
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Pharmacol., 14 January 2021
Sec. Drugs Outcomes Research and Policies
Volume 11 - 2020 | https://doi.org/10.3389/fphar.2020.588106
 Israel Abebrese Sefah1,2
Israel Abebrese Sefah1,2 Olayinka O. Ogunleye3,4
Olayinka O. Ogunleye3,4 Darius Obeng Essah1
Darius Obeng Essah1 Sylvia A. Opanga5
Sylvia A. Opanga5 Nadia Butt6
Nadia Butt6 Annie Wamaitha6
Annie Wamaitha6 Anastasia Nkatha Guantai7
Anastasia Nkatha Guantai7 Ibrahim Chikowe8
Ibrahim Chikowe8 Felix Khuluza8
Felix Khuluza8 Dan Kibuule9
Dan Kibuule9 Lahya Nambahu9
Lahya Nambahu9 Abdullahi Rabiu Abubakar10
Abdullahi Rabiu Abubakar10 Ibrahim Haruna Sani11
Ibrahim Haruna Sani11 Zikria Saleem12
Zikria Saleem12 Aubrey C. Kalungia13
Aubrey C. Kalungia13 Thuy Nguyen Thi Phuong14
Thuy Nguyen Thi Phuong14 Mainul Haque15
Mainul Haque15 Salequl Islam16
Salequl Islam16 Santosh Kumar17
Santosh Kumar17 Jacqueline Sneddon18
Jacqueline Sneddon18 Joshua Wamboga19
Joshua Wamboga19 Janney Wale20
Janney Wale20 Nenad Miljković21
Nenad Miljković21 Amanj Kurdi22,23
Amanj Kurdi22,23 Antony P. Martin24,25
Antony P. Martin24,25 Brian Godman22,26,27,28*
Brian Godman22,26,27,28*Background: Countries across Africa and Asia have introduced a variety of measures to prevent and treat COVID-19 with medicines and personal protective equipment (PPE). However, there has been considerable controversy surrounding some treatments including hydroxychloroquine where the initial hype and misinformation led to shortages, price rises and suicides. Price rises and shortages were also seen for PPE. Such activities can have catastrophic consequences especially in countries with high co-payment levels. Consequently, there is a need to investigate this further.
Objective: Assess changes in utilisation, prices, and shortages of pertinent medicines and PPE among African and Asian countries since the start of pandemic.
Our approach: Data gathering among community pharmacists to assess changes in patterns from the beginning of March until principally the end of May 2020. In addition, suggestions on ways to reduce misinformation.
Results: One hundred and thirty one pharmacists took part building on the earlier studies across Asia. There were increases in the utilisation of principally antimalarials (hydroxychloroquine) and antibiotics (azithromycin) especially in Nigeria and Ghana. There were limited changes in Namibia and Vietnam reflecting current initiatives to reduce inappropriate prescribing and dispensing of antimicrobials. Encouragingly, there was increased use of vitamins/immune boosters and PPE across the countries where documented. In addition, generally limited change in the utilisation of herbal medicines. However, shortages have resulted in appreciable price increases in some countries although moderated in others through government initiatives. Suggestions in Namibia going forward included better planning and educating patients.
Conclusion: Encouraging to see increases in the utilisation of vitamins/immune boosters and PPE. However, concerns with increased utilisation of antimicrobials needs addressing alongside misinformation, unintended consequences from the pandemic and any appreciable price rises. Community pharmacists and patient organisations can play key roles in providing evidence-based advice, helping moderate prices through improved stock management, and helping address unintended consequences of the pandemic.
We have recently published regarding ongoing activities across Africa to prevent and treat COVID-19 (Ogunleye et al., 2020). Activities to reduce the spread of COVID-19 were centered around measures to close borders, quarantine returning travellers and their contacts, restrict movement as well as track and trace citizens (Ogunleye et al., 2020). However, the various measures and initiatives were introduced at different times and with different intensities leading to differences in prevalence and mortality rates seen to date. We also see similar activities introduced among Asian countries including Bangladesh, Pakistan, and Vietnam (Table 1) with again variable impact on prevalence and mortality rates (Godman et al., 2020a; Haque et al., 2020a). Vietnam aggressively introduced a range of measures to prevent the spread of COVID-19 under the banner “Fighting the epidemic is like fighting again’t the enemy,” which together with other factors resulted in only 383 reported cases by 19 July and no deaths (Godman et al., 2020a; Jones, 2020; Pham et al., 2020; WHO, 2020a). This increased to 1,069 cases by 27 September and only 35 reported deaths (Godman et al., 2020a; WHO, 2020b). In Namibia in sub-Saharan Africa there were 1,247 reported cases and only 3 deaths up to July 19, 2020 following multiple measures (Table 1), although this is changing (Ogunleye et al., 2020; WHO, 2020b). In addition, in Ghana with its multiple activities there were only 148 recorded deaths from 27,667 confirmed cases by July 19, 2020 increasing to 46,222 confirmed cases by September 27, 2020 and 299 deaths, with Ghana seen as a model country for managing COVID-19 in sub-Saharan Africa (Ogunleye et al., 2020; WHO, 2020a; WHO, 2020b; Afriyie et al., 2020). However, it is recognised that there is severe under-reporting of prevalence rates and deaths in a number of countries due to low rates of testing and the robustness of reporting systems certainly initially (Godman et al., 2020a; Haque et al., 2020a; Ogunleye et al., 2020).
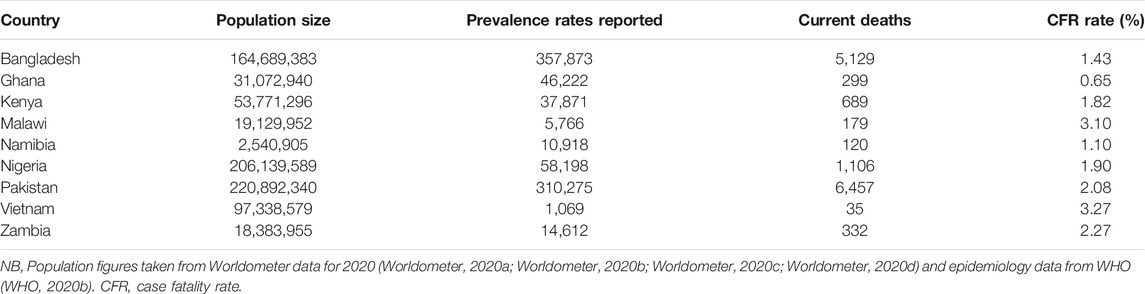
TABLE 1. Confirmed prevalence and mortality rates for COVID-19 among selected African and Asian countries (September 27, 2020).
Table 1 documents current prevalence and mortality rates for a range of African countries where there can be high co-payments for medicines, as well as high rates of self-medication with antimicrobials despite regulations banning this, with potentially catastrophic consequences for some families in a number of countries when family members become ill (Kalungia et al., 2016; McHenga et al., 2017; Afari-Asiedu et al., 2018; Aregbeshola and Khan, 2018; Salari et al., 2019; Kaonga et al., 2019; Godman et al., 2020b). We also see a similar situation in Bangladesh and Pakistan with high co-payments levels and potentially catastrophic consequences for families when members become ill (Haque, 2017; Datta et al., 2019; Hsu et al., 2018; Pakistan Today, 2020). Increased social insurance coverage has reduced out-of-pocket payments in Vietnam; however, these still exist with potentially distressing consequences for a minority of families when members become ill. In addition, a high percentage of patients in Vietnam still visit pharmacists first for their illnesses (Pekerti et al., 2017; Hoa et al., 2019; Lee et al., 2019). The situation is different in Namibia with universal healthcare, provision of well accepted guidelines, monitoring of physician prescribing against current guidance as well as regulations banning the self-purchasing of antimicrobials (Nashilongo et al., 2017; Kamati et al., 2019; Niaz et al., 2019; Niaz et al., 2020).
Supplementary Table A1 in the Appendix summarises some of the activities that the chosen Asian countries have instigated to help reduce the spread of COVID-19. Activities among the selected African and Asian countries to reduce the spread of COVID-19 can be found in Godman et al. (2020a) and Ogunleye et al. (2020).
Whilst no medicine is currently fully recommended for treating COVID-19, there has been appreciable controversy surrounding the use of chloroquine and hydroxychloroquine with or without antibiotics including azithromycin (Ogunleye et al., 2020). There was considerable hype surrounding early reports regarding the effectiveness of hydroxychloroquine in reducing the impact of COVID-19 resulting in shortages, price rises, and deaths (Abena et al., 2020; Busari and Adebayo, 2020; Nga et al., 2020; Politi, 2020). However, there were concerns regarding the efficacy data with a lack of control arms in the early studies, endorsed by later studies showing no proven benefit from using hydroxychloroquine along with potential harm (Borba et al., 2020; Ferner and Aronson, 2020; ISAC/Elsevier, 2020; International Society of Antimicrobial Chemotherapy, 2020; Horby et al., 2020; Geleris et al., 2020; Littlejohn, 2020; WHO Solidarity Trial Consortium, 2020). Following these studies, the WHO halted the hydroxychloroquine arm in its ongoing Solidarity Trial with the National Institute of Health (NIH) in the United States also halting hydroxychloroquine arms in its studies (NIH, 2020; WHO, 2020c). Alongside this, in Africa the South African Pharmacy Council warned against the misuse of hydroxychloroquine for the treatment of COVID-19, building on concerns from the South African regulatory agency regarding the lack of evidence (SAHPRA, 2020; Masango, 2020). There have been similar concerns with lopinavir-ritonavir, with most studies failing to show clinical benefit including the United Kingdom (United Kingdom) Recovery study (RECOVERY Collaborative Group, 2020; Ford et al., 2020). As a result, the WHO has now also dropped lopinavir-ritonavir from the Solidarity trial (WHO Solidarity Trial Consortium, 2020; WHO, 2020c). There are now similar concerns with remdesivir (WHO Solidarity Trial Consortium, 2020; Dyer, 2020; McCreary and Angus, 2020; Wang et al., 2020). Early premature recommendations are a concern not only in rasing false hope among patients and physicians but also potentially exposing patients to severe adverse drug reactions as well as diverting valuable resources away from funding other priority disease areas. In addition, the over use of antimicrobials will enhance resistance rates, which is already a concern across Africa and Asia (Godman et al., 2020b). This includes hydroxychloroquine with artemetherlumefantrine or artesunate-amodiaquine now typically recommended for the treatment of uncomplicated malaria across Africa with hydroxychloroquine reserved due to resistance and other concerns (WHO, 2018; Conrad and Rosenthal, 2019).
Considerable price rises of antimalarials have already been seen in Bangladesh and Nigeria as a result of the hype surrounding hydroxychloroquine, which is a concern (Busari and Adebayo, 2020; Haque et al., 2020a). Considerable price rises have also been seen for personal protective equipement (PPE) in Bangladesh and Sudan, which again causes concern if increased spending on these items following price hikes reduces available resouces for food and medicines for other high priority disease areas (Weston, 2020).
There are also concerns with the inappropriate use of medicinal plants to prevent and treat COVID-19 as this could cause more harm than good (Ekor, 2014; Liwa et al., 2014; Nkeck et al., 2020; Nordling, 2020; Yang, 2020). We are aware some herbal medicines are showing promise in treating patients with COVID-19 based on in vitro and small-scale clinical studies (Ang et al., 2020; Luo E. et al., 2020; Luo L. et al., 2020; Vellingiri et al., 2020; Yang, 2020; Zhang et al., 2020). However, their use outside of formal trials is a concern until more data becomes available especially if taking these medicines causes delay in patients seeking more appropriate care (Yang, 2020), mirroring the controversies seen with hydroxychloroquine.
There are also unintended consequences from lockdown and other measures associated with the pandemic (Godman, 2020). These include concerns with the negative impact on immunisation and prevention programmes for infectious diseases as well as reduced control of non-communicable diseases (NCDs) such as cancer, coronary vascular diseases (CVD), hypertension and type 2 diabetes (T2DM) if patients fail to collect and/or take their medicines (Basu et al, 2020; Banerjee, 2020; Chandir et al., 2020; Kluge et al., 2020; UNICEF South Africa, 2020; WHO, 2020d). Recently Abbas et al. (2020) calculated that as a result of reduced immunisation programmes from lockdown and other activities, coupled with a lack of catch-up activities as lockdown measures ease, that for every one excess COVID-19 death acquired during routine vaccination clinic visits, 84 deaths in children could be avoided (Abbas et al., 2020). Equally, any appreciable reduction in the distribution of protective bed nets (75%), coupled with a lack of medicines to treat malaria due to lockdown and other activities, combined with lack of media campaigns, could result in up to 18 million additional cases and up to 30,000 additional deaths in sub-Saharan Africa alone compared to 2018 (Krubiner et al., 2020; Cash and Patel, 2020; WHO, 2020e).
Community pharmacists can play a key role helping with immunisation programmes as well as enhancing the appropriate use of antimicrobials. This is in addition to educating patients regarding effective strategies to prevent the spread of COVID-19 as well as help address misinformation especially surronding hydroxychloroquine and herbal medicines through posters, leaflets and other media. Alongside this, working with physicians and other groups to increase access to medicines for patients espeically those with chronic NCDs through mobile telephones and other technologies (Markovic-Pekovic et al., 2017; Ahmad et al., 2020; Cadogan and Hughes, 2020; Dzingirai et al., 2020; Erku et al., 2020; FIP, 2017; FIP, 2020; Godman et al., 2020b; Kretchy et al., 2020). However, community pharmacists need to be mindful of their own potential for catching the virus and taking appropriate precautions including when re-stocking from suppliers (Dzingirai et al., 2020; Ogunleye et al., 2020). Pharmacy groups can also help address shortages through proactive measures including better stock management, which could be critical for medicines to treat malaria and other priority disease areas across Africa. This is because medicine shortages are an increasing concern among African countries where typically up to 94% of medicines are imported (N Gage Consuting, 2017; Bavier, 2020; Dugmore, 2020). This is leading to calls to increase local production, building on initiatives to address the lack of ventilators and testing equipment at the start of the pandemic in Africa, with such calls likely to continue post pandemic (EAC, 2020; GhanaWeb, 2020a; Ogunleye et al., 2020).
Consequently, we believe there is a need to rapidly determine changes in utilisation and prices as well as shortages of recommended medicines and PPE for the prevention and treatment of COVID-19 in the early stages of the pandemic especially among African countries to help guide future strategies. This includes changes in utilisation and prices of hydroxychloroquine, antibiotics especially azithromycin, and herbal medicines arising from any early endorsement. We are aware that patient groups are important to convey correct information about effective preventative measures as well as address misinformation including misconceptions about vaccines and the consequences (Anna, 2020; Ogunleye et al., 2020). We are also aware that groups such as the International Alliance of Patients’ Organizations (IAPO) have developed resource hubs to provide reliable and updated information to mitigate against misinformation and promote effective preventative activities (International Alliance of Patients’ Organizations, 2020). In addition, patient groups are vital to help reduce any stigma associated with COVID-19 (AFP-JIJI, 2020; Kamal, 2020; IFRC, UNICEF and WHO, 2020; GhanaWeb, 2020b; He et al., 2020; Ogunleye et al., 2020). However, this is outside of this current project.
We adopted a similar comprehensive strategy applied in Bangladesh (Haque et al., 2020a), and subsequently used among other Asian countries (Godman et al., 2020a; Haque et al., 2020b), building on previous knowledge of activities across Africa just before and after the first cases of COVID-19 were identified in Africa (Ogunleye et al., 2020). This included a questionnaire survey among community pharmacies in Africa including Ghana, Kenya, Namibia, Malawi, Nigeria, and Zambia as well as among three comparative Asian countries including Bangladesh, Pakistan and Vietnam. Box 1 summarises the open ended questions building on published studies (Haque et al., 2020a; Haque et al., 2020b). Impressions were requested if this was the only information available due to issues of confidentiality and culture as no payment was made to pharmacists for the information provided (Godman et al., 2020a; Haque et al., 2020a). The objective was to assess the current situation regarding usage patterns, prices, and availability of selected medicines and PPE used in prevention and management of COVID-19 soon after the start of the pandemic. The baseline was early 2020, i.e., just before active preventative measures in a number of the countries. More specific data on actual changes in utilisation and prices was asked if this was available; however, this did not include asking the pharmacists to break down changes in utilisation patterns and prices per month as this was deemed too problematic for this initial study. In addition, it was envisaged there would be limited impact of seasonality in view of year-round influenza activity in some African countries and no real pattern in others (WHO, 2012; Dawa et al., 2020; WHO Regional Office for Africa, 2020) although research is ongoing in this area to address current knowledge gaps (Sambala et al., 2018). In addition, generally limited use of hydroxychloroquine in immunological diseases such as rheumatoid arthritis with concerns over its effectiveness compared with other disease modifying therapies (Rempenault et al., 2020). A more detailed description of the questionnaire can be found in Haque et al. (2020a).
BOX 1 | Open ended questions to community pharmacists across Africa regarding pertinent medicines and equipment to prevent and treat COVID-19.
• Country?
• What changes in purchasing/utilisation patterns have you noticed in your pharmacy from the beginning of March, i.e. with the first cases being recorded and just before lockdown and other measures typically introduced, until the end of May 2020 for antimalarials (hydroxychloroquine), antibiotics (e.g. azithromycin), multivitamins including vitamin C, analgesics and herbal medicines (where pertinent)? The baseline is early 2020, i.e. pre the pandemic. Please base this information on invoices where possible or other information sources; otherwise, impressions
• What changes in the prices have you noticed for these medicines from the beginning of March until end May 2020 – again based on invoices or other information sources where possible; otherwise impressions. The baseline is again early 2020
• Have there been any shortages for these pertinent medicines from the beginning of March until end May 2020 ? If so, what has been the extent if known?
• Similarly, for PPE including face masks and other equipment such as hand sanitisers from the beginning of March until the end May 2020 (baseline early 2020) - based again on invoices or other information sources/impressions where possible
• What suggestions can you give the authorities to address misinformation regarding the current pandemic (if pertinent) as well as any inappropriate self-medication with antimicrobials for future pandemics given current concerns?
We did not factor inflation into the impressions as the study period only covered a short time, and per annum inflation in the chosen African countries typically ranged between 6 and 16% per annum (Focus Economics, 2020; Trading Economics, 2020a; Trading Economics, 2020b; Trading Economics, 2020c; Trading Economics, 2020d; Trading Economics, 2020e).
The Asian countries chosen for comparative purposes had instigated similar activities to prevent the spread of COVID-19 as those seen in Africa and where there can be high patient co-payments for medicines (Godman et al., 2020a).
Convenience sampling was again used to select pharmacists through emails, telephone contact, personal contacts and other mechanisms similar to the studies across Asia (Godman et al., 2020a; Haque et al., 2020a). As before, there was no sample size calculation as there was no previous data to base calculations upon at the start of the study and this was a pilot study with a minimum of six pharmacies contacted in all countries apart from Namibia to determine the need for additional follow-up studies.
The findings were subsequently consolidated into categories in a tabular format to aid comparisons between regions and countries, with more specific data available in country publications (Haque et al., 2020a; Haque et al., 2020b). We believed that there would be price rises and shortages in other countries apart from Bangladesh. However, the nature and extent would depend on ongoing programmes within the country.
We also explored the situation regarding the preparedness of community pharmacists in Namibia to the pandemic to help enhance future guidance to Governments and other key stakeholder groups. This included questions on i) Key measures/interventions the pharmacy has put in place during the pandemic to curb the spread of COVID-19 in the community (maximum of three from a pre-arranged list of seven known activities); ii) Suggestions on the role (current and new) of pharmacists/pharmaceutical technicians/pharmacist assistants during current and future pandemics (up to three from a pre-arranged list of five potential activities); iii) The main challenges experienced by pharmacy personnel during the pandemic (maximum of three from a pre-arranged list of seven known activities); iv) Changes in utilization, prices and shortages of pertinent medicines and PPE used in the prevention and management of COVID-19 from the beginning of March to end June 2020 (Supplementary Appendix A1). The study was extended to the end of June to provide greater insight.
Potential future guidance for governments, pharmacists and patients will build on the experiences of the pharmacists and others involved in the study in Namibia and across all the studied countries, the co-authors and previous suggestions documented in Ogunleye et al. (2020).
Ethical approval for this study was not required according to our national legislation and institutional guidelines. However, as before in Bangladesh, all pharmacists freely provided the requested information having been given the opportunity to refuse to participate. This is in line with previous studies undertaken by the co-authors in this and related areas including analysis of policies to enhance the use of biosimilars and the rationale use of medicines, pricing policies as well as issues surrounding shortages and generics, which typically involved direct contact with health authority personnel and other key stakeholders (Godman et al., 2014; Godman et al., 2015; Moorkens et al., 2017; Godman et al., 2019; Gad et al., 2020; Godman et al., 2020a; Godman et al., 2020b; Godman et al., 2020c; Godman et al., 2020d; Haque et al., 2020a; Miljković et al., 2020a).
Table 2 documents the number of community pharmacists involved in Ghana, Kenya, Namibia, Malawi, Nigeria, and Zambia as well as Pakistan and Vietnam building on the published paper of Haque et al. (2020a) and Godman et al. (2020b). As mentioned, typically pilot studies were conducted in all countries apart from Namibia to provide direction for future studies if needed building on this rapid pilot study.
Table 3 depict changes in the utilisation patterns for the various medicines, vitamins, and PPE (where documented) from the beginning of March until the end of May 2020 among the studied countries.
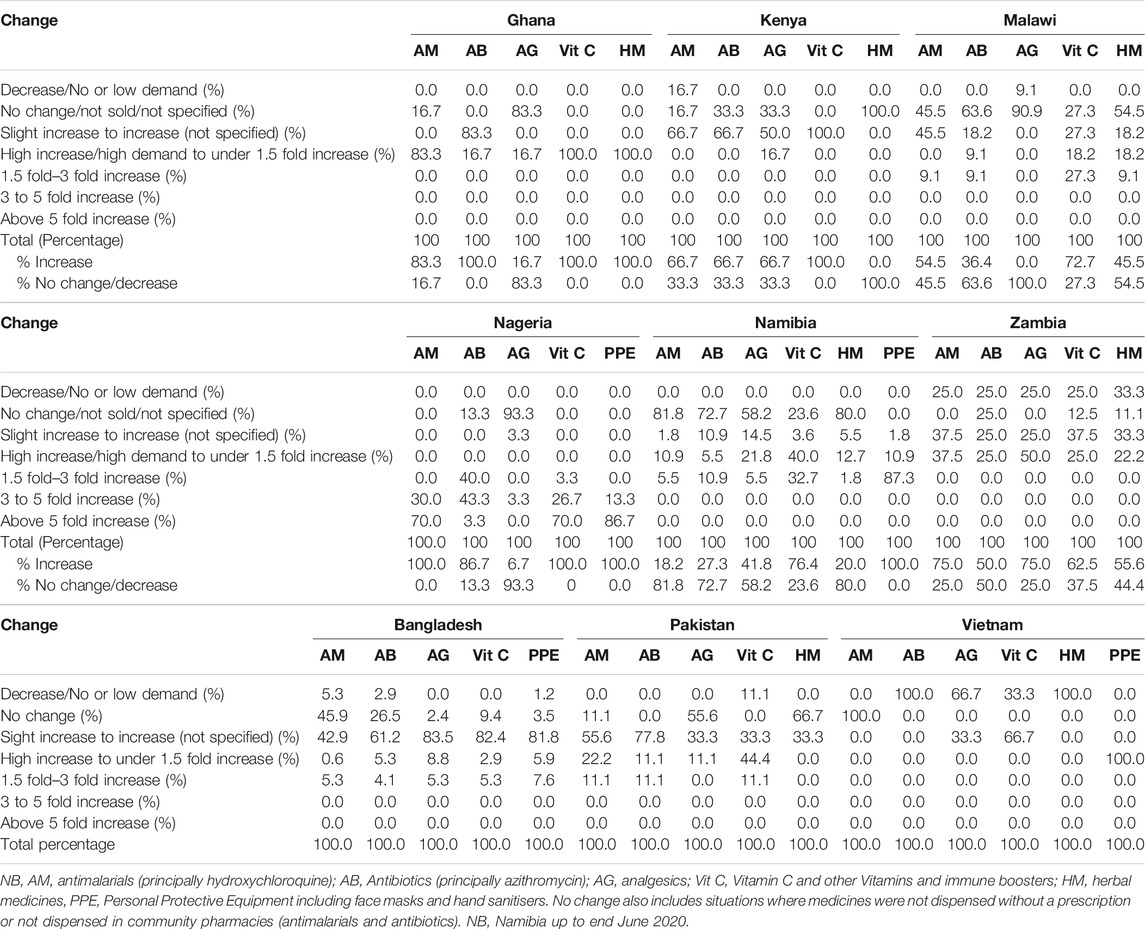
TABLE 3. Utilisation changes (percentages) for medicines and PPE between beginning March 2020 and end May 2020 among pharmacies across the countries.
There was an increase in the utilisation of antimalarials (principally hydroxychloroquine) among all the African countries, greatest in Ghana, Nigeria and Zambia (Table 3). This is similar to Pakistan although increases appear less than seen in Ghana and Nigeria, but appreciably different to Vietnam. There were also increases in the utilisation of antibiotics (principally azithromycin) among all the African countries, greatest in Ghana, Kenya and Nigeria. There was also increased utilisation of antibiotics in Pakistan vs. Bangladesh and Vietnam. There was generally more limited increase in the utilisation of analgesics across countries, with a decrease seen in Vietnam. Encouragingly, there was an increase in the utilisation of vitamins and immune boosters across countries, and similarly for PPE (Table 3). There were variable increases in the utilisation of herbal medicines among the studied countries, greatest in Ghana vs. no or limited change in Kenya and Namibia.
Table 4 depicts price changes for pertinent medicines and PPE during the study period. Again, there were differences between countries reflecting differences in utilisation rates (Table 3) and shortages (Table 5).
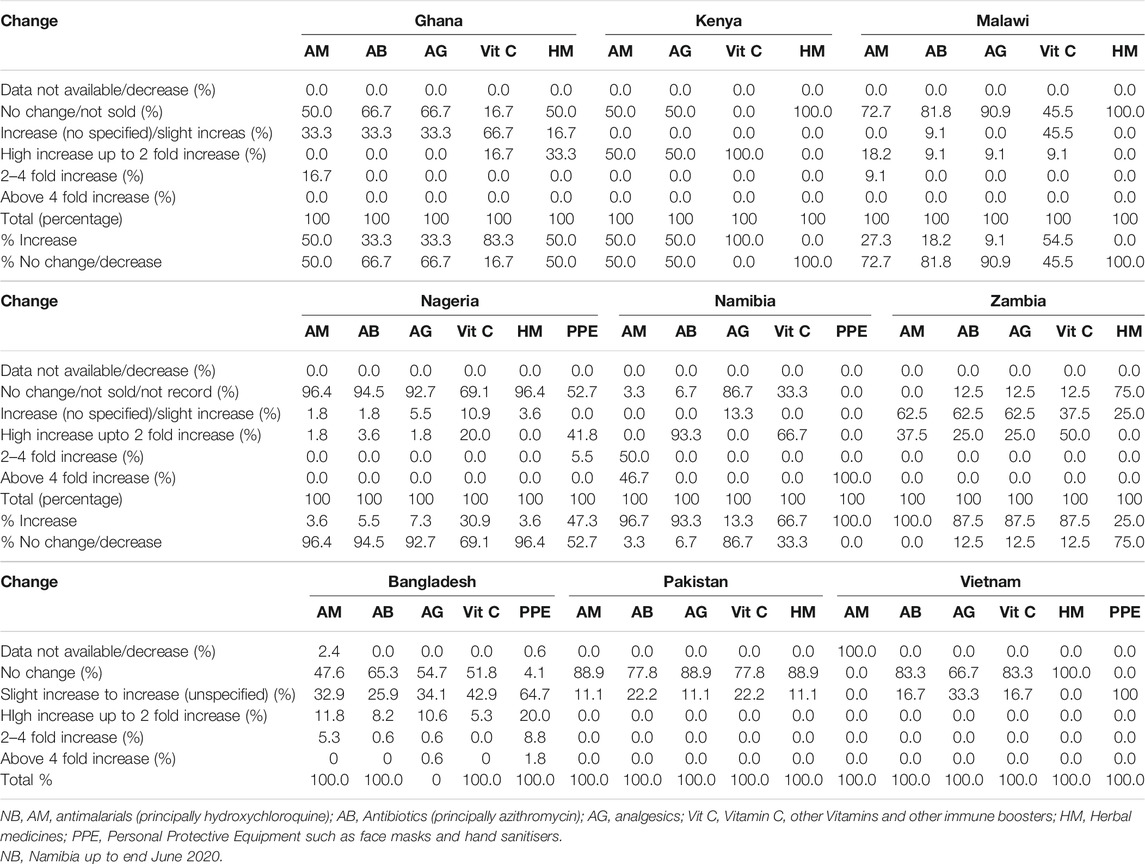
TABLE 4. Price changes for medicines and PPE between beginning March 2020 and end May 2020 among pharmacies across the countries.
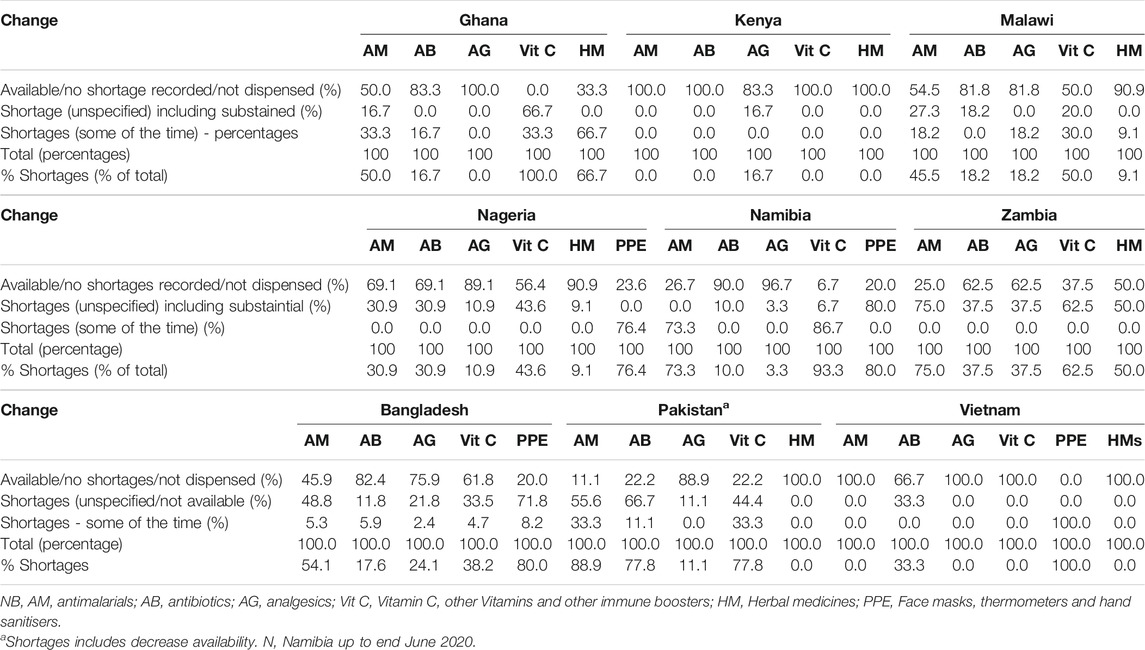
TABLE 5. Shortages for medicines and PPE between beginning March 2020 and end May 2020 among pharmacies across the countries.
There were price rises for antimalarials (hydroxychloroquine) in an appreciable number of participating pharmacies in Nigeria and Zambia during the study period, with price rises in Ghana, Kenya and Malawi some of which were appreciable. Price rises were also seen in some of the pharmacies in Bangladesh, some of which were substantial; however, not in Pakistan nor Vietnam (Table 4). There was a similar picture for antibiotics (azithromycin). We also saw price increases for analgesics in Kenya and Zambia, some of which were appreciable. However, limited or no change in most of the pharmacies in the studied countries including the three Asian countries. There were also price increases for vitamin C/immune boosters across countries, some of which were substantial, e.g., Nigeria. There were price increases for PPE among all the studied countries (Table 4).
Perhaps not surprisingly, shortages were seen for a number of the surveyed medicines across Africa, especially antimalarials (hydroxychloroquine) and vitamin C/immune boosters, mirroring the situation among the participating Asian countries (Table 5). However to a lesser extent for antibiotics (principally azithromycin) and analgesics across the studied countries (Table 5). Where recorded, shortages of PPE were seen in all countries including Kenya and Malawi (not shown as not recorded in all pharmacies visited) influencing the extent of price rises seen in practice (Table 4).
Fifty five public and private pharmacists from 10 out of the 11 regions in Namibia took part among rural (18.2% of pharmacists), semi-urban (29.1%) and urban settings (52.7% of all pharmacists). Among these, 15 out of 55 (27.3%) pharmacists were prepared for the pandemic. All of these 15 pharmacies bulk ordered medicines, sanitizers/disinfectants and PPE in anticipation of increased demand with two out of the 15 (13.3%) pharmacies also making arrangements for enough staff to be available to cope with the anticipated increase in demand.
Pharmacists had put in place a number of measures to help curb the spread of COVID-19 with promoting prevention including hand sanitization and social distancing key suggested activities. These are described in Table 6 with all pharmacists (55 in all) putting in place at least one measure, 51 (92.7%) pharmacists instigating at least two measures and 23 pharmacists (41.8%) three measures – with only a maximum of three asked in the questionnaire.
Table 7 contains suggestions from pharmacists, pharmaceutical technicians, and pharmacist assistants on their current and future potential roles to reduce the spread of any virus during a pandemic, with educating patients and advising on potential treatment plans key activities going forward. 53 pharmacists (96.4%) suggested one role, 28 (50.1%) two roles and one pharmacist three roles.
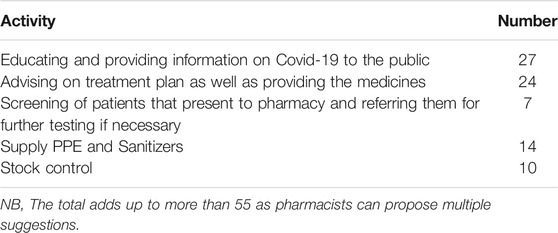
TABLE 7. Suggestions on the role of pharmacists/pharmaceutical technicians/pharmacist assistant during this pandemic.
Table 8 discusses the principal challenges experienced by pharmacy personnel in Namibia during the pandemic. 54 (98.2%) pharmacists documented one challenge, 26 (47.3%) two challenges and two pharmacists (3.6%) three challenges. Not surprisingly, inadequate stock of PPE and other preventative measures were key challenges building on observations documented in Table 6.
Potential ways forward for all key stakeholder groups are contained in Table 9, building on comments in Tables 7 and 8 as well as the feedback from other community pharmacists and the co-authors from across Africa and other countries.
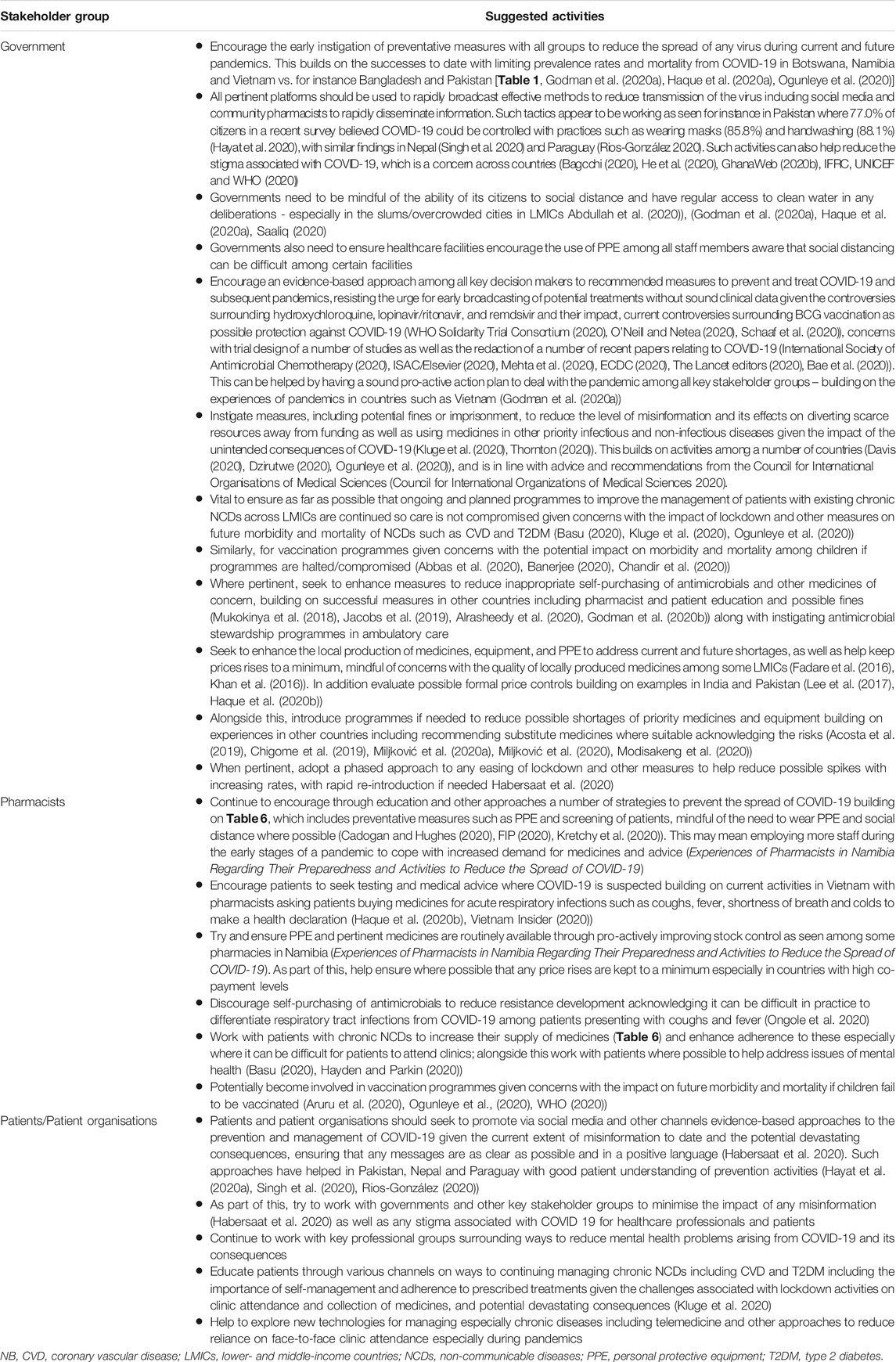
TABLE 9. Potential activities among stakeholder groups to improve prevention and management of patients with COVID-19.
We believe this is the first study undertaken across Africa, as well as a number of Asian countries, to rapidly assess the impact of information, misinformation, and advice regarding pertinent technologies to prevent and treat COVID-19, including hydroxychloroquine with or without azithromycin, on subsequent utilisation, shortages and prices in the first few months following the pandemic. Pertinent medicines included antimalarials (hydroxychloroquine), antibiotics including azithromycin, analgesics as well as vitamins and immune boosters.
There were increases in the utilisation of antimalarials (hydroxychloroquine) across most African countries with the exception of Namibia, with more modest increases in Kenya and Malawi vs. for instance Nigeria. This may reflect greater control on the prescribing and dispensing of antimalarial treatments in these countries; however, further research is need before any definitive statements can be made. There was also increased utilisation of antimalarials in Bangladesh and Pakistan but not in Vietnam (Table 3). This may again reflect greater controls on the dispensing of antimalarials in Vietnam, although further research is needed to confirm this (Godman et al., 2020a).
There were also increases in the utilisation of antibiotics across most of the studied African countries as well as Bangladesh and Pakistan although typically more modest compared with changes in the utilisation of antimalarials, with an actual reduction in utilisation in Vietnam (Table 3). This may reflect a more conscious effort not to dispense antibiotics for suspected viral infections in Malawi, Namibia, and Vietnam; however, further research is needed before any definitive statements can be made. Increases in the utilisation of antimicrobials across countries is a concern as this will increase resistance rates (Llor and Bjerrum, 2014; Wojkowska-Mach et al., 2018; Wu et al., 2018; Godman et al., 2020b). Multiple strategies including educational strategies and antimicrobial stewardship programmes are typically needed among all key stakeholders in ambulatory care to reduce inappropriate prescribing and dispensing of antimicrobials, building on successful activities across lower- and middle-income countries (LMICs) (Bojanic et al., 2018; Mukokinya et al., 2018; Bishop et al., 2019; Jacobs et al., 2019; Godman et al., 2020b; Ogunleye et al., 2020). However, fining pharmacists for breaking current legislation may be difficult to enforce especially in rural areas of Africa where community pharmacists are typically the principal healthcare professional available and where there are no physician fees to contend with in the absence of universal healthcare (Kalungia and Godman, 2019; Alrasheedy et al., 2020). Other strategies may though be needed to reduce inappropriate dispensing of antimicrobials. These include greater education in pharmacy school to address information gaps regarding antimicrobials and antimicrobial resistance (AMR), developing and implementing national guidelines for the management of infectious diseases typically seen in ambulatory care acknowledging the WHO AWaRe list of antibiotics, as well as monitoring community pharmacists’ activities through for instance mobile technologies (Markovic-Pekovic et al., 2017; Hoxha et al., 2018; Kalungia and Godman, 2019; Saleem et al., 2019; Saleem et al., 2020). Community pharmacists should be mindful though that it can be difficult in practice to differentiate respiratory tract infections from COVID-19 among patients presenting with coughs and fever (Ongole et al., 2020), and they should encourage testing and referrals where there are concerns.
Encouragingly, there was increased use of vitamins/immune boosters across all the studied countries, with appreciable increases in some, mirroring the situation in Bangladesh, Pakistan and Vietnam (Table 3). Differences in utilisation rates between the countries may simply reflect different prevalence rates for COVID-19. However, more research is needed before any definitive statements can be made. There was also increased utilisation of analgesics among the studied countries; however, typically to a lesser degree than seen with vitamins/immune boosters. Again, differences may reflect different prevalence rates and other factors across countries. Encouragingly as well, there were appreciable increases in the utilisation of PPE where recorded (Table 3). This included Malawi where increases of up to two-fold were seen where recorded.
There was also appreciable increases in the prices for antimalarials (hydroxychloroquine) during the study period across a number of the studied countries including Bangladesh and Nigeria, with the latter building on earlier observations (Busari and Adebayo, 2020; Godman et al., 2020a; Haque et al., 2020a); however, to a lesser extent in Namibia and Pakistan (Table 4). This may well reflect some of the shortages seen in these countries (Table 5); however, further research is needed. We believe the limited price increases seen in Pakistan reflects greater price controls for medicines in the country than seen in a number of other countries (Lee et al., 2017; Godman et al., 2020a). There was a similar situation for antibiotics (principally azithromycin) (Tables 4 and 5) as well as for vitamins/immune boosters. Nigeria recorded the largest price increase among the African and Asian countries for antibiotics and vitamins (Table 4) potentially reflecting the shortages seen with vitamins but not necessarily with antibiotics (Table 5). Further studies though are needed before any definitive statements can be made.
Encouragingly as well, there were limited price increases for analgesics across the studied countries apart from Zambia, perhaps reflecting more limited increases in utilisation (Table 3). Where recorded, there were also price increases for PPE across the countries, again potentially reflecting appreciable increases in utilisation and shortages during the study period (Tables 3 and 5). However, again further research is needed before we can say anything with certainty. In Malawi, there were also price increase for PPE up to 50% to double in the majority of situations where this was recorded.
Lastly, it was also encouraging to see limited changes in the utilisation of herbal medicines among the studied countries (Table 3), with typically limited shortages apart from Ghana and Namibia. This is important given, as mentioned, that the inappropriate use of medicinal plants to prevent and treat COVID-19 can cause more harm than good (Ekor, 2014; Liwa et al., 2014; Nkeck et al., 2020; Nordling, 2020; Yang, 2020), and should be avoided until more information becomes available.
Potential ways forward to improve prevention and management of patients with COVID-19 among key stakeholder groups, and for future pandemics, are contained in Table 9. This includes potential ways to address concerns with shortages of medicines and PPE, including greater pro-activity, and suggesting possible alternatives with care, as well as increasing local production. These build on the suggestions among the pharmacists in Namibia (Table 8). We are already seeing activities within African countries, as well as consortium forming across Africa, to address current shortages with medicines and equipment including greater local production, and this is likely to grow, building on innovations with the production of ventilators across a number of African countries (Afriyie et al., 2020; EAC, 2020; Bissada, 2020; Kaine and Nwokik, 2020; Ogunleye et al., 2020; South African Government, 2020). However, there needs to be care with the quality of locally produced medicines given some concerns including the quality of generics (Fadare et al., 2016; Khan et al., 2016).
Suggestions outlined in Table 9 also include potential ways forward with community pharmacists, patient organisations, and others, to address the unintended consequences of COVID-19, especially if lockdown and other activities continue to adversely affect immunisation and prevention programmes for infectious diseases such as malaria. In addition, increase morbidity associated with NCDs such as CVD and T2DM if medicines are not being taken correctly. We will be following this up in the future.
We are aware of a number of limitations with this study. These include the fact that we only approached a limited number of pharmacists among the studied countries with the exception of Namibia as this was principally a pilot study in these countries to gain a rapid assessment of the current situation given concerns with shortages, price rises and deaths with some of the recommended medicines and strategies. In addition, we were unable to obtain exact details on changes in the utilisation and prices of pertinent medicines and PPEs from all the pharmacists visited due to issues of confidentiality, culture with lack of payment, available time with them and having the relevant information readily to hand when visited. Consequently, we could only collect impressions regarding any changes among a number of the visited pharmacists, which will be subject to bias. We were also unable to undertake any time series analysis or assess issues such as seasonality as we were primarily interested in changes post the pandemic; however, concerns with seasonality appear less of an issue among the African countries for the reasons stated. Despite these limitations, we believe our findings from this rapid study do provide direction for future research as well as address some of the concerns regarding the pandemic especially the impact of misinformation and shortages for patient care in this and other priority diseases.
We have seen increases in the utilisation and prices for both antimalarials, principally hydroxychloroquine, and antibiotics, principally azithromycin, among the studied African and Asian countries arising from the COVID-19 pandemic, with considerable increases in some of the countries. These increases in antimicrobial utilisation need addressing where there are concerns through educational and other activities in order to prevent future rises in AMR. Community pharmacies, patient organisations, and others can play a key role in this respect as well as reduce the impact of any misinformation given the consequences experienced among countries.
Community pharmacists, patient organisations, and others, can also help address the unintended consequences from lockdown activities. These include addressing potential increases in infectious diseases from reduced immunisation and prevention programmes as well as helping to counteract greater morbidity from NCDs through addressing concerns with medicine availability and consumption, and we will be monitoring this in the future. Encouragingly, there was increased use of vitamins/immune boosters and PPE among the studied countries, which is likely to continue. However, this remains to be shown. The apparent considerable price rises seen for medicines and PPE in countries with existing high co-payment levels is a concern as this will impact on available resources for treating other priority infectious and non-infectious diseases. This urgently needs addressing, with community pharmacists again potentially playing an appreciable role alongside the Government.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
IS, OO, MH, AK, JS, NM and BG devised the concept for the paper. IS, DE, SO, ND, AW, IC, FK, DK, LH, AA, IS, ZS, AK and TP collected the data. All authors contributed to developing the paper and approving the final submissiom.
AM was employed by HCD Economics during this study.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fphar.2020.588106/full#supplementary-material.
Abbas, K., Procter, S. R., van Zandvoort, K., Clark, A., Funk, S., Mengistu, T., et al. (2020). Routine childhood immunisation during the COVID-19 pandemic in Africa: a benefit-risk analysis of health benefits versus excess risk of SARS-CoV-2 infection. Lancet Glob. Health 8, E1264–E1272. doi:10.1016/S2214-109X(20)30308-9
Abdullah, A., Arif, M., Macktoom, S., Saleem, A., Toheed, M., Anwar, N. H., et al. (2020). Why the COVID-19 crisis is an urban crisis. Available at: https://www.dawn.com/news/1544933.
Abena, P. M., Decloedt, E. H., Bottieau, E., Suleman, F., Adejumo, P., Sam-Agudu, N. A., et al. (2020). Chloroquine and hydroxychloroquine for the prevention or treatment of COVID-19 in Africa: caution for inappropriate off-label use in healthcare settings. Am. J. Trop. Med. Hyg. 102 (6), 1184–1188. doi:10.4269/ajtmh.20-0290
Acosta, A., Vanegas, E. P., Rovira, J., Godman, B., and Bochenek, T. (2019). Medicine shortages: gaps between countries and global perspectives. Front. Pharmacol. 10, 763. doi:10.3389/fphar.2019.00763
Afari-Asiedu, S., Kinsman, J., Boamah-Kaali, E., Abdulai, M. A., Gyapong, M., Sankoh, O., et al. (2018). To sell or not to sell; the differences between regulatory and community demands regarding access to antibiotics in rural Ghana. J. Pharm. Policy Pract. 11 (1), 30. doi:10.1186/s40545-018-0158-6
AFP-JIJI (2020). Coronavirus stigma weighs heavily in sub-Saharan Africa. Available at: https://www.japantimes.co.jp/news/2020/05/20/world/social-issues-world/virus-stigma-sub-saharan-africa/#.XsYjk2hKjIU.
Afriyie, D. K., Asare, G. A., Amponsah, S. K., and Godman, B. (2020). COVID-19 pandemic in resource-poor countries: challenges, experiences and opportunities in Ghana. J. Infect. Dev. Ctries 14 (8), 838–843. doi:10.3855/jidc.12909
Ahmad, A., Alkharfy, K. M., Alrabiah, Z., and Alhossan, A. (2020). Saudi Arabia, pharmacists and COVID-19 pandemic. J. Pharm. Policy Pract. 13 (1), 41. doi:10.1186/s40545-020-00243-1
Alrasheedy, A. A., Alsalloum, M. A., Almuqbil, F. A., Almuzaini, M. A., Aba Alkhayl, B. S., Albishri, A. S., et al. (2020). The impact of law enforcement on dispensing antibiotics without prescription: a multi-methods study from Saudi Arabia. Expert Rev. Anti Infect. Ther. 18 (1), 87–97. doi:10.1080/14787210.2020.1705156.
Ang, L., Lee, H. W., Choi, J. Y., Zhang, J., and Soo Lee, M. (2020). Herbal medicine and pattern identification for treating COVID-19: a rapid review of guidelines. Integr. Med. Res. 9 (2), 100407. doi:10.1016/j.imr.2020.100407
Anna, C. (2020). Protest vs. Africa’s 1st COVID-19 vaccine trial shows fears. Available at: https://news.yahoo.com/protest-vs-africas-1st-covid-102207018.html.
Aregbeshola, B. S., and Khan, S. M. (2018). Out-of-pocket payments, catastrophic health expenditure and poverty among households in Nigeria 2010. Int. J. Health Pol. Manag. 7 (9), 798–806. doi:10.15171/ijhpm.2018.19
Aruru, M., Truong, H. A., and Clark, S. (2020). Pharmacy emergency preparedness and response (PEPR): a proposed framework for expanding pharmacy professionals’ roles and contributions to emergency preparedness and response during the COVID-19 pandemic and beyond. Res. Soc. Adm. Pharm. S1551–7411, 30323–30325. doi:10.1016/j.sapharm.2020.04.002
Bae, S., Kim, M. C., Kim, J. Y., Cha, H. H., Lim, J. S., Jung, J., et al. (2020). Notice of retraction: effectiveness of surgical and cotton masks in blocking SARS-CoV-2. Ann. Intern. Med. 173, 79. doi:10.7326/L20-0745
Bagcchi, S. (2020). Stigma during the COVID-19 pandemic. Lancet Infect. Dis. 20 (7), 782. doi:10.1016/S1473-3099(20)30498-9
Banerjee, S. K. (2020). Dealing with immunisation during the COVID-19 pandemic: India’s experience. Available at: https://www.europeanpharmaceuticalreview.com/article/119520/dealing-with-immunisation-during-the-covid-19-pandemic-indias-experience/.
Basu, S. (2020). Non-communicable disease management in vulnerable patients during COVID-19. Indian J. Med. Ethics V (2), 103–105. doi:10.20529/IJME.2020.041
Bavier, J. (2020). At least 300,000 Africans expected to die in pandemic. U.N. Agency Available at: https://www.reuters.com/article/us-health-coronavirus-africa-un/at-least-300000-africans-expected-to-die-in-pandemic-u-n-agency-idUSKBN21Z1LW.
Bishop, C., Yacoob, Z., Knobloch, M. J., and Safdar, N. (2019). Community pharmacy interventions to improve antibiotic stewardship and implications for pharmacy education: a narrative overview. Res. Soc. Adm. Pharm. 15 (6), 627–631. doi:10.1016/j.sapharm.2018.09.017
Bissada, A.-M. (2020). Coronavirus: 3D print of ventilators, easy and cheap to produce says lead researcher. Available at: https://www.theafricareport.com/28212/coronavirus-3d-print-of-ventilators-easy-and-cheap-to-produce-says-lead-researcher/.
Bojanic, L., Markovic-Pekovic, V., Skrbic, R., Stojakovic, N., Ethermanovic, M., Bojanic, J., et al. (2018). Recent initiatives in the republic of srpska to enhance appropriate use of antibiotics in ambulatory care; their influence and implications. Front. Pharmacol. 9, 442. doi:10.3389/fphar.2018.00442
Borba, M. G. S., Almeida Val, F. F., Sampaio, V. S., Alexandre, M. A. A., Melo, G. C., Brito, M., et al. (2020). Chloroquine diphosphate in two different dosages as adjunctive therapy of hospitalized patients with severe respiratory syndrome in the context of coronavirus (SARS-CoV-2) infection: preliminary safety results of a randomized, double-blinded, phase IIb clinical trial (Cloro COVID-19 Study). medRxiv preprint. doi:10.1101/2020.04.07.20056424 Available at: https://www.medrxiv.org/content/10.1101/2020.04.07.20056424v2.full.pdf.
Busari, S., and Adebayo, B. (2020). Nigeria records chloroquine poisoning after Trump endorses it for coronavirus treatment. Available at: https://www.cnnphilippines.com/world/2020/3/23/nigeria-chloroquine-poisoning-trump-coronavirus.html.
Cadogan, C. A., and Hughes, C. M. (2020). On the frontline against COVID-19: community pharmacists’ contribution during a public health crisis. Res. Soc. Adm. Pharm. S1551–7411, 30292–30298. doi:10.1016/j.sapharm.2020.03.015
Cash, R., and Patel, V. (2020). Has COVID-19 subverted global health? Lancet 395, 1687–1688. doi:10238, P1687-1688, MAY 30, 2020
Chandir, S., Siddiqi, D. A., Setayesh, H., and Khan, A. J. (2020). Impact of COVID-19 lockdown on routine immunisation in Karachi, Pakistan. Lancet Glob. Health 8, e1118–e1120. doi:10.1016/S2214-109X(20)30290-4
Chigome, A. K., Matlala, M., Godman, B., and Meyer, J. C. (2019). Availability and use of therapeutic interchange policies in managing antimicrobial shortages among South African public sector hospitals; findings and implications. Antibiotics (Basel) 9 (1), 4. doi:10.3390/antibiotics9010004
Conrad, M. D., and Rosenthal, P. J. (2019). Antimalarial drug resistance in Africa: the calm before the storm? Lancet Infect. Dis. 19 (10), e338–e351. doi:10.1016/S1473-3099(19)30261-0
Council for International Organizations of Medical Sciences (2020). Medicines assessment during public health emergencies needs good science, best practices and proper communication. Available at: https://cioms.ch/wp-content/uploads/2020/06/CIOMS_WGXII_Statement.pdf.
Datta, B. K., Husain, M. J., and Asma, S. (2019). Assessing the relationship between out-of-pocket spending on blood pressure and diabetes medication and household catastrophic health expenditure: evidence from Pakistan. Int. J. Equity Health 18 (1), 9. doi:10.1186/s12939-018-0906-x
Davis, R. (2020). Viral outbreak: fake news spreads in SA in tandem with COVID-19. Available at: https://www.dailymaverick.co.za/article/2020-03-31-viral-outbreak-fake-news-spreads-in-sa-in-tandem-with-covid-19/.
Dawa, J., Emukule, G. O., Barasa, E., Widdowson, M. A., Anzala, O., van Leeuwen, E., et al. (2020). Seasonal influenza vaccination in Kenya: an economic evaluation using dynamic transmission modelling. BMC Med. 18 (1), 223. doi:10.1186/s12916-020-01687-7
Dugmore, H. (2020). COVID-19 leaves SA at the mercy of overseas drug exporters. Available at: https://mg.co.za/article/2020-03-25-covid-19-leaves-sa-at-the-mercy-of-overseas-drug-exporters/.
Dyer, O. (2020). COVID-19: remdesivir has little or no impact on survival, WHO trial shows. BMJ 371, m4057. doi:10.1136/bmj.m4057
Dzingirai, B., Matyanga, C. M. J., Mudzviti, T., Siyawamwaya, M., and Tagwireyi, D. (2020). Risks to the community pharmacists and pharmacy personnel during COVID-19 pandemic: perspectives from a low-income country. J. Pharm. Policy Pract. 13 (1), 42. doi:10.1186/s40545-020-00250-2
Dzirutwe, M. (2020). Zimbabwe president threatens 20 years jail over fake COVID-19 statement. Available at: https://www.sowetanlive.co.za/news/africa/2020-04-14-zimbabwe-president-threatens-20-years-jail-over-fake-covid-19-statement/.
EAC (2020). EAC partner states directed to support local production of essential medical products and supplies to combat COVID-19 in the region. Available at: https://www.eac.int/press-releases/147-health/1724-eac-partner-state-directed-to-support-local-prodcution-of-essential-medical-products-and-suupliees-to-combat-covid-19-in-the-region.
ECDC (2020). Vaccines and treatment of COVID-19. Available at: https://www.ecdc.europa.eu/en/covid-19/latest-evidence/vaccines-and-treatment.
Ekor, M. (2014). The growing use of herbal medicines: issues relating to adverse reactions and challenges in monitoring safety. Front. Pharmacol. 4 177. doi:10.3389/fphar.2013.00177
Erku, D. A., Belachew, S. A., Abrha, S., Sinnollareddy, M., Thomas, J., Steadman, K. J., et al. (2020). When fear and misinformation go viral: pharmacists’ role in deterring medication misinformation during the ‘infodemic’ surrounding COVID-19. Res. Soc. Adm. Pharm. S1551–7411, 30455-1. doi:10.1016/j.sapharm.2020.04.032
Fadare, J. O., Adeoti, A. O., Desalu, O. O., Enwere, O. O., Makusidi, A. M., Ogunleye, O., et al. (2016). The prescribing of generic medicines in Nigeria: knowledge, perceptions and attitudes of physicians. Expert Rev. Pharm. Outcomes Res. 16 (5), 639–650. doi:10.1586/14737167.2016.1120673
Ferner, R. E., and Aronson, J. K. (2020). Chloroquine and hydroxychloroquine in COVID-19. BMJ 369, m1432. doi:10.1136/bmj.m1432
FIP (2017). FIP statement of policy - control of antimicrobial medicines resistance (AMR). Available at: http://www.fip.org/www/uploads/database_file.php?id=289&table_id.
FIP (2020). Fip health advisory coronavirus SARS-COV-2/COVID-19 pandemic: information and interim guidelines for pharmacists and the pharmacy workforce. Available at: https://www.fip.org/files/content/priority-areas/coronavirus/Coronavirus-guidance-update-ENGLISH.pdf.
Focus Economics (2020). Kenya inflation March 2020. Available at: https://www.focus-economics.com/countries/kenya/news/inflation/inflation-drops-in-march.
Ford, N., Vitoria, M., Rangaraj, A., Norris, S. L., Calmy, A., and Doherty, M. (2020). Systematic review of the efficacy and safety of antiretroviral drugs against SARS, MERS or COVID-19: initial assessment. J. Int. AIDS Soc. 23 (4), e25489. doi:10.1002/jia2.25489
Gad, M., Salem, A., Oortwijn, W., Hill, R., and Godman, B. (2020). Mapping of current obstacles for rationalizing use of medicines (CORUM) in europe: current situation and potential solutions. Front. Pharmacol. 11, 144. doi:10.3389/fphar.2020.00144
Geleris, J., Sun, Y., Platt, J., Zucker, J., Baldwin, M., Hripcsak, G., et al. (2020). Observational study of hydroxychloroquine in hospitalized patients with COVID-19. N. Engl. J. Med. 382 (25), 2411–2418. doi:10.1056/NEJMoa2012410
GhanaWeb (2020a). Pharmaceutical companies to produce 70% of country’s drug needs. Available at: https://www.ghanaweb.com/GhanaHomePage/NewsArchive/Pharmaceutical-companies-to-produce-70-of-country-s-drug-needs-936016.
GhanaWeb (2020b). Coronavirus: stop discriminating against recovered patients. Available at: https://www.ghanaweb.com/GhanaHomePage/NewsArchive/Coronavirus-Stop-discriminating-against-recovered-patients-Fred-Drah-926353.
Godman, B., Wettermark, B., van Woerkom, M., Fraeyman, J., Alvarez-Madrazo, S., Berg, C., et al. (2014). Multiple policies to enhance prescribing efficiency for established medicines in Europe with a particular focus on demand-side measures: findings and future implications. Front. Pharmacol. 5, 106. doi:10.3389/fphar.2014.00106
Godman, B., Wilcock, M., Martin, A., Bryson, S., Baumgärtel, C., Bochenek, T., and de Bruyn, M. (2015). Generic pregabalin; current situation and implications for health authorities, generics and biosimilars manufacturers in the future. GaBI J. 4 (3), doi:10.5639/gabij.2015.0403.028125–135
Godman, B., Hill, A., Simoens, S., Kurdi, A., Gulbinovič, J., Martin, A. P., et al. (2019). Pricing of oral generic cancer medicines in 25 European countries; findings and implications. GaBI J. 8 (2), 49–70. doi:10.5639/gabij.2019.0802.007
Godman, B. (2020). Combating COVID-19: lessons learnt particularly among developing countries and the implications. Bangladesh J. Medi. Sci. 19 S103–S108. doi:10.3329/bjms.v19i0.48413
Godman, B., Haque, M., Islam, S., Iqbal, S., Urmi, U. L., Kamal, Z. M., et al. (2020a). Rapid assessment of price instability and paucity of medicines and protection for COVID-19 across Asia: findings and public health implications for the future. Front. Public Health. doi:10.3389/fpubh.2020.585832
Godman, B., Haque, M., McKimm, J., Abu Bakar, M., Sneddon, J., Wale, J., et al. (2020b). Ongoing strategies to improve the management of upper respiratory tract infections and reduce inappropriate antibiotic use particularly among lower and middle-income countries: findings and implications for the future. Curr. Med. Res. Opin. 36 (2), 301–327. doi:10.1080/03007995.2019.1700947
Godman, B., Basu, D., Pillay, Y., Mwita, J. C., Rwegerera, G. M., Anand Paramadhas, B. D., et al. (2020c). Review of ongoing activities and challenges to improve the care of patients with type 2 diabetes across Africa and the implications for the future. Front. Pharmacol. 11, 108. doi:10.3389/fphar.2020.00108
Godman, B., McCabe, H., Leong, T. D., Mueller, D., Martin,, A. P., Hoxha, I., et al. (2020d). Fixed dose drug combinations - are they pharmacoeconomically sound? Findings and implications especially for lower- and middle-income countries. Expert Rev. Pharm. Outcomes Res. 20 (1), 1–26. doi:10.1080/14737167.2020.1734456
Habersaat, K. B., Betsch, C., Danchin, M., Sunstein, C. R., Böhm, R., Falk, A., et al. (2020). Ten considerations for effectively managing the COVID-19 transition. Nat. Hum. Behav. 4, 677–687. doi:10.1038/s41562-020-0906-x
Haque, M. (2017). Antimicrobial use, prescribing, and resistance in selected ten selected developing countries: a brief overview. Asian J. Pharmaceut. Clin. Res. 10 (8), 37–45. 10.22159/ajpcr.2017.v10i8.19468
Haque, M., Islam, S., Iqbal, S., Urmi, U. L., Kamal, Z. M., Shuvo, S. A., et al. (2020a). Availability and price changes of potential medicines and equipment for the prevention and treatment of COVID-19 among pharmacy and drug stores in Bangladesh; findings and implications. Bangladesh J. Med. Sci. 19, S36–S50. doi:10.3329/bjms.v19i0.48106
Haque, M., Kumar, S., Charan, J., Bhatt, R., Islam, S., Dutta, S., et al. (2020b). Utilisation, availability and price changes of medicines and protection equipment for COVID-19 in India: findings and implications Short title: COVID-19 and price changes of treatments in India. Front. Pharmacol. doi:10.3389/fphar.2020.582154
Hayat, K., Rosenthal, M., Xu, S., Arshed, M., Li, P., Zhai, P., et al. (2020). View of Pakistani residents toward coronavirus disease (COVID-19) during a rapid outbreak: a rapid online survey. Int. J. Environ. Res. Publ. Health 17, 10. doi:10.3390/ijerph17103347
Hayden, J. C., and Parkin, R. (2020). The challenges of COVID-19 for community pharmacists and opportunities for the future. Ir. J. Psychol. Med. 37 (3), 198–203. doi:10.1017/ipm.2020.52
He, J., He, L., Zhou, W., Nie, X., and He, M. (2020). Discrimination and social exclusion in the outbreak of COVID-19. Int. J. Environ. Res. Publ. Health 17, 8. doi:10.3390/ijerph17082933
Hoa, N. T., Tam, N. M., Derese, A., Markuns, J. F., and Peersman, W. (2019). Patient experiences of primary care quality amongst different types of health care facilities in central Vietnam. BMC Health Servic. Res. 19 (1), 275. doi:10.1186/s12913-019-4089-y
Horby, P., Mafham, M., Linsell, L., Bell, J. L., Staplin, N., Emberson, J. R., et al. (2020). Effect of hydroxychloroquine in hospitalized patients with COVID-19. N. Engl. J. Med. 383, 2030–2040. doi:10.1056/NEJMoa2022926
Hoxha, I., Malaj, A., Kraja, B., Bino, S., Oluka, M., Markovic-Pekovic, V., et al. (2018). Are pharmacists’ good knowledge and awareness on antibiotics taken for granted? The situation in Albania and future implications across countries. J. Glob. Antimicrob. Resist. 13, 240–245. doi:10.1016/j.jgar.2018.01.019
Hsu, J., Flores, G., Evans, D., Mills, A., and Hanson, K. (2018). Measuring financial protection against catastrophic health expenditures: methodological challenges for global monitoring. Int. J. Equity Health 17 (1), 69. doi:10.1186/s12939-018-0749-5
IFRC, UNICEF and WHO (2020). Social stigma associated with COVID-19. Available at: https://reliefweb.int/sites/reliefweb.int/files/resources/covid19-stigma-guide.pdf.
International Alliance of Patients’ Organizations (2020). COVID-19 resources hub. Available at: https://www.iapo.org.uk/covid-19-resources-hub.
International Society of Antimicrobial Chemotherapy (2020). Official Statement from International Society of Antimicrobial Chemotherapy (ISAC) - hydroxychloroquine and azithromycin as a treatment of COVID-19: results of an open-label non-randomized clinical trial (Gautret P et al. PMID 32205204). Available at: https://www.isac.world/news-and-publications/official-isac-statement.
ISAC/Elsevier (2020). Joint ISAC and Elsevier statement on Gautret et al. paper [PMID 32205204]. Available at: https://www.isac.world/news-and-publications/isac-elsevier-statement.
Jacobs, T. G., Robertson, J., van den Ham, H. A., Iwamoto, K., Bak Pedersen, H., and Mantel-Teeuwisse, A. K. (2019). Assessing the impact of law enforcement to reduce over-the-counter (OTC) sales of antibiotics in low- and middle-income countries; a systematic literature review. BMC Health Services Res. 19 (1), 536. doi:10.1186/s12913-019-4359-8
Jones, A. (2020). Coronavirus: how ‘overreaction’ made Vietnam a virus success. Available at: https://www.bbc.co.uk/news/world-asia-52628283.
Kaine, E., and Nwokik, J. (2020). scaling up african pharmaceutical manufacturing in a time of COVID-19. Available at: https://www.cfr.org/blog/scaling-african-pharmaceutical-manufacturing-time-covid-19.
Kalungia, A., and Godman, B. (2019). Implications of non-prescription antibiotic sales in China. Lancet Infect. Dis. 19 (12), 1272–1273. doi:10.1016/S1473-3099(19)30408-6
Kalungia, A. C., Burger, J., Godman, B., Costa, J. O., and Simuwelu, C. (2016). Non-prescription sale and dispensing of antibiotics in community pharmacies in Zambia. Expert Rev. Anti Infect. Ther. 14 (12), 1215–1223. doi:10.1080/14787210.2016.1227702
Kamal, R. S. (2020). Fear, hatred and stigmatization grip Bangladesh amid COVID-19 outbreak. Available at: https://tbsnews.net/thoughts/fear-hatred-and-stigmatization-grip-bangladesh-amid-covid-19-outbreak-61129.
Kamati, M., Godman, B., and Kibuule, D. (2019). Prevalence of self-medication for acute respiratory infections in young children in Namibia: findings and implications. J. Res. Pharm. Pract. 8 (4), 220–224. doi:10.4103/jrpp.JRPP_19_121
Kaonga, O., Banda, C., and Masiye, F. (2019). Hardship financing of out-of-pocket payments in the context of free healthcare in Zambia. PLoS One 14 (4), e0214750. doi:10.1371/journal.pone.0214750
Khan, B. G. B., Babar, A., Hussain, S., Mahmood, S., and Aqeel, T. (2016). Assessment of active pharmaceutical ingredients in the registration procedures in Pakistan: implications for the future. GaBI J. 5 (4), 156–163. doi:10.5639/gabij.2016.0504.041
Kluge, H. H. P., Wickramasinghe, K., Rippin, H. L., Mendes, R., Peters, D. H., Kontsevaya, A., et al. (2020). Prevention and control of non-communicable diseases in the COVID-19 response. Lancet 395 (10238), 1678–1680. doi:10.1016/S0140-6736(20)31067-9
Kretchy, I. A., Asiedu-Danso, M., and Kretchy, J. P. (2020). Medication management and adherence during the COVID-19 pandemic: perspectives and experiences from low-and middle-income countries. Res. Soc. Adm. Pharm. doi:10.1016/j.sapharm.2020.04.007
Krubiner, C., Keller, J. M., and Kaufman, J. (2020). Balancing the COVID-19 response with wider health needs: key decision-making considerations for low- and middle-income countries. Available at: https://www.cgdev.org/sites/default/files/balancing-covid-19-response-wider-health-needs-key-decision-making-considerations-low.pdf.
Lee, H.-Y., Oh, J., Hoang, V. M., Moon, J. R., and Subramanian, S. V. (2019). Use of high-level health facilities and catastrophic expenditure in Vietnam: can health insurance moderate this relationship? BMC Health Services Res. 19 (1), 318. doi:10.1186/s12913-019-4115-0
Lee, K. S., Shahidullah, A., Zaidi, S. T. R., Patel, R. P., Ming, L. C., Tariq, M. H., et al. (2017). The crux of the medicine prices’ controversy in Pakistan. Front. Pharmacol. 8, 504. doi:10.3389/fphar.2017.00504
Littlejohn, E. (2020). Hydroxychloroquine use in the COVID-19 patient. Cleve. Clin. J. Med. doi:10.3949/ccjm.87a.ccc011
Liwa, A. C., Smart, L. R., Frumkin, A., Epstein, H-A. B., Fitzgerald, D. W., and Peck, R. N. (2014). Traditional herbal medicine use among hypertensive patients in sub-Saharan Africa: a systematic review. Curr. Hypertens. Rep. 16 (6), 437. doi:10.1007/s11906-014-0437-9
Llor, C., and Bjerrum, L. (2014). Antimicrobial resistance: risk associated with antibiotic overuse and initiatives to reduce the problem. Therapeut. Adv. Drug. Saf. 5 (6), 229–241. doi:10.1177/2042098614554919
Luo, E., Zhang, D., Luo, H., Liu, B., Zhao, K., Zhao, Y., et al. (2020). Treatment efficacy analysis of traditional Chinese medicine for novel coronavirus pneumonia (COVID-19): an empirical study from Wuhan, Hubei Province, China. Chin. Med. 15, 34. doi:10.1186/s13020-020-00317-x
Luo, L., Jiang, J., Wang, C., Fitzgerald, M., Hu, W., Zhou, Y., et al. (2020). Analysis on herbal medicines utilized for treatment of COVID-19. Acta Pharm. Sin. B 10, 1192‒1204. doi:10.1016/j.apsb.2020.05.007
Markovic-Pekovic, V., Grubisa, N., Burger, J., Bojanic, L., and Godman, B. (2017). Initiatives to reduce nonprescription sales and dispensing of antibiotics: findings and implications. J. Res. Pharm. Pract. 6 (2), 120–125. doi:10.4103/jrpp.JRPP_17_12
Masango, T. A. (2020). Misuse of chloroquine, azithromycin and lopinavir-ritonavir for the prevention and/or potential treatment of COVID-19. Available at: https://www.biznews.com/briefs/2020/03/24/pharmacy-body-anti-malaria-drugs-covid-19.
McCreary, E. K., and Angus, D. C. (2020). Efficacy of remdesivir in COVID-19. JAMA 324 (11), 1041–1042. doi:10.1001/jama.2020.16337
McHenga, M., Chirwa, G. C., and Chiwaula, L. S. (2017). Impoverishing effects of catastrophic health expenditures in Malawi. Int. J. Equity Health 16 (1), 25. doi:10.1186/s12939-017-0515-0
Mehta, H. B., Ehrhardt, S., Moore, T. J., Segal, J. B., and Alexander, G. C. (2020). Characteristics of registered clinical trials assessing treatments for COVID-19: a cross-sectional analysis. BMJ Open 10 (6), e039978. doi:10.1136/bmjopen-2020-039978
Miljković, N., Godman, B., Kovačević, M., Polidori, P., Tzimis, L., Hoppe-Tichy, T., et al. (2020a). Prospective risk assessment of medicine shortages in europe and Israel: findings and implications. Front. Pharmacol. 11, 357. doi:10.3389/fphar.2020.00357
Miljković, N., Godman, B., van Overbeeke, E., Kovačević, M., Tsiakitzis, K., Apatsidou, A., et al. (2020b). Risks in antibiotic substitution following medicine shortage: a health-care failure mode and effect analysis of six European hospitals. Front. Med. 7, 157. doi:10.3389/fmed.2020.00157
Modisakeng, C., Matlala, M., Godman, B., and Meyer, J. C. (2020). Medicine shortages and challenges with the procurement process among public sector hospitals in South Africa; findings and implications. BMC Health Services Res. 20 (1), 234. doi:10.1186/s12913-020-05080-1
Moorkens, E., Vulto, A. G., Huys, I., Dylst, P., Godman, B., Keuerleber, S., et al. (2017). Policies for biosimilar uptake in Europe: an overview. PLoS One 12 (12), e0190147. doi:10.1371/journal.pone.0190147
Mukokinya, M., Opanga, S., Oluka, M., and Godman, B. (2018). Dispensing of antimicrobials in Kenya: a cross-sectional pilot study and its implications. J. Res. Pharm. Pract. 7 (2), 77–82. doi:10.4103/jrpp.JRPP_17_88
N Gage Consuting (2017). Egypt’s pharmaceutical sector following bold economic reforms: challenges and opportunities. Available at: https://www.ngage-consulting.com/downloads/Pharmaceutical_PDF_Final_Version_K_and_A.pdf.
Nashilongo, M. M., Singu, B., Kalemeera, F., Mubita, M., Naikaku, E., Baker, A., et al. (2017). Assessing adherence to antihypertensive therapy in primary health care in Namibia: findings and implications. Cardiovasc. Drugs Ther. 31 (5‒6), 565–578. doi:10.1007/s10557-017-6756-8
Nga, L., Phuong, L., and Anh, P. (2020). Hanoi man OD’s on rumored malaria drug cure for COVID-19. Available at: https://e.vnexpress.net/news/news/hanoi-man-od-s-on-rumored-malaria-drug-cure-for-covid-19-4073488.html.
Niaz, Q., Godman, B., Campbell, S., and Kibuule, D. (2020). Compliance to prescribing guidelines among public health care facilities in Namibia; findings and implications. Int. J. Clin. Pharm. 42, 1227–1236. doi:10.1007/s11096-020-01056-7
Niaz, Q., Godman, B., Massele, A., Campbell, S., Kurdi, A., Kagoya, H. R., et al. (2019). Validity of World Health Organisation prescribing indicators in Namibia’s primary healthcare: findings and implications. Int. J. Qual. Health Care 31 (5), 338–345. doi:10.1093/intqhc/mzy172
NIH (2020). NIH halts clinical trial of hydroxychloroquine. Available at: https://www.nhlbi.nih.gov/news/2020/nih-halts-clinical-trial-hydroxychloroquine.
Nkeck, J. R., Tsafack, E. E., Ndoadoumgue, A. L., and Endomba, F. T. (2020). An alert on the incautious use of herbal medicines by sub-Saharan African populations to fight against the COVID-19. PAMJ 35 (2), 26. doi:10.11604/pamj.supp.2020.35.2.23161
Nordling, N. (2020). Unproven herbal remedy against COVID-19 could fuel drug-resistant malaria, scientists warn. Available at: https://www.sciencemag.org/news/2020/05/unproven-herbal-remedy-against-covid-19-could-fuel-drug-resistant-malaria-scientists.
O’Neill, L. A. J., and Netea, M. G. (2020). BCG-induced trained immunity: can it offer protection against COVID-19? Nat. Rev. Immunol. 20 (6), 335–337. doi:10.1038/s41577-020-0337-y
Ogunleye, O. O., Basu, D., Mueller, D., Sneddon, J., Seaton, R. A., Yinka-Ogunleye, A. F., et al. (2020). Response to the novel corona virus (COVID-19) pandemic across Africa: successes, challenges, and implications for the future. Front. Pharmacol. 11, 1205. doi:10.3389/fphar.2020.01205
Ongole, J. J., Rossouw, T. M., Fourie, P. B., Stoltz, A. C., Hugo, J., and Marcus, T. S. (2020). Sustaining essential healthcare in Africa during the COVID19 pandemic. Available at: https://www.theunion.org/news-centre/news/body/IJTLD-June-0214_Ongole.pdf.
Pakistan Today (2020). Pakistan’s healthcare system. Available at: https://www.pakistantoday.com.pk/2020/01/08/pakistans-healthcare-system/.
Pekerti, A., Vuong, Q-H., Ho, T. M., and Vuong, T-T. (2017). Health care payments in Vietnam: patients’ quagmire of caring for health versus economic destitution. Int. J. Environ. Res. Publ. Health 14 (10), 1118. doi:10.3390/ijerph14101118
Pham, Q. T., Rabaa, M. A., Duong, H. L., Dang, Q. T., Tran, D. Q., Quach, H. L., et al. (2020). The first 100 days of SARS-CoV-2 control in Vietnam. Clin. Infect. Dis. ciaa1130. doi:10.1093/cid/ciaa1130
Politi, D. (2020). Nigeria reports chloroquine poisonings as trump keeps pushing drug against coronavirus. Available at: https://slate.com/news-and-politics/2020/03/nigeria-chloroquine-poisonings-trump-pushing-drug-coronavirus.html.
RECOVERY Collaborative Group (2020). Lopinavir-ritonavir in patients admitted to hospital with COVID-19 (RECOVERY): a randomised, controlled, open-label, platform trial. Lancet 396 (10259), 1345–1352. doi:10.1016/S0140-6736(20)32013-4
Rempenault, C., Combe, B., Barnetche, T., Gaujoux-Viala, C., Lukas, C., Morel, J., et al. (2020). Clinical and structural efficacy of hydroxychloroquine in rheumatoid arthritis: a systematic review. Arthr. Care Res. 72 (1), 36–40. doi:10.1002/acr.23826
Rios-González, C. M. (2020) Knowledge, attitudes and practices towards COVID-19 in Paraguayans during outbreaks: a quick online survey. Available at: https://preprints.scielo.org/index.php/scielo/preprint/download/149/179/164.
Saaliq, S. (2020). Limited access to clean water among India’s poor spawns coronavirus concerns. Available at: https://news.yahoo.com/limited-access-clean-water-among-130525398.html.
SAHPRA (2020). SAHPRA cautions against medicine stockpiling including Chloroquine containing products. Available at: http://www.sahpra.org.za/wp-content/uploads/2020/03/SAHPRA-communique_Chloroquine-Stockpiling_23032020.pdf.
Salari, P., Di Giorgio, L., Ilinca, S., and Chuma, J. (2019). The catastrophic and impoverishing effects of out-of-pocket healthcare payments in Kenya, 2018. BMJ Global Health 4 (6), e001809. doi:10.1136/bmjgh-2019-001809
Saleem, Z., Hassali, M. A., Godman, B., Fatima, M., Ahmad, Z., Sajid, A., et al. (2020). Sale of WHO AWaRe groups antibiotics without a prescription in Pakistan: a simulated client study. J. Pharm. Policy Pract. 13 (1), 26.
Saleem, Z., Hassali, M. A., Hashmi, F. K., Godman, B., and Saleem, F. (2019). Antimicrobial dispensing practices and determinants of antimicrobial resistance: a qualitative study among community pharmacists in Pakistan. Family Med. Commu. Health 7 (3), e000138.
Sambala, E. Z., Mdolo, A., Banda, R., Phiri, A., Wiyeh, A. B., and Wiysonge, C. S. (2018). Burden of seasonal influenza in sub-Saharan Africa: a systematic review protocol. BMJ Open 8 (10), e022949.
Schaaf, H. S., du Preez, K., Kruger, M., Solomons, R., Taljaard, J. J., Rabie, H., et al. (2020). Bacille Calmette-Guérin (BCG) vaccine and the COVID-19 pandemic: responsible stewardship is needed. Available at: https://www.theunion.org/news-centre/news/body/IJTLD-0267_Schaaf.pdf.
Singh, D. R., Sunuwar, D. R., Karki, K., Ghimire, S., and Shrestha, N. (2020). Knowledge and perception towards universal safety precautions during early phase of the COVID-19 outbreak in Nepal. J. Community Health 45 (6), 1116–1122. doi:10.1007/s10900-020-00839-3
South African Government (2020). President Ramaphosa launches the Africa medical supplies platform to help fight COVID-19 coronavirus pandemic. Available at: https://www.gov.za/speeches/president-ramaphosa-launches-africa-medical-supplies-platform-help-fight-covid-19.
The Lancet Editors (2020). Expression of concern: hydroxychloroquine or chloroquine with or without a macrolide for treatment of COVID-19: a multinational registry analysis. Lancet 395 (10240), e102. doi:10.1016/S0140-6736(20)31290-3
Thornton, J. (2020). COVID-19: keep essential malaria services going during pandemic, urges WHO. BMJ 369, m1637. doi:10.1136/bmj.m1637
Trading Economics (2020a). Namibia inflation rate. Available at: https://tradingeconomics.com/namibia/inflation-cpi.
Trading Economics (2020b). Ghana inflation rate. Available at: https://tradingeconomics.com/ghana/inflation-cpi.
Trading Economics (2020c). Malawi inflation rate. Available at: https://tradingeconomics.com/malawi/inflation-cpi.
Trading Economics (2020d). Nigeria inflation rate. Available at: https://tradingeconomics.com/nigeria/inflation-cpi.
Trading Economics (2020e). Zambia inflation rate. Available at: https://tradingeconomics.com/zambia/inflation-cpi.
UNICEF South Africa (2020). Immunization against vaccine-preventable diseases is essential to protect children African vaccination week 2020 focuses on the importance of immunization in a time of COVID-19. Available at: https://www.unicef.org/southafrica/stories/immunization-against-vaccine-preventable-diseases-essential-protect-children.
Vellingiri, B., Jayaramayya, K., Iyer, M., Narayanasamy, A., Govindasamy, V., Giridharan, B., et al. (2020). COVID-19: a promising cure for the global panic. Sci. Total Environ. 725, 138277. doi:10.1016/j.scitotenv.2020.138277
Vietnam Insider (2020). Hanoi asks pharmacies to report people buying medicines for COVID-19-like symptoms. Available at: https://vietnaminsider.vn/hanoi-asks-pharmacies-to-report-people-buying-medicines-for-covid-19-like-symptoms/.
Wang, Y., Zhang, D., Du, G., Du, R., Zhao, J., Jin, Y., et al. (2020). Remdesivir in adults with severe COVID-19: a randomised, double-blind, placebo-controlled, multicentre trial. Lancet 395 (10236), 1569–1578. doi:10.1016/S0140-6736(20)31022-9
Weston, M. (2020). Coronavirus reaches Sudan, one of the countries least equipped to cope with it. Available at: https://mg.co.za/africa/2020-03-24-coronavirus-reaches-sudan-one-of-the-countries-least-equipped-to-cope-with-it/.
WHO (2018). World malaria report 2018. Available at: https://www.who.int/malaria/publications/world-malaria-report-2018/en/.
WHO (2020a). Coronavirus disease (COVID-19) situation report – 182. Available at: https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200720-covid-19-sitrep-182.pdf?sfvrsn=60aabc5c_2.
WHO (2020b). Coronavirus disease (COVID-19) situation report - 27 September 2020. Available at: https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200928-weekly-epi-update.pdf?sfvrsn=9e354665_4.
WHO (2020c). WHO discontinues hydroxychloroquine and lopinavir/ritonavir treatment arms for COVID-19. Available at: https://www.who.int/news-room/detail/04-07-2020-who-discontinues-hydroxychloroquine-and-lopinavir-ritonavir-treatment-arms-for-covid-19.
WHO. (2020d). WHO and UNICEF warn of a decline in vaccinations during COVID-19. Available at: https://www.who.int/news-room/detail/15-07-2020-who-and-unicef-warn-of-a-decline-in-vaccinations-during-covid-19.
WHO (2020e). The potential impact of health service disruptions on the burden of malaria: a modelling analysis for countries in sub-Saharan Africa. Available at: https://apps.who.int/iris/bitstream/handle/10665/331845/9789240004641-eng.pdf?sequence=1&isAllowedy.
WHO Regional Office for Africa Influenza virological surveillance in the WHO african region - epidemiological week 42, October 16‒22. 2017. Available at: https://apps.who.int/iris/bitstream/handle/10665/259530/IB3-42.pdf;jsessionid=8CB844AA273CB1AAB5BA3AFC13F8486B?sequence=1.
WHO Solidarity Trial Consortium (2020). Repurposed antiviral drugs for COVID-19 –interim WHO SOLIDARITY trial results. Available at: https://doi.org/10.1101/2020.10.15.20209817. MedRxiv (October 15) version.
Wojkowska-Mach, J., Godman, B., Glassman, A., Kurdi, A., Pilc, A., Rozanska, A., et al. (2018). Antibiotic consumption and antimicrobial resistance in Poland; findings and implications. Antimicrob. Resist. Infect. Contr. 7 (1), 136. doi:10.1186/s13756-018-0428-8
Worldometer (2020a). African countries by population. Available at: https://www.worldometers.info/population/countries-in-africa-by-population/.
Worldometer (2020b). Eastern Asia by population. Available at: https://www.worldometers.info/world-population/eastern-asia-population/.
Worldometer (2020c). South-Eastern Asia by population. Available at: https://www.worldometers.info/world-population/south-eastern-asia-population/.
Worldometer (202d). Southern Asia by population Available at: https://www.worldometers.info/world-population/southern-asia-population/.
Wu, J., Taylor, D., Ovchinikova, L., Heaney, A., Morgan, T., Dartnell, J., et al. (2018). Relationship between antimicrobial-resistance programs and antibiotic dispensing for upper respiratory tract infection: an analysis of Australian data between 2004 and 2015. J. Int. Med. Res. 46 (4), 1326–1338. doi:10.1177/0300060517740813
Yang, Y. (2020). Use of herbal drugs to treat COVID-19 should be with caution. Lancet (London, England) 395 (10238), 1689–1690. doi:10.1142/S0192415X2050038X
Keywords: Africa, Asia, community pharmacists, COVID-19, medicines, protective equipment, price rises, shortages
Citation: Sefah IA, Ogunleye OO, Essah DO, Opanga SA, Butt N, Wamaitha A, Guantai AN, Chikowe I, Khuluza F, Kibuule D, Nambahu L, Abubakar AR, Sani IH, Saleem Z, Kalungia AC, Thi Phuong TN, Haque M, Islam S, Kumar S, Sneddon J, Wamboga J, Wale J, Miljković N, Kurdi A, Martin AP and Godman B (2021) Rapid Assessment of the Potential Paucity and Price Increases for Suggested Medicines and Protection Equipment for COVID-19 Across Developing Countries With a Particular Focus on Africa and the Implications. Front. Pharmacol. 11:588106. doi: 10.3389/fphar.2020.588106
Received: 28 July 2020; Accepted: 11 November 2020;
Published: 14 January 2021.
Edited by:
Sam Salek, University of Hertfordshire, United KingdomReviewed by:
Robert Sewell, Cardiff University, United KingdomCopyright © 2021 Sefah, Ogunleye, Essah, Opanga, Butt, Wamaitha, Guantai, Chikowe, Khuluza, Kibuule, Nambahu, Abubakar, Sani, Saleem, Kalungia, Thi Phuong, Haque, Islam, Kumar, Sneddon, Wamboga, Wale, Miljković, Kurdi, Martin and Godman. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Brian Godman, QnJpYW4uZ29kbWFuQHN0cmF0aC5hYy51aw==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.