- 1Pediatric Pharmacology and Pharmacometrics, University of Basel Children’s Hospital, Basel, Switzerland
- 2Division of Clinical Pharmacology and Toxicology, University Hospital Basel, Basel, Switzerland
- 3National Poisons Information Centre, Tox Info Suisse, Associated Institute of the University of Zurich, Zurich, Switzerland
- 4Institute of Clinical Chemistry, University Hospital Zürich, Zurich, Switzerland
- 5Department of Internal Medicine, Hirslanden Klinik St. Anna, Lucerne, Switzerland
- 6Transplantation Immunology and Nephrology, University Hospital Basel, Basel, Switzerland
We present the case of a kidney transplant patient (Cockroft-Gault estimated creatinine clearance 14 ml/min) who was inadvertently eight-fold overdosed with a single dose of 500 mg intravenous ganciclovir. To prevent the immunosuppressed patient from being exposed to severe risks of prolonged ganciclovir overdosing, including potentially fatal bone marrow suppression and severe neurotoxicity, the patient was treated with hemodiafiltration (HDF) to enhance drug elimination. Since the product label reports a 50% decrease of ganciclovir plasma concentrations after intermittent hemodialysis (HD), two HDF sessions were considered necessary to achieve a ≥75% elimination of the drug by precaution, despite targeted intense HDF prescription. Ganciclovir plasma concentration data were obtained during both HDF sessions and were analyzed retrospectively. Pharmacokinetic analysis revealed that prescribed HDF successfully decreased drug plasma concentrations by ≥90%. This ganciclovir reduction ratio matched the urea reduction ratio achieved (≥92%). Model-based assessment of ganciclovir dialysis clearance (estimated to be 445 ml/min), accounting for its two-compartmental kinetics, was higher than urea dialysis clearance (estimated to be 310 ml/min). This suggests potential relevant accumulation of ganciclovir into blood cells, at least in this patient after overdosing. The amount (fraction) of drug removed by 1st HDF was estimated to 269 mg (93% of total amount of 288 mg eliminated during the 1st HDF session; estimated amount in the body prior to 1st HDF: 380 mg). A literature review was performed to summarize and systematically compare available information on ganciclovir elimination during intermittent renal replacement therapy. In conclusion, the high ganciclovir HDF clearance measured in our patient largely exceeded previously reported elimination during HD, meaning that HDF prescription was highly efficient in the present case, and that a second HDF session might not have been necessary. This finding may be considered to guide renal replacement therapy in the scope of drug overdosing. It may also be evaluated for ganciclovir dose adjustment in patients on chronic HD or HDF with high small solute clearance, since a strong correlation between ganciclovir and urea elimination efficiency was observed.
Background
Active cytomegalovirus (CMV) infection and disease is a major and common complication in solid organ transplant recipients and is associated with an increased risk of all types of infections, graft loss, and with decreased survival. Intravenous ganciclovir is an antiviral agent of choice for prevention and treatment of CMV infections in this population (Kotton et al., 2018). It is a nucleoside analogue that requires intracellular activation by phosphorylation via viral and cellular kinases. The active triphosphate derivative acts as an inhibitor of viral DNA polymerases and shows a long intra-cellular half-life (~16.5h) compared to plasma half-life of the unphosphorylated parent drug (2–4 h in patients with normal renal function) (Scott et al., 2004).
Ganciclovir is a small molecule (molecular weight 255.2 Da) with low protein binding (2%) and a small volume of distribution (0.54–0.87 l/kg). It is mainly (>90%) cleared renally by glomerular filtration and active tubular secretion (Cymevene Swiss Product Information., ). Hence, dose adjustment in renal impairment is necessary, with the elimination half-life of ganciclovir being prolonged up to >10-fold in patients with renal failure (30 h in patients with endstage renal disease) (Lake et al., 1988). Pharmacological properties suggest efficient elimination by hemodialysis (HD) (diffusive dialysis clearance) and hemodiafiltration (HDF) (by both diffusive and convective clearance) (Gotta et al., 2017; Gotta et al., 2020). The manufacturer states that one HD session decreases ganciclovir plasma concentrations by approximately 50% and suggests considering HD to treat overdosing. Indeed, cases of fatal bone marrow suppression have been reported in patients with renal failure who were accidentally overdosed due to omission of dose adjustment according to renal function (Ar et al., 2009). Under therapeutic doses, neutropenia is a common side effect occurring in approximately one third of patients, however in this setting, it is mostly reversible. Further severe adverse reactions associated with overdose may include neurotoxicity (confusion, hallucinations, seizures, coma), acute renal failure, and hepatitis (Cymevene Swiss Product Information., ).
We present a case of a kidney transplant patient with an estimated creatinine clearance of 14 ml/min (Cockroft-Gault) who accidentally received an eight-fold overdose with a single dose of 500 mg ganciclovir and who was treated with HDF to enhance drug elimination. According to available literature two HDF sessions were performed to ensure an 75% elimination of the drug. Ganciclovir plasma concentration data obtained during HDF and analyzed retrospectively revealed that the first HDF session successfully decreased drug plasma concentration by 92%, suggesting that a second HDF session might not have been necessary.
We report our case according to the EQUATOR (Enhancing the QUAlity and Transparency Of health Research) network recommended guidelines for case studies on extracorporeal treatments in poisonings (Lavergne et al., 2014).
Case Presentation
A 70-year old woman, who received a deceased donor renal transplant in 2017, was treated with ganciclovir for CMV disease with ulcerative esophagitis. In this patient weighing 44 kg with an estimated creatinine clearance of 14 ml/min ganciclovir was started at a reduced dose of 65 mg i.v. 22 months after transplantation. At this time the patient was under immunosuppressive therapy with tacrolimus and prednisolone, whereas mycophenolate mofetil was paused due to intermitted neutropenia. Eleven days after start of ganciclovir treatment, the patient received inadvertently an overdose of ganciclovir with a single dose of 500 mg.
To prevent the immunosuppressed patient from being exposed to severe risks of prolonged ganciclovir overdosing, a first session of intermittent post-dilution HDF with standard blood and dialysate flow (Table 1) and high ultrafiltration (34 L per 4 h session) was started 5 h after recognizing the dosing error. Using a dialysate containing 4 mmol/L potassium and additional administration of potassium phosphate (30 mmol over 4 h) successfully prevented hypokalemia and hypophosphatemia despite highly intense HDF.
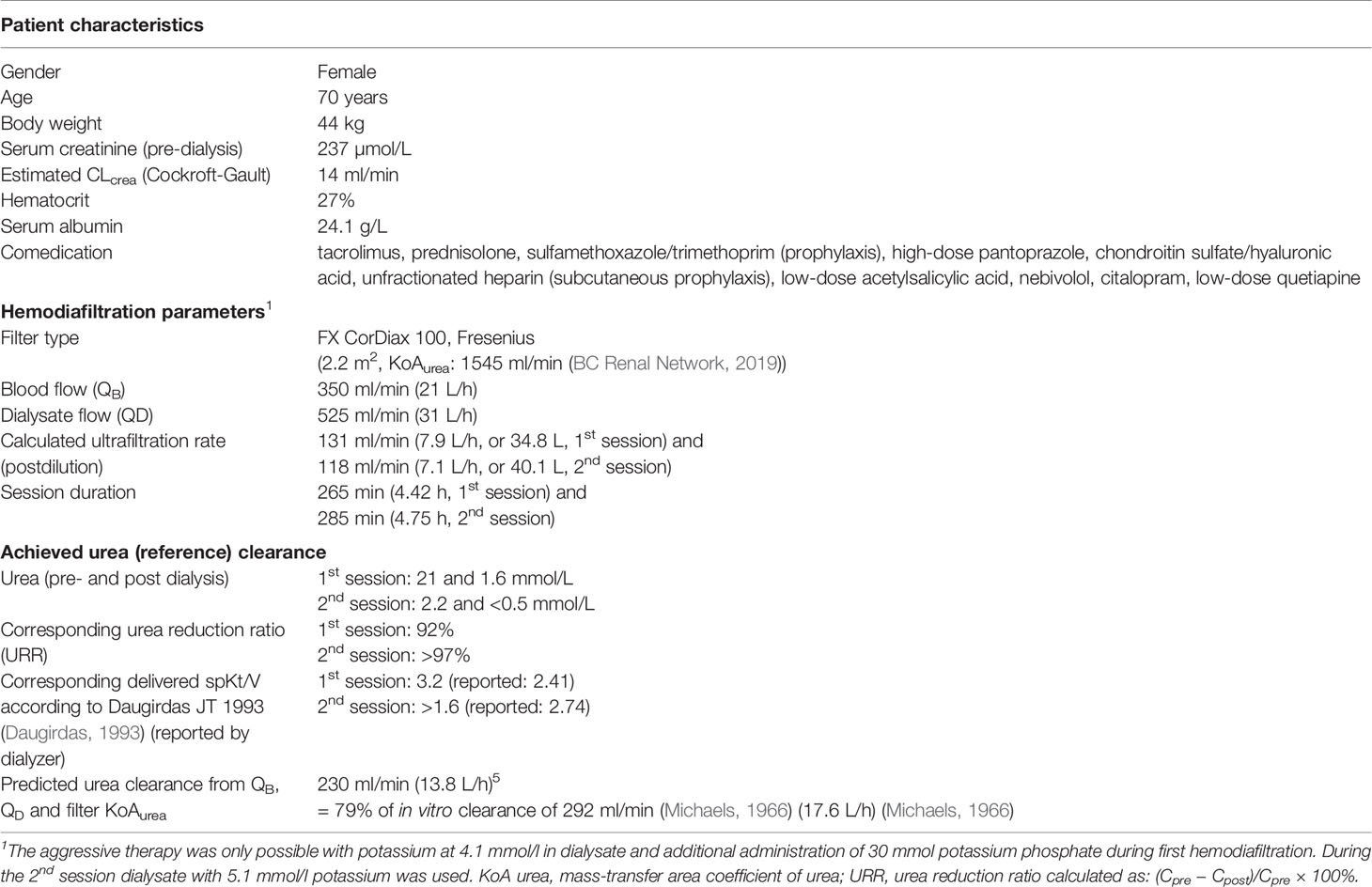
A complete summary of patient characteristics, concomitant drug treatments, dialysis prescription, and efficiency in terms of small molecule clearance (measured by urea clearance) is given in Table 1.
Written informed consent was obtained from the patient for publication of her case.
Pharmacokinetic Sampling and Calculated Kinetic Parameters
Plasma samples for pharmacokinetic analysis were taken before, during and after the two HDF sessions at in total eight time points. Paired pre- and post-filter concentration samples (Cpre-filter and Cpost-filter) were taken at three time points to calculate the extraction ratio (ER) (Table 2A, Figure 1A):
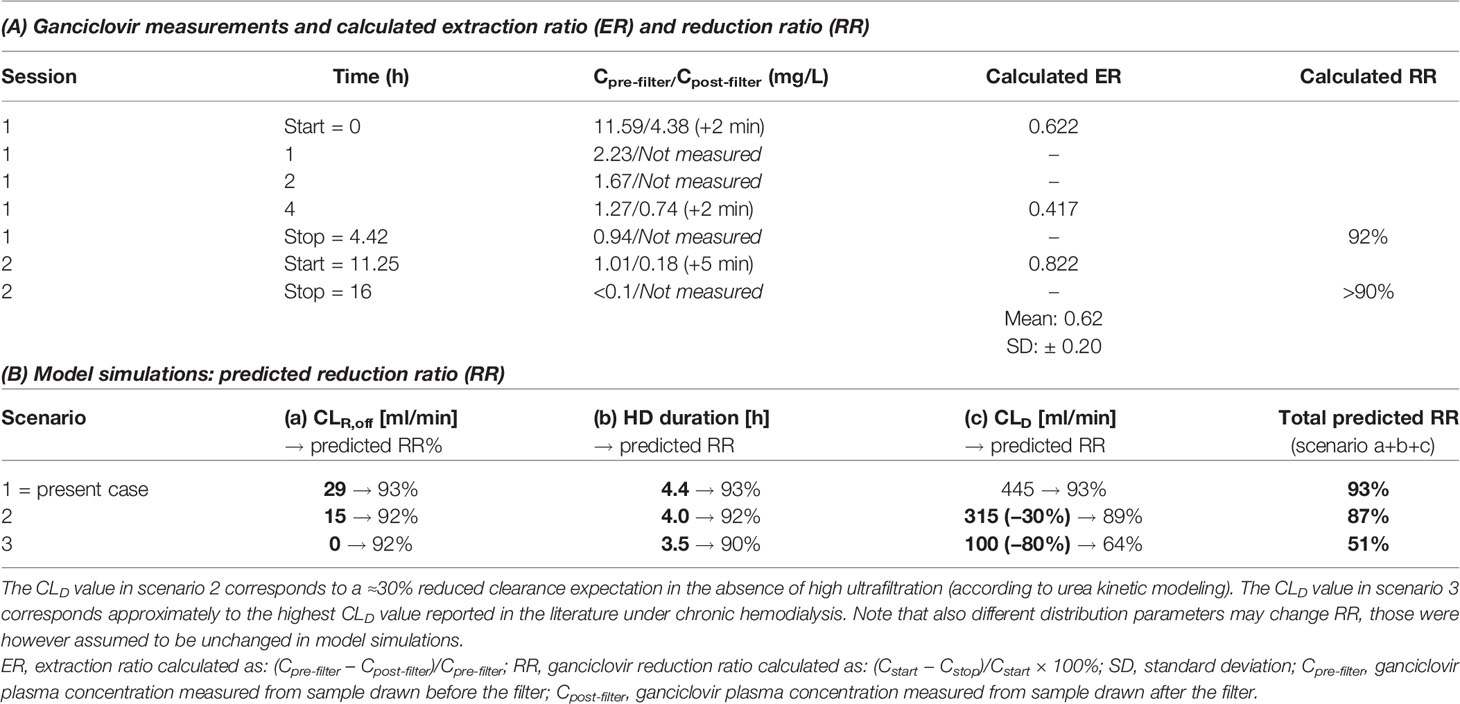
Table 2 (A) Ganciclovir plasma concentrations measured during 2 dialysis sessions and calculated extraction ratio (ER) and reduction ratio (RR). (B) Predicted RR from model simulations under different alternative scenarios.
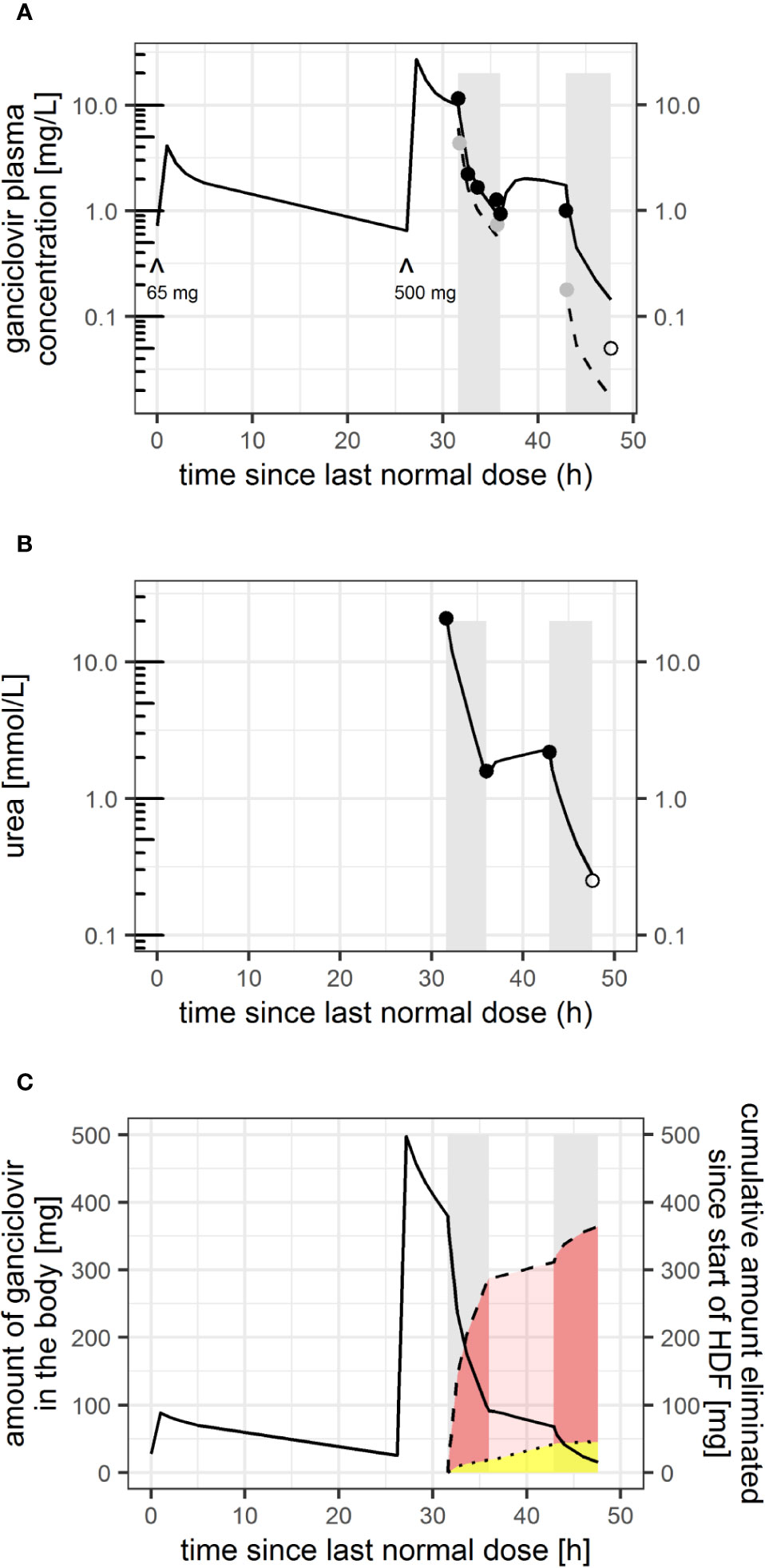
Figure 1 (A) Ganciclovir plasma concentration measured (black dots: pre-filter, gray dots: post-filter) and model-predicted individual concentration-time profile since last normal (for renal function adjusted) ganciclovir dose (black line: pre-filter and intra-dialytic plasma concentration, dashed line: post-filter concentration assuming a constant extraction ratio within each hemodiafiltration session). ^: time and dose of i.v. ganciclovir administered. Gray bars indicate time on hemodiafiltration. (B) Urea concentration measured (dots) and model-predicted urea concentration-time profile. Open circles: (pre-filter) concentrations below limit of quantification (LOQ) (0.1 for ganciclovir, 0.5 mmol/L for urea), plotted at LOQ/2. (C) model-predicted amount of ganciclovir in the body (black solid line), and predicted total amount eliminated since start of first HDF session (dashed line), which is the sum of elimination by residual ganciclovir clearance of the patient (yellow shaded area, limited by dotted line) and HDF (red shaded area).
The ganciclovir reduction ratio (RR) during HDF was calculated in line with the calculated urea reduction ratio (Table 1) from pre-HDF (Cstart, at start of HDF) and post-HDF (Cend, after stopping HDF) ganciclovir pre-filter concentrations:
Calculated ganciclovir HDF clearance (KHDF) was derived from expected diffusive (Kd) and convective clearance (Kc), accounting for the average ER measured:
Where QB = prescribed blood flow, Rbp = blood-to-plasma concentration ratio (assumed to equal 1 as average from in silico (Lukacova et al., 2016) and in vitro (Perrottet et al., 2007) estimates), and ER = average extraction ratio of 0.62.
With UF = ultrafiltration used (131 ml/min for 1st session and 118 ml/min for 2nd session, respectively), SR = solute ratio (or sieving coefficient), assumed to equal 1 for a small molecule like ganciclovir, and f = factor by which Kc is expected to be reduced in the presence of diffusive clearance (=(1-Kd/Qb) in this calculation (Depner, 2012))
Total calculated KHDF hence calculates to:
Note that uncertainties exist concerning Rbp – in literature on ganciclovir dialysis clearance (see below) no distribution into blood cells has partly been assumed (i.e. Rbp = 1-hematocrit, which would result in a lower Kd estimate for our patient of 217 ml/min × (1–0.27) = 158 ml/min, and KHDF of 203–208 ml/min), while pharmacologically distribution into blood cells is necessary for its mechanism of action.
Concentrations were measured by liquid chromatography coupled to tandem mass spectrometry (LC-MS/MS) using an accredited and validated method. Imprecision of the method expressed as coefficient of variation was <7.3%, cumulative trueness from the last four rounds of external quality assessment (EQA) was −5.2%. EQA samples were obtained from KKGT (Den Haag, The Netherlands).
Model-Based Estimation of Ganciclovir HDF Clearance and Fraction of Drug Removed by HDF
Due to uncertainties in KHDF calculation mentioned above, and uncertainties in the volume of distribution to be used for calculating the amount and fraction of drug removed by HDF (Aremoved,HDF and fremoved,HDF, respectively), especially for this drug which is known to have two-comparmental distribution kinetics in plasma, a model-based pharmacokinetic analysis was performed using NONMEM (version 7.4.1, Icon Development Solutions, Ellicott City, MD) to estimate individual ganciclovir renal and HDF clearances (CLR and CLHDF), and to derive Aremoved,HDF and fremoved,HDF. Typical pharmacokinetic parameters of a two-compartmental model were used according to the population pharmacokinetic model published by Caldes et al. developed from a population of solid organ transplant patients with mean body weight of 66 kg (Caldés et al., 2009) (mixed residual error: proportional error: 14.3%, additive error: ± 0.465 mg/L). The last concentration measured below the limit of quantification (LOQ) of 0.1 mg/L was set to LOQ/2.
In the used model the prior expectation (typical value) of renal clearance (CLR) is a function of estimated creatinine clearance (CLcrea − Cockroft-Gault estimate) (Caldés et al., 2009):
Peripheral distribution parameters (peripheral volume of distribution, V2, and inter-compartmental distribution clearance Q) were additionally allometrically scaled by body weight, since physiologically those kinetic parameters are expected to be lower in a 44 kg patient as compared to a 66 kg patient for a molecule that mainly distributes within total body water:
Total clearance (CL) was set equal to the sum of CLR and CLHDF during hemodialysis and to CLR off-dialysis:
Based on those parameters, expected inter-patient variability (33% in prior CLR, 48% in central volume of distribution, V1, with prior [typical] value of V1 = 31.9 L (Caldés et al., 2009)), and the measured pre-filter ganciclovir concentration samples, individual parameters of CLR, V1, and CLHDF were estimated using Bayesian feedback to the following maximum a posteriori estimates: CLR = 1.8 (95% CI: 1.29–2.60) L/h [= 30 ml/min], V1 = 14.1 (95% CI: 7.4–26.8) L, and CLHDF = 26.7 L/h (relative standard error <1%) [445 ml/min]. Inter-session variability in CLHDF was evaluated and was—with an estimate of <1%—considered negligible. Based on individual distribution and clearance parameters, the amount of ganciclovir in the body prior to the first HDF session was predicted to be 380 mg, which was reduced by 288 mg (76%) during the first HDF session. 269 mg (93%) were predicted to be eliminated by HDF (=Aremoved,HDF and fremoved,HDF) and 19 mg (7%) by patient’s residual clearance (Figure 1C).
In a sensitivity analysis, CLHDF was fixed to calculatory KHDF, which yielded individual estimates of CLR= 2.4 L/h [40 ml/min] and V1 = 9.9 L, and a slightly worse model fit (P = 0.02, likelihood ratio test). The amount of ganciclovir in the body prior to the first HDF session was predicted to 320 mg, which was reduced by 220 mg (69%) during the first HDF session. 191 mg (89%) were predicted to be eliminated by HDF (=Aremoved,HDF and fremoved,HDF) and 29 mg (13%) by patient’s residual clearance.
Modeling of Post-Filter Ganciclovir Concentrations
Post-filter concentrations (Cpost-filter) were modeled assuming a constant ER, to estimate the effective kinetic plasma flow through the filter (QEFF) (Atkinson and Umans, 2009):
Assuming diffusive clearance to represent the major mechanism of elimination for a small molecule during HDF (Tattersall and Blankestijn, 2019), QEFF would be limited by the blood flow (QB) through the filter, but can exceed QB for molecules that accumulate in blood cells, i.e. for drugs with a blood-to-plasma concentration ratio (Rbp) >1, since QEFF = QB × Rbp (Atkinson and Umans, 2009). For molecules that do not distribute into blood cells QEFF would in turn equal the plasma water flow, i.e. QEFF = QB × (1 − hematocrit). In HDF, QEFF can further increase by high ultrafiltration.
Allowing for inter-session variability in the ER (suggested in Table 2), QEFF was estimated to be 47.4 L/h (relative standard error <1%) [788 ml/min], corresponding to a mean ER of 0.56, with considerable inter-session variability of 49%. The proportional residual error in predicted Cpost-filter concentrations was estimated to be 25%, an additive error was not quantifiable.
Modelling Cpost-filter did not affect the ganciclovir CLHDF estimate.
Ganciclovir Model Simulations
Model simulations using different hypothetical CLR, dialysis duration, and dialysis clearance were performed using Berkeley Madonna (version 8.3.18) to evaluate the impact of those parameters on the reduction ratio (Table 2B), and to better compare our results to literature (see below).
Comparative Kinetic Analysis of Urea as Reference Solute
Urea—just like ganciclovir—follows two-compartmental distribution kinetics (Clark et al., 1999). Urea dialysis clearance (CLHDF,urea) was also estimated kinetically using a model-based analysis. Urea distribution parameters (V1, V2, Q) and residual error were fixed to values predicted from a urea kinetic model accounting for weight-based changes in inter-compartmental clearance (Gotta et al., 2020). Renal urea clearance (CLR,urea) was assumed to be related to creatinine clearance (CLR,crea as follows:
considering their correlation with glomerular filtration rate (GRF), which is approximately 15% overpredicted by CLR,crea (undergoing tubular secretion) and 15% underpredicted by CLR,urea (Almond et al., 2008).
The urea generation rate was initially fixed to 0.104 mmol/min (Clark et al., 1999). In a second step an individual value was estimated using prior values estimated from a small population of patients on chronic HD (prior mean: 0.17 mmol/min, inter-individual variability: 38%) (Pfister et al., 2004). The last concentration measured below the LOQ of 0.5 mmol/L was set to LOQ/2.
Total urea clearance (CLurea) was set equal to the sum of CLR,urea and CLHDF,urea during hemodialysis and to CLR,urea off-dialysis:
This approach yielded an estimate of total CLHDF,urea of 310 ml/min, i.e. larger than the diffusive clearance mechanistically predicted from filter characteristics, blood flow, and dialysate flow (predicted urea clearance: 230 ml/min, Table 1) (Gotta et al., 2020). The individual urea generation rate was estimated to 0.056 mmol/min.
The complete NONMEM model codes for ganciclovir and urea can be found in the supplemental data. All model predictions are shown in Figure 1.
Review of the Literature
Publications relating to intermittent renal replacement therapy for comparison of our data were searched on MEDLINE during October 2019 using “renal dialysis” (MeSH) AND (“ganciclovir” OR “valganciclovir”). This search resulted in 32 references, whose abstracts were screened for pharmacokinetic data, which were then extracted from the full publication. In total seven publications reporting pharmacokinetic data in patients on intermittent hemodialysis were identified. Reported and calculated pharmacokinetic parameters of interest are summarized in Table 3.
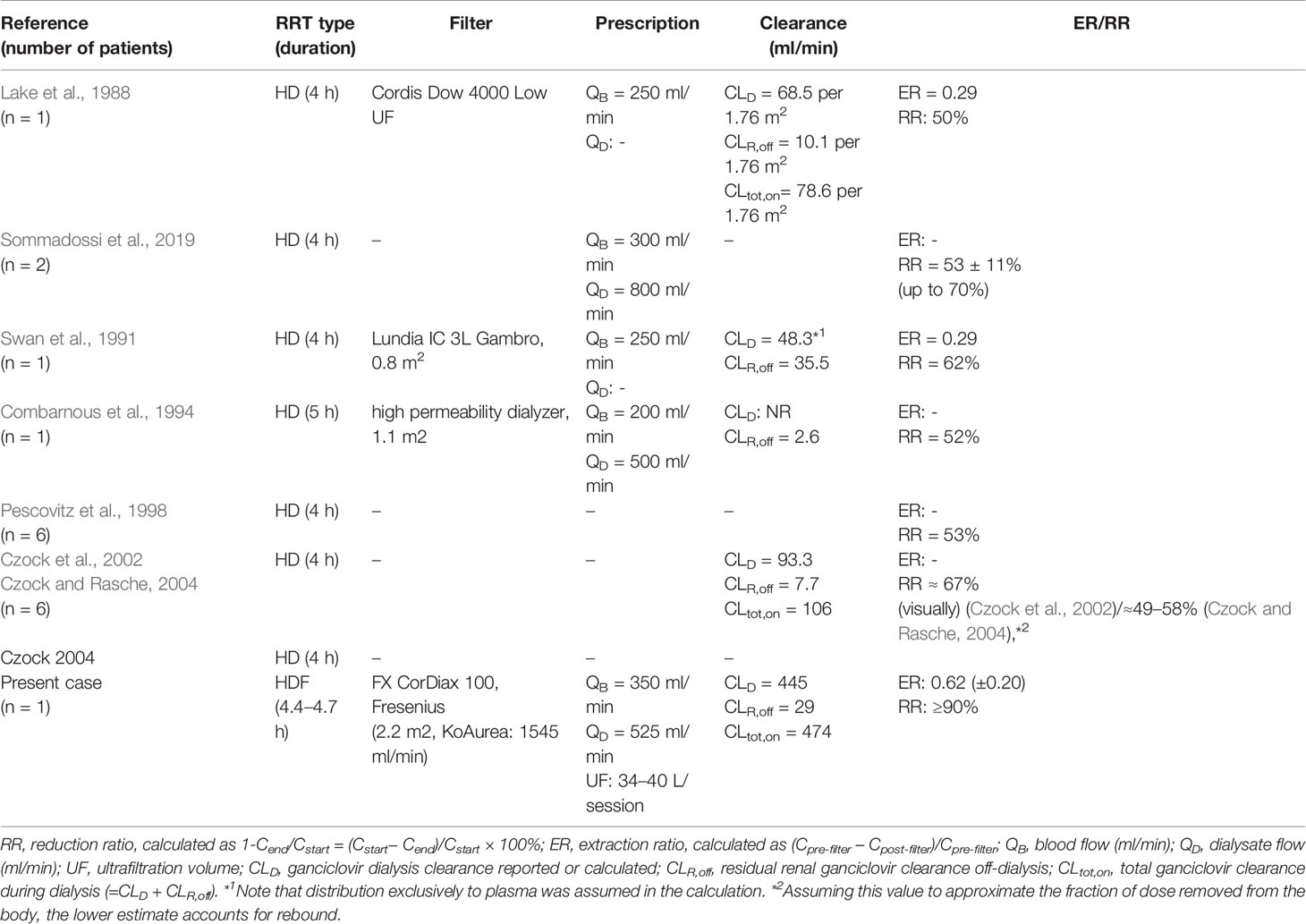
Table 3 Review of existing literature (chronologically ordered) on ganciclovir elimination during different types of intermittent renal replacement therapy (RRT) and comparison with estimates for the present patient.
Discussion
We present a case of an inadvertent eight-fold ganciclovir overdose in a 70-year-old kidney transplant patient, successfully treated with two sessions of intermittent HDF. Retrospective analysis of ganciclovir pharmacokinetic data revealed that HDF was much more efficient at removing ganciclovir from the patient’s plasma (reduction ratio: ≥90%) than previously reported for endstage-renal disease patients on chronic HD (50–67%, Table 3).
While it must be noted that residual renal ganciclovir clearance in our patient (estimated to be 30 ml/min by Bayesian feedback, i.e. twice her creatinine clearance) may have contributed to the high reduction ratio during a HDF session of 4.4 h, model-based analysis showed that it contributed to only 7% of total clearance during HDF (estimated to be 475 ml/min). A model-based analysis was considered necessary to calculate CLHDF due to the delayed two-compartmental distribution kinetics of the drug (Czock et al., 2002; Caldés et al., 2009) and since assessment of dialysis clearance by the ER only is complicated by limited knowledge about the distribution into blood cells that would be required to make correct assumptions about the effective pharmacokinetic plasma flow through the filter (Atkinson and Umans, 2009). The ganciclovir CLHDF estimate of 445 ml/min was very close to the sum of prescribed blood flow and ultrafiltration rate (350 + 131 ml/min = 481 ml/min) and was higher than urea dialysis clearance estimated (310 ml/min). This suggests an accumulation of ganciclovir in the blood cells in this patient (Rbp > 1). To our knowledge, Rbp has not been measured in vivo for ganciclovir. Based on its pharmacologic action, requiring intracellular phosphorylation leading to a long intra-cellular half-life (discussed in the introduction) and accumulation in peripheral blood mononuclear cells (Billat et al., 2016), it may be hypothesized that an Rbp > 1 would pharmacologically be expected. An erythrocyte/plasma value of 1.11 has indeed been measured in vitro by Perrottet et al. (2007). We acknowledge that an in silico estimate of 0.89 has been proposed (Lukacova et al., 2016)). in contrast to our expectation, which is however usually based on physiochemical properties only (e.g. polarity and lipophilicity) (Peters, 2012) and which may ignore active transmembrane transport mechanisms known for ganciclovir (Lukacova et al., 2016). If ganciclovir would distribute like the small molecule urea (molecular weight: 60 Da) homogenously and passively between plasma and red blood cells (Rbp = 1), CLHDF of ganciclovir could physiologically not exceed the estimated CLHDF,urea value of 310 ml/min. Collection of dialysate and ultrafiltrate to measure the recovered ganciclovir amount and CLHDF directly would have been additionally useful as gold-standard method, but was not practical. Serial measurements of intra-cellular ganciclovir and application of a multi-compartment distribution model (Billat et al., 2016) could have further enhanced our mechanistic understanding of the high CLHDF calculated. Importantly, highly efficient elimination of ganciclovir by HDF as reported here may not be sufficient to prevent hematologic and neurologic toxicity completely as intracellular accumulation still may occur. Our patient did not show any signs of neurotoxicity and she recovered from intermittent leukopenia, which was apparent before overdosing and may have other reasons as cytotoxicity due to CMV infection.
Interestingly however, there was a very strong correlation between the ganciclovir and urea reduction ratio calculated (both ratios calculated to 92% during the first session), which may be an approximation for the amount of drug removed during HDF. This may suggest—independent of red blood cell distribution—that efficiency of urea removal can be used as a surrogate marker for ganciclovir removal. The estimated CLHDF,urea of 310 ml/min exceeded the mechanistically predicted diffusive in vivo urea clearance of 230 ml/min by 35%, suggesting significant contribution of convective clearance by the high ultrafiltration used in this HDF setting. The high blood flow compared to cases reported in the literature probably also contributed to a high diffusive clearance. The difference of 80 ml/min, relating to convective urea clearance, corresponds to 0.61–0.67 of the ultrafiltration rate used. This fraction may be interpreted as net sieving coefficient, which is expected to be reduced in the presence of diffusion (Tattersall and Blankestijn, 2019) compared to its expected value of 1.
In conclusion, this case illustrates highly efficient elimination of ganciclovir by intermittent HDF in a patient treated for inadvertent overdose potentially associated with intermittent leukopenia. Ganciclovir elimination by targeted intense HDF largely exceeded elimination reported by previous publications for patients on intermittent HD. The high elimination in the present case may be explained by several factors. First, a relevant contribution of convection to CLHDF at the high ultrafiltration rate used could be quantified for the reference molecule urea. Second, the blood flow of 350 ml/min was higher and the HDF session duration of 4.4–4.7 h was longer than in previous references reporting on ganciclovir elimination during HD. Third, while it is difficult to conclude on the importance of filter characteristics, since details were frequently not provided in the literature, the filter used in this case may have been characterized by a larger surface area and higher dialytic efficiency than filters used in the past. In fact, some drug dose recommendations for patients on RRT issued before the year 2000 are likely outdated due to advanced technology (Mueller and Smoyer, 2009). The reduction ratio of reference molecules like urea, which is routinely assessed during HD and HDF, could be evaluated as an indicator of ganciclovir removal in future studies.
Data Availability Statement
All datasets presented in this study are included in the article/Supplementary Material.
Ethics Statement
Written informed consent was obtained from the individual for the publication of any potentially identifiable images or data included in this article.
Author Contributions
Conception/data acquisition: MG, AJ. Conception/data analysis: DM, MP, VG, and AL-T. All authors were involved in interpretation of data. VG and AJ drafted the manuscript. All authors contributed to the article and approved the submitted version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fphar.2020.00882/full#supplementary-material
References
Almond, A., Siddiqui, S., Robertson, S., Norrie, J., Isles, C. (2008). Comparison of combined urea and creatinine clearance and prediction equations as measures of residual renal function when GFR is low. Qjm. 101 (8), 619–624. doi: 10.1093/qjmed/hcn032
Ar, M. C., Ozbalak, M., Tuzuner, N., Bekoz, H., Ozer, O., Ugurlu, K., et al. (2009). Severe Bone Marrow Failure Due to Valganciclovir Overdose After Renal Transplantation From Cadaveric Donors: Four Consecutive Cases. Transplant. Proc. 41 (5), 1648–1653. doi: 10.1016/j.transproceed.2009.02.093
Atkinson, A. J., Umans, J. G. (2009). Pharmacokinetic studies in hemodialysis patients. Clin. Pharmacol. Ther. 86 (5), 548–552. doi: 10.1038/clpt.2009.147
BC Renal Network. 2019. Commonly used dialyzer specifications and substitution chart for visiting patients, accessed 10/2019 http://www.bcrenalagency.ca/.
Billat, P. A., Woillard, J. B., Essig, M., Sauvage, F. L., Picard, N., Alain, S., et al. (2016). Plasma and intracellular exposure to ganciclovir in adult renal transplant recipients: Is there an association with haematological toxicity? J. Antimicrob. Chemother. 71 (2), 484–489. doi: 10.1093/jac/dkv342
Caldés, A., Colom, H., Armendariz, Y., Garrido, M. J., Troconiz, I. F., Gil-Vernet, S., et al. (2009). Population pharmacokinetics of ganciclovir after intravenous ganciclovir and oral valganciclovir administration in solid organ transplant patients infected with cytomegalovirus. Antimicrob. Agents Chemother. 53 (11), 4816–4824. doi: 10.1128/AAC.00085-09
Clark, W. R., Leypoldt, J. K., Henderson, L. W., Mueller, B. A., Scott, M. K., Vonesh, E. F. (1999). Quantifying the effect of changes in the hemodialysis prescription on effective solute removal with a mathematical model. J. Am. Soc. Nephrol. 10 (3), 601–609.
Combarnous, E., Fouque, D., Bernard, N., Boulieu, R., Chossegros, P., Laville, M., et al. (1994). Pharmacokinetics of ganciclovir in a patient undergoing chronic haemodialysis. Eur. J. Clin. Pharmacol. 46, 379–381. doi: 10.1007/BF00194410
Czock, D., Rasche, F. M. (2004). New AUC-Based Method to Estimate Drug Fraction Removed by Hemodialysis. Kidney Blood Press Res. 27 (3), 172–176. doi: 10.1159/000079806
Czock, D., Scholle, C., Rasche, F. M., Schaarschmidt, D., Keller, F. (2002). Pharmacoldnctics of valganciclovir and ganciclovir in renal impairment. Clin. Pharmacol. Ther. 72 (2), 142–150. doi: 10.1067/mcp.2002.126306
Daugirdas, J. T. (1993). Second generation logarithmic estimates of single-pool variable volume Kt/V: an analysis of error. J. Am. Soc. Nephrol. 4 (5), 1205–1213.
Depner, T. A. (2012). “Approach to Hemodialysis Kinetic Modeling,” in Principles and Practice of Dialysis. Ed. Henrich, W. L. (Philadelphia: Lippincott Williams & Wilkins), 73–96.
Gotta, V., Dao, K., Rodieux, F., Buclin, T., Livio, F., Pfister, M. (2017). Guidance to develop individual dose recommendations for patients on chronic hemodialysis. Expert Rev. Clin. Pharmacol. 10 (7), 737–752. doi: 10.1080/17512433.2017.1323632
Gotta, V., Marsenic, O., Pfister, M. (2020). Understanding Urea Kinetic Factors That Enhance Personalized Hemodialysis Prescription in Children. ASAIO J. 66 (1), 115–123. doi: 10.1097/mat.0000000000000941
Kotton, C. N., Kumar, D., Caliendo, A. M., Huprikar, S., Chou, S., Danziger-Isakov, L., et al. (2018). The Third International Consensus Guidelines on the Management of Cytomegalovirus in Solid-Organ Transplantation, Vol. 102. doi: 10.1097/TP.0000000000002191
Lake, K. D., Fletcher, C. V., Love, K. R., Brown, D. C., Joyce, L. D., Pritzker, M. R. (1988). Ganciclovir pharmacokinetics during renal impairment. Antimicrob. Agents Chemother. 32 (12), 1899–1900. doi: 10.1128/AAC.32.12.1899
Lavergne, V., Ouellet, G., Bouchard, J., Galvao, T., Kielstein, J. T., Roberts, D. M., et al. (2014). Guidelines for reporting case studies on extracorporeal treatments in poisonings: Methodology. Semin. Dial. 27 (4), 407–414. doi: 10.1111/sdi.12251
Lukacova, V., Goelzer, P., Reddy, M., Greig, G., Reigner, B. (2016). Parrott N. A Physiologically Based Pharmacokinetic Model for Ganciclovir and Its Prodrug Valganciclovir in Adults and Children. AAPS J. 18 (6), 1453–1463. doi: 10.1208/s12248-016-9956-4
Michaels, A. S. (1966). Operating parameters and performance criteria for hemodialyzers and other membrane-separation devices. Trans. Am. Soc. Artif. Intern Organs. 12, 387–392.
Mueller, B. A., Smoyer, W. E. (2009). Challenges in developing evidence-based drug dosing guidelines for adults and children receiving renal replacement therapy. Clin. Pharmacol. Ther. 86 (5), 479–482. doi: 10.1038/clpt.2009.150
Perrottet, N., Beguin, A., Meylan, P., Pascual, M., Manuel, O., Buclin, T., et al. (2007). Determination of aciclovir and ganciclovir in human plasma by liquid chromatography-spectrofluorimetric detection and stability studies in blood samples. J. Chromatogr B Anal. Technol. BioMed. Life Sci. 852 (1-2), 420–429. doi: 10.1016/j.jchromb.2007.01.045
Pescovitz, M. D., Pruett, T. L., Gonwa, T., Brook, B., McGory, R., Wicker, K., et al. (1998). Oral ganciclovir dosing in transplant recipients and dialysis patients based on renal function. Transplantation. 66 (8), 1104–1107. doi: 10.1097/00007890-199810270-00023
Peters, S. A. (2012). Physiologically-Based Pharmacokinetic (PBPK) Modeling and Simulations: Principles, Methods, and Applications in the Pharmaceutical Industry. 1st ed. (Hoboken, New Jersey: Wiley).
Pfister, M., Uehlinger, D. E., Hung, A. M., Schaedeli, F., Sheiner, L. B. (2004). A new Bayesian method to forecast and fine tune individual hemodialysis dose. Hemodial Int. 8 (3), 244–256. doi: 10.1111/j.1492-7535.2004.01102.x
Scott, J. C., Partovi, N., Ensom, M. H. H. (2004). Ganciclovir in Solid Organ Transplant Recipients. Ther. Drug Monit. 26 (1), 68–77. doi: 10.1097/00007691-200402000-00014
Sommadossi, A. J., Bevan, R., Ling, F., Lee, T., Mastre, B., Chaplin, M. D., et al. (2019). “Clinical Pharmacokinetics of Ganciclovir in Patients with Normal and Impaired Renal Function Source : Reviews of Infectious Diseases,” in Cytomegalovirus Infection and Treatment with Ganciclovir, vol. 10, S507–S5S5, Supplement 3.
Swan, S., Munar, M., Wigger, M., Bennett, W. (1991). Pharmacokinetics of ganciclovir in a patient undergoing hemodialysis. Am. J. Kidney Dis. 17 (1), 69–72. doi: 10.1016/S0272-6386(12)80253-8
Keywords: ganciclovir, valganciclovir, hemodialysis, hemodiafiltration, overdose, toxicity, blood-to-plasma concentration ratio
Citation: Gotta V, Leuppi-Taegtmeyer A, Gessler M, Pfister M, Müller D and Jehle AW (2020) Intensive Hemodiafiltration Successfully Removes Ganciclovir Overdose and Largely Exceeds Reported Elimination During Hemodialysis—A Case Report and Review of the Literature. Front. Pharmacol. 11:882. doi: 10.3389/fphar.2020.00882
Received: 31 March 2020; Accepted: 28 May 2020;
Published: 12 June 2020.
Edited by:
Roberto Paganelli, University of Studies G. d’Annunzio Chieti and Pescara, ItalyReviewed by:
Anders Åsberg, University of Oslo, NorwayBernard J. M. Canaud, Université de Montpellier, France
Copyright © 2020 Gotta, Leuppi-Taegtmeyer, Gessler, Pfister, Müller and Jehle. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Verena Gotta, dmVyZW5hLmdvdHRhQHVrYmIuY2g=
 Verena Gotta
Verena Gotta Anne Leuppi-Taegtmeyer
Anne Leuppi-Taegtmeyer Mirjam Gessler3
Mirjam Gessler3 Andreas Werner Jehle
Andreas Werner Jehle