- 1Policy Research Institute, Kathmandu, Nepal
- 2Institute for Poverty Alleviation and International Development, Yonsei University, Wonju, South Korea
- 3Manmohan Memorial Institute of Health Science, Kathmandu, Nepal
- 4Department of Gerontology, Pai Chai University, Daejeon, South Korea
- 5Department of Preventive Medicine, Yonsei University Wonju College of Medicine, Wonju, South Korea
- 6Department of Global Health Economics and Policy, University of Kragujevac, Kragujevac, Serbia
- 7Division of Health Economics, Lund University, Lund, Sweden
Background: Tobacco use in youths is a major public health challenge globally, and approaches to the challenge have not been sufficiently addressed. The existing policies for tobacco control are not well specified by age.
Objective: Our study aims to systematically investigate existing tobacco control policies, potential impacts, and national and international challenges to control tobacco use targeting the youth.
Data sources: We used the statistics of the Global Youth Tobacco Survey (GYTS), studies, and approaches of tobacco control policies targeting youth. Considering country, continent, age, and significance, PubMed, Health Inter-Network Access to Research Initiative (HINARI), Scopus, the Cochrane Library, Google, and Google Scholar were searched. The related keywords were tobacco control, youth, smoking, smoking reduction policies, prevalence of tobacco use in youth, classification of tobacco control policies, incentives to prevent young people from using tobacco, WHO Framework Convention on Tobacco Control (FTCT), etc. The search strategy was by timeline, specific and popular policies, reliability, significance, and applicability.
Results: We found 122 studies related to this topic. There were 25 studies focusing on situation, significance, and theoretical aspects of tobacco control policies associated with youth; 41 studies on national population polices and challenges; and 7 studies for global challenges to overcome the youth tobacco epidemic. All national policies have been guided by WHO-MPOWER strategies. Increases in tobacco tax, warning signs on packaging, restriction of tobacco product advertisements, national law to discourage young people, and peer-based approaches to quit tobacco are popular policies. Smuggling of tobacco products by youth and ignorance of smokeless tobacco control approach are major challenges.
Limitation: Our study was flexible for the standard age of youth and we were not able to include all countries in the world and most of the studies focused on smoking control rather than all smokeless tobaccos.
Conclusion: The policies of tobacco control adopted by many countries are based on the WHO Framework Convention on Tobacco Control but not necessarily focused on youth. Due to the physical and economic burden of tobacco consumption by youth, this is a high priority that needs to be addressed. Youth-focused creative policies are necessary, and more priority must be given to tobacco prevention in youth. Tobacco control should be a social, public health, and quality-of-life concern rather than a business and trade issue.
Implication of key findings: There is limited research on how and in what ways tobacco control policies reach young people and their engagement with these policies from physical, physiological, and psychological aspects. Analysis of these aspects, popular polices practiced in different countries, and creative strategies support the need to review current practices and future ways to discourage youth from tobacco use.
Introduction
Tobacco consumption is a major challenge for the 21st century because tobacco-related deaths are increasing, destroying the young generation and promoting an environmental threat. Globally, tobacco has killed 100 million people in the 20th century, much more than all deaths in World Wars I and II combined, and tobacco-related deaths will number around 1 billion in the 21st century if current tobacco use patterns continue (Eriksen et al., 2015). Of the 100 million projected tobacco-related deaths over the next 20 years, about half will be of people in the productive ages of 35–69 (Centers for Disease Control and Prevention, 2000). Regardless of many national bans on tobacco sales to minors, approximately 25% of people under 18 years old are using tobacco and 12.6% are using more than two types of tobacco products (Arrazola et al., 2014). There are multiple impacts (economic, health, social, family, and peer groups) of tobacco use in youth because they are losing high amount of money, as the tax on tobacco increases year by year, risk factors for many disease, vulnerability to alcohol use and drugs, and copying his/her tobacco use by juniors in schools and sibling in family put them at risk for tobacco use.
There are a variety of programs and policies for tobacco control, but policy analyses on age-specific tobacco control are very rare. It is important because the resources, efforts, and approaches to quitting tobacco for people 60 years of age and those 16 years age do not have a similar impact. A study pointed out that there is a need for a comprehensive multifaceted approach to tobacco control policies for youth (Grimsaw and Stanton, 2017; Cancer Council., 2017a). There is a need to observe that as a foundation and productive age group, youth should be a high priority because interventions would be cost-effective and more productive to family and the nation. Moreover, approaches to controlling tobacco in youth are easy in comparison with late adults and the elderly because nicotine addiction in the late stage is difficult to overcome. From the point of its effectiveness, preventive and nominal remedial approaches are sufficient for youth. In contrast, more resources and complex medical approaches are necessary in late-stage addiction. Likewise, different kinds of medical risk can be prevented in the early stage (youth) but are hardly possible in the late stage. Previous studies, research, policies, and programs are not clearly distinctly age-specific tobacco control approaches, and in our study, we explore the different dynamics of tobacco control policies focusing on youth.
Prevalence of Tobacco Use Among Youth
Tobacco use among youth remains a major public health concern worldwide. Globally, there are about 1.2 billion smokers, of whom more than 50% are young people; the prevalence varies by region, country, and gender (Khuder et al., 2008; Lim et al., 2010; Al-Sadat et al., 2010). By gender, smoking among boys (16%) is almost three times than that among girls (6%) globally. In the West Pacific, the prevalence of smoking among boys (18%) is four times than that among girls (4%), whereas in the United States and Europe, the gap between boys and girls is less than double. Smokeless tobacco is also gaining popularity and is currently used globally by 8% (6% in boys and 2% in girls). The highest proportion of girls using smokeless tobacco (17%) is found in the West Pacific and the lowest (2%) is found in Europe (World Health Organization., 2012). India, with 327 million adolescents, has one of the youngest populations in the world; the number of adolescents using tobacco is approximately 21% of the country’s population (Vidhubala et al., 2014). Since 1980, large reductions in the estimated prevalence of daily smoking have been observed at the global level for both boys and girls (e.g., in the United States, about 10% from 1980 to 1990 of 12th-grade students), (Nelson et al., 2008) but because of population growth, the gross number of smokers has increased significantly (Ng et al., 2014). According to the Global Youth Tobacco Survey (GYTS) 2011, the top three countries for tobacco consumption rates were Papua New Guinea (43.8%), Chile (31.5%), and Lithuania (30.8%), while Cambodia consumption rate was the lowest (0.2%) (World Health Organization, 2011). Prevalence of youth tobacco use reduces life expectancy (Ranabhat et al., 2018; Ranabhat et al., 2019). Socially, youth from disadvantaged groups are more vulnerable to smoking because of their social context (Hefler and Chapman, 2014). Despite the variation in statistics between different classifications of youth, youth smoking is a major threat in every aspect.
Understanding Youth
Youth is a critical and foundation period of human life; however, there is no consistent definition. Youth is the time of life when one is young, but often means the time between childhood and adulthood (maturity) (Walker et al., 2013). Around the world, the English terms youth, adolescent, teenager, kid, and young person are interchanged, often meaning the same thing (Konopka, 1973). The United Nations has defined the contextual definition of youth: age between 15 and 24 by UN secretaries, UNESCO, and ILO; age of 15–32 by UN habitat; age of 10–24 by UNFPA and WHO; child until 18 by UNICEF; and age between 15 and 35 by the African youth charter (United Nation., 2016). Beyond this, different countries have defined the youth in their context, and we have used the term youth as a wide concept as used by different scholars and organization. The focus of this study is on tobacco control policies applicable for youth despite the age variation.
Youth Period and Risk for Tobacco Use/Smoking
There are theoretical and empirical studies about the risk of youth tobacco use/smoking. Youth may initiate smoking by i) social learning theory; youth are eager to try something new, i.e., attention, retention, motor reproduction, and reproduction and motivation process; (Bandura and McClelland, 1977) ii) psychological development theory; they decide whether they should use or not, i.e., age, self-control, academic achievement, growth trend, and distal structure (parents or peer); (Jessor and Jessor, 1977) iii) behavior theory; the attitude of acceptance and to continue or not, i.e., person’s behavior is a function of behavioral intention, which is determined by attitude toward the act; (Ajzen and Fishbein, 1970), and iv) self-conceiving theory; every activity of human is determined by self-conception (Rosenberg, 1986). Blum has explored different aspects of human emotions, motivation, and perceptions, particularly during the period of youth (Blum, 2009). Due to their age, physiological changes, and family and social environments, youth often perpetuate smoking practices, and they ultimately become addicted. Indeed, youth tobacco use is a primary source of substance use and other social deviations. High school male students who have smokers in family and school, smoker friends, media and advertisement influence, and easy access to the purchase of cigarettes are factors to youth smoking; smokers often lack self-control even though they know smoking is harmful (Simons-Morton et al., 1999; Alexander et al., 2001; Ertas, 2007).
Key Questions
KQ1—What is the current situation of youth tobacco use in terms of prevalence and control policy pattern?
KQ2—What are the major and popular policies to control tobacco in the national and global context targeting youth?
KQ3—What could be the best creative policies for tobacco control for youth?
Objective of the Study
The aim of this study is to systematically investigate the situation regarding youth tobacco use, existing policies, effectiveness, and challenges in the national and global context.
Methods
Eligibility Criteria
We focused precisely on tobacco control policies, targeting youth, policies adopted by countries, challenges to implementing those policies, publications in English, and availability of latest prevalence data.
Studies were included based on the following PICOS strategies.
1. Population: Youth population and age limit vary between countries.
2. Intervention: Popular and successful intervention policies to control tobacco use targeting for youth.
a. Disconnect youth from tobacco
b. Smoking/tobacco use cessation
3. Comparison: Comparison of tobacco control policies by country and intervention time duration.
4. Outcomes: Prevalence of tobacco use before intervention and after intervention.
5. Study types: Interventional studies, surveys (cross-sectional and follow up), cohort and randomized control trials, core contents related to study from official web pages and some gray materials.
Exclusion:
1. Did not meet the inclusion criteria.
2. General tobacco control not applicable for youth; data available are not in English; mixed studies with tobacco use; coffee, alcohol, and other substance use/abuse; and data with mixed/overlap of age (youth and adult/youth and elder).
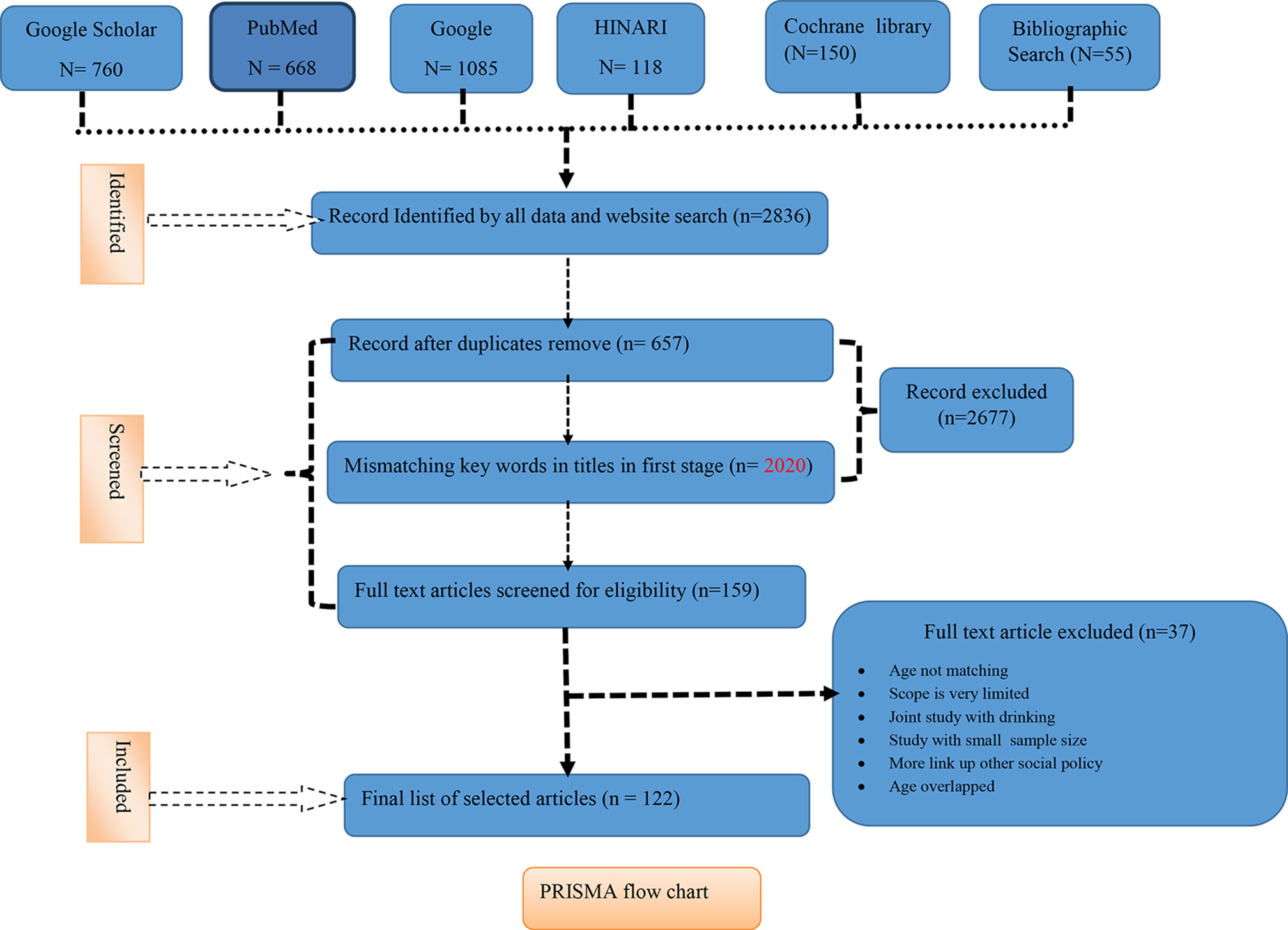
The details of excluded data with reason are available in the PRISMA flowchart (Figure 1).
Data Searching Strategy
Literature search strategies were developed using Medical Subjects Headings (MeSH) terms and keywords. Different health and social science search engines and databases were used (PubMed, Scopus, the Cochrane Library, HINARI, Google, and Google Scholar) to find sources regarding global and national policies mostly focusing on youth tobacco use. We used single, double, or multiple MeSH terms, free text, and specific terms under a subheading to identify relevant studies from the online data sources. Search strategy also included content, synonyms, year, and country names (Box 1). We downloaded and analyzed relevant journal articles, books, survey results, analytical views related to the WHO FCTC, and unpublished reports.
Box 1. Electronic data search strategy.
Terminology used for search
Tobacco control policies, Smoking reduction policy, Youth and smoking, Tobacco use by adolescents , Comparative studies of tobacco use by boys and girls, Systemic review of tobacco control policies, Classification of tobacco control policies, Incentives on preventing and cessation of smoking, Legal provision for tobacco control, Effectiveness of WHO FCTC, Interventions for tobacco control on youth, MPOWER strategies, tobacco control policies by country continent, age gender, Effectiveness of MPOWER etc.
PubMed Search Options
● Search by: Terminology mentioned above
● Search Details: Single, double or multiple MeSH terms as mentioned in terminology
● Article type: All
● Text availability: Abstract and all text
● Publication date: Any time
● Complementary search: Similar articles
Scopus search options
● Search by: Subject area and title
● Display options: All available
● Source type: Journal, Book Series and Conference preceding
Cochrane library
● Search by: Key words and titles
● Date: before 2005 and between 2005 – 2019
● Language: English
● Search folder: Cochrane review, Cochrane protocol, Trial and Special collection
Google Scholar
● Search terminologies: As mentioned above by key words and titles
● Time: Any times
● Sort by: Relevance
● Included: Related citations
Health Inter Network Access to Research Initiative (HINARI)
● Search terminologies: As mentioned above by key words and titles
● Content type: Journal article, Publication, Book Chapter, Conference preceding, Data, Government documents
● Publication date: Before 2005 and between 2005 – 2019
● Discipline: Medicine, Public health, Policy
● Language: English
● Key words: As mentioned above by key words and titles
● Display: all
● Purpose: Screening key titles
Data Source Management
We, all authors, established the inclusion and exclusion criteria and data search strategies. CR and MBP searched all data and CBK and MJ verified those data. There were some data that were ambiguous and less relevant to our study but we decided to include some in our study.
Ways of Screening and Selection of Data Sources
The title of the study was screened by search engines using major keywords and titles. Many times, search engines were used to find the appropriate titles. After that, the titles were selected. In a second step, abstract and full-length studies were selected by database search engines. In the third stage, full-length articles were screened based on inclusion criteria. Studies were assessed using criteria developed, for example, effective for public health implications, representativeness of study samples, comparability, credibility of data collection tools, and attributability to the intervention. An additional criterion of “generalizability” assessed whether findings were likely to be transferable at a global, regional, or national level. Particular attention was paid to internal and external validity; important quality and validity issues are discussed alongside study results.
Quality Assessment
For quality assessment of resources, we used the Effective Public Health Practice Project (EPHPP) Quality Assessment Tool for Intervention (Higgins and Green, 2011) as reference. All research studies applied in this paper were searched and screened by two authors (Chhabi Ranabhat and Myung-Bae Park), with any disagreement resolved by consensus or arbitration of authors during meetings. For the risk of bias, we considered only selection bias and data collection method.
Results
Search Outcome
The cumulative total records found in our search screen were 2,836 from PubMed (n = 668) Google Scholar (n = 760), Google (n = 1,085), Health Inter-Network Access to Research Initiative (HINARI n = 118), Cochrane library (n = 150), and Bibliographic Search (n = 55). The total excluded 2677 records in the first stage: duplicates (n = 657) and mismatching keywords in titles in the first stage (n = 2020) were removed. From record screening, we found n = 159 full text sources, and out of 159 full-length articles, we excluded 37 articles due to age not matching, scope is very limited, joint study with drinking, study with a small sample size, and more links to other social policy, and we finally included 122 articles in our full study (see the PRISMA flowchart).
Study Characteristics
Table 1 shows the general characteristics of the study. Almost fifty percent (44.94%, n = 89) of our retrieved studies were about youth-targeted tobacco control in youth and most of the data (87.60%, n = 121) are from 2005 to 2019. We set the time frame for the study because before 2005, there was a situation of tobacco epidemic and individual countries were doing their own efforts on controlling tobacco use after 2005 (actually after signature on WHO FCTC by different countries). Regarding national policies from different continents, more than 1/3 (41.46%) are from Asian countries.
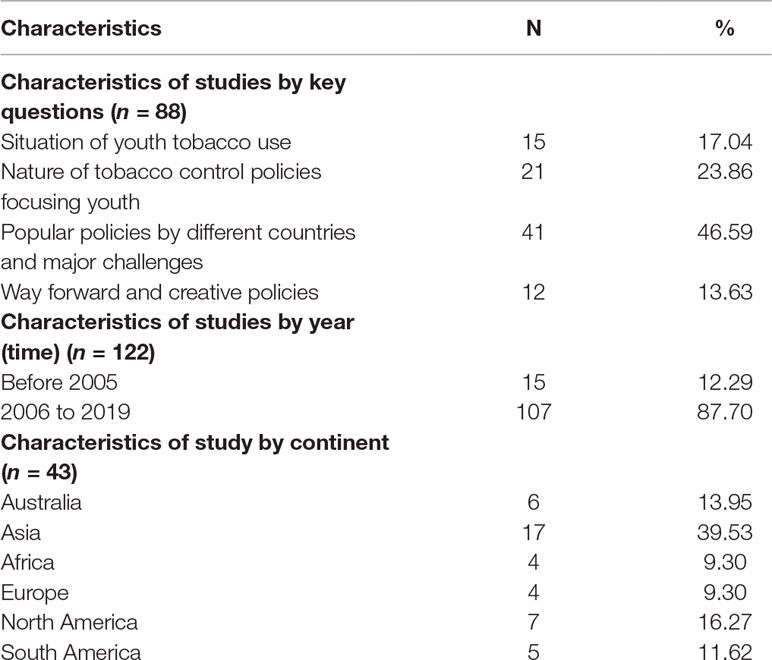
Table 1 General characteristics of included studies based on key questions, time interval, and region.
Analysis on Risk of Bias
Risk of bias analysis is not perfectly attractive with our study. We did not analyze the attrition bias because our study is a comparison of interventional studies and attrition bias occurs for randomized control trials. Moreover, we had very low influence of selection bias because all the interventions in this study were based on WHO MPOWER strategies. Studies by country and continent are not in equal proportion. We found that there were few studies in Africa, and more studies were available for Asia, but the creative policies we presented have no geographical boundaries. The number of studies for Asian countries is more than that from other continents because Asia has more than 2/3 of the world population and there are a higher number of countries compared to other continents. Most importantly, we focused on the policies related to youth and policies applicable to all age groups; gender and location were not prioritized. We applied almost all national representative survey results and global studies. There were no significant issues on data collection from the aspect on risk of bias.
Synthesis of Result
We synthesized the results via a descriptive approach in three perspectives. The first one is youth-targeted current pattern of tobacco control policies and their impact. We have divided the policy pattern into two categories: i) protect the youth form tobacco use and ii) help the youth quit tobacco use. Likewise, we compared the effectiveness and challenges of tobacco control in different countries. Other important aspects are global challenges and ways on controlling tobacco use among youth.
Patterns of Youth Tobacco Control Policies
Over the past two decades, a number of tobacco control policies have been implemented to prevent smoking initiation and encourage cessation among adolescents. To expand the fight against the tobacco epidemic, WHO introduced MPOWER, an initiative that includes six strategies: monitor tobacco use and prevention policies; protect people from tobacco smoke; offer help to people who want to quit using tobacco; warn about the dangers of tobacco; enforce bans on tobacco advertising, promotion, and sponsorship; and raise taxes on tobacco (World Health Organization, 2008). The effectiveness of MPOWER on youth is distinct. The International Agency for Research on Cancer (IARC) found that after increasing the tax and price of tobacco, there was significant reduction in tobacco use because youth are price sensitive and have a limited amount of resources (World Health Organization, 2011). Similarly, the smoke-free air law has a protective effect on young people and reduced smoking prevalence among boys of high socioeconomic status (Tauras et al., 2013). Most youth are influenced by tobacco advertisements, and according to the WHO, 24 countries have implemented a complete ban on direct and indirect tobacco advertising, promotion and sponsorship (TAPS) (World Health Organization, 2013). A study in 19 developing countries showed that there was a positive correlation between smoking and exposure to advertising (Kostova and Blecher, 2013). There were no appropriate research examining the effectiveness of offering to quit tobacco/smoking and warning of the harmful effects of tobacco applicable for youth. Therefore, in high-, (Dupont and Ward, 2002) low-, and middle-income countries, (Joseph, 2010) raising the price of tobacco and the tax on tobacco is more effective in reducing youth tobacco use than other strategies. The US Centers for Disease Control and Prevention (CDC) identified seven basic principles for tobacco control; three of these policies are relevant to youth: reducing tobacco use among adolescents; reducing the initiation of tobacco use among children, adolescents, and young adults; and increasing smoking cessation attempts among adolescent smokers (Centers for Disease Control Prevention (CDC)., 2007). A tobacco control plan in the United Kingdom has implemented three strategies to protect youth from tobacco use: reducing tobacco consumption, supporting parents and youths, and reinforcing the benefits of clean air spaces (National Health Service., 2015). Policy researchers have classified tobacco control initiatives into two groups: those intending to prevent first-time tobacco users (adolescents) and those aiming for cessation of tobacco use among current users, including both occasional and frequent users. These initiatives are based on multipronged approach, described below.
Disconnect Youth From Tobacco and Use Advertising Campaigns and Laws to Demotivate Youth From Tobacco Consumption
Popular policies within this guideline include cigarette tax increases, smoke-free air laws, and youth access laws (laws on sales to minors and laws against youth possession, use, and purchase)(Warner et al., 2003). Ross and Chaloupka highlighted that in the United States, higher cigarette prices reduced the probability of youth smoking, and the teen-specific perceived price of cigarettes had a negative effect on demand (Ross and Chaloupka, 2003). Similar findings have been reported by other researchers, and some have found that increased price decreased current smoking prevalence and the number of cigarettes smoked per day among youth and young adult smokers (Wasserman et al., 1991; Tauras, 2004; Levy et al., 2004). Other approaches to discourage adolescent smoking are restrictions on smoking at home, more extensive bans on smoking in public places, and enforced bans on smoking at school (Wakefield et al., 2000; Farkas et al., 2000). Sales to minors (STM) laws, which penalize merchants and retailers for selling tobacco to youth, and possession, use, and purchase laws, which punish youth themselves for possessing, using, or purchasing tobacco products, have also been applied (Rabin and Sugarman, 2001). Some studies have revealed an association between youth access and STM laws, but a sustained relationship between those laws and decreased youth smoking prevalence has been questioned. A study from Bangladesh shows that youth are more vulnerable due to a tobacco-friendly environment in school (Kabir et al., 2013). When the price increase policy was endorsed in the United States, it had a mixed impact, but a systematic review revealed no significant change in youth smoking. This law was also controversial, and cases were brought to court (Jason et al., 2005). Raising taxes on tobacco and STM laws have thus shown mixed effects, along with legal restrictions on adolescent smoking in the United States.
Increasing Smoking Cessation
Tobacco cessation, especially smoking cessation, depends on patterns of smoking such as age, peer pressure, influences of electronic media, and effective counseling to users. Among youth, quitting smoking has had no special program, and only 2–8% of youth smokers have attempted to quit in the Grimshaw et al., 2003 study. Hodder et al. suggested that universal school-based interventions could be an effective way to get youth to quit using tobacco and alcohol (Hodder et al., 2014).
In family and school, both approaches can be equally useful because some family members, teachers, and seniors need to quit smoking and pupils at risk must be disconnected from the first puff of smoking. Preventing youth from starting tobacco use is more effective and costs less than helping users quit, but no proper comparative studies have examined the different patterns and effects of youth tobacco control policies.
Major National Tobacco Control Policies Intervention, Outcomes, and Challenges
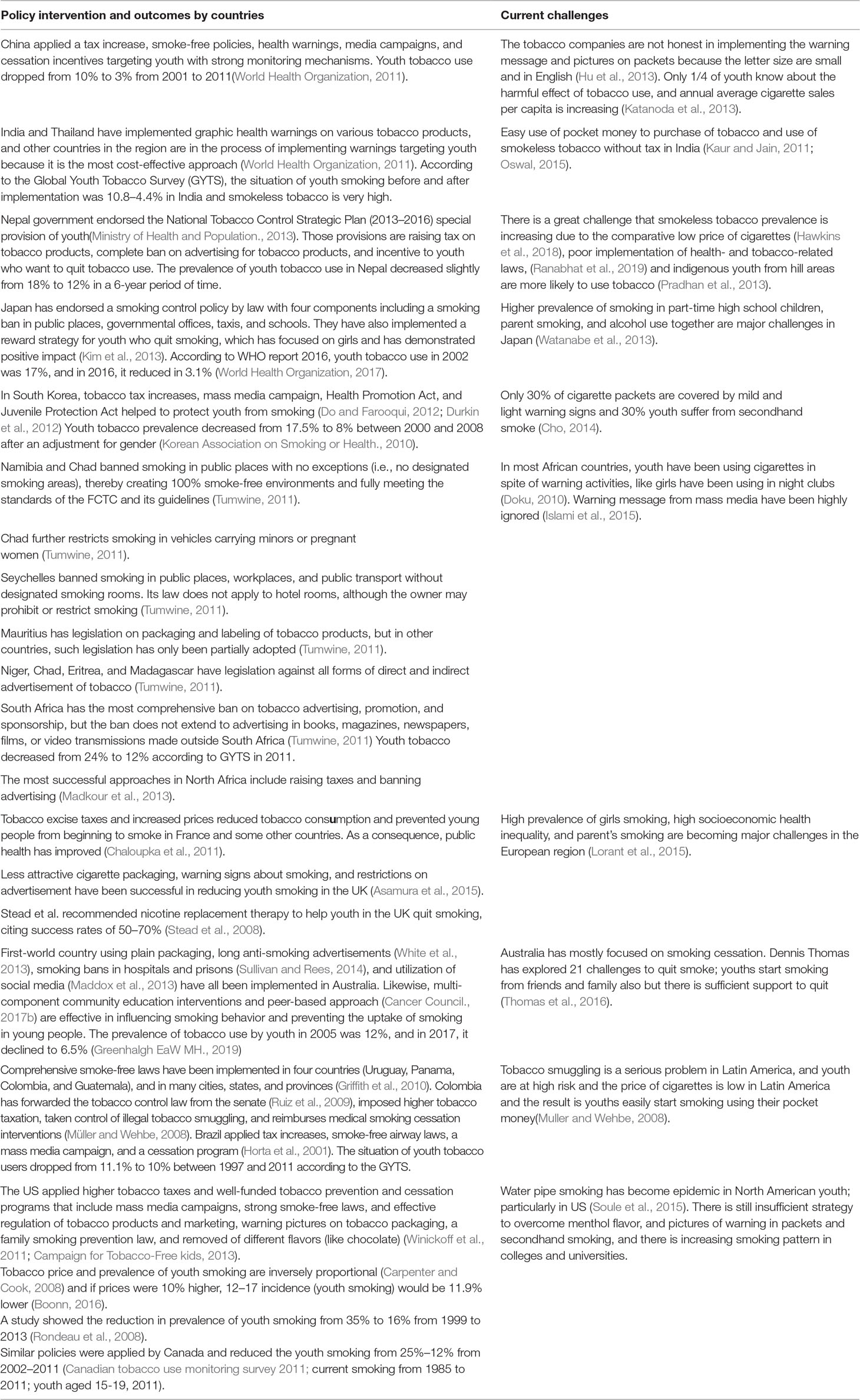
Table 2 shows the national tobacco control policies targeting youth. In 26 studies, researchers explored the overview and impact of youth-related tobacco control policies from China, India, Nepal, Thailand, Japan, South Korea, Namibia, Chad, Seychelles, Mauritius, Niger, Eritrea, Madagascar, South Africa, North Africa, France, United Kingdom, Australia, Uruguay, Panama, Colombia, Guatemala, Brazil, United States, and Canada. Likewise, in 15 studies, the challenges to control tobacco use in those countries were investigated. Seven studies were used as representative of global situations and challenges.
The direction of current policies has shifted significantly after WHO FCTC in tobacco control movement. The average strength of policies adopted varies significantly by country efforts. Cultural diversity leads to different pros and cons of tobacco control initiatives to any age, gender, geography, etc., and these subtleties must be taken into account when forming policies, and the FCTC was implemented on a national and local level.
A report of the US Surgeon General in 2012 showed that the global youth tobacco use rate was decreasing satisfactorily; the rate was 28% in 2000 and had declined to 8% by 2013 (Health UDo, Services H., 2012), but that survey did not match the GYTS of 2011. WHO FCTC has a comprehensive and global impact, specific to reducing the burden of youth tobacco use, but countries are reluctant to take proactive roles and prepare specific strategies due to lack of strong monitoring by WHO (Warner and Tam, 2012). Nevertheless, taxation, clean indoor air policies, and warning labels are ranked as the highest priorities but are general approaches, and there is still a need for more specific guidelines, integrated approaches, and age-specific tobacco control initiatives.
Tobacco companies around the world are focusing on strategic plans to block the implementation of Article 11 of the WHO FCTC, which sets guidelines on packaging and labeling of tobacco products (Sebrié et al., 2010) because youth are their target group as after they have become addicted, youth become regular customers. Tobacco companies have the power and money to influence legislators (Patel et al., 2007) and challenge the government’s legislative powers through litigation (Holden and Lee, 2009). The British American Tobacco (BAT) company’s former quality controller appealed against the ban on public smoking in Uganda; however, it was not successful. The tobacco industry in Kenya went to court to challenge the Tobacco Control Act of 2007, which created challenges for public smoking ban in public places (Tumwine, 2011). Similar cases have also been seen in the US high courts without decisions, representing a challenge to implement the WHO FCTC. Tobacco companies have litigated against new cigarette labeling policies in Uruguay, Brazil, and Paraguay to stop or delay the implementation of pictorial warnings (Sebrié et al., 2010) Thus, tobacco control stakeholders and tobacco production, manufacturing, and distribution companies need to continue to fight. It shows that tobacco companies may be a negative influence on youth-friendly tobacco control policies in the future.
Discussion
The WHO FCTC sought to substantially reduce and sustain reductions in indoor smoking and had high levels of public support and a strong public commitment with close monitoring in France, (Fong et al., 2013) China, (Levy et al., 2014) the United States and Canada, (House of Representative, USA., 2009; Levy et al., 2011; Hitchman et al., 2013) South Africa, (Reddy et al., 2013) South Korea, (Levy et al., 2010) and Brazil (Levy et al., 2012) (Table 1). The popular policies were tax increase, restriction on advertisement, and smoking ban in public places, but the most effective policy is raising the tax on tobacco products (Health NCfCDPaHPUOoSa., 2012) Abuse of youth to promote smoking by companies and smuggling are major challenges, particularly in Africa and South America. The above policies showed that hard policies (legal provision) could be more effective and long lasting. Some creative soft policies (program and interventions) were also equally effective but policies related to tobacco cessation are not enough. Primarily, strong monitoring and creative preventive policies led to satisfactory reduction on prevalence on youth tobacco use.
In our study, we explored the need to formulate tobacco control policies by age groups, and the vulnerable age group is the youth; there is a need for a preventive way that is cost-effective and a lesser burden to the disease both clinically and economically. There are some similar conclusions in our studies. Saleheen et al. suggested that there is need for targeted policies for youth and burden of diseases produced by tobacco (Saleheen et al., 2014). Another systematic review by Jawad with 36 studies from 15 countries yielding 125 elasticity estimates found that a 10% price increase would reduce demand by 8.3% for cigars, 6.4% for roll your owns, 5.7% for bidis, and 2.1% for smokeless tobacco (Jawad et al., 2018), mostly to youth (Levy et al., 2018). Another systematic review from 16 studies by Duncan found that a tobacco control approach in health care settings is more effective than in school and at home (Duncan et al., 2018). A policy review by Glantz concluded that e-cigarettes are replacing conventional cigarettes, but it is not a good approach to reducing nicotine dependency (Glantz and Bareham, 2018). Now, the JUUL lab’s mission is to eliminate cigarettes, but it does not relieve nicotine dependency as it only replaces traditional tobaccos; the challenge for JUUL is to eliminate nicotine dependency in the future. The tobacco control project period is also a significant factor because comprehensive tobacco control programs lead to an 8% short-term relative reduction, increasing to a 12% long-term relative reduction in smoking prevalence through the greater impact on youth smoking (Levy et al., 2018).
Way Forward
We discussed the situation of youth tobacco use, its effectiveness, and major challenges. Now, there is the question of the way forward. UN sustainable development goal 3a indicates strengthening the implementation of the WHO Framework Convention on Tobacco Control in all countries, as appropriate. Multiple impacts of tobacco control focusing on youth directly reduce adult and premature mortality rate (Ranabhat et al., 2017). Thus, there is a need for specific policies by age because growth and development, psychology, social environment, responsibilities, and pathophysiology are not similar for all ages. In this line, there should be different policies, programs, interventions, and remedies. Similarly, the priority of tobacco control should be different because intervention for youth and the elderly does not provide similar outcomes. Other public health projects like maternal health, child reproductive health, disease control, etc., are a matter of resource allocation, and we expect measurable outcomes in each micro activity. There is no debate that tobacco prevention for youth ensures low cost and higher output. The funding organizations for tobacco control have not encouraged or disappointed because such organizations have not provided significant outcomes. If we distinguish by age, specific tobacco control, and prevention program, funding projects may revisit their policies and invest more on youth due to their economic productive life. It is possible because youth have short exposure to tobacco addiction, can make strong commitments to quit tobacco, are easy to motivate to quit tobacco, and have family and social pressure in comparison with adults and the elderly. A similar analysis can be found in The State of Youth Tobacco Prevention and Control Spending in Alabama: Struggles, Consequences, and Solutions report 2014 (Dunlap and McCallum, 2014).
The average strength of policies varied significantly by country. The success of tobacco control initiatives was significantly associated with the number and types of policy adopted (Wipfli and Huang, 2011). In European countries, limiting youth exposure to smoking in movies might be an effective way to prevent adolescent smoking onset (Morgenstern et al., 2013). In addition, a family smoking prevention law in the United States has reduced the prevalence of youth smoking (Ribisl, 2012). Recently, Nepal drafted a clear provision that people who use tobacco (including smokeless tobacco) will not be eligible as government employees; this policy is appealing because it directly affects unemployed youth (Sinha et al., 2012). Peer-based approach projects are best models in youth tobacco control in Australia. Youth are active users of social media such as Facebook, Twitter, YouTube, Messenger, and other apps. Creative mobilization of information technology could be useful for implementation and monitoring of youth tobacco use (Freeman, 2012). Social drama, documentary, family movies, cartoons about tobacco use impact on youth from elementary school could also discourage youth from using tobacco (Merchant, 2013). Hence, appropriate use of mass media and social network is more effective. The e-cigarette is another option for tobacco control, but regulatory issues surrounding audit of electronic cigarettes is unknown (Jovanovic and Jakovljevic, 2015). A systematic review by Park et al. concluded that the use of multimedia, tailored approaches, personalized feedback, and interactive feature programs could positively affect tobacco prevention and cessation (Park and Drake, 2015). Likewise, receptivity to tobacco advertising was significantly associated with progression toward use in adolescents (Pierce et al., 2018).
Strengths and Limitations
This article describes tobacco control policies with a focus on the younger generation. This is an issue that is significant but often neglected. This article is intended for a wide range of readers (basic readers to policy makers, policy researchers, and other stakeholders related to tobacco control). However, this paper also has some limitations. We used the term youth as used by different authors in their articles and context than any fixed age. Here, we have used terms such as boys, girls, adolescents, elder children, and teenagers synonymously with youth. Tobacco use is focused mostly on smoking, though smokeless tobacco is also a major problem that the world also needs to face. Being a comprehensive review, all components of systematic review and meta-analysis are not applicable to use.
Conclusion
About 1/5 of youth used tobacco globally and it has multiple impacts on health economy and family integrity. The prevalence of tobacco use is decreasing but not at a satisfactory rate. The policies of tobacco control adopted by many countries are based on the WHO Framework Convention on Tobacco Control but have not necessarily focused on youth. Due to the physical and economic burden of tobacco consumption by youth, this is a high priority that needs to be addressed. In this digital age, creative tobacco control policies focusing on youth must be applied. Successful policies of tobacco control for youth that need to be replicated by context, country, region, and gender can be recommended. Tobacco control should be a social, public health, and quality-of-life concern rather than a business and trade issue.
Author Contributions
CR prepared the research concept and framework, collected the articles, prepared the manuscript, and overall pursued the article. C-BK verified the concept, verified the reference, and reviewed the manuscript. MBP verified all references and prepared the composition of contents. MJ reviewed the manuscript and rearranged some parts.
Funding
This study was supported by a National Research Foundation Grant of Korea, Korean Government (NRF-2016S1A5B892520) and the Korean Medical Association (RIHP-2015-02).
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Abbreviations
CDC, Centers for Disease Control and Prevention; FCTC, Framework Convention on Tobacco Control; GYTS, Global Youth Tobacco Survey; NRF, National Research Foundation; STM, Sales to minor; WHO, World Health Organization; IARC, International Agency for Research on Cancer; BAT, British American Tobacco.
Acknowledgments
We sincerely acknowledge Prof. Indeok Kong, Dr. Shambu Prasad Acharaya (WHO), Dr. Nabin Baral and Arthur Atkinson for their quick review and Margaret Storey for English language improvement.
References
Agaku, I., King, B., Dube, S. R., Office on Smoking and Health, National Center for Chronic Disease Prevention and Health Promotion, CDC. (2013). Current cigarette smoking among adults—United States, 2011. JAMA. 309(6):539–541. doi 10.1001/jama.201.114523
Ajzen, I., Fishbein, M. (1970). The prediction of behavior from attitudinal and normative variables. J. Exp. Soc. Psychol. 6 (4), 466–487. doi: 10.1016/0022-1031(70)90057-0
Alexander, C., Piazza, M., Mekos, D., Valente, T. (2001). Peers, schools, and adolescent cigarette smoking. J. Adolesc. Health 29 (1), 22–30. doi: 10.1016/S1054-139X(01)00210-5
Al-Sadat, N., Misau, A., Zarihah, Z., Maznah, D., Su, T. T. (2010). Adolescent tobacco use and health in South East Asia. Asia-Pac. J. Public Health 22 (3 suppl), 175S–180S. doi: 10.1177/1010539510372835
Arrazola, R. A., Neff, L. J., Kennedy, S. M., Holder-Hayes, E., Jones, C. D., Centers for Disease and Control Prevention (CDC). (2014). Tobacco use among middle and high school students—United States, 2013. MMWR Morb. Mortal. Wkly. Rep. 63 (45), 1021–1026.
Asamura, H., Chansky, K., Crowley, J., Goldstraw, P., Rusch, V. W., Vansteenkiste, J. F., et al. (2015). The International Association for the Study of Lung Cancer Staging Project: proposals for the revision of the N descriptors in the forthcoming 8th edition of the TNM classification for lung cancer. J. Thorac. Oncol. 10 (12), 1675–1684. doi: 10.1097/JTO.0000000000000678
Bandura, A. (1976). Social learning theory. Stanford University. New York, USA: General Learning Press.
Blum, L. A. (2009). Friendship, altruism and morality (Routledge Revivals). New York, USA: Routledge (Taylor & Francis Group). doi: 10.4324/9780203857304
Boonn, A. (2016). Raising cigarette taxes reduces smoking, especially among kids (and the cigarette companies know it). Campaign Tob. Free Kids. https://www.tobaccofreekids.org/assets/factsheets/0146.pdf
Campaign for Tobacco-Free Kids. New survey shows U.S. youth smoking rates fell to record lows in 2013. (2013) http://www.tobaccofreekids.org/press_releases/post/2013_12_18_youth_rates. Accessed May 05, 2015.
Canada. (2011). Canadian Tobacco Use Monitoring Survey (CTUMS) 2011: https://www.canada.ca/en/health-canada/services/publications/healthy-living/canadian-tobacco-use-monitoring-survey-ctums-2011.html?wbdisable=true. Accessed August 14 2018.
Cancer Council. (2017b). Peer Based Approach. http://www.tobaccoinaustralia.org.au/chapter-5-uptake/5-28-peer-based-approaches.
Carpenter, C., Cook, P. J. (2008). Cigarette taxes and youth smoking: new evidence from national, state, and local youth risk behavior surveys. J. Health Econ. 27 (2), 287–299. doi: 10.1016/j.jhealeco.2007.05.008
Centers for Disease Control and Prevention., Cigarette smoking among adults and trends in smoking cessation—United States 2012. (2000).
Centers for Disease Control Prevention (CDC) (2007). Best practices for comprehensive tobacco control programs 2007. Atlanta: U.S. Department of Health and Human Services, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health.
Chaloupka, F. J., Straif, K., Leon, M. E. (2011). Effectiveness of tax and price policies in tobacco control. Trop. Biomed. 20 (3), 235–238. doi: 10.1136/tc.2010.039982
Cho, H. J. (2014). The status and future challenges of tobacco control policy in Korea. J. Prev. Med. Public Health 47 (3), 129. doi: 10.3961/jpmph.2014.47.3.129
Do, Y. K., Farooqui, M. A. (2012). Differential subjective responsiveness to a future cigarette price increase among South Korean youth smokers. Nicotine Tob. Res. 14 (2), 209–216. doi: 10.1093/ntr/ntr187
Doku, D. (2010). The tobacco industry tactics—a challenge for tobacco control in low and middle income countries. Afr. Health Sci. 10 (2), 201–203.
Duncan, L. R., Pearson, E. S., Maddison, R. (2018). Smoking prevention in children and adolescents: a systematic review of individualized interventions. Patient Educ. Couns. 101 (3), 375–388. doi: 10.1016/j.pec.2017.09.011
Dunlap, S. T., McCallum, D. M. (2014). The state of youth tobacco prevention and control spending in Alabama: struggles, consequences, and solutions. Alabama: The Institute for Social Science Research, University of Alabama.
Dupont, D., Ward, A. J. (2002). The economic impacts of cigarette tax reductions on youth smoking in Canada. Ste-Catherines: Brock University.
Durkin, S., Brennan, E., Wakefield, M. (2012). Mass media campaigns to promote smoking cessation among adults: an integrative review. Trop. Biomed. 21 (2), 127–138. doi: 10.1136/tobaccocontrol-2011-050345
Eriksen, M., Mackay, J., Schluger, N. (2015). The tobacco atlas. Fifth Atlanta: The American Cancer Society.
Ertas, N. (2007). Factors associated with stages of cigarette smoking among Turkish youth. Eur. J. Public Health 17 (2), 155–161. doi: 10.1093/eurpub/ckl095
Farkas, A. J., Gilpin, E. A., White, M. M., Pierce, J. P. (2000). Association between household and workplace smoking restrictions and adolescent smoking. J. Am. Med. Assoc. 284 (6), 717–722. doi: 10.1001/jama.284.6.717
Fong, G. T., Craig, L. V., Guignard, R., Nagelhout, G. E., Tait, M. K., Driezen, P., et al. (2013). Evaluating the effectiveness of France’s indoor smoke-free law 1 year and 5 years after implementation: findings from the ITC France survey. PloS One 8 (6), e66692. doi: 10.1371/journal.pone.0066692
Freeman, B. (2012). New media and tobacco control. Trop. Biomed. 21 (2), 139–144. doi: 10.1136/tobaccocontrol-2011-050193
Glantz, S. A., Bareham, D. W. (2018). E-cigarettes: Use, effects on smoking, risks, and policy implications. Annu. Rev. Public Health 39, 215–235. doi: 10.1146/annurev-publhealth-040617-013757
Greenhalgh, EaW, MH. (2019). Tobacco in Australia: comprehensive online sources. https://www.tobaccoinaustralia.org.au/chapter-1-prevalence/1-6-prevalence-of-smoking-teenagers.
Griffith, G., Cardone, A., Jo, C., Valdemoro, A., Sebrié, E. (2010). Implementation of smokefree workplaces: challenges in Latin America. SciElo Public Health 52, S347–S354. doi: 10.1590/S0036-36342010000800033
Grimshaw, G., Stanton, A., Blackburn, C., Andrews, K., Grimshaw, C., Vinogradova, Y., et al. (2003). Patterns of smoking, quit attempts and services for a cohort of 15-to 19-year-olds. Child Care Health Dev. 29 (6), 457–464. doi: 10.1046/j.1365-2214.2003.00365.x
Hawkins, S. S., Bach, N., Baum, C. F. (2018). Impact of tobacco control policies on adolescent smokeless tobacco and cigar use: a difference-in-differences approach. BMC Public Health 18 (1), 154. doi: 10.1186/s12889-018-5063-z
Health UDo, Services H. (2012). Preventing tobacco use among young people: a report of the Surgeon General. Atlanta, GA: US Department of Health and Human Services, Public Health Service, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health.
Hefler, M., Chapman, S. (2014). Disadvantaged youth and smoking in mature tobacco control contexts: a systematic review and synthesis of qualitative research. Trop. Biomed. 5 (17), 56. doi: 10.1136/tobaccocontrol-2014-051756
Higgins, J., Green, S. (2011). Cochrane handbook for systematic reviews of interventions version 5.1. 0. London, UK: the cochrane collaboration.
Hitchman, S. C., Driezen, P., Logel, C., Hammond, D., Fong, G. T. (2013). Changes in effectiveness of cigarette health warnings over time in Canada and the United States, 2002–2011. Nicotine Tob. Res. 16 (5), 536–543. doi: 10.1093/ntr/ntt196
Hodder, R. K., Freund, M., Wolfenden, L., Bowman, J., Gillham, K., Dray, J., et al. (2014). Systematic review of universal school-based resilience interventions targeting adolescent tobacco, alcohol or illicit drug use: review protocol. BMJ Open 4 (5), e004718. doi: 10.1136/bmjopen-2013-004718
Holden, C., Lee, K. (2009). Corporate power and social policy the political economy of the transnational tobacco companies. Glob. Soc. Policy 9 (3), 328–354. doi: 10.1177/1468018109343638
Horta, B. L., Calheiros, P., Pinheiro, R. T., Tomasi, E., Amaral, K. D. (2001). Tobacco smoking among teenagers in an urban area in Southern Brazil. Rev. Saúde. Pública. 35 (2), 159–164. doi: 10.1590/S0034-89102001000200009
House of Representative, USA. (2009). A family smoking prevention and tobacco control act. In: Public Law.
Hu, T. W., Lee, A. H., Mao, Z. (2013). WHO Framework Convention on Tobacco Control in China: barriers, challenges and recommendations. Glob. Health Promot. 20 (4), 13–22. doi: 10.1177/1757975913501910
Islami, F., Stoklosa, M., Drope, J., Jemal, A. (2015). Global and regional patterns of tobacco smoking and tobacco control policies. Eur. Urol. Focus 1 (1), 3–16. doi: 10.1016/j.euf.2014.10.001
Jason, L. A., Pokorny, S. B., Muldowney, K., Velez, M. (2005). Youth tobacco sales-to-minors and possession-use-purchase laws: a public health controversy. J. Drug Educ. 35 (4), 275–290. doi: 10.2190/1F1R-KGTL-PVDE-V9EJ
Jawad, M., Lee, J. T., Glantz, S., Millett, C. (2018). Price elasticity of demand of non-cigarette tobacco products: a systematic review and meta-analysis. Tob. Control 27 (6), 689–695. doi: 10.1136/tobaccocontrol-2017-054056
Jessor, R., Jessor, S. L. (1977). Problem behavior and psychosocial development: a longitudinal study of youth. New York, USA: Academic Press.
Jovanovic, M., Jakovljevic, M. (2015). Regulatory issues surrounding audit of electronic cigarette charge composition. Front. Psychiatry 6, 133. doi: 10.3389/fpsyt.2015.00133
Kabir, M., Goh, K.-L., Khan, M. (2013). Adolescent tobacco use and its determinants evidence from Global Youth Tobacco Survey. Asia-Pac. J. Public Health 27 (2), 1579–1589. doi: 10.1177/1010539512472357
Katanoda, K., Jiang, Y., Park, S., Lim, M. K., Qiao, Y. L., Inoue, M. (2014). Tobacco control challenges in East Asia: proposals for change in the world’s largest epidemic region. Tob. Control 23 (4), 359–368. doi: 10.1136/tobaccocontrol-2012-050852
Kaur, J., Jain, D. (2011). Tobacco control policies in India: implementation and challenges. Indian J. Public Health 55 (3), 220. doi: 10.4103/0019-557X.89941
Khuder, S. A., Price, J. H., Jordan, T., Khuder, S. S., Silvestri, K. (2008). Cigarette smoking among adolescents in Northwest Ohio: correlates of prevalence and age at onset. Int. J. Environ. Res. Public Health 5 (4), 278–289. doi: 10.3390/ijerph5040278
Kim, J. A., Lee, C. Y., Lim, E. S., Kim, G. S. (2013). Smoking cessation and characteristics of success and failure among female high-school smokers. Jpn. J. Nurs. Sci. 10 (1), 68–78. doi: 10.1111/j.1742-7924.2012.00212.x
Konopka, G. (1973). Requirements for healthy development of adolescent youth. Adolescence 8 (31), 291-316. https://psycnet.apa.org/record/1974-22647-001
Korean Association on Smoking or Health. (2010). Smoking Prevalence of Youth http://www.kash.or.kr/user_new/pds_view.asp.
Kostova, D., Blecher, E. (2013). Does advertising matter? Estimating the impact of cigarette advertising on smoking among youth in developing countries. Contemp. Econ. Policy 31 (3), 537–548. doi: 10.1111/j.1465-7287.2012.00323.x
Levy, D. T., Chaloupka, F., Gitchell, J. (2004). The effects of tobacco control policies on smoking rates: a tobacco control scorecard. J. Public Health Manage. Pract. 10 (4), 338–353. doi: 10.1097/00124784-200407000-00011
Levy, D. T., Cho, S. I., Kim, Y. M., Park, S., Suh, M. K., Kam, S. (2010). SimSmoke model evaluation of the effect of tobacco control policies in Korea: the unknown success story. Am. J. Public Health 100 (7), 1267–1273. doi: 10.2105/AJPH.2009.166900
Levy, D. T., Pearson, J. L., Villanti, A. C., Blackman, K., Vallone, D.M., Niaura, R. S., et al. (2011). Modeling the future effects of a menthol ban on smoking prevalence and smoking-attributable deaths in the United States. Am. J. Public Health 101 (7), 1236–1240. doi: 10.2105/AJPH.2011.300179
Levy, D., de Almeida, L. M., Szklo, A. (2012). The Brazil SimSmoke policy simulation model: the effect of strong tobacco control policies on smoking prevalence and smoking-attributable deaths in a middle income nation. PLoS Med. 9 (11), e1001336. doi: 10.1371/journal.pmed.1001336
Levy, D., Rodríguez-Buño, R. L., Hu, T. W., Moran, A. E. (2014). The potential effects of tobacco control in China: projections from the China SimSmoke simulation model. Br. Med. J. 348 (10), g1134. doi: 10.1136/bmj.g1134
Levy, D. T., Tam, J., Kuo, C., Fong, G. T., Chaloupka, F. (2018). Research full report: the impact of implementing tobacco control policies: the 2017 tobacco control policy scorecard. J. Public Health Manage. Pract. 24 (5), 448. doi: 10.1097/PHH.0000000000000780
Lim, K. H., Sumarni, M., Kee, C. C., Christopher, V. M., Noruiza Hana, M., Lim, K. K., et al. (2010). Prevalence and factors associated with smoking among form four students in Petaling District, Selangor, Malaysia. Trop. Biomed. 27 (3), 394–403.
Lindblom, E. (2005). Raising cigarette taxes reduces smoking, especially among kids (and the cigarette companies know it). Campaign for Tobacco-Free Kids, January 31. (Smoke Free South Carolina). https://www.tobaccofreekids.org/microsites/passthebuck_sc/resources/sccigtaxandkids.pdf. Accessed May 05, 2015.
Lorant, V., Soto, V. E., Alves, J., Federico, B., Kinnunen, J., Kuipers, M., et al. (2015). Smoking in school-aged adolescents: design of a social network survey in six European countries. BMC Res. Notes 8 (1), 91. doi: 10.1186/s13104-015-1041-z
Maddox, R., Davey, R., Cochrane, T., Lovett, R., van der Sterren, A. (2013). Study protocol—Indigenous Australian social networks and the impact on smoking policy and programs in Australia: protocol for a mixed-method prospective study. BMC Public Health 13 (1), 879. doi: 10.1186/1471-2458-13-879
Madkour, A. S., Ledford, E. C., Andersen, L., Johnson, C. C. (2013). Tobacco advertising/promotions and adolescents’ smoking risk in Northern Africa. Trop. Biomed. 23, 244–252. doi: 10.1136/tobaccocontrol-2012-050593
Merchant, Z. F. (2013). A study on the depiction of drug usage, alcohol consumption and cigarette smoking in movies and its perceived effect on a young audience. A comparative study of American and Indian cinema and their respective Audiences. South Florida: Department of Mass Communications University of South Florida.
Ministry of Health and Population. (2013). National Tobacco Control Strategic Plan (2013–2016). Teku, Kathmandu, Nepal: National Health Education Information and Communication Center.
Morgenstern, M., Sargent, J. D., Engels, R. C. M. E., Scholte, R. H. J., Florek, E., Hunt, K., et al. (2013). Smoking in movies and adolescent smoking initiation: Longitudinal study in six European countries. Am. J. Prev. Med. 44 (4), 339–344. doi: 10.1016/j.amepre.2012.11.037
Muller, F., Wehbe, L. (2008). Smoking and smoking cessation in Latin America: a review of the current situation and available treatments. Int. J. Chron. Obstruct. Pulmon. Dis. 3 (2), 285. doi: 10.2147/COPD.S2654
Müller, F., Wehbe, L. (2008). Smoking and smoking cessation in Latin America: a review of the current situation and available treatments. Int. J.COPD 3 (2), 285–293. doi: 10.2147/COPD.S2654
National Health Service. (2015). Smokefree. 2015/03/15; https://www.nhs.uk/smokefree. Accessed 2015/03/15.
Nelson, D. E., Mowery, P., Asman, K., Pederson, L. L., O'Malley, P. M., Malarcher, A., et al. (2008). Long-term trends in adolescent and young adult smoking in the United States: metapatterns and implications. Am. J. Public Health 98 (5), 905–915. doi: 10.2105/AJPH.2007.115931
Ng, M., Freeman, M. K., Fleming, T. D., Robinson, M., Dwyer-Lindgren, L., Thomson, B., et al. (2014). Smoking prevalence and cigarette consumption in 187 countries, 1980–2012. J. Am. Med. Assoc. 311 (2), 183–192. doi: 10.1001/jama.2013.284692
Organization WH. (2011). WHO Report on The Global Tobacco Epidemic: Global youth tobacco survey data 2011. Geneva: World Health Organization.
Organization WH. (2013). WHO report on the global tobacco epidemic, 2013: Enforcing bans on tobacco advertising, promotion and sponsorship. World Health Organization.
Organization WH. (2017). WHO report on the global tobacco epidemic, 2017: Monitoring tobacco use and prevention policies. World Health Organization.
Oswal, K. C. (2015). Factors associated with tobacco use among adolescents in India results from the Global Youth Tobacco Survey, India. Asia-Pac. J. Public Health 27 (2), NP203–NP211. doi: 10.1177/1010539511436322
Park, E., Drake, E. (2015). Systematic review: internet-based program for youth smoking prevention and cessation. J. Nurs. Scholarsh. 47 (1), 43–50. doi: 10.1111/jnu.12104
Patel, P., Collin, J., Gilmore, A. B. (2007). The law was actually drafted by us but the Government is to be congratulated on its wise actions: British American Tobacco and public policy in Kenya. Trop. Biomed. 16 (1), e1–e1. doi: 10.1136/tc.2006.016071
Pierce, J. P., Sargent, J. D., Portnoy, D. B., White, M., Noble, M., Kealey, S., et al. (2018). Association between receptivity to tobacco advertising and progression to tobacco use in youth and young adults in the PATH Study. JAMA Pediat. 172 (5), 444–451. doi: 10.1001/jamapediatrics.2017.5756
Pradhan, P. M. S., Niraula, S. R., Ghimire, A., Singh, S. B., Pokharel, P. K. (2013). Tobacco use and associated factors among adolescent students in Dharan, Eastern Nepal: a cross-sectional questionnaire survey. BMJ Open 3 (2), e002123. doi: 10.1136/bmjopen-2012-002123
Ranabhat, C. L., Kim, C. B., Park, M. B., Acharaya, S. (2017). Multiple disparities in adult mortality in relation to social and health care perspective: results from different data sources. Glob. Health 13 (1), 57. doi: 10.1186/s12992-017-0283-z
Ranabhat, C. L., Atkinson, J., Park, M. B., Kim, C. B., Jakovljevic, M. (2018). The influence of universal health coverage on life expectancy at birth (LEAB) and healthy life expectancy (HALE): a multi-country cross-sectional study. Front. Pharmacol. 9, 960. doi: 10.3389/fphar.2018.00960
Ranabhat, C. L., Park, M. B., Kim, C. B., Kim, C. S., Jeong, H. S., Koh, S. B., et al. (2018). Influence of key health related indicators on adult mortality: result from UN member countries. Iran. J. Public Health 47 (6), 794–802.
Ranabhat, C. L., Kim, C. B., Singh, A., Acharya, D., Pathak, K., Sharma, B., et al. (2019). Challenges and opportunities towards the road of universal health coverage (UHC) in Nepal: a systematic review. Arch. Public Health 77 (1), 5. doi: 10.1186/s13690-019-0331-7
Reddy, P., James, S., Sewpaul, R., Yach, D., Resnicow, K., Sifunda, S., et al. (2013). A decade of tobacco control: the South African case of politics, health policy, health promotion and behaviour change. S. Afr. Med. J. 103 (11), 835–840. doi: 10.7196/samj.6910
Ribisl, K. M. (2012). Research gaps related to tobacco product marketing and sales in the family smoking prevention and tobacco control act. Nicotine Tob. Res. 14 (1), 43–53. doi: 10.1093/ntr/ntr098
Rondeau, V., Allain, H., Bakchine, S., Bonet, P., Brudon, F., Chauplannaz, G., et al. (2008). General practice-based intervention for suspecting and detecting dementia in France: a cluster randomized controlled trial. Dementia 7 (4), 433–450. doi: 10.1177/1471301208096628
Ross, H., Chaloupka, F. J. (2003). The effect of cigarette prices on youth smoking. Health Econ. 12 (3), 217–230. doi: 10.1002/hec.709
Ruiz, M. A., Rivera-Rodríguez, D. E., Marín, Y., González, J. C., Moreno, R. H. (2009). Tobacco control initiatives in Colombia’s congress, 1992-2007. Rev. Panam. Salud Publica/Pan. Am. J. Public Health 25 (6), 471–480.
Saleheen, D., Zhao, W., Rasheed, A. (2014). Epidemiology and public health policy of tobacco use and cardiovascular disorders in low- and middle-income countries. Arterioscler. Thromb. Vasc. Biol. 34 (9), 1811–1819. doi: 10.1161/ATVBAHA.114.303826
Sebrié, E. M., Blanco, A., Glantz, S. A. (2010). Cigarette labeling policies in Latin America and the Caribbean: progress and obstacles. Salud Pública Méx. 52, S233–S243. doi: 10.1590/S0036-36342010000800019
Simons-Morton, B., Crump, A. D., Haynie, D. L., Saylor, K. E., Eitel, P., Yu, K. (1999). Psychosocial, school, and parent factors associated with recent smoking among early-adolescent boys and girls. Prev. Med. 28 (2), 138–148. doi: 10.1006/pmed.1998.0404
Sinha, D., Bajracharya, B., Khadka, B., Rinchen, S., Bhattad, V., Singh, P. (2012). Smokeless tobacco use in Nepal. Indian J. Cancer 49 (4), 352. doi: 10.4103/0019-509X.107728
Soule, E. K., Lipato, T., Eissenberg, T. (2015). Waterpipe tobacco-smoking: a new smoking epidemic among the young? Curr. Pulmonol. Rep. 4 (4), 163–172. doi: 10.1007/s13665-015-0124-6
Stanton, A,, Grimshaw, G.. (2013). Tobacco cessation interventions for young people. Cochrane Database Syst. Rev. (8), CD003289. doi: 10.1002/14651858.CD003289.pub5
Stead, L. F., Perera, R., Bullen, C., Mant, D., Lancaster, T. (2008). Nicotine replacement therapy for smoking cessation. Cochrane Database Syst. Rev. 1 (1). CD000146. doi: 10.1002/14651858.CD000146.pub3
Sullivan, D. H., Rees, M. A. (2014). Smoking bans in secure psychiatric hospitals and prisons. J. Law Med. 22 (1), 22–30.
Tauras, J. A. (2004). Public policy and smoking cessation among young adults in the United States. Health Policy 68 (3), 321–332. doi: 10.1016/j.healthpol.2003.10.007
Tauras, J. A., Huang, J., Chaloupka, F. J. (2013). Differential impact of tobacco control policies on youth sub-populations. Int. J. Environ. Res. Public Health 10 (9), 4306–4322. doi: 10.3390/ijerph10094306
Thomas, D., Mackinnon, A. J., Bonevski, B., Abramson, M. J., Taylor, S., Poole, S. G., et al. (2016). Development and validation of a 21-item challenges to stopping smoking (CSS-21) scale. BMJ Open 6 (3), e011265. doi: 10.1136/bmjopen-2016-011265
Tumwine, J. (2011). Implementation of the framework convention on tobacco control in Africa: current status of legislation. Int. J. Environ. Res. Public Health 8 (11), 4312–4331. doi: 10.3390/ijerph8114312
United Nation. (2016) Definition of Youth 2009; http://www.un.org/esa/socdev/documents/youth/fact-sheets/youth-definition.pd. Accessed 05/22.
United States Congress House of Represen. (2010). Family Smoking Prevention and Tobacco Control ACT. BiblioGov. Washington DC, USA.
Vidhubala, E., Sahaya, G., Vijayalakshmi, S., Bharathi, P., Quarishy, Z. B. (2014). Prevalence of tobacco use among school children, exposure to passive smoking and their knowledge level about tobacco control in Chennai city, Tamil Nadu-A School Based Survey. J. Indian Assoc. Child Adolesc. Ment. Health 10 (2), 110–131.
Wakefield, M. A., Chaloupka, F. J., Kaufman, N. J., Orleans, C. T., Barker, D. C., Ruel, E. E. (2000). Effect of restrictions on smoking at home, at school, and in public places on teenage smoking: cross sectional study. Br. Med. J. 321 (7257), 333–337. doi: 10.1136/bmj.321.7257.333
Walker, S., Sanci, L., Temple-Smith, M. (2013). Sexting: young women's and men's views on its nature and origins. J. Adolesc. Health 52 (6), 697-701. doi: 10.1016/j.jadohealth.2013.01.026
Warner, K. E., Tam, J. (2012). The impact of tobacco control research on policy: 20 years of progress. Trop. Biomed. 21 (2), 103–109. doi: 10.1136/tobaccocontrol-2011-050396
Warner, K., Jacobson, P., Kaufman, N. (2003). Innovative approaches to youth tobacco control: introduction and overview. Trop. Biomed. 12 (suppl 1), i1–i5. doi: 10.1136/tc.12.suppl_1.i1
Wasserman, J., Manning, W. G., Newhouse, J. P., Winkler, J. D. (1991). The effects of excise taxes and regulations on cigarette smoking. J. Health Econ. 10 (1), 43–64. doi: 10.1016/0167-6296(91)90016-G
Watanabe, I., Shigeta, M., Inoue, K., Matsui, D., Ozaki, E., Kuriyama, N., et al. (2013). Personal factors associated with smoking among marginalized and disadvantaged youth in Japan. A strong relationship between smoking and convenience store use. Int. J. Behav. Med. 20 (4), 504–513. doi: 10.1007/s12529-012-9268-8
White, V. M., Durkin, S. J., Coomber, K., Wakefield, M. A. (2013). What is the role of tobacco control advertising intensity and duration in reducing adolescent smoking prevalence? Findings from 16 years of tobacco control mass media advertising in Australia. Trop. Biomed. 05 (09), 45. doi: 10.1136/tobaccocontrol-2012-050945
Winickoff, J. P., McMillen, R. C., Vallone, D. M., Pearson, J. L., Tanski, S.E., Dempsey, J. H., et al. (2011). US attitudes about banning menthol in cigarettes: results from a nationally representative survey. Am. J. Public Health 101 (7), 1234–1236. doi: 10.2105/AJPH.2011.300146
Wipfli, H., Huang, G. (2011). Power of the process: Evaluating the impact of the Framework Convention on Tobacco Control negotiations. Health Policy 100 (2), 107–115. doi: 10.1016/j.healthpol.2010.08.014
World Health Organization. (2008) WHO Report on the global tobacco epidemic, 2008: The MPOWER package. Geneva: World Health Organization.
World Health Organization. (2011) WHO report on the global tobacco epidemic, 2011: warning about the dangers of tobacco. Geneva: World Health Organization.
World Health Organization. (2011). WHO report on the global tobacco epidemic: Global youth tobacco survey data 2011. Geneva: World Health Organization.
World Health Organization. (2011). Effectiveness of tax and price policies for tobacco control. Geneva: World Health Organization.
World Health Organization. (2012). Global progress report on implementation of the WHO Framework Convention on Tobacco Control. Geneva: World Health Organization.
World Health Organization. (2013). WHO report on the global tobacco epidemic, 2013: Enforcing bans on tobacco advertising, promotion and sponsorship. Geneva: World Health Organization.
Keywords: tobacco control, smoking, policies, youth, preventive measure, tobacco products
Citation: Ranabhat CL, Kim C-B, Park MB and Jakovljevic M(M) (2019) Situation, Impacts, and Future Challenges of Tobacco Control Policies for Youth: An Explorative Systematic Policy Review. Front. Pharmacol. 10:981. doi: 10.3389/fphar.2019.00981
Received: 20 November 2018; Accepted: 31 July 2019;
Published: 09 September 2019.
Edited by:
Cristiane De Cássia Bergamaschi, Universidade de Sorocaba, BrazilReviewed by:
Juman Abdulelah Dujaili, Monash University Malaysia, MalaysiaJuan Carlos Sanchez-Salgado, Institute of Molecular Medicine and Advanced Sciences, Mexico
Robert L Lins, Independent Researcher, Antwerp, Belgium
HyunSook Lee, Kongju National University, South Korea
Copyright © 2019 Ranabhat, Kim, Park and Jakovljevic. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Chhabi Lal Ranabhat Y2hoYWJpckBnbWFpbC5jb20=; Chun-Bae Kim a2ltY2JAeW9uc2VpLmFjLmty
 Chhabi Lal Ranabhat
Chhabi Lal Ranabhat Chun-Bae Kim
Chun-Bae Kim Myung Bae Park
Myung Bae Park Mihajlo (Michael) Jakovljevic
Mihajlo (Michael) Jakovljevic