- 1Department of Ophthalmology, Chengdu First People's Hospital/Chengdu Integrated TCM & Western Medicine Hospital, Chengdu, Sichuan, China
- 2Department of Respiration, Chengdu First People's Hospital/Chengdu Integrated TCM & Western Medicine Hospital, Chengdu, Sichuan, China
- 3Development Department, Chengdu First People's Hospital/Chengdu Integrated TCM & Western Medicine Hospital, Chengdu, Sichuan, China
- 4High-tech Zone Healthcare Development Center, Chengdu, Sichuan, China
- 5High-tech Zone Education Development Center, Chengdu, Sichuan, China
- 6High-tech Zone Zhonghe Primary School, Chengdu, Sichuan, China
- 7Department of Ophthalmology, High-Tech Zone Zhonghe Community Health Service Center, Chengdu, Sichuan, China
Objective: To analyze the prevalence of myopia among children and adolescents in Chengdu from 2021 to 2023, providing insights for myopia prevention and control.
Methods: This study was a school-based cross-sectional study in children and adolescents aged 3–18 years in Hi-tech District of Chengdu City. All the students underwent comprehensive ocular measurement, including uncorrected binocular visual acuity (VA), spherical equivalent error (SER) with noncycloplegic autorefraction, corneal radius (CR), and axial length (AL).
Results: Over the three-year study period from 2021 to 2023, the overall prevalence of myopia was 38.15%, with annual rates of 38.74% in 2021, 38.67% in 2022, and 37.03% in 2023. The prevalence and severity of myopia increased significantly with age (P < 0.001). The prevalence was consistently higher among girls (P < 0.001) with 40.17% in 2021, 39.43% in 2022, and 38.33% in 2023 compared to 37.03%, 38.05% and 35.85% among boys in the years, respectively. The myopia prevalence increased with school level (P < 0.001). Mild myopia was the most common (24.47%), followed by moderate (10.77%) and severe myopia (2.91%). The mean SER were −1.72 ± 1.57 D in 2021, −1.32 ± 1.51 D in 2022, and −1.42 ± 1.36 D in 2023 (P < 0.001). AL was stable across most age groups, with mean AL across the overall sample of 23.80 ± 1.02 mm in 2021, 23.79 ± 1.04 mm in 2022, and 23.81 ± 1.04 mm in 2023.
Conclusion: Myopic prevalence among children and adolescents in Hi-tech District of Chengdu City decreased from 2021 to 2023. The prevalence increased with age and school level, indicating a need for targeted interventions. Significant changes in spherical equivalent refraction and AL emphasize the importance of early intervention and regular monitoring of myopia for an effective management.
Introduction
Myopia, also known as nearsightedness, has emerged as the predominant type of refractive error worldwide, significantly impacting visual health, particularly in Asian countries. By 2050, it is projected that nearly 50% of the global population will exhibit some degree of myopia, with high myopia affecting approximately 10% (1). The escalating prevalence of myopia poses a substantial public health challenge which is alarming due to the associated risk of severe ocular complications such as myopic macular degeneration, choroidal neovascularization, retinal detachment, and glaucoma, causing irreversible visual impairment (2).
Environmental and lifestyle factors, including increased near work activities and decreased outdoor exposure, have been implicated in the surge of myopia cases. Studies suggest that time spent outdoors may mitigate the onset and progression of myopia, likely through mechanisms involving retinal dopamine release stimulated by bright light (3). Moreover, the rise in myopia prevalence has been linked to socioeconomic factors, with a higher prevalence reported in urban and economically developed regions. This suggests a complex interplay of genetic, environmental, and lifestyle influences on myopia development and progression (4).
A higher rate of myopic progression among Chinese schoolchildren during the period of the COVID-19 pandemic was demonstrated and myopia progressed more rapidly during the period (5, 6). Despite extensive research, the dynamic trends of myopia in rapidly urbanizing regions remain under-explored. Moreover, there is a paucity of cross-sectional data on the prevalence of myopia among children and adolescents in this area. Therefore, we have assessed the prevalence of myopia among children and adolescents in Hi-tech District of Chengdu City in China, provide direction and theoretical basis for the prevention and control of myopia in children and adolescents and reduce the social and economic burden of the disease. This study aims to investigate the prevalence of myopia over a three-year period among school-aged children and adolescents in Chengdu. The result will be instrumental in developing effective myopia prevention strategies during the health policy planning.
Methods
Study design and subjects
This was a school-based, cross-sectional epidemiological study conducted between October 2021 and November 2023 in the Hi-tech District of Chengdu City, Sichuan Province, China. The study was conducted in accordance to the principles of the Declaration of Helsinki. All students and their guardians were informed about the objectives, contents, and significance of the study prior to enrolment and provided verbal agreement. Those diagnosed with eye diseases other than refractive errors, such as cataract, glaucoma, keratopathy, and retinal disease were excluded. Moreover, students wearing orthokeratology lenses were classified as myopic based on their pre-orthokeratology refractive error. The participating students were enrolled from all 228 schools including kindergartens, primary schools, junior high schools, and senior high schools within the district, where the compulsory education enrollment rate was 100%. Data collection was conducted annually from October to November to minimize variations in refractive status that might arise between the conclusion of the previous school year and the onset of the next.
Examinations
Binocular uncorrected distance vision was tested using an international standard logarithmic visual acuity chart and a liquid crystal display (LCD) vision tester (Suowei). Visual acuity (VA) was recorded as decimals, with vision tested at a distance of 5 m. Non-cycloplegic refraction was measured using autorefractor (RKT-700A, NIDEK, Gamagori, Japan), with each eye measured at least three times. If any reading deviated by more than 0.50 diopters (D), the measurements were repeated until three consistent values were obtained which were then averaged for analysis. Ocular biometry parameters, including axial length (AL) and corneal radius (CR), were measured using non-contact partial coherence interferometry (SUOER SW-9000, China).
Definitions
Myopia was defined as a spherical equivalent refraction (SER) ≤−0.75D without cycloplegia, and uncorrected visual acuity (UCVA) thresholds were set according to age: UCVA >0.3 logMAR for children aged 3, >0.2 logMAR for children aged 4 to 5, and >0 logMAR for those aged 6 or older (7, 8). Myopia was further categorized into three levels: mild myopia (<−0.5D to ≥−3.0D), moderate myopia (<−3.0D to ≥−6.0), and severe myopia (<−6.0D) (9).
Data quality control
All procedures were performed by trained ophthalmologists, nurses, and technicians in line with standard operating protocols. Instruments were calibrated before use, and examiners underwent standardized training and assessment before the study. A detection error was defined as a discrepancy of more than ±1 line in visual acuity or ±0.50D in SER. If the error rate exceeded 5%, the testing data were retested (10). Data entry was meticulously double-checked to ensure accuracy; only data for the right eye was analyzed due to a high correlation between two eyes.
Statistical analysis
The decimal vision was converted into minimum resolution angular logarithmic vision for statistical analysis. Data were analyzed using SPSS 20.0 (IBM SPSS, Chicago, IL, USA). Categorical data are presented as frequencies and percentages, while continuous data are given as means ± standard deviation or medians (range). Chi-squared or Fisher's exact tests were used to compare myopia prevalence across different subgroups. Univariate analysis of variance (ANOVA) was applied to compare refractive parameters across years. A P-value <0.05 was considered statistically significant.
Results
Patients' demographic characteristics
A total of 136,195, 146,342, and 165,460 students were initially enrolled in 2021, 2022, and 2023, respectively. Of the total, 128,706 in 2021, 140,558 in 2022, and 163,670 in 2023 were eligible for the final analysis with overall participation rate of 94.50%, 94.50%, 96.05%, and 98.92% for each respective year. Of the total sample, 66,617 were boys, accounting for 51.76%, and 62,089 were girls, accounting for 48.24% of the study population. In 2021, 22,982 students were kindergarten, accounting for 23.29%, age from 3 to 5 years. Primary school students were 6–12 years old with 66,194, accounting for 51.43%. 19,335 students in junior high school were 13–15 years old, accounting for 15.02%. Senior high school and vocational high school students were 16–18 years old with 13,195, accounting for 10.25%.
Prevalence of myopia
Table 1 summarises the prevalence of myopia among genders, school type and age for the study years. Over the three-year study period from 2021 to 2023, the overall prevalence of myopia was 38.15%. Specifically, the prevalence of myopia was 38.74% in 2021, 38.67% in 2022, and 37.03% in 2023. Notably, the prevalence of myopia increased significantly with age (all P < 0.001). The prevalence of myopia was consistently higher among girls compared to boys in each year (P < 0.01). In 2021, the prevalence of myopia was 37.40% among boys and 40.17% among girls, with a similar trend observed in 2022 (38.05% in boys and 39.43% in girls) and 2023 (35.85% in boys and 38.33% in girls). The analysis of myopia prevalence across different school age segments revealed that the higher the school level, the higher the prevalence of myopia (all P < 0.001) (Table 1).
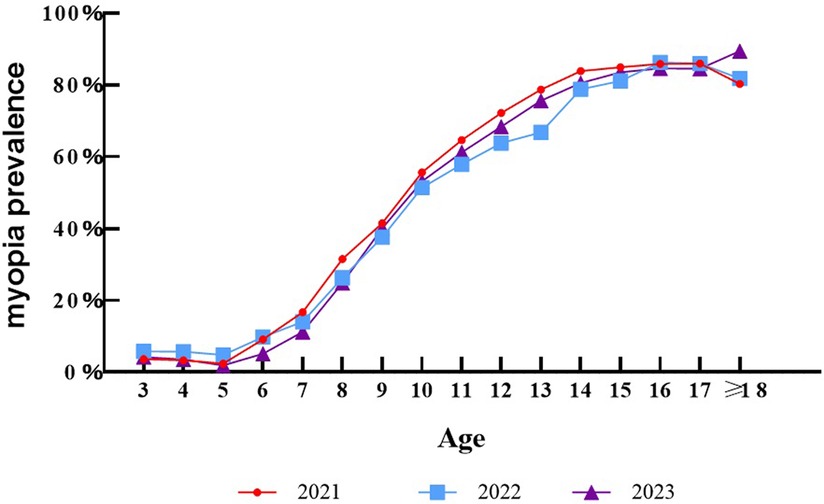
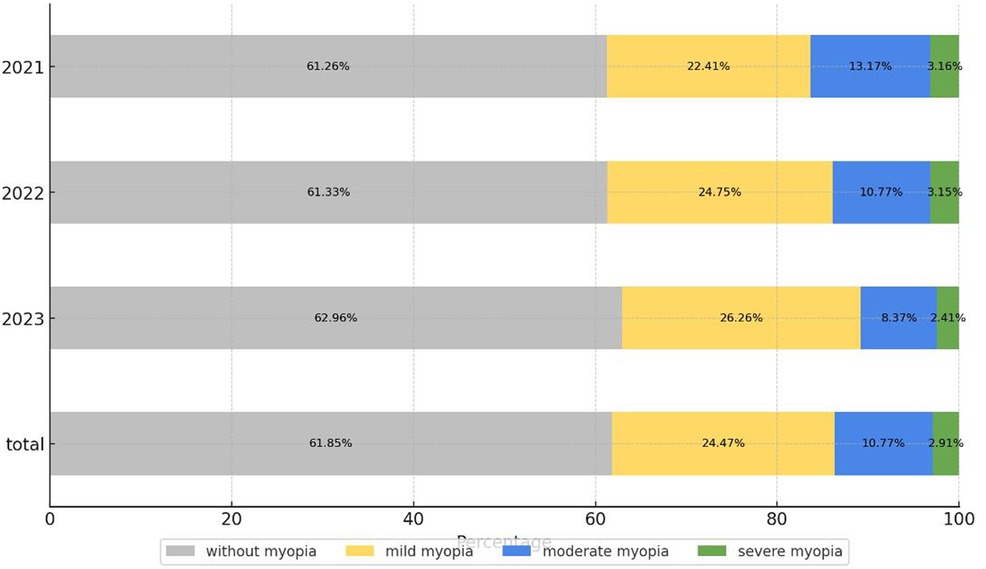
The detailed distribution of myopia severity in each year is depicted in Figure 1. Mild myopia constituted the largest proportion (24.47%), followed by moderate myopia (10.77%) and severe myopia (2.91%). There were statistically significant differences in the prevalence of myopia in different years, wherein the proportion of mild myopia in 2023 was significantly higher than that in 2021 and 2022, and there was no statistically significant difference in specific categories of myopia. As seen in Figure 2, the overall prevalence of myopia increased in a nearly linear fashion with age in each year, however, at the age of 14, the incidence of myopia was tending towards stability. The myopia rate of 3–5 years old was low and stable.
Majority of the children at the age 12 years of below had mild myopia, while the proportion of moderate myopia increased rapidly starting around 9 years old and stabilized after the age of 15. The prevalence of severe myopia began to increase at the age of 12 and gradually stabilized at the age of 16–18. With the increase of age, the degree of myopia in children and adolescents gradually increased, which is in line with the overall characteristics of myopia epidemic. The proportion of mild, moderate and severe myopia showed a step distribution, and the whole was dominated by mild and moderate myopia.
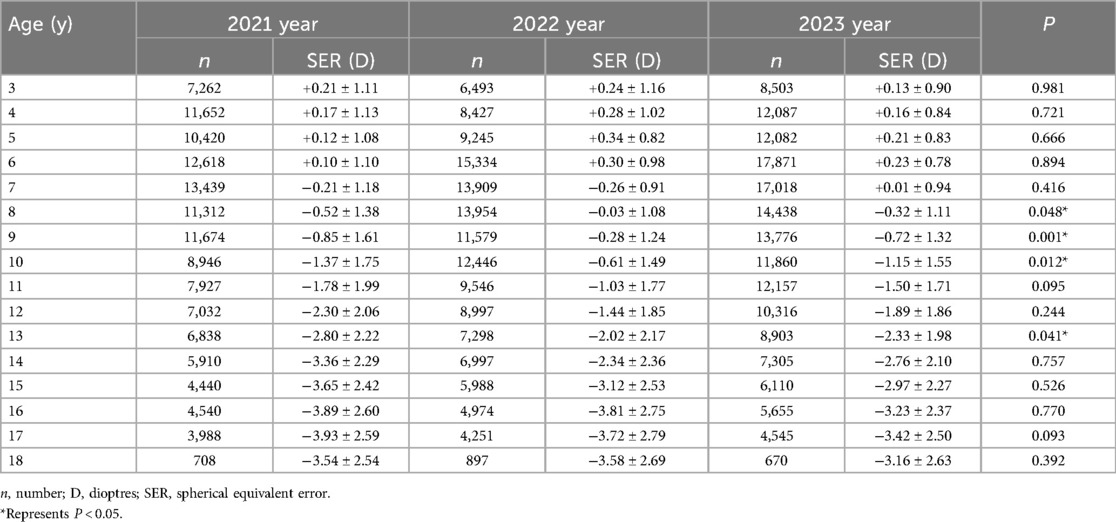
Spherical equivalent refraction
The analysis of the SER revealed a variation over the three-year study period. Specifically, the overall mean SER was −1.72 ± 1.57D in 2021, −1.32 ± 1.51D in 2022 and −1.42 ± 1.36D in 2023 (P < 0.001). The SER of different age between 2021 and 2023 are shown in Table 2. The mean SER decreased significantly with age from 3 years-old to 18 years-old (P < 0.001). There were no significant differences in each year except ages 8–10 years and 13 years old. Children and adolescents in the age range of 3–6 years old showed farsightedness as a whole, 7 years old tended to be emmetropization, and 8–18 years old children and adolescents show myopia. This variation in SER may reflect changes in refractive error patterns among the student population over time.
Axial length and axial length/corneal radius
The results of the AL analyses across the age groups are detailed in the Table 3. The mean AL was 23.80 ± 1.02 mm in 2021, 23.79 ± 1.04 mm in 2022, and 23.81 ± 1.04 mm in 2023. From ages 5–17 years, there were no significant differences in AL changes between 2021 and 2023 (P > 0.05). Statistically significant differences in AL were primarily seen in the youngest (ages 3 and 4) and oldest (age 18) age groups. (P < 0.05). The AL appears to increase progressively with age, as expected, with the highest mean values observed in older age groups (15–17 years). The axial length/corneal radius (AL/CR) ratio were analyzed across different age groups from 2021 to 2023, as detailed in Table 4. The total AL/CR was 3.07 ± 0.13 in 2021, 3.08 ± 0.13 in 2022, and 3.07 ± 0.12 in 2023. The mean AL/CR showed a significant age-related increase (P < 0.05), while no significant annual variation was detected across the study period (P > 0.05).
Discussion
In this three-year epidemiological study conducted from 2021 to 2023, we comprehensively assessed the prevalence of myopia among children and adolescents residing in the Hi-tech District of Chengdu City. Our findings revealed a significantly higher prevalence of myopia in 2021 compared to the subsequent years, albeit with annual fluctuations. This study provides valuable insights into the evolving epidemiology of myopia and underscores the need for targeted interventions to address this public health concern. During 2021 and 2022, the COVID-19 pandemic was prevalent, leading to lockdowns in Chengdu and a subsequent reduction in students' outdoor activity time. However, in early 2023, with the easing of COVID-19 restrictions, there was an increase in outdoor activity time among students.
The present study observed a near-linear increase in the prevalence of myopia with age in each year, indicating a consistent pattern of myopia development across the school-aged population. These observations align with the results of previous domestic epidemiological investigations (11). Notably, the incidence of myopia tended to stabilize at age of 14 years, indicating a potential deceleration in the progression of myopia during the later adolescent years. This finding is consistent with prior research that associates myopia progression with the adolescent growth spurt. However, the leveling off of myopia prevalence after post-16 highlights the importance of implementing proactive myopia prevention and control measures during early adolescence to mitigate the rapid progression of myopia and reduce the risk of high myopia.
The significant annual changes in SER observed from 2021 to 2023 suggest notable shifts in refractive error patterns among school-aged children. The marked shift towards more negative SER values from 2022 to 2023 is particularly concerning, as it may be linked to increased online learning, reduced outdoor activities, and extended screen time. This trend reveals the profound impact of lifestyle changes on the visual health of youth, necessitating further investigation into these environmental factors and their role in refractive error development. During the outbreak of COVID-19, many environmental changes occurred including the reduced time outdoors and increase in screen time, which may contribute to the increase of myopia shift and elongation of axial length during the home quarantine (12). Future research should focus on devising targeted interventions to enhance visual health in students by mitigating modifiable lifestyle factors, such as promoting outdoor activities and regulating screen time (13).
Overall, the combination of SER and AL data provides insights into the refractive status and ocular growth patterns among school-aged children over time. As AL is a crucial indicator of myopia risk, accurate measurement and long-term monitoring of AL are essential for developing personalized myopia prevention strategies. Future research should focus on elucidating the physiological and pathological mechanisms underlying AL changes in these specific age groups. Understanding these factors is critical for the advancement of targeted interventions aimed at mitigating myopia progression in vulnerable populations (14). Given the strong correlation between the AL/CR ratio and SER, several studies propose that the AL/CR ratio may serve as a sensitive indicator for early myopia detection (15, 16). The combined use of UCVA and non-cycloplegic SER tests and the combined use of AL/CR and non-cycloplegic SER tests achieved optimal accuracy for myopia screening (17). In our study, the age-proportional increase in AL/CR aligns with previous studies associating higher AL/CR ratios with increased myopia risk during critical developmental years. These findings support the use of AL/CR as a reliable indicator to emphasize the importance of early screening in younger populations, particularly as the AL/CR ratio begins to approach critical thresholds predictive of myopia (15).
In this study, we acknowledge the potential bias introduced by using a noncycloplegic refraction, which tends to overestimate the magnitude of myopia. To mitigate this limitation, we have employed a rigorous definition of myopia that combines non-cycloplegic SER and UCVA measurements. Specifically, we defined myopia as a UCVA greater than 0.0 logMAR and SER of −0.75 D or less in right eye. This definition is intended to account for the non-cycloplegic nature of the autorefraction, which is known to overstate the prevalence of myopia among younger populations (18, 19). Given the concern about the overestimation of myopia prevalence due to non-cycloplegic refraction, researchers have explored alternative methods to improve accuracy (17). Thorn proposed that combining non-cycloplegic refraction with VA measurements can enhance the accuracy of myopia diagnosis compared to relying solely on non-cycloplegic refraction (20). We concur with this approach and have implemented it in our study. It is worth noting that for younger children aged 3–6 years, the criteria for myopia should be tailored to each age group, as the average visual acuity varies with age (17). Therefore, when applying our definition of myopia to this younger age group, it is essential to consider the normal range of VA for that specific age. By doing so, we can ensure a more precise and accurate assessment of myopia in children.
This comprehensive study accentuates a pivotal trend in the escalating prevalence of myopia based on school type, particularly as they progress through higher grade levels. The data reveals a stark increase, peaking at an alarming 85.70% in general high schools, which is attributed not only to the cumulative nature of myopia but potentially also to the augmentation of academic demands and the intensified use of the visual system as students ascend grade levels. Despite the introduction of policies aimed at alleviating the academic workload in various regions of China, and their diligent implementation by schools, the current burden on students remains substantial (21). Additionally, the phenomenon of parents adopting a “starting line” mentality, effectively shifting the reduced schoolwork pressure onto their children, has significantly augmented ocular strain, thereby contributing to the persistently high prevalence of myopia among children (22).
Conclusions
This three-year long study revealed an overall myopia prevalence of 38.15% among children and adolescents in Hi-tech District of Chengdu City, with the highest rates observed among older students and girls. Myopic prevalence among children and adolescents was shown to decrease from 2021 to 2023. The prevalence increased with age and school level, highlighting the need for targeted myopia prevention and control strategies. Analysis of SER indicated significant changes in refractive error patterns, with myopia becoming prevalent from age 8 onwards. AL measurements showed consistent growth patterns across most age groups, though significant differences were noted at the youngest and oldest ages. These findings warrant the importance of early intervention and regular monitoring to address the rising trend of myopia and to support ocular health in school-aged populations.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by the Ethics Committee of Chengdu First People's Hospital (Chengdu, China). The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants' legal guardians/next of kin.
Author contributions
XW: Writing – original draft, Funding acquisition, Formal Analysis, Data curation. LZ: Writing – review & editing, Conceptualization. YX: Writing – original draft, Conceptualization. MX: Writing – original draft, Conceptualization. QS: Writing – review & editing, Formal Analysis, Data curation. WL: Writing – review & editing, Formal Analysis, Data curation. LL: Writing – review & editing, Formal Analysis, Data curation. YL: Writing – review & editing, Formal Analysis, Data curation. RZ: Writing – review & editing, Formal Analysis, Data curation. KS: Writing – review & editing, Formal Analysis, Data curation. XT: Writing – review & editing, Conceptualization. HG: Data curation, Formal Analysis, Project administration, Writing – review & editing. CY: Data curation, Formal Analysis, Project administration, Writing – review & editing. CL: Data curation, Formal Analysis, Resources, Writing – review & editing. XL: Data curation, Formal Analysis, Project administration, Writing – review & editing. HL: Writing – review & editing, Supervision. LY: Writing – review & editing, Supervision. JL: Writing – review & editing, Methodology. ZC: Writing – review & editing, Methodology, Conceptualization.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This work is supported by Health Commission of Chengdu general project (No. 2023120) and Sichuan Province 2023 stick hanging project (No. 2023YFS0506).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Holden BA, Fricke TR, Wilson DA, Jong M, Naidoo KS, Sankaridurg P, et al. Global prevalence of myopia and high myopia and temporal trends from 2000 through 2050. Ophthalmology. (2016) 123(5):1036–42. doi: 10.1016/j.ophtha.2016.01.006
2. Wong YL, Saw SM. Epidemiology of pathologic myopia in Asia and worldwide. Asia Pac J Ophthalmol (Phila). (2016) 5(6):394–402. doi: 10.1097/APO.0000000000000234
3. Dhakal R, Shah R, Huntjens B, Verkicharla PK, Lawrenson JG. Time spent outdoors as an intervention for myopia prevention and control in children: an overview of systematic reviews. Ophthalmic Physiol Opt. (2022) 42(3):545–58. doi: 10.1111/opo.12945
4. Kai JY, Li DL, Hu HH, Zhang XF, Pan CW. Impact of area-level socioeconomic and environmental measures on reduced visual acuity among children and adolescents. Invest Ophthalmol Vis Sci. (2023) 64(7):23. doi: 10.1167/iovs.64.7.23
5. Luo Z, Guo C, Yang X, Zhang M. Comparison of myopia progression among Chinese schoolchildren before and during COVID-19 pandemic: a meta-analysis. Int Ophthalmol. (2023) 43(10):3911–21. doi: 10.1007/s10792-023-02777-0
6. Laan D, Tan E, Huis IHVP, Jellema HM, Jenniskens K. Myopia progression in children during home confinement in the COVID-19 pandemic: a systematic review and meta-analysis. J Optom. (2024) 17(1):100493. doi: 10.1016/j.optom.2023.100493
7. Wang J, Liu J, Ma W, Zhang Q, Li R, He X, et al. Prevalence of myopia in 3–14-year-old Chinese children: a school-based cross-sectional study in Chengdu. BMC Ophthalmol. (2021) 21(1):318. doi: 10.1186/s12886-021-02071-6
8. Zhang J, Li Z, Ren J, Wang W, Dai J, Li C, et al. Prevalence of myopia: a large-scale population-based study among children and adolescents in Weifang, China. Front Public Health. (2022) 10:924566. doi: 10.3389/fpubh.2022.924566
9. Zhang D, Sun B, Wu M, Liu H, Zhou L, Guo L. Prevalence and associated factors of myopia among school students in Shenyang, China: a cross-sectional study. Front Public Health. (2023) 11:1239158. doi: 10.3389/fpubh.2023.1239158
10. Zhu MH, Lin TN, Lin JH, Wen Q. Myopia among children and adolescents: an epidemiological study in Fuzhou city. Front Pediatr. (2023) 11:1161329. doi: 10.3389/fped.2023.1161329
11. Lin T, Hu J, Lin J, Chen J, Wen Q. Epidemiological investigation of the status of myopia in children and adolescents in Fujian Province in 2020. Jpn J Ophthalmol. (2023) 67(3):335–45. doi: 10.1007/s10384-023-00991-y
12. Pan W, Lin J, Zheng L, Lan W, Ying G, Yang Z, et al. Myopia and axial length in school-aged children before, during, and after the COVID-19 lockdown-A population-based study. Front Public Health. (2022) 10:992784. doi: 10.3389/fpubh.2022.992784
13. Zong Z, Zhang Y, Qiao J, Tian Y, Xu S. The association between screen time exposure and myopia in children and adolescents: a meta-analysis. BMC Public Health. (2024) 24(1):1625. doi: 10.1186/s12889-024-19113-5
14. Jiang F, Wang D, Yin Q, He M, Li Z. Longitudinal changes in axial length and spherical equivalent in children and adolescents with high myopia. Invest Ophthalmol Vis Sci. (2023) 64(12):6. doi: 10.1167/iovs.64.12.6
15. He X, Zou H, Lu L, Zhao R, Zhao H, Li Q, et al. Axial length/corneal radius ratio: association with refractive state and role on myopia detection combined with visual acuity in Chinese schoolchildren. PLoS One. (2015) 10(2):e111766. doi: 10.1371/journal.pone.0111766
16. Zhao E, Wang X, Zhang H, Zhao E, Wang J, Yang Y, et al. Ocular biometrics and uncorrected visual acuity for detecting myopia in Chinese school students. Sci Rep. (2022) 12(1):18644. doi: 10.1038/s41598-022-23409-0
17. Wang J, Xie H, Morgan I, Chen J, Yao C, Zhu J, et al. How to conduct school myopia screening: comparison among myopia screening tests and determination of associated cutoffs. Asia Pac J Ophthalmol (Phila). (2022) 11(1):12–8. doi: 10.1097/APO.0000000000000487
18. Flitcroft DI, He M, Jonas JB, Jong M, Naidoo K, Ohno-Matsui K, et al. IMI—defining and classifying myopia: a proposed set of standards for clinical and epidemiologic studies. Invest Ophthalmol Vis Sci. (2019) 60(3):M20–30. doi: 10.1167/iovs.18-25957
19. Gopalakrishnan A, Hussaindeen JR, Sivaraman V, Swaminathan M, Wong YL, Armitage JA, et al. The Sankara Nethralaya Tamil Nadu Essilor Myopia (STEM) study-defining a threshold for non-cycloplegic myopia prevalence in children. J Clin Med. (2021) 10(6):1215. doi: 10.3390/jcm10061215
20. Thorn F, Chen J, Li C, Jiang D, Chen W, Lin Y, et al. Refractive status and prevalence of myopia among Chinese primary school students. Clin Exp Optom. (2020) 103(2):177–83. doi: 10.1111/cxo.12980
21. Wang Y. Exploring the impact of workload, organizational support, and work engagement on teachers' Psychological wellbeing: a structural equation modeling approach. Front Psychol. (2023) 14:1345740. doi: 10.3389/fpsyg.2023.1345740
Keywords: myopia, prevalence, spherical equivalent error, axial length, epidemiological
Citation: Wang X, Zeng L, Xian Y, Xin M, Shan Q, Li W, Lv L, Liu Y, Zhang R, Song K, Tian X, Guo H, Yan C, Li C, Luo X, Luo H, Yang L, Luo J and Chen Z (2025) Prevalence of myopia and refractive parameters among children and adolescents in Hi-tech District of Chengdu City. Front. Pediatr. 12:1502660. doi: 10.3389/fped.2024.1502660
Received: 27 September 2024; Accepted: 25 November 2024;
Published: 3 February 2025.
Edited by:
Siti Nurliyana Abdullah, Raja Isteri Pengiran Anak Saleha Hospital, BruneiReviewed by:
Ikrami Azmi, Ministry of Health, BruneiJit Ale Magar, Children's Health Queensland, Australia
Copyright: © 2025 Wang, Zeng, Xian, Xin, Shan, Li, Lv, Liu, Zhang, Song, Tian, Guo, Yan, Li, Luo, Luo, Yang, Luo and Chen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zejun Chen, Mjk2MTUwNzM4QHFxLmNvbQ==
 Xiaoqin Wang1
Xiaoqin Wang1 Liuzhi Zeng
Liuzhi Zeng Zejun Chen
Zejun Chen