
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Pharmacol. , 30 November 2020
Sec. Cardiovascular and Smooth Muscle Pharmacology
Volume 11 - 2020 | https://doi.org/10.3389/fphar.2020.566956
This article is part of the Research Topic New Trends and Approaches in Perioperative Pharmacotherapy: an Update View all 12 articles
 Alexandre B. Todeschini1
Alexandre B. Todeschini1 Alberto A. Uribe1*
Alberto A. Uribe1* Marco Echeverria-Villalobos1
Marco Echeverria-Villalobos1 Juan Fiorda-Diaz1
Juan Fiorda-Diaz1 Mahmoud Abdel-Rasoul2
Mahmoud Abdel-Rasoul2 Benjamin G. McGahan3
Benjamin G. McGahan3 Andrew J. Grossbach3
Andrew J. Grossbach3 Stephanus Viljoen3
Stephanus Viljoen3 Sergio D. Bergese1,3,4
Sergio D. Bergese1,3,4Introduction: Acute perioperative blood loss is a common and potentially major complication of multilevel spinal surgery, usually worsened by the number of levels fused and of osteotomies performed. Pharmacological approaches to blood conservation during spinal surgery include the use of intravenous tranexamic acid (TXA), an anti-fibrinolytic that has been widely used to reduce blood loss in cardiac and orthopedic surgery. The primary objective of this study was to assess the efficacy of intraoperative TXA in reducing estimated blood loss (EBL) and red blood cell (RBC) transfusion requirements in patients undergoing multilevel spinal fusion.
Materials and Methods: This a single-center, retrospective study of subjects who underwent multilevel (≥7) spinal fusion surgery who received (TXA group) or did not receive (control group) IV TXA at The Ohio State University Wexner Medical Center between January 1st, 2016 and November 30th, 2018. Patient demographics, EBL, TXA doses, blood product requirements and postoperative complications were recorded.
Results: A total of 76 adult subjects were included, of whom 34 received TXA during surgery (TXA group). The mean fusion length was 12 levels. The mean total loading, maintenance surgery and total dose of IV TXA was 1.5, 2.1 mg per kilo (mg/kg) per hour and 33.8 mg/kg, respectively. The mean EBL in the control was higher than the TXA group, 3,594.1 [2,689.7, 4,298.5] vs. 2,184.2 [1,290.2, 3,078.3] ml. Among all subjects, the mean number of intraoperative RBC and FFP units transfused was significantly higher in the control than in the TXA group. The total mean number of RBC and FFP units transfused in the control group was 8.1 [6.6, 9.7] and 7.7 [6.1, 9.4] compared with 5.1 [3.4, 6.8] and 4.6 [2.8, 6.4], respectively. There were no statistically significant differences in postoperative blood product transfusion rates between both groups. Additionally, there were no significant differences in the incidence of 30-days postoperative complications between both groups.
Conclusion: Our results suggest that the prophylactic use of TXA may reduce intraoperative EBL and RBC unit transfusion requirements in patients undergoing multilevel spinal fusion procedures ≥7 levels.
Multilevel spinal fusion surgery is among the most common procedures (ranked fifth in 2017) performed on inpatients in the United States (Healthcare Cost and Utilization Project (HCUP), 2017; Goobie et al., 2018; Verma et al., 2010). Acute perioperative blood loss is a common and potentially major complication of multilevel spinal surgery, usually worsened by the number of levels fused and of osteotomies performed (Lin et al., 2018; Lu et al., 2018; Shakeri et al., 2018). For cases involving more levels, the larger operative wound and area of bleeding surfaces exposed have been associated with increased blood loss (Nagabhushan et al., 2018).
There are several patient factors that contribute to the significant intraoperative blood loss in spinal fusion surgery including, but not limited to: height of the patient, length of surgical field exposure and severity or type of spine deformity (Verma et al., 2010). Additionally, there are surgical factors that include: length of surgery, type of procedure, combined approaches (anterior and posterior), number of levels fused, number of anchors placed, intraoperative maintenance of the mean arterial pressure, utilization of blood salvage techniques, history of coagulopathy and the use of anti-fibrinolytic drugs (Verma et al., 2010). Also, the prone position might lead to hemodynamic challenges during surgery by restricting the blood flow of the inferior vena cava and consequently distending the paravertebral and epidural veins, which contributes to increased bleeding (DePasse et al., 2015). In order to minimize this, the use of the Jackson table has been recommended due to its capacity to reduce intra-abdominal pressure (Jackson, 1992; Mathai et al., 2012).
The prevention of blood loss is crucial to spinal surgery since massive blood loss can contribute to coagulopathy and disseminated intravascular coagulation, increasing the risk of postoperative hematoma and neurological deficits (Hu, 2004; Elgafy et al., 2010).
Traumatic hemorrhage, as well as profuse intraoperative bleeding, promotes massive release of tissue plasminogen activator (tPA) inducing hyperfibrinolysis (Kashuk et al., 2010; Chapman et al., 2016). Plasminogen, produced by the liver, and tPA bind to C-terminal lysine residues on fibrin leading to localized plasmin formation and fibrin cleavage (Chapman et al., 2016). Tranexamic Acid (TXA) is an anti-fibrinolytic that has been widely used to prevent massive blood loss in cardiac and orthopedic surgery, with an increased use in spinal surgeries. (Verma et al., 2010; Hunt, 2015; Yoo et al., 2019). TXA inhibits the capacity of plasminogen and plasmin to bind to fibrin, hence preserving blood clots from plasmin-mediated lysis (Verma et al., 2010; Hunt, 2015). TXA, a synthetic derivative of lysine, exerts its antifibrinolytic activity by reversibly and competitively binding to lysine-binding sites on the structural proteins of plasmin, plasminogen, and as well as tPA, this consequently inhibits the degradation of fibrin molecules (McCormack, 2012). Each plasminogen molecule has up to five binding sites for TXA, with one site of high affinity (McCormack, 2012). Data from animal models of traumatic injuries also suggests a delayed release of urokinase plasminogen activator (uPA) (Hijazi et al., 2015). Physiologically, TXA catalyzes the conversion of plasminogen to active plasmin, which induces controlled anticoagulation and clot breakdown (Hijazi et al., 2015). There is evidence showing that TXA has pharmacological actions other than inhibition of fibrinolysis (Couturier and Grassin-Delyle, 2014), such as clot stabilization (Dai et al., 2011), improvement of platelet function (Blake et al., 2006), inhibition of apoptosis (Hsia et al., 2010), and prevention of pro-inflammatory cytokine production (Jimenez et al., 2007). However, its safety and efficacy profiles are not well known in spinal surgery (Lin et al., 2018; Lu et al., 2018; Luo et al., 2018; Nagabhushan et al., 2018; Shakeri et al., 2018; Xue et al., 2018; Karimi et al., 2019).
The literature describes different volume, timing and route of TXA administration for spinal procedures. Intravenous administration is the most Common, ranging from 10–20 mg per kilogram (mg/kg) as a loading dose and 1–10 mg per kilogram per hour (mg/kg/h) as a maintenance dose (Walterscheid et al., 2017). Similar to its use in other surgical procedures, the most common side effects related to TXA are seizures, acute kidney injury, liver injury, and mainly thromboembolic events (myocardial infarction, stroke, deep vein thrombosis and pulmonary embolism), particularly in elderly patients (Neilipovitz et al., 2001; Verma et al., 2010; Colomina et al., 2017; Grassin-Delyle et al., 2018; Nagabhushan et al., 2018). The efficacy of its use has been assessed in spinal surgery and the results are inconclusive due to the complexity and diversity of the dosing regimen (Neilipovitz et al., 2001; Wong et al., 2008; Verma et al., 2010; Farrokhi et al., 2011; Colomina et al., 2017; Johnson et al., 2017; Carabini et al., 2018; Grassin-Delyle et al., 2018; Lin et al., 2018; Lu et al., 2018; Nagabhushan et al., 2018; Karimi et al., 2019). After the consideration of intraoperative blood loss and the incidence of autologous transfusion, the benefit of using TXA might outweigh the undesirable side effects. However, although it is widely used, it is not currently considered part of standard of care in spinal surgeries (Verma et al., 2010; Walterscheid et al., 2017).
The efficacy profile of TXA in spinal procedures remains unclear and should be investigated. Therefore, we designed a retrospective study with the hypothesis that patients undergoing primary or revision spinal fusion surgery (≥7 levels) who received intravenous (IV) TXA would have a significant reduction in intraoperative estimated blood loss (EBL) and red blood cell (RBC) transfusions compared with patients who did not receive IV TXA. The primary objective of the study was to assess the efficacy of intraoperative TXA in reducing EBL and RBC transfusions in patients undergoing multilevel spinal fusion.
We conducted a single-center, retrospective study that reviewed electronic medical records from subjects who underwent multilevel (≥7) spinal fusion surgery and received (TXA group) or did not receive (control group) IV TXA at The Ohio State University Wexner Medical Center between January 1st, 2016 and November 30th, 2018. The decision of dosing TXA during surgery was at the surgeon’s discretion. After obtaining the approval of our Institutional Review Board (Office of Responsible Research Practices, The Ohio State University), we accessed electronic medical records in order to assess eligibility and collect perioperative information from 404 subjects.
Subjects 18 years and older that underwent ≥7 levels spinal fusion surgery (primary or revision) using a posterior midline approach and received loading and maintenance dose TXA between January 1st, 2016 and November 30th, 2018 at The Ohio State University Wexner Medical Center, Department of Neurosurgery, were included in the study. Prisoners, pregnant women, history of congenital coagulation disorders, chronic kidney disease (baseline serum creatinine >1.36 mg per deciliter [mg/dl]), chronic liver disease, concomitant use of coagulation-altering medications, or undergoing active treatment for malignancies were excluded from the study.
The following information was collected for analysis purposes: demographics (age, gender, race, height, weight, BMI), the American Society of Anesthesiology (ASA) physical status, perioperative coagulation and hematologic parameters, surgical variables (number of levels fused, length of surgery and of anesthesia, previous spinal surgery, spinal surgeon, type of spinal pathology, type of surgical technique, EBL, units, volume and type of blood transfusions administered (considering that the threshold for blood products transfusion was hemoglobin ≤7 mg/dl), total dose of IV TXA administration, length of post-anesthesia care unit (PACU) and hospital stay. In addition, type and units of blood product transfusions administered during the first 24 h after the end of surgery and any complications diagnosed in a 30-days period after surgery were also collected. Intraoperative transfusions were performed in accordance with our institutional transfusion protocol (“Transfusion Therapy: Indications for Ordering”). If the patient was hemodynamically stable, intraoperative blood transfusion was considered at a hemoglobin threshold of <8 gm/dl, if intraoperative bleeding is not expected to be life-threaten. In addition, the decision to transfuse blood products during surgery was made by the anesthesiology care provider following our institutional transfusion protocol. Consequently, as part of our institutional transfusion protocol, platelets can be ordered for pooled (4 or 6 units) prior to surgery and if more units are required, single units are dispensed and all blood products used at our institution are leukoreduced. In addition, the intraoperative estimation of EBL was made according to the standard procedure as the difference between the total surgical suctioned volume and the total amount of irrigation used during the case. The hemoglobin concentration was measured in all patients preoperatively. All gauzes and lap sponges were wringed into the field, circulated through the suction device, and accounted for by EBL. Postoperative EBL was estimated by postoperative drain output.
The primary outcomes were incidence and quantity of intraoperative EBL and RBC transfusions. Our secondary outcomes were the incidence and quantity of other perioperative blood product transfusion requirements, surgical variables (length of surgery, anesthesia, PACU, intensive care unit (ICU) and hospitalization stay) the incidence of 30-days postoperative complications in both groups.
Continuous patient demographic and clinical/surgical variables were summarized as means (±standard deviations) and categorical variables were summarized as frequencies (percentages). Student’s t-tests or Mann-Whitney U tests were used to test demographic differences between study groups for continuous variables where appropriate. Chi-square or Fisher’s exact tests were used to test for differences in categorical variables between study groups where appropriate. Linear regression models were fit for each of the outcomes in the primary aim adjusting for potential confounders and effect modifiers, including number of spinal levels, cell saver use and number of surgeons variable. The final models for RBC and FFP included main effects for study group and number of spine levels. The final model for EBL also included an interaction term between study group and number of spine levels. All models were checked to verify that statistical assumptions of normality of residuals and equal variance were not violated. Hypothesis testing comparing outcomes between study groups was administered based on the final model estimates for each outcome and conducted at a two-sided alpha of 0.05. All statistical analyses were performed using SAS/STAT software version 9.4 (SAS Institute Inc., Cary, NC).
A total of 404 charts were initially reviewed. Data from 328 subjects were not eligible based on inclusion and exclusion criteria; the main reasons for exclusion were cervical spinal surgeries, fewer than seven levels fused and minimally invasive procedures. Therefore, this study included 76 subjects for data analysis, of whom 42 (55.3%) did not receive IV TXA (control group) and 34 (44.7%) received IV TXA (TXA group) during surgery. The flow-diagram of this retrospective observational trial according to the Consolidated Standards of Reporting Trials (CONSORT) is shown in Figure 1 (Begg et al., 1996).
A summary of demographic and perioperative variables is listed in Table 1. The mean age was 59.3 (±12.0) years in the control group and 58 (±12.0) years in the TXA group. The mean total loading dose, dose rate for maintenance and total dose administered during maintenance of IV TXA administration was 1.5 (±0.9) mg, 2.1 (±1.3) mg/kg/h and 33.8 (±20.3) mg/kg, respectively. There was not a statistically significant difference in demographic and clinical characteristics except for length of anesthesia and surgery. Subjects in the TXA group had a significantly shorter mean length of anesthesia (9.8 ± 1.8 vs. 10.9 ± 2.3 h; p-value = 0.0296) and surgery (7.2 ± 1.6 vs. 8.3 ± 2.3 h; p-value = 0.0227).
The mean EBL in the control was higher than the TXA group, 3,494.1 [2,689.7, 4,298.5] vs. 2,184.2 [1,290.2, 3,078.3] ml (95% confidence interval [CI]; p-value = 0.0332) (Table 2). Among all subjects, the mean number of intraoperative RBC and FFP units transfused was significantly higher (95% CI; p-value < 0.05) in the control group than in the TXA group. The total mean number of RBC and FFP units given to subjects in the control group was 8.1 [6.6, 9.7] and 7.7 [6.1, 9.4] compared with 5.1 [3.4, 6.8] and 4.6 [2.8, 6.4], respectively (Table 2).
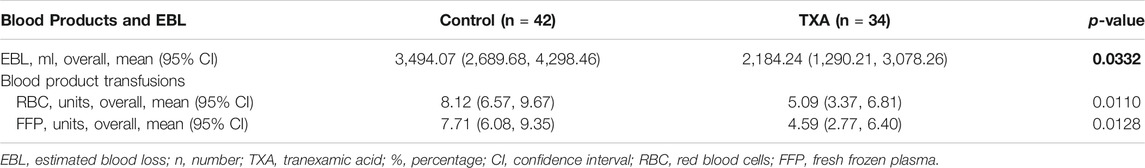
TABLE 2. Estimated blood loss and amount of intraoperative blood transfusion from univariate models.
A multivariate model predicting EBL was fit including main effects for study group, number of spine levels and the interaction between the two variables. EBL increased at a greater rate for the control group compared to the TXA group as number of spine levels increased (interaction term p-value = 0.0386) (Table 3; Figure 2). Additionally, a multivariate model predicting RBC transfusion was fit including main effects for study group and number of spine levels. RBC transfusion was significantly higher on average for the control group compared to the TXA group (p-value = 0.0123). There was also a significant increase in blood loss as number of spine levels increased (p-value = 0.0001). An interaction term between study group and the number of spine levels was not included in the final multivariable RBC model as it was not statistically significant (p-value = 0.1708) (Table 3; Figure 3). Ultimately, a multivariate model predicting FFP transfusion was fit including main effects for study group and number of spine levels. FFP was significantly higher for the control group compared to the TXA group (p-value = 0.0143) after adjusting for number of spine levels. An interaction term between study group and number of spine levels was not included in the final multivariable FFP administration model as it was not statistically significant (p-value = 0.1697) (Table 3; Figure 4).
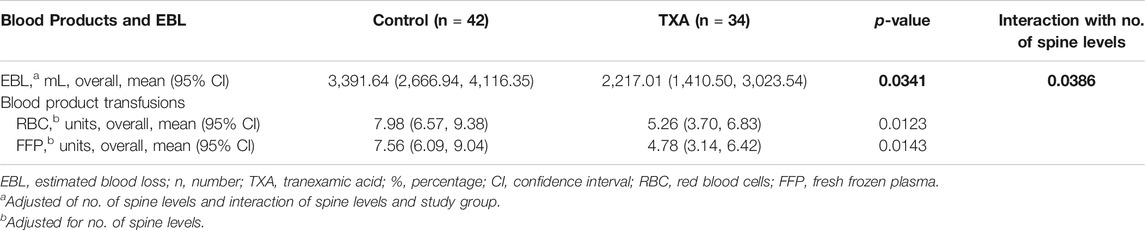
TABLE 3. Estimated blood loss and amount of intraoperative blood transfusion from multivariate models.
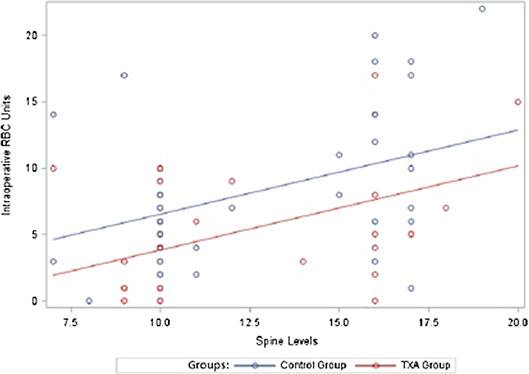
FIGURE 3. Intraoperative transfused red blood cell units. RBC, red blood cells; TXA, tranexamic acid.
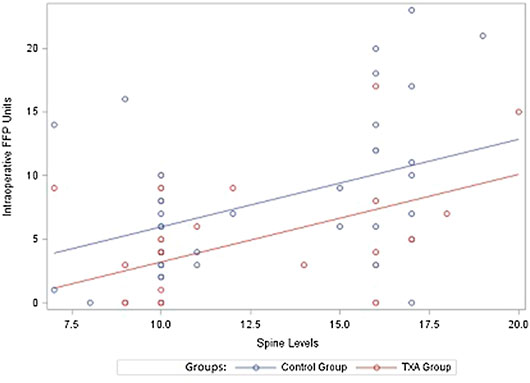
FIGURE 4. Intraoperative transfused frozen fresh plasma units. FFP, fresh frozen plasma; TXA, tranexamic acid.
Subsequently, there was no statistical difference in postoperative blood product transfusion rates between both groups. As a final point, there was no significant difference in the incidence of 30-days postoperative complications between both groups (Table 4).
In the present retrospective study, 76 subjects underwent multilevel (≥7 levels) spinal fusion and 34 of them received intraoperative loading and maintenance doses of TXA. Both groups were similar in the demographics and surgical procedure. The primary objective of the study was to assess the efficacy of intraoperative TXA in reducing EBL and RBC transfusions in patients undergoing multilevel (≥7 levels) spinal fusion. The results have shown significant difference in both groups; EBL during surgery and the number of intraoperative RBC transfused was reduced by 37% with the use of IV TXA. There was also a significant difference in the number of intraoperative RBC and FFP units transfused with the need of intraoperative transfusion being reduced by 37% and 40% in the TXA group compared to the control group (p-value = 0.0123 and 0.0143). A mean IV TXA loading and maintenance dose of 1.5 g and 2.1 mg/kg/h was well tolerated by subjects in the TXA group and there were no significant differences in the postoperative complications associated with its use. The results from this study will serve to direct the design and power analysis of a prospective double-blind randomized clinical trial assessing efficacy of using TXA administration in patients undergoing multilevel spinal fusion.
Complex multilevel spinal decompression, fusion and osteotomies have been associated with profuse perioperative blood loss and greater use of blood transfusions with subsequent increased risk of coagulation impairment, blood-borne infectious disease transmission, postoperative hematoma formation, shock and pulmonary edema (Johnson et al., 1989; Mirza et al., 2008; Naik et al., 2017). Studies describing the impact of perioperative TXA administration on blood loss and blood transfusion may vary among institutions. Choi et al. reviewed 132 consecutive patients (adults and children) undergoing multilevel (≥5 levels) posterior spinal instrumented fusion (Choi et al., 2017). TXA was administered in 67% of the patients (n = 89). For adult patients, an IV TXA loading dose of 10 mg/kg was used, followed by a continuous maintenance infusion dose of 1 mg/kg/h (Choi et al., 2017). In pediatrics (<18 years old), IV TXA 5 mg/kg/h. was used for maintenance following a 50 mg/kg loading dose (Choi et al., 2017). A significant reduction in EBL (841 vs. 1,396 ml; p = 0.002), intra- and postoperative transfusion volume (544 vs. 812 ml; p = 0.012 and 193 vs. 359 ml; p = 0.034, respectively) was reported in patients who received TXA when compared to patients in which TXA was not used (Choi et al., 2017). A multiple regression analysis demonstrated an association between TXA administration and decreased surgical bleeding (Choi et al., 2017).
Loading TXA doses are highly variable among published randomized clinical trials (RCTs) conducted in patients undergoing spinal surgeries, whereas infusion or maintenance doses seem to be more consistent. Moreover, reported intra- and postoperative outcomes may also vary. Shakeri et al. studied the efficacy of a single TXA dose of 15 mg/kg compared to placebo in 50 patients undergoing laminectomy (≥2 levels) with postero-lateral fusion. A significant reduction in mean total amount of bleeding (632.2 vs. 1,037 ml; p = 0.0001), RBC transfusion required (440 vs. 1,320 ml; p = 0.0001) and length of hospital stay (2.28 vs. 3.36 days, p = 0.001) was reported in patients who received TXA (Shakeri et al., 2018).
In a multicenter study, Colomina et al. randomized 95 patients undergoing posterior spinal surgery to receive either IV TXA (10 mg/kg infusion in 20 min before surgical incision followed by a 2 mg/kg/h until closure) or matched saline solution (Colomina et al., 2017). Patients undergoing thoracic or lumbar spinal fusions (>3 levels) were included in this study. Posterior and posterolateral techniques, spinal osteotomies, posterior lumbar interbody fusion (PLIF), transforaminal lumbar interbody fusion (TLIF) and instrumented procedures of at least four vertebrae (i.e. wires, pedicle screws) were some of the types of surgeries included (Colomina et al., 2017). The mean intraoperative and total blood loss was significantly reduced in patients receiving TXA when compared to placebo (p = 0.01) (Colomina et al., 2017). However, total number of RBC transfused was similar between groups (0.85 vs. 1.42 respectively, p = 0.06) (Colomina et al., 2017). Conversely, Carabini et al. reported a significant reduction in RBC transfused in patients receiving TXA (loading dose 10 mg/kg followed by 1 mg/kg/h maintenance infusion) for complex spinal fusions when compared to matched placebo (1,140 ml vs. 1,460 respectively, p = 0.034). Moreover, TXA use was also associated with significant decreased cell saver transfusion (256 vs. 490 ml respectively, p = 0.042) (Carabini et al., 2018).
A meta-analysis of 11 RCTs published in 2015 by Cheriyan et al. reported variability on TXA doses from 1 to 15 mg/kg among 644 patients undergoing spinal surgeries (Cheriyan et al., 2015). A significant reduction in intra- and postoperative blood loss was associated with TXA administration (Cheriyan et al., 2015). Moreover, total perioperative blood loss was significantly lowered in patients receiving TXA when compared to placebo (p-value <0.0001) with no increase in the incidence of thromboembolic events among trials (Cheriyan et al., 2015).
Another systematic review and meta-analysis recently published in 2019 by Zhang et al. assessed the influence of TXA on blood loss and blood transfusion in multiple-level spine surgery from six RCT studies and five retrospective studies (Zhang et al., 2019). This study demonstrated that the administration of TXA can effectively decrease intraoperative blood loss and blood loss in spinal surgeries in contrast to the control group (p-value = 0.004) (Zhang et al., 2019). In addition, this study showed that the TXA group could maintain higher levels of postoperative hemoglobin when compared to the control group (p-value 0.009) (Zhang et al., 2019).
Goobie et al. studied the effect of higher TXA doses in 111 adolescent patients undergoing spinal surgery due to idiopathic scoliosis (Goobie et al., 2018). Patients were randomized into two groups: TXA (loading dose of 50 mg/kg after anesthesia induction followed by a maintenance dose of 10 mg/kg/h) or placebo (Goobie et al., 2018). The TXA group experienced a significantly lower amount of intraoperative bleeding (per spine level, rate per hour and total) when compared to placebo (p = 0.01, p < 0.001, and p = 0.02 respectively) (Goobie et al., 2018). Moreover, placebo was associated with a significant increase in postoperative bleeding when compared to the TXA group (645 ± 318 ml vs. 498 ± 228 respectively, p = 0.009) (Goobie et al., 2018). In addition, the relative risk of relevant blood loss (defined by authors as >20 ml/kg) was increased by 2.1 in patients receiving placebo with no thromboembolic events or seizures reported in any of the groups (Goobie et al., 2018). Nevertheless, in a series of 100 cases of patients undergoing complex spinal surgery and receiving a loading IV TXA dose of 50 mg/kg and a maintenance dose of 5 mg/kg/h, Lin et al. reported an incidence of 3% of thromboembolic events potentially related to TXA administration (Goobie et al., 2018). One patient (n = 1) experienced pulmonary embolism (PE) whereas deep vein thrombosis (DVT) was diagnosed in two patients. No myocardial infraction, seizures, stroke or renal failure was reported (Goobie et al., 2018).
This retrospective study demonstrated a higher portion of PE with TXA (2 subjects (4.3%) vs. 0%, p = 0.0487, respectively). When analyzing thrombotic complications together (PE and DVT) there was no difference between TXA and control. We believe this is likely due to the relatively small size of this study.
An essential limitation of this observational study was its retrospective design and single-center population. Therefore, the high variability of the data limited the number of eligible subjects for data analysis. Secondly, due to the retrospective nature of this study, the doses of loading and maintenance dose were not standardized and were instead at the surgeon’s discretion, leading to variability in dosing and possible influence over the results. Thirdly, as described by several studies with similar patient population, blood loss is also affected by other variables, such as the number and type of osteotomies performed (posterior column osteotomy, pedicle subtraction osteotomy or vertebral column resection) and the number and type of interbody fusions (posterior or transforaminal) performed (Johnson et al., 1989; Mirza et al., 2008; Naik et al., 2017). Fourthly, the number of subjects included in the data analysis for each group was not similar, resulting in 42 subjects in the control group and 34 in the TXA group. Lastly, this study was not powered to assess the hypothesis that the administration of IV TXA could decrease EBL and/or RBC units transfused.
The results from the statistical analysis of this study suggest that the prophylactic use of intraoperative IV TXA during multilevel spinal fusion surgery could reduce intraoperative EBL and RBC unit transfusion requirements. Due to associated limitations of the retrospective design of this study, our findings should be corroborated in a prospective randomized dose-response study for further evaluation of the efficacy of standardized doses of TXA administration in this patient population.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by The Office of Responsible Research Practices—The Ohio State University. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
Study conception and design: AU, AT, ME-V, JF-D, BM, AG, SV, SB. Acquisition of data: AU, AT. Analysis and interpretation of data: AU, AT, MA-R. Drafting of manuscript: AU, AT, MA-R, ME-V, JF-D. Critical revision: AU, AT, ME-V, JF-D, BM, MA-R, AG, SV, SB.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The authors gratefully acknowledge Garegin Soghomonyan, B.Sc. and Andrew Costa, B.Sc. for their writing and editing collaboration, and Johnny McKeown, BSPS and Alicia Nahhas, BS for their editing collaboration (all of them provided authorization to be named on this publication).
ABT, allogeneic blood transfusions; ASA, American Society of Anesthesiology; CONSORT, Consolidated Standards of Reporting Trials; CI, confidence interval; DVT, deep vein thrombosis; EBL, estimated blood loss; ICU, intensive care unit; IV, intravenous; RBCs, red blood cells; FFP, fresh frozen plasma; TXA, tranexamic acid; PACU, post-anesthesia care unit; PE, pulmonary embolism.
Begg, C., Cho, M., Eastwood, S., Horton, R., Moher, D., Olkin, I., et al. (1996). Improving the quality of reporting of randomized controlled trials. The CONSORT statement. J. Am. Med. Assoc. 276, 637–639. doi:10.1001/jama.1996.03540080059030
Blake, D. R., Robson, P., Ho, M., Jubb, R. W., and McCabe, C. S. (2006). Preliminary assessment of the efficacy, tolerability and safety of a cannabis-based medicine (Sativex) in the treatment of pain caused by rheumatoid arthritis. Rheumatology 45, 50–52. doi:10.1093/rheumatology/kei183
Carabini, L. M., Moreland, N. C., Vealey, R. J., Bebawy, J. F., Koski, T. R., Koht, A., et al. (2018). A randomized controlled trial of low-dose tranexamic acid versus placebo to reduce red blood cell transfusion during complex multilevel spine fusion surgery. World Neurosurg. 110, e572–e579. doi:10.1016/j.wneu.2017.11.070
Chapman, M. P., Moore, E. E., Moore, H. B., Gonzalez, E., Gamboni, F., Chandler, J. G., et al. (2016). Overwhelming tPA release, not PAI-1 degradation, is responsible for hyperfibrinolysis in severely injured trauma patients. J. Trauma Acute Care Surg. 80, 16–23; discussion 23-5. doi:10.1097/ta.0000000000000885
Cheriyan, T., Maier, S. P., Bianco, K., Slobodyanyuk, K., Rattenni, R. N., Lafage, V., et al. (2015). Efficacy of tranexamic acid on surgical bleeding in spine surgery: a meta-analysis. Spine J. 15, 752–761. doi:10.1016/j.spinee.2015.01.013
Choi, H. Y., Hyun, S.-J., Kim, K.-J., Jahng, T.-A., and Kim, H.-J. (2017). Effectiveness and safety of tranexamic acid in spinal deformity surgery. J. Korean Neurosurg. Soc. 60, 75–81. doi:10.3340/jkns.2016.0505.004
Colomina, M. J., Koo, M., Basora, M., Pizones, J., Mora, L., and Bagó, J. (2017). Intraoperative tranexamic acid use in major spine surgery in adults: a multicentre, randomized, placebo-controlled trial † †This Article is accompanied by Editorial Aew470. Br. J. Anaesth. 118, 380–390. doi:10.1093/bja/aew434
Couturier, R., and Grassin-Delyle, S. (2014). Tranexamic acid. Anesth. Analg. 119, 498–499. doi:10.1213/ane.0000000000000254
Dai, L., Bevan, D., Rangarajan, S., Sørensen, B., and Mitchell, M. (2011). Stabilization of fibrin clots by activated prothrombin complex concentrate and tranexamic acid in FVIII inhibitor plasma. Haemophilia 17, e944–e948. doi:10.1111/j.1365-2516.2011.02491.x
DePasse, J. M., Palumbo, M. A., Haque, M., Eberson, C. P., and Daniels, A. H. (2015). Complications associated with prone positioning in elective spinal surgery. World J. Orthop. 6, 351–359.doi:10.5312/wjo.v6.i3.351
Elgafy, H., Bransford, R. J., McGuire, R. A., Dettori, J. R., and Fischer, D. (2010). Blood loss in major spine surgery. Spine 35, S47–S56. doi:10.1097/brs.0b013e3181d833f6
Goobie, S. M., Zurakowski, D., Glotzbecker, M. P., McCann, M. E., Hedequist, D., Brustowicz, R. M., et al. (2018). Tranexamic acid is efficacious at decreasing the rate of blood loss in adolescent scoliosis surgery. J. Bone Joint Surg. 100, 2024–2032. doi:10.2106/jbjs.18.00314
Grassin-Delyle, S., Theusinger, O. M., Albrecht, R., Mueller, S., Spahn, D. R., Urien, S., et al. (2018). Optimisation of the dosage of tranexamic acid in trauma patients with population pharmacokinetic analysis. Anaesthesia 73, 719–729. doi:10.1111/anae.14184
Healthcare Cost and Utilization Project (HCUP) (2017). Most common operations during inpatient stays
Hunt, B. J. (2015). The current place of tranexamic acid in the management of bleeding. Anaesthesia 70 (Suppl. 1), 50–53, e18. doi:10.1111/anae.12910
Farrokhi, M. R., Kazemi, A. P., Eftekharian, H. R., and Akbari, K. (2011). Efficacy of prophylactic low dose of tranexamic acid in spinal fixation surgery. J. Neurosurg. Anesthesiol. 23, 290–296. doi:10.1097/ana.0b013e31822914a1
Hijazi, N., Abu Fanne, R., Abramovitch, R., Yarovoi, S., Higazi, M., Abdeen, S., et al. (2015). Endogenous plasminogen activators mediate progressive intracerebral hemorrhage after traumatic brain injury in mice. Blood 125, 2558–2567. doi:10.1182/blood-2014-08-588442
Hsia, T.-Y., McQuinn, T. C., Mukherjee, R., Deardorff, R. L., Squires, J. E., Stroud, R. E., et al. (2010). Effects of aprotinin or tranexamic acid on proteolytic/cytokine profiles in infants after cardiac surgery. Ann. Thorac. Surg. 89, 1843–1852. doi:10.1016/j.athoracsur.2010.02.069
Hu, S. S. (2004). Blood loss in adult spinal surgery. Eur. Spine J. 13 (Suppl. 1), S3–S5. doi:10.1007/s00586-004-0753-x
Jimenez, J. J., Iribarren, J. L., Lorente, L., Rodriguez, J. M., Hernandez, D., Nassar, M. I., et al. (2007). Tranexamic acid attenuates inflammatory response in cardiopulmonary bypass surgery through blockade of fibrinolysis: a case control study followed by a randomized double-blind controlled trial. Crit. Care 11, R117. doi:10.1186/cc6173
Johnson, D. J., Johnson, C. C., Goobie, S. M., Nami, N., Wetzler, J. A., Sponseller, P. D., et al. (2017). High-dose versus low-dose tranexamic acid to reduce transfusion requirements in pediatric scoliosis surgery. J. Pediatr. Orthop. 37, e552–e557. doi:10.1097/bpo.0000000000000820
Johnson, R. G., Murphy, M., and Miller, M. (1989). Fusions and transfusions. Spine 14, 358–362. doi:10.1097/00007632-198904000-00002
Karimi, S., Lu, V. M., Nambiar, M., Phan, K., Ambikaipalan, A., and Mobbs, R. J. (2019). Antifibrinolytic agents for paediatric scoliosis surgery: a systematic review and meta-analysis. Eur. Spine J. 28, 1023–1034.
Kashuk, J. L., Moore, E. E., Sawyer, M., Wohlauer, M., Pezold, M., Barnett, C., et al. (2010). Primary fibrinolysis is integral in the pathogenesis of the acute coagulopathy of trauma. Ann. Surg. 252, 434–442; discussion 443-4. doi:10.1097/SLA.0b013e3181f09191
Lin, J. D., Lenke, L. G., Shillingford, J. N., Laratta, J. L., Tan, L. A., Fischer, C. R., et al. (2018). Safety of a high-dose tranexamic acid protocol in complex adult spinal deformity: analysis of 100 consecutive cases. Spine Deformity 6, 189–194. doi:10.1016/j.jspd.2017.08.007
Lu, V. M., Ho, Y.-T., Nambiar, M., Mobbs, R. J., and Phan, K. (2018). The perioperative efficacy and safety of antifibrinolytics in adult spinal fusion surgery. Spine 43, E949–E958. doi:10.1097/brs.0000000000002580
Mathai, K. M., Kang, J. D., Donaldson, W. F., Lee, J. Y., and Buffington, C. W. (2012). Prediction of blood loss during surgery on the lumbar spine with the patient supported prone on the Jackson table. Spine J. 12, 1103–1110. doi:10.1016/j.spinee.2012.10.027
Mirza, S. K., Deyo, R. A., Heagerty, P. J., Konodi, M. A., Lee, L. A., Turner, J. A., et al. (2008). Development of an index to characterize the “invasiveness” of spine surgery. Spine 33, 2651–2661; discussion 2662. doi:10.1097/brs.0b013e31818dad07
Luo, W., Sun, R. X., Jiang, H., and Ma, X. L. (2018). The efficacy and safety of topical administration of tranexamic acid in spine surgery: a meta-analysis. J. Orthop. Surg. Res. 13, 96. doi:10.1186/s13018-018-0815-0
Nagabhushan, R. M., Shetty, A. P., Dumpa, S. R., Subramanian, B., Kanna, R. M., and Shanmuganathan, R. (2018). Effectiveness and safety of batroxobin, tranexamic acid and a combination in reduction of blood loss in lumbar spinal fusion surgery. Spine 43, E267–E273. doi:10.1097/brs.0000000000002315
Naik, B. I., Nemergut, E. C., and Durieux, M. E. (2017). Complexities of bleeding during spine surgery: it'll take your (mechanical) breath away. Anesthesiology 126, 195. doi:10.1097/aln.0000000000001411
Neilipovitz, D. T., Murto, K., Hall, L., Barrowman, N. J., and Splinter, W. M. (2001). A randomized trial of tranexamic acid to reduce blood transfusion for scoliosis surgery. Anesth. Analg. 93, 82–87. doi:10.1097/00000539-200107000-00018
Shakeri, M., Salehpour, F., Shokouhi, G., Aeinfar, K., Aghazadeh, J., Mirzaei, F., et al. (2018). Minimal dose of tranexamic acid is effective in reducing blood loss in complex spine surgeries: a randomized double-blind placebo controlled study. Asian Spine J. 12, 484–489. doi:10.4184/asj.2018.12.3.484
Verma, K., Errico, T. J., Vaz, K. M., and Lonner, B. S. (2010). A prospective, randomized, double-blinded single-site control study comparing blood loss prevention of tranexamic acid (TXA) to epsilon aminocaproic acid (EACA) for corrective spinal surgery. BMC Surg. 10, 13. doi:10.1186/1471-2482-10-13
Walterscheid, Z., O’Neill, C., and Carmouche, J. (2017). Tranexamic acid in adult elective orthopaedic and complex spinal surgery: a review. Surg Rehabil 1, 1–4. doi:10.15761/srj.1000104
Wong, J., El Beheiry, H., Rampersaud, Y. R., Lewis, S., Ahn, H., De Silva, Y., et al. (2008). Tranexamic Acid reduces perioperative blood loss in adult patients having spinal fusion surgery. Anesth. Analg. 107, 1479–1486. doi:10.1213/ane.0b013e3181831e44
Xue, P., Yang, J., Xu, X., Liu, T., Huang, Y., Qiao, F., et al. (2018). The efficacy and safety of tranexamic acid in reducing perioperative blood loss in patients with multilevel thoracic spinal stenosis. Medicine 97, e13643. doi:10.1097/md.0000000000013643
Yoo, J. S., Ahn, J., Karmarkar, S. S., Lamoutte, E. H., and Singh, K. (2019). The use of tranexamic acid in spine surgery. Ann. Transl. Med. 7 (Suppl. 5), S172. doi:10.21037/atm.2019.05.36
Keywords: neurosurgery, spinal surgery, blood loss, tranexamic acid, spinal fusion, blood transfusion
Citation: Todeschini AB, Uribe AA, Echeverria-Villalobos M, Fiorda-Diaz J, Abdel-Rasoul M, McGahan BG, Grossbach AJ, Viljoen S and Bergese SD (2020) Efficacy of Intravenous Tranexamic Acid in Reducing Perioperative Blood Loss and Blood Product Transfusion Requirements in Patients Undergoing Multilevel Thoracic and Lumbar Spinal Surgeries: A Retrospective Study. Front. Pharmacol. 11:566956. doi: 10.3389/fphar.2020.566956
Received: 29 May 2020; Accepted: 15 October 2020;
Published: 30 November 2020.
Edited by:
Francesco Rossi, University of Campania Luigi Vanvitelli, ItalyReviewed by:
Stuart McCluskey, University of Toronto, CanadaCopyright © 2020 Echeverria-Villalobos, Fiorda-Diaz, Abdel-Rasoul, McGahan, Grossbach, Viljoen and Bergese. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Alberto A. Uribe, QWxiZXJ0by5VcmliZUBvc3VtYy5lZHU=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.