppressive Medication Adherence Among Heart Transplant (HTx) Patients, as Assessed in a Cross-Sectional Study with the Basel Assessment of Adherence to Immunosuppressive Medications Scale (BAASIS)[J]. Clin. Transpl. 31 (10). doi:10.1111/ctr.13053
Shen, Y., Peng, X., Wang, M., Zheng, X., Xu, G., Lü, L., et al. (2017). Family Member-Based Supervision of Patients with Hypertension: a Cluster Randomized Trial in Rural China. J. Hum. Hypertens. 31 (1), 29–36. doi:10.1038/jhh.2016.8
Spivey, C. A., Chisholm-Burns, M. A., Damadzadeh, B., and Billheimer, D. (2014). Determining the Effect of Immunosuppressant Adherence on Graft Failure Risk Among Renal Transplant Recipients. Clin. Transpl. 28 (1), 96–104. doi:10.1111/ctr.12283
Teng, S., Zhang, W., Lin, X., Shang, Y., Peng, X., and Liu, H. (2015). Beliefs about and Adherence to Immunosuppressants in Adult Renal Transplant Recipients[J]. J. Nurs. Sci. 30 (18), 5. doi:10.3870/hlxzz.2015.18.001
Tonelli, M., Wiebe, N., Knoll, G., Bello, A., Browne, S., Jadhav, D., et al. (2011). Systematic Review: Kidney Transplantation Compared with Dialysis in Clinically Relevant Outcomes. Am. J. Transpl. 11 (10), 2093–2109. doi:10.1111/j.1600-6143.2011.03686.x
Wang, S.-L., Charron-Prochownik, D., Sereika, S. M., Siminerio, L., and Kim, Y. (2006). Comparing Three Theories in Predicting Reproductive Health Behavioral Intention in Adolescent Women with Diabetes. Pediatr. Diabetes 7 (2), 108–115. doi:10.1111/j.1399-543x.2006.00154.x
Xia, M., Yan, J., Liu, S., and Liu, J. (2019). Beliefs of Immunosuppressive Medication Among Chinese Renal Transplant Recipients, as Assessed in a Cross-Sectional Study with the Basel Assessment of Adherence to Immunosuppressive Medications Scale. Transplant. Proc. 51 (3), 742–748. doi:10.1016/j.transproceed.2018.10.029
Yadav, K., Vock, D. M., Matas, A. J., Robiner, W. N., and Nevins, T. E. (2019). Medication Adherence Is Associated with an Increased Risk of Cancer in Kidney Transplant Recipients: a Cohort Study. Nephrol. Dial. Transpl. 34 (2), 364–370. doi:10.1093/ndt/gfy210
Yang, S., He, C., Zhang, X., Sun, K., Wu, S., Sun, X., et al. (2016). Determinants of Antihypertensive Adherence Among Patients in Beijing: Application of the Health Belief Model. Patient Educ. Couns. 99 (11), 1894–1900. doi:10.1016/j.pec.2016.06.014
Zhao, L., Yan, J., Yang, G.-L., and Liu, Y. (2017). A Study on Adherence to Follow-Up, Quality of Life, and Associated Factors Among Renal Transplant Recipients in China. Transplant. Proc. 49 (6), 1285–1290. doi:10.1016/j.transproceed.2017.03.086
Keywords: renal transplantation, immunosuppressive medication nonadherence, theory of planned behavior, health belief model, structural equation
Citation: Zhang P, Zhu X, Yan J and Liu J (2021) Identification of Immunosuppressive Medication Nonadherence Factors Through a Combined Theory Model in Renal Transplant Recipients. Front. Pharmacol. 12:655836. doi: 10.3389/fphar.2021.655836
Received: 20 January 2021; Accepted: 07 May 2021;
Published: 26 May 2021.
Edited by:
Elizabeth Manias, Deakin University, AustraliaReviewed by:
Olumuyiwa Omonaiye, Deakin University, AustraliaCopyright © 2021 Zhang, Zhu, Yan and Liu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jia Liu, Y2h1Y2tsZWpsQDE2My5jb20=
†These authors have contributed equally to this work and share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.