
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
CASE REPORT article
Front. Pediatr. , 14 March 2025
Sec. Pediatric Critical Care
Volume 13 - 2025 | https://doi.org/10.3389/fped.2025.1525365
This article is part of the Research Topic Rehabilitation of mechanically ventilated and tracheostomized patients View all articles
 Pien M. M. Weerkamp1
Pien M. M. Weerkamp1 Mark Voermans2
Mark Voermans2 Moniek Finders2
Moniek Finders2 Arno Brouwers2
Arno Brouwers2 Philippe Collin1,3
Philippe Collin1,3 Sylvia Klinkenberg1,4,5
Sylvia Klinkenberg1,4,5 Jos. G. M. Hendriksen1,5,6*
Jos. G. M. Hendriksen1,5,6*
This case report describes initiation of Nocturnal Non-Invasive Ventilation in home settings for two adolescents with Duchenne Muscular Dystrophy and different neuropsychiatric and neurocognitive comorbidities: one has Autism Spectrum Disorder, and the other has Attention Deficit Hyperactivity Disorder, obsessive thinking and anxiety. This report emphasizes the need for a multidisciplinary team approach, incorporating medical, psychological and psychopharmacological interventions for successful Non-Invasive Ventilation implementation. Challenges include recognition of neuropsychiatric and neurocognitive comorbidities often seen in Duchenne Muscular Dystrophy. Lessons learned from these cases underscore the importance of: coordinated multidisciplinary efforts, early advanced care planning, accurate psychoeducation, cautious psychopharmacological interventions, and parental and patient involvement. To our knowledge, this is the first case report describing implementing Nocturnal Non-Invasive Ventilation in home settings in adolescents with Duchenne Muscular Dystrophy and neuropsychiatric and neurocognitive comorbidities. In conclusion, implementation at home can be successful and become a realistic target for each individual with Duchenne Muscular dystrophy.
Duchenne Muscular Dystrophy (DMD) is a neuromuscular disorder characterized by the dysfunction of the dystrophin protein which results in a spectrum of severe clinical manifestations, including delayed motor milestones, the eventual loss of independent ambulation, and the development of life limiting cardiac and respiratory complications (1). In line with the standards of care (2), mechanical ventilatory support becomes an essential intervention during the second to third decade of the patient's life. Initially, this support is introduced to address sleep-related breathing disorders and hypoventilation and is thereby important for improvement of quality of life as e.g., fatigue may play a serious debilitating role in daily functioning. As the disease progresses Non-Invasive Ventilation (NIV) becomes necessary, as respiratory muscles further deteriorate. The progression of the disease eventually leads to a stage of full dependence on mechanical ventilation.
The profound impact of ventilatory support on DMD patients survival is noteworthy, extending life expectancy from 19 to 27 years (3). These results suggest that NIV contributes to improved survival in DMD, though outcomes may vary depending on disease progression, comorbidities, and adherence to ventilation therapy. Nonetheless, the results are promising. However, limited data exists regarding NIV adherence among (pediatric) patients with neuromuscular disorders. Only a few studies report on this (4–8). A recent study on NIV adherence in adolescents with DMD has indicated that internalizing problems (e.g., depression and anxiety) may cause challenges (5). Notably, the risk of neuropsychiatric comorbidities in DMD is higher than in the general population [see Pascual-Morena et al. (9) for a systematic review and meta-analysis]. The overall prevalence of Autism Spectrum Disorder (ASD), Attention Deficit Hyperactivity Disorder (ADHD), anxiety disorders and obsessive compulsive disorders are 7.0%, 18.0%, 24.0%, and 12% respectively, underscoring the significance of addressing these disorders in the context of NIV at home.
In this context, we describe two patients that shed light on the specific – nonphysical - psychological challenges faced by DMD adolescents when introducing home ventilation. Aim of this case report is to describe the interplay between behavioral factors and (nocturnal) NIV usage, and identify potential psychological and psychopharmacological strategies for successful NIV implementation at home. To our knowledge, this is the first case report of two adolescents with DMD with neuropsychiatric and neurocognitive comorbidities where NIV is initiated in the home situation.
A sixteen-year-old male adolescent diagnosed with DMD (deletion of exon 46–50 in the dystrophin gene) and comorbid ASD diagnosis [based on the Diagnostic and Statistical Manual of Mental Disorders fifth edition (10)]. His medical history indicates the administration of on intermittent prednisolone regimen, periodic use of melatonin ante noctem and in the past he (effectively) used Risperdal (0.5 mg) for a short period of time.
A structured neuropsychological assessment was conducted at the age of 13.5 showing a disharmonic profile with strong visual thinking (nonverbal concept formation) and weak verbal capacities (receptive and expressive). See Appendix 1 (Table 4) for an overview. Assessment of his respiratory function before the initiation of nocturnal home ventilation showed that the criteria for NIV implementation were met (see Table 1). According to the 2021 Dutch Guidelines on Chronic Ventilation (11), NIV is recommended for neuromuscular patients when pCO₂ or transcutaneous CO₂ exceeds 6.0 kPa, Forced Vital Capacity (FVC) falls below 50%, or hypoventilation-related symptoms are present. The NIV settings were titrated based on nocturnal transcutaneous CO2 measurements and data retrieved from the ventilator, with particular attention given to tidal volumes and respiratory frequency. These measurements were performed in a home setting.
In view of previous reported serious behavioral problems with novel situations (change of bedroom) in combination with the diagnosed ASD, it was decided that initiating NIV in a pediatric ICU environment was not realistic. In contrast to adult care (12, 13), initiating nocturnal ventilation at home has not yet been applied in children in the Netherlands. A 12-month timeframe was set. The main intervention strategies were, initially, putting a multidisciplinary team together including: his parents, a pediatric intensivist and specialized nurse (both from the department of home ventilation), a child clinical psychologist, child neurologist, child psychiatrist, and from school (special education) a nurse, speech therapist, and teacher (see Table 2 for further elaboration on the responsibilities per team role). Secondly, the best possible preparation for using and getting acquainted to the ventilator was communicated through visual support (pictograms). Furthermore, it was determined with his parents prior to his implementation when and what to share with the patient, managing the flow of information, timing, and extent of patient involvement. It was also considered important to create a detailed schedule which maintained the “normal” structure in the home environment according to the - Treatment and Education of Autistic and related Communication handicapped Children (TEACCH)-principle (14). Last of all, psychopharmacological treatment (Risperdal start 0.5 mg/day, max. 1.0 mg/day) was initiated weeks before start of home ventilation. With the expectation that it would be effective again, as it had been previously and its evidence in literature (15). Following this preparation he accepted the ventilation without any problems from the second night on. The psychopharmacological treatment was successfully tapered down after some weeks.
Within two months of starting NIV, the patient exhibited a noticeable improvement in sleep patterns, as reported by the parents. The adolescent woke up feeling more rested and happier compared to before the treatment. Furthermore, the parents also reported positive effects on the adolescent's overall development.
A seventeen-year-old male adolescent diagnosed with DMD (deletion of exon 49–50 in the dystrophin gene) and a comorbid diagnosis of ADHD (based on DSM-5 criteria).
At the age of thirteen, a structured neuropsychological assessment indicated average intelligence scores, with below-average performance in working memory and a low score in arithmetic (see Appendix 1 for an overview). At the age of 15 he experienced a disrupted sleep pattern and increasing fatigue. Based on the combination of clinical symptoms and tCO2 measurement (see Table 1 for the results of respiratory assessment) the criteria for NIV implementation were met. In accordance with the normal procedure this was attempted at the age of 15 on the pediatric ICU of our hospital. This first attempt was unsuccessful due to: (1) the inadequacy in empowering the patient to make well-informed decisions, (2) insufficient detailed information -concerning home ventilation in daily practice, (3) insufficiently detailed time plan regarding initiation of ventilation, and (4) too much perceived pressure from the team on the patient to make it successful in a clinical setting.
Considering his unsuccessful and traumatic hospital experiences, a decision was made to attempt initiating NIV at home at age 17. Collaborating with the adolescent, his parents, and the same teams from the department of home ventilation and Kempenhaeghe (see Table 2) a plan was developed. Stress reduction techniques using mindfulness and hypnotherapy, EMDR-like approaches, as well as cognitive behavior therapy interventions (helpful thinking) were implemented, acknowledging that breathing exercises during NIV might not be effective.
After nine months a new attempt was made to set up NIV at home. Additionally, treatment with Fluoxetine was initiated because of obsessive thoughts and worrying because of his earlier experiences with NIV. This led to diminishing of obsessive thoughts and significant improvement of his mood. He gradually adjusted to the face mask and could relax while using it, even managing short periods of sleep. However, a viral respiratory infection disrupted progress despite his determination. Initially, he decided in consultation with our team to make a new attempt a few months later. At that moment however he indicated that he understood what benefits the treatment could bring him but that stress related to the ventilation had the upper hand. He decided not to start the treatment again and choose quality of life instead of quantity of life.
In Table 3 we summarize our lessons learned from both cases and may offer a guideline for other clinicians.
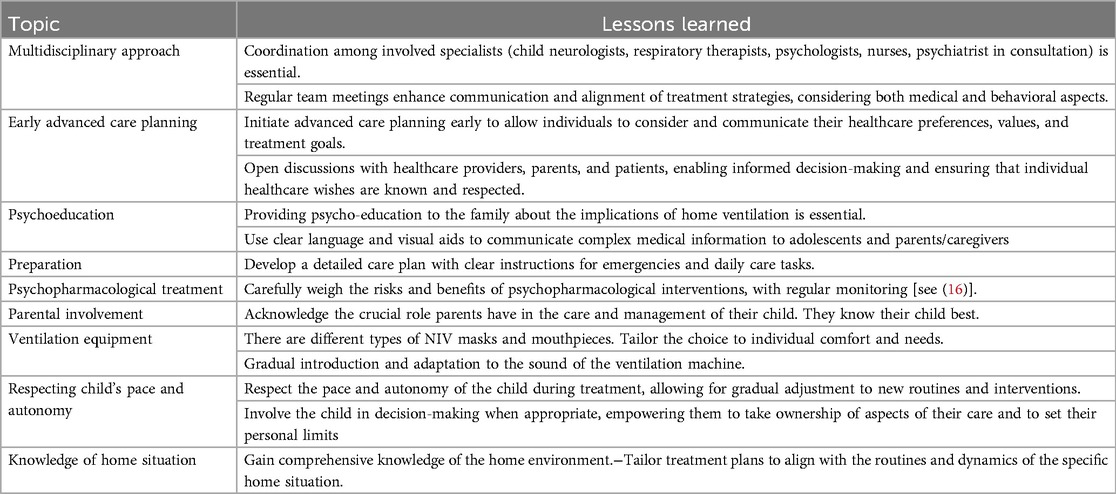
Table 3. Lessons learned from Two boys with duchenne muscular dystrophy and brain related comorbidities requiring home ventilation.
These cases show that home NIV coordinated by a multidisciplinary team may be a safe and important option to consider, especially when neuropsychiatric and neurocognitive comorbidities play a role in daily functioning. The combination of preparation, environmental structuring, psycho-education, and psychopharmacological treatment is essential. The big advantage of initiating this treatment at home is the embedding of the NIV in the daily structure and routine of the safe home environment including more autonomy for the patient. In the second case we were unable to initiate NIV at home during the first attempt due to acute medical circumstances. Furthermore, the distressing experiences of his attempt in the hospital setting and the interfering viral respiratory infection disrupted progress, which left him unable to start home NIV again for the moment. However, these experiences gave him an insight on the importance of quality of life and gaining more autonomy in decision making.
These results align with previous research, notably the study conducted by Pascoe et al. (5), highlighting the significance of a multidisciplinary approach in promoting NIV adherence in DMD and addressing the negative impact of internalized behavioral issues, such as anxiety and depression. A previous case study described a 20 year old male with DMD, who refused Positive Airway Pressure therapy due to claustrophobia and panic attacks in. This lead to admission to the emergency room with acute neurological symptoms. Also, this case emphasizes the importance offering essential psychological support to DMD patients (6) during life-changing events.
In light of the findings presented in these cases, it is concluded that a combination of careful preparation and psychological treatment holds promise in facilitating the implementation of home NIV in adolescents with DMD and comorbid neurodevelopmental or (internalized) behavioral symptoms. As such, it is strongly recommended to adopt a multidisciplinary timely approach when managing such cases, with particular attention to identifying and addressing potential psychological challenges, in order to optimize the support of the physical course of DMD. The possibility of nocturnal NIV should be discussed well in advance and a plan should be drawn up and discussed to provide adequate information to empower patients to make an informed decision together with their parents.
The datasets for this article are not publicly available due to concerns regarding participant/patient anonymity. Requests to access the datasets should be directed to the corresponding author.
The studies involving humans were approved by Lokale Medisch Ethische Commissie (LMEC). The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants' legal guardians/next of kin. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
PW: Conceptualization, Data curation, Investigation, Project administration, Visualization, Writing – original draft, Writing – review & editing. MV: Data curation, Writing – review & editing. MF: Data curation, Writing – review & editing. AB: Conceptualization, Data curation, Investigation, Methodology, Resources, Supervision, Writing – review & editing. PC: Conceptualization, Data curation, Investigation, Methodology, Resources, Writing – review & editing. SK: Conceptualization, Data curation, Funding acquisition, Investigation, Methodology, Resources, Supervision, Writing – review & editing. JH: Conceptualization, Data curation, Investigation, Methodology, Project administration, Resources, Supervision, Visualization, Writing – review & editing.
The author(s) declare financial support was received for the research and/or publication of this article. This work is generated within the European Reference Network for Neuromuscular Diseases. We gratefully acknowledge support to P.W. and J.H. from the European Union Horizon 2020 Framework Programme research and innovation programme “Brain Involvement iN Dystrophinopathies” (grant agreement, 847826). We also genuinely thank Duchenne Parent Project Netherlands for their financial support to J.H. during this research project.
This work is generated within the European Reference Network for Neuromuscular Diseases.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declare that no Generative AI was used in the creation of this manuscript.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Emery AE. The muscular dystrophies. Lancet. (2002) 359:687–95. doi: 10.1016/S0140-6736(02)07815-7
2. Birnkrant DJ, Bushby K, Bann CM, Alman BA, Apkon SD, Blackwell A, et al. Diagnosis and management of Duchenne muscular dystrophy, part 2: respiratory, cardiac, bone health, and orthopaedic management. Lancet Neurol. (2018) 17:347–61. doi: 10.1016/S1474-4422(18)30025-5
3. Landfeldt E, Thompson R, Sejersen T, McMillan HJ, Kirschner J, Lochmüller H. Life expectancy at birth in Duchenne muscular dystrophy: a systematic review and meta-analysis. Eur J Epidemiol. (2020) 35:643–53. doi: 10.1007/s10654-020-00613-8
4. Hurvitz MS, Bhattacharjee R, Lesser DJ, Skalsky AJ, Orr JE. Determinants of usage and nonadherence to noninvasive ventilation in children and adults with Duchenne muscular dystrophy. J Clin Sleep Med. (2021) 17:1973–80. doi: 10.5664/jcsm.9400
5. Pascoe JE, Sawnani H, Hater B, Sketch M, Modi AC. Understanding adherence to noninvasive ventilation in youth with Duchenne muscular dystrophy. Pediatr Pulmonol. (2019) 54:2035–43. doi: 10.1002/ppul.24484
6. Annunziata A, Coppola A, Marotta A, Fiorentino G. MPV Promote adherence to nocturnal NIV in a Duchenne patient. Acta Myol. (2020) 39:101. doi: 10.36185/2532-1900-014
7. Rautemaa V, Roberts ME, Bentley A, Felton TW. The role of noninvasive ventilation in the management of type II respiratory failure in patients with myotonic dystrophy. ERJ Open Res. (2021) 7:00192-2020. doi: 10.1183/23120541.00192-2020
8. Amaddeo A, Frapin A, Touil S, Khirani S, Griffon L, Fauroux B. Outpatient initiation of long-term continuous positive airway pressure in children. Pediatr Pulmonol. (2018) 53:1422–8. doi: 10.1002/ppul.24138
9. Pascual-Morena C, Cavero-Redondo I, Reina-Gutiérrez S, Saz-Lara A, López-Gil JF, Martínez-Vizcaíno V. Prevalence of neuropsychiatric disorders in Duchenne and Becker muscular dystrophies: a systematic review and meta-analysis. Arch Phys Med Rehabil. (2022) 103:2444–53. doi: 10.1016/j.apmr.2022.05.015
10. American Psychiatric Association D, American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM-5. Washington, DC: American Psychiatric Association (2013).
11. Dutch Guidelines Chronic Ventilation 2021—Vereniging Samenwerkingsverband Chronische Ademhalingsondersteuning.pdf.
13. Hazenberg A, Kerstjens HA, Prins SC, Vermeulen KM, Wijkstra PJ. Initiation of home mechanical ventilation at home: a randomised controlled trial of efficacy, feasibility and costs. Respir Med. (2014) 108:1387–95. doi: 10.1016/j.rmed.2014.07.008
14. Mesibov GB, Shea V, Schopler E. The TEACCH Approach to Autism spectrum Disorders. New York: Springer Science & Business Media (2005).
15. Maneeton N, Maneeton B, Putthisri S, Woottiluk P, Narkpongphun A, Srisurapanont M. Risperidone for children and adolescents with autism spectrum disorder: a systematic review. Neuropsychiatr Dis Treat. (2018) 14:1811. doi: 10.2147/NDT.S151802
16. Weerkamp PM, Geuens S, Collin P, Goemans N, Vermeulen RJ, De Waele L, et al. Psychopharmaceutical treatment for neurobehavioral problems in Duchenne muscular dystrophy: a descriptive study using real-world data. Neuromuscul Disord. (2023) 33(7):2444–53. doi: 10.1016/j.apmr.2022.05.015
Keywords: Duchenne muscular dystrophy, nocturnal non-Invasive ventilation, neuropsychiatric and neurocognitive comorbidities, psychological intervention, psychopharmacological intervention, case report
Citation: Weerkamp PMM, Voermans M, Finders M, Brouwers A, Collin P, Klinkenberg S and Hendriksen JGM (2025) Case Report: Home initiation of nocturnal non-invasive ventilation in two adolescents with Duchenne muscular dystrophy and comorbid autism spectrum disorder and ADHD. Front. Pediatr. 13:1525365. doi: 10.3389/fped.2025.1525365
Received: 15 November 2024; Accepted: 20 February 2025;
Published: 14 March 2025.
Edited by:
Martin Groß, MEDIAN Clinic Bad Tennstedt, GermanyReviewed by:
Elizabeth Super, Oregon Health and Science University, United StatesCopyright: © 2025 Weerkamp, Voermans, Finders, Brouwers, Collin, Klinkenberg and Hendriksen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jos. G. M. Hendriksen, aGVuZHJpa3NlbmpAa2VtcGVuaGFlZ2hlLm5s
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.