- 1Department of Pharmacy, Zhongshan Hospital Fudan University, Shanghai, China
- 2Department of Nephrology, Zhongshan Hospital Fudan University, Shanghai, China
Background: Vancomycin-associated acute kidney injury (VA-AKI) is a recognizable condition with known risk factors. However, the use of vancomycin in clinical practices in China is distinct from other countries. We conducted this longitudinal study to show the characteristics of VA-AKI and how to manage it in clinical practice.
Patients and Methods: We included patients admitted to hospital, who received vancomycin therapy between January 1, 2016 and June 2019. VA-AKI was defined as a patient having developed AKI during vancomycin therapy or within 48 h following the withdrawal of vancomycin therapy.
Results: A total of 3719 patients from 7058 possible participants were included in the study. 998 patients were excluded because of lacking of serum creatinine measurement. The incidence of VA-AKI was 14.3%. Only 32.3% (963/2990) of recommended patients performed therapeutic drug monitoring of vancomycin. Patients with VA-AKI were more likely to concomitant administration of cephalosporin (OR 1.55, 95% CI 1.08–2.21, p = 0.017), carbapenems (OR 1.46, 95% CI 1.11–1.91, p = 0.006) and piperacillin-tazobactam (OR 3.12, 95% CI 1.50–6.49, p = 0.002). Full renal recovery (OR 0.208, p = 0.005) was independent protective factors for mortality. Compared with acute kidney injury stage 1, AKI stage 2 (OR 2.174, p = 0.005) and AKI stage 3 (OR 2.210, p = 0.005) were independent risk factors for fail to full renal recovery.
Conclusion: Lack of a serum creatinine measurement for the diagnosis of AKI and lack of standardization of vancomycin therapeutic drug monitoring should be improved. Patient concomitant with piperacillin-tazobactam are at higher risk. Full renal recovery was associated with a significantly reduced morality.
Introduction
Currently, vancomycin is the first-line treatment for methicillin-resistant Staphylococcus aureus (MRSA) infections. However, it has also been associated with significant acute kidney injury (AKI) (Chen et al., 2011; Liu et al., 2011), which is a common disorder with a high risk of mortality, the development of chronic kidney disease, and substantial medical expense (Yang et al., 2015). There is considerable variation in the incidence of reported vancomycin-associated AKI (VA-AKI), which ranges from 5 to 43% (van Hal et al., 2013). There are numerous potential risk factors for VA-AKI including race, obesity, vancomycin exposure, pre-existing kidney disease, severity of illness, concurrent nephrotoxin exposure, concurrent piperacillin-tazobactam use, etc. (Filippone et al., 2017). However, due to variations in study populations and sample sizes, different studies have identified conflicting risk factors. Several studies have shown that specific races (e.g., African-Americans) have a higher risk for VA-AKI (Bosso et al., 2011; Womble et al., 2019); although, studies specifically investigating Asian populations are lacking. For patients developed VA-AKI, how to reduce mortality and improve renal recovery is still a difficult problem to be explored.
We previously have reported that current literature on VA-AKI mainly came from American hospitals (Pan et al., 2019). However, the clinical use of vancomycin in China is distinct from other countries. For instance, vancomycin and piperacillin-tazobactam are among the most commonly prescribed antibiotics in American hospitals, which are associated with significant increases in the incidence of AKI compared to vancomycin monotherapy or other empirical combinations (Balci et al., 2018; Carreno et al., 2018; Ide et al., 2019; Avedissian et al., 2020; Ciarambino et al., 2020). In contrast, previous studies have shown that, in China, the most common antibiotic combinations with vancomycin are carbapenems (Pan et al., 2017; Pan et al., 2018). Liang et al. found that vancomycin nephrotoxicity was significantly correlated with the trough concentration and reported the first cut-point as 13 mg/L for the Chinese population (Liang et al., 2018). This was in contrast to trough concentrations exceeding 15 mg/L cited in American guidelines (Rybak et al., 2009; Ye et al., 2016). (Yang et al., 2015). found that, in China, a higher proportion of nephrotoxic drug exposure (71.6%) occurred before or while AKI develops as opposed to what has been reported by developed countries (20–50%) (Yang et al., 2015). Therefore, we designed this cohort study to include large sample patients, who are widely distributed and included a comprehensive number of risk factors. We believe that data from China, the most populous country in Asia, and the world’s largest developing nation, will provide valuable information for assessing the burden of VA-AKI in this population, as well as describe its clinical characteristics, show how to recognize and manage VA-AKI in clinical practice.
Methods
Study Design and Patient Population
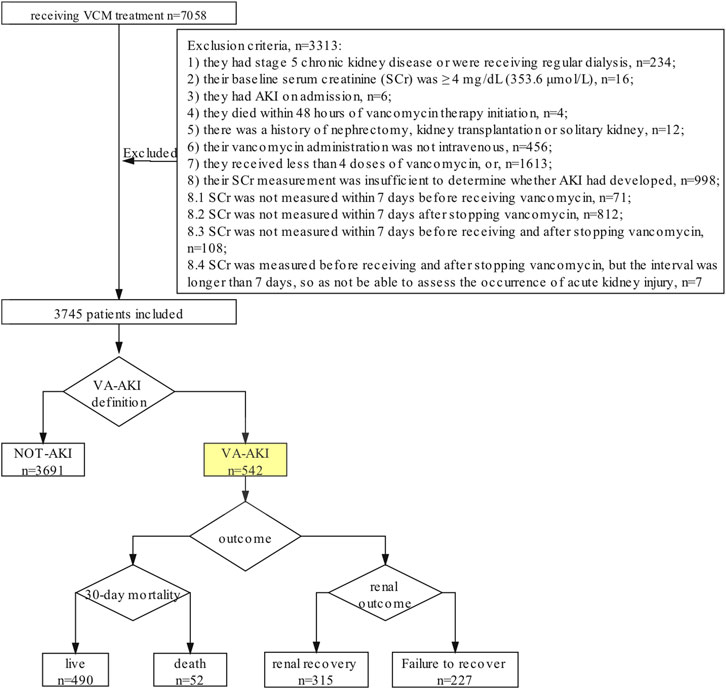
This was a retrospective observational cohort study performed at Zhongshan Hospital Fudan University, a comprehensive, 2005-bed teaching hospital. The survey of VA-AKI was designed to include three steps (Figure 1). First, all adult inpatients treated with vancomycin from January 2016 to June 2019 were evaluated for study inclusion. Patients were excluded if 1) they had stage 5 chronic kidney disease or were receiving regular dialysis; 2) their baseline serum creatinine (SCr) was ≥4 mg/dL (353.6 μmol/L); 3) they had AKI on admission; 4) they died within 48 h of vancomycin therapy initiation; 5) there was a history of nephrectomy, kidney transplantation or solitary kidney; 6) their vancomycin administration was not intravenous; 7) they received less than four doses of vancomycin, or; 8) their SCr measurement was insufficient to determine whether AKI had developed.
Second, we recorded the SCr of the included patients and separated the patients into two groups: the NOT-AKI group and the VA-AKI group. We used the 2012 Kidney Disease:Improving Global Outcomes (KDIGO) definition of AKI as the primary screening criterion, e.g., an increase in SCr by ≥ 0.3 mg/dL (≥26.5 μmol/L) within 48 h or an increase in SCr to ≥1.5 times baseline, which was known or presumed to have occurred within the prior 7 days (KDIGO Acute Kidney Injury Work Group, 2012). VA-AKI was defined as a patient having developed AKI during vancomycin therapy or within 48 h following the withdrawal of vancomycin therapy.
Third, for patients who developed AKI, we further analyzed the severity and outcome of the condition. Severity was assessed based on the highest AKI stage (1, 2, or 3) according to the KDIGO criterion. VA-AKI outcomes for the study included length of hospital stay (LOS), renal recovery, and 30-day mortality rates. Renal recovery was categorized into three levels: full recovery, partial recovery and failure to recover. We defined renal recovery at discharge as full recovery with SCr decreased to the baseline. We defined partial recovery as SCr decreased by 25% or more from peak concentration but remaining higher than baseline. We defined failure to recover as patient still dependent on dialysis or SCr decreased by less than 25% from peak concentration until discharged.
Data Collection
Data was extracted from the hospital’s electronic database. A researcher uninvolved in the study anonymized patient information. The following variables were collected: demographic information, concomitant underlying diseases, severity of disease, vancomycin exposure, vancomycin variety (Wenkexin vs. Laikexin; trade name: Wenkexin, generic name: Vancomycin Hydrochloride for Injection, manufacturer: VIANEX S.A. (PLANT C), Greece, specification: 500 mg/bottle; and, trade name: Laikexin, generic name: Vancomycin Hydrochloride for Injection, manufacturers: Zhejiang Medicine Co., Ltd. Xinchang Pharmaceutical Factory, China, specification: 500 mg/bottle), therapeutic drug monitoring (TDM) rates, and concomitant nephrotoxic drugs. We also collected data on economic factors and patient outcomes including renal recovery, LOS, and 30- and 90-day mortality rates (Supplementary Table S1).
Data Analysis
Variables were assessed for normality using the Kolmogorov-Smirnov test. Based on these tests, quantitative variables are presented as means and standard deviations (SDs) or medians and interquartile ranges (IQRs). Variables were then compared between groups using independent t-tests or rank-sum tests. Qualitative variables are presented as frequencies and corresponding percentages and were compared using chi-squared or Fisher’s exact tests.
A multivariate logistic regression analysis was used to assess independent risk factors for VA-AKI occurrence, full renal recovery and mortality. All potential risk factors with a p value ≤ 0.05 in the univariate analysis were used in the multiple logistic regression analysis (Supplementary Table S2). A backwards conditional approach was used to enter new terms into the logistic regression. The good of fit was evaluated by the analysis of Hosmer and Lemeshow. All p values were two-sided, and a p value ≤ 0.05 was considered statistically significant. All statistical analyses were performed using SPSS statistics version 26.0 (IBM Inc., Armonk, NY, United States).
Results
There were 7058 patients evaluated for study inclusion. After applying the exclusion criteria, 3339 (47.3%) patients were omitted from the study. Of those excluded, 998 patients lacked a SCr measurement, typically within 7 days after receiving vancomycin therapy (Figure 1). A total of 3719 patients were included for analysis. Of these, 66.3% were male and 33.7% were female. The median age was 60 years (IQR, 48.0–68.0).
The incidence of VA-AKI was 14.3% (532/3719) and occurred after 3.0 (IQR, 1.0–7.0) days of treatment. During vancomycin therapy, 86.2% of the patients received at least one nephrotoxic drug. The percentage of patients who received nephrotoxic drugs in combination with vancomycin was 36.8% for one drug, 32.8% for two drugs and 12.5% for three drugs (Supplementary Table S3). The ROC curve analysis indicated that a limit of 1.5 combined nephrotoxic agents was the optimal cut-off value for defining VA-AKI high-risk individuals (Supplementary Figure S1). The most common antibiotic used in combination therapy was carbapenem (58.7%, 2186/3719), while the rate of piperacillin-tazobactam use was 1.6% (62/3719).
Regional Distribution of the Patients Included
Patients included in the study came from 219 (65.6%, 219/334) municipal boroughs in 30 (88.2%, 30/34) provincial-level administrative regions in China. There are 34 provincial-level administrative regions includes 23 provinces, five autonomous regions, four municipalities and two special administrative regions in China (China Government Network, 2005) (See Supplementary Table S4 for details).
Therapeutic Drug Monitoring of Patients
According to the vancomycin TDM guidelines issued by the Chinese Pharmacological Society (Ye et al., 2016), 3524 patients were recommended to receive TDM. However, only 1051 (29.8%) patients received it. Monitoring was initiated before the fourth or fifth vancomycin administration in 21.5% patients. A steady state valley concentration between 10 and 20 μmol/L occurred in 42.6% patients, while 27.6% had a concentration greater than 20 μmol/L. The highest monitoring rates occurred in patients with hepatic insufficiency (48.2%) and renal insufficiency (45.5%) (Supplementary Table S5).
Comparison of Risk Factors Between Patients with and Without VA-AKI
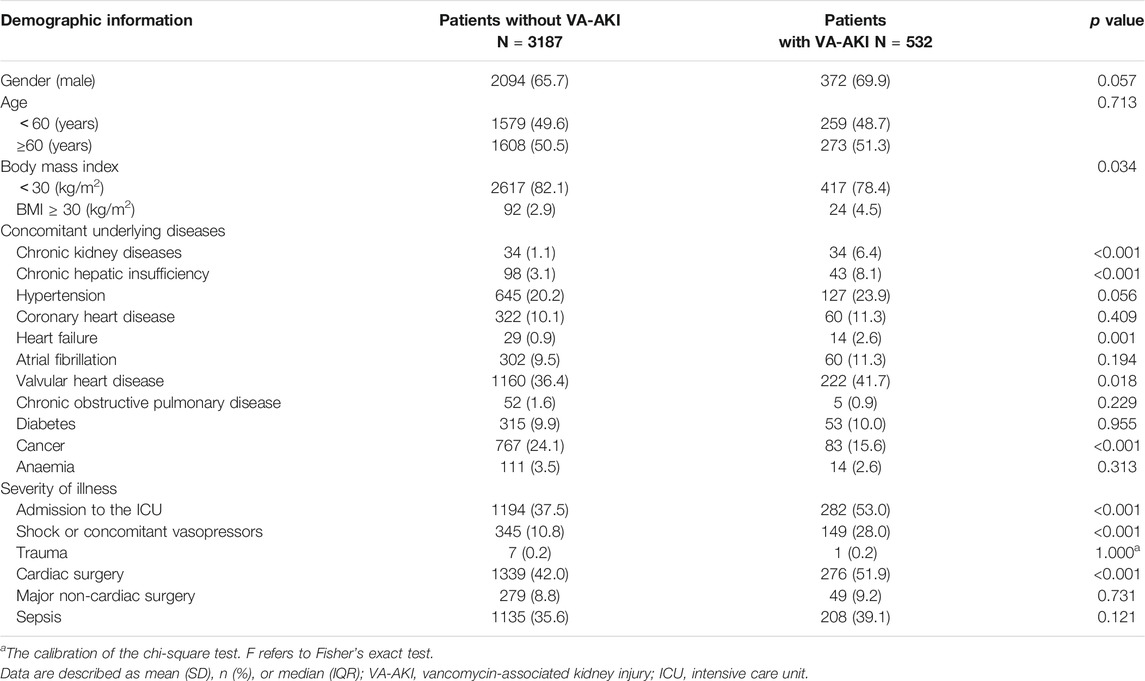
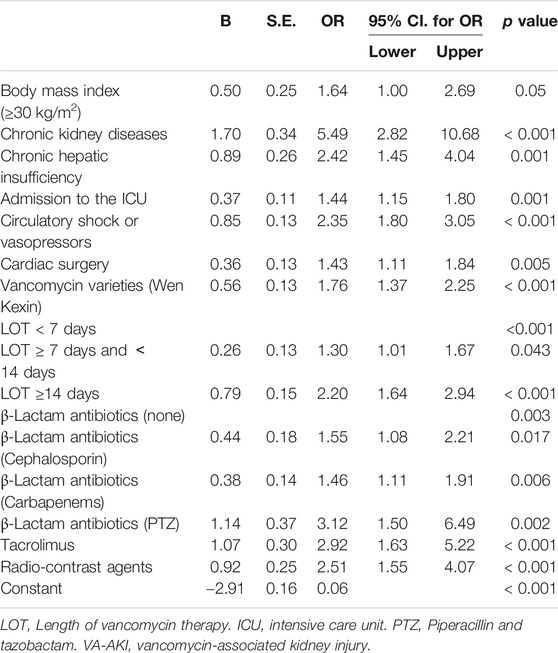
Table 1 displays patient demographic information, concomitant underlying diseases, and severity of illness. Table 2 lists patient vancomycin exposure and concomitant nephrotoxic drugs. The multivariable logistic regression of factors for development of VA-AKI can be seen in Table 3. Patients with VA-AKI were more likely to concomitant with BMI ≥ 30 kg/m2 (OR 1.64, 95% CI 1.00–2.69, p = 0.05) than those without VA-AKI. There was no significant difference in age or sex between the two groups.
More patients in VA-AKI group had concomitant chronic kidney disease (OR 5.49, 95% CI 2.82–10.68, p < 0.001) or chronic hepatic insufficiency (OR 2.42, 95% CI 1.45–4.04, p = 0.001) and were more likely to have concomitant heart failure (2.6 vs. 0.9%, p = 0.001) and valvular heart disease (41.7% vs. 36.4%, p = 0.018), but less likely to have cancer (15.6 vs. 24.1%, p < 0.001). Patients in VA-AKI group were also more likely to be admitted to the ICU (OR 1.44, 95% CI 1.15–1.80, p = 0.001), to experience shock or be given concomitant vasopressors (OR 2.35, 95% CI 1.80–3.05, p < 0.001) and undergo cardiac surgery (OR 1.43, 95% CI 1.11–1.84, p = 0.005).
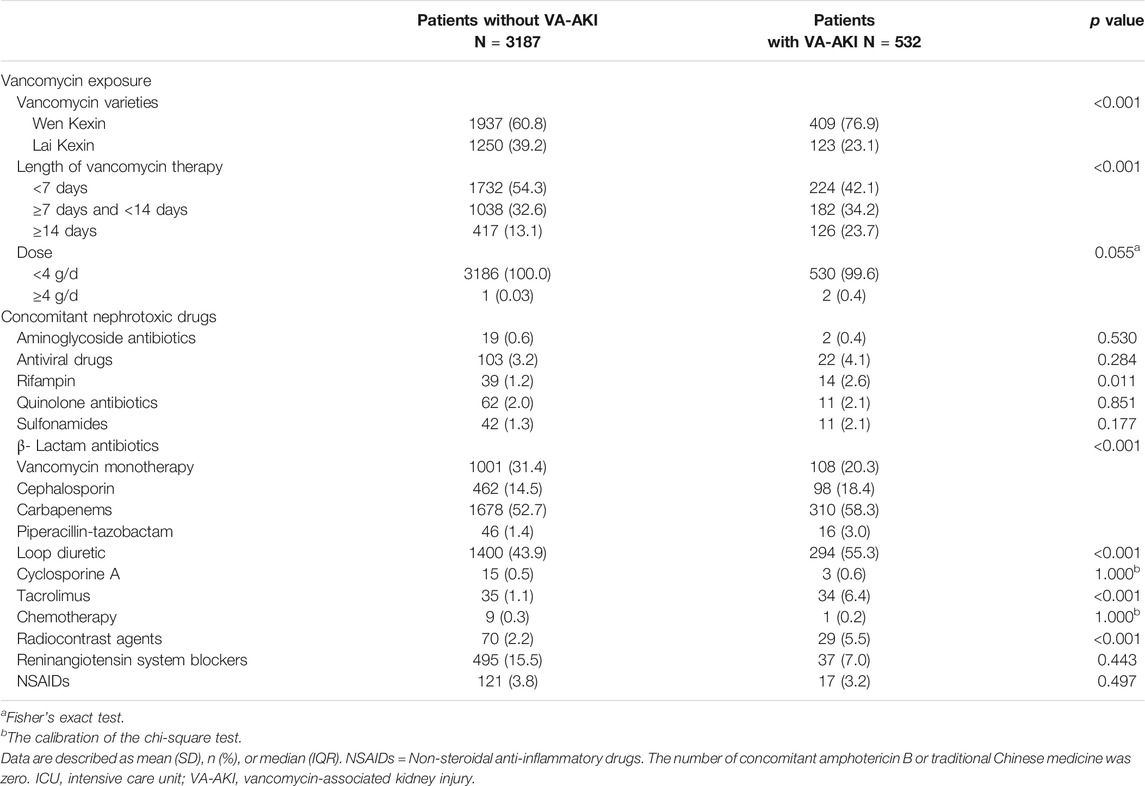
Patients with VA-AKI received more Wen Kexin (vs. Lai Kexin) (OR 1.76, 95% CI 1.37–2.25, p < 0.001), compared with those without VA-AKI. In addition, patients in the VA-AKI group underwent a longer therapy course. Exposure to loop diuretics (5.5 vs. 2.2%, p < 0.001), tacrolimus (OR 2.92, 95% CI 1.63–5.22, p < 0.001), and radio-contrast agents (OR 2.51, 95% CI 1.55–4.07, p < 0.001) were also more frequent in the VA-AKI group. Furthermore, patients with VA-AKI were more likely to concomitant with concomitant administration of cephalosporin (OR 1.55, 95% CI 1.08–2.21, p = 0.017), carbapenems (OR 1.46, 95% CI 1.11–1.91, p = 0.006) and piperacillin-tazobactam (OR 3.12, 95% CI 1.50–6.49, p = 0.002).
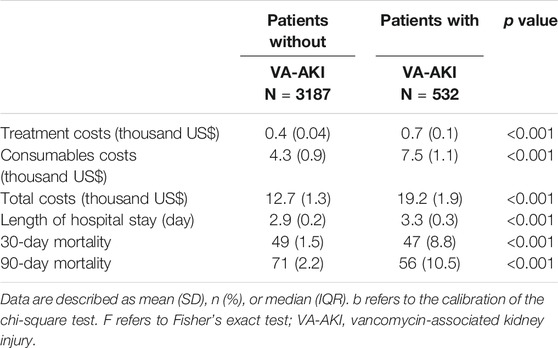
Comparison of Medical Costs and Outcomes for Patients with and Without VA-AKI
Patients with VA-AKI were more likely to have higher medication costs (6.1 vs. 3.6 thousand US dollars, p < 0.001), treatment costs (0.7 vs. 0.4 thousand US dollars, p < 0.001) and total costs (19.2 vs. 12.7 thousand US dollars, p < 0.001). Patients in the VA-AKI group also had longer hospital stays (23 vs. 20 days, p < 0.001) and a higher 30-days mortality rate (8.8% vs. 1.5%, p < 0.001) (Table 4).
Severity and Outcomes of VA-AKI Patients
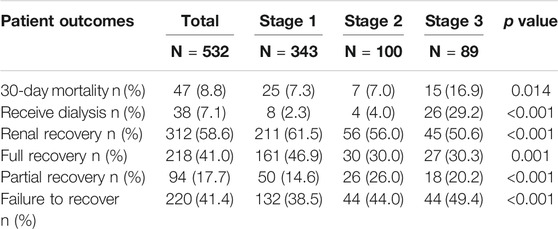
There were 343 VA-AKI patients (64.5%) with KDIGO stage 1 AKI. Thirty-eight patients (7.1%) received dialysis, and those with stage 3 VA-AKI experienced the highest dialysis rate (29.2%).
The 30-day mortality rate of the VA-AKI patients was 8.8%, and 29.8% (14/47) of patients had SCr within the normal range (44–115 μmol L−1) at the time of death. For patients with stage 3 AKI the mortality was 16.9%.
58.6% (312/542) of VA-AKI patients have a renal recovery (full recovery or partial recovery), of which 40.2% (218/542) patients fully recovered. The median time to renal recovery is 4.1 (IQR = 5.0) days after VA-AKI occur. Patients with stage 1 AKI had the highest renal recovery rate (46.9%) (Table 5).
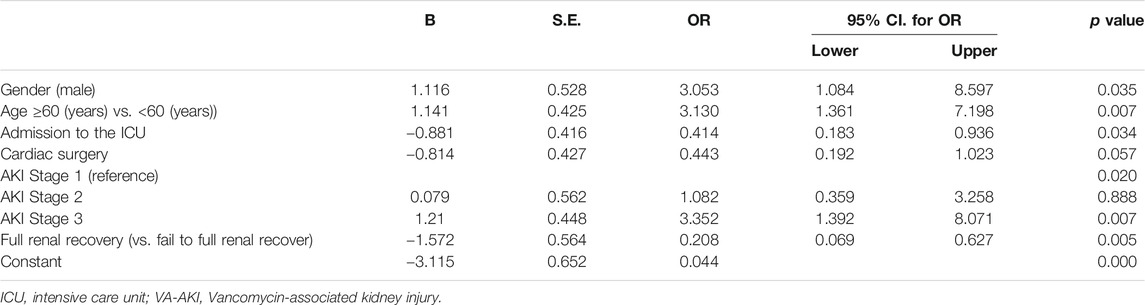
Risk Factors for Mortality of VA-AKI Patients
Multiple logistic regression analysis revealed that gender (male) (OR 3.053, p = 0.035) and age (≥60 years) (OR 3.13, p = 0.007) were independent risk factors for mortality. Compared with AKI stage 1, AKI stage 3 (OR 3.352, p = 0.007) was an independent risk factor for mortality. Full renal recovery (OR 0.208, p = 0.005) and admission to the ICU (OR 0.414, p = 0.034) were independent protective factors for mortality (Table 6).
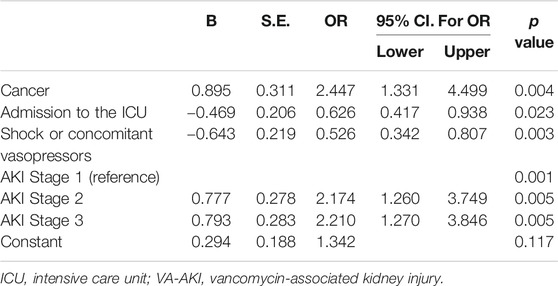
Risk Factors for Fail to Full Renal Recovery of VA-AKI Patients
Multiple logistic regression analysis revealed that cancer (OR 2.447, p = 0.004) was an independent risk factor for fail to full renal recovery. Compared with AKI stage 1, AKI stage 2 (OR 2.174, p = 0.005) and AKI stage 3(OR 2.210, p = 0.005) were independent risk factors for fail to full renal recovery. Admission to the ICU (OR 0.626, p = 0.023) and shock or concomitant vasopressors (OR 0.526, p = 0.003) were independent protective factors for fail to full renal recovery (Table 7).
Discussion
This single-center cohort study, including 3719 patients from 30 of 34 provincial-level administrative regions in China, have investigated the burden and characteristics of VA-AKI in China. Our survey, with to our knowledge, the largest sample size so far and covering patients from different areas in China, further uncovered the risk factors for prognosis of VA-AKI patients.
Our results showed that the incidence of VA-AKI was 14.3%, however, this could be an underestimate as 998 patients were excluded due to insufficient SCr measurements, which is consistent with our previous research (Pan et al., 2018). Therefore, our results may have missed a number of VA-AKI patients.
Currently, TDM is an effective measure used to reduce VA-AKI. However, we found several issues with its use, including an insufficient monitoring rate of the target population, inappropriate TDM start times, and an insufficient rate of achieving steady-state concentrations. The TDM guidelines for vancomycin was issued by the American Society of Health-System Pharmacists in 2009 (Rybak et al., 2009), updated in 2020 (Rybak et al., 2020), and issued by the Chinese Pharmacological Society in 2016 (Ye et al., 2016). However, a survey of vancomycin TDM involving 214 medical institutions in China revealed that vancomycin-monitoring technology, while adequately advanced, was not standardized for monitoring time or target populations in clinical practice (Zhou et al., 2019). This may be due to clinicians in China having high-work loads leading to time constraints and distractions (Jiang et al., 2019).
A complete diagnosis of AKI by SCr measurements and standardized vancomycin TDM is necessary for its management. The most current 2020 guidelines recommend using Bayesian-derived AUC monitoring rather than trough concentrations (Rybak et al., 2020). Several studies have shown that pharmacists who lead or participate in vancomycin medication management programs are conducive in improving the effective use of vancomycin and reducing the mean duration of vancomycin therapy and medical expenses (Willis and Jhaveri, 2018; Dadzie et al., 2019; Porter et al., 2019). Therefore, clinical pharmacists may be able to reduce both the workload of doctors and medical expenses (Willis and Jhaveri, 2018). Thus, hospital administrators should consider increasing their investment in clinical pharmacists to reduce the incidence of VA-AKI.
One distinct feature of this study was the high proportion of concomitant nephrotoxic medication use (86.2%) compared with the 28–71% reported in hospitals from the United States (Hidayat et al., 2006; Choi et al., 2017). Previous investigations have indicated that a combination of vancomycin and nephrotoxic agents is associated with nephrotoxicity (Castanheira et al., 2016; Yang, 2017). Uekl et al. showed that the number of combined nephrotoxic agents (OR, 1.590, p = 0.010) was significantly related to nephrotoxicity (Ueki et al., 2020). In accordance with these results, we also observed a significantly higher incidence of VA-AKI in patients given combined multiple nephrotoxic drugs, especially combinations of more than two drugs.
Another distinct finding of this Chinese VA-AKI study was the high proportion of the combined use of carbapenems (especially mipenem and meropenem) with vancomycin, rather than piperacillin-tazobactam (59.3 vs. 1.7%). Vancomycin and piperacillin-tazobactam are among the most commonly prescribed antibiotics in hospitals in the United States, and this particular combination of antibiotics may be empirically useful due to the broad Gram-positive activity of vancomycin and broad Gram-negative activity of piperacillin-tazobactam (Carreno et al., 2018). Both piperacillin-tazobactam and carbapenems have broad Gram-negative activity and are recommended in clinical practice guidelines in China (Ran et al., 2019; Wu and Ren, 2020). We speculate that one reason for more combinations with carbapenems is that piperacillin-tazobactam requires a skin test before administration in China, while carbapenem antibiotics do not. The concern is that penicillin-based antibiotics may cause severe allergic reactions such as anaphylactic shock (Yang, 2017). Therefore, the People's Republic of China Pharmacopoeia Clinical Medication Instructions require skin tests before using penicillin (Yang, 2017). Hence, carbapenem antibiotics are preferred as they are more convenient. Another possible reason for more combinations with carbapenems is the higher prevalence of extended-spectrum beta-lactamase (ESBL) in China, compared to United States. One study that collected 15,588 Enterobacteriaceae isolates from 63 hospitals in the United States from 2012 to 2014, found a prevalence of ESBL-producing strains of 13.6% for Escherichia coli, 17.4% for Klebsiella pneumoniae, 10.8% for Klebsiella. oxytoca and 5.7% for Proteus mirabilis (5.7%) (Castanheira et al., 2016). In contrast, in 2014 the China Antimicrobial Surveillance Network collected 78,955 Enterobacteriaceae isolates from 15 general hospitals and two children’s hospitals and found that the prevalence of ESBL-producing strains was 55.3% for E. coli, 22.9% for K. pneumoniae and K. oxytoca, and 24.7% for P. mirabilis (Hu et al., 2016). Carbapenem antibiotics produce strong antibacterial activity against ESBL-producing strains and are currently the most effective and reliable antibacterial drugs for the treatment of various infections caused by ESBL-producing Enterobacteriaceae bacteria (Zhou et al., 2014).
The combination of vancomycin plus piperacillin-tazobactam increases the odds of inducing AKI, thus vancomycin plus carbapenems may contribute to a lower rate of VA-AKI in China (Balci et al., 2018; Carreno et al., 2018; Ide et al., 2019; Avedissian et al., 2020; Ciarambino et al., 2020). Our multiple regression analysis showed that both carbapenem and piperacillin-tazobactam antibiotics were independent risk factors for VA-AKI, and the OR value of piperacillin-tazobactam was higher than carbapenems (OR = 3.12 vs. OR = 1.46), which is consistent with previous reports (Ide et al., 2019). The potential mechanism underlying the enhanced toxicity of this combination remains uncertain (Gomes et al., 2014). has suggested that subclinical interstitial nephritis caused by piperacillin-tazobactam in combination with the oxidative stress of vancomycin might lead to increased renal injury (Gomes et al., 2014). (Burgess and Drew, 2014) has posited that piperacillin-tazobactam might reduce vancomycin clearance, resulting in increased exposure in the kidney and, hence, further injury (Burgess and Drew, 2014). Therefore, from the perspective of reducing VA-AKI, the combined use of carbapenem antibiotics, rather than piperacillin-tazobactam should be considered a better choice.
Our study had several strengths. First, the sample size was relatively large, and the population was geographically widely distributed. Second, in terms of nephrotoxic drugs, we included categories that were as comprehensive as possible. Third, we gathered data regarding associated medical costs, which has rarely been addressed in the literature. This study also had some limitations. Due to the retrospective design, we were only able to show associations between vancomycin and AKI and not causality. In addition, urine output was not assessed and this may have affected the rates of identified AKI. Furthermore, as trough levels were not drawn for every patient, we were unable to evaluate the potential effect of vancomycin concentration on the development of AKI, which is a well-known risk factor for nephrotoxicity.
VA-AKI is associated with a higher medical expenses and risk of mortality. We carried out this longitudinal study to further analyze the factors that affect the prognosis of patients with VA-AKI, which was rarely involved in previous studies. Our research shows that full renal recovery is an independent protective factor for mortality. Approximately 70% of patients died with impaired renal function, and we speculate that the deaths of these patients may be related to AKI. Compared with unchangeable factors such as gender and age, renal recovery is a risk factor that can be improved, so it is the focus of efforts to reduce the mortality of patients. Only 41.2% of the patients with VA-AKI recovered renal function during hospitalization, which is lower than the 58–81% reported in developed countries (Pritchard et al., 2010; Lacave et al., 2017). Once the patient develops AKI, we recommend prompt and active treatment. Admission to ICU helps improve the patient's full renal recovery reduce mortality. We speculate that patients in the ICU can receive more comprehensive monitoring and timely treatment. Higher AKI stages are independent risk factors of failure to full renal recovery and mortality, which is consistent with previous studies (Forni et al., 2017). In conclusion, it may be necessary to suspend vancomycin or adjust the dosage in a timely manner for the renal recovery (Rybak et al., 2020), especially for patients with high KDIGO AKI stages.
Conclusion
Lack of a serum creatinine measurement for the diagnosis of AKI and lack of standardization of vancomycin therapeutic drug monitoring should be improved. Patient concomitant with piperacillin-tazobactam are at higher risk. Full renal recovery was associated with a significantly reduced morality.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation. Requests to access the datasets should be directed to the corresponding Author.
Ethics Statement
The study was approved by the Ethics Committee of Zhongshan Hospital of Fudan University (Approval No: B2019-194R). Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
Author Contributions
PK, DX, LX and LQ made contributions to the conception and design of the study. PM, CC and CZ acquired the data. PK, WW, XQ analyzed the data. PM drafted the article and LQ made contributions to revising it critically for important intellectual content. All authors contribute to final approval of the version to be submitted.
Funding
This research was funded by the Youth Fund of Zhongshan Hospital Fudan University (Fund no. 2018ZSQN30).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fphar.2021.632107/full#supplementary-material.
References
Avedissian, S. N., Pais, G. M., Liu, J., Rhodes, N. J., and Scheetz, M. H. (2020). Piperacillin-tazobactam added to vancomycin increases risk for acute kidney injury: fact or fiction? Clin. Infect. Dis. 71, 426–432. doi:10.1093/cid/ciz1189
Balci, C., Uzun, O., Arici, M., Hayran, S. A., Yuce, D., and Unal, S. (2018). Nephrotoxicity of piperacillin/tazobactam combined with vancomycin: should it be a concern? Int. J. Antimicrob. Ag 52, 180–184. doi:10.1016/j.ijantimicag.2018.03.024
Bosso, J. A., Nappi, J., Rudisill, C., Wellein, M., Bookstaver, P. B., Swindler, J., et al. (2011). Relationship between vancomycin trough concentrations and nephrotoxicity: a prospective multicenter trial. Antimicrob. Agents Chemother. 55, 5475–5479. doi:10.1128/aac.00168-11
Burgess, L. D., and Drew, R. H. (2014). Comparison of the incidence of vancomycin-induced nephrotoxicity in hospitalized patients with and without concomitant piperacillin-tazobactam. Pharmacotherapy 34, 670–676. doi:10.1002/phar.1442
Carreno, J., Smiraglia, T., Hunter, C., Tobin, E., and Lomaestro, B. (2018). Comparative incidence and excess risk of acute kidney injury in hospitalised patients receiving vancomycin and piperacillin/tazobactam in combination or as monotherapy. Int. J. Antimicrob. Agents 52, 643–650. doi:10.1016/j.ijantimicag.2018.08.001
Castanheira, M., Mendes, R. E., Jones, R. N., and Sader, H. S. (2016). Changes in the frequencies of β-lactamase genes among Enterobacteriaceae isolates in U.S. hospitals, 2012 to 2014: activity of ceftazidime-avibactam tested against β-lactamase-producing isolates. Antimicrob. Agents Chemother. 60, 4770–4777. doi:10.1128/aac.00540-16
Chen, B. Y., Guan, X. D., He, L. X., Hu, J., Huang, Z. Y., Li, G. H., et al. (2011). Chinese expert consensus on the clinical application of vancomycin. Chin. J. New Drugs Clin. Rem 30, 561–573. doi:10.1002/cjoc.201100012
China Government Network (2005). The central People’s government of the People’s Republic of China. administrative divisions of the people’s republic of china. Available at: http://www.gov.cn/guoqing/2005-09/13/content_5043917.htm (Accessed February 18, 2020)
Choi, Y. C., Saw, S., Soliman, D., Bingham, A. L., Pontiggia, L., Hunter, K., et al. (2017). Intravenous vancomycin associated with the development of nephrotoxicity in patients with class III obesity. Ann. Pharmacother. 51, 937–944. doi:10.1177/1060028017720946
Ciarambino, T., Giannico, O. V., Campanile, A., Tirelli, P., Para, O., Signoriello, G., et al. (2020). Acute kidney injury and vancomycin/piperacillin/tazobactam in adult patients: a systematic review. Intern. Emerg. Med. 15, 327–331. doi:10.1007/s11739-020-02287-2
Dadzie, P., Dietrich, T., and Ashurst, J. (2019). Impact of a pharmacist-driven methicillin-resistant Staphylococcus aureus polymerase chain reaction nasal swab protocol on the de-escalation of empiric vancomycin in patients with pneumonia in a rural healthcare setting. Cureus 11, e6378. doi:10.7759/cureus.6378
Filippone, E., Kraft, W., and Farber, J. (2017). The nephrotoxicity of vancomycin. Clin. Pharmacol. Ther. 102, 459–469. doi:10.1002/cpt.726
Forni, L. G., Darmon, M., Ostermann, M., Oudemans-van Straaten, H. M., Pettilä, V., Prowle, J. R., et al. (2017). Renal recovery after acute kidney injury. Intensive Care Med. 43, 855–866. doi:10.1007/s00134-017-4809-x
Gomes, D. M., Smotherman, C., Birch, A., Dupree, L., Della Vecchia, B. J., Kraemer, D. F., et al. (2014). Comparison of acute kidney injury during treatment with vancomycin in combination with piperacillin-tazobactam or cefepime. Pharmacotherapy 34, 662–669. doi:10.1002/phar.1428
Hidayat, L. K., Hsu, D. I., Quist, R., Shriner, K. A., and Wong-Beringer, A. (2006). High-dose vancomycin therapy for methicillin-resistant Staphylococcus aureus infections: efficacy and toxicity. Arch. Intern. Med. 166, 2138–2144. doi:10.1001/archinte.166.19.2138
Hu, F. P., Zhu, D. M., Wang, F., Jiang, X. F., Xu, Y. C., Zhang, X. J., et al. (2016). CHINET 2014 surveillance of bacterial resistance in China. Chin. J. Infect. Checker 15, 401–410. doi:10.1007/s10096-019-03673-1
Ide, N., Sato, S., and Sawaguchi, K. (2019). Risk of acute kidney injury in patients treated with vancomycin and piperacillin/tazobactam compared to vancomycin and meropenem or doripenem: a retrospective cohort study. Yakugaku Zasshi 139, 1609–1614. doi:10.1248/yakushi.19-00137
Jiang, Y., Guan, Y.-J., Dai, D.-W., Huang, W., and Huang, Z.-Y. (2019). Prevalence of stress and its determinants among residents enrolled in China Standardized training program for resident doctor (C-STRD) program: a cross-sectional study. PLos One 14 (1), e0207258. doi:10.1371/journal.pone.0207258
KDIGO Acute Kidney Injury Work Group (2012). KDIGO clinical practice guideline for acute kidney injury. Kidney Int. Suppl. 2, 1–138. doi:10.1038/kisup.2012.6
Lacave, G., Caille, V., Bruneel, F., Palette, C., Legriel, S., Grimaldi, D., et al. (2017). Incidence and risk factors of acute kidney injury associated with continuous intravenous high-dose vancomycin in critically ill patients. Medicine 96, e6023. doi:10.1097/md.0000000000006023
Liang, X., Fan, Y., Yang, M., Zhang, J., Wu, J., Yu, J., et al. (2018). A prospective multicenter clinical observational study on vancomycin efficiency and safety with therapeutic drug monitoring. Clin. Infect. Dis. 67, S249–S255. doi:10.1093/cid/ciy680
Liu, C., Bayer, A., Cosgrove, S. E., Daum, R. S., Fridkin, S. K., Gorwitz, R. J., et al. (2011). Clinical practice guidelines by the infectious diseases society of America for the treatment of methicillin-resistant Staphylococcus aureus infections in adults and children: executive summary. Clin. Infect. Dis. 52, 285–292. doi:10.1093/cid/cir034
Pan, K.-M., Wu, Y., Chen, C., Chen, Z.-Z., Xu, J.-A., Cao, L., et al. (2018). Vancomycin-induced acute kidney injury in elderly Chinese patients: a single-centre cross-sectional study. Br. J. Clin. Pharmacol. 84, 1706–1718. doi:10.1111/bcp.13594
Pan, K. M., Chen, C., Chen, Z. Z., Xu, Q., Lv, Q. Z., and Li, X. Y. (2019). Bibliometric analysis of vancomycin-associated acute kidney injury. Cent. South Pharm. 17, 2195–2199. doi:10.7539/j.issn.1672-2981.2019.12.041
Pan, K. M., Ma, L. Y., Xiang, Q., Li, X. Y., Li, H. X., Zhou, Y., et al. (2017). Vancomycin-associated acute kidney injury: a cross-sectional study from a single center in China. PLos One 12, e0175688. doi:10.1371/journal.pone.0175688
Pritchard, L., Baker, C., Leggett, J., Sehdev, P., Brown, A., and Bayley, K. B. (2010). Increasing vancomycin serum trough concentrations and incidence of nephrotoxicity. Am. J. Med. 123, 1143–1149. doi:10.1016/j.amjmed.2010.07.025
Porter, A. M., Bland, C. M., Young, H. N., Allen, D. R., Croft, S. R., Gayheart, R. E., et al. (2019). Comparison of pharmacist-directed management of multiplex PCR blood culture results with conventional microbiology methods on effective and optimal therapy within a community hospital. Antimicrob. Agents Chemother. 63, e01575–01518. doi:10.1128/AAC.01575-18
Ran, X. W., Jia, W. P., Wang, G. Q., and Fu, X. B. (2019). Guidelines for prevention and treatment of diabetic foot in China. Chin. J. Diabetes Mellitus 11, 238–247. doi:10.3760/cma.j.issn.1674-5809.2019.02.004
Rybak, M. J., Le, J., Lodise, T. P., Levine, D. P., Bradley, J. S., Liu, C., et al. (2020). Therapeutic monitoring of vancomycin for serious methicillin-resistant Staphylococcus aureus infections: a revised consensus guideline and review by the American society of health-system pharmacists, the infectious diseases society of America, the pediatric infectious diseases society, and the society of infectious diseases pharmacists. Am. J. Health Syst. Pharm. 77, 835–864. doi:10.1093/ajhp/zxaa036
Rybak, M., Lomaestro, B., Rotschafer, J. C., Moellering, R., Craig, W., Billeter, M., et al. (2009). Therapeutic monitoring of vancomycin in adult patients: a consensus review of the American society of health-system pharmacists, the infectious diseases society of America, and the society of infectious diseases pharmacists. Am. J. Health Syst. Pharm. 66, 82–98. doi:10.2146/ajhp080434
Ueki, T., Sanematsu, E., Furuya, Y., Shinohara, Y., Murakami, Y., Miyazaki, A., et al. (2020). Relationship between vancomycin-associated nephrotoxicity and the number of combined nephrotoxic agents. Pharmazie 75, 279–283. doi:10.1691/ph.2020.0393
van Hal, S. J., Paterson, D. L., and Lodise, T. P. (2013). Systematic review and meta-analysis of vancomycin-induced nephrotoxicity associated with dosing schedules that maintain troughs between 15 and 20 milligrams per liter. Antimicrob. Agents Chemother. 57, 734–744. doi:10.1128/aac.01568-12
Willis, Z. I., and Jhaveri, R. (2018). The cost of vancomycin and piperacillin/tazobactam treatment. JAMA Pediatr. 172, 494. doi:10.1001/jamapediatrics.2018.0052
Womble, T. N., King, J. D., Hamilton, D. H., Shrout, M. A., Jacobs, C. A., and Duncan, S. T. (2019). Greater rates of acute kidney injury in african American total knee arthroplasty patients. The J. Arthroplasty 34, 1240–1243. doi:10.1016/j.arth.2019.01.058
Wu, X. W., and Ren, J. A. (2020). Guidelines for the diagnosis and treatment of abdominal cavity infection in China. Chin. J. Pract. Surg. 40, 1–16.
Yang, F. (2017). Expert consensus on penicillin skin test. Nat. Med. J. China 97, 3143–3146. doi:10.3760/cma.j.issn.0376-2491.2017.40.005
Yang, L., Xing, G., Wang, L., Wu, Y., Li, S., Xu, G., et al. (2015). Acute kidney injury in China: a cross-sectional survey. Lancet 386, 1465–1471. doi:10.1016/s0140-6736(15)00344-x
Ye, Z.-K., Chen, Y.-L., Chen, K., Zhang, X.-L., Du, G.-H., He, B., et al. (2016). Therapeutic drug monitoring of vancomycin: a guideline of the division of therapeutic drug monitoring, Chinese pharmacological society. J. Antimicrob. Chemother. 71, 3020–3025. doi:10.1093/jac/dkw254
Zhou, H., Li, G. H., Chen, B. Y., Zhuo, C., Cao, B., Yang, Y., et al. (2014). Expert consensus on strategies to cope with infections of Enterobacteriaceae with extended-spectrum β-lactamases produced in China. Nat. Med. J. China 94, 1847–1856. doi:10.3760/cma.j.issn.0376-2491.2014.24.003
Keywords: vancomycin, acute kidney injury, risk factors, renal recovery, morality
Citation: Kunming P, Can C, Zhangzhang C, Wei W, Qing X, Xiaoqiang D, Xiaoyu L and Qianzhou L (2021) Vancomycin Associated Acute Kidney Injury: A Longitudinal Study in China. Front. Pharmacol. 12:632107. doi: 10.3389/fphar.2021.632107
Received: 22 November 2020; Accepted: 01 February 2021;
Published: 08 March 2021.
Edited by:
Elena Ramírez, University Hospital La Paz, SpainReviewed by:
Welder Zamoner, São Paulo State University, BrazilLucia Llanos, Health Research Institute Foundation Jimenez Diaz (IIS-FJD), Spain
Copyright © 2021 Kunming, Can, Zhangzhang, Wei, Qing, Xiaoqiang, Xiaoyu and Qianzhou. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ding Xiaoqiang, ZGluZy54aWFvcWlhbmdAenMtaG9zcGl0YWwuc2guY24=; Li Xiaoyu, bGkueGlhb3l1QHpzLWhvc3BpdGFsLnNoLmNu; Lv Qianzhou, bHYucWlhbnpob3VAenMtaG9zcGl0YWwuc2guY24=
 Pan Kunming
Pan Kunming Chen Can
Chen Can Chen Zhangzhang1
Chen Zhangzhang1 Wu Wei
Wu Wei