
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
REVIEW article
Front. Pharmacol., 11 September 2020
Sec. Drugs Outcomes Research and Policies
Volume 11 - 2020 | https://doi.org/10.3389/fphar.2020.01205
 Olayinka O. Ogunleye1,2
Olayinka O. Ogunleye1,2 Debashis Basu3,4
Debashis Basu3,4 Debjani Mueller5
Debjani Mueller5 Jacqueline Sneddon6
Jacqueline Sneddon6 R. Andrew Seaton6,7,8
R. Andrew Seaton6,7,8 Adesola F. Yinka-Ogunleye9
Adesola F. Yinka-Ogunleye9 Joshua Wamboga10
Joshua Wamboga10 Nenad Miljković11
Nenad Miljković11 Julius C. Mwita12
Julius C. Mwita12 Godfrey Mutashambara Rwegerera13
Godfrey Mutashambara Rwegerera13 Amos Massele14
Amos Massele14 Okwen Patrick15,16
Okwen Patrick15,16 Loveline Lum Niba15,17
Loveline Lum Niba15,17 Melaine Nsaikila15
Melaine Nsaikila15 Wafaa M. Rashed18
Wafaa M. Rashed18 Mohamed Ali Hussein18
Mohamed Ali Hussein18 Rehab Hegazy19
Rehab Hegazy19 Adefolarin A. Amu20
Adefolarin A. Amu20 Baffour Boaten Boahen-Boaten21
Baffour Boaten Boahen-Boaten21 Zinhle Matsebula22
Zinhle Matsebula22 Prudence Gwebu22
Prudence Gwebu22 Bongani Chirigo22
Bongani Chirigo22 Nongabisa Mkhabela22
Nongabisa Mkhabela22 Tenelisiwe Dlamini22
Tenelisiwe Dlamini22 Siphiwe Sithole22
Siphiwe Sithole22 Sandile Malaza22
Sandile Malaza22 Sikhumbuzo Dlamini22
Sikhumbuzo Dlamini22 Daniel Afriyie23
Daniel Afriyie23 George Awuku Asare24
George Awuku Asare24 Seth Kwabena Amponsah25
Seth Kwabena Amponsah25 Israel Sefah26,27
Israel Sefah26,27 Margaret Oluka28
Margaret Oluka28 Anastasia N. Guantai28
Anastasia N. Guantai28 Sylvia A. Opanga29
Sylvia A. Opanga29 Tebello Violet Sarele30
Tebello Violet Sarele30 Refeletse Keabetsoe Mafisa31
Refeletse Keabetsoe Mafisa31 Ibrahim Chikowe32
Ibrahim Chikowe32 Felix Khuluza32
Felix Khuluza32 Dan Kibuule33
Dan Kibuule33 Francis Kalemeera33
Francis Kalemeera33 Mwangana Mubita33
Mwangana Mubita33 Joseph Fadare34,35
Joseph Fadare34,35 Laurien Sibomana36
Laurien Sibomana36 Gwendoline Malegwale Ramokgopa3,4
Gwendoline Malegwale Ramokgopa3,4 Carmen Whyte3,4
Carmen Whyte3,4 Tshegofatso Maimela3,4
Tshegofatso Maimela3,4 Johannes Hugo4,37
Johannes Hugo4,37 Johanna C. Meyer38
Johanna C. Meyer38 Natalie Schellack38
Natalie Schellack38 Enos M. Rampamba38,39
Enos M. Rampamba38,39 Adel Visser40
Adel Visser40 Abubakr Alfadl41,42
Abubakr Alfadl41,42 Elfatih M. Malik43,44
Elfatih M. Malik43,44 Oliver Ombeva Malande45,46
Oliver Ombeva Malande45,46 Aubrey C. Kalungia47
Aubrey C. Kalungia47 Chiluba Mwila47
Chiluba Mwila47 Trust Zaranyika48
Trust Zaranyika48 Blessmore Vimbai Chaibva49
Blessmore Vimbai Chaibva49 Ioana D. Olaru50,51
Ioana D. Olaru50,51 Nyasha Masuka52
Nyasha Masuka52 Janney Wale53
Janney Wale53 Lenias Hwenda54
Lenias Hwenda54 Regina Kamoga10,55
Regina Kamoga10,55 Ruaraidh Hill56
Ruaraidh Hill56 Corrado Barbui57
Corrado Barbui57 Tomasz Bochenek58
Tomasz Bochenek58 Amanj Kurdi59,60
Amanj Kurdi59,60 Stephen Campbell61,62
Stephen Campbell61,62 Antony P. Martin63,64
Antony P. Martin63,64 Thuy Nguyen Thi Phuong65
Thuy Nguyen Thi Phuong65 Binh Nguyen Thanh65
Binh Nguyen Thanh65 Brian Godman38,59,66,67*
Brian Godman38,59,66,67*Background: The COVID-19 pandemic has already claimed considerable lives. There are major concerns in Africa due to existing high prevalence rates for both infectious and non-infectious diseases and limited resources in terms of personnel, beds and equipment. Alongside this, concerns that lockdown and other measures will have on prevention and management of other infectious diseases and non-communicable diseases (NCDs). NCDs are an increasing issue with rising morbidity and mortality rates. The World Health Organization (WHO) warns that a lack of nets and treatment could result in up to 18 million additional cases of malaria and up to 30,000 additional deaths in sub-Saharan Africa.
Objective: Document current prevalence and mortality rates from COVID-19 alongside economic and other measures to reduce its spread and impact across Africa. In addition, suggested ways forward among all key stakeholder groups.
Our Approach: Contextualise the findings from a wide range of publications including internet-based publications coupled with input from senior-level personnel.
Ongoing Activities: Prevalence and mortality rates are currently lower in Africa than among several Western countries and the USA. This could be due to a number of factors including early instigation of lockdown and border closures, the younger age of the population, lack of robust reporting systems and as yet unidentified genetic and other factors. Innovation is accelerating to address concerns with available equipment. There are ongoing steps to address the level of misinformation and its consequences including fines. There are also ongoing initiatives across Africa to start addressing the unintended consequences of COVID-19 activities including lockdown measures and their impact on NCDs including the likely rise in mental health disorders, exacerbated by increasing stigma associated with COVID-19. Strategies include extending prescription lengths, telemedicine and encouraging vaccination. However, these need to be accelerated to prevent increased morbidity and mortality.
Conclusion: There are multiple activities across Africa to reduce the spread of COVID-19 and address misinformation, which can have catastrophic consequences, assisted by the WHO and others, which appear to be working in a number of countries. Research is ongoing to clarify the unintended consequences given ongoing concerns to guide future activities. Countries are learning from each other.
The novel coronavirus named SARS-CoV-2 causing COVID-19 was first reported in Hubei Province in China in December 2019 (Guan et al., 2020; Li Q. et al., 2020; World Health Organisation, 2020a; Wu and McGoogan, 2020), and has subsequently spread to all continents (WHO, 2020a). COVID-19 is transmitted from person to person through respiratory droplets as well as directly through touching surfaces and other fomites (Chiang and El Sony, 2020; Huang et al., 2020; Perencevich et al., 2020; WHO, 2020b; World Health Organisation, 2020b). Initial observations from China suggested a case fatality ratio (CFR) of 2.3% (Wu and McGoogan, 2020). In their July 1, 2020 report, the World Health Organization (WHO) suggested a case fatality ratio (CFR) of 4.91% based on 10,357,662 confirmed cases worldwide and 508,055 recorded deaths (WHO, 2020a).
Increased morbidity and case fatality from COVID-19 is associated with a number of underlying health conditions, alongside male gender and older age. These include hypertension, cardiovascular disease (CVD), diabetes, obesity, chronic kidney disease, chronic obstructive pulmonary disease (COPD), and history of smoking and shortness of breath, as well as some immunosuppressive conditions and potentially blood type (Basu, 2020; Bode et al., 2020; CDC COVID-19 Response Team, 2020; Centre for Disease Prevention and Control, 2020; Di Lorenzo and Di Trolio, 2020; Dietz and Santos-Burgoa, 2020; Docherty et al., 2020; Du et al., 2020; Ellinghaus et al., 2020; Fang et al., 2020; Hamid et al., 2020; Huang et al., 2020; Inciardi et al., 2020; Khunti et al., 2020; Kirby, 2020; Kluge et al., 2020; Matos and Chung, 2020; Richardson et al., 2020; Ryan et al., 2020; Shah et al., 2020; Vardavas and Nikitara, 2020; Williams et al., 2020; Zheng Z. et al., 2020). Ethnicity, particularly for people of Black Afro-Caribbean origin alongside those from South Asia, has also emerged as a significant factor associated with a higher mortality risk versus the white population in Europe and the United States of America (USA) (Bambra et al., 2020; Khunti et al., 2020; Kirby, 2020; Pan et al., 2020; Pareek et al., 2020; Public Health England, 2020). However, it is currently not fully understood how ethnicity, poverty and deprivation, cultural and behavioral differences, as well as underlying health, interplay in morbidity or mortality risk especially with currently lower mortality rates in Africa at the end of June 2020 compared with a number of European countries and the USA (WHO, 2020a).
Response activities to the COVID-19 pandemic typically included personal protection through physical distancing and hand washing coupled with respiratory precautions through face covering (Courtemanche et al., 2020; Ng et al., 2020; WHO, 2020b; WHO, 2020c; WHO, 2020d; World Health Organisation, 2020b). Increased testing and screening with contact tracing are fundamental to transmission control, and this has been variably combined with “locking down” of public places including educational establishments, retail outlets, factories and offices combined with closure of borders and quarantining suspected persons (Nussbaumer-Streit et al., 2020; Rajendran et al., 2020; WHO, 2020d). Case management of patients includes supportive care with supplementary oxygen coupled with ventilatory support for those most severely affected (Berlin et al., 2020; Marini and Gattinoni, 2020; Matos and Chung, 2020; Meng et al., 2020; Nigeria Centre for Disease Control, 2020a; World Health Organisation, 2020b). Depending on the threshold for hospital admission, it is estimated that up to 17% of hospitalized patients will require intensive care, with an appreciable proportion needing mechanical ventilation (World Health Organisation Europe, 2020; Docherty et al., 2020; Mahase, 2020a; Richardson et al., 2020). This is a concern even in high-income countries where there have been challenges with the availability of critical care beds, appropriately trained staff and personal protective equipment (PPE) (Di Lorenzo and Di Trolio, 2020; IHME, 2020a; IHME, 2020b; Lacobucci, 2020; Massonnaud et al., 2020).
An encouraging example of a positive response among low- and middle- income countries (LMICs) is Vietnam where multiple activities including extensive testing, contact tracing, and social distancing, under the government slogan “Fighting the epidemic is like fighting against the enemy”, have been successful in limiting the tranmission of COVID-19 with only 355 confirmed cases by the end of June 2020 and no recorded attributable mortality (Hall, 2020; Jones, 2020; Ministry of Health, VietNam, 2020; Pearson and Nguyen, 2020; Thai et al., 2020; WHO, 2020a).
Currently, there does not appear to be a cure for COVID-19; however, there are a number of medicines undergoing trials including antivirals, steroids, antimalarials, immunomodulators, and herbal medicines, some of which have shown positive findings although there have been concerns with the trial design of a number of studies (Das et al., 2020; ECDC, 2020a; Geleris et al., 2020; Luo L. et al., 2020; Mehta et al., 2020; Pradhan et al., 2020; Recovery Collaborative Group, 2020; Sanders et al., 2020; Scavone et al., 2020; Zhong H. et al., 2020).
The most promising therapeutic breakthrough to date has come from the UK-based adaptive randomised Recovery trial (ECDC, 2020a; Recovery Collaborative Group, 2020). The low cost corticosteroid dexamethasone has recently been shown to significantly reduce mortality in the most severely affected patients with COVID-19; patients with an oxygen requirement and those requiring ventilatory support (Recovery Collaborative Group, 2020). Other recent studies have also shown benefit from corticosteroids in critically ill patients increasing the number of days alive and free of mechanical ventilation as well as reducing mortality (Sterne et al., 2020; Tomazini et al., 2020). The prescribing of 6mg of dexamethasone daily for 10 days is now recommended for widespread use in the UK unless contraindicated for other reasons as well as endorsed by the National Institute of Health (NIH) in the USA (NIH, 2020a; Rees, 2020). However, currently optimal dosing and duration of dexamethasone in COVID-19 is unknown; consequently, current recommendations reflect those used in the Recovery trial.
Initial studies with remdesivir failed to demonstrate clinical benefit over placebo although these were underpowered (The Guardian, 2020a; BMJ Best Practice - Coronavirus disease 2019 (COVID-19), 2020; Wang Y. et al., 2020). More recently, larger scale studies conducted by NIH in the USA have shown encouraging results including a reduction in the time to recovery and a trend towards lower mortality (hazard ratio for death = 0.70) leading to the issuance of an Emergency Use Authorization by the US FDA as well as endorsement by the European Medicines Agency and the NHS in the UK (Beigel et al., 2020; EMA, 2020; NIH, 2020b; UK Medicines & Healthcare products Regulatory Agency, 2020; US Food and Drug Administration, 2020). However, further studies are needed before the prescribing of remdesivir can be fully endorsed.
However, much controversy surrounds the use of chloroquine and hydroxychloroquine with or without azithromycin for both the prevention and treatment of COVID-19. Following initial studies in China, coupled with the findings of Gautret et al. (2020) (Boulware et al., 2020; Das et al., 2020; Cortegiani et al., 2020; Gao et al., 2020; Gautret et al., 2020), its use was endorsed among a number of governments and medical societies (Bokpe, 2020; Channnel News Asia, 2020; East African, 2020; Rich, 2020; Sciama, 2020; Tilangi et al., 2020). However, the lack of a comparator arm in the initial studies has been heavily criticised coupled with concerns with side-effects including cardiac side-effects with hydroxychloroquine (International Society of Antimicrobial Chemotherapy, 2020; Gautret et al., 2020; ISAC/ Elsevier, 2020; Borba et al., 2020; Ferner and Aronson, 2020; Littlejohn, 2020) as well as reports of fatal overdoses (Abena et al., 2020; Das et al., 2020; GuruGamer, 2020; Nga et al., 2020; Politi, 2020). Recent studies have failed to demonstrate any clinical benefit for both the prevention and treatment of COVID-19 (Boulware et al., 2020; Geleris et al., 2020; Recovery Trial, 2020a; Rosenberg et al., 2020). The study by Mehra et al. (Mehra et al., 2020) also showed increased mortality with chloroquine or hydroxychloroquine; however, this has now been retracted subject to external auditing (Mehra et al., 2020; The Lancet, 2020). The European Medicines Agency now advises caution with the prescribing of hydroxychloroquine outside of clinical trials (European Medicine Agency, 2020a), and the WHO has halted the hydroxychloroquine arm in its ongoing Solidarity Trial with the NIH in the USA also halting the use of hydroxychloroquine in its studies (WHO, 2020e; ECDC, 2020a; NIH, 2020c). In South Africa, the South African Pharmacy Council has also warned against the misuse of hydroxychloroquine for the treatment of COVID-19, which builds on concerns from the regulatory agency given the lack of evidence (Masango, 2020; SAHPRA, 2020a).
The antiretroviral treatment (ART) lopinavir-ritonavir, which showed activity against MERS-CoV, has also been recommended for treating COVID-19 patients alongside arbidol (Cao et al., 2020; Kumar et al., 2020; Mitjà and Clotet, 2020; Zhong H. et al., 2020; Zhu et al., 2020). However, there have also been contrasting data regarding its effectiveness in COVID-19 patients, with most studies failing to show any clinical benefit including the UK Recovery study (Cao et al., 2020; ECDC, 2020a; Ford et al., 2020; Recovery Trial, 2020b). Consequently, lopinavir-ritonavir cannot currently be recommended for use outside of clinical trials and more recently the WHO has discontinued the lopinavir-ritonavir arm in the Solidarity Trial (WHO, 2020e). A recent study though by Hung et al. (2020) found that early triple antiviral therapy with interferon beta-1b, lopinavir/ritonavir and ribavirin alleviated the symptoms and shortened the duration of viral shedding and hospital stay compared with lopinavir/ ritonavir alone in patients with mild to moderate COVID-19 (Hung et al., 2020). Any positive findings though with combination therapies need confirmation before they can be endorsed. Studies regarding the potential effectiveness of nasal irrigation are also ongoing (US National Library of Medicine - ClinicalTrials.gov, 2020a; US National Library of Medicine - ClinicalTrials.gov, 2020b). This follows a pilot randomised study showing improvements in the duration of symptoms and viral shedding in patients with upper respiratory tract infections (Ramalingam et al., 2019), with a post-hoc re-analysis with a focus on those infected with coronaviruses also showing benefit (Ramalingam et al., 2020).
A number of other treatments focusing on the late inflammatory complications of COVID-19 (Gaborit et al., 2020; Jose and Manuel, 2020; Monteleone et al., 2020) are also under review. These include tocilizumab, which is widely used in rheumatoid arthritis and blocks Interleukin-6 (IL-6), a combination of emapalumab, anakinra and sarilumab (Clinical Trials Arena, 2020; Di Lorenzo and Di Trolio, 2020; Luo et al., 2020; Roumier et al., 2020; Toniati et al., 2020; Xu et al., 2020; Zhang C. et al., 2020), and interferons (Andreakos and Tsiodras, 2020; Prokunina-Olsson et al., 2020; Shalhoub, 2020; Tu et al., 2020). These are currently not recommended for use outside of clinical trials. Ongoing studies are also using the plasma from affected patients along with prior titration of neutralising antibodies (Bloch et al., 2020; ECDC, 2020a; UK Department of Health and Social Care, 2020; Tu et al., 2020; Wu et al., 2020), and anticoagulants for hypercoagulability states (Cunningham et al., 2020; Paranjpe et al., 2020; Shi et al., 2020; Tang et al., 2020; Xu et al., 2020). Again, these experimental therapies cannot be recommended until more clinical trial data becomes available.
There has also been controversy surrounding BCG vaccination as possible protection against COVID-19 (O'Neill and Netea, 2020; Schaaf et al., 2020). The WHO is warning against claims of effectiveness based on current ecological studies, with the South African Government and leading scientists also warning against diverting stocks away from neonatal vaccination programmes given concerns with shortages until more trial data becomes available (Medical Brief, 2020a; SAHPRA, 2020b; Schaaf et al., 2020; WHO, 2020f).
There are also concerns with the inappropriate use of medicinal plants to prevent and treat COVID-19, which such use particularly prevalent in some sub-Saharan African countries as this can cause more harm than good (Ekor, 2014; Liwa et al., 2014; Nkeck et al., 2020; Nordling, 2020; Yang, 2020). Safety fears are enhanced by the lack of data when used to prevent or treat COVID-19 along with other treatments that patients may be taking including antivirals, antibiotics as well as medicines for non-communicable diseases (NCDs) (Nkeck et al., 2020; Yang, 2020). We are aware that some herbal medicines are showing promise based on in vitro and small-scale clinical studies (Ang et al., 2020; Luo E. et al., 2020; Luo L. et al., 2020; Vellingiri et al., 2020; Yang, 2020; Zhang L. et al., 2020). However, their use outside of such studies is a concern until more data becomes available especially if their use causes delay in patients seeking appropriate care from healthcare professionals as their symptoms develop (Yang, 2020).
The controversies and issues surrounding a number of the treatments, the redaction of recent studies, as well as concerns with trial design in a number of studies (Bae et al., 2020; ECDC, 2020a; International Society of Antimicrobial Chemotherapy, 2020; ISAC/ Elsevier, 2020; Mehta et al., 2020; The Lancet, 2020), means it is essential that treatment recommendations should only be made once the results of robust trials are known (Council for International Organizations of Medical Sciences, 2020; Godman, 2020).
There are a number of unintended consequences arising from COVID-19. These include Governments diverting personnel and resources away from priority diseases including both infectious and non-infectious diseases. Reducing antimicrobial resistance (AMR) is a key activity across countries especially among LMICs as it increases morbidity, mortality and costs (Founou et al., 2017; Cassini et al., 2019; Hofer, 2019; Khan et al., 2019). However, diverting attention away from AMR, including ongoing efforts to reduce inappropriate self-purchasing of antibiotics, which is prevalent across many countries, as well as routine immunisation programmes for existing infectious diseases, will inevitably have a significant impact on future patient care (Ghosal and Milko, 2020; World Health Organization, 2020c; Health 24, 2020; Kalungia et al., 2016; Auta et al., 2019; Kalungia and Godman, 2019; Godman et al., 2020a; Hofman and Goldstein, 2020; Jerving, 2020; Lorgelly and Adler, 2020; Thornton, 2020; UN News, 2020; World Health Organisation, 2020d). Self-purchasing of antibiotics is a particular concern with the clinical presentation of COVID-19 overlapping with other infectious diseases including tuberculosis (TB), viral and bacterial respiratory tract infections, and pneumonia, making a differential diagnosis challenging exacerbated by limited diagnostic facilities in most communities (Godman et al., 2020b; Kasozi et al., 2020; Ongole et al., 2020). In hospitals, establishing antimicrobial stewardship programmes and other activities (Mendelson and Matsoso, 2015; Ghana Ministry of Health, 2018; Schellack et al., 2018; Anand Paramadhas et al., 2019; Afriyie et al., 2020; Godman et al., 2020b) can improve antibiotic prescribing where there is little evidence of bacterial co-infection (Godman et al., 2020a; Seaton, 2020; Zhou et al., 2020). Consequently, it is essential that such activities be introduced where necessary to guide future antibiotic prescribing among suspected COVID-19 patients (Seaton, 2020).
We are aware that the Ebola outbreak in Guinea, Liberia, and Sierra Leone between 2014 and 2016 resulted in as many people dying from HIV/AIDS, TB, and malaria as Ebola due to reduced access to health care (Parpia et al., 2016; Ghosal and Milko, 2020; Krubiner et al., 2020). There are also concerns that an appreciable reduction in the distribution of protective bed nets (75%) and medicines for treating malaria due to lockdown measures, combined with no media campaigns, could result in up to 18 million additional cases and up to 30,000 additional deaths in sub-Saharan Africa alone compared to 2018 (Cash and Patel, 2020; Krubiner et al., 2020; World Health Organisation, 2020c). Whilst the latest evidence suggests that HIV positive patients do not have a higher COVID-19 infection rate, or a significantly different disease course than HIV-negative individuals (Blanco et al., 2020; Guo et al., 2020; Härter et al., 2020; Tarkang, 2020), patients’ fears of contracting COVID-19 when they attend clinics, as well as limited access to health facilities and treatment during lockdown, will negatively impact on treatment and adherence to medicines as well as initial diagnosis (Africa News, 2020a; Chaiyachati et al., 2014; Mbuagbaw et al., 2015; Jerving, 2020; Krubiner et al., 2020; Tarkang, 2020). Medicine supplies can potentially be addressed through differentiated service delivery and other programmes (Jerving, 2020; Tarkang, 2020; Wilkinson and Grimsrud, 2020). Telemedicine and other technologies could also potentially help with consultations, with mobile technologies helping with tracking and tracing COVID-19 patients (Cohen et al., 2020; IOL, 2020; LinksCommunity, 2020).
There are also concerns that lockdown measures will negatively impact of the management of patients with non-communicable diseases (NCDs) (Kluge et al., 2020). This includes a lack of support and access to facilities to improve lifestyle management, monitor patient and regularly provide essential medicines (Kluge et al., 2020). Ongoing national plans to reduce morbidity and mortality due to NCDs, especially CVD and diabetes, across continents including Africa (Mensah et al., 2015; Amegah, 2018; Godman et al., 2020c; Godman et al., 2020d) could also be compromised by reduced access to medicines, cancelled or missed appointments due to patients' reduced access to facilities and fear of coming into contact with COVID-19 patients in healthcare facilities, and not following lifestyle advice (Kabale et al., 2020; Kluge et al., 2020; Nachimuthu et al., 2020). However, we are aware that governments are committing extra resources to try and minimise these unintended consequences (Ebrahim and Lakay, 2020). Issues relating to medical supplies can again be addressed by measures to extend prescription lengths (Al-Quteimat and Amer, 2020; Republic of South Africa Government Gazette, 2020; Lakay, 2020) as well as home delivery of medicines, with concerns with consultations potentially addressed through technologies such as telemedicine (Africa Health IT News, 2020a; LinksCommunity, 2020; Webster, 2020).
Other serious consequences include the exacerbation of mental health conditions during lockdown, the implications for frontline healthcare workers in terms of their health and wellbeing, and anxiety of citizens about their health (Brooks et al., 2020; Cullen et al., 2020; Endomba et al., 2020; González-Sanguino et al., 2020; Habersaat et al., 2020; Hwang et al., 2020; Kaufman et al., 2020; Li W. et al., 2020; Rajkumar, 2020; Ren et al., 2020; Wang C. et al., 2020a; Wang C. et al., 2020b; WHO, 2020g; Xiang et al., 2020). Patients with COVID-19 are also at increased risk of requiring psychotropic medicines because mild-to-moderate illness may result in adverse psychological effects from the diagnosis, from the symptoms, the need for forced isolation, any associated loss of income, and the potential risk of death. This might trigger new psychiatric symptoms or exacerbate underlying psychiatric conditions. In moderate-to-severe clinical situations, there is a risk that patients could develop altered states of consciousness such as hypo- or hyperkinetic delirium, which may require treatment with psychotropic medications (Reade and Finfer, 2014). In addition, some of the medical treatments that have been proposed for COVID-19 could contribute to onset or worsening of psychiatric symptoms. These include psychiatric disturbances with antivirals and steroids as well as depressive-dysphoric experiences with interferons (Tamam et al., 2003; Warrington and Bostwick, 2006; Manfredi et al., 2010; Kenna et al., 2011).
In addition, patients with existing mental illnesses may well have difficulties with accessing regular help during the pandemic unless pro-actively addressed (United Nations, 2020a; Yao et al., 2020). This includes continued access to medicines and treatments for those with long-term mental health conditions since sudden discontinuation should be avoided (WHO, 2020g). Worsening of mental health may be greater in patients with conditions such as schizophrenia with challenges in continuing active case management in the community during the pandemic as well as concerns with administering long-acting injections where pertinent, and performing regular blood tests in patients prescribed clozapine (Kozloff et al., 2020). Pro-active and timely support is needed for all patients with mental health conditions to avoid deteriorating conditions (Endomba et al., 2020; Salum et al., 2020; WHO, 2020g; Xiang et al., 2020). There are also reports of an increase in gender-based violence across countries, including African countries, as a result of lockdown measures, which also needs addressing going forward (Campbell, 2020; Chandan et al., 2020; Mahase, 2020b; SADC, 2020; United Nations., 2020b).
COVID-19 poses a particular challenge for the African continent because of existing high prevalence rates of other infectious diseases including human immunodeficiency virus (HIV)/ acquired immunodeficiency syndrome (AIDS), TB, cholera, and malaria, along with high rates of AMR and a disproportionate burden of poverty (UNAIDS, 2019; World Health Organisation, 2019; WHO, 2019a; Ataguba, 2020; Godman et al., 2020a; Simpson, 2020; United Nations Economic Commission for Africa, 2020a; WHO, 2020b; WHO, 2020c), with ongoing infectious disease initiatives appreciably challenged by COVID-19 (Mendelson and Matsoso, 2015; Ghana Ministry of Health, 2018; Godman et al., 2020a; Kowalska et al., 2020). The presence of multi-morbidity with NCDs will aggravate the situation further (Oni et al., 2015; So-Armah and Freiberg, 2018; Achwoka et al., 2019; Chang et al., 2019; Kansiime et al., 2019; Woldesemayat, 2020), with already high rates of CVD and diabetes a growing concern across Africa (Mensah et al., 2015; Godman et al., 2020b; Godman et al., 2020c).
Alongside this, there are ongoing challenges with available financial and human resources across Africa (Craven et al., 2020; Glied and Levy, 2020; Jayaram et al., 2020; Shepherd and van der Mark, 2020) including more limited availability of healthcare personnel and hospital beds including intensive care unit (ICU) beds (Murthy et al., 2015; Bates et al., 2018; Godman et al., 2019; El-Sadr and Justman, 2020; Godman et al., 2020c; Godman et al., 2020d; Martinez-Alvarez et al., 2020; United Nations, 2020b). Reports suggest there were just 1.8 hospital beds per 1,000 people across Africa before the pandemic, less than a third of those in France (Bavier, 2020). Oxygen is also not widely available and single room isolation can be a rarity making nosocomial transmission a concern. Overall, there appeared to be less than one ventilator and less than one ICU bed per 100,000 people in Africa compared with up to thirty times that number in the USA before the pandemic (Houreld et al., 2020), although there is regional variation (Murthy et al., 2015; El-Sadr and Justman, 2020; Shepherd and van der Mark, 2020; van den Heever, 2020). The availability of PPE across Africa was also a challenge in the early stages of the pandemic putting healthcare professionals at risk (Aljazeera, 2020; Lapolla et al., 2020; Le Roux and Dramowski, 2020; Saba and Jika, 2020). However, this is changing with increased local production of PPE, new local designs for face masks and ventilators (Bissada, 2020; Kenyatta University, 2020; Mining Review, 2020; Nyavor, 2020), as well as improved procurement processes enhanced by the recent launch of the pan-African medical supplies platform (South African Government, 2020a).
Most challenging though is over-crowding and lack of running water (and therefore a lack of hand washing) among the population, with an estimated 34% to 36% of people in Africa having no access to basic household washing facilities and 30% having only limited access (Bavier, 2020; El-Sadr and Justman, 2020; United Nations Economic Commission for Africa, 2020b). This is a particular concern among refugees, who require additional efforts to help prevent the spread of the virus including education on the rationale behind lockdown activities where pertinent (Associated Press, 2020; UNHCR, 2020).
Given these multiple issues and concerns, the UN Economic Commission for Africa (UNECA) initially estimated that the COVID-19 pandemic could potentially lead to 300,000 deaths across Africa and push 29 million people into extreme poverty (Bavier, 2020). In mid-April, the WHO warned that there could be up to 10 million cases of COVID-19 in Africa within six months (Aljazeera News, 2020a), rising to between 29 million and 44 million in the first year, with up to 190,000 deaths if containment measures failed (United Nations Africa Renewal, 2020). By the end of June 2020, there were over 303,000 COVID-19 cases among the WHO African countries with over 6000 deaths giving a CFR of 2.02% (WHO Regional Office Africa, 2020a). Consequently, absolute numbers of COVID-19 related deaths to date are still lower in Africa compared with other continents including the Americas and Europe (WHO, 2020a); however, this is changing as prevalence rates rise. There are also concerns with the reliability of the data among some of the African countries due to limited detection capacity and reliable tests as well as under-reporting of both deaths and prevalence rates (Ashly, 2020; Bruton and Edwards, 2020; Chiang and El Sony, 2020; Houreld and Lewis, 2020; McCaffrey, 2020; Mules, 2020; Shepherd and van der Mark, 2020; United Nations, 2020; WHO, 2020h). For instance, there has been no official data released from Tanzania since 8 May with the President stating the pandemic has largely been defeated despite concerns with truck drivers testing positive at borders and continued ongoing concerns with under-reporting (Houreld and Lewis, 2020; Mules, 2020; Mwai and Giles, 2020). Having said this, there have been concerns with the reliability of testing equipment (Aljazeera News, 2020b).
Other potential factors for currently lower prevalence rates and deaths in Africa compared with other continents could be a comparatively younger population as well as rapid instigation of lockdown and other measures. which build on experiences with other infectious diseases aided by the African Union, WHO Africa and the African Centre for Disease Control (CDC), as well as sensitivity of the virus to ambient temperatures (Africa CDC, 2020; Cash and Patel, 2020; EAC Secretariat, 2020; Lancet editorial, 2020; Pilling, 2020; WHO, 2020h; WHO, 2020i). The African CDC has been actively coordinating a strong multilateral response amongst African governments and other stakeholders towards COVID-19 building on the activities by the WHO in Africa and others (WHO Regional Office Africa, 2020b; WHO, 2020i; WHO, 2020j). The establishment of National Public Health Institutes among many African countries has also improved the response to public health threats (Nigeria CDC, 2018). Activities across Africa include developing laboratory expertise, training a volunteer health workforce, and risk communication. As mentioned, these built on Africa´s experience in dealing with other infectious diseases including Ebola, HIV, malaria and TB (El-Sadr and Justman, 2020; Nkengasong and Mankoula, 2020; Payne, 2020). The United Nations has also established a knowledge hub for COVID-19 to help African countries learn from each other (United Nations Economic Commission for Africa, 2020b). Testing has also appreciably increased in recent weeks across Africa (Burke, 2020) helped by Africa CDC and the WHO Africa, who have provided testing kits and training, with 48 African countries able to test for COVID-19 by 29 April 2020 compared with just two countries at the start of the pandemic (Ighobor, 2020; Simpson, 2020; WHO Regional Office Africa, 2020c).
Most African countries also rapidly instigated lockdown measures as well as social distancing to reduce the spread of the virus (Bavier, 2020; Dyer, 2020; United Nations., 2020b; United Nations Economic Commission for Africa, 2020a; WHO Regional Office Africa, 2020d). Similar to several African countries, Ghana early on began testing travellers on arrival in the country and isolating positive cases, as well as instigating testing among its citizens. Overall, Ghana has one of the highest testing rates in Africa having performed between 110,000 and 120,000 tests by the end of April 2020 (Di Caro, 2020). The Government of Ghana also established five key objectives to reduce the spread of the virus (Ghana News Agency, 2020; Zurek, 2020). Similar to most African countries, South Africa declared a national state of disaster in terms of section 27 (2) of the Disaster Management Act, 2002, and implemented a phased approach to lockdown with stage 5 introduced on March 27 2020, easing to stage 4 with effect from May 1 2020, which remains in place (Abdool Karim, 2020; South African Government, 2020b). Lockdown measures have now been eased among several countries following concerns about the economic and other issues including the potential for increased violence, whilst still maintaining an active response should the need arise (Moore, 2020; Shepherd and van der Mark, 2020; Tih, 2020). However, this situation is being actively monitored in case of a spike in prevalence rates.
Medicine shortages are an increasing concern across countries (Acosta et al., 2019) and are a particular issue in Africa where typically up to 94% of its medicines are imported (N Gage Consulting, 2017; Bavier, 2020; Dugmore, 2020), and supply issues can be exacerbated in countries with ongoing conflicts (ALCED, 2020). However, African countries are already taking steps to address concerns with shortages before and during the pandemic including suggesting potential alternatives (Chigome et al., 2019; Medical Brief, 2020b; Modisakeng et al., 2020; Review Online, 2020; Tomlinson, 2020). There are also ongoing programmes to address the quality of medicines across Africa. The potential for substandard and falsified medications is exacerbated when prices appreciably increase and shortages occur following endorsement of potential treatments for COVID-19 in the media (Abena et al., 2020; Haque et al., 2020; Kindzeka, 2020; Knott, 2020; World Health Organisation, 2020e). Government activities are likely to accelerate with the launch of the Lomé initiative placing falsified and substandard medicines on the highest political agenda with ongoing measures to strengthen the legal response to these medicines (WHO, 2020k).
COVID-19 has accelerated discussions on local pharmaceutical production in Africa (GhanaWeb, 2020a) with, for instance, the East African Community States seeking to support local production of essential medical products and supplies. Products include masks, sanitizers and ventilators, to address shortages in the region (EAC, 2020). In addition, several local companies have come forward to produce medical equipment and other products to manage the pandemic, and this will continue (Defy, 2020; Kaine and Nwokik, 2020; Nyaira, 2020). This is in line with the philosophy to develop regional hubs involving several African countries to address issues of economies of scale (Conway et al., 2020).
Given the multiple issues and challenges facing African countries, we believe there is an urgent need to consolidate knowledge of ongoing activities across Africa to address the COVID-19 pandemic and to understand its impact. Similarly, there is a need to evaluate the impact of re-directing activities away from the care of patients in other priority disease areas in Africa towards COVID-19 activities given the likely consequences on increased morbidity and mortality alongside the economic and social impact (Cash and Patel, 2020; Lancet editorial, 2020; Thornton, 2020).
We are aware that several regional financial institutions, including the African Development Bank and the African Export-Import Bank, have announced significant financial support for this purpose (African Development Bank, 2020; Okonjo-Iweala et al., 2020). The commitments of the World Bank and the International Monetary Fund also provide additional mechanisms, including suspending debts, to free resources towards the COVID-19 response (Ataguba, 2020). These measures should help address existing concerns regarding the financial impact of government measures including lockdown measures on the livelihoods of African citizens, with many currently working in the informal sector (Bonnet et al., 2019; Ataguba, 2020; Cash and Patel, 2020).
Containing the spread and impact of COVID-19, including the substantial economic impact, will though require a multipronged approach and co-operation among all key stakeholder groups going forward, including patients, with countries learning from each other (Ataguba, 2020). Ongoing activities include addressing the considerable misinformation about COVID-19 and potential treatments including vaccines and herbal medicines (Anna, 2020; Brennen et al., 2020; Forrest, 2020; Gallagher, 2020; Haque et al, 2020; Larson, 2020; Neil and Campbell, 2020; Newton and Bond, 2020; Nkeck et al., 2020; Serwornoo and Abrokwah, 2020; Smith, 2020; The Guardian, 2020; World Health Organisation, 2020f; Yang, 2020). The current controversies surrounding chloroquine/ hydroxychloroquine is just one example. As a result, there is a recognized need for scientific integrity and credibility when developing and discussing possible treatments for COVID-19 in line with recommendations from the Council for International Organizations for Medical Services (Council for International Organizations of Medical Sciences, 2020; Godman, 2020). This is to ensure future public and physician trust in treatment recommendations, which forms an integral part of effectively dealing with COVID-19 (Pitts, 2019; Abena et al., 2020; Goodman and Borio, 2020; Perry Wilson, 2020; Pitts, 2020; Rubin et al., 2020).
We are aware that early in the pandemic, Africa CDC, as well as WHO Africa and their partners, spearheaded efforts to train and sensitize African governments on the need to effectively counter and reduce the levels of misinformation (Budoo, 2020; Davis, 2020; Media Foundation West Africa, 2020). Their activities included training on risk communication and regular briefings to heads of state as well as relevant sectors of government. Additional efforts have also been provided by groups such as the International Alliance of Patients' Organizations (IAPO), which have developed resource hubs to provide reliable and updated information to mitigate against misinformation and promote preventative activities (International Alliance of Patients' Organizations, 2020).
Education among patients can also help reduce any stigma associated with COVID-19 for recovering patients and their families as well as any mistrust by the people in their governments (Adusei, 2020; AFP-JIJI, 2020; Habersaat et al., 2020; IFRC, UNICEF and WHO, 2020; Lubega and Ekol, 2020; United Nations, 2020b). We know that countries and governments have the potential to learn from the evidence base of HIV-related stigma interventions to help address such issues, as well as previous pandemics as seen with Vietnam (Logie, 2020; United Nations., 2020b; WHO, 2020a). Potential activities among patients and their organizations include active discussions around how stigma affects different communities, reflections on personal biases, and the instigation of institutional support programmes (Logie, 2020; He et al., 2020). This is important as the COVID-19 pandemic has already provoked stigmatisation and discriminatory behaviors against people of certain ethnic backgrounds as well as anyone perceived to have been in contact with or recovered from the virus (AFP-JIJI, 2020; GhanaWeb, 2020b; IFRC, UNICEF and WHO, 2020; ). Having said this, we have seen reasonable knowledge, attitudes and practices towards most aspects of COVID-19 among the public in China, Nepal, Pakistan and Paraguay although still room for improvement (Rios-González, 2020; Hayat et al., 2020; Singh et al., 2020a; Zhong B. L. et al., 2020). Surveys in the UK and US have also shown that participants generally had good knowledge about the main means of transmission and the common symptoms of COVID-19 (Geldsetzer, 2020). In Cameroon, the population is also aware of the disease and preventive measures (Nicholas et al., 2020). Further research is ongoing regarding why some people fail to adhere to suggested preventative measures, and we will be monitoring this (Chan et al., 2020).
Consequently, the objective of this paper is to summarise and consolidate our knowledge of current activities across Africa related to COVID-19 to help provide future guidance to all key stakeholder groups. This includes following up on clinical trial activities across Africa since an early concern was that few clinical trials were being conducted across Africa (Mabuka-Maroa, 2020; Roussi and Maxmen, 2020). This is beginning to change, building on examples in Burkina Faso, Kenya, Nigeria, South Africa and the WHO Solidarity Trial across several African countries (Anna, 2020; Coulibaly, 2020; Olafusi, 2020; WHO, 2020l). By doing so, we believe we can support African countries' efforts to continue to work together to tackle the pandemic, including jointly pursuing loan waivers to help protect against the financial consequences of COVID-19 (Phiri, 2020; President Republic of Kenya, 2020a).
This will be the first paper in this series as more information and findings become available. This builds on a recent systematic review regarding the importance of viral diseases in Africa, and the fact that different approaches will be needed across Africa to tackle COVID-19, depending on current circumstances (Chauhan et al., 2020; Mehtar et al., 2020; Shepherd and van der Mark, 2020).
We adopted a mixed methods approach. This initially involved conducting a narrative review of the published literature as well as papers awaiting publication and internet references known to the co-authors. We did not perform a systematic review. We were aware that some systematic reviews have already been conducted and published in this area including potential treatments despite the lack of data from robust clinical trials (Alqahtani et al., 2020; Castagnoli et al., 2020; Chowdhury et al., 2020; Cortegiani et al., 2020; Das et al., 2020; Ford et al., 2020; Huang et al., 2020; Nussbaumer-Streit et al., 2020; Sarma et al., 2020; Singh et al., 2020b; Vardavas and Nikitara, 2020; Zheng Z. et al., 2020). A number of the publications surrounding COVID-19 are also currently only available in pre-publication form and not peer-reviewed. Alongside this, much of the information regarding ongoing activities across Africa are from internet sources, and it is too early to assess the impact of these, especially as COVID-19 cases appeared later in Africa than in either China or Europe.
We also did not systematically review each paper for its quality using well-known scales such as the Newcastle-Ottawa scale or the Cochrane risk of bias tool as our emphasis was on contextualizing the findings rather than performing a systematic review (Marra et al., 2016; Almeida et al., 2018; da Silva et al., 2018; Ong et al., 2018; Saleem et al., 2019). However, the publications and internet sources were filtered by the co-authors to add robustness to the present paper and its suggestions.
In view of this, and to provide direction for the future, we supplemented information from the literature and internet sources with additional current information from co-authors across Africa. The co-authors include senior level personnel from governments and their advisers, lecturers and researchers from academia, and clinicians, as well as those involved with activities to enhance the rational use of medicine, undertake Health Technology Assessment (HTA), document medicine shortages, and involved with patient organizations from across Africa and wider. The co-authors were asked to provide information on the following themes or topics, where known, in their own country to supplement the ongoing literature:
● Details about the current epidemiology of COVID-19 including CFRs, national responses to date and an assessment of the effectiveness, if known
● The socio-economic impact as well as the impact on healthcare delivery in other priority disease areas including medicine and equipment shortages as well as attendance at clinics. This includes any information on the unintended consequences of COVID-19 in other disease areas if known
● How issues such as medicine shortages are being addressed and the implications for local manufacturing in the future
● Current medicines and other approaches to treating patients with COVID-19 as well as ongoing studies that address issues such as false claims and hopes. In addition, ongoing activities to address falsified and sub-standard medicines
● Key lessons for the future for all key stakeholder groups
The same questions were asked of each co-author, with country-specific replies typically consolidated where there were multiple authors in a country. The information was subsequently consolidated by two of the authors (OO and BG) and checked with each co-author during manuscript preparation to add robustness to the findings and suggestions.
We also documented ongoing technology innovations across Africa, which we believe is important as Africa seeks to become self-sufficient in the management of patients with COVID-19 and beyond.
Documented prevalence and mortality rates will typically be based on WHO date for consistency and reliability as there have been challenges with generating up-to-date data among a number of African countries due to the availability of testing facilities and testing kits, as well as concerns with some testing kits; however, as mentioned, this is now being addressed with the help of the WHO and others (Aljazeera News, 2020b; Burke, 2020; Simpson, 2020; UNICEF, 2020; WHO Regional Office Africa, 2020c).
The African countries chosen reflect a wide range of geographies and population sizes. We did not divide them into low- or middle-income countries as COVID-19 is likely to affect all African countries and they can learn from each other.
Statistical analysis of the different measures and initiatives and their possible impact on the epidemiology, morbidity and mortality rates, has not been undertaken as this is too early given rising prevalence rates across Africa. In addition, our principal aim was to provide a comprehensive analysis of the current situation across Africa, including the potential implications for other infectious and non-infectious disease areas within the African continent, to stimulate ongoing debates regarding potential future activities. This is important across Africa with high prevalence rates for both infectious and non-infectious diseases, We have successfully used this dual approach in previous publications to stimulate debate in important healthcare areas and situations to provide future guidance as countries seek to improve the quality and efficiency of their approaches to medicine use, including during pandemics (Godman et al., 2014a; Godman et al., 2014b; Godman et al., 2015; Ermisch et al., 2016; Bochenek et al., 2017; Ferrario et al., 2017; Moorkens et al., 2017; Godman et al., 2018; Godman et al., 2019; Godman et al., 2020b; Godman et al., 2020c; Godman et al., 2020d; Miljković et al., 2020).
The findings and activities are divided into sections to meet the study objectives. These include documenting the epidemiology among a range of African countries principally based on epidemiology data provided by the WHO. The aforementioned precedes discussing ongoing strategies to limit the spread of COVID-19 as well as their subsequent impact on morbidity and mortality in populations across Africa.
The impact of COVID-19, including the unintended consequences on the healthcare system and patients, along with financial and socioeconomic issues, will be explored before documenting the subsequent impact on increased local production of pharmaceuticals and other supplies as well as any ongoing clinical studies and innovations across Africa aiming at improving future care. Finally, potential ways forward will be debated among all key stakeholder groups based on the experiences of the co-authors to provide future guidance. This includes key issues of shortages, unintended consequences, and misinformation as well as the role of patients and patient organizations in preventative measures and other interventions.
There is considerable variation in the number of recorded cases, deaths and CFRs across Africa following the first reported case on February 14, 2020 (United Nations., 2020b), with some countries yet to record their first deaths due to COVID-19 and some countries recording only a few deaths to date (Table 1), potentially reflecting different approaches and circumstances (Tables 2 and 2A). Table 1A in the Data Sheet gives further details of the epidemiology over time as well as recovered cases where known and documented.
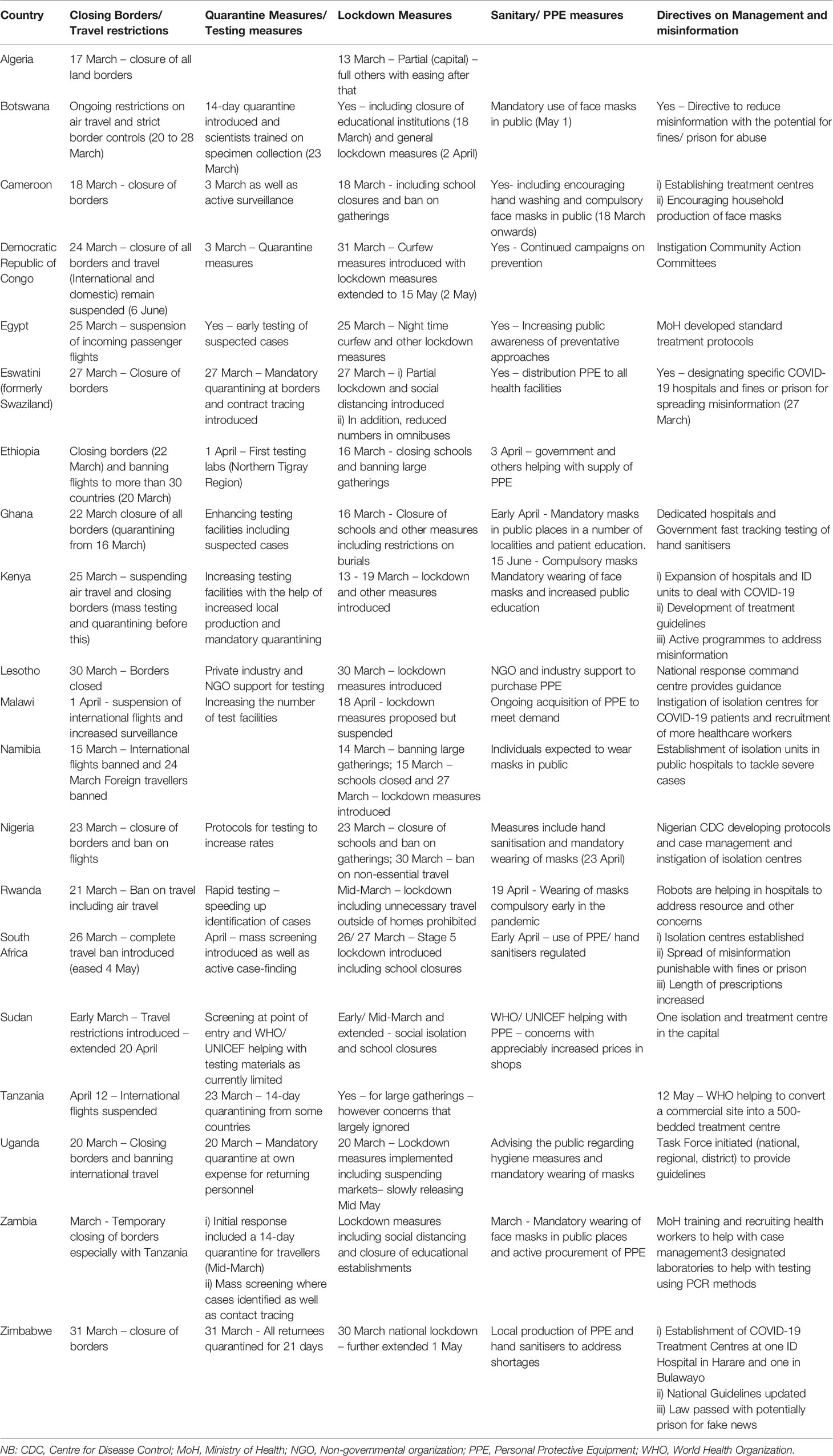
Table 2 Ongoing activities across Africa to help prevent the spread of COVID-19 including dates and examples.
Different activities are ongoing across Africa to try and limit the impact of COVID-19. These are summarised in Table 2, with Table 2A in the Data Sheet giving additional details for those interested. As seen, prevention and treatment approaches remain broadly similar among the African countries, with a number of African countries combining approaches to provide joint guidance and updates on suggested activities, such as the East African Community (EAC Secretariat, 2020). There are concerns though with limited activity in some countries, e.g., Tanzania, as well as fears that if lockdown measures are released too early due to financial and resource issues for citizens and governments these will appreciably enhance future prevalence rates (Schroder et al., 2020).
Measures to limit the spread of COVID-19 are having a considerable impact on other disease areas including both infectious and non-infectious diseases. Table 3 contains details of the considerable healthcare and financial impact of COVID-19 as well as ongoing activities among African countries to address these. We will be examining unintended consequences in more detail in future research projects. Similarly, there are considerable financial and socioeconomic consequences which are also being addressed, with countries having the opportunity to learn from each other.
There are shortages of medicines across Africa as most medicines are imported (Table 3A). We are likely to see local production increasing as part of future strategies to address ongoing shortages as a result of COVID-19, and we will be monitoring this in the future.
Table 3A in the Data Sheet contains details of ongoing shortages across Africa with countries starting to implement robust strategies to help deal with these in the future.
As mentioned, there has been limited clinical trial activity across Africa compared with higher income countries; however, this is beginning to change:
● In Botswana, there are currently no on-going clinical trials on COVID-19; however, the University of Botswana (a government-funded institution) has called for proposals on COVID-19 research, which was open until May 15, 2020.
● Egypt appears to be undertaking several clinical trials with currently 14 registered clinical trials granted expedited approval by review boards utilizing different medicines and treatment modalities (US National Library of Medicine, 2020).
● Currently there are no known clinical trials commissioned in Eswatini with no demonstrable commitment to commissioning COVID-19- related clinical research activities given the current pressure on resources.
● In Ghana, there currently appears to be no clinical trial research activities related to COVID-19. However, some medicinal plants with potential antiviral activity have been identified and submitted to the Centre for Scientific Research into Plant Medicine and Noguchi Memorial Institute for Medical Research for the commencement of studies/screening on their potential therapeutic anti-COVID-19/SARS-CoV-2 activities.
● Kenya is currently involved in WHO clinical trials for three medicines used in combating COVID-19. A vaccine clinical trial is envisaged in the next two or three months at the Kilifi KEMRI/Welcome Trust collaborating research site. The Institutional Review Boards have established electronic systems for protocol submissions and review feedback and expediting the review process (3-4 days for first response) to facilitate implementation.
● Three clinical trials have been registered in Nigeria but currently none have started recruiting (Global Coronavirus COVID-19 Clinical Trial Tracker, 2020). However, Nigeria has been included in the WHO SOLIDARITY trial with five treatment centres participating.
● A number of clinical trials are currently ongoing in South Africa for both pharmaceutical and non-pharmaceutical interventions with the Institutional Review Boards in South Africa having established electronic systems and expediting the review process to facilitate these. This includes the SOLIDARITY WHO trial with the South African research team being led by senior academics and clinicians from eight medical schools (Baleta, 2020) as well as the BCG vaccination trial programme for healthcare workers (NIH ClinicalTrials.gov, 2020a) and the South African Ox1Cov-19 Vaccine VIDA-Trial, the first clinical trial for a vaccine against Covid-19 in South Africa with the first patients enrolled the week of June 23, 2020 (NIH ClinicalTrials.gov, 2020b; Wits University, 2020a).
● Zimbabwe is also involved in the WHO SOLIDARITY Trial.
There are many ongoing innovations across Africa to tackle COVID-19, and these are expected to continue. In Senegal, the Institut Pasteur, with support from the WHO, developed a US$1 COVID-19 Rapid Testing Kit to enable the country to undertake considerable testing with the government currently seeking approval for their kits to be used in other African countries (Kavanagh et al., 2020; LaMarca, 2020; Roberto, 2020). Scientists and industry partners in Ghana have also developed a test for COVID-19, a finger-prick blood test to rapidly detect antibodies, which is seen as beneficial among asymptomatic cases to reduce the spread (Nyavor, 2020).
Students at the Jomo Kenyatta University of Agriculture and Technology in Kenya developed a Mobile app to help with contact tracing, triaging and case management of COVID-19 patients (JKUAT, 2020a), with other students in Kenya also developing and making ventilators to address shortages (JKAUT, 2020b; Kenyatta University, 2020; University of Nairobi, 2020). A multidisciplinary team at Wits University in South Africa used their design and engineering skills to create face shields (Wits University, 2020b). A multi-disciplinary team from Honoris United Universities from across Africa, including doctors, engineers, and students, have developed a prototype for a new non-invasive respirator alongside face shields and splash protection masks, which can be quickly and affordably manufactured via 3D printing to address current shortages (Bissada, 2020).
Scientists in Uganda have also developed hands-free hand sanitisers and rapid testing kits with a team at Makerere University involved in manufacturing low-cost ventilators to bolster the country's capacity in case demand increases (Achan, 2020; Daily Monitor, 2020; School of Public Health Makerere University, 2020).
The Gauteng Department of Health in South Africa has introduced an app (Mpilo) based platform that supports improved service delivery and improved patient experiences in Gauteng Health facilities (Matshediso, 2020). The University of Pretoria in South Africa has also produced an interactive app with real-time data on COVID-19 infections to help with management (Gower, 2020). The governments in Egypt and Ghana have also recently launched apps to help with tracing people who have come into contact with COVID-19 positive patients as well as provide advice on management (El-Sabaa, 2020; Ministry of Communications, Republic of Ghana, 2020).
Scientists in Ghana have also successfully sequenced the genomes of SARS-COV-2 from 15 of the samples obtained from confirmed COVID-19 cases through active collaboration using the Next Generation Sequencing (NGS) Core and High-Performance Computing system (University of Ghana News Release, 2020). Whilst there have been some differences in the strains between countries, all 15 genomes typically resembled (>92% similarity) the original strain isolated from China (University of Ghana News Release, 2020). Scientists from the Nigerian Centre for Disease Control (NCDC) and others from across Nigeria, including from Lagos University Teaching Hospital, have also reported sequencing of the SARS-CoV-2 from the first confirmed case of COVID-19 in Nigeria (Pauloluniyi, 2020).
Tabel 4A (Data Sheet) summarises key lessons learnt among a number of African countries going forward in the management of COVID-19 and other disease areas based on their experiences.
Boxes 1–6 consolidate potential activities that could be undertaken across Africa to improve the future care of patients with COVID-19 building on existing activities (Tables 2 and 2A). However, we need to be mindful of a range of healthcare issues including the unintended consequences on both health and socioeconomic circumstances. This builds on Table 3, as well as Tables 3A and 4A, for individual African countries combined with recommendations for all key stakeholder groups in Africa going forward in the management of both infectious and non-infectious diseases as well as clinical and economic issues surrounding fixed dose combinations (Godman et al., 2019; Godman et al., 2020a; Godman et al., 2020b; Godman et al., 2020c; Godman et al., 2020d).
Box 1. National/ regional governments and authorities.
Leadership and Governance
● Instigation of national/ regional pandemic planning. This includes the need for active surveillance with appropriate personnel and facilities as well as ensuring necessary healthcare workforce and structures including adequate supplies of PPE and other necessary equipment, and communication including all key stakeholder groups with reserved funds for such health emergencies. In addition, a phased approach to easing restrictions when pertinent (Habersaat et al., 2020). Such activities have worked well across countries (Jones, 2020; Wang C. J. et al., 2020)
● Development and implementation of occupational health and safety protocols, policies and legislative frameworks taking cognisance of the risks and mechanisms of COVID-19 infection. Such protocols, policies and legislative frameworks should be consistent with national and international workplace safety policies and guidelines. Effective enforcement and monitoring mechanisms should be put in place
● Planning should take account of the impact of COVID-19 on the mental health of patients and healthcare professionals as well as other priority disease areas and potential ways to address these. This requires a sound understanding of investment/ priority decision making and activities including HTA EBM principles
● Actively plan for misinformation building on the considerable levels of misinformation already seen by end June 2020 (Habersaat et al., 2020)
● Good communication and financial planning are vital to address concerns with any lockdown/ curfew measures especially in countries with high levels of informal sector workers/ high level of workers dependent on a daily wage for their survival
● Lead the development of care guidelines nationally as well as take part in the development of any Pan-African care guidelines. This builds on HTA/ EBM approaches
● Ensure longer term that all healthcare professionals have the necessary training to improve the management of patients with infectious diseases as well as likely co-morbidities especially among African patients. This includes instigating antimicrobial stewardship programmes as well as Infection Prevention Control groups in hospitals where these do not currently exist
● Enhance collaboration between African countries, especially those with shared borders. This builds on ongoing collaborations including the East African Community with their shared plans to tackle COVID-19 (EAC Secretariat, 2020)
● Explore telemedicine and other similar approaches to help with diagnosis of infectious diseases and address unintended consequences especially in patients with chronic NCDs (Africa Health IT News, 2020b; Bonner, 2020; LinksCommunity, 2020; Webster, 2020) as a consequence of any lockdown, alongside investigating the potential of robots for care delivery
● Continue with measures to reduce the extent of falsified and sub-standard medicines within Africa as well as measures to address concerns with misinformation. Alongside this, seek ways to enhance local/ regional production of medicines, PPE and other equipment to reduce reliance on imports
Health Care Workforce (HCW)
● Strengthen health care systems including ambulatory care systems as well as policies and initiatives to improve identification and management of COVID-19, as well as other high priority disease areas (capacity building)
● Instigate practices to ensure that essential health services offered by the private healthcare sector are not compromised
● Seek to address shortages of physicians where applicable including training and utilising of other healthcare professionals. This can include task shifting including a greater role for other professionals such as pharmacists (Box 4). As part of this, develop medium to long term epidemic/pandemic training for healthcare personnel to improve their preparedness and capacities for such health emergencies
● Enhance the professionalism of HCWs including initiatives to reduce inappropriate prescribing of antimicrobials where this occurs (Godman et al., 2020a; Khan et al., 2020)
● Strengthen community systems through capacity building of community owned resources including community extension health workers as well as voluntary healthcare workers as these are typically the first point of contact in communities
● Ensure HCWs continue to have access to PPE as well as additional training (where relevant) in dealing with pandemics as the safety of HCWs and patients is critical during pandemics
● Seek to share basic best practices across countries, including what works well in COVID-19 case management, infection, prevention and control.
Financing/Socioeconomic issues
● As most African currently countries rely on foreign input, governments need to find alternative sources of income in the future through agriculture and technology advances building on current innovations
● Minimize the socioeconomic impact through enhancing national solidarity and prioritization of social cohesion.
● Seek to protect vulnerable populations including the benefits and privileges of low-wage workers as well as address access to healthcare and support for all to reduce the burden that makes vulnerable people less able to follow public health directives
● Make it possible for small-scale business to survive periods of economic downturns occasioned by public health crisis. This can include facilitating the disbursement of interest loans to SMEs as well as reward local companies in the country with tax incentives/guaranteed bank loans to enable them recover post COVID-19
Research Including Unintended Consequences for Both Infectious Diseases (including AMR) and non-infectious diseases
● Promote and fund operational/national research on the impact of COVID-19 on infectious diseases (including AMR) and non-infectious diseases especially the unintended consequences (Table 3). This is particularly important in Africa where national programmes are just starting to address AMR as well as NCDs including CVD, diabetes, and mental health (Mendelson and Matsoso, 2015; Keates et al., 2017; Ghana Ministry of Health, 2018; Godman et al., 2020a; Godman et al., 2020b; Godman et al., 2020c)
● Continue to promote research into potential risk factors for morbidity and mortality among African patients given the differences that can exist between patients in Africa and those in high income countries
● Continue with research programmes aimed at mitigating against infectious diseases (including AMR) and non-infectious diseases across countries to add to the debate about the potential impact of unintended consequences
● Instigate research into new ways to manage patients with both infectious diseases and NCDs where there are constraints on patient access including better use of new technologies including telemedicine and consultations through the internet/ mobile telephones
NB: AMR, Antimicrobial Rsistance; CVD, Coronary Vascular Disease; EBM, Evidence-base medicine; HTA, Health Technology Assessment; NCDs, Non-communicable diseases; PPE, Personal Protective Equipment; SME, Small and Medium size enterprise.
Box 2. Health technology assessment/ evidence based medicine.
Short Term
● Continue reviewing emerging medicines that could be used in the management of COVID-19 to inform and update clinical protocols
● Disseminate findings via Ministry of Health and other websites to address current levels of misinformation
● Continue to undertake research for evidence-based interventions given the current controversies surrounding a number of suggested treatments for COVID-19, and encourage greater collaboration between governments, healthcare professionals and patient organizations researching and disseminating the findings
● Strengthen HTA capabilities especially when Ministries of Health are confronted with different potential interventions to address COVID-19 coupled with limited resources. This builds on existing initiatives across Africa including Ghana, Kenya and South Africa as well as the recent cost-benefit analysis on social distancing in Ghana and ICU versus care in general wards for patients with severe COVID-19 (Ghana Prorities Project, 2020; Hernandez-Villafuerte et al., 2016; Mueller et al., 2017; Hollingworth et al., 2018; Southern African Health Technology Assessment Society (SAHTAS), 2019; SAMRC, 2020)
● As part of this, upgrade research into priority decision making especially given the many competing healthcare needs among patients in Africa including those with infectious and non-infectious diseases as well as co-morbidities
Longer Term
● Seek to invest in personnel and resources to enhance HTA/ EBM capabilities within countries where currently limited personnel and resources to enable greater critique of evidence based alternatives
● Seek to establish HTA collaborations across African countries to avoid duplication building on experiences in Europe (European Observatory, 2016; KCE Report, 2017; Vella Bonanno et al., 2019)
NB: EBM, Evidence-base medicine; HTA, Health Technology Assessment.; ICU, intensive care unit.
Box 3. Physicians (hospital and ambulatory care).
Short Term
● Deployment of higher number of physicians where possible to help deal with the pandemic as well as other priority disease areas. Ensure physicians are motivated emotionally, mentally and financially to help deal with the pandemic especially given the likely impact of the virus on their mental health. Educational interventions and psychological support will be needed to ensure greater understanding of COVID-19 and its implications including better coping strategies. Psychological support could include development of support systems among all stakeholders and the general community.
● Physicians need to be provided with adequate PPE and training to address current fears, with hospitals provided with adequate logistical support (PPE, ventilators, medication, non-consumables)
● Embrace alternative ways of working including devolved responsibilities as well as the use of new technologies that help improve the care of all patients during pandemics
● Introduce greater opportunities for the training and re-training of ambulatory care physicians in the management of patients with COVID-19 and any co-morbidities given the challenges that can exist with differential diagnosis. As part of this, push for the instigation of antimicrobial stewardship programmes as well as IPC groups in hospitals where these do not currently exist
● Work with others to address concerns with misinformation as well as falsified and sub-standard medicines. In addition, concerns with potential shortages of medicines and equipment and alternative approaches
Longer Term
● Building on current experiences and collaborations on the best way to treat patients with COVID-19 and the aftermath including concerns with mental health disorders
● Focus on training of sufficient physicians from non-public health or circulatory medicine specialities to ensure a higher number of staff with transferable skills relevant to a pandemic that can be rapidly re-deployed
● There is an urgent need generally to employ more health personnel to augment current inadequacies across Africa. This includes exploring measures to attain and retain physicians
NB: IPC, Infection, prevention and control; PPE, Personal Protective Equipment.
Box 4. Pharmacists (hospital and ambulatory care).
Short Term
● Seek ways to ensure that medicines, or suitable alternatives, that are deemed helpful to patients with COVID-19 are routinely available coupled with medicines for other priority disease areas
● Work with Government agencies when falsified or sub-standard medicines are suspected to reduce their supply
● In hospitals, seek to ensure that hospital pharmacists are part of COVID-19 treatment teams including ASPs and IPC teams. This means that hospital pharmacist must keep abreast on current treatment research and protocols for COVID-19 and be familiar with EBM techniques given ongoing controversies (Al-Quteimat and Amer, 2020). In addition, should be provided with any necessary PPE including face shields and googles
● Hospital pharmacists should be involved in educating patients/staff on COVID-19 management especially on non-pharmacological and pharmacological interventions
● Where appropriate, pharmacist should be encouraged to prepare cost-effective WHO-recommended hand sanitizers for their facilities
● In the community, pharmacists have a vital role as they are often the first healthcare professional that patients contact regarding respiratory/ influenza diseases especially in countries with high patient co-payments, concerns with access to ambulatory healthcare facilities as well as issues of affordability to pay for a physician and their medicines (Markovic-Pekovic et al., 2017; Mukokinya et al., 2018; Adunlin et al., 2020; Al-Quteimat and Amer, 2020; Godman et al., 2020a). This includes encouraging self care/ hygiene measures including the supplying and wearing of masks and the need for regular hand washing as well as trying to protect patients against stock-outs of pertinent medicines (Al-Quteimat and Amer, 2020; Amariles et al., 2020; Haque et al., 2020; Ung, 2020)
● Community pharmacists can also discuss appropriate treatments including arguing against the need for antibiotics where this is a concern and encouraging appropriate referral where possible (Mukokinya et al., 2018; Amariles et al., 2020; Godman et al., 2020a)
● Community pharmacists and others can also push for extended supply of medicines where appropriate as well as help engage in discussions regarding adherence to medicines using different technologies especially given ongoing concerns with adherence to medicines without regular input from pharmacists and other professionals (Al-Quteimat and Amer, 2020; Kretchy et al., 2020; Zheng S. Q. et al., 2020).
● Pharmacists can also suggest alternative approaches during times of medicine shortages including potential OTC treatments (Cadogan and Hughes, 2020).
● They can also help improve stock controls to reduce potential shortages of key medicines with associated price increases, which is important in LMICs with high patient co-payments (Haque et al., 2020; Godman, 2020).
● Community pharmacists can also be involved in vaccination programmes given current concerns, as well as help administer a vaccine for COVID-19 when available with research suggesting that when pharmacists provide immunizations, they substantially increase the number of vaccinated people in the community (Hedima et al., 2020)
Longer Term
● Increase the training of Pharmacists at both hospital and community levels to be prepared/actively involved in management of COVID-19 patients as well as addressing unintended consequences including the use of technology to address issues with adherence
● Pharmacists should be part of appropriate relevant training and the development of emergency plans and workflows to deal with future pandemics and their consequences (Aruru et al., 2020)
NB: ASPs, Antimicrobial Stewardship Programmes; EBM, Evidence-based medicine; IPC, Infection, Prevention and Control; PPE, Personal protective equipment.
Box 5. Other healthcare professionals in ambulatory and hospital care.
Short Term
● Work with other professionals to identify optimal methods to deal with the care of patients with COVID-19 both in hospitals and in the community
● This includes making sure that healthcare professionals have the necessary PPE and equipment to deal with COVID-19 patients
● Seek to instigate training regarding the proper donning and removal of PPE during routine duties and in the management of suspected/positive COVID-19 cases if not in place
● Be part of ongoing plans to help improve the management of high priority disease areas outside of COVID-19 to make sure these patients are not neglected
● Work with necessary professionals to ensure the mental health of healthcare professionals and patients is not neglected during and post the pandemic. This includes helping to address issues of stigma
Longer Term
● Be part of elaborate plans to improve the management of patients with COVID-19 and other priority disease areas including re-distribution of activities to address shortages with physicians and other HCPs
● Seek to work with universities, companies and other groups to develop in-house/ in-country technologies to treat COVID-19 patients and be less reliant on imports in the future
NB: HCPs, Healthcare Professionals; PPE, Personal protective equipment.
Box 6. Suggested activities among patients/patient organizations.
Short Term
● Mobilize and engage with traditional, cultural, and other leaders who are respected and listened to in their communities to disseminate important health messages including hygiene and social distance measures associated with COVID-19 to help address current low levels of health literacy in a number of African countries. This includes addressing current misconceptions about the importance of using face masks, and how to use them appropriately, as many patients do not appreciate the need as well as helping acknowledge that some people with respiratory problems may have difficulties using masks for long, which needs to be effectively tackled
● Engage with various channels to help reassure COVID-19 patients that they pose no threat to the community after treatment, and should continue with their lives, as well as help address issues of stigma and discrimination against COVID-19 patients when these arise
● Work with government bodies to help address issues of misinformation about vaccines and treatments including misconceptions about vaccines and the consequences (Anna, 2020). In addition, work with all key stakeholder groups to help address the mental health issues that will arise from the current pandemic
● Patients organizations should work with regulatory authorities and professionals generally to strengthen ethical conduct and professionalism post the pandemic including promoting only evidence-based approaches across social and other media given concerns with the level of misinformation during the pandemic (Godman, 2020)
● Recovered COVID-19 patients can be used as ambassadors to sensitise the populace about the reality of the pandemic, and the need to avoid stigmatization
● Social media has proved useful and can provide an efficient means for patients and patient organizations to effectively communicate with their communities. However, this needs to be carefully managed to reduce the level of any misinformation and subsequent adverse consequences. This builds on activities with traditional, cultural, and other leaders
● Empower patients on medication safety and polypharmacy concerns as well as educate patients about self-management generally of their conditions especially patients with chronic NCDs in the absence of routine clinics
● Help explore possible telemedicine approaches to reduce reliance on clinic attendance, which in itself can be problematic outside of the pandemic if this involves extensive travel and waiting times
Longer Term
● Seek to develop patient-level data bases to routinely collect data on patients to help with future planning and care delivery
● Enhance the role of patient organizations within countries where pertinent as they can play a long-term role regarding advocacy and the spreading of information not only on COVID-19 but also other diseases and concerns. Patient organizations also have a key role generally to encourage changes in behaviors that promote good underlying health to support health outcomes and reduce the risk of severe symptomatic responses to a pandemic
A key area will be patients especially in view of their necessary compliance with any lockdown and social distancing activities as well as considerations for the unintended consequences of COVID-19. These include mental health considerations, managing maternal and childbirth challenges, the identification and management of other NCDs as well as other infectious diseases.
HTA will also be a crucial area especially given concerns with the extent of misinformation regarding COVID-19 and the implications. In addition, the need for governments to prioritise their limited resources across disease areas (Hatswell, 2020; Allen and Mirsaeidi, 2020), rather than devoting appreciable personnel and resources to one area to the detriment of others as seen currently with activities regarding COVID-19 (Tables 2, 2A, and 3). However, there are challenges including available personnel and resources as well as typically a greater focus on medicines among HTA units rather than other technologies (Hernandez-Villafuerte et al., 2016; Bijlmakers et al., 2017; MacQuilkan et al., 2018; Fasseeh et al., 2020). This is changing with studies in Ghana evaluating the cost-benefit of moderate social distancing policies (Ghana Prorities Project, 2020) and the cost-effectiveness of different prevention measures (Asamoah et al., 2020) as well as groups in South Africa HTA evaluating the cost-effectiveness of ICU versus care on general wards with patients with severe COVID-19 (SAMRC et al., 2020).
HTA and EBM will also be important in the development of clinical guidelines for Africa considering the costs involved with developing de-novo guidelines. Africa could certainly gain from a Pan-African guideline for the management of COVID-19 as knowledge grows to provide scientifically-based recommendations, similar to initiatives for NCDs (Okwen et al., 2019). Global evidence communities including the BMJ under its Best Practice series are already adopting this approach for knowledge generation, synthesis, and translation to facilitate evidence-based decisions (BMJ Best Practice - Coronavirus disease 2019 (COVID-19), 2020; McMaster University. COVID-END, 2020), and any Pan-African initiatives should build on this. Groups such as IAPO are also important with their resource hubs to provide robust, reliable, and updated information to help improve the care of patients (International Alliance of Patients' Organizations, 2020). In the meantime, we are beginning to see African countries taking steps to reduce the level of misinformation and this is likely to grow (Budoo, 2020; Davis, 2020).
We believe this is the first study to comprehensively document ongoing activities throughout Africa to tackle the health, financial and socioeconomic consequences of COVID-19. This is important given the high prevalence of both infectious and non-infectious diseases in Africa, the high number of people at or below the poverty level compared with other continents and higher income countries, as well as concerns with the lack of personnel, hospital beds and equipment (Murthy et al., 2015; UNAIDS, 2019; WHO, 2019a; World Health Organisation, 2019; Ataguba, 2020; Godman et al., 2020a; Godman et al., 2020b; Houreld et al., 2020; Martinez-Alvarez et al., 2020; Simpson, 2020; WHO, 2020c).
There have been different activities across Africa to prevent the spread of COVID-19 and reduce mortality rates (Tables 2 and 2A). African countries have broadly followed similar multiple approaches in terms of prevention including closing borders and instigating lockdown measures including travel restrictions, social distancing and testing. Closure of borders and quarantining along with other public health measures appear successful in reducing the spread of the virus (Nussbaumer-Streit et al., 2020), and this certainly appears to be the case among a number of the African countries. Encouragingly, to date there have been no or very few reported deaths among some of the African countries (Tables 1 and 1A), mirroring for instance the situation in other LMICs including Vietnam (WHO, 2020a). Encouragingly as well, there have been a number of innovations coming from the African continent to help with identification and management of patients with COVID-19, which includes local production of hygiene equipment as well as low-cost ventilators (Section 3.6). Alongside this, initiatives to enhance the production of medicines in Africa to reduce their reliance on imported medicines and other essential supplies. This bodes well with dealing with future pandemics in Africa. We will continue though to monitor prevalence and mortality rates across Africa as well as potential reasons for the limited mortality up to late June 2020, certainly when compared with a number of European countries and the USA, including potential issues around ethnicity and other factors.
However, extensive lockdown and other measures to help control the spread of the virus have been at a cost including the negative impact on other disease areas as well as financial and socioeconomic consequences (Table 3). This includes an increase in mental health disorders exacerbated by issues of stigma. Table 3 shows clearly the need to strengthen or enhance existing healthcare infrastructures in many countries to respond to such pandemics and indeed promote better population health and underlying lifestyle behaviors. While good health system infrastructure does not guarantee better health outcomes it increases the opportunities for these to happen (Donabedian, 2005).
Groups such as IAPO are important to reduce any stigma associated with COVID-19 (IFRC, UNICEF and WHO, 2020; Lubega and Ekol, 2020). In the process of stigmatisation, people are being labelled, stereotyped, separated, and/or experience loss of status and discrimination because of a potential negative affiliation with the disease. Stigma can drive people to hide their illness to avoid discrimination, which potentially prevents them from promptly seeking help, and could discourage them from adopting healthy behaviors, which is concerning (Thornicroft et al., 2007). This is because such barriers could potentially contribute to more severe health problems, ongoing transmission, and difficulties with controlling infectious diseases. As a result, there are ongoing strategies to address these challenges including a greater role for patient organizations (Kaufman et al., 2020).
There are real concerns though if lockdown policies are eased too early due to financial and socioeconomic pressures (Schroder et al., 2020), and we will be following this up in future research projects. We will also be following up the unintended consequences of COVID-19 on other infectious and non-infectious disease areas as well as vaccination programmes. In the meantime, Boxes 1–6 provide direction to African countries going forward as they start to ease their lockdown restrictions and address the unintended consequences of the pandemic.
We are aware that we have not undertaken a systematic review. This is because, as mentioned, a number of quoted papers have not been formally peer-reviewed and a great deal of information regarding country activities is currently only available on the internet. In addition, cases of COVID-19 started later in Africa than in China and Europe, and it is too early to formally assess the impact of polices. A number of clinical trials regarding possible treatments for COVID-19 have also only recently started.
However, we believe the strength of our paper lies in its comprehensive approach including ongoing and planned activities from across Africa and next steps from senior level personnel, which we will be building upon as more data becomes available. This includes activities against COVID-19 and future activities to re-balance the care of patients with other infectious diseases as well as NCDs.
There have been multiple activities across Africa to try and reduce the spread of COVID-19 with its subsequent impact on morbidity and mortality with the help of international and national groups including the WHO and African CDC. This is despite concerns with available resources, personnel and equipment compared with higher income countries. To date, mortality rates appear appreciably lower than seen in a number of European countries and the USA possibly due to early lockdown and other measures including early closure of borders and quarantining of returning travellers, which is encouraging given initial concerns in Africa. However, infection rates continue to rise which is a concern especially as lockdown measures are being eased in a number of African countries. Encouragingly, multiple activities were typically introduced early across Africa building on the experiences with other infectious diseases, with countries continuing to learn from each other. However, there are a number of unintended consequences which are likely to result in increased morbidity and mortality of other infectious diseases and NCDs. Activities are ongoing to try and reduce the impact, and we will be monitoring these in the future.
Olayinka O. Ogunleye, orcid.org/0000-0002-8921-1909
Debjani Mueller, orcid.org/0000-0001-7796-982X
Nenad Miljkovic, orcid.org/0000-0003-1282-3883
Julius C. Mwita, orcid.org/0000-0002-5947-3684
Godfrey Mutashambara Rwegerera, orcid.org/0000-0002-5896-6065
Bene D Anand Paramadhas, orcid.org/0000-0002-8204-1417
Mohamed Hussein, orcid.org/0000-0003-0349-7262
Wafaa M. Rashed, orcid.org/0000-0001-7531-2840
Loveline Niba, orcid.org/0000-0002-5938-4913
Melaine Nsaikila, orcid.org/0000-0003-2335-3768
Adefolarin A. Amu, orcid.org/0000-0003-3212-2283
Daniel Afriyie, orcid.org/0000-0001-8859-3565
Seth K. Amponsah, orcid.org/0000-0001-7411-0972
Israel Sefah, orcid.org/0000-0001-6963-0519
Tebello Violet Sarele, orcid.org/0000-0002-5874-6599
Refeletse Keabetsoe Mafisa, orcid.org/0000-0001-9713-466X
Felix Khuluza, orcid.org/0000-0002-8334-0160
Dan Kibuule, orcid.org/0000-0002-6908-2177
Francis Kalemeera, orcid.org/0000-0002-4320-5087
Mwangana Mubita, orcid.org/0000-0002-8732-8644
Tshegofatso Maimela, orcid.org/0000-0002-8554-1329
Joseph Fadare, orcid.org/0000-0002-5641-1402
Johannes Hugo, orcid.org/0000-0002-9406-8801
Ibrahim Chikowe, orcid.org/0000-0002-8231-9140
Johanna C. Meyer, orcid.org/0000-0003-0462-5713
Enos M. Rampamba, orcid.org/0000-0002-3492-9104
Abubakr Alfadl, orcid.org/0000-0002-3014-1408
Elfatih M. Malik, orcid.org/0000-0002-8071-8092
Ombeva Malande, orcid.org/0000-0002-1840-7402
Aubrey Kalungia, orcid.org/0000-0003-2554-1236
Chiluba Mwila, orcid.org/0000-0003-0160-1222
Ioana D. Olaru, orcid.org/0000-0003-3392-9257
Trust Zaranyika, orcid.org/0000-0003-4363-7709
Blessmore V Chaibva, orcid.org/0000-0001-7858-3814
Nyasha Masuka, orcid.org/0000-0003-4653-8626
Corrado Barbui, orcid.org/0000-0003-1073-9282
Ruaraidh Hill, orcid.org/0000-0002-2801-0505
Tomasz Bochenek, orcid.org/0000-0001-9915-7267
Amanj Kurdi, orcid.org/0000-0001-5036-1988
Stephen Campbell, orcid.org/0000-0002-2328-4136
Thuy Nguyen Thi Phuong, orcid.org/0000-0001-7939-5276
Antony P Martin, orcid.org/0000-0003-4383-6038
Brian Godman, orcid.org/0000-0001-6539-6972
OOO, DB, JF, and BG developed the concept of the paper and undertook the initial literature review. OOO, JF, JMe, ACK, and BG developed the draft questionnaire. All authors subsequently contributed to the development of the paper including country activities as well as critiqued subsequent drafts before submission.
AM is employed by HCD Economics.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest. However, a number of them are employed by national or regional governments in Ministries of Health or are advisers to them.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fphar.2020.01205/full#supplementary-material
Abbas, K., Procter, S. R., van Zandvoort, K., Clark, A., Funk, S., Mengistu, T., et al (2020). Routine childhood immunisation during the COVID-19 pandemic in Africa: a benefit-risk analysis of health benefits versus excess risk of SARS-CoV-2 infection. Lancet Glob. Health (EPrint).
Abdool Karim, S. S. (2020). The South African Response to the Pandemic. N Engl. J. Med. 382 (24), e95.
Abena, P. M., Decloedt, E. H., Bottieau, E., Suleman, F., Adejumo, P., Sam-Agudu, N. A., et al. (2020). Chloroquine and Hydroxychloroquine for the Prevention or Treatment of COVID-19 in Africa: Caution for Inappropriate Off-label Use in Healthcare Settings. Am. J. Trop. Med. Hyg. 102 (6), 1184–1188.
Achan, J. (2020). Dr. Wayengera: The man behind Uganda's COVID-19 testing kits. Available at: https://www.newvision.co.ug/new_vision/news/1518668/dr-misaki-wayengera-uganda-covid-19-test-kits.
Achwoka, D., Waruru, A., Chen, T. H., Masamaro, K., Ngugi, E., Kimani, M., et al. (2019). Noncommunicable disease burden among HIV patients in care: a national retrospective longitudinal analysis of HIV-treatment outcomes in Kenya, 2003-2013. BMC Public Health 19 (1), 372.
Acosta, A., Vanegas, E. P., Rovira, J., Godman, B., Bochenek, T. (2019). Medicine Shortages: Gaps Between Countries and Global Perspectives. Front. Pharmacol. 10 (763).
Adow, M. (2020). COVID-19 adds to DR Congo's multiple health crises - The healthcare system in one of the world's poorest countries is struggling to treat cholera, measles, ebola - and now coronavirus. Available at: https://www.aljazeera.com/news/2020/04/covid-19-adds-dr-congos-multiple-health-crises-200413180551574.html
Adunlin, G., Murphy, P. Z., Manis, M. (2020). COVID-19: How Can Rural Community Pharmacies Respond to the Outbreak? J. Rural Health.
AFP-JIJI (2020). Coronavirus stigma weighs heavily in sub-Saharan Africa. Available at: https://www.japantimes.co.jp/news/2020/05/20/world/social-issues-world/virus-stigma-sub-saharan-africa/#.XsYjk2hKjIU.
Africa CDC (2020). Coronavirus Disease 2019 (COVID-19). Available at: https://africacdc.org/covid-19/.
Africa Health IT News (2020a). Minet, clinic launch telemedicine service in Kenya. Available at: http://africahealthitnews.com/minet-clinic-launch-telemedicine-service-in-kenya/.
Africa Health IT News (2020b). Telemedicine Technology deplore in Kenya To Enhance Fight Against Covid-19. Available at: http://africahealthitnews.com/telemedicine-technology-deplore-in-kenya-d-to-enhance-fight-against-covid-19/.
Africa News Agency (2020). Malawi public transport operators raise fares to offset restrictions. Available at: https://www.iol.co.za/news/africa/malawi-public-transport-operators-raise-fares-to-offset-restrictions-45983229.
Africa News (2020a). HIV-positive people in SA skipping treatment over Covid-19 fears. Available at: https://www.africannewsagency.com/news-politics/HIV-positive-people-in-SA-skipping-treatment-over-Covid-19-fears-24770911.
African Development Bank (2020). President Adesina discusses the immediate and long-term impact of COVID-19 in Africa. Available at: https://www.afdb.org/en/news-and-events/multimedia/video/president-adesina-discusses-immediate-and-long-term-impact-covid-19-africa-35755.
Africa News (2020b). Malawi coronavirus: health workers protest over risk allowance. Available at: https://www.africanews.com/2020/04/21/malawi-coronavirus-health-workers-protest-over-risk-allowance//.
Afriyie, D. K., Sefah, I. A., Sneddon, J., Malcom, W., McKinney, R., Cooper, L., et al. (2020). Antimicrobial Point Prevalence Surveys in two Ghanaian hospitals: opportunities for antimicrobial stewardship. JAC Antimicrob. Resist. 1–9.
Agbobli, S. (2020). ICGC donates GHC 100K towards COVID-19 trust fund. Available at: https://www.theghanareport.com/icgc-donates-gh%E2%82%B5100k-towards-covid-19-trust-fund/.
Agence de Presse Africaine (2020). Ghana Chamber of Mines donates $2m to Covid-19-Trust Fund. Available at: http://apanews.net/en/news/ghana-chamber-of-mines-donates-2m-to-covid-19-trust-fund.
ALCED. (2020). Time Period:02/05/2019-02/05/2020. Available at: https://acleddata.com/dashboard/#/dashboard.
Aljazeera News (2020a). Africa coronavirus cases could hit 10 million in six months: WHO COVID-19 cases on the continent may shoot up from thousands to millions if models are accurate, UN health agency says. Available at: https://www.aljazeera.com/news/2020/04/africa-coronavirus-cases-hit-10-million-months-200417055006127.html.
Aljazeera News (2020b). Tanzania president questions coronavirus kits after animal test - President Magufuli says tests were found to be faulty after goat, sheep and pawpaw samples test positive for COVID-19. Available at: https://www.aljazeera.com/news/2020/05/tanzania-president-questions-coronavirus-kits-animal-test-200503174100809.html.
Aljazeera News (2020c). Kenya floods kill 194 people, displace tens of thousands - Government says 100,000 people displaced following torrential rain in the western part of the country. Available at: https://www.aljazeera.com/news/2020/05/kenya-floods-kill-194-people-displace-tens-thousands-200506133348867.html.
Aljazeera (2020). All you need to know about PPE. Available at: https://www.aljazeera.com/news/2020/04/ppes-important-200419071536635.html.
All Africa (2020). Kenya: Denmark Gives Kenya Sh320m to Boost COVID-19 Fund. Available at: https://allafrica.com/stories/202004050111.html.
Allen, M. B., Mirsaeidi, M. (2020). Health and Economy in COVID-19 Era: A Plan for Reconstituting Long-Term Economic Security. Front. Public Health 8 (235), 1–3.
Almeida, P., Silva, T. B. C., de Assis Acurcio, F., Guerra Junior, A. A., Araujo, V. E., Diniz, L. M., et al. (2018). Quality of Life of Patients with Type 1 Diabetes Mellitus Using Insulin Analog Glargine Compared with NPH Insulin: A Systematic Review and Policy Implications. Patient 11 (4), 377–389.
Alqahtani, J. S., Oyelade, T., Aldhahir, A. M., Alghamdi, S. M., Almehmadi, M., Alqahtani, A. S., et al. (2020). Prevalence, Severity and Mortality associated with COPD and Smoking in patients with COVID-19: A Rapid Systematic Review and Meta-Analysis. PLoS One 15 (5), 1–13.
Al-Quteimat, O. M., Amer, A. M. (2020). SARS-CoV-2 outbreak: How can pharmacists help? Res. Soc. Adm. Pharm.
Amariles, P., Ledezma-Morales, M., Salazar-Ospina, A., Hincapié-García, J. A. (2020). How to link patients with suspicious COVID-19 to health system from the community pharmacies? A route proposal. Res. Soc. Adm. Pharm.
Amegah, A. K. (2018). Tackling the Growing Burden of Cardiovascular Diseases in Sub-Saharan Africa. Circulation 138 (22), 2449–2451.
Anand Paramadhas, B. D., Tiroyakgosi, C., Mpinda-Joseph, P., Morokotso, M., Matome, M., Sinkala, F., et al. (2019). Point prevalence study of antimicrobial use among hospitals across Botswana; findings and implications. Expert Rev. Anti-Infe. Ther. 17 (7), 535–546.
Andreakos, E., Tsiodras, S. (2020). COVID-19: lambda interferon against viral load and hyperinflammation. EMBO Mol. Med. 12 (e12465), 1–4.
Ang, L., Lee, H. W., Choi, J. Y., Zhang, J., Soo Lee, M. (2020). Herbal medicine and pattern identification for treating COVID-19: a rapid review of guidelines. Integr. Med. Res. 9 (2), 100407.
Anna, C. (2020). Protest vs. Africa's 1st COVID-19 vaccine trial shows fears. Available at: https://news.yahoo.com/protest-vs-africas-1st-covid-102207018.html.
Arhinful, E. (2020). Pay attention to Meningitis outbreak in Upper West Region- Parliament directs Health Ministry. Available at: https://citinewsroom.com/2020/04/pay-attention-to-meningitis-outbreak-in-upper-west-region-parliament-directs-health-ministry/.
Aruru, M., Truong, H. A., Clark, S. (2020). Pharmacy Emergency Preparedness and Response (PEPR): a proposed framework for expanding pharmacy professionals' roles and contributions to emergency preparedness and response during the COVID-19 pandemic and beyond. Res. Soc. Adm. Pharm.
Asamoah, A. (2020). Methodist Church donated GHC 100,000 towards coronavirus fight. Available at: https://www.theghanareport.com/methodist-church-donates-ghc100000-towards-coronavirus-fight/.
Asamoah, J. K. K., Owusu, M. A., Jin, Z., Oduro, F. T., Abidemi, A., Gyasi, E. O., et al. (2020). Global stability and cost-effectiveness analysis of COVID-19 considering the impact of the environment: using data from Ghana. Chaos Solitions Fractals 140, 110103.
Ashly, J. (2020). Is Tanzania covering up the real number of coronavirus deaths? Suspicion over official COVID-19 numbers grows as critics accuse gov't of of failing to inform public on true extent. Available at: https://www.aljazeera.com/news/2020/05/tanzania-covering-real-number-coronavirus-deaths-200511054304751.html.
Associated Press. (2020). Refugees Protest Under Coronavirus Lockdown in Rwanda. 17 April 2020. Available at: https://www.voanews.com/covid-19-pandemic/refugees-protest-under-coronavirus-lockdown-rwanda.
Ataguba, J. E. (2020). COVID-19 Pandemic, a War to be Won: Understanding its Economic Implications for Africa. Appl. Health Econ. Health Policy 18 (3), 325–328.
Athumani, H. (2020). Ugandan HIV-Positive Volunteer Goes Distance to Deliver ARVs. Available at: https://www.voanews.com/covid-19-pandemic/ugandan-hiv-positive-volunteer-goes-distance-deliver-arvs.
Auta, A., Hadi, M. A., Oga, E., Adewuyi, E. O., Abdu-Aguye, S. N., Adeloye, D., et al. (2019). Global access to antibiotics without prescription in community pharmacies: A systematic review and meta-analysis. J. Infection 78 (1), 8–18.
Bae, S., Kim, M. C., Kim, J. Y., Cha, H. H., Lim, J. S., Jung, J., et al. (2020). Notice of Retraction: Effectiveness of Surgical and Cotton Masks in Blocking SARS-CoV-2. Ann. Internal Med. 173 (1), 79.
Baleta, A. (2020). COVID-19: SA to start enrolling patients in landmark WHO trial. Available at: https://www.spotlightnsp.co.za/2020/04/01/covid-19-sa-to-start-enrolling-patients-in-landmark-who-trial/
Bambra, C., Riordan, R., Ford, J., Matthews, F. (2020). The COVID-19 pandemic and health inequalities. J. Epidemiol. Community Health, jech-2020–214401.
Basu, S. (2020). Non-communicable disease management in vulnerable patients during Covid-19. Indian J. Med. Ethics V (2), 103–105.
Bates, I., John, C., Seegobin, P., Bruno, A. (2018). An analysis of the global pharmacy workforce capacity trends from 2006 to 2012. Hum. Resour. Health 16 (1), 3.
Bavier, J. (2020). At least 300,000 Africans expected to die in pandemic: U.N. agency. Available at: https://www.reuters.com/article/us-health-coronavirus-africa-un/at-least-300000-africans-expected-to-die-in-pandemic-u-n-agency-idUSKBN21Z1LW.
Beigel, J. H., Tomashek, K. M., Dodd, L. E., Mehta, A. K., Zingman, B. S., Kalil, A. C., et al. (2020). Remdesivir for the Treatment of Covid-19 - Preliminary Report. N Engl. J. Med.
Bijlmakers, L., Mueller, D., Kahveci, R., Chen, Y., van der Wilt, G. J. (2017). Integrate-HTA: A Low- And Middle-Income Country Perspective. Int. J. Technol. Assess. Health Care 33 (5), 599–604.
Bissada, A.-M. (2020). Coronavirus: 3D print of ventilators, easy and cheap to produce says lead researcher. Available at: https://www.theafricareport.com/28212/coronavirus-3d-print-of-ventilators-easy-and-cheap-to-produce-says-lead-researcher/.
Blanco, J. L., Ambrosioni, J., Garcia, F., Martinez, E., Soriano, A., Mallolas, J., et al. (2020). COVID-19 in patients with HIV: clinical case series. Lancet HIV 7 (5), e314–e316
Bloch, E. M., Shoham, S., Casadevall, A., Sachais, B. S., Shaz, B., Winters, J. L., et al. (2020). Deployment of convalescent plasma for the prevention and treatment of COVID-19. J. Clin. Invest.
BMJ Best Practice - Coronavirus disease 2019 (COVID-19). (2020). 7 May 2020. https://bestpractice.bmj.com/topics/en-gb/3000168/pdf/3000168/Coronavirus%20disease%202019%20%28COVID-19%29.pdf.
Bochenek, T., Abilova, V., Alkan, A., Asanin, B., de Miguel Beriain, I., Besovic, Z., et al. (2017). Systemic Measures and Legislative and Organizational Frameworks Aimed at Preventing or Mitigating Drug Shortages in 28 European and Western Asian Countries. Front. Pharmacol. 8, (942), 1–24.
Bode, B., Garrett, V., Messler, J., McFarland, R., Crowe, J., Booth, R., et al. (2020). Glycemic Characteristics and Clinical Outcomes of COVID-19 Patients Hospitalized in the United States. J. Diabetes Sci. Technol. 14 (4), 813–821
Bokpe, S. (2020). Watch out for counterfeit chloroquine on the market-FDA warns. Available at: https://www.theghanareport.com/fda/.
Bonner, L. (2020). Kenya Opens First Telemedicine Center For Covid-19 Detection. Available at: https://www.axisimagingnews.com/news/kenya-opens-first-telemedicine-center-for-covid-19-detection.
Bonnet, F., Vanek, J., Chen, M. (2019). Women and men in the informal economy: a statistical picture. Available at: https://www.ilo.org/wcmsp5/groups/public/—ed_protect/—protrav/—travail/documents/publication/wcms_711798.pdf.
Borba, M. G. S., Almeida Val, F. F., Sampaio, V. S., Alexandre, M. A. A., Melo, G. C., Brito, M., et al. (2020). Chloroquine diphosphate in two different dosages as adjunctive therapy of hospitalized patients with severe respiratory syndrome in the context of coronavirus (SARS-CoV-2) infection: Preliminary safety results of a randomized, double-blinded, phase IIb clinical trial (CloroCovid-19 Study). MedRxiv preprint. Available at: https://www.medrxiv.org/content/10.1101/2020.04.07.20056424v2.full.pdf. doi: 10.1101/2020.04.07.20056424
Boulware, D. R., Pullen, M. F., Bangdiwala, A. S., Pastick, K. A., Lofgren, S. M., Okafor, E. C., et al. (2020). A Randomized Trial of Hydroxychloroquine as Postexposure Prophylaxis for Covid-19. N Engl. J. Med. 383 (6), 517–525
Brennen, S., Simon, F., Howard, P. N., Nielsen, R. K. (2020). Types, sources, and claims of COVID-19 misinformation. Available at: https://reutersinstitute.politics.ox.ac.uk/types-sources-and-claims-covid-19-misinformation.
Brooks, S. K., Webster, R. K., Smith, L. E., Woodland, L., Wessely, S., Greenberg, N., et al. (2020). The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet 395 (10227), 912–920.
Bruton, B., Edwards, N. (2020). Barriers to mass testing for COVID-19 in Africa. Available at: https://www.atlanticcouncil.org/blogs/africasource/barriers-to-mass-testing-for-covid-19-in-africa/.
Budoo, A. (2020). In Africa, government attempts to fight misinformation are also limiting freedom of expression. Available at: https://www.niemanlab.org/2020/05/in-africa-government-attempts-to-fight-misinformation-are-also-limiting-freedom-of-expression/.
Burke, J. (2020). It's just beginning here': Africa turns to testing as pandemic grips the continent. Available at: https://www.msn.com/en-gb/news/world/its-just-beginning-here-africa-turns-to-testing-as-pandemic-grips-the-continent/ar-BB13de1l?ocid=spartandhp.
Cadogan, C. A., Hughes, C. M. (2020). On the frontline against COVID-19: Community pharmacists' contribution during a public health crisis. Res. Soc. Adm. Pharm.
Campbell, A. M. (2020). An increasing risk of family violence during the Covid-19 pandemic: Strengthening community collaborations to save lives. Forensic Sci. Int.: Rep. 2100089.
Cao, B., Wang, Y., Wen, D., Liu, W., Wang, J., Fan, G., et al. (2020). A Trial of Lopinavir-Ritonavir in Adults Hospitalized with Severe Covid-19. N Engl. J. Med. 382 (19), 1787–1799.
Cash, R., Patel, V. (2020). The art of medicine - Has COVID-19 subverted global health? Lancet 395, 1687–1688.
Cassini, A., Hogberg, L. D., Plachouras, D., Quattrocchi, A., Hoxha, A., Simonsen, G. S., et al. (2019). Attributable deaths and disability-adjusted life-years caused by infections with antibiotic-resistant bacteria in the EU and the European Economic Area in 2015: a population-level modelling analysis. Lancet Infect. Dis. 19 (1), 56–66.
Castagnoli, R., Votto, M., Licari, A., Brambilla, I., Bruno, R., Perlini, S., et al. (2020). Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) Infection in Children and Adolescents: A Systematic Review. JAMA Pediatr.
Centre for Disease Prevention and Control (2020). People Who Are at Higher Risk for Severe Illness. Available at: https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-at-higher-risk.html?CDC_AA_refVal=https%3A%2F%2Fwww.cdc.gov%2Fcoronavirus%2F2019-ncov%2Fspecific-groups%2Fpeople-at-higher-risk.html.
CDC COVID-19 Response Team (2020). Preliminary Estimates of the Prevalence of Selected Underlying Health Conditions Among Patients with Coronavirus Disease 2019 - United States, February 12-March 28, 2020. Morbid. Mortal. Wkly. Rep. 69 (13), 382–386.
CGTN Africa (2020). Uganda urges public on HIV/AIDS spread amid COVID-19 pandemic. Available at: https://africa.cgtn.com/2020/05/06/uganda-urges-public-on-hiv-aids-spread-amid-covid-19-pandemic/.
Chaiyachati, K. H., Ogbuoji, O., Price, M., Suthar, A. B., Negussie, E. K., Bärnighausen, T. (2014). Interventions to improve adherence to antiretroviral therapy: a rapid systematic review. AIDS 28 (Suppl 2), S187–S204.
Chan, D. K. C., Zhang, C. Q., Josefsson, K. W. (2020). Why People Failed to Adhere to COVID-19 Preventive Behaviors? Perspectives from an Integrated Behavior Change Model. Infection Control Hosp. Epidemiol., 1–6.
Chandan, J. S., Taylor, J., Bradbury-Jones, C., Nirantharakumar, K., Kane, E., Bandyopadhyay, S. (2020). COVID-19: a public health approach to manage domestic violence is needed. Lancet Public Health. 5 (6), e309
Chang, A. Y., Gómez-Olivé, F. X., Manne-Goehler, J., Wade, A. N., Tollman, S., Gaziano, T. A., et al. (2019). Multimorbidity and care for hypertension, diabetes and HIV among older adults in rural South Africa. Bull. World Health Organ 97 (1), 10–23.
Channnel News Asia. (2020). Malaysia still using hydroxychloroquine to treat COVID-19 patients; health ministry monitoring side effects. 26 May 2020. Available at: https://www.channelnewsasia.com/news/asia/covid-19-malaysia-hydroxychloroquine-still-using-treatment-12771770.
Chauhan, R. P., Dessie, Z. G., Noreddin, A., El Zowalaty, M. E. (2020). Systematic Review of Important Viral Diseases in Africa in Light of the 'One Health' Concept. Pathog. 9 (4), 1–83.
Chiang, C. Y., El Sony, A. (2020). Tackling the threat of COVID-19 in Africa: an urgent need for practical planning. Int. J. Tuberculosis Lung Dis. 24 (5), 541–542.
Chigome, A. K., Matlala, M., Godman, B., Meyer, J. C. (2019). Availability and Use of Therapeutic Interchange Policies in Managing Antimicrobial Shortages among South African Public Sector Hospitals; Findings and Implications. Antibiotics 9 (1), 1–11.
Chilinda, W. (2020). Government To Recruit 8,000 Health Work In 2020. Available at: https://www.znbc.co.zm/news/government-to-recruit-8000-health-work-in-2020/.
Chowdhury, M. S., Rathod, J., Gernsheimer, J. (2020). A Rapid Systematic Review of Clinical Trials Utilizing Chloroquine and Hydroxychloroquine as a Treatment for COVID-19. Acad. Emergency Med. 27 (6), 493–504.
Clinical Trials Arena (2020). Genentech's arthritis drug tocilizumab shows promise in Covid-19 trial. Available at: https://www.clinicaltrialsarena.com/news/french-early-trial-tocilizumab-covid-19/.
Cohen, I. G., Gostin, L. O., Weitzner, D. J. (2020). Digital Smartphone Tracking for COVID-19: Public Health and Civil Liberties in Tension. JAMA.
Conway, M., Holt, T., Sabow, A., Sun, I. Y. (2020). Should sub-Saharan Africa make its own drugs? Available at: https://www.mckinsey.com/industries/public-sector/our-insights/should-sub-saharan-africa-make-its-own-drugs
Cortegiani, A., Ingoglia, G., Ippolito, M., Giarratano, A., Einav, S. (2020). A systematic review on the efficacy and safety of chloroquine for the treatment of COVID-19. J. Crit. Care 57, 279–283.
Coulibaly, N. (2020). To fight coronavirus, Burkina Faso is tempted by chloroquine. Available at: https://www.theafricareport.com/25416/to-fight-coronavirus-burkina-faso-is-tempted-by-chloroquine/
Council for International Organizations of Medical Sciences (2020). Medicines assessment during public health emergencies needs good science, best practices and proper communication. Available at: https://cioms.ch/wp-content/uploads/2020/06/CIOMS_WGXII_Statement.pdf.
Courtemanche, C., Garuccio, J., Le, A., Pinkston, J., Yelowitz, A. (2020). Strong Social Distancing Measures In The United States Reduced The COVID-19 Growth Rate. Health Affairs.
Craven, M., Mysore, M., Singhal, S., Wilson, M. (2020). COVID-19: Briefing note, April 13, 2020 - Our latest perspectives on the coronavirus pandemic. Available at: https://www.mckinsey.com/business-functions/risk/our-insights/covid-19-implications-for-business
Cullen, W., Gulati, G., Kelly, B. D. (2020). Mental health in the COVID-19 pandemic. QJM Monthly J. Assoc. Phys. 113 (5), 311–312.
Cunningham, A. C., Goh, H. P., Koh, D. (2020). Treatment of COVID-19: old tricks for new challenges. Crit. Care 24 (1), 91.
da Silva, W. C., de Araujo, V. E., Lima, E., Dos Santos, J. B. R., Silva, M., Almeida, P., et al. (2018). Comparative Effectiveness and Safety of Monoclonal Antibodies (Bevacizumab, Cetuximab, and Panitumumab) in Combination with Chemotherapy for Metastatic Colorectal Cancer: A Systematic Review and Meta-Analysis. BioDrugs 32 (6), 585–606.
Dabanga (2020). OCHA Sudan: Medical supplies may be affected by Covid-19 measures. Available at: https://www.dabangasudan.org/en/relief-news/article/ocha-sudan-medical-supplies-may-be-affected-by-covid-19-measures.
Daily Monitor (2020). Uganda scientists develop devices to fight Covid-19. Available at: https://www.monitor.co.ug/News/National/Uganda-scientists-develop-devices-to-fight-Covid19/688334-5530170-11h0vedz/index.html.
Das, S., Bhowmick, S., Tiwari, S., Sen, S. (2020). An Updated Systematic Review of the Therapeutic Role of Hydroxychloroquine in Coronavirus Disease-19 (COVID-19). Clin. Drug Invest. 40 (7), 591–601.
Davis, R. (2020). Viral outbreak: Fake news spreads in SA in tandem with Covid-19. Available at: https://www.dailymaverick.co.za/article/2020-03-31-viral-outbreak-fake-news-spreads-in-sa-in-tandem-with-covid-19/.
Defy (2020). Doing Our Part. Available at: https://www.defy.co.za/doing-our-part/.
Di Caro, B. (2020). COVID-19 in Africa: insights from our 30 April WHO media briefing. Available at: https://www.weforum.org/agenda/2020/04/covid-19-in-africa-insights-from-our-30-april-who-media-briefing/.
Di Lorenzo, G., Di Trolio, R. (2020). Coronavirus Disease (COVID-19) in Italy: Analysis of Risk Factors and Proposed Remedial Measures. Front. Med. 7 (140), 1–4.
Dietz, W., Santos-Burgoa, C. (2020). Obesity and its Implications for COVID-19 Mortality. Obesity 28 (6), 1005.
Docherty, A. B., Harrison, E. M., Green, C. A., Hardwick, H. E., Pius, R., Norman, L., et al. (2020). Features of 20 133 UK patients in hospital with covid-19 using the ISARIC WHO Clinical Characterisation Protocol: prospective observational cohort study. BMJ 369, m1985. doi: 10.1136/bmj.m1985
Du, R. H., Liang, L. R., Yang, C. Q., Wang, W., Cao, T. Z., Li, M., et al. (2020). Predictors of Mortality for Patients with COVID-19 Pneumonia Caused by SARS-CoV-2: A Prospective Cohort Study. Eur. Respir. J. 55 (5), 2000524
Ducomble, T., Gignoux, E. (2020). Learning from a massive epidemic: measles in DRC. Lancet Infect. Dis. 20 (5), 542.
Dugmore, H. (2020). Covid-19 leaves SA at the mercy of overseas drug exporters. Available at: https://mg.co.za/article/2020-03-25-covid-19-leaves-sa-at-the-mercy-of-overseas-drug-exporters/.
Dyer, O. (2020). Covid-19: Africa records over 10 000 cases as lockdowns take hold. BMJ (Clin. Res. Ed.) 369, m1439.
EAC Secretariat (2020). East African Community COVID-19 Response Plan. Available at: https://www.eac.int/coronavirus.
EAC (2020). EAC Partner States directed to support local production of essential medical products and supplies to combat COVID-19 in the region. Available at: https://www.eac.int/press-releases/147-health/1724-eac-partner-state-directed-to-support-local-prodcution-of-essential-medical-products-and-suupliees-to-combat-covid-19-in-the-region.
East African (2020). Uganda endorses anti-malaria drug under clinical trial to cure Covid-19. Available at: https://www.monitor.co.ug/News/National/Uganda-endorses-anti-malaria-drug-clinical-trial-cure-Covid-19/688334-5531292-rob53m/index.html.
Ebrahim, E., Lakay, B. (2020). Mkhize: Health sector must manage chronic patients amid Covid-19 - or it may bring a new challenge. Available at: https://www.health24.com/Medical/Infectious-diseases/Coronavirus/mkhize-health-sector-must-manage-chronic-patients-amid-covid-19-or-it-may-bring-a-new-challenge-20200430.
ECDC (2020a). Vaccines and treatment of COVID-19. Available at: https://www.ecdc.europa.eu/en/covid-19/latest-evidence/vaccines-and-treatment.
ECDC (2020b). Ebola outbreak in the Democratic Republic of the Congo. Available at: https://www.ecdc.europa.eu/en/ebola-virus-disease-outbreak-democratic-republic-congo-ongoing.
Editor Food Business Africa (2020). Trade Kings Foundation launches hygiene drive against Covid-19 in Lusaka. Available at: https://www.foodbusinessafrica.com/2020/04/22/trade-kings-foundation-launches-hygiene-drive-against-covid-19-in-lusaka/.
Ekor, M. (2014). The growing use of herbal medicines: issues relating to adverse reactions and challenges in monitoring safety. Front. Pharmacol. 4 (177), 1–10.
Ellinghaus, D., Degenhardt, F., Bujanda, L., Buti, M., Albillos, A., Invernizzi, P., et al. (2020). Genomewide Association Study of Severe Covid-19 with Respiratory Failure. N Engl. J. Med.
El-Sabaa, R. (2020). Egypt's health ministry launches coronavirus mobile application. Available at: http://english.ahram.org.eg/NewsContent/1/64/367263/Egypt/Politics-/Egypts-health-ministry-launches-coronavirus-mobile.aspx.
EMA. (2020). First COVID-19 treatment recommended for EU authorisation. 25 June 2020. Available at: https://www.ema.europa.eu/en/news/first-covid-19-treatment-recommended-eu-authorisation.
Endomba, F. T., Wouna, D. L. A., Danwang, C. (2020). Mental health during the coronavirus disease 2019 (Covid-19) pandemic: more is still to be done. PAMJ 35 (2), 7. doi: 10.11604/pamj.supp.2020.35.2.22605
Ermisch, M., Bucsics, A., Vella Bonanno, P., Arickx, F., Bybau, A., Bochenek, T., et al. (2016). Payers' Views of the Changes Arising through the Possible Adoption of Adaptive Pathways. Front. Pharmacol. 7 (305), 1–9.
European Medicine Agency (2020a). COVID-19: reminder of risk of serious side effects with chloroquine and hydroxychloroquine. Available at: https://www.ema.europa.eu/en/news/covid-19-reminder-risk-serious-side-effects-chloroquine-hydroxychloroquine.
European Medicines Agency (2020b). EU authorities agree new measures to support availability of medicines used in the COVID-19 pandemic. Available at: https://www.ema.europa.eu/en/news/eu-authorities-agree-new-measures-support-availability-medicines-used-covid-19-pandemic.
European Observatory. (2016). How can voluntary cross-border collaboration in public procurement improve access to health technologies in Europe? Available at: http://www.euro.who.int/:data/assets/pdf_file/0009/331992/PB21.pdf?ua=1.
EY Tax News Update (2020). Zambia issues additional fiscal measures to mitigate the impact of COVID-19. Available at: https://taxnews.ey.com/news/2020-1113-zambia-issues-additional-fiscal-measures-to-mitigate-the-impact-of-covid-19?uAlertID=Sd%2FG8rua1oj6%2Fl58EZ2AiA%3D%3D.
Fang, L., Karakiulakis, G., Roth, M. (2020). Are patients with hypertension and diabetes mellitus at increased risk for COVID-19 infection? Lancet Respir. Med. 8 (4), e21.
Fasseeh, A., Karam, R., Jameleddine, M., George, M., Kristensen, F. B., Al-Rabayah, A. A., et al. (2020). Implementation of Health Technology Assessment in the Middle East and North Africa: Comparison Between the Current and Preferred Status. Front. Pharmacol. 11 (15), 1–9.
Ferner, R. E., Aronson, J. K. (2020). Chloroquine and hydroxychloroquine in covid-19. BMJ 369, m1432.
Ferrario, A., Arāja, D., Bochenek, T., Čatić, T., Dankó, D., Dimitrova, M., et al. (2017). The Implementation of Managed Entry Agreements in Central and Eastern Europe: Findings and Implications. PharmacoEconomics 35 (12), 1271–1285.
Ford, N., Vitoria, M., Rangaraj, A., Norris, S. L., Calmy, A., Doherty, M. (2020). Systematic review of the efficacy and safety of antiretroviral drugs against SARS, MERS or COVID-19: initial assessment. J. Int. AIDS Soc. 23 (4), e25489.
Forrest, A. (2020). Coronavirus: 700 dead in Iran after drinking toxic methanol alcohol to cure Covid-19. Available at: https://www.msn.com/en-gb/news/coronavirus/coronavirus-700-dead-in-iran-after-drinking-toxic-methanol-alcohol-to-cure-covid-19/ar-BB13jC6f?ocid=spartandhp.
Founou, R. C., Founou, L. L., Essack, S. Y. (2017). Clinical and economic impact of antibiotic resistance in developing countries: A systematic review and meta-analysis. PLoS One 12 (12), 1–18.
Gaborit, B. J., Bergmann, J. F., Mussini, C., Arribas, J. R., Behrens, G., Walmsley, S., et al. (2020). Plea for multitargeted interventions for severe COVID-19. Lancet Infect. Dis.
Gallagher, F. (2020). Tracking hydroxychloroquine misinformation: How an unproven COVID-19 treatment ended up being endorsed by Trump. ABC News. Available at: https://abcnews.go.com/Health/tracking-hydroxychloroquine-misinformation-unproven-covid-19-treatment-ended/story?id=70074235.
Gao, J., Tian, Z., Yang, X. (2020). Breakthrough: Chloroquine phosphate has shown apparent efficacy in treatment of COVID-19 associated pneumonia in clinical studies. Biosci. Trends 14 (1), 72–73.
Gautret, P., Lagier, J. C., Parola, P., Hoang, V. T., Meddeb, L., Mailhe, M., et al. (2020). Hydroxychloroquine and azithromycin as a treatment of COVID-19: results of an open-label non-randomized clinical trial. Int. J. Antimicrob. Agents, 105949.
Geldsetzer, P. (2020). Use of Rapid Online Surveys to Assess People's Perceptions During Infectious Disease Outbreaks: A Cross-sectional Survey on COVID-19. J. Med. Internet Res. 22 (4), e18790–e1879e.
Geleris, J., Sun, Y., Platt, J., Zucker, J., Baldwin, M., Hripcsak, G., et al. (2020). Observational Study of Hydroxychloroquine in Hospitalized Patients with Covid-19. N Engl. J. Med. 382 (25), 2411–2418.
Ghana Ministry of Health. (2018). Ministry of Food and Agriculture, Ministry of Environment, Science, Technology and Innovation, Ministry of Fisheries and Aquaculture Development. Ghana National Action Plan for Antimicrobial Use and Resistance. 2017 - 2021. Available at: http://www.moh.gov.gh/wp-content/uploads/2018/04/NAP_FINAL_PDF_A4_19.03.2018-SIGNED-1.pdf.
Ghana News Agency. (2020). Successful testing regime and controls inform lifting of lockdown. Issued April 20 2020. Available at: https://newsghana.com.gh/successful-testing-regime-and-controls-inform-lifting-of-lockdown/.
Ghana Prorities Project. (2020). A rapid cost-benefit analysis of moderate social distancing in response to the COVID-19 pandemic in Ghana. 20 May 2020. Available at: https://www.copenhagenconsensus.com/sites/default/files/covid_brief_for_ndpc_ghana_final.pdf.
GhanaWeb (2020a). Pharmaceutical companies to produce 70% of country's drug needs. Available at: https://www.ghanaweb.com/GhanaHomePage/NewsArchive/Pharmaceutical-companies-to-produce-70-of-country-s-drug-needs-936016.
GhanaWeb (2020b). Coronavirus: Stop discriminating against recovered patients. Available at: https://www.ghanaweb.com/GhanaHomePage/NewsArchive/Coronavirus-Stop-discriminating-against-recovered-patients-Fred-Drah-926353.
Ghosal, A., Milko, V. Coronavirus could erode global fight against other diseases. Available at: https://www.msn.com/en-gb/news/world/coronavirus-could-erode-global-fight-against-other-diseases/ar-BB12HxuG?ocid=spartandhp#image=1.
Global Coronavirus COVID-19 Clinical Trial Tracker. (2020). Available at: https://www.covid-trials.org/.
Glied, S., Levy, H. (2020). The Potential Effects of Coronavirus on National Health Expenditures. JAMA.
Godman, B., Wettermark, B., van Woerkom, M., Fraeyman, J., Alvarez-Madrazo, S., Berg, C., et al. (2014). Multiple policies to enhance prescribing efficiency for established medicines in Europe with a particular focus on demand-side measures: findings and future implications. Front. Pharmacol. 5, 106.
Godman, B., Malmstrom, R. E., Diogene, E., Jayathissa, S., McTaggart, S., Cars, T., et al. (2014b). Dabigatran - a continuing exemplar case history demonstrating the need for comprehensive models to optimize the utilization of new drugs. Front. Pharmacol. 5, 109.
Godman, B., Malmstrom, R. E., Diogene, E., Gray, A., Jayathissa, S., Timoney, A., et al. (2015). Are new models needed to optimize the utilization of new medicines to sustain healthcare systems? Expert Rev. Clin. Pharmacol. 8 (1), 77–94.
Godman, B., Bucsics, A., Vella Bonanno, P., Oortwijn, W., Rothe, C. C., Ferrario, A., et al. (2018). Barriers for Access to New Medicines: Searching for the Balance Between Rising Costs and Limited Budgets. Front. Public Health 6, 328.
Godman, B., Grobler, C., Van-De-Lisle, M., Wale, J., Barbosa, W. B., Massele, A., et al. (2019). Pharmacotherapeutic interventions for bipolar disorder type II: addressing multiple symptoms and approaches with a particular emphasis on strategies in lower and middle-income countries. Expert Opin. Pharmacother. 20 (18), 2237–2255.
Godman, B. (2020). Combating COVID-19: Lessons learnt particularly among developing countries and the implications. Bangladesh J. Med. Sci. S103–8. doi: 10.3329/bjms.v19i0.48413
Godman, B., Haque, M., McKimm, J., Abu Bakar, M., Sneddon, J., Wale, J., et al. (2020a). Ongoing strategies to improve the management of upper respiratory tract infections and reduce inappropriate antibiotic use particularly among lower and middle-income countries: findings and implications for the future. Curr. Med. Res. Opin. 36 (2), 301–327.
Godman, B., Basu, D., Pillay, Y., Almeida, P., Mwita, J. C., Rwegerera, G. M., et al. (2020b). Ongoing and planned activities to improve the management of patients with Type 1 diabetes across Africa; implications for the future. Hosp. Pract. 48 (2), 51–67.
Godman, B., Basu, D., Pillay, Y., Mwita, J. C., Rwegerera, G. M., Anand Paramadhas, B. D., et al. (2020c). Review of Ongoing Activities and Challenges to Improve the Care of Patients With Type 2 Diabetes Across Africa and the Implications for the Future. Front. Pharmacol. 11 (108), 1–21.
Godman, B., McCabe, H., Leong, T. D. (2020d). Fixed dose drug combinations - are they pharmacoeconomically sound? Findings and implications especially for lower- and middle-income countries. Expert Rev. Pharmacoecon. Outc. Res. 20 (1), 1–26.
González-Sanguino, C., Ausín, B., Castellanos, M., Saiz, J., López-Gómez, A., Ugidos, C., et al. (2020). Mental health consequences during the initial stage of the 2020 Coronavirus pandemic (COVID-19) in Spain. Brain Behav. Immun.
Goodman, J. L., Borio, L. (2020). Finding Effective Treatments for COVID-19: Scientific Integrity and Public Confidence in a Time of Crisis. JAMA 87, 172–176.
Gounden, P., Barden, C., Charter, C. (2020). Taking stock: Competition law's response to the novel COVID-19 outbreak. Available at: https://www.cliffedekkerhofmeyr.com/en/news/publications/2020/Competition/competition-alert-1-april-Taking-stock-Competition-laws-response-to-the-novel-COVID-19-outbreak.html.
Government of The Kingdom of Eswatini (2020). Prime Minister's Statement - Partial Lockdown Strengthened Measures. Available at: http://www.gov.sz/images/CORONA/PM-statement-22-April-2020.pdf.
Gower, P. (2020). UP produces interactive app with real-time data on COVID-19 infections. Available at: https://www.up.ac.za/news/post_2885914-up-produces-interactive-app-with-real-time-data-on-covid-19-infections.
Guan, W.-J., Ni, Z.-Y., Hu, Y., Liang, W.-H., Ou, C.-Q., He, J.-X., et al. (2020). Clinical Characteristics of Coronavirus Disease 2019 in China. New Engl. J. Med. 382 (18), 1708–1720.
Guo, W., Ming, F., Dong, Y., Zhang, Q., Zhang, X., Mo, P., et al. (2020). A Survey for COVID-19 Among HIV/AIDS Patients in Two Districts of Wuhan, China. Lancet.
GuruGamer (2020). Warning: An American Died Of Using A Chloroquine Overdose Suggested As A Coronavirus Cure By President Trump. Available at: https://gurugamer.com/features/an-american-died-of-using-a-chloroquine-overdose-suggested-as-a-coronavirus-cure-by-president-trump-9466.
Habersaat, K. B., Betsch, C., Danchin, M., Sunstein, C. R., Böhm, R., Falk, A., et al. (2020). Ten considerations for effectively managing the COVID-19 transition. Nat. Hum. Behav. 4 (7), 677–687.
Haigh, L. (2020). Malaria in Zimbabwe exacerbated by Covid-19. Available at: https://www.itij.com/latest/news/malaria-zimbabwe-exacerbated-covid-19.
Hall, C. (2020). This One Thing Could Be the Key to Reducing the Progression of COVID-19. Available at: https://www.msn.com/en-us/health/medical/this-one-thing-could-be-the-key-to-reducing-the-progression-of-covid-19/ar-BB12Wb84.
Hamid, S., Mir, M. Y., Rohela, G. K. (2020). Novel coronavirus disease (COVID-19): a pandemic (epidemiology, pathogenesis and potential therapeutics). New Microbes New Infect. 35, 100679.
Haque, M., Islam, S., Iqbal, S., Urmi, U. L., Kamal, Z. M., Shuvo, S. A., et al. (2020). Availability and price changes of potential medicines and equipment for the prevention and treatment of COVID-19 among pharmacy and drug stores in Bangladesh; findings and implications. Bangladesh J. Med. Sci. 19 (Special Issue on Covid19), S36–S50.
Härter, G., Spinner, C. D., Roider, J., Bickel, M., Krznaric, I., Grunwald, S., et al. (2020). COVID-19 in people living with human immunodeficiency virus: a case series of 33 patients. Infection, 1–6.
Hatswell, A. J. (2020). Learnings for Health Economics from the Early Stages of the COVID-19 Pandemic. PharmacoEconom. - Open 4 (2), 203–205.
Hayat, K., Rosenthal, M., Xu, S., Arshed, M., Li, P., Zhai, P., et al. (2020). View of Pakistani Residents toward Coronavirus Disease (COVID-19) during a Rapid Outbreak: A Rapid Online Survey. Int. J. Environ. Res. Public Health 17 (10), 1–10.
He, J., He, L., Zhou, W., Nie, X., He, M. (2020). Discrimination and Social Exclusion in the Outbreak of COVID-19. Int. J. Environ. Res. Public Health 17 (8), 1–4.
Health 24. (2020). Dramatic drop in SA's immunisation rates. 26 June 2020. Available at: https://www.health24.com/Medical/Childhood-diseases/Vaccinations/dramatic-drop-in-sas-immunisation-rates-20200624-4.
Hedima, E. W., Adeyemi, M. S., Ikunaiye, N. Y. (2020). Community Pharmacists: On the frontline of health service against COVID-19 in LMICs. Res. Soc. Adm. Pharm.
Hernandez-Villafuerte, K., Li, R., Hofman, K. J. (2016). Bibliometric trends of health economic evaluation in Sub-Saharan Africa. Global Health 12 (1), 50.
High Commission of the Republic of Zambia (2020). Statement by the Hon. Minister of finance on covid-19. Available at: https://www.zambiahc.org.uk/news_events/statement-by-the-hon-minister-of-finance-on-covid-19/.
Ho, U. (2020). Covid-19 precaution: Some patients on chronic meds to have prescriptions filled for up to four months. Sportlight Health Journalism. 31 March 2020. Available from URL: http://www.msn.com/en-za/health/healthnews/covid-19-precaution-some-patients-on-chronic-meds-to-have-prescriptions-filled-for-up-to-four-months/ar-BB11VVGr
Hofman, K., Goldstein, S. (2020). COVID-19 risks forcing SA to make health trade-offs it can ill afford. Available at: https://www.wits.ac.za/covid19/covid19-news/latest/covid-19-risks-forcing-sa-to-make-health-trade-offs-it-can-ill-afford.html.
Hollingworth, S., Odame, E., Winch, A. (2018). Understanding data needs for HTA in Sub-Saharan Africa – a framework and Ghana case study. Available at: https://www.idsihealth.org/wp-content/uploads/2018/10/Data-Sources-.pdf.
Houreld, K., Lewis, D. (2020). In Africa, lack of coronavirus data raises fears of silent epidemic. 8 July 2020. Available at: https://www.yahoo.com/news/africa-lack-coronavirus-data-raises-081603106.html
Houreld, K., Lewis, D., McNeill, R., Granado, S. (2020). Virus exposes gaping holes in Africa's health systems. Available at: https://graphics.reuters.com/HEALTH-CORONAVIRUS/AFRICA/yzdpxoqbdvx/?fbclid=IwAR2Xu9J5CLPuUfxWyzFzi-uiSlixjgxsJDPXh0Loa40HNnEnisi0glXCG_A.
Huang, C., Wang, Y., Li, X., Ren, L., Zhao, J., Hu, Y., et al. (2020). Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 395 (10223), 497–506.
Huang, I., Lim, M. A., Pranata, R. (2020). Diabetes mellitus is associated with increased mortality and severity of disease in COVID-19 pneumonia - A systematic review, meta-analysis, and meta-regression. Diabetes Metab. Syndrome 14 (4), 395–403.
Hung, I. F.-N., Lung, K.-C., Tso, E. Y.-K., Liu, R., Chung, T. W.-H., Chu, M.-Y., et al. (2020). Triple combination of interferon beta-1b, lopinavir–ritonavir, and ribavirin in the treatment of patients admitted to hospital with COVID-19: an open-label, randomised, phase 2 trial. Lancet 395 (10238), 1695–1704.
Hwang, T. J., Rabheru, K., Peisah, C., Reichman, W., Ikeda, M. (2020). Loneliness and Social Isolation during the COVID-19 Pandemic. Int. Psychogeriatrics 1–15.
IFRC, UNICEF and WHO (2020). Social Stigma associated with COVID-19. Available at: https://reliefweb.int/sites/reliefweb.int/files/resources/covid19-stigma-guide.pdf.
Ighobor, K. (2020). Together we can win the war against COVID-19. Available at: https://www.un.org/africarenewal/magazine/special-edition-covid-19/together-we-can-win-war-against-covid-19.
IHME (2020a). New COVID-19 forecasts for Europe: Italy & Spain have passed the peak of their epidemics; UK, early in its epidemic, faces a fast-mounting death toll. Available at: http://www.healthdata.org/news-release/new-covid-19-forecasts-europe-italy-spain-have-passed-peak-their-epidemics-uk-early-its.
IHME (2020b). New COVID-19 forecasts: US hospitals could be overwhelmed in the second week of April by demand for ICU beds, and US deaths could total 81,000 by July. Available at: http://www.healthdata.org/news-release/new-covid-19-forecasts-us-hospitals-could-be-overwhelmed-second-week-april-demand-icu.
IMF (2020). IMF Executive Board Approves a US$491.5 Million Disbursement to Uganda to Address the COVID-19 Pandemic. Available at: https://www.imf.org/en/News/Articles/2020/05/06/pr20206-uganda-imf-executive-board-approves-us-million-disbursement-address-the-covid-19-pandemic.
Inciardi, R. M., Lupi, L., Zaccone, G., Italia, L., Raffo, M., Tomasoni, D., et al. (2020). Cardiac Involvement in a Patient With Coronavirus Disease 2019 (COVID-19). JAMA Cardiol. 5 (7), 1–6.
International Alliance of Patients' Organizations. (2020). COVID-19 Resources Hub. Available at: https://www.iapo.org.uk/covid-19-resources-hub.
International Society of Antimicrobial Chemotherapy. (2020). Official Statement from International Society of Antimicrobial Chemotherapy (ISAC) - Hydroxychloroquine and azithromycin as a treatment of COVID-19: results of an open-label non-randomized clinical trial (Gautret P et al. PMID 32205204). Available at: https://www.isac.world/news-and-publications/official-isac-statement.
IOL (2020). In a Covid-19 world, telemedicine will be the new normal. Available at: https://www.iol.co.za/lifestyle/health/in-a-covid-19-world-telemedicine-will-be-the-new-normal-47357559.
ISAC/ Elsevier (2020). Joint ISAC and Elsevier statement on Gautret et al. paper [PMID 32205204]. Available at: https://www.isac.world/news-and-publications/isac-elsevier-statement.
Jayaram, K., Leke, A., Ooko-Ombaka, A., Sun, Y. S. (2020). Tackling COVID-19 in Africa - An unfolding health and economic crisis that demands bold action. Available at: https://www.mckinsey.com/featured-insights/middle-east-and-africa/tackling-covid-19-in-africa#.
Jerving, S. (2020). How COVID-19 could complicate treatment for HIV patients. Available at: https://www.devex.com/news/how-covid-19-could-complicate-treatment-for-hiv-patients-96884.
JKUAT (2020a). JKUAT Trio Develop Apps to Trace, Triage and Manage COVID-19. Available at: http://www.jkuat.ac.ke/jkuat-trio-develop-contact-tracing-and-case-management-apps/.
JKAUT (2020b). JKUAT's Team of Engineers Invent Ventilators to Fill Shortage. Available at: http://www.jkuat.ac.ke/jkuats-team-of-engineers-invent-ventilators-to-fill-shortage/.
Jones, A. (2020). Coronavirus: How 'overreaction' made Vietnam a virus success. Available at: https://www.bbc.co.uk/news/world-asia-52628283.
Jose, R. J., Manuel, A. (2020). COVID-19 cytokine storm: the interplay between inflammation and coagulation. Lancet Respir. Med. 8 (6), e46–e47.
Journal du Cameroun. (2020). Cameroon: Monkey pox hits East region, kills one. Available at: https://www.journalducameroun.com/en/cameroon-monkey-pox-hits-east-region-kills-one/.
Kabale, N., Otsialo, M., Makong, B., Njeru, A., Muchui, D., Chepngeno, E., et al. (2020). Concern as patients shun health centres. Available at: https://www.nation.co.ke/news/Concern-as-patients-shun-health-centres/1056-5543778-13ejdvwz/index.html.
Kaine, E., Nwokik, J. (2020). Scaling Up African Pharmaceutical Manufacturing in a Time of COVID-19. Available at: https://www.cfr.org/blog/scaling-african-pharmaceutical-manufacturing-time-covid-19.
Kalungia, A., Godman, B. (2019). Implications of non-prescription antibiotic sales in China. Lancet Infect. Dis. 19 (12), 1272–1273.
Kalungia, A. C., Burger, J., Godman, B., Costa, J. O., Simuwelu, C. (2016). Non-prescription sale and dispensing of antibiotics in community pharmacies in Zambia. Expert Rev. Anti-Infe. Ther. 14 (12), 1215–1223.
Kansiime, S., Mwesigire, D., Mugerwa, H. (2019). Prevalence of non-communicable diseases among HIV positive patients on antiretroviral therapy at joint clinical research centre, Lubowa, Uganda. PLoS One 14 (8), e0221022.
Kasozi, K. I., Mujinya, R., Bogere, P., Ekou, J., Zirintunda, G., Ahimbisibwe, S., et al. (2020). Pandemic panic and anxiety in developing countries. Embracing One Health offers practical strategies in management of COVID-19 for Africa. PAMJ 35 (2):3. doi: 10.11604/pamj.supp.2020.35.2.22637
Kaufman, K. R., Petkova, E., Bhui, K. S., Schulze, T. G. (2020). A global needs assessment in times of a global crisis: world psychiatry response to the COVID-19 pandemic. BJPsych. Open 6 (3), e48.
Kavanagh, M. M., Erondu, N. A., Tomori, O., Dzau, V. J., Okiro, E. A., Maleche, A., et al. (2020). Access to lifesaving medical resources for African countries: COVID-19 testing and response, ethics, and politics. Lancet 395 (10238), 1735–1738.
KCE Report. (2017). KCE Report number 283. Horizon Scanning For Pharmaceuticals: Proposal For The Beneluxa Collaboration. Available at: http://www.beneluxa.org/sites/beneluxa.org/files/2017-07/Horizon%20scanning_ScientificReport_full.pdf.
Keates, A. K., Mocumbi, A. O., Ntsekhe, M., Sliwa, K., Stewart, S. (2017). Cardiovascular disease in Africa: epidemiological profile and challenges. Nat. Rev. Cardiol. 14 (5), 273–293.
Kenna, H. A., Poon, A. W., de los Angeles, C. P., Koran, L. M. (2011). Psychiatric complications of treatment with corticosteroids: review with case report. Psychiatry Clin. Neurosci. 65 (6), 549–560.
Kenyatta University (2020). K.U Makes Ventilators. Available at: http://www.ku.ac.ke/component/k2/item/1655-k-u-makes-ventilators.
Khan, M. S., Durrance-Bagale, A., Legido-Quigley, H., Mateus, A., Hasan, R., Spencer, J., et al. (2019). ‘LMICs as reservoirs of AMR': a comparative analysis of policy discourse on antimicrobial resistance with reference to Pakistan. Health Policy Plan 34 (3), 178–187.
Khan, M. S., Bory, S., Rego, S., Suy, S., Durrance-Bagale, A., Sultana, Z., et al. (2020). Is enhancing the professionalism of healthcare providers critical to tackling antimicrobial resistance in low- and middle-income countries? Hum. Resour. Health 18 (1), 10.
Khunti, K., Singh, A. K., Pareek, M., Hanif, W. (2020). Is ethnicity linked to incidence or outcomes of covid-19? BMJ 369, m1548.
Kindzeka, M. E. (2019a). More Deaths Feared From Cholera in Cameroon. Available at: https://www.voanews.com/africa/more-deaths-feared-cholera-cameroon.
Kindzeka, M. E. (2019b). Cameroon Launches Vaccination Campaign to Contain Measles Outbreak. Available at: https://www.voanews.com/africa/cameroon-launches-vaccination-campaign-contain-measles-outbreak.
Kindzeka, M. K. (2020). Cameroon Seizes Fake Coronavirus Drugs Sold by Scammers. Available at: https://www.voanews.com/science-health/coronavirus-outbreak/cameroon-seizes-fake-coronavirus-drugs-sold-scammers.
Kirby, T. (2020). Evidence mounts on the disproportionate effect of COVID-19 on ethnic minorities. Lancet Respir. Med. 8 (6), 547–548.
Kluge, H. H. P., Wickramasinghe, K., Rippin, H. L., Mendes, R., Peters, D. H., Kontsevaya, A., et al. (2020). Prevention and control of non-communicable diseases in the COVID-19 response. Lancet 395 (10238), 1678–1680.
Knott, S. (2020). Covid-19 could mark a deadly turn in Ghana's fight against fake drugs. Available at: https://www.theguardian.com/global-development/2020/apr/30/covid-19-could-mark-a-deadly-turn-in-ghana-fight-against-fake-drugs.
Kowalska, J. D., Skrzat-Klapaczyńska, A., Bursa, D., Balayan, T., Begovac, J., Chkhartishvili, N., et al. (2020). HIV care in times of the COVID-19 crisis - where are we now in Central and Eastern Europe? Int. J. Infect. Dis. 96, 311–314.
Kozloff, N., Mulsant, B. H., Stergiopoulos, V., Voineskos, A. N. (2020). The COVID-19 Global Pandemic: Implications for People With Schizophrenia and Related Disorders. Schizophr. Bull. 46 (4), 752–757.
Kretchy, I. A., Asiedu-Danso, M., Kretchy, J. P. (2020). Medication management and adherence during the COVID-19 pandemic: Perspectives and experiences from low-and middle-income countries. Res. Soc. Adm. Pharm.
Krubiner, C., Keller, J. M., Kaufman, J. (2020). Balancing the COVID-19 Response with Wider Health Needs: Key Decision-Making Considerations for Low- and Middle-Income Countries. Available at: https://www.cgdev.org/sites/default/files/balancing-covid-19-response-wider-health-needs-key-decision-making-considerations-low.pdf.
Kumar, S. U., Kumar, D. T., Christopher, B. P., Doss, C. G. P. (2020). The Rise and Impact of COVID-19 in India. Front. Med. 7, 250.
Kumwenda, T. (2020). CFTC Cautions 11 Pharmacies On Over-charging Items. Available at: https://www.zodiakmalawi.com/nw/national-news/64-news-in-northern-region/1528-cftc-cautions-11-pharmacies-on-over-charging-items.
Kyeyune, H. (2020). Shutdown in Uganda over COVID-19 hits poor hard - Times tough not only due to fears of infection but also because of poverty, says shop owner. Available at: https://www.aa.com.tr/en/africa/shutdown-in-uganda-over-covid-19-hits-poor-hard/1787526.
Lakay, B. (2020). Your 6-month prescription expiring? Your pharmacist may extend it, new regulations state. Available at: https://www.health24.com/Medical/Infectious-diseases/Coronavirus/your-6-month-prescription-expiring-your-pharmacist-may-extend-it-new-regulations-state-20200430-2.
LaMarca, S. (2020). Scientists In Senegal Developed A $1 COVID-19 Testing Kit And Plan To Export Millions To African Countries. Available at: https://tanksgoodnews.com/2020/04/29/senegal-1-testing-kit/.
Lapolla, P., Mingoli, A., Lee, R. (2020). Deaths from COVID-19 in healthcare workers in Italy - what can we learn? Infection Control Hosp. Epidemiol. 1–4.
Larson, H. (2020). Blocking information on COVID-19 can fuel the spread of misinformation - Governments need to think twice before they suppress messages related to COVID-19. Nature 580, 306.
Le Roux, C., Dramowski, A. (2020). Personal protective equipment (PPE) in a pandemic: Approaches to PPE preservation for South African healthcare facilities. S. Afr. Med. J. 110 (6), 466–468.
Li, Q., Guan, X., Wu, P., Wang, X., Zhou, L., Tong, Y., et al. (2020). Early Transmission Dynamics in Wuhan, China, of Novel Coronavirus-Infected Pneumonia. N Engl. J. Med. 382 (13), 1199–1207.
Li, W., Yang, Y., Liu, Z. H., Zhao, Y. J., Zhang, Q., Zhang, L., et al. (2020). Progression of Mental Health Services during the COVID-19 Outbreak in China. Int. J. Biol. Sci. 16 (10), 1732–1738.
LinksCommunity (2020). Leveraging Technology to Improve Health Care During the COVID-19 Pandemic and Beyond. Available at: https://linkscommunity.org/assets/PDFs/cov039_telemedicine_v3_14may2020.pdf.
Liwa, A. C., Smart, L. R., Frumkin, A., Epstein, H.-A. B., Fitzgerald, D. W., Peck, R. N. (2014). Traditional herbal medicine use among hypertensive patients in sub-Saharan Africa: a systematic review. Curr. Hypertens. Rep. 16 (6), 437.
Logie, C. H. (2020). Lessons learned from HIV can inform our approach to COVID-19 stigma. J. Int. AIDS Soc. 23, e25504.
Lorgelly, P. K., Adler, A. (2020). Impact of a Global Pandemic on Health Technology Assessment. Appl. Health Econ. Health Policy 18 (3), 339–343
Lubega, M., Ekol, J. E. (2020). Preparing communities to receive persons recently suspected or diagnosed with COVID-19. Pan Afr. Med. J. 35 (2), 21.
Luo, L., Jiang, J., Wang, C., Fitzgerald, M., Hu, W., Zhou, Y., et al. (2020). Analysis on herbal medicines utilized for treatment of COVID-19. Acta Pharm. Sin. B.
Luo, P., Liu, Y., Qiu, L., Liu, X., Liu, D., Li, J. (2020). Tocilizumab treatment in COVID-19: A single center experience. J. Med. Virol. 92 (7), 814–818.
Luo, E., Zhang, D., Luo, H., Liu, B., Zhao, K., Zhao, Y., et al. (2020). Treatment efficacy analysis of traditional Chinese medicine for novel coronavirus pneumonia (COVID-19): an empirical study from Wuhan, Hubei Province, China. Chin. Med. 15 (34), 1–13.
Lusakatimes (2020). Government Suspended customs duties and VAT on additional medical supplies used in the fight against COVID-19. Available at: https://www.lusakatimes.com/2020/04/20/government-suspended-customs-duties-and-vat-on-additional-medical-supplies-used-in-the-fight-against-covid-19/.
Mabuka-Maroa, J. (2020). Few clinical trials are done in Africa: COVID-19 shows why this urgently needs to change. Available at: https://theconversation.com/few-clinical-trials-are-done-in-africa-covid-19-shows-why-this-urgently-needs-to-change-135117.
MacQuilkan, K., Baker, P., Downey, L., Ruiz, F., Chalkidou, K., Prinja, S., et al. (2018). Strengthening health technology assessment systems in the global south: a comparative analysis of the HTA journeys of China, India and South Africa. Glob. Health Action 11 (1), 1527556.
Mahase, E. (2020b). Covid-19: EU states report 60% rise in emergency calls about domestic violence. BMJ 369, m1872.
Manfredi, G., Kotzalidis, G. D., Sani, G., Koukopoulos, A. E., Savoja, V., Lazanio, S., et al. (2010). Persistent interferon-ß-1b-induced psychosis in a patient with multiple sclerosis. Psychiatry Clin. Neurosci. 64 (5), 584–586.
Markovic-Pekovic, V., Grubisa, N., Burger, J., Bojanic, L., Godman, B. (2017). Initiatives to Reduce Nonprescription Sales and Dispensing of Antibiotics: Findings and Implications. J. Res. Pharm. Pract. 6 (2), 120–125.
Marra, L. P., Araujo, V. E., Silva, T. B., Diniz, L. M., Guerra Junior, A. A., Acurcio, F. A., et al. (2016). Clinical Effectiveness and Safety of Analog Glargine in Type 1 Diabetes: A Systematic Review and Meta-Analysis. Diabetes Ther. 7 (2), 241–258.
Martinez-Alvarez, M., Jarde, A., Usuf, E., Brotherton, H., Bittaye, M., Samateh, A. L., et al. (2020). COVID-19 pandemic in west Africa. Lancet Global Health 8 (5), e631–e632.
Masango, T. A. (2020). Misuse of chloroquine, azithromycin and lopinavir-ritonavir for the prevention and/or potential treatment of Covid-19. Available at: https://www.biznews.com/briefs/2020/03/24/pharmacy-body-anti-malaria-drugs-covid-19.
Masina, L. (2020a). Malawi President Announces New Measures Against Coronavirus. Available at: https://www.voanews.com/covid-19-pandemic/malawi-president-announces-new-measures-against-coronavirus.
Masina, L. (2020b). UN in Malawi Launches Emergency Appeal for COVID-19 Response. Available at: https://www.voanews.com/covid-19-pandemic/un-malawi-launches-emergency-appeal-covid-19-response.
Massonnaud, C., Roux, J., Crépey, P. (2020). COVID-19: Forecasting short term hospital needs in France. MedRxiv preprint. Available at: https://www.medrxiv.org/content/10.1101/2020.03.16.20036939v1.full.pdf. doi: 10.1101/2020.03.16.20036939
Matengo, D. (2019). Cameroon declares polio emergency. Available at: https://africa.cgtn.com/2019/06/01/cameroon-declares-polio-emergency/.
Matos, R. I., Chung, K. K. (2020). DoD COVID-19 Practice Management Guide. Available at: http://www.med.umich.edu/surgery/mcccn/documents/DoD-COVID-19-Practice-Management-Guide-V10.
Matshediso, M. (2020). Gauteng Health adds COVID-19 feature to Mpilo App. Available at: https://www.vukuzenzele.gov.za/gauteng-health-adds-covid-19-feature-mpilo-app.
Mbuagbaw, L., Sivaramalingam, B., Navarro, T., Hobson, N., Keepanasseril, A., Wilczynski, N. J., et al. (2015). Interventions for Enhancing Adherence to Antiretroviral Therapy (ART): A Systematic Review of High Quality Studies. AIDS patient Care STDs 29 (5), 248–266.
McCaffrey, D. (2020). Analysis: Africa's unexpected COVID-19 figures. Available at: https://www.euronews.com/2020/05/12/analysis-africa-s-unexpected-covid-19-figures.
McMaster University. COVID-END (2020). COVID-19 Evidence Network to support Decision-making. Available at: https://www.mcmasterforum.org/networks/covid-end.
Media Foundation West Africa (2020). Curbing Misinformation in a COVID -19 Era, Ghana's Approach. Available at: https://www.mfwa.org/issues-in-focus/curbing-misinformation-in-a-covid-19-era-ghanas-approach/.
Medical Brief (2020a). Cape Town's BCG trials threatened by demands from advocacy group. Available at: https://www.medicalbrief.co.za/archives/cape-towns-bcg-trials-threatened-by-demands-from-advocacy-group/.
Medical Brief (2020b). Health Department 'taking steps' over shortage of antidepressants and antipsychotics. Available at: https://www.medicalbrief.co.za/archives/health-department-taking-steps-over-shortage-of-antidepressants-and-antipsychotics/.
Mehra, M. R., Desai, S. S., Ruschitzka, F., Patel, A. N. (2020). Retracted: Hydroxychloroquine or chloroquine with or without a macrolide for treatment of COVID-19: a multinational registry analysis. Lancet. doi: 10.1016/S0140-6736(20)31180-6
Mehta, H. B., Ehrhardt, S., Moore, T. J., Segal, J. B., Alexander, G. C. (2020). Characteristics of registered clinical trials assessing treatments for COVID-19: a cross-sectional analysis. BMJ Open 10 (6), e039978.
Mehtar, S., Preiser, P., Lakhe, N. A., Bousso, A., TamFum, J.-J. M., Kallay, O., et al. (2020). Limiting the spread of COVID-19 in Africa: one size mitigation strategies do not fit all countries. Lancet Global Health. 8 (7), e881–e883.
Mendelson, M., Matsoso, M. (2015). The South African Antimicrobial Resistance Strategy Framework. AMR Control, 54–61.
Meng, L., Qiu, H., Wan, L., Ai, Y., Xue, Z., Guo, Q., et al. (2020). Intubation and Ventilation amid the COVID-19 Outbreak: Wuhan's Experience. Anesthesiology 132 (6), 1317–1332.
Mensah, G. A., Roth, G. A., Sampson, U. K., Moran, A. E., Feigin, V. L., Forouzanfar, M. H., et al. (2015). Mortality from cardiovascular diseases in sub-Saharan Africa, 1990-2013: a systematic analysis of data from the Global Burden of Disease Study 2013. Cardiovasc. J. Afr. 26 (2 Suppl 1), S6–10.
Miljković, N., Godman, B., Kovačević, M., Polidori, P., Tzimis, L., Hoppe-Tichy, T., et al. (2020). Prospective Risk Assessment of Medicine Shortages in Europe and Israel: Findings and Implications. Front. Pharmacol. 11 (357), 1–4.
Mining Review (2020). South's Africa COVID-19 PPE shortage being addressed. Available at: https://www.miningreview.com/health-and-safety/souths-africa-covid-19-ppe-shortage-being-addressed/.
Ministry of Communications, Republic of Ghana (2020). Launch of GH COVID-19 Tracker App. Available at: https://www.moc.gov.gh/launch-gh-covid-19-tracker-app.
Ministry of Health, VietNam (2020). Hướng dẫn chẩn đoán và điều trị viêm đường hô hấp cấp do SARS-CoV-2 (COVID-19) phiên bản lần thứ 3. Available at: https://kcb.vn/huong-dan-chan-doan-va-dieu-tri-viem-duong-ho-hap-cap-do-sar-cov-2-covid-19-phien-ban-lan-thu-3.html.
Mitjà, O., Clotet, B. (2020). Use of antiviral drugs to reduce COVID-19 transmission. Lancet Global Health 8 (5), e639–ee40.
Modisakeng, C., Matlala, M., Godman, B., Meyer, J. C. (2020). Medicine shortages and challenges with the procurement process among public sector hospitals in South Africa; findings and implications. BMC Health Serv. Res. 20 (1), 234.
Monteleone, G., Sarzi-Puttini, P. C., Ardizzone, S. (2020). Preventing COVID-19-induced pneumonia with anticytokine therapy. Lancet Rheumatol. 2 (5), E255–E256.
Moore, W. G. (2020). Curfews are a safer plan than total lockdowns to slow Covid-19's spread in informal economies. Available at: https://qz.com/africa/1836458/curfews-not-lockdowns-will-slow-covid-19-spread-in-africa/.
Moorkens, E., Vulto, A. G., Huys, I., Dylst, P., Godman, B., Keuerleber, S., et al. (2017). Policies for biosimilar uptake in Europe: An overview. PLoS One 12 (12), e0190147.
MSF (2019). A multidisciplinary approach to stem the spread of cholera. Available at: https://www.msf.org/how-stem-spread-cholera-cameroon-and-lake-chad-region.
MSF (2020). Eswatini: Responding to COVID-19 in a country already fighting a dual HIV/TB epidemic. Available at: https://www.msf.org/responding-covid-19-eswatini.
Mueller, D., Tivey, D., Croce, D. (2017). Health-technology assessment: Its role in strengthening health systems in developing countries. South. Afr. J. Public Health 2 (1), 6–11.
Mukokinya, M., Opanga, S., Oluka, M., Godman, B. (2018). Dispensing of antimicrobials in Kenya: A cross-sectional pilot study and its implications. J. Res. Pharm. Pract. 7 (2), 77–82.
Mules, I. (2020). Tanzania under fire from WHO for lackluster response to COVID-19 pandemic. Available at: https://www.dw.com/en/tanzania-under-fire-from-who-for-lackluster-response-to-covid-19-pandemic/a-53304699.
Muraya, J. (2020). Govt turns spotlight on refugee camps as COVID-19 hits 490 in Kenya. Available at: https://www.capitalfm.co.ke/news/2020/05/govt-turns-spotlight-on-refugee-camps-as-covid-19-hits-490-in-kenya/.
Murthy, S., Leligdowicz, A., Adhikari, N. K. (2015). Intensive care unit capacity in low-income countries: a systematic review. PLoS One 10 (1), e0116949.
Mutahi, B. (2020). Coronavirus: The fear of being sentenced to a Kenyan quarantine centre. Available at: https://www.bbc.co.uk/news/world-africa-52326316.
Mwai, P., Giles, C. (2020). Coronavirus in Tanzania: What do we know? Available at: https://www.bbc.co.uk/news/world-africa-52723594.
N Gage Consulting (2017). Egypt's Pharmaceutical Sector Following Bold Economic Reforms: Challenges and Opportunities. Available at: https://www.ngage-consulting.com/downloads/Pharmaceutical_PDF_Final_Version_K_and_A.pdf.
Nachimuthu, S., Vijayalakshmi, R., Sudha, M., Viswanathan, V. (2020). Coping with diabetes during the COVID - 19 lockdown in India: Results of an online pilot survey. Diabetes Metab. Syndrome 14 (4), 579–582.
Neil, S., Campbell, E. M. (2020). Fake Science: XMRV, COVID-19 And The Toxic Legacy of Dr Judy Mikovits. AIDS Res. Hum. Retrov. 36 (7), 545–549 .
Newton, P. N., Bond, K. C. (2020). COVID-19 and risks to the supply and quality of tests, drugs, and vaccines. Lancet Global Health. 8 (6), e754–e755.
Ng, Y., Li, Z., Chua, Y. X., Chaw, W. L., Zhao, Z., Er, B., et al. (2020). Evaluation of the Effectiveness of Surveillance and Containment Measures for the First 100 Patients with COVID-19 in Singapore - January 2-February 29, 2020. MMWR Morbid. Mortal. Wkly. Rep. 69 (11), 307–311.
Nga, L., Phuong, L., Anh, P. (2020). Hanoi man OD's on rumored malaria drug cure for Covid-19. 23 March 2020. Available at: https://e.vnexpress.net/news/news/hanoi-man-od-s-on-rumored-malaria-drug-cure-for-covid-19-4073488.html
Nicholas, T., Mandaah, F. V., Esemu, S. N., Vanessa, A. B. T., Gilchrist, K. T. D., Vanessa, L. F., et al. (2020). COVID-19 knowledge, attitudes and practices in a conflict affected area of the South West Region of Cameroon. PAMJ 35 (2), 34. doi: 10.11604/pamj.supp.2020.35.2.22963
Nigeria CDC (2018). A home coming: My visit to Liberia's new National Public Health Institute. Available at: https://ncdc.gov.ng/blog/post/29/?t=a-home-coming:-my-visit-to-liberia%E2%80%99s-new-national-public-health-institute.
Nigeria Centre for Disease Control (2020a). Guidelines and Protocols - National Interim Guidelines for Clinical Management of COVID-19. Available at: https://ncdc.gov.ng/themes/common/docs/protocols/177_1584210847.pdf.
Nigeria Centre for Disease Control (2020b). An update of Lassa fever outbreak in Nigeria. Available at: https://ncdc.gov.ng/diseases/sitreps/?cat=5&name=An%20update%20of%20Lassa%20fever%20outbreak%20in%20Nigeria.
NIH ClinicalTrials.gov (2020a). BCG Vaccination for Healthcare Workers in COVID-19 Pandemic. Available at: https://clinicaltrials.gov/ct2/show/NCT04379336?cond=COVID-19&cntry=ZA&draw=2.
NIH ClinicalTrials.gov (2020b). COVID-19 Vaccine (ChAdOx1 nCoV-19) Trial in South African Adults With and Without HIV-infection. Available at: https://clinicaltrials.gov/ct2/show/NCT04444674?cond=COVID-19&cntry=ZA&draw=2&rank=7.
NIH. (2020a). The National Institutes of Health COVID-19 Treatment Guidelines Panel Provides Recommendations for Dexamethasone in Patients with COVID-19. 25 June 2020. Available at: https://www.covid19treatmentguidelines.nih.gov/dexamethasone/.
NIH. (2020b). NIH Clinical Trial Shows Remdesivir Accelerates Recovery from Advanced COVID-19. 29 April 2020. Available at: https://www.niaid.nih.gov/news-events/nih-clinical-trial-shows-remdesivir-accelerates-recovery-advanced-covid-19.
NIH. (2020c). NIH halts clinical trial of hydroxychloroquine. 20 June 2020. Available at: https://www.nhlbi.nih.gov/news/2020/nih-halts-clinical-trial-hydroxychloroquine.
Nkeck, J. R., Tsafack, E. E., Ndoadoumgue, A. L., Endomba, F. T. (2020). An alert on the incautious use of herbal medicines by sub-Saharan African populations to fight against the COVID-19. PAMJ 35 (2), 26. doi: 10.11604/pamj.supp.2020.35.2.23161
Nkengasong, J. N., Mankoula, W. (2020). Looming threat of COVID-19 infection in Africa: act collectively, and fast. Lancet 395 (10227), 841–842.
Nordling, N. (2020). Unproven herbal remedy against COVID-19 could fuel drug-resistant malaria, scientists warn. Available at: https://www.sciencemag.org/news/2020/05/unproven-herbal-remedy-against-covid-19-could-fuel-drug-resistant-malaria-scientists.
Nussbaumer-Streit, B., Mayr, V., Dobrescu, A. I., Chapman, A., Persad, E., Klerings, I., et al. (2020). Quarantine alone or in combination with other public health measures to control COVID-19: a rapid review. Cochrane Database Syst. Rev. 4, Cd013574.
Nyaira, S. (2020). Ways Africa's Free Trade Area could help mitigate effects of COVID-19. Available at: https://www.un.org/africarenewal/web-features/coronavirus/ways-africa%E2%80%99s-free-trade-area-could-help-mitigate-effects-covid-19.
Nyavor, G. (2020). Breakthrough as Ghana researchers develop rapid diagnostic testing for Covid-19. Available at: https://www.myjoyonline.com/news/health/breakthrough-as-ghana-researchers-develop-rapid-diagnostic-testing-for-covid-19/.
O'Neill, L. A. J., Netea, M. G. (2020). BCG-induced trained immunity: can it offer protection against COVID-19? Nat. Rev. Immunol. 20 (6), 335–337.
OCHA Zimbabwe (2020). Situation Reports Highlights. 7 May 2020. Available at: https://reliefweb.int/sites/reliefweb.int/files/resources/Situation%20Report%20-%20Zimbabwe%20-%206%20May%202020.pdf.
OCHA. (2020). Sudan Situation Report Updated. 19 March 2020. Available at: https://reliefweb.int/sites/reliefweb.int/files/resources/Situation%20Report%20-%20Sudan%20-%2019%20Mar%202020.pdf.
OECD (2020). The Covid-19 Crisis in Egypt. Available at: https://www.oecd.org/mena/competitiveness/The-Covid-19-Crisis-in-Egypt.pdf.
Okonjo-Iweala, N., Coulibaly, B. S., Thiam, T., Kaberuka, D., Songwe, V., Masiyiwa, S., et al. (2020). Africa needs debt relief to fight COVID-19. Available at: https://www.brookings.edu/opinions/africa-needs-debt-relief-to-fight-covid-19/.
Okwen, P. M., Maweu, I., Grimmer, K., Margarita Dizon, J. (2019). Evaluation of all African clinical practice guidelines for hypertension: Quality and opportunities for improvement. J. Eval. Clin. Pract. 25 (4), 565–574.
Olafusi, E. (2020). The World Health Organisation (WHO) says Nigeria has expressed interest to be part of the global solidarity drug trial to combat COVID-19. Available at: https://www.thecable.ng/who-nigeria-has-expressed-interest-to-be-part-of-covid-19-drug-trials.
Ong, S. E., Koh, J. J. K., Toh, S. E. S., Chia, K. S., Balabanova, D., McKee, M., et al. (2018). Assessing the influence of health systems on Type 2 Diabetes Mellitus awareness, treatment, adherence, and control: A systematic review. PLoS One 13 (3), e0195086.
Ongole, J. J., Rossouw, T. M., Fourie, P. B., Stoltz, A. C., Hugo, J., Marcus, T. S. (2020). Sustaining essential healthcare in Africa during the COVID19 pandemic. Available at: https://www.theunion.org/news-centre/news/body/IJTLD-June-0214_Ongole.pdf.
Oni, T., Youngblood, E., Boulle, A., McGrath, N., Wilkinson, R. J., Levitt, N. S. (2015). Patterns of HIV, TB, and non-communicable disease multi-morbidity in peri-urban South Africa- a cross sectional study. BMC Infect. Dis. 15, 20.
Outbreak News (2020). Cameroon monkeypox: Follow-up and more details. Available at: http://outbreaknewstoday.com/cameroon-monkeypox-follow-up-and-more-details-15866/.
Pan, D., Sze, S., Minhas, J. S., Bangash, M. N., Pareek, N., Divall, P., et al. (2020). The impact of ethnicity on clinical outcomes in COVID-19: A systematic review. EClinicalMedicine 23, 100404.
Paranjpe, I., Fuster, V., Lala, A., Russak, A., Glicksberg, B. S., Levin, M. A., et al. (2020). Association of Treatment Dose Anticoagulation with In-Hospital Survival Among Hospitalized Patients with COVID-19. J. Am. Coll. Cardiol. 76 (1), 122–124.
Pareek, M., Bangash, M. N., Pareek, N., Pan, D., Sze, S., Minhas, J. S., et al. (2020). Ethnicity and COVID-19: an urgent public health research priority. Lancet 395 (10234), 1421–1422.
Parpia, A. S., Ndeffo-Mbah, M. L., Wenzel, N. S., Galvani, A. P. (2016). Effects of Response to 2014-2015 Ebola Outbreak on Deaths from Malaria, HIV/AIDS, and Tuberculosis, West Africa. Emerg. Infect. Dis. 22 (3), 433–441.
Pauloluniyi (2020). First African SARS-CoV-2 genome sequence from Nigerian COVID-19 case. Available at: http://virological.org/t/first-african-sars-cov-2-genome-sequence-from-nigerian-covid-19-case/421.
Pearson, J., Nguyen, P. (2020). Vietnam to ease nationwide coronavirus lockdown. Available at: https://uk.reuters.com/article/uk-health-coronavirus-vietnam/vietnam-to-ease-nationwide-coronavirus-lockdown-idUKKCN2241LD.
Perencevich, E. N., Diekema, D. J., Edmond, M. B. (2020). Moving Personal Protective Equipment Into the Community: Face Shields and Containment of COVID-19. JAMA.
Perry Wilson, F. (2020). COVID-19, Hydroxycloroquine, and the Death of Evidence-Based Medicine. Available at: https://www.methodsman.com/blog/covid-19-evidence.
Phiri, C. (2020). African Countries Urged To Collaborate More In The Fight Against Covid-19. Available at: https://zambiareports.com/2020/04/30/african-countries-urged-collaborate-fight-covid-19/.
Pilling, D. (2020). Low Covid-19 death toll raises hopes Africa may be spared worst. Available at: https://www.ft.com/content/e9cf5ed0-a590-4bd6-8c00-b41d0c4ae6e0.
Pitts, P. J. (2019). Towards Meaningful Engagement for the Patient Voice. Patient - Patient-Centered Outc. Res. 12 (4), 361–363.
Pitts, P. J. (2020). Our Most Powerful Weapon to Fight COVID-19: Patient Involvement. Patient - Patient-Centered Outc. Res. 13 (3), 255.
Politi, D. (2020). Nigeria Reports Chloroquine Poisonings as Trump Keeps Pushing Drug Against Coronavirus. Available at: https://slate.com/news-and-politics/2020/03/nigeria-chloroquine-poisonings-trump-pushing-drug-coronavirus.html.
Pradhan, D., Biswasroy, P., Kumar Naik, P., Ghosh, G., Rath, G. (2020). A Review of Current Interventions for COVID-19 Prevention. Arch. Med. Res. 51 (5), 363–374.
President Republic of Kenya (2020a). Africa To Pursue Loan Waivers As Safeguard Against Adverse Economic Impact Of Coronavirus. Available at: https://www.president.go.ke/2020/04/04/africa-to-pursue-loan-waivers-as-safeguard-against-adverse-economic-impact-of-coronavirus/.
President Republic of Kenya. (2020b)Presidential Address on The State Interventions to Cushion Kenyans Against Economic Effects Of Covid-19 Pandemic on 25th March, 2020. Available at: https://www.president.go.ke/2020/03/25/presidential-address-on-the-state-interventions-to-cushion-kenyans-against-economic-effects-of-covid-19-pandemic-on-25th-march-2020/.
Prokunina-Olsson, L., Alphonse, N., Dickenson, R. E., Durbin, J. E., Glenn, J. S., Hartmann, R., et al. (2020). COVID-19 and emerging viral infections: The case for interferon lambda. J. Exp. Med. 217 (5), 1–4.
Public Health England (2020). Disparities in the risk and outcomes of COVID-19. Available at: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/892085/disparities_review.pdf.
Rajendran, D. K., Rajagopal, V., Alagumanian, S., Santhosh Kumar, T., Sathiya Prabhakaran, S. P., Kasilingam, D. (2020). Systematic literature review on novel corona virus SARS-CoV-2: a threat to human era. VirusDisease 31 (2), 161–173.
Rajkumar, R. P. (2020). COVID-19 and mental health: A review of the existing literature. Asian J. Psychiatry 52, 102066.
Ramalingam, S., Graham, C., Dove, J., Morrice, L., Sheikh, A. (2019). A pilot, open labelled, randomised controlled trial of hypertonic saline nasal irrigation and gargling for the common cold. Sci. Rep. 9 (1), 1015.
Ramalingam, S., Graham, C., Dove, J., Morrice, L., Sheikh, A. (2020). Hypertonic saline nasal irrigation and gargling should be considered as a treatment option for COVID-19. J. Global Health 10 (1), 010332.
Reade, M. C., Finfer, S. (2014). Sedation and delirium in the intensive care unit. N Engl. J. Med. 370 (5), 444–454.
Recovery Collaborative Group, Horby, P., Lim, W.S., Emberson Mafham, M., JR, Bell, J.L., Linsell, L., et al. (2020). Dexamethasone in Hospitalized Patients with Covid-19 - Preliminary Report. N Engl J Med. doi: 10.1056/NEJMoa2021436
Recovery Trial (2020a). No clinical benefit from use of hydroxychloroquine in hospitalised patients with COVID-19. Available at: https://www.recoverytrial.net/news/statement-from-the-chief-investigators-of-the-randomised-evaluation-of-covid-19-therapy-recovery-trial-on-hydroxychloroquine-5-june-2020-no-clinical-benefit-from-use-of-hydroxychloroquine-in-hospitalised-patients-with-covid-19.
Recovery Trial (2020b). Statement from the Chief Investigators of the Randomised Evaluation of COVid-19 thERapY (RECOVERY) Trial on lopinavir-ritonavir, 29 June 2020. No clinical benefit from use of lopinavir-ritonavir in hospitalised COVID-19 patients studied in RECOVERY. Available at: https://www.recoverytrial.net/files/lopinavir-ritonavir-recovery-statement-29062020_final.pdf.
Recovery Trial (2020a). No clinical benefit from use of hydroxychloroquine in hospitalised patients with COVID-19. Available at: https://www.recoverytrial.net/news/statement-from-the-chief-investigators-of-the-randomised-evaluation-of-covid-19-therapy-recovery-trial-on-hydroxychloroquine-5-june-2020-no-clinical-benefit-from-use-of-hydroxychloroquine-in-hospitalised-patients-with-covid-19.
Rees, V. Dexamethasone to be available on NHS as COVID-19 treatment. 22 June 2020. Available at: https://www.europeanpharmaceuticalreview.com/news/121560/dexamethasone-to-be-available-on-nhs-as-covid-19-treatment/
ReliefWeb (2020a). Democratic Republic of Congo: Coronavirus (COVID-19) Situation Report 5. Available at: https://reliefweb.int/report/democratic-republic-congo/democratic-republic-congo-coronavirus-covid-19-situation-report-5.
ReliefWeb (2020b). Namibia launches COVID-19 Communication Centre. Available at: https://reliefweb.int/report/namibia/namibia-launches-covid-19-communication-centre.
Ren, Y., Zhou, Y., Qian, W., Zhang, X., Liu, Z., Wang, R., et al. (2020). Letter to the Editor “A longitudinal study on the mental health of general population during the COVID-19 epidemic in China”. Brain Behav. Immun. 87, 132–133.
Republic of South Africa Government Gazette. (2020). Exclusion Of Schedule 2, Schedule 3 And Schedule 4 Substances From The Operation Of Certain Provisions Of The Medicines And Related Substances Act, 1965 (Act No. 101 of 1965). April 2020. Available at: https://edit.laws.africa/works/akn/za/act/gn/2020/r481/media/publication/za-act-gn-2020-r481-publication-document.pdf.
Review Online (2020). No lithium tablets: anti-depressant shortage looms. Available at: https://reviewonline.co.za/404809/no-lithium-tablets-anti-depressant-shortage-looms/.
Rich, D. (2020). Covid-19: In Cameroon, chloroquine therapy hailed by French expert becomes state protocol. Available at: https://www.france24.com/en/20200503-covid-19-in-cameroon-a-chloroquine-therapy-hailed-by-french-expert-becomes-state-protocol.
Richardson, S., Hirsch, J. S., Narasimhan, M., Crawford, J. M., McGinn, T., Davidson, K. W., et al. (2020). Presenting Characteristics, Comorbidities, and Outcomes Among 5700 Patients Hospitalized With COVID-19 in the New York City Area. JAMA 323 (20), 2052–2059.
Rios-González, C. M. (2020). Knowledge, attitudes and practices towards COVID-19 in Paraguayans during outbreaks: a quick online survey. Available at: https://preprints.scielo.org/index.php/scielo/preprint/download/149/179/164
Roberto, M. (2020). Testing COVID-19 costs KSh 100 in Senegal while Kenyan hospital charges KSh 10k for same service. Available at: https://www.msn.com/en-xl/news/other/testing-covid-19-costs-ksh-100-in-senegal-while-kenyan-hospital-charges-ksh-10k-for-same-service/ar-BB13gPE3.
Rosenberg, E. S., Dufort, E. M., Udo, T., Wilberschied, L. A., Kumar, J., Tesoriero, J., et al. (2020). Association of Treatment With Hydroxychloroquine or Azithromycin With In-Hospital Mortality in Patients With COVID-19 in New York State. JAMA 323 (24), 2493–2502.
Roumier, M., Paule, R., Groh, M., Vallee, A., Ackermann, F. (2020). Interleukin-6 blockade for severe COVID-19. medrxiv 04 (20), 20061861.
Rubin, E. J., Harrington, D. P., Hogan, J. W., Gatsonis, C., Baden, L. R., Hamel, M. B. (2020). The Urgency of Care during the Covid-19 Pandemic - Learning as We Go. N Engl. J. Med. 382 (25), 2461–2462.
Ryan, D. H., Ravussin, E., Heymsfield, S. (2020). COVID 19 and the Patient with Obesity - The Editors Speak Out. Obesity 28 (5), 847.
Saba, A., Jika, T. (2020). Eastern Cape's PPE shortage endangers healthcare workers. Available at: https://mg.co.za/article/2020-04-23-eastern-capes-ppe-shortage-endangers-healthcare-workers/
SADC (2020). Statement by the SADC Executive Secretary, H.E. Dr Stergomena Lawrence Tax on Covid-19 and Gender Based Violence and Domestic Violence. Available at: https://www.sadc.int/news-events/news/statement-sadc-executive-secretary-he-dr-stergomena-lawrence-tax-covid-19-and-gender-based-violence-and-domestic-violence/.
SAHPRA (2020a). SAHPRA cautions against medicine stockpiling including Chloroquine containing products. Available at: http://www.sahpra.org.za/wp-content/uploads/2020/03/SAHPRA-communique_Chloroquine-Stockpiling_23032020.pdf.
SAHPRA (2020b). SAHPRA STATEMENT: BCG Vaccination and COVID-19 Disease. Available at: http://www.sahpra.org.za/wp-content/uploads/2020/04/SAHPRA-STATEMENT_BCGVaccinations-and-COVID-19.pdf.
Saleem, Z., Godman, B., Hassali, M. A., Hashmi, F. K., Azhar, F., Rehman, I. U. (2019). Point prevalence surveys of health-care-associated infections: a systematic review. Pathog. Global Health 1–15.
Salum, G. A., Rehmenklau, J. F., Csordas, M. C., Pereira, F. P., Castan, J. U., Ferreira, A. B., et al. (2020). Supporting people with severe mental health conditions during the COVID-19 pandemic: considerations for low- and middle-income countries using telehealth case management. Rev. Bras. Psiquiatria.
Sanders, J. M., Monogue, M. L., Jodlowski, T. Z., Cutrell, J. B. (2020). Pharmacologic Treatments for Coronavirus Disease 2019 (COVID-19): A Review. JAMA.
SAMRC. (2020). COVID-19 research - Systematic Reviews to inform Public Health Guidance on COVID-19. Available at: https://www.samrc.ac.za/intramural-research-units/covid-19-research.
SAPC. (2020). South African Pharmacy Council discourages panic-fuelled bulk purchases of essential supplies and medicinal items amid the coronavirus outbreak. Media Statement. 22 March 2020. Available at: https://www.sapc.za.org/Media/Default/Documents/SAPC%20Media%20Statement_Panic-fueled%20purchases.pdf.
Sarma, P., Kaur, H., Kumar, H., Mahendru, D., Avti, P., Bhattacharyya, A., et al. (2020). Virological and clinical cure in COVID-19 patients treated with hydroxychloroquine: A systematic review and meta-analysis. J. Med. Virol. 92 (7), 776–785.
Scavone, C., Brusco, S., Bertini, M., Sportiello, L., Rafaniello, C., Zoccoli, A., et al. (2020). Current pharmacological treatments for COVID-19: what's next? Br. J. Pharmacol.
Schaaf, H. S., du Preez, K., Kruger, M., Solomons, R., Taljaard, J. J., Rabie, H., et al. (2020). Bacille Calmette-Guérin (BCG) vaccine and the COVID-19 pandemic: responsible stewardship is needed. Available at: https://www.theunion.org/news-centre/news/body/IJTLD-0267_Schaaf.pdf.
Schellack, N., Bronkhorst, E., Coetzee, R., Godman, B., Gous, A. G. S., Kolman, S., et al. (2018). SASOCP position statement on the pharmacist's role in antibiotic stewardship 2018. South Afr. J. Infect. Dis. 33 (1), 28–35.
School of Public Health Makerere University (2020). Inside the Makerere Covid-19 Innovation activities. Available at: https://sph.mak.ac.ug/news/inside-makerere-covid-19-innovation-activities.
Schroder, M., Bossert, A., Kersting, M., Aeffner, S., Coetzee, J., Timme, M., et al. (2020). COVID-19 in Africa: outbreak despite interventions? MedRxiv preprint. Available at: https://www.medrxiv.org/content/10.1101/2020.04.24.20077891v1.full.pdf. doi: 10.1101/2020.04.24.20077891.t
Sciama, Y. (2020). Is France's president fueling the hype over an unproven coronavirus treatment? Available at: https://www.sciencemag.org/news/2020/04/france-s-president-fueling-hype-over-unproven-coronavirus-treatment.
Seaton, A. (2020). COVID-19 and its impact on antimicrobial stewardship. Available at: https://revive.gardp.org/covid-19-and-its-impact-on-antimicrobial-stewardship/.
Serwornoo, M., Abrokwah, R. (2020). Ghana: Coronavirus and the media. Available at: https://en.ejo.ch/ethics-quality/ghana-coronavirus-and-the-media.
Shah, M., Sachdeva, M., Dodiuk-Gad, R. P. (2020). COVID-19 and Racial Disparities. J. Am. Acad. Dermatol.
Shepherd, B., van der Mark, N. (2020). Beyond Lockdown: Africa's Options for Responding to COVID-19. Available at: https://www.chathamhouse.org/expert/comment/beyond-lockdown-africa-s-options-responding-covid-19.
Shi, C., Wang, C., Wang, H., Yang, C., Cai, F., Zeng, F., et al. (2020). Clinical observations of low molecular weight heparin in relieving inflammation in COVID-19 patients: A retrospective cohort study. medrxiv. doi: 10.1101/2020.03.28.20046144
Simpson, B. W. (2020). In COVID-19, the Africa CDC Faces Its Greatest Challenge. Available at: https://www.globalhealthnow.org/2020-03/covid-19-3-year-old-africa-cdc-faces-its-greatest-challenge.
Singh, D. R., Sunuwar, D. R., Karki, K., Ghimire, S., Shrestha, N. (2020a). Knowledge and Perception Towards Universal Safety Precautions During Early Phase of the COVID-19 Outbreak in Nepal. J. Community Health, 1–7.
Singh, A. K., Singh, A., Singh, R., Misra, A. (2020b). Hydroxychloroquine in patients with COVID-19: A Systematic Review and meta-analysis. Diabetes Metab. Syndrome 14 (4), 589–596.
Smith, G. (2020). Stamping out misinformation in Kenya's COVID-19 fight - Volunteers and activists work to diffuse spread of fake information, false 'remedies' as Kenya steps up pandemic battle. Available at: https://www.aljazeera.com/news/2020/04/stamping-misinformation-kenya-covid-19-fight-200424195805081.html.
So-Armah, K., Freiberg, M. S. (2018). HIV and Cardiovascular Disease: Update on Clinical Events, Special Populations, and Novel Biomarkers. Curr. HIV/AIDS Rep. 15 (3), 233–244.
South African Government (2020a). President Ramaphosa launches the Africa Medical Supplies Platform to help fight COVID-19 Coronavirus Pandemic. Available at: https://www.gov.za/speeches/president-ramaphosa-launches-africa-medical-supplies-platform-help-fight-covid-19.
South African Government (2020b). Regulations and Guidelines - Coronavirus Covid-19. Available at: https://www.gov.za/coronavirus/guidelines.
South African Government. (2020c). President Cyril Ramaphosa: Additional Coronavirus COVID-19 economic and social relief measures. 21 April 2020. Available at: https://www.gov.za/speeches/president-cyril-ramaphosa-additional-coronavirus-covid-19-economic-and-social-relief.
South African Government (2020d). Social grants - Coronavirus COVID-19. Available at: https://www.gov.za/coronavirus/socialgrants.
Southern African Health Technology Assessment Society (SAHTAS) (2019). http://www.htasa.org.za/.
Sterne, J. A. C., Murthy, S., Diaz, J. V., Slutsky, A. S., Villar, J., Angus, D., et al. (2020). Association Between Administration of Systemic Corticosteroids and Mortality Among Critically Ill Patients With COVID-19: A Meta-analysis. Jama (EPrint).
Takyi-Boadu, C. (2020). Government Officials Donate 3 months Salaries to Help Fight Covid-19. Available at: https://dailyguidenetwork.com/government-officials-donate-3months-salaries-to-help-fight-covid-19/.
Tamam, L., Yerdelen, D., Ozpoyraz, N. (2003). Psychosis associated with interferon alfa therapy for chronic hepatitis B. Ann. Pharmacother. 37 (3), 384–387.
Tang, N., Bai, H., Chen, X., Gong, J., Li, D., Sun, Z. (2020). Anticoagulant treatment is associated with decreased mortality in severe coronavirus disease 2019 patients with coagulopathy. J. Thromb. Haemostasis 18 (5), 1094–1099.
Tarkang, E. E. (2020). The fight against COVID-19 in sub-Saharan Africa-a threat to the continuous management of HIV patients: application of the action areas of the Ottawa charter for health promotion. PAMJ 35 (2), 25. doi: 10.11604/pamj.supp.2020.35.2.23224
Tembo, L. (2020). Coping with school closures during the COVID-19 pandemic - Keeping children learning is a priority. Available at: https://www.unicef.org/malawi/stories/coping-school-closures-during-covid-19-pandemic.
Thai, P. Q., Rabaa, M. A., Luong, D. H., Tan, D. Q., Quang, T. D., Quach, H.-L., et al. (2020). The first 100 days of SARS-CoV-2 control in Vietnam. Clin Infect. Dis. doi: 10.1093/cid/ciaa1130
The East African (2020). Seven die, 134 treated after cholera outbreak in northern Kenya. Available at: https://www.theeastafrican.co.ke/scienceandhealth/Cholera-kills-7-in-northern-Kenya/3073694-5538830-c21ggo/index.html.
The Guardian. (2020a). High hopes' drug for Covid-19 treatment failed in full trial. April 2020. Available at: https://www.msn.com/en-gb/news/coronavirus/high-hopes-drug-for-covid-19-treatment-failed-in-full-trial/ar-BB136z6g?ocid=spartandhp.
The Guardian. (2020b). Coronavirus: world's biggest trial of drug to treat Covid-19 begins in UK. Available at: https://www.theguardian.com/world/2020/apr/17/world-biggest-drug-trial-covid-19-uk.
The Lancet Editorial. (2020). Expression of concern: Hydroxychloroquine or chloroquine with or without a macrolide for treatment of COVID-19: a multinational registry analysis. Lancet (London England) 395 (10240), e102–e10e.
The Reportor. (2020). Lesotho now doing own COVID-19 testing. 26 June 2020. Available at: https://www.pressreader.com/lesotho/the-reporter/20200626/281500753517045.
The World Bank (2020a). World Bank Group Supports Ghana's COVID-19 Response. Available at: https://www.worldbank.org/en/news/press-release/2020/04/02/world-bank-group-supports-ghanas-covid-19-response.
The World Bank (2020b). Kenya Receives $50 Million World Bank Group Support to Address COVID-19 Pandemic. Available at: https://www.worldbank.org/en/news/press-release/2020/04/02/kenya-receives-50-million-world-bank-group-support-to-address-covid-19-pandemic.
Thornicroft, G., Rose, D., Kassam, A., Sartorius, N. (2007). Stigma: ignorance, prejudice or discrimination? Br. J. Psychiatry J. Ment. sci. 190, 192–193.
Thornton, J. (2020). Covid-19: Keep essential malaria services going during pandemic, urges WHO. BMJ 369, m1637.
Tih, F. (2020). African countries ease COVID-19 lockdown restrictions - Governments say there is need to resume economic activities with imperative to contain virus. Available at: https://www.aa.com.tr/en/africa/african-countries-ease-covid-19-lockdown-restrictions/1827900.
Tilangi, P., Desai, D., Khan, A., Soneja, M. (2020). Hydroxychloroquine prophylaxis for high-risk COVID-19 contacts in India: a prudent approach. Lancet Infect. Dis.
Times of Swaziland (2020). Over 100 Companies to Lay Off Staff. Available at: http://www.times.co.sz/news/127933-over-100-companies-to-lay-off-staff.html.
Tomlinson, C. (2020). Covid-19: Is South Africa prepared for medicine shortages? (City Press). Available at: https://city-press.news24.com/News/covid-19-is-south-africa-prepared-for-medicine-shortages-20200316-2.
Tomazini, B. M., Maia, I. S., Cavalcanti, A. B., Berwanger, O., Rosa, R. G., Veiga, V. C., et al. (2020). Effect of Dexamethasone on Days Alive and Ventilator-Free in Patients With Moderate or Severe Acute Respiratory Distress Syndrome and COVID-19: The CoDEX Randomized Clinical Trial. Jama (EPrint).
Toniati, P., Piva, S., Cattalini, M., Garrafa, E., Regola, F., Castelli, F., et al. (2020). Tocilizumab for the treatment of severe COVID-19 pneumonia with hyperinflammatory syndrome and acute respiratory failure: A single center study of 100 patients in Brescia, Italy. Autoimmun. Rev. 19 (7), 102568.
TradingEconomics (2020). Swaziland Interest Rate. Available at: https://tradingeconomics.com/swaziland/interest-rate.
Tu, Y. F., Chien, C. S., Yarmishyn, A. A., Lin, Y. Y., Luo, Y. H., Lin, Y. T., et al. (2020). A Review of SARS-CoV-2 and the Ongoing Clinical Trials. Int. J. Mol. Sci. 21 (7), 1–19.
UK Department of Health and Social Care. (2020). Clinical trial approved to help the NHS treat COVID-19 patients using plasma. April 2020. Available at: https://www.gov.uk/government/news/clinical-trial-approved-to-help-the-nhs-treat-covid-19-patients-using-plasma.
UK Medicines & Healthcare Products Regulatory Agency. EAMS 11972/0001 Remdesivir 100 mg powder for concentrate for solution for infusion. May 2020. Available at: https://www.gov.uk/government/publications/early-access-to-medicines-scheme-eams-scientific-opinion-remdesivir-in-the-treatment-of-patients-hospitalised-with-suspected-or-laboratory-confirme/treatment-protocol-for-healthcare-professionals_eams-119720001-remdesivir-100-mg-powder-for-concentrate-for-solution-for-infusion.
UN News (2020). Vaccine bottlenecks from COVID lockdown put children's lives at stake: UNICEF. Available at: https://news.un.org/en/story/2020/05/1063002.
UNAIDS. (2019) Global HIV & AIDS statistics — 2019 fact sheet. Available at: https://www.unaids.org/sites/default/files/media_asset/UNAIDS_FactSheet_en.pdf.
Ung, C. O. L. (2020). Community pharmacist in public health emergencies: Quick to action against the coronavirus 2019-nCoV outbreak. Res. Soc. Adm. Pharm. 16 (4), 583–586.
UNHCR (2020). Across West Africa dual challenge of conflict and coronavirus threatens millions of people. Available at: https://www.unhcr.org/uk/news/latest/2020/4/5e99b5074/across-west-africa-dual-challenge-conflict-coronavirus-threatens-millions.html.
UNICEF Malawi. (2020) UNICEF Malawi Supply Update on Coronavirus Disease (COVID-19) Response - Prepositioned and locally procured supplies provide critical input to Malawi response in combating COVID-19. Available at: https://www.unicef.org/malawi/coronavirus-disease-covid-19/unicef-malawi-supply-update-coronavirus-disease-covid-19-response.
UNICEF South Africa (2020). Immunization against vaccine-preventable diseases is essential to protect children African Vaccination Week 2020 focuses on the importance of immunization in a time of COVID-19. Available at: https://www.unicef.org/southafrica/stories/immunization-against-vaccine-preventable-diseases-essential-protect-children.
UNICEF (2020). COVID-19: Gavi and UNICEF to secure equipment and diagnostics for lower-income countries. Available at: https://www.unicef.org/press-releases/covid-19-gavi-and-unicef-secure-equipment-and-diagnostics-lower-income-countries.
United Nations Africa Renewal. (2020) Coronavirus Updates and Resources. 7 May 2020. Available at: https://www.un.org/africarenewal/news/coronavirus/new-who-estimates-190-000-people-could-die-covid-19-africa-if-not-controlled.
United Nations Economic Commission for Africa (2020a). UN sets up regional knowledge hub to fight COVID-19. Available at: https://www.uneca.org/stories/un-sets-regional-knowledge-hub-fight-covid-19.
United Nations Economic Commission for Africa (2020b). COVID-19 in Africa: Protecting Lives and Economies. Available at: https://www.uneca.org/sites/default/files/PublicationFiles/eca_covid_report_en_24apr_web1.pdf.
United Nations Malawi (2020). COVID-19 Update. Available at: https://reliefweb.int/sites/reliefweb.int/files/resources/Malawi-COVID-19-Situation-Update-03.04.20.pdf.
United Nations (2020a). Policy Brief: COVID-19 and the Need for Action on Mental Health. Available at: https://www.un.org/sites/un2.un.org/files/un_policy_brief-covid_and_mental_health_final.pdf.
United Nations (2020b). Policy Brief: Impact of COVID-19 in Africa. Available at: https://www.un.org/sites/un2.un.org/files/sg_policy_brief_on_covid-19_impact_on_africa_may_2020.pdf.
University of Ghana News Release (2020). University of Ghana (UG) Scientists Sequence Genomes of Novel Coronavirus. Available at: https://www.ug.edu.gh/news/news-release-university-ghana-scientists-sequence-genomes-novel-coronavirus.
University of Nairobi (2020). UoN Ventilators, ready for production model. Available at: https://www.uonbi.ac.ke/news/uon-ventilators-ready-production-model.
US Food and Drug Administration (2020). Emergency Use Authorization (EUA) for emergency use of remdesivir for the treatment of hospitalized coronavirus disease (COVID-19) patients. Available at: https://www.fda.gov/media/137564/download.
US National Library of Medicine - ClinicalTrials.gov (2020a). Impact of Nasal Saline Irrigations on Viral Load in Patients With COVID-19. Available at: https://clinicaltrials.gov/ct2/show/NCT04347538.
US National Library of Medicine - ClinicalTrials.gov (2020b). Gargling and Nasal Rinses to Reduce Oro- and Nasopharyngeal Viral Load in Patients With COVID-19. Available at: https://clinicaltrials.gov/ct2/show/NCT04344236.
US National Library of Medicine. (2020). ClinicalTrials.gov. Available at: https://clinicaltrials.gov/ct2/results?cond=COVID-19&cntry=EG&age_v=&gndr=&type=Intr&rslt=&Search=Apply.
van den Heever, A. (2020). Projections on SA health system and whether there are enough hospital beds to cope. Available at: https://www.dailymaverick.co.za/article/2020-03-16-projections-on-sa-health-system-and-whether-there-enough-hospital-beds-to-cope/.
Vardavas, C. I., Nikitara, K. (2020). COVID-19 and smoking: A systematic review of the evidence. Tobacco Induced Dis. 18, 20.
Vella Bonanno, P., Bucsics, A., Simoens, S., Martin, A. P., Oortwijn, W., Gulbinovic, J., et al. (2019). Proposal for a regulation on health technology assessment in Europe - opinions of policy makers, payers and academics from the field of HTA. Expert Rev. Pharmacoecon. Outc. Res. 19 (3), 251–261.
Vellingiri, B., Jayaramayya, K., Iyer, M., Narayanasamy, A., Govindasamy, V., Giridharan, B., et al. (2020). COVID-19: A promising cure for the global panic. Sci. Total Environ. 725, 138277.
Wang, C., Pan, R., Wan, X., Tan, Y., Xu, L., Ho, C. S., et al. (2020a). Immediate Psychological Responses and Associated Factors during the Initial Stage of the 2019 Coronavirus Disease (COVID-19) Epidemic among the General Population in China. Int. J. Environ. Res. Public Health 17 (5) 1–25.
Wang, C., Pan, R., Wan, X., Tan, Y., Xu, L., McIntyre, R. S., et al. (2020b). A longitudinal study on the mental health of general population during the COVID-19 epidemic in China. Brain Behav. Immun. 87, 40–48.
Wang, C. J., Ng, C. Y., Brook, R. H. (2020). Response to COVID-19 in Taiwan: Big Data Analytics, New Technology, and Proactive Testing. JAMA.
Wang, Y., Zhang, D., Du, G., Du, R., Zhao, J., Jin, Y., et al. (2020). Remdesivir in adults with severe COVID-19: a randomised, double-blind, placebo-controlled, multicentre trial. Lancet 395 (10236), 1569–1578.
Warrington, T. P., Bostwick, J. M. (2006). Psychiatric adverse effects of corticosteroids. Mayo Clin. Proc. 81 (10), 1361–1367.
WHO Regional Office Africa. (2020a). COVID-19 - Situation Update for the WHO African Region - 1 July 2020. External Situation Report 18. Available at: https://apps.who.int/iris/bitstream/handle/10665/332929/SITREP_COVID-19_WHOAFRO_20200701-eng.pdf.
WHO Regional Office Africa (2020b). COVID-19 in the WHO African Region. Available at: https://www.afro.who.int/health-topics/coronavirus-covid-19.
WHO Regional Office Africa. (2020c). African countries move from COVID-19 readiness to response as many confirm cases. 29 April 2020. Available at: https://www.afro.who.int/health-topics/coronavirus-covid-19.
WHO Regional Office Africa. (2020d). COVID-19 - External Situation Report 9. 29 April 2020. Available at: https://apps.who.int/iris/bitstream/handle/10665/331935/SITREP_COVID-19_WHOAFRO_20200429-eng.pdf.
WHO. Coronavirus disease (COVID-19) Situation Report – 151. Available at: https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200619-covid-19-sitrep-151.pdf?sfvrsn=8b23b56e_2.
WHO (2019a). Global Tuberculosis Report Executive Summary. Available at: https://www.who.int/tb/publications/global_report/tb19_Exec_Sum_15October2019.pdf?ua=1.
WHO (2019b). Global Tuberculosis Report (Full). Available at: https://apps.who.int/iris/bitstream/handle/10665/329368/9789241565714-eng.pdf?ua=1.
WHO. (2019c) World Malaria Report 2019. Available at: https://www.who.int/publications-detail/world-malaria-report-2019.
WHO (2020a). Coronavirus disease (COVID-19) Situation Report – 163. Available at: https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200701-covid-19-sitrep-163.pdf?sfvrsn=c202f05b_2.
WHO (2020b). Modes of transmission of virus causing COVID-19: implications for IPC precaution recommendations. Available at: https://www.who.int/news-room/commentaries/detail/modes-of-transmission-of-virus-causing-covid-19-implications-for-ipc-precaution-recommendations.
WHO. (2020c) COVID-19 Strategy update. Available at: https://www.who.int/docs/default-source/coronaviruse/covid-strategy-update-14april2020.pdf?sfvrsn=29da3ba.
WHO (2020d). COVID-19 Strategic Preparedness and Response Plan - OPERATIONAL PLANNING GUIDELINES TO SUPPORT COUNTRY PREPAREDNESS AND RESPONSE. Available at: https://www.who.int/docs/default-source/coronaviruse/covid-19-sprp-unct-guidelines.pdf.
WHO (2020e). WHO discontinues hydroxychloroquine and lopinavir/ritonavir treatment arms for COVID-19. 4 July 2020. Available at: https://www.who.int/news-room/detail/04-07-2020-who-discontinues-hydroxychloroquine-and-lopinavir-ritonavir-treatment-arms-for-covid-19.
WHO (2020f). Bacille Calmette-Guérin (BCG) vaccination and COVID-19 - Scientific Brief. Available at: https://www.who.int/news-room/commentaries/detail/bacille-calmette-gu%C3%A9rin-(bcg)-vaccination-and-covid-19.
WHO (2020g). Mental health and psychosocial considerations during the COVID-19 outbreak. Available at: https://www.who.int/publications-detail/WHO-2019-nCoV-MentalHealth-2020.1.
WHO. (2020h) WHO Director-General's opening remarks at the media briefing on COVID-19 - 25 May 2020. Available at: https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19—25-may-2020.
WHO (2020i). Emergency Ministerial meeting on COVID-19 organized by the African Union and the Africa Centres for Disease Control and Prevention. Available at: https://www.who.int/dg/speeches/detail/emergency-ministerial-meeting-on-covid-19-organized-by-the-african-union-and-the-africa-centres-for-disease-control-and-prevention.
WHO (2020j). Coronavirus disease (COVID-19) pandemic. Available at: https://www.who.int/emergencies/diseases/novel-coronavirus-2019.
WHO (2020k). Launch of the Lomé Initiative. Available at: https://www.who.int/dg/speeches/detail/launch-of-the-lom%C3%A9-initiative.
WHO (2020l). “Solidarity” clinical trial for COVID-19 treatments. Available at: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/global-research-on-novel-coronavirus-2019-ncov/solidarity-clinical-trial-for-covid-19-treatments.
WHO (2020m). Ebola virus disease – Democratic Republic of the Congo. Available at: https://www.who.int/csr/don/23-April-2020-ebola-drc/en/.
WHO (2020n). Protecting lifesaving immunization services during COVID-19: New guidance from WHO. Available at: https://www.who.int/immunization/news_guidance_immunization_services_during_COVID-19/en/.
Wilkinson, L., Grimsrud, A. (2020). The time is now: expedited HIV differentiated service delivery during the COVID-19 pandemic. J. Int. AIDS Soc. 23, e25503.
Williams, F. M. K., Freidin, M. B., Mangino, M., Couvreur, S., Visconti, A., Bowyer, R. C. E., et al. (2020). Self-reported symptoms of covid-19 including symptoms most predictive of SARS-CoV2 infection, are heritable. MedRxiv preprint. Available at: https://www.medrxiv.org/content/10.1101/2020.04.22.20072124v2.full.pdf. doi: 10.1101/2020.04.22.20072124
Wits University. (2020a) The first Covid-19 vaccine trial in South Africa begins. 23 June 2020. Available at: https://www.wits.ac.za/covid19/covid19-news/latest/the-first-covid-19-vaccine-trial-in-south-africa-begins.html.
Wits University (2020b). Wits engineers make face shields to protect healthcare workers. Available at: https://www.wits.ac.za/covid19/covid19-news/latest/wits-engineers-make-face-shields-to-protect-healthcare-workers.html.
Woldesemayat, E. M. (2020). Chronic Diseases Multimorbidity among Adult People Living with HIV at Hawassa University Comprehensive Specialized Hospital, Southern Ethiopia. Int. J. Chronic Dis. 2020, 2190395.
World Bank (2020). South Sudan: World Bank Provides $7.6 Million in Support of Coronavirus Emergency Response. Available at: https://www.worldbank.org/en/news/press-release/2020/04/09/south-sudan-world-bank-provides-76-million-in-support-of-coronavirus-emergency-response.
World Food Programme (2020). COVID-19 will double number of people facing food crises unless swift action is taken. Available at: https://www.wfp.org/news/covid-19-will-double-number-people-facing-food-crises-unless-swift-action-taken.
World Health Organisation Europe. (2020) Health Systems Respond to COVID-19 Technical Guidance 2 - Creating surge capacity for acute and intensive care - Recommendations for the WHO European Region . Available at: http://www.euro.who.int/:data/assets/pdf_file/0006/437469/TG2-CreatingSurgeAcuteICUcapacity-eng.pdf.
World Health Organisation (2019). Global Health Observatory data repository. Number of people (all ages) living with HIV - Estimates by WHO region. Available at: https://apps.who.int/gho/data/view.main.22100WHO?lang=en.
World Health Organisation. (2020a). Naming the coronavirus disease (COVID-19) and the virus that causes it. Available at: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/technical-guidance/naming-the-coronavirus-disease-(covid-2019)-and-the-virus-that-causes-it.
World Health Organisation. (2020b). Operational considerations for case management of COVID-19 in health facility and community: interim guidance, 19 March 2020. Available at: https://apps.who.int/iris/handle/10665/331492.
World Health Organisation (2020c). The potential impact of health service disruptions on the burden of malaria: a modelling analysis for countries in sub-Saharan Africa. Available at: https://apps.who.int/iris/bitstream/handle/10665/331845/9789240004641-eng.pdf?sequence=1&isAllowed=y.
World Health Organization. (2020d) Guiding principles for immunization activities during the COVID-19 pandemic: interim guidance, 26 March 2020. Available at: https://apps.who.int/iris/handle/10665/331590.
World Health Organisation (2020e). Medical Product Alert N°4/2020 - Falsified chloroquine products circulating in the WHO region of Africa. Available at: https://www.who.int/docs/default-source/essential-medicines/drug-alerts20/drug-alert-4/n-4-2020-falsified-chloroquine-en.pdf?sfvrsn=c4354802_6.
World Health Organisation (2020f). Coronavirus disease (COVID-19) advice for the public: Myth busters. Available at: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public/myth-busters.
Worldometer (2020). African Countries by population. Available at: https://www.worldometers.info/population/countries-in-africa-by-population/.
Wu, Z., McGoogan, J. M. (2020). Characteristics of and Important Lessons From the Coronavirus Disease 2019 (COVID-19) Outbreak in China: Summary of a Report of 72 314 Cases From the Chinese Center for Disease Control and Prevention. JAMA 323 (13), 123942.
Wu, F., Wang, A., Liu, M., Wang, Q., Chen, J., Xia, S., et al. (2020). Neutralizing antibody responses to SARS-CoV-2 in a COVID-19 recovered patient cohort and their implications. MedRxiv preprint. Available at: https://www.medrxiv.org/content/10.1101/2020.03.30.20047365v2.full.pdf. doi: 10.1101/2020.03.30.20047365
Xiang, Y. T., Yang, Y., Li, W., Zhang, L., Zhang, Q., Cheung, T., et al. (2020). Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. Lancet Psychiatry 7 (3), 228–229.
Xinhua (2020a). Uganda braces for economic impact of COVID-19. Available at: http://www.xinhuanet.com/english/2020-03/20/c_138898637.htm.
Xinhua (2020b). China's Jack Ma gives Zambia COVID-19 medical supplies. Available at: https://www.focac.org/eng/zfgx_4/jmhz/t1760745.htm.
Xu, X., Ong, Y. K., Wang, D. Y. (2020). Role of adjunctive treatment strategies in COVID-19 and a review of international and national clinical guidelines. Mil. Med. Res. 7 (1), 22 .
Yang, Y. (2020). Use of herbal drugs to treat COVID-19 should be with caution. Lancet 395 (10238), 1689–1690.
Yao, H., Chen, J. H., Xu, Y. F. (2020). Patients with mental health disorders in the COVID-19 epidemic. Lancet Psychiatry 7 (4), e21.
Zhang, C., Wu, Z., Li, J. W., Zhao, H., Wang, G. Q. (2020). The cytokine release syndrome (CRS) of severe COVID-19 and Interleukin-6 receptor (IL-6R) antagonist Tocilizumab may be the key to reduce the mortality. Int. J. Antimicrob. Agents 105954, 1–6.
Zhang, L., Yu, J., Zhou, Y., Shen, M., Sun, L. (2020). Becoming a Faithful Defender: Traditional Chinese Medicine against Coronavirus Disease 2019 (COVID-19). Am. J. Chin. Med. 48 (4), 763–777.
Zheng, Z., Peng, F., Xu, B., Zhao, J., Liu, H., Peng, J., et al. (2020). Risk factors of critical & mortal COVID-19 cases: A systematic literature review and meta-analysis. J. Infection.
Zheng, S. Q., Yang, L., Zhou, P. X., Li, H. B., Liu, F., Zhao, R. S. (2020). Recommendations and guidance for providing pharmaceutical care services during COVID-19 pandemic: A China perspective. Res. Soc. Adm. Pharm.
Zhong, H., Wang, Y., Zhang, Z. L., Liu, Y. X., Le, K. J., Cui, M., et al. (2020). Efficacy and safety of current therapeutic options for COVID-19 - lessons to be learnt from SARS and MERS epidemic: A systematic review and meta-analysis. Pharmacol. Res. 157, 104872.
Zhong, B. L., Luo, W., Li, H. M., Zhang, Q. Q., Liu, X. G., Li, W. T., et al. (2020). Knowledge, attitudes, and practices towards COVID-19 among Chinese residents during the rapid rise period of the COVID-19 outbreak: a quick online cross-sectional survey. Int. J. Biol. Sci. 16 (10), 1745–1752.
Zhou, F., Yu, T., Du, R., Fan, G., Liu, Y., Liu, Z., et al. (2020). Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet 395 (10229), 1054–1062.
Zhu, Z., Lu, Z., Xu, T., Chen, C., Yang, G., Zha, T., et al. (2020). Arbidol monotherapy is superior to lopinavir/ritonavir in treating COVID-19. J. Infection 81 (1), e21–ee3.
Zurek, K. (2020). COVID-19: President Akufo-Addo lifts partial lockdown effective Monday. Available at: https://www.graphic.com.gh/news/general-news/prez-akufo-addo-covid-update-7.html.
Keywords: COVID-19, Africa, prevalence, treatment, misinformation, health policy, unintended consequences, review
Citation: Ogunleye OO, Basu D, Mueller D, Sneddon J, Seaton RA, Yinka-Ogunleye AF, Wamboga J, Miljković N, Mwita JC, Rwegerera GM, Massele A, Patrick O, Niba LL, Nsaikila M, Rashed WM, Hussein MA, Hegazy R, Amu AA, Boahen-Boaten BB, Matsebula Z, Gwebu P, Chirigo B, Mkhabela N, Dlamini T, Sithole S, Malaza S, Dlamini S, Afriyie D, Asare GA, Amponsah SK, Sefah I, Oluka M, Guantai AN, Opanga SA, Sarele TV, Mafisa RK, Chikowe I, Khuluza F, Kibuule D, Kalemeera F, Mubita M, Fadare J, Sibomana L, Ramokgopa GM, Whyte C, Maimela T, Hugo J, Meyer JC, Schellack N, Rampamba EM, Visser A, Alfadl A, Malik EM, Malande OO, Kalungia AC, Mwila C, Zaranyika T, Chaibva BV, Olaru ID, Masuka N, Wale J, Hwenda L, Kamoga R, Hill R, Barbui C, Bochenek T, Kurdi A, Campbell S, Martin AP, Phuong TNT, Thanh BN and Godman B (2020) Response to the Novel Corona Virus (COVID-19) Pandemic Across Africa: Successes, Challenges, and Implications for the Future. Front. Pharmacol. 11:1205. doi: 10.3389/fphar.2020.01205
Received: 02 June 2020; Accepted: 23 July 2020;
Published: 11 September 2020.
Edited by:
Sam Salek, University of Hertfordshire, United KingdomCopyright © 2020 Ogunleye, Basu, Mueller, Sneddon, Seaton, Yinka-Ogunleye, Wamboga, Miljković, Mwita, Rwegerera, Massele, Patrick, Niba, Nsaikila, Rashed, Hussein, Hegazy, Amu, Boahen-Boaten, Matsebula, Gwebu, Chirigo, Mkhabela, Dlamini, Sithole, Malaza, Dlamini, Afriyie, Asare, Amponsah, Sefah, Oluka, Guantai, Opanga, Sarele, Mafisa, Chikowe, Khuluza, Kibuule, Kalemeera, Mubita, Fadare, Sibomana, Ramokgopa, Whyte, Maimela, Hugo, Meyer, Schellack, Rampamba, Visser, Alfadl, Malik, Malande, Kalungia, Mwila, Zaranyika, Chaibva, Olaru, Masuka, Wale, Hwenda, Kamoga, Hill, Barbui, Bochenek, Kurdi, Campbell, Martin, Phuong, Thanh and Godman. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Brian Godman, YnJpYW4uZ29kbWFuQHN0cmF0aC5hYy51aw==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.