- 1Gillberg Neuropsychiatry Center, Sahlgrenska Academy, University of Gothenburg, Gothenburg, Sweden
- 2Child and Adolescent Specialist Centre, Angered Hospital, SV Hospital Group, Gothenburg, Sweden
- 3Institute of Neuroscience and Physiology, Sahlgrenska Academy, University of Gothenburg, Gothenburg, Sweden
Aim: This study aimed to evaluate a clinical project aiming to address gaps in healthcare for young children in an immigrant, low-resource district from early identification of regulatory problems, autism, and other neurodevelopmental symptoms by child health services to assessment and interventions in specialist care.
Methods: A mixed-model design was employed, consisting of a description of the clinical project and data from healthcare statistics to evaluating the care chain. Qualitative in-depth interviews were conducted to capture the perspectives of participating child health nurses. Data were analyzed using content analysis.
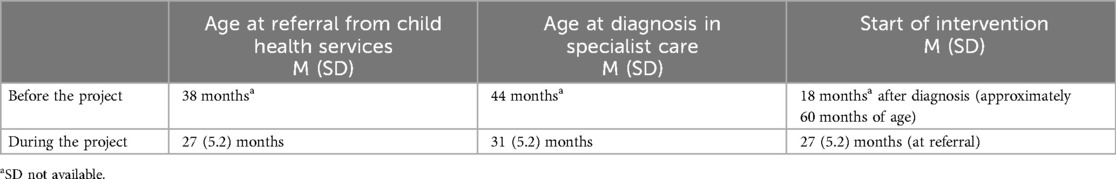
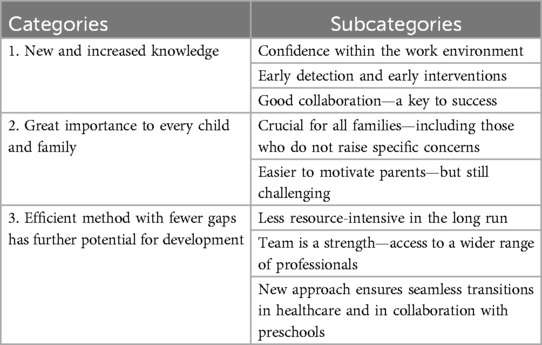
Results: The mean age for referral from primary to specialist care for suspected autism decreased from 38 to 27 months at (n = 59). A total of 55 children were diagnosed with autism. The mean age at autism diagnosis decreased from 44 to 31 months. Waiting times from referral to intervention were shortened. Interventions were already initiated in primary care at the time of referral. Qualitative analyses of nurse experiences revealed three main categories: (1) new and increased knowledge, (2) great importance for every child and family, and (3) an efficient method with fewer gaps, which holds further potential for development.
Conclusion: Professionals’ increased knowledge of early symptoms in children, combined with novel healthcare methods for close collaboration, made it possible to bridge the gaps and provide young children and their families with early assessments and essential early interventions. The study results point to opportunities for integrated healthcare and collaboration with families and preschools.
1 Introduction
Healthcare faces significant challenges in meeting the diverse needs of young children and their families. In Sweden, 95%–99% (1) of children are regularly followed up through Child Health Services (CHS), which monitors the health and development milestones of children. However, there still remain delays in identifying early signs of autism and other neurodevelopmental disorders (NDDs). When autism and/or other NDDs are suspected, a referral is usually sent from primary care for further investigation at specialist units. A major general problem in many parts of our country and globally is long waiting times for evaluations, which can delay essential interventions for several years (2, 3). A recent study examining care pathways for children and adolescents with autism across three European countries reported significant shortcomings in healthcare, including long delays from initial concerns to screening and confirmed diagnosis, long waiting times for interventions, and no access to interventions (4). In addition to gaps in the care chain, there is often a lack of coordination with other parts of care regarding coexisting conditions, e.g., feeding difficulties and medical conditions, in young children with autism.
Early difficulties in crying, sleeping, and feeding, often referred to as regulatory problems (RPs), are common concerns in child health, affecting approximately 20% of infants (5).While these issues are only temporary for most children (5, 6), some children experience persistent RPs, which can cause great concern for the family and lead to frequent healthcare interactions. Several studies have drawn attention to persisting RPs beyond 3–4 months (7, 8) and the increased risk for continued developmental difficulties during childhood. These issues commonly occur in combination, e.g., sleeping and feeding problems. A Danish population study found persistent combined RPs in 8.6% of the children aged 8–11 months (7). A study from our group (8) found RPs in 50% of children with autism and, specifically, persisting RPs regarding feeding and eating in children who were later diagnosed with autism and continued eating difficulties. Given the increased risk for developmental problems, there is a need for early interventions and comprehensive follow-up for children with persisting RPs. A recent review by Asmussen et al. (9) pointed out the need for more research on the longitudinal relationship between combined RPs and mental health problems in children and the importance of investigating preventive interventions targeting persisting RPs.
Research emphasizes the importance of early identification of autism and early interventions (10). The core symptoms of autism, such as deficits in social communication and repetitive behaviours, can be observed as early as the first year of life, with most children displaying these symptoms between 12 and 24 months (11). Other early symptoms include sensory and motor deviations and regulatory problems (11, 12). Increased knowledge among professionals and screening programs in many countries have led to progress in the early identification of autism (10, 13, 14). Autism can be reliably diagnosed as early as 18 months of age (14, 15), and several studies have reported early parental concern around 18 months in children who are later diagnosed with autism (16, 17). However, there is often a delay of several years in diagnosis, and the median age of autism diagnosis is reported to be over the age of 4 years (2, 18).
The first years of life are considered a critical period, offering the best opportunities for interventions by significant neural plasticity (19). For children under 3 years of age, there is growing evidence for interventions covered under the umbrella term Naturalistic Developmental Behavioural Interventions (NDBI) (20, 21). These interventions integrate behavioural and developmental strategies within the child's naturalistic environment during daily activities. The most studied NDBIs is the Early Start Denver Model (ESDM) developed for children aged 12–48 months (22, 23, 24, 25). The ESDM is a comprehensive intervention focusing on the child's social-emotional, cognitive, and language development and broadly covering the different developmental areas. The individual child's motivation and interest are essential, and the learning context for the individualized interventions is embedded in child's daily activities in which adults create opportunities for learning and interaction through play activities and daily routines. Parental engagement is emphasized, and parents are trained to implement ESDM into their daily interactions with their children (26, 27).
Approximately 1% of children are diagnosed with autism around the world, but prevalence estimates vary significantly within and across sociodemographic groups (28). Autism is highly correlated to other NDDs, e.g., attention disorders, language disorders, motor disabilities, and intellectual disabilities (29, 30). To capture the different early manifestations of NDDs, affecting motor, social, and communication development, feeding, sleeping, and behavioural regulation, Gillberg coined the term ESSENCE (Early Symptomatic Syndromes Eliciting Neurodevelopmental Clinical Examinations). The ESSENCE concept underscores the need to follow-up and assess broadly when early concerning symptoms or disorders are identified. In the last few decades, more attention has also been paid to coexisting medical conditions in autism, which may influence the child's behaviour and need targeted treatments (14, 31, 32).
The biological basis of autism is heterogeneous and complex (33). Twin and family studies have demonstrated that genetic factors play a major role (34, 35). Various environmental factors, including pre- and perinatal factors and epigenetic mechanisms, have been proposed to interact and contribute to the manifestation of atypical neurodevelopmental patterns in autism (36, 37). However, the role of environmental factors is still not fully understood. In the last decade, several studies have indicated an association between maternal migration and the risk of autism (38, 39). In a previous study by our group, we reported a high prevalence of autism, 3.7%, among preschool children in an immigrant population (40). The high prevalence and the many needs of children and families in immigrant populations served as the basis for this study.
Barriers in healthcare service systems, including long waiting lists and separate disconnected units, pose significant challenges for young children and their families, hindering their access to timely assessments and early essential interventions (3, 4, 41). The situation is even more difficult for immigrant families in low-resource settings (28, 42). These healthcare barriers served as the catalyst for the clinical project examined in this study.
The aim of the study was to evaluate the novel methods within the clinical project to address gaps in healthcare. An additional aim was to explore the experiences of new methods and structures in CHS from the perspectives of child health nurses.
2 Methods
The study follows a mixed-model design, consisting of data from medical statistic charts and qualitative interviews to capture the perspectives of the included nurses.
2.1 Study context and participants
2.1.2 Clinical project
The study is based on a clinical project aimed at developing effective integrated healthcare for children under 3 years old with RPs, autism, and other coexisting NDDs and medical conditions. The clinical project was conducted (from 2021 to 2023) within a low-resource area, where an extremely large proportion (approximately 80%) of families have an immigrant background. The clinical project was founded by the Västra Götaland region. The target group consisted of approximately 1,600 children, ranging from birth to 3 years old, who were followed up within the child health services. Three child health units were a part of the clinical project, with a total of 12 child health nurses. General practitioners were responsible for medical assessment within the regular health program, and psychologists could be consulted. Primary care staff from child health services, specialist healthcare providers, and habilitation professionals were included in the collaborative project. In addition, the preschool administration, represented by special educators in the district, was also included.
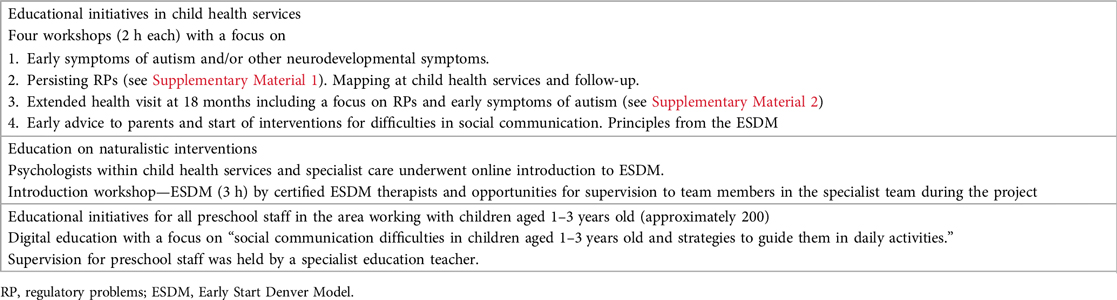
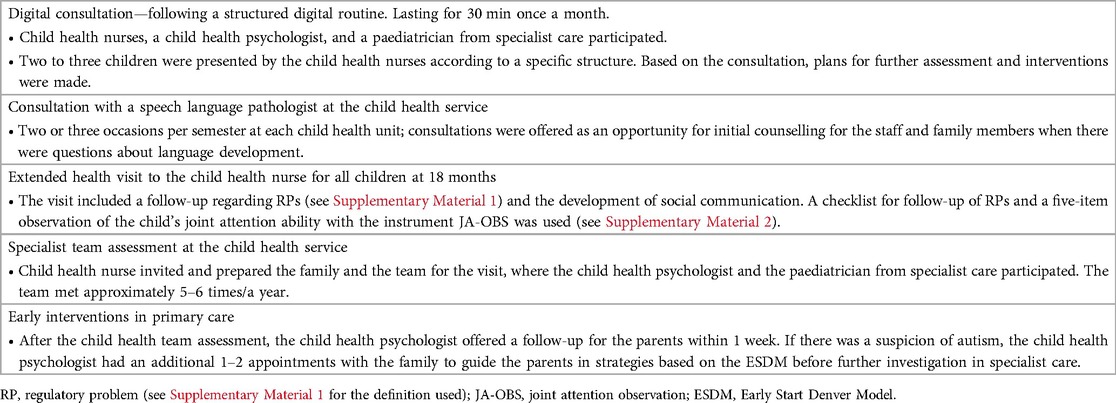
The clinical project included educational efforts to increase professionals’ knowledge about early neurodevelopmental symptoms, persisting RPs, symptom mapping, assessments and interventions (see Table 1), and new methods for collaboration to ensure coherent care (see Table 2).
At monthly digital consultations for each child health unit (30 min), joint assessment and planning were possible for children with concerns (see Table 2). Novel methods that supported the joint work included templates for mapping RP symptoms and a template for an extended 18-month health visit to the child health nurse (Table 2; Supplementary Material 2). There were also opportunities, every second month, for assessments by a specialist child health team (consisting of the responsible child health nurse, a child health psychologist, and a paediatrician from specialist care). The initial interventions started via child health services, where the child health psychologist offered a follow-up for the family within 1 week, offering more information and support based on the individual needs of each child and family. In cases of suspected autism, an additional one to two appointments were offered to guide parents in strategies based on the ESDM before further investigation in specialist healthcare.
The multiprofessional evaluation was based on the referral from child health services, including medical records from the neonatal period. In the first meeting, a survey of the family's social situation, current needs, and the child's preschool situation was conducted. The evaluation included (i) an observation of the child during play activities and a parental interview during a team visit with the paediatrician and psychologist, (ii) a physical developmental examination of the child, followed by complementary medical investigations based on the paediatrician's assessment, (iii) psychological assessments using standardized diagnostic instruments, and (iv) information from preschool, obtained from the special education teacher, along with an observation of the child in the preschool.
The goal was to assess the child within 4–6 weeks, summarize the investigation and diagnostic assessment results with the parents, and create an intervention plan with them. The same team was responsible for treatment efforts and follow-up during the 1-year period within the local team. For children with autism, the interventions were based on the ESDM (22). The parents were coached in strategies for their child twice a month. Meetings with the preschool were held to share information and involve the preschool staff as much as possible in the goals. According to the child’s individual needs and coexisting conditions, other treatments and interventions were provided.
2.2 Data collection
Data, including waiting times for children referred from primary care for evaluations due to a suspicion of a neurodevelopmental disorder and the age at diagnosis, were collected retrospectively and prospectively from medical statistics in healthcare.
2.3 Participants’ qualitative part
Eight child health nurses out of 12 possible nurses working at the included CHS were recruited for the interviews. The inclusion criterion was that the nurse needed to have been part of the clinical project. In total, six interviews were conducted; two of these interviews included a pair of two nurses each.
2.4 Data collection qualitative part
The interviews were conducted by author EC, who was not a part of the specialist team. The interviews were semi-structured, audio-recorded, and subsequently transcribed verbatim (43). The interviews were conducted using a question guide developed by two of the authors (EC and GN). The questions were informed by prior clinical experiences and previous research. The guide included questions such as: “What does the care process look like for these children and their parents?, How do you perceive your opportunities to support the parents?”. The first interview served as a pilot to evaluate the questions and refine them if necessary. However, no changes were made.
2.5 Qualitative data analysis interviews with nurses
The author EC transcribed all interviews and then read the transcriptions multiple times to gain an overview before analyzing and interpreting the data using content analysis as described by Graneheim and Lundman (44). The structured analysis involved sorting the material into meaning units. After identifying all meaning units, the author labelled each unit with a code. The analysis involved ongoing discussions among the authors to ensure methodological rigour and the trustworthiness of the results. The authors reflected on and discussed similarities and differences among codes, which led to the development of categories and subcategories. They continually reviewed and refined interpretations of these categories (45).
2.6 Ethics
This study was approved by the Swedish Ethical Review Authority (Dnr 2022-02070-01). All participating nurses received oral and written information and provided written informed consent. To ensure anonymity, names were removed.
3 Results
The results are divided into two parts: the quantitative findings, which include data from medical statistical charts, and the qualitative findings, derived from interviews with healthcare nurses.
3.1 Healthcare statistics
Table 3 shows the time from detection of neurodevelopmental symptoms to diagnosis and the start of interventions, before and after the project started. Fifty-nine children (28% girls) were referred to the multiprofessional team with suspected autism and/or other neurodevelopmental disorders. Among them, 55 were diagnosed with autism and other coexisting conditions, while the other four were diagnosed with “non-autism” neurodevelopmental disorders. The average age at diagnosis was 27 months.
When persistent RPs were identified, mapping and assessments were conducted at the child health service by the nurse and the child health specialist team. Most families were offered support and follow-up within the child health services, while some were referred to the child health specialist team. A total of 13 children with RPs were referred to the specialist team for medical assessment and interventions towards more severe RPs, in most cases feeding/eating problems. The average age at referral or at the time of assessment in specialist care was 15 months.
3.2 Qualitative results
Findings from the qualitative data conducted through interviews showed three categories: (1) new and increased knowledge, (2) great importance for every child and family, and (3) efficient method with fewer gaps, which has further potential for development, with eight subcategories presented in Table 4.
3.3 New and increased knowledge
The category “new and increased knowledge” captured the nurses’ experiences of gaining new knowledge through the project. This encompassed both the development and implementation of new methods and structures, as well as the educational part of the project, which included workshops and discussions.
3.3.1 Confidence within the work environment
The nurses indicated that through collaboration and participation in the project, they felt an increased sense of confidence in their professional roles. The collaboration between primary care and specialist care made the child health nurses feel supported and enhanced their knowledge and confidence. Continuous consultation and team collaboration were critical improvements, allowing the included staff to use a “common” language.
“It makes it easier for me if I involve the parents, I also think it’s a kind of security for me.”
3.3.2 Early detection and early interventions
The nurses shared their experiences of detecting difficulties earlier, allowing them to support and reach out to families sooner. They expressed having more effective tools for discussing their observations with parents. The increased knowledge about early signs of developmental difficulties in children made the nurses more confident about discussing their worries with parents and more likely to see early signs of developmental difficulties.
“That one can find them [early signs of developmental difficulties] … and talk about it in a better way with the parents.”
3.3.3 Good collaboration—a key to success
All included healthcare and preschool staff work towards the same goal. Nurses expressed that the new routines and close contact with the team and project leader were crucial to increasing collaboration and minimizing gaps. Through collaborative work and educational sessions, the nurses increased their knowledge and confidence.
“That everyone participates with great interest and commitment … that it is a task that one finds exciting and motivating”.
3.4 Great importance to every child and family
The category “great importance to every child and family” consisted of two subcategories focusing on children and families. According to the nurses, these subcategories demonstrated that the new way of working was beneficial for all families, including those whose children were of concern and those whole children who developed as expected.
3.4.1 Crucial for all families—including those who do not raise specific concerns
The increased knowledge gained through the project provided the nurses with “tools” in their “toolbox” for assessing children who raised concerns; these tools proved to be useful in their general work as well. The “new” structure and methods were helpful for all children, not just those of concern. Asking parents more about RPs proved beneficial for several families. Although the nurses mentioned that they had previously inquired about RPs, they now had a more structured approach to addressing these issues. In addition, they had resources to support families by offering digital consultations and/or referrals to specialist CHS.
“ I also think that with the knowledge that has increased within oneself, it also helps other families where there is no concern.”
3.4.2 Easier to motivate parents—but still challenging
The new tools, shorter waiting times, routines for specialist assessments in close connection with nurse visits, and the possibility to offer psychological support for parents facilitated motivational work with parents. It helped them motivate parents to accept further referrals. However, they described that it could still be challenging to help parents understand the importance of sending a referral. There were different opinions regarding early detection between nurses; some thought it affected parents’ motivation, since some parents did not worry since there were several years until their 2-year-old started school.
“Those who have been uncertain and had to wait a bit and receive support in between, well … many say yes afterwards.”
3.5 Efficient method with fewer gaps has further potential for development
The category “efficient method with fewer gaps” highlights the potential for further development; it focused on how the new methods worked, the benefits of teamwork, how the new structures improved healthcare transitions, and making collaboration with preschools easier and more effective.
3.5.1 Less resource-intensive in the long run
The improved healthcare chain with reduced waiting times and fewer gaps was more resource-effective due to the nurses’ experiences. Significant time and resource savings were achieved by preventing families from waiting and ensuring they received support and/or interventions as soon as concern about their child's development was identified. The nurses described that they had got more “tools” and knowledge of how to support families. “In that case, it would have required even more resources later on, so I think it's a resource-saving measure overall.”
3.5.2 Team is a strength—access to a wider range of professionals
Having access to a team, i.e., the possibility to consult a doctor or psychologist, was beneficial and valuable for daily work, not least when being new at work. The nurses said that the fact that they worked together with other professions made them gain new knowledge and develop their professional skills.
“I feel like I have very good support from them. Especially if you haven’t been working for very long.”
3.5.3 A new approach ensures easy and smooth transitions in healthcare and in collaboration with preschools
The new structure and collaboration within the project made transitions smoother between healthcare levels and facilitated the nurses’ work. One key point highlighted by the nurses was that knowing parents could access support without long waiting times made it easier for them to discuss their concerns with the parents. It was also beneficial when collaborating with preschools and preschool staff.
4 Discussion
The aim of the study was to evaluate novel methods within a clinical collaborative project to address gaps in healthcare for young children with autism and other NDDs. An additional aim was to explore the experiences of new methods and structures in CHS from the perspectives of child health nurses.
The results showed that the mean age for identifying autism signs and referring children from CHS to specialist care decreased by 11 months, from 38 to 27 months. The shortened wait time for specialist care evaluations resulted in a mean age of autism diagnosis of 31 months, compared to 44 months previously. Interventions were started already at the point of autism suspicion in primary care (27 months). The results showed a significant improvement regarding age for autism diagnosis and opportunities for interventions compared to the local average (60 months) for interventions. The results for age at diagnosis are also well below what globally is reported (18). The mean age for diagnosis is also significantly lower than global average (18). Several studies have highlighted the increased prevalence of autism in children from immigrant populations (38, 39, 40) and have also noted the risk of delayed diagnosis and lack of services for these children (46). As the current study was conducted in an immigrant population in a low-resource city district, the results that show access to healthcare with reduced waiting times are promising findings.
Research emphasizes the importance of early identification of autism, persistent RPs, and other early NDDs. Coexisting neurodevelopmental conditions are more the rule than the exception (30) and must be broadly assessed for targeted interventions. Specialization in care and organizational shortcomings, including long waiting lists, can, when symptoms have been identified, become an obstacle for assessments and targeted interventions for different simultaneous neurodevelopmental and medical conditions (29, 31). It may take several years after symptoms have been identified before targeted interventions can begin, which can entail significant consequences for the individual child and family. Novel methods, such as mapping templates for RPs and a new extended form for an 18-month developmental check-up, including the observation of joint attention ability, the joint attention observation (JA-OBS) (13), provided support in early identification of autism signs and/or other neurodevelopmental symptoms; these tools also facilitated collaboration with, and referrals to, specialist care. When persistent RPs were identified within CHS, most families were offered early interventions and follow-up within CHS, and some children were referred to specialist care for further medical assessments and treatment. The reason for referral to specialist care was, in most cases, feeding/eating problems, with the average mean age for referral being 15 months. The nurses reported the increased knowledge and structural approach to addressing early symptoms, including RPs, opportunities for team collaboration, and consultations with specialist care, as critical improvements.
The qualitative results showed three main categories. The first, new and increased knowledge, included descriptions from the nurses that knowledge of and the ability to identify early neurodevelopmental symptoms and medical conditions form the basis for timely assessments and interventions. The nurses described that the increased knowledge gained through initial educational investment and an ongoing opportunity for learning through new ways of collaborating with healthcare specialists played a decisive role. increased knowledge and “common language” were the basis for more effective cooperation in care to identify difficulties in children's development, engage in conversations with parents, and offer investigations and interventions. When collaborating with preschools and preschool staff, it was also beneficial to gain a “common” language.
The second main category, great importance to every child and family, addresses issues of and includes descriptions from the nurses that the new methods and structures were beneficial for children suspected of having NDDs, but they highlight its value for all children and families that took part in CHS. The first meetings within child health services could create conditions for building trust and forming an alliance with parents (47), which was very important when the child was referred for further investigation and interventions in specialist care. Earlier studies have highlighted the importance of assessing the individual needs of the child and family in a holistic way (30, 48, 49). The nurses described that the family and child's situation in preschools must be considered. In all interventions for the child, the alliance with the parents is crucial (47, 49).
The third main category, Efficient method—fewer gaps—further potential for development, the new structure and collaboration within the project made transitions smoother between different healthcare levels and facilitated the nurses’ work. One key point highlighted by the nurses was that knowing parents could access support, without long waiting times, made it easier for them to discuss their concerns with the parents. This finding is important for future guidance on improving and developing healthcare pathways for children and their families, which is in line with earlier-presented suggestions by Mendez et al. (4).
4.1 Strengths and limitations
To strengthen the trustworthiness, an interview guide was employed to ensure that the questions were aligned with the study's aim, strengthening dependability. Confirmability was ensured by using quotes from the interviews to illustrate subcategories, and reflexivity was maintained throughout continuous discussions among the authors during analysis (50).
This study did not include the parents’ experiences, nor did it explore the children's developmental trajectories or their future access to interventions. For replication and extension beyond the current population, a larger study would be necessary to learn more about its possibility for generalizations in other settings.
4.2 Future research
In a future study, the prevalence of RPs, their course, and any underlying and coexisting conditions will be examined. Moreover, while health-economic benefits were not within the scope of this study, they represent an important and interesting avenue for further exploration. The clinical experiences within specialist care suggested that most families were well prepared when they came with their children for the investigations. Many parents expressed that they had already received much help from the child health team and learned strategies to help their child. This would be interesting for a future study.
4.3 Conclusion
Professionals’ increased knowledge of early symptoms and neurodevelopmental concerns in preschool children, coupled with well-structured healthcare that foster close collaboration, made it possible to bridge the gaps and provide young children and their families with early assessments and essential interventions. The results of our study point towards better opportunities for integrated healthcare and collaboration with families and preschools.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors without undue reservation.
Ethics statement
The studies involving humans were approved by the Swedish Ethical Review Authority (Dnr 2022-02070-01). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
GN: Conceptualization, Formal Analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Validation, Visualization, Writing – original draft, Writing – review & editing. CG: Conceptualization, Supervision, Writing – original draft, Writing – review & editing. EC: Conceptualization, Formal Analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Validation, Visualization, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. The study was supported by grants from the Research department at Angereds Hospital SV Hospital Group, Gothenburg, Sweden, and FOU VGR Regionala FoU-medel, Västra Götalandsregionen.
Acknowledgments
The authors thank all colleagues involved in the clinical project for their collaboration.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fped.2025.1501650/full#supplementary-material
References
1. Wettergren B, Blennow M, Hjern A, Söder O, Ludvigsson JF. Child health systems in Sweden. J Pediatr. (2016) 177:187–202. doi: 10.1016/j.jpeds.2016.04.055
2. Baio J, Wiggins L, Christensen DL, Maenner MJ, Daniels J, Warren Z, et al. Prevalence of autism spectrum disorder among children aged 8 years—autism and developmental disabilities monitoring network, 11 sites, United States, 2014. MMWR Surveill Summ. (2018) 67(6):1–23. doi: 10.15585/mmwr.ss6706a1
3. Lappé M, Lau L, Dudovitz RN, Nelson BB, Karp EA, Kuo AA. The diagnostic odyssey of autism spectrum disorder. Pediatrics. (2018) 141(Suppl 4):S272–9. doi: 10.1542/peds.2016-4300C
4. Mendez MA, Oakley B, Canitano R, San José-Cáceres A, Tinelli M, Knapp M, et al. Autism care pathway in Europe. Eur Psychiatry. (2023) 66(1):e81. doi: 10.1192/j.eurpsy.2023.2435
5. Hemmi MH, Wolke D, Schneider S. Associations between problems with crying, sleeping and/or feeding in infancy and long-term behavioural outcomes in childhood: a meta-analysis. Arch Dis Child. (2011) 96(7):622–9. doi: 10.1136/adc.2010.191312
6. Cook F, et al. Infant regulation and child mental health concerns: a longitudinal study. Pediatrics. (2019) 143(3):e20180575. doi: 10.1542/peds.2018-0977
7. Olsen AL, et al. Problems of feeding, sleeping and excessive crying in infancy: a general population study. Arch Dis Child. (2019) 104(11):1034–41. doi: 10.1136/archdischild-2019-316851
8. Nygren G, Linnsand P, Hermansson J, Dinkler L, Johansson M, Gillberg C. Feeding problems including avoidant restrictive food intake disorder in young children with autism spectrum disorder in a multiethnic population. Front Pediatr. (2021) 9:780680. doi: 10.3389/fped.2021.780680
9. Asmussen J, Davidsen KA, Olsen AL, Skovgaard AM, Bilenberg N. The longitudinal association of combined regulatory problems in infancy and mental health outcome in early childhood: a systematic review. Eur Child Adolesc Psychiatry. (2024) 33(11):3679–92. doi: 10.1007/s00787-023-02262-0
10. Zwaigenbaum L, et al. Early intervention for children with autism spectrum disorder under 3 years of age: recommendations for practice and research. Pediatrics. (2015) 136(Suppl 1):60–81. doi: 10.1542/peds.2014-3667
11. Ozonoff S, Iosif AM, Baguio F, Cook IC, Hill MM, Hutman T, et al. A prospective study of the emergence of early behavioral signs of autism. J Am Acad Child Adolesc Psychiatry. (2010) 49(3):256–66. doi: 10.1016/j.jaac.2009.11.009
12. Dahlgren SO, Gillberg C. Symptoms in the first two years of life. A preliminary population study of infantile autism. Eur Arch Psychiatry Neurol Sci. (1989) 238(3):169–74. doi: 10.1007/BF00451006
13. Nygren G, Sandberg E, Gillstedt F, Ekeroth G, Arvidsson T, Gillberg C. A new screening programme for autism in a general population of Swedish toddlers. Res Dev Disabil. (2012) 33(4):1200–10. doi: 10.1016/j.ridd.2012.02.018
14. Hyman SL, Levy SE, Myers SM, Kuo DZ, Apkon CS, Davidson LF, et al. Identification, evaluation, and management of children with autism spectrum disorder. Pediatrics. (2020) 145(1):e20193447. doi: 10.1542/peds.2019-3447
15. Ozonoff S, Young GS, Landa RJ, Brian J, Bryson S, Charman T, et al. Diagnostic stability in young children at risk for autism spectrum disorder: a baby siblings research consortium study. J Child Psychol Psychiatry. (2015) 56(9):988–98. doi: 10.1111/jcpp.12421
16. Howlin P, Moore A. Diagnosis in autism: a survey of over 1200 patients in the UK. Autism. (1997) 1(2):135–62. doi: 10.1177/1362361397012003
17. De Giacomo A, Fombonne E. Parental recognition of developmental abnormalities in autism. Eur Child Adolesc Psychiatry. (1998) 7(3):131–6. doi: 10.1007/s007870050058
18. Christensen DL, Maenner MJ, Bilder D, Constantino JN, Daniels J, Durkin MS, et al. Prevalence and characteristics of autism spectrum disorder among children aged 4 years—early autism and developmental disabilities monitoring network, seven sites, United States, 2010, 2012, and 2014. MMWR Surveill Summ. (2019) 68(2):1–19. doi: 10.15585/mmwr.ss6802a1
19. Ismail FY, Fatemi SA, Johnston MV. Cerebral plasticity: windows of opportunity in the developing brain. Eur J Paediatr Neurol. (2017) 21(1):23–48. doi: 10.1016/j.ejpn.2016.07.007
20. Schreibman L, Dawson G, Stahmer AC, Landa R, Rogers SJ, McGee GG, et al. Naturalistic developmental behavioral interventions: empirically validated treatments for autism spectrum disorder. J Autism Dev Disord. (2015) 45:2411–28. doi: 10.1007/s10803-015-2407-8
21. Sandbank M, Bottema-Beutel K, LaPoint SC, Feldman JI, Barrett DJ, Caldwell N, et al. Autism intervention meta-analysis of early childhood studies (project AIM): updated systematic review and secondary analysis. BMJ. (2023) 383:e076733. doi: 10.1136/bmj-2023-076733
22. Rogers SJ, Dawson G. Early Start Denver Model for Young Children with Autism: Promoting Language, Learning, and Engagement. New York, NY: Guilford Press (2010).
23. Wang Z, Loh SC, Tian J, Chen QJ. A meta-analysis of the effect of the early start Denver model in children with autism spectrum disorder. Int J Dev Disabil. (2022) 68(5):587–97. doi: 10.1080/20473869.2020.1870419
24. Fuller EA, Oliver K, Vejnoska SF, Rogers SJ. The effects of the early start Denver model for children with autism spectrum disorder: a meta-analysis. Brain Sci. (2020) 10(6):175. doi: 10.3390/brainsci10060368
25. Linnsand P, Nygren G, Hermansson J, Gillberg C, Carlsson E. Intervention in autism based on early start Denver model in a multiethnic immigrant setting—experiences of preschool staff involved in its implementation. Front Child Adolesc Psychiatry. (2024) 3:1341729. doi: 10.3389/frcha.2024.1341729
26. Carlsson E, Nygren G, Gillberg C, Linnsand P. “The package has been opened”: parents’ perspective and social validity of an early start Denver model intervention for young children with autism. Front Child Adolesc Psychiatry. (2024) 3:1509828. doi: 10.3389/frcha.2024.1509828
27. Rogers SJ, Vismara LA, Dawson G. Coaching Parents of Young Children with Autism: Promoting Connection, Communication, and Learning. New York, NY: Guilford Publications (2021).
28. Zeidan J, Fombonne E, Scorah J, Ibrahim A, Durkin MS, Saxena S, et al. Global prevalence of autism: a systematic review update. Autism Res. (2022) 15(5):778–90. doi: 10.1002/aur.2696
29. Gillberg C. The ESSENCE in child psychiatry: early symptomatic syndromes eliciting neurodevelopmental clinical examinations. Res Dev Disabil. (2010) 31(6):1543–51. doi: 10.1016/j.ridd.2010.06.002
30. Fernell E, Gillberg C. Autism under the umbrella of ESSENCE. Front Psychiatry. (2023) 14:1002228. doi: 10.3389/fpsyt.2023.1002228
31. Soke GN, Maenner MJ, Christensen D, Kurzius-Spencer M, Schieve LA. Prevalence of co-occurring medical and behavioral conditions/symptoms among 4- and 8-year-old children with autism spectrum disorder in selected areas of the United States in 2010. J Autism Dev Disord. (2018) 48(8):2663–76. doi: 10.1007/s10803-018-3521-1
32. Restrepo B, Angkustsiri K, Taylor SL, Rogers SJ, Cabral J, Heath B, et al. Developmental–behavioral profiles in children with autism spectrum disorder and co-occurring gastrointestinal symptoms. Autism Res. (2020) 13(10):1778–89. doi: 10.1002/aur.2354
34. Lai MC, Lombardo MV, Baron-Cohen S. Autism. Lancet. (2014) 383(9920):896–910. doi: 10.1016/S0140-6736(13)61539-1
35. Taylor MJ, Rosenqvist MA, Larsson H, Gillberg C, D’Onofrio BM, Lichtenstein P, et al. Etiology of autism spectrum disorders and autistic traits over time. JAMA Psychiatry. (2020) 77(9):936–43. doi: 10.1001/jamapsychiatry.2020.0680
36. Bölte S, Girdler S, Marschik PB. The contribution of environmental exposure to the etiology of autism spectrum disorder. Cell Mol Life Sci. (2019) 76(7):1275–97. doi: 10.1007/s00018-018-2988-4
37. Ng M, de Montigny JG, Ofner M, Do MT. Environmental factors associated with autism spectrum disorder: a scoping review for the years 2003–2013. Health Promot Chronic Dis Prev Can. (2017) 37(1):1–23. doi: 10.24095/hpcdp.37.1.01
38. Abdullahi I, Livingston G, Thomas J, Johnson E, Wang Y, Ma Y, et al. Risk of developmental disorders in children of immigrant mothers: a population-based data linkage evaluation. J Pediatr. (2019) 204:275–84.e3. doi: 10.1016/j.jpeds.2018.08.047
39. Schmengler H, Cohen D, Tordjman S, Melchior M. Autism spectrum and other neurodevelopmental disorders in children of immigrants: a brief review of current evidence and implications for clinical practice. Front Psychiatry. (2021) 12:566368. doi: 10.3389/fpsyt.2021.566368
40. Linnsand P, Gillberg C, Nilses Å, Hagberg B, Nygren G. A high prevalence of autism spectrum disorder in preschool children in an immigrant, multiethnic population in Sweden: challenges for health care. J Autism Dev Disord. (2021) 51(2):538–49. doi: 10.1007/s10803-020-04563-8
41. Kanne SM, Bishop SL. Editorial perspective: the autism waitlist crisis and remembering what families need. J Child Psychol Psychiatry. (2021) 62(2):140–2. doi: 10.1111/jcpp.13254
42. Nilses Å, Jingrot M, Linnsand P, Gillberg C, Nygren G. Experiences of immigrant parents in Sweden participating in a community assessment and intervention program for preschool children with autism. Neuropsychiatr Dis Treat. (2019) 15:3397–410. doi: 10.2147/NDT.S221908
44. Graneheim UH, Lundman B. Qualitative content analysis in nursing research: concepts, procedures and measures to achieve trustworthiness. Nurse Educ Today. (2004) 24(2):105–12. doi: 10.1016/j.nedt.2003.10.001
45. Lindgren BM, Lundman B, Graneheim UH. Abstraction and interpretation during the qualitative content analysis process. Int J Nurs Stud. (2020) 108:103632. doi: 10.1016/j.ijnurstu.2020.103632
46. Sritharan B, Koola MM. Barriers faced by immigrant families of children with autism: a program to address the challenges. Asian J Psychiatry. (2019) 39:53–7. doi: 10.1016/j.ajp.2018.11.017
47. Mangrio E, Persson K. Immigrant parents’ experience with the Swedish child health care system: a qualitative study. BMC Fam Pract. (2017) 18:1–9. doi: 10.1186/s12875-017-0604-6
48. Wallace KS, Rogers SJ. Intervening in infancy: implications for autism spectrum disorders. J Child Psychol Psychiatry. (2010) 51(12):1300–20. doi: 10.1111/j.1469-7610.2010.02308.x
49. Vivanti G, Prior M, Williams K, Dissanayake C. Predictors of outcomes in autism early intervention: why don’t we know more? Front Pediatr. (2014) 2:58. doi: 10.3389/fped.2014.00058
Keywords: coordinated healthcare, collaboration, increased knowledge, training of medical staff, regulatory problems, autism, immigrant families
Citation: Nygren G, Gillberg C and Carlsson E (2025) Bridging gaps in healthcare: child health services and specialist care collaboration for young children with autism and coexisting conditions. Front. Pediatr. 13:1501650. doi: 10.3389/fped.2025.1501650
Received: 25 September 2024; Accepted: 7 January 2025;
Published: 6 February 2025.
Edited by:
Fabrizio Pecoraro, National Research Council (CNR), ItalyReviewed by:
Anna Rozensztrauch, Wroclaw Medical University, PolandAlexia E. Metz, University of Toledo, United States
Copyright: © 2025 Nygren, Gillberg and Carlsson. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Emilia Carlsson, ZW1pbGlhLmNhcmxzc29uQG5ldXJvLmd1LnNl
 Gudrun Nygren
Gudrun Nygren Christopher Gillberg
Christopher Gillberg Emilia Carlsson
Emilia Carlsson