- 1Department of Child and Adolescent Mental Health, University Hospital Erlangen, Friedrich-Alexander-Universität Erlangen-Nürnberg (FAU), Erlangen, Germany
- 2Department of Pediatric Cardiac Surgery, University Hospital Erlangen, Friedrich-Alexander-Universität Erlangen-Nürnberg (FAU), Erlangen, Germany
- 3Department of Pediatric Cardiovascular Surgery, Pediatric Heart Center, University Children’s Hospital Zürich, Zürich, Switzerland
Introduction: Many studies have investigated the impact of congenital heart defects (CHD) on child development. However, because CHD not only affects the child and his or her development but, also the entire family, family functioning after pediatric cardiac surgery is of increasing research interest. This prospective childhood-adolescence case-control study aimed to examine differences and changes in parenting behavior and mother-child relationship quality after early surgical repair of an isolated ventricular septum defect (VSD) compared to non-affected controls.
Patients and methods: 39 affected children (M = 7.3 years) with surgically repaired VSD and their mothers were compared with a matched, non-affected control group of 39 mother-child-dyads (M = 7.3 years) during primary school age (t1). At child early adolescence, 24 affected children (M = 12.4 years) and 24 children of the control group (M = 13.2 years) were examined again (t2). Parenting behavior characteristics (t1: mother report; t2: mother- and child report) and mother-child relationship quality (t2: child report) were measured by standardized questionnaires.
Results: The mother-rated parenting behavior dimensions Involvement (p < .001, η2p = .37), Parental Monitoring (p = .014, η2p = .17) and Corporal Punishment (p < .001, η2p = .57) significantly decreased from t1 to t2 in both cohorts. Responsible Parenting Behavior tended to decrease from t1 to t2 in the control group, while remaining stable in the VSD-group (p = .088, η2p = .09). Independent of the group, higher mother-child relationship quality was associated with more Positive Parenting Behavior (p < .001, η2p = .34), more Involvement (p = .003, η2p = .22) and fewer Inconsistency (p < .001, η2p = .31) in the child-rating; and more Positive Parenting Behavior in the mother-rating (p = .039, η2p = .10).
Conclusion: VSD affected mother-child-dyads were mostly comparable in their parenting behavior characteristics and mother-child relationship quality to non-affected controls. The absence of a decrease in maternal Responsible Parenting Behavior in the VSD group may indicate challenges during the developmental task of autonomy in adolescence. Nevertheless, adaptive family functioning after early pediatric surgical VSD repair seems possible.
Introduction
Occurring in one percent of newborns congenital heart defects (CHDs) are the most common form of organ mutation in humans (1), with approximately 90% of the affected children reaching adulthood (2). CHDs include various types of defects, ranging from mild to drastically severe (3). Of these, ventricular septal defects (VSDs) are the most common form of CHD, with a prevalence of 3 per 1,000 live births (4). Isolated VSDs are considered a “simple” form of severity compared to more complex forms such as tetralogy of Fallot or univentricular hearts (5). Due to medical advancements, morbidity and mortality rates as well as potential complications are considerably low and the morbidity and mortality rates have been drastically reduced in the last few decades. Thus, long-term physical outcomes after surgery are described as excellent (6). Although treated children with VSD are expected to have almost similar somatic developmental outcomes to non-affected children, little research has been devoted to the psychosocial adjustment of affected children. Recent studies have shown that psychosocial adjustment and a high quality of life after early VSD repair are possible, especially when mothers of affected children reported low anxiety levels and highly proactive and warm parenting styles (7, 8).
CHDs and the resulting need for early pediatric cardiac surgery can place a heavy burden on the whole family (7, 9) Parents of affected children may show signs of increased stress (increased cortisol concentrations) and anxiety levels (9–12), which may be explained by various factors such as receiving the initial diagnosis, the process of surgery, and separation from parents during treatment and lack of psychological support during this period (13). Families with fewer psychosocial resources and less social support are at an even greater risk of experiencing stress and lower quality of life in the following period (14). In addition, affected parents may develop long-term symptoms of post-traumatic stress disorder (PTSD) due to the diagnosis and associated stress (10). Clinical symptoms of trauma can be found in one-third of mothers and one-fifth of fathers one month after surgery (15). Next to increased stress levels, 18% of parents of children with CHD reported unusual levels of anxiety (16).
Impaired parental mental health may therefore influence the socioemotional, behavioral, and cognitive development of the child, for example through less sensitive parental care (17, 18). Ongoing trauma reactions can impair parents’ ability to be available and to provide sensitive and attentive care to their child and maternal anxiety is the most important risk factor for developing behavioral problems in children with CHD (19). Some studies have already demonstrated that parental stress and maternal anxiety increase the risk of behavior problems in CHD cohorts (19–21). In addition to surgery and subsequent medical treatment parental characteristics also have an additional influence on child development (22). Particularly when coping with early open heart surgery in early childhood, children rely on their parent's support in behavioral and emotional regulation (23), thus highlighting the role of parents for their affected children (7, 8, 24).
Based on the hypothesized underlying mechanism of parental characteristics influencing child development psychosocial stressors—such as parental psychopathology or poor health condition of the child—have a negative impact on mother-child interaction by impairing emotionally warm and sensitive interaction with their child, resulting in negative consequences for child development (10, 25, 26). Difficulties in mother-child interaction in families with CHD-affected children due to increased psychosocial stress have already been reported (26), and linked parental stress to altered parenting behaviors as well as dysfunctional infant brain development and behavioral, cognitive, and socio-emotional impairments in affected children (24, 27).
The existing literature provides mixed results on the association between the severity of CHD and the impact on parental outcomes. Some studies have demonstrated higher parental stress levels and more mental health problems with increasing severity of diagnosis (28–30), while in contrast, others reported no significant predictive value of CHD severity on parental outcomes (25, 31, 32).
Although VSD is considered to be a “simple” form of CHD with an almost similar somatic developmental outcome as described earlier (6), previous results examining our cohort of isolated VSD-affected children and their mothers demonstrated lower levels of maternal hair cortisol concentrations (hypocortisolism) during children`s primary school age (6–9 years) resulting in higher maternal stress levels (9). Furthermore, anxiety symptoms were elevated at primary school age when their mother had anxiety symptoms herself. However, positive parenting behaviors and a positive mother-child relationship could be protective factors and attenuate the impact of parental stress and anxiety on the child (7). This raises the question of whether parenting behaviors and the quality of the mother-child relationship are affected after the child's early surgical repair of VSD. As parenting behaviors and the mother-child relationship are important predictors for child development (17), this is crucial for later psychosocial adjustment.
Although other studies have investigated the impact of CHD on child development, little is known about characteristics of parenting behavior and parent-child relationship quality in primary school age and adolescence, with the focus of research predominantly being on infants and toddlers (33). Therefore, this prospective case-control study aimed to examine differences and changes in parenting behavior characteristics and mother-child relationship quality of the previously reported VSD-corrected group compared to a non-affected control group from primary school age to early adolescence (7–9).
Methods
Participants and study design
The present study is part of a longitudinal research project of the Department of Child and Adolescent Mental Health and the Department of Pediatric Cardiac Surgery at the University Hospital Erlangen, Germany (7). Aim of the longitudinal research project was to investigate the long-term psychological consequences of early surgical correction of isolated VSD from child primary-school age to early adolescence. From March 2006 to March 2012, 86 children underwent surgery for isolated VSD before their third birthday (t0, see Figure 1).
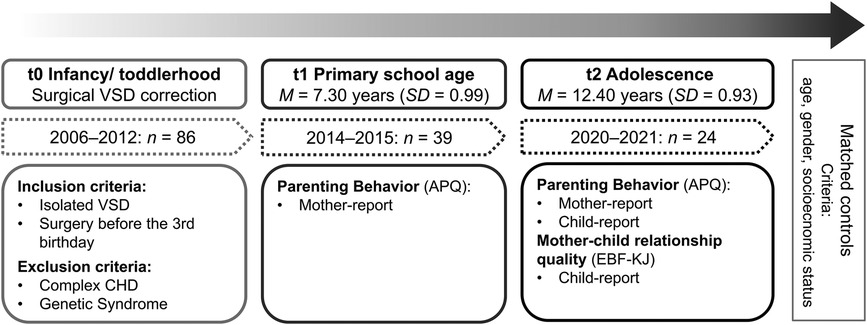
Figure 1. Study design. VSD, ventricular septal defect; CHD, congenital heart diseases; APQ, Alabama parenting questionnaire (34), EBF-KJ, Parent Image Questionnaire for Children and Adolescents (35).
In 2015, families were invited to participate in the follow-up study. Children with a genetic syndrome (e.g., Down syndrome; n = 14), additional congenital malformations (e.g., VACTERL association; n = 5), and complex heart defects (e.g., tetralogy of Fallot; n = 6) were excluded to provide a homogenous cohort without data corruption by complex differences of the underlying heart disease. Families whose current address could not be determined (n = 6) were also excluded from the sample. One child died from non-cardiological causes. The remaining 54 families were contacted by mail, of which 39 families participated in the first data collection at child primary-school age (t1, survey period 2014–2015; drop-out rate 28%). In 2020, the n = 39 families were contacted again and invited to a follow-up survey in early adolescence (t2). Of these, n = 24 children participated with their mothers in the second data collection (drop-out rate 38%). At both measurement times, the VSD group was matched with a non-affected control group for sex, age, and socioeconomic status recruited from the Franconian Cognition and Emotion Studies child and adolescent general-population sample (36). More detailed information on the study cohort the control group was recruited from can be found in the related study protocols (8, 9). Descriptive data and a comparison between the VSD-group and the control group are presented in Table 1. The adolescents in the VSD group were about 1 year younger than the control group at t2. Our data collection took place during the COVID-19 pandemic, which caused some delays in the course of the study, resulting in the age difference.
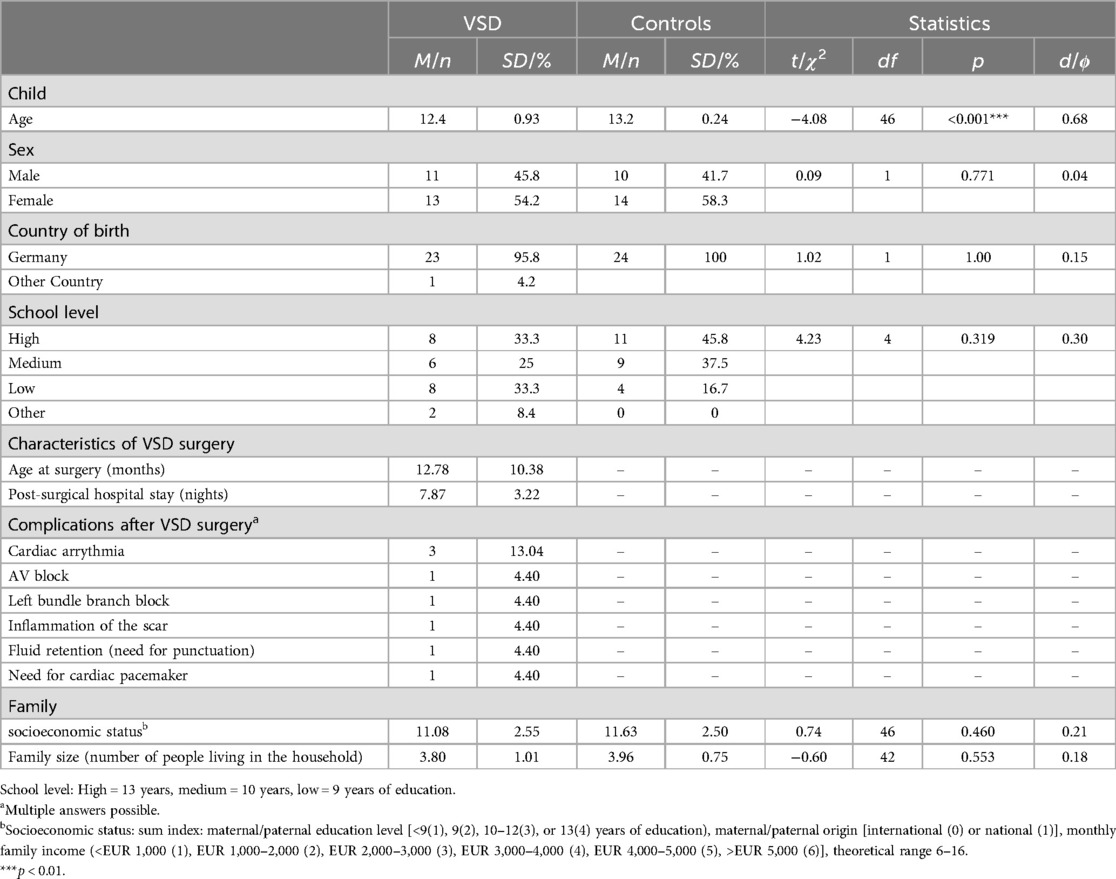
Table 1. Child and family descriptive data at t2 (adolescence) in VSD (n = 24) and control group (n = 24).
At t1 and t2, mothers filled out questionnaires on their parenting behavior; at t2, adolescents answered questionnaires on the mother-child relationship quality and maternal parenting behavior.
The study protocol was approved by the local ethics committee of the Medical Faculty of the University of Erlangen-Nürnberg (t1: 4,596, 2 April 2014; t2: 353_18B, 12 April 2019), and was conducted in accordance with the Declaration of Helsinki. All mothers gave written informed consent for the study as well as for publication of the results, all children gave informed assent.
Measures
Maternal parenting behavior
The German 40-item version of the Alabama Parenting Questionnaire (APQ) (34, 37) for parents (t1 and t2), and the 41-item version for their children (t2) is well-validated and was used to assess maternal parenting behavior dimensions in a pen-and-paper format. For the mother, the APQ captures the dimensions of Inconsistency (6 items), Positive Parenting Behavior (6 items), Involvement (6 items), Low Monitoring (6 items), Corporal Punishment (4 items), Powerful Enforcement (6 items), and Responsible Parenting behavior (6 items). For the child, the APQ captures the dimensions of Inconsistency (6 items), Positive Parenting Behavior (8 items), Involvement (17 items), and Low Monitoring (10 items) on four subscales. Each item is assessed using a five-point Likert scale [“almost never” (1) to “almost always” (5)], resulting in subscale mean value ranges from 1 to 5. The dimension of Inconsistency assesses parenting behavior that lacks consistency, such as threatening to punish a child but failing to follow through. Realibility for Inconsistency is high (Cronbach's α = 0.72). Positive Parental Behavior (α = 0.84) involves emotional warmth and child-centered interactions, such as praising a child for doing well. Involvement (α = 0.66) measures active parental support for a child's development through participation in activities, such as helping with homework. The dimension Low Monitoring (α = 0.75) is used to measure the extent to which parents lack information about their child's social contacts and activities, for instance, if a child is out of the house and the parent is unaware of their whereabouts. The dimension Corporal Punishment (α = 0.60) includes examples such as holding children down or shaking them when they do something wrong. Powerful Enforcement (α = 0.71) examines an authoritarian parenting style and is described as overreacting and emotionally negative. Responsible Parenting Behavior (α = 0.72) captures a conscious educational attitude of the parent, such as discussing free time activities with the child (37).
Mother-child relationship quality
The child-rated mother-child relationship quality was assessed using the Parent Image Questionnaire for Children and Adolescents (EBF-KJ) (35) in a pen-and-paper format. The questionnaire consists of three resource dimensions (Cohesion: 5 items, Identification: 4 items, Autonomy: 4 items) and five risk dimensions (Conflicts, Rejection/Indifference, Punishment, Emotional Appropriation, Fears/Overprotection). Each item is rated using a five-point Likert scale [“never” (1), “rarely” (2), “sometimes” (3), “often” (4), “always” (5)]. For each dimension, a mean total score was calculated and transformed into sex- and age-standardized T-Scores (M = 50, SD = 10). To calculate the score for the mother-child relationship quality, the sum of the five risk dimensions was subtracted from the sum of the three resource dimensions, resulting in an index value (T-values with a theoretical range between 0 and 84). T-Scores < 35 indicate strained, lower relationship quality, and high T-Scores > 65 indicate above-average positive relationship quality (38). The overall reliability of the EBF-KJ is high (α > 0.80).
Socioeconomic status
Socioeconomic Status was assessed by creating a sum index based on parental education level [four categories: <9 (1), 9 (2), 10–12 (3), or 13 (4) years of education], parental origin [two categories: international (0) or national (1)] and monthly family income [six categories: <EUR 1,000 (1), EUR 1,000–2,000 (2), EUR 2,000–3,000 (3), EUR 3,000–4,000 (4), EUR 4,000–5,000 (5), >EUR 5,000 (6)] with a theoretical range from 6 to 16 (7).
Statistical analyses
Statistical analyses were conducted using IBM® SPSS® Statistics version 28 (IBM Corporation, Armonk, NY, USA, 2021). Normal distribution (Shapiro-Wilk test) and variance homogeneity (Levene's test) were tested without any abnormalities. Two-sided tests were performed, and α = 5% was specified (p < .05 = significant, p < .01 = highly significant, p < .10 = trend significant). Due to the small sample size, we also reported trend significance. Effect sizes (Phi Coefficient φ, Cohen's d, Partial Eta Squared η2p) were expressed in absolute numbers and interpreted as follows: η2p ≥ .01 small, η2p ≥ .06 medium, η2p ≥ .14 large effect; d ≥ .20 small, d ≥ .50 medium, d ≥ .80 large effect; φ ≥ .10 weak, φ ≥ .30 medium, and φ ≥ .50 strong association (39). For hypotheses testing, first, asking for parenting behavior differences between the VSD- and control group in primary-school age (t1) and adolescence (t2), analyses of variance with repeated measures (ANOVArm) were conducted for each dimension of the mother-rated parenting behavior questionnaire (between-subject factor: VSD group yes/no; time factor: primary-school age t1, adolescence t2). The group main effect (is there a general difference between VSDs and controls in the parenting behavior dimension?), the time main effect (is there a general developmental effect in the parenting behavior dimension independent of group status?), and the group*time interaction (is there a developmental time-effect for only one group?) effect were interpreted. When interaction effects were significant, post hoc comparisons (t-tests) were calculated. Second, unpaired t-tests were calculated to compare VSD-affected children with non-affected controls in terms of maternal parenting behavior dimensions and mother-child relationship quality. Third, asking for effects of maternal parenting behavior dimensions on child-rated mother-child relationship quality, analyses of covariance (ANCOVA) were calculated with the mother-child relationship quality as a dependent measure (between-subject factor: VSD group yes/no; independent measures/covariates: mother-/child-rated parenting behavior at t1 and t2) with post hoc pair-wise t-tests were interaction effects were significant.
Results
Descriptive data
Sample characteristics are depicted in Table 1. Adolescents in the VSD-group were younger (M = 12.4, SD = 0.93) than in the non-affected control group (M = 13.2, SD = 0.24; p < .001). Descriptive parenting behavior data can be found in Table 2.
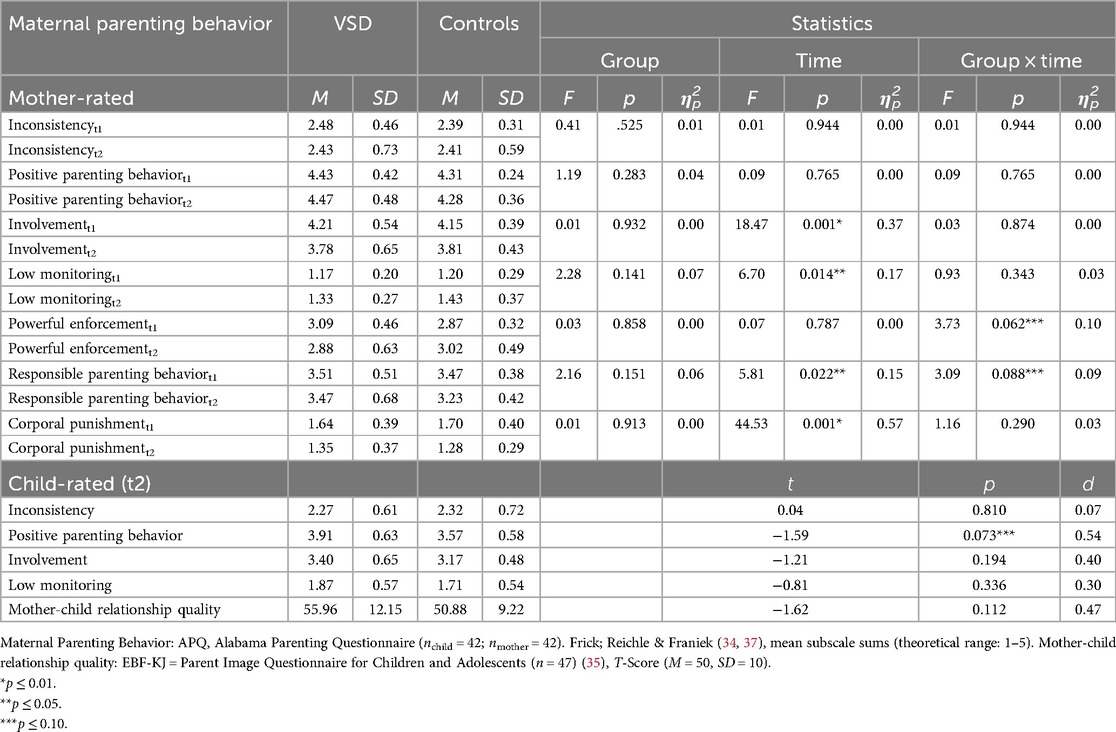
Table 2. Questionnaire descriptive data and mean differences in mother-rated maternal parenting behavior dimensions between groups (VSD vs. controls) and over time (t1 to t2), ANOVArm results.
Developmental change (t1 to t2) and group differences (VSD vs. controls) in mother-rated maternal parenting behavior
ANOVArm results are presented in Table 2. There were no significant time, group, or interaction effects for the parenting dimensions Inconsistency and Positive Parenting. Thus, there was no general developmental effect from primary school age to adolescence or a VSD vs. control group difference at no measurement time point. Significant general developmental effects—independent of VSD status—from t1 to t2 were found for Involvement (p < .001, η2p = .37), Responsible Parenting (p = .022, η2p = .15), Monitoring (p = .014, η2p = .17) and Corporal Punishment (p < .001, η2p = .57): These four parenting strategies decreased from t1 to t2 for all study participants (see Figure 2). The effects were large. For Powerful Enforcement and Responsible Parenting, there were interaction effects by trend (p = .062, η2p = .10/p = .088, η2p = .09) at medium effect size. There were no significant post hoc results for Powerful Enforcement. However, post hoc tests revealed that Responsible Parenting differed in adolescence between the VSD-group and controls (p = .051, η2p = .11) and the decrease was only significant for controls (p < .05, η2p = .20), whereas it remained stable over time in the VSD-group (see Figure 2).
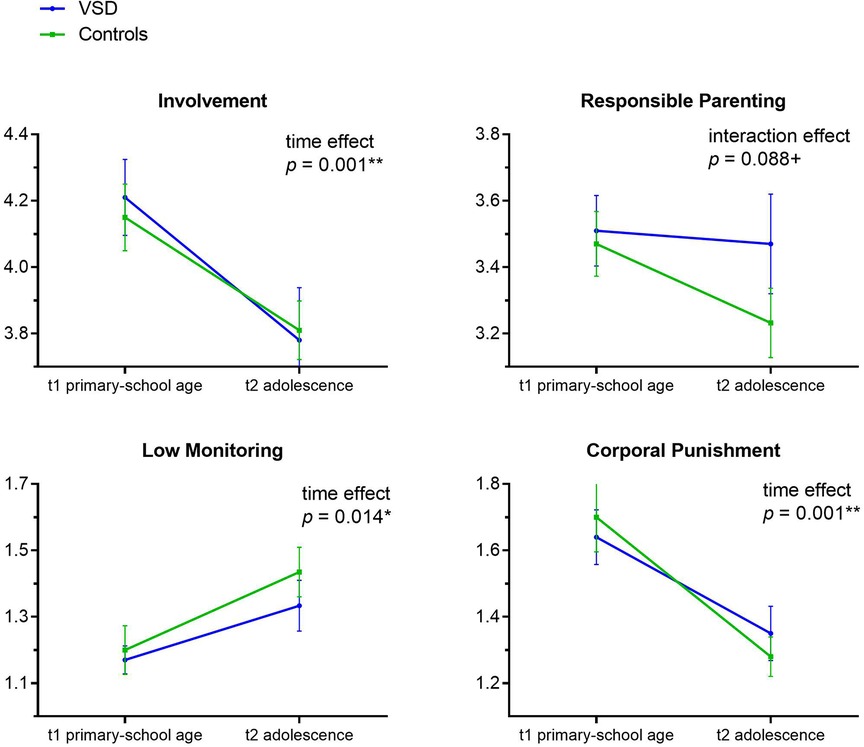
Figure 2. Developmental changes in maternal parenting behaviour dimensions from primary-school age (t1) to adolescence (t2) for significant ANOVA results. Alabama Parenting Questionnaire Subscale Scores, theoretical range 1–5 (37).
Post hoc power analyses
Post hoc power analyses for ANOVArm and within-between subject factor interaction with a sample size of n = 48 and an α error probability of 0.05 revealed observed effect sizes in the range of 0.09 < η2p < 0.57 statistically relevant effects with a statistical power (1 – β) of > 0.98.
Group differences (VSD vs. controls) of child-rated maternal parenting behavior in adolescence
Unpaired t-tests revealed that adolescents of the VSD-group reported their mothers showed more Positive Parenting Behavior than adolescents in the control group by trend with medium effect size [t(48) = −.159, p = .073, d = 0.54; Table 2]. There were no other significant differences in child-rated maternal parenting behaviors showing that both groups rated their mothers as comparable in behaviors such as Inconsistency, Involvement, and Low Monitoring.
Post hoc power analyses
Post hoc power analysis for unpaired t-tests with a sample size of n = 48 and an α error probability of 0.05 revealed the observed effect size d = 0.54 statistically relevant effects with a statistical power (1 – β) of 0.45.
Group differences in child-rated mother-child relationship quality under consideration of parenting behavior
Table 3 presents the pre-correlations of mother-child relationship quality dimensions [child-rating, (t2)] and parenting behavior dimensions [mother-ratings (t1, t2) and child-rating (t2)]. The following parenting behavior dimensions were added as covariates to the ANCOVA analysis: Mother-rating (t2): Positive Parenting; child-rating (t2): Inconsistency, Positive Parenting and Involvement.
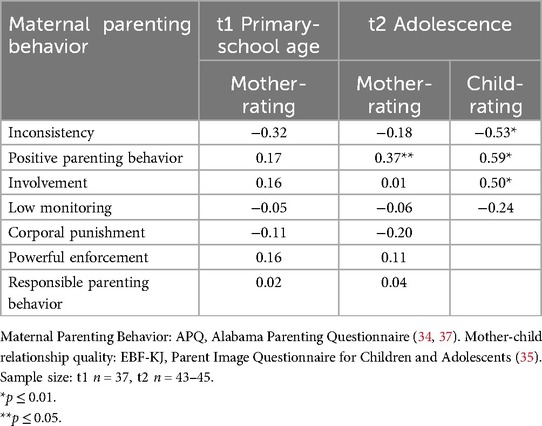
Table 3. Pearson correlations of mother-child relationship quality (total score, t2) with maternal parenting behavior dimensions.
Table 4 shows the ANCOVA results, analyzing the effects of maternal parenting behavior dimensions on child-rated mother-child relationship quality in separate analyses. Independent of group, less Inconsistency [F (1, 40) = 17.92, p < .001, η2p = .31], more Positive Parenting [F (1, 41) = 20.83, p < .001, η2p = .34] and more Involvement [F (1, 38) = 10.40, p < .05, η2p = .22] in the child-rating were associated with higher mother-child relationship quality; the results were significant and of large effect size. At medium effect size, the maternal Positive Parenting rating was significantly positively associated with mother-child relationship quality [F (1, 39) = 4.54, p < .05, η2p = .10]. Meaning, independent of VSD-status, for all study participants named parenting behavior dimensions correlated with a positive mother-child relationship in adolescence. Furthermore, analyses revealed a marginal group effect, when child-rated Inconsistency was added as a covariate: The mother-child relationship quality rating was higher for VSD-affected adolescents than for controls [F (1, 40) = 2.87, p = .098, η2p = .07; see Table 4]. The effect was of medium size. There were no significant covariate × group interaction effects for any of the parenting behavior dimensions, including Low Monitoring, Inconsistency, Corporal Punishment, Powerful Enforcement, and Responsible Parenting Behavior (p = .184–.822). This indicates that the effects of parenting behavior on the mother-child relationship were independent of group status.
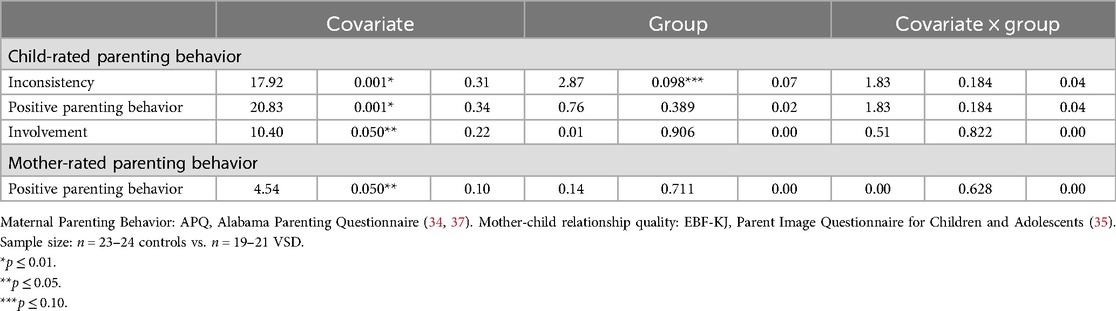
Table 4. Mean group differences (VSD vs. controls) in child-rated mother-child relationship quality at t2 (adolescence, total score) under consideration of parenting behavior dimensions at t2 (covariates) in separate ANCOVAs (F, p, η2p).
Post hoc power analyses
Post hoc power analyses for ANCOVAs with a sample size of n = 45 and an α error probability of 0.05 revealed observed effect sizes in the range of 0.07 < η2p < 0.31 statistically relevant effects with a statistical power (1 – β) of 0.44–0.99.
Discussion
Our study aimed to determine potential differences in parenting behaviors and the mother-child-relationship between mother-child-dyads with VSD-affected children in comparison to a non-affected control group.
Stability and change of maternal parenting behavior in children with early surgical VSD repair and controls
Inconsistency
Our results showed that, in both groups, mother-rated Inconsistency remained stable from t1 to t2. Moreover, maternal inconsistency scores in our sample varied on a medium level, indicating a stable level of inconsistent discipline strategies in both groups from primary school to adolescence. Other studies investigating the effects of inconsistent parenting behavior on child development also found that inconsistent parental behavior towards children remained stable over time (40, 41). Research on personality traits may provide a possible explanation for the stability of inconsistent parental behavior over time: According to this, inconsistent behavior is associated with emotion dysregulation, especially in parent-child interactions, as found in individuals with certain personality traits, such as a more neurotic personality (42, 43). Personality traits are thought to be stable, especially in adulthood (44). Thus, certain personality traits may be related to more inconsistent parental behavior and may explain the stability of this behavior and should be included in future studies.
Positive parenting behavior
Furthermore, maternal Positive Parenting Behavior remained stable from child primary-school age through adolescence in both groups. Regardless of group, all mothers reported themselves as highly emotionally warm and supportive in interaction with their children. Also, previous research has reported on the stability of positive, sensitive, and supportive parenting behaviors (45–47). Our data suggest that a high level of Positive Parenting Behavior appears to be relevant throughout the developmental period from primary school age to (early) adolescence. Other studies also emphasize the important role of parental warmth and sensitivity for child development, both in normal and at-risk samples such as children with surgically repaired VSDs (7–9, 17, 18).
Involvement and monitoring
Both, maternal Involvement and Monitoring decreased (or rather the values in Low Monitoring increased) from child primary-school age to adolescence. A possible explanation is that both parenting behavior dimensions are based on child's age as well as developmental status and tasks. Whereas Involvement reflects parenting behavior of active support in child development and is represented in participating in child activities, Monitoring describes the parent's knowledge and information about the child's activities and social contacts. In child adolescence, mothers might gradually reduce their Involvement and Monitoring as adolescents become increasingly independent and strive for more autonomy. In addition, children in primary school age allow their parents to be more involved in their own lives than they do when children become adolescents (48). A decrease in parental Involvement and Monitoring with increasing age appears to be important for adolescents’ development (49, 50). The developmental task of autonomy in adolescence is underlined once again by findings that show that continued or even increased Involvement during adolescence has a counterproductive effect on adolescent well-being (51). Our findings of a decrease in maternal Involvement and Monitoring in both groups show that the detachment process in adolescents who underwent surgical VSD repair is age-appropriate and develops normally compared to non-affected controls.
Corporal punishment
Our results also showed a significant decrease in Corporal Punishment from child primary school age to adolescence from the mothers’ perspective. Overall and in both groups, mothers reported very low levels of Corporal Punishment at t1 and t2, meaning that mothers in this sample reported rarely using behaviors such as shaking, hitting, or grabbing to discipline their child; and that low use of Corporal Punishment decreased to an even lower level from t1 to t2. Looking at the results in a developmental context, age could be an explanation for the decrease in Corporal Punishment. Adolescents have grown in physical strength and size compared to children in primary school age, so mothers may find less Corporal Punishment appropriate during discussions. Another possible explanation could be that rates of Corporal Punishment are higher in (early) childhood than in adolescence (52) because parents might feel it is a more appropriate discipline strategy at younger child age than later in adolescence (53).
Powerful enforcement
Powerful Enforcement reflects parenting behavior of a more authoritarian parenting style (49) as it includes overreactive behavior and strict implementation of family rules in combination with an emotionally negative atmosphere in the family. For this parenting behavior dimension, we found a significant interaction between group and time. Our results suggest that Powerful Enforcement differs over time from the perspective of the mothers of children who underwent early pediatric cardiac surgery compared to the mothers of the non-affected control group. However, the pairwise comparisons of t1 and t2 in the VSD and control group were not significant. A possible explanation for this result could be the slightly modified test variables used in the ANOVA and post hoc analysis. The ANOVA tests whether the interaction between groups and Powerful Enforcement is significantly different from zero over time, while the post hoc analyses test whether the differences between the factors are significantly different from zero. Because the null hypotheses of the two analyses are different, the interaction and post hoc analyses may yield different results. One explanation for the non-significant pairwise comparisons could be the different sample sizes of the respective groups. Thus, we interpreted maternal Powerful Enforcement as rather comparable in both groups.
Responsible parenting behavior
Parents with high scores on Responsible Parenting Behavior describe themselves as highly proactive in child rearing, have a conscious educational attitude, and discuss free time activities with their children. In group comparisons, we found maternal Responsible Parenting Behavior to decrease over time only in the non-affected control group. In contrast, it was stable in the VSD group from child primary school age to adolescence. At least two possible explanations seem plausible. On the one hand, the age difference of almost one year between the two groups could explain the difference. Since children in the control group were already about one year older than children in the VSD group, the step towards emotional detachment from the family and home may have already taken place, and the parents may already be giving the adolescents more autonomy. On the other hand, mothers of children who underwent early pediatric cardiac surgery might want to be closer to their children based on potential remaining concerns for the child's physical health. In line with this thought, studies have shown higher levels of overprotectiveness and vigilance among mothers of children who underwent early pediatric cardiac surgery (54, 55). In contrast, mothers with typically developing children might go through the natural detachment process in adolescence which is also reflected in our data by a decrease in Responsive Parenting Behavior only in the control group.
In summary, our results indicate that mostly, mothers of children who underwent early pediatric cardiac surgery show comparable and as much adequate parenting behavior as mothers of non-affected controls. The only significant difference between the groups was in Responsible Parenting Behaviors during child adolescence. Therefore, the question remains as to why no group differences could be found in the present study regarding the remaining parenting behaviors recorded. Maternal adaptation in the group of heart-operated children could be a possible explanation: Despite difficulties in early childhood education and interaction (16, 33), mothers of heart-operated children seem to be able to educate their children during the primary-school years into early adolescence in the same way as mothers in the non-affected control group. This finding is consistent with previous studies reporting no difference in parenting between mothers with heart-operated children and non-affected children (54), as well as an improvement in the quality of life of parents of children with congenital heart defects with increasing time (56). It is possible that improved quality of life could be an indicator of parents’ development of adaptive capacity about their child's health status. In contrast, Involvement, Low Monitoring, and Corporal Punishment decreased from primary school age to early adolescence in both groups. The results of changing parenting behaviors are consistent with developmental psychological findings that assume higher aspirational autonomy in adolescents as they age (51). An adjustment in parenting behaviors may already occur in early adolescence and the pursuit of autonomy may also be of great importance in early adolescence. Inconsistency and Positive Parenting Behavior were found to be stable parenting practices. This could be attributed to parenting attitudes and personality structures (45–47).
In addition, only Responsible Parenting Behaviors in adolescents were found to differ between VSD and non-affected groups, whereas the other parenting behavior dimensions did not differ between groups. Overall, the existing literature showed less engagement of parents of children with cardiac surgery in early childhood (33, 47, 57); these studies focused on different congenital heart defects and not exclusively on isolated VSD. Another study found increased parent burden and reduced maternal engagement in interactions with their children, particularly after the time of diagnosis of the congenital heart defect and the child's cardiac surgery (15). In previously published data of the present study at child primary school age, mothers of children who underwent early pediatric cardiac surgery showed an increased physiological stress response (12), suggesting that mothers of children who have undergone early pediatric cardiac surgery are particularly vulnerable (9). Additionally, parental stress is positively associated with the severity of the child's heart defect (58). In turn, high levels of psychosocial stress may have a negative impact on parenting behavior (17). However, at child primary school age and in adolescence, the present study could hardly find differences in parenting behaviors in mothers of children with a surgically repaired isolated VSD compared to non-affected controls, so the risk factor of cardiac surgery due to an isolated VSD does not seem to play a role in parenting behaviors, for at least several years after the pediatric cardiac surgery. In line with this thought, previous findings of our sample showed that affected mothers were well adapted regarding psychological and neurobiological stress levels, especially during adolescence, and thus probably had sufficient resources to engage in appropriate parenting behaviors (9). Even after parental stress experiences around the child's pediatric cardiac surgery in early childhood have occurred, there could be an adjustment in parenting behavior accompanied by an improvement in parental quality of life (56). Nevertheless, our results are not transferable to other or even more severe CHD, so that support for affected families through appropriate interventions may be necessary. Especially in the period before and after the child's heart surgery psychological support for parents might be crucial, in order to promote positive parenting behaviors and a secure caregiver-child attachments to enable a favourable developmental outcome for the affected child.
Mother-child relationship in the VSD-group compared to non-affected controls and influence of maternal parenting behavior
Influence of parenting behavior from a mother's perspective
In both groups, a high level of mother-reported Positive Parenting Behavior at t2 was associated with a more positive mother-child relationship quality. The finding suggests that, in general, mothers can contribute to a better child-reported relationship quality through parenting behaviors like emotional warmth as well as friendly, child-centered interactions. In line with this, adolescent-reported maternal Positive Parenting Behavior was also associated with higher mother-child relationship quality. Our results are consistent with previous research reporting on positive relations between Positive Parenting Behavior and mother-child relationship (55).
Overall, from the mother's perspective, only Positive Parenting Behavior and no other parenting behavior dimensions were related to child-rated mother-child relationship quality. This could be due to the discrepancy between self-report and third-party reports regarding parenting behavior dimensions. Discrepancies between self-reports and third-party reports - also about parenting behavior and relationship quality - are also reported in other studies [e.g., (59)]. Another explanation could be that self-report questionnaires are not effective in capturing one's behavior because of biases such as social desirability (37), again fostering discrepancies between self- and third-party reports.
Currently, there are limited studies on parenting behavior and the mother-child relationship in families with children who underwent early pediatric cardiac surgery. Most of these studies are limited to early childhood (60, 61). This study aims to contribute to the still unclear research field of the unique relationship between parents and children with cardiac surgery in later childhood and early adolescence. However, there are still some unclear aspects regarding parenting behavior and the mother-child relationship in children and adolescents who underwent early pediatric cardiac surgery. Therefore, further research is necessary.
Additionally, the presented results have practical implications for support services aimed at parents and children who underwent early pediatric cardiac surgery. Previous studies have demonstrated the significance of information and support services provided by professionals for affected families, particularly during early childhood, to promote the development of a healthy parent-child relationship and positive parenting behavior (33). Furthermore, the available results suggest that mothers of children who underwent early pediatric cardiac surgery may have difficulties granting them complete autonomy, especially in late adolescence. Therefore, counseling services for parents of affected children could be beneficial.
Influence of adolescent-reported parenting behavior
In summary, the results indicate a close relation between adolescents’ perceptions of parenting behavior and mother-child relationship quality. From the adolescents’ perspective, Positive Parenting Behavior, Parental Involvement, and low Inconsistency in parenting behavior were needed for high mother-child relationship quality. This appears to be true for all adolescents, as the self-reported relationship quality of the heart-operated adolescents was comparable to that of the non-affected control group. Adolescents of the VSD-group even reported their mothers show more Positive Parenting Behavior, which might be explained by potential remaining concerns for the child's physical health as described earlier.
In contrast, studies focusing on the mother-child relationship in CHD-affected samples in early childhood reported a less secure attachment and unstable relationship between parent and heart-operated child (33, 57). In addition, previous research found increased stress levels and anxiety in parents of heart-operated children in early childhood (21). It is possible that authoritative parenting behavior – often reflected in high parental sensitivity - represents a protective factor against the influence of risks on child development (7, 17, 18) and favors the development of a positive mother-child relationship in adolescence. Moreover, high mother-child relationship quality in the EBF-KJ is characterized by dimensions such as emotional attachment, identification with parents, autonomy, and low levels of negative parenting behaviors such as punishment or rejection, so the association between relationship quality and Positive Parenting Behaviors seems plausible in terms of attachment theory and parenting behavior research (62).
Overall, our findings suggest that adolescents who underwent early cardiac surgery had a relationship quality with their mothers that was as good as that of non-affected adolescents. The descriptive data even showed slightly higher mother-child relationship quality ratings in the VSD-group compared to controls, but this difference did not reach statistical significance. A possible explanation could be the age difference between the VSD and control group at t2: The non-affected adolescents were about one year older than adolescents in the VSD-group, and descriptively reported more conflicts with their parents. One reason for this may be the more advanced stage of puberty compared to the one-year younger adolescents who underwent early pediatric cardiac surgery.
Strengths and limitations
When examining parenting behavior, using both the mother's and child's perspectives provided an advantage in mitigating potential biases. However, the limited sample size restricts the generalizability of the findings. Although the sample size was small, it was possible to form a homogeneous group of children with early surgically corrected VSD and to compare their development to a non-affected, matched control group. Nonetheless, it was difficult to statistically detect actual differences between this group and the control group. In addition, the data collected are based solely on questionnaire data and thus only on the subjective views of the children and their mothers, taking into account social desirability bias. However, questionnaires are a very economical way of recording parenting behavior and relationship quality. In future studies, it would be valuable to include multi-informative approaches to examine differences and changes in parenting behavior and mother-child relationship quality. This could involve gathering information from other individuals close to the child, such as teachers or relatives. In addition, utilizing more objective measurement methods, such as behavioral observations and standardized interviews or interactional tasks would be beneficial.
Moreover, the present study did not examine the father's perspective. However, few studies found differences in maternal and paternal stress responses facing a child with chronic disease (63, 64). For this reason, and from a family systemic perspective, future studies should include fathers in their analyses to uncover potential differences in parenting of children undergoing early pediatric cardiac surgery.
Another issue to discuss is the small sample size. Consequently, the results and statistical power were limited. This was accepted in favor of the benefits and the intention of the project. With this in mind, the results should be interpreted with caution and larger sample sizes should be aimed for in the future.
Conclusion
Mothers of children with early surgically corrected VSD showed comparable parenting behaviors to mothers of non-affected children. A favorable influence of Positive Parenting Behavior on the mother-child relationship can be assumed. In addition, from the affected adolescent's perspective, the quality of the relationship between mother and child seems to develop comparably to non-affected adolescents. The absence of a decrease in maternal Responsible Parenting Behavior in the VSD group may indicate challenges during the developmental task of autonomy in adolescence. Nevertheless, our findings suggest that an adaptive family functioning after early pediatric surgical VSD repair is possible.
Data availability statement
The raw data supporting the conclusions of this article will be made available upon reasonable request by the corresponding author. The data are not publicly available due to privacy restrictions and the data protection law in Germany.
Ethics statement
The studies involving humans were approved by Ethics Committee of the Erlangen University Hospital, Friedrich-Alexander-Universität Erlangen-Nürnberg. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants’ legal guardians/next of kin.
Author contributions
JH: Investigation, Formal Analysis, Writing – original draft. SM: Writing – original draft, Investigation, Formal Analysis. HN: Writing – review & editing, Software, Investigation, Formal Analysis, Data curation. AP: Writing – review & editing, Validation, Methodology, Conceptualization. RC: Writing – review & editing, Validation, Supervision, Resources, Methodology, Conceptualization. OK: Writing – review & editing, Supervision, Resources, Methodology, Funding acquisition, Conceptualization. AE: Writing – review & editing, Visualization, Validation, Supervision, Project administration, Methodology, Funding acquisition, Formal Analysis, Data curation, Conceptualization. JG: Writing – review & editing, Supervision, Project administration, Investigation, Formal Analysis, Data curation.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This research was funded by the Robert-Enke Foundation, Barsinghausen, Germany, with EUR 41000 provided at t1, and by the German Foundation of Heart Research, Frankfurt am Main, Germany, with EUR 58000 (F/28/19) provided at t2 to AE.
Acknowledgments
We would like to thank all participating children and their mothers for taking part in this study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Liu Y, Chen S, Zühlke L, Babu-Narayan SV, Black GC, Choy MK, et al. Global prevalence of congenital heart disease in school-age children: a meta-analysis and systematic review. BMC Cardiovasc Disord. (2020) 20(1):488. doi: 10.1186/s12872-020-01781-x
2. Spector LG, Menk JS, Knight JH, McCracken C, Thomas AS, Vinocur JM, et al. Trends in long-term mortality after congenital heart surgery. J Am Coll Cardiol. (2018) 71(21):2434–46. doi: 10.1016/j.jacc.2018.03.491
3. Zomer AC, Vaartjes I, Grobbee DE, Mulder BJ. Adult congenital heart disease: new challenges. Int J Cardiol. (2013) 163(2):105–7. doi: 10.1016/j.ijcard.2012.03.035
4. Adan A, Eleyan L, Zaidi M, Ashry A, Dhannapuneni R, Harky A. Ventricular septal defect: diagnosis and treatments in the neonates: a systematic review. Cardiol Young. (2021) 31(5):756–61. doi: 10.1017/S1047951120004576
5. Marino BS, Lipkin PH, Newburger JW, Peacock G, Gerdes M, Gaynor JW, et al. Neurodevelopmental outcomes in children with congenital heart disease: evaluation and management: a scientific statement from the American Heart Association. Circulation. (2012) 126(9):1143–72. doi: 10.1161/CIR.0b013e318265ee8a
6. Patel T, Ilardi D, Kochilas L. Neurodevelopmental outcomes in children with congenital heart disease: ten years after the American Heart Association statement. Clin Perinatol. (2023) 50(1):53–66. doi: 10.1016/j.clp.2022.10.002
7. Eichler A, Köhler-Jonas N, Stonawski V, Purbojo A, Moll GH, Heinrich H, et al. Child neurodevelopment and mental health after surgical ventricular septal defect repair: risk and protective factors. Dev Med Child Neurol. (2019) 61(2):152–60. doi: 10.1111/dmcn.13992
8. Lang L, Gerlach J, Plank AC, Purbojo A, Cesnjevar RA, Kratz O, et al. Becoming a teenager after early surgical ventricular septal defect (VSD) repair: longitudinal biopsychological data on mental health and maternal involvement. J Clin Med. (2022) 11:23. doi: 10.3390/jcm11237242
9. Gerlach J, Decker ES, Plank A-C, Mestermann S, Purbojo A, Cesnjevar RA, et al. Long-term effects of child early surgical ventricular septal defect repair on maternal stress. Children. (2023) 10(12):1832. doi: 10.3390/children10121832
10. Lisanti AJ. Parental stress and resilience in CHD: a new frontier for health disparities research. Cardiol Young. (2018) 28(9):1142–50. doi: 10.1017/S1047951118000963
11. Mangin-Heimos KS, Strube M, Taylor K, Galbraith K, O'Brien E, Rogers C, et al. Trajectories of maternal and paternal psychological distress after fetal diagnosis of moderate-severe congenital heart disease. J Pediatr Psychol. (2023) 48(4):305–16. doi: 10.1093/jpepsy/jsac067
12. Stonawski V, Vollmer L, Köhler-Jonas N, Rohleder N, Golub Y, Purbojo A, et al. Long-term associations of an early corrected ventricular septal defect and stress systems of child and mother at primary school age. Front Pediatr. (2018) 5:293. doi: 10.3389/fped.2017.00293
13. Clancy T, Jordan B, de Weerth C, Muscara F. Early emotional, behavioural and social development of infants and young children with congenital heart disease: a systematic review. J Clin Psychol Med Settings. (2020) 27(4):686–703. doi: 10.1007/s10880-019-09651-1
14. Jackson AC, Frydenberg E, Liang RP, Higgins RO, Murphy BM. Familial impact and coping with child heart disease: a systematic review. Pediatr Cardiol. (2015) 36(4):695–712. doi: 10.1007/s00246-015-1121-9
15. Franich-Ray C, Bright MA, Anderson V, Northam E, Cochrane A, Menahem S, et al. Trauma reactions in mothers and fathers after their infant’s cardiac surgery. J Pediatr Psychol. (2013) 38(5):494–505. doi: 10.1093/jpepsy/jst015
16. Lawoko S, Soares JJF. Distress and hopelessness among parents of children with congenital heart disease, parents of children with other diseases, and parents of healthy children. J Psychosom Res. (2002) 52(4):193–208. doi: 10.1016/S0022-3999(02)00301-X
17. Gerlach J, Fößel J, Vierhaus M, Sann A, Eickhorst A, Zimmermann P, et al. Family risk and early attachment development: the differential role of parental sensitivity. Infant Ment Health J. (2022) 2(43):340–56. doi: 10.25968/opus-2162
18. Whittaker JEV, Harden BJ, See HM, Meisch AD, Westbrook TPR. Family risks and protective factors: pathways to early head start toddlers’ social–emotional functioning. Early Child Res Q. (2011) 26(1):74–86. doi: 10.1016/j.ecresq.2010.04.007
19. Guan G, Liu H, Wang Y, Han B, Jin Y. Behavioural and emotional outcomes in school-aged children after surgery or transcatheter closure treatment for ventricular septal defect. Cardiol Young. (2014) 24(5):910–7. doi: 10.1017/S104795111300142X
20. Brosig CL, Mussatto K, Kuhn EM, Tweddell JS. Psychosocial outcomes for preschool children and families after surgery for complex congenital heart disease. Pediatr Cardiol. (2007) 28(4):255–62. doi: 10.1007/s00246-006-0013-4
21. Re JM, Dean S, Mullaert J, Guedeney A, Menahem S. Maternal distress and infant social withdrawal (ADBB) following infant cardiac surgery for congenital heart disease. World J Pediatr Congenit Heart Surg. (2018) 9(6):624–37. doi: 10.1177/2150135118788788
22. Jaschinski C, Knetsch V, Parzer P, Meyr J, Schroeder B, Fonseca E, et al. Psychosocial impact of congenital heart diseases on patients and their families: a parent’s perspective. World J Pediatr Congenit Heart Surg. (2022) 13(1):9–15. doi: 10.1177/21501351211044127
23. Rattaz V, Puglisi N, Tissot H, Favez N. Associations between parent-infant interactions, cortisol and vagal regulation in infants, and socioemotional outcomes: a systematic review. Infant Behav Dev. (2022) 67:101687. doi: 10.1016/j.infbeh.2022.101687
24. Roberts SD, Kazazian V, Ford MK, Marini D, Miller SP, Chau V, et al. The association between parent stress, coping and mental health, and neurodevelopmental outcomes of infants with congenital heart disease. Clin Neuropsychol. (2021) 35(5):948–72. doi: 10.1080/13854046.2021.1896037
25. Kolaitis GA, Meentken MG, Utens E. Mental health problems in parents of children with congenital heart disease. Front Pediatr. (2017) 5:102. doi: 10.3389/fped.2017.00102
26. Tesson S, Butow PN, Marshall K, Fonagy P, Kasparian NA. Parent-child bonding and attachment during pregnancy and early childhood following congenital heart disease diagnosis. Health Psychol Rev. (2022) 16(3):378–411. doi: 10.1080/17437199.2021.1927136
27. McWhorter LG, Christofferson J, Neely T, Hildenbrand AK, Alderfer MA, Randall A, et al. Parental post-traumatic stress, overprotective parenting, and emotional and behavioural problems for children with critical congenital heart disease. Cardiol Young. (2022) 32(5):738–45. doi: 10.1017/s1047951121002912
28. Soulvie MA, Desai PP, White CP, Sullivan BN. Psychological distress experienced by parents of young children with congenital heart defects: a comprehensive review of literature. J Soc Serv Res. (2012) 38(4):484–502. doi: 10.1080/01488376.2012.696410
29. Woolf-King SE, Anger A, Arnold EA, Weiss SJ, Teitel D. Mental health among parents of children with critical congenital heart defects: a systematic review. J Am Heart Assoc. (2017) 6(2):e004862. doi: 10.1161/jaha.116.004862
30. Wray J, Cassedy A, Ernst MM, Franklin RC, Brown K, Marino BS. Psychosocial functioning of parents of children with heart disease—describing the landscape. Eur J Pediatr. (2018) 177(12):1811–21. doi: 10.1007/s00431-018-3250-7
31. Franck LS, McQuillan A, Wray J, Grocott MPW, Goldman A. Parent stress levels during children’s hospital recovery after congenital heart surgery. Pediatr Cardiol. (2010) 31(7):961–8. doi: 10.1007/s00246-010-9726-5
32. Lawoko S, Soares JJ. Psychosocial morbidity among parents of children with congenital heart disease: a prospective longitudinal study. Heart Lung. (2006) 35(5):301–14. doi: 10.1016/j.hrtlng.2006.01.004
33. Biber S, Andonian C, Beckmann J, Ewert P, Freilinger S, Nagdyman N, et al. Current research status on the psychological situation of parents of children with congenital heart disease. Cardiovasc Diagn Ther. (2019) 9(Suppl 2):S369–76. doi: 10.21037/cdt.2019.07.07
34. Shelton KK, Frick PJ, Wootton J. Assessment of parenting practices in families of elementary school-age children. J Clin Child Psychol. (1996) 25(3):317–29. doi: 10.1207/s15374424jccp2503_8
35. Titze K, Wiefel A, Assheuer J, Biermann M, Führer D, Riezler B, et al. Der elternbildfragebogen für kinder- und jugendliche (EBF-KJ). Diagnostica. (2010) 56(2):68–81. doi: 10.1026/0012-1924/a000002
36. Roetner J, Van Doren J, Maschke J, Kulke L, Pontones C, Fasching PA, et al. Effects of prenatal alcohol exposition on cognitive outcomes in childhood and youth: a longitudinal analysis based on meconium ethyl glucuronide. Eur Arch Psychiatry Clin Neurosci. (2024) 274(2):343–52. doi: 10.1007/s00406-023-01657-z
37. Reichle B, Franiek S. Self-reported parenting style—german extended version of the Alabama parenting questionnaire for elementary school age children. Z Entwicklungspsychol Paedagog Psychol. (2009) 41:12–25. doi: 10.1026/0049-8637.41.1.12
38. Titze K, Lehmkuhl U. EBF-KJ. Elternbildfragebogen für Kinder und Jugendliche. Manual [Parent Image Questionnaire for Children and Adolescents. Manual). Göttingen: Hogrefe (2010).
39. Cohen J. Statistical Power Analysis for the Behavioral Sciences. Hillsdale, New Jersey: Erlbaum (1988).
40. Carrasco MÁ, Holgado-Tello FP, RodrÍguez Serrano MÁ. Intraparental inconsistency: the influence of parenting behaviors on aggression and depression in children. Fam Relat. (2015) 64(5):621–34. doi: 10.1111/fare.12168
41. Dwairy M. Parental inconsistency: a third cross-cultural research on parenting and psychological adjustment of children. J Child Fam Stud. (2010) 19(1):23–9. doi: 10.1007/s10826-009-9339-x
42. Fingerman KL, Chen P-C, Hay E, Cichy KE, Lefkowitz ES. Ambivalent reactions in the parent and offspring relationship. J Gerontol B. (2006) 61(3):P152–60. doi: 10.1093/geronb/61.3.P152
43. Kokkonen M, Pulkkinen L. Extraversion and neuroticism as antecedents of emotion regulation and dysregulation in adulthood. Eur J Pers. (2001) 15(6):407–24. doi: 10.1002/per.425
44. Costa PT, McCrae RR. Personality in adulthood: a six-year longitudinal study of self-reports and spouse ratings on the NEO personality inventory. J Pers Soc Psychol. (1988) 54(5):853–63. doi: 10.1037/0022-3514.54.5.853
45. Dallaire DH, Weinraub M. The stability of parenting behaviors over the first 6 years of life. Early Child Res Q. (2005) 20(2):201–19. doi: 10.1016/j.ecresq.2005.04.008
46. Forehand R, Jones DJ. The stability of parenting: a longitudinal analysis of inner-city African-American mothers. J Child Fam Stud. (2002) 11(4):455–67. doi: 10.1023/A:1020935525335
47. Loeber R, Drinkwater M, Yin Y, Anderson SJ, Schmidt LC, Crawford A. Stability of family interaction from ages 6 to 18. J Abnorm Child Psychol. (2000) 28(4):353–69. doi: 10.1023/A:1005169026208
48. Stattin H, Kerr M. Parental monitoring: a reinterpretation. Child Dev. (2000) 71(4):1072–85. doi: 10.1111/1467-8624.00210
49. Baumrind D. Effective parenting during the early adolescent transition. In: Cowan PA, Hetherington EM, editors. Family Transitions. Hillsdale, NJ, US: Lawrence Erlbaum Associates, Inc. (1991). p. 111–63.
50. Pettit GS, Laird RD. Psychological control and monitoring in early adolescence: the role of parental involvement and earlier child adjustment. In: Barber BK, editor. Intrusive Parenting: How Psychological Control Affects Children and Adolescents. Washington, DC: American Psychological Association (2002). p. 97–123. doi: 10.1037/10422-004
51. LeMoyne T, Buchanan T. Does “hovering” matter? Helicopter parenting and its effect on well-being. Sociol Spectr. (2011) 31(4):399–418. doi: 10.1080/02732173.2011.574038
52. Mahoney A, Donnelly WO, Lewis T, Maynard C. Mother and father self-reports of corporal punishment and severe physical aggression toward clinic-referred youth. J Clin Child Psychol. (2000) 29(2):266–81. doi: 10.1207/S15374424jccp2902_12
53. Gershoff ET. Corporal punishment by parents and associated child behaviors and experiences: a meta-analytic and theoretical review. Psychol Bull. (2002) 128(4):539–79. doi: 10.1037/0033-2909.128.4.539
54. Carey LK, Nicholson BC, Fox RA. Maternal factors related to parenting young children with congenital heart disease. J Pediatr Nurs. (2002) 17(3):174–83. doi: 10.1053/jpdn.2002.124111
55. Pinquart M. Do the parent-child relationship and parenting behaviors differ between families with a child with and without chronic illness? A meta-analysis. J Pediatr Psychol. (2013) 38(7):708–21. doi: 10.1093/jpepsy/jst020
56. Gregory MRB, Prouhet PM, Russell CL, Pfannenstiel BR. Quality of life for parents of children with congenital heart defect: a systematic review. J Cardiovasc Nurs. (2018) 33(4):363–71. doi: 10.1097/JCN.0000000000000466
57. Goldberg S, Morris P, Simmons RJ, Fowler RS, Levison H. Chronic illness in infancy and parenting stress: a comparison of three groups of parents. J Pediatr Psychol. (1990) 15(3):347–58. doi: 10.1093/jpepsy/15.3.347
58. O'Connor AM, Cassedy A, Wray J, Brown KL, Cohen M, Franklin RCG, et al. Differences in quality of life in children across the Spectrum of congenital heart disease. J Pediatr. (2023):113701. doi: 10.1016/j.jpeds.2023.113701
59. Hendriks AM, Van der Giessen D, Stams G, Overbeek G. The association between parent-reported and observed parenting: a multi-level meta-analysis. Psychol Assess. (2018) 30(5):621–33. doi: 10.1037/pas0000500
60. Lumsden MR, Smith DM, Wittkowski A. Coping in parents of children with congenital heart disease: a systematic review and meta-synthesis. J Child Fam Stud. (2019) 28(7):1736–53. doi: 10.1007/s10826-019-01406-8
61. Nayeri ND, Roddehghan Z, Mahmoodi F, Mahmoodi P. Being parent of a child with congenital heart disease, what does it mean? A qualitative research. BMC Psychol. (2021) 9(1):33. doi: 10.1186/s40359-021-00539-0
62. Ainsworth MDS. Attachment as related to mother-infant interaction. In: Rosenblatt JS, Hinde RA, Beer C, Busnel M-C, editors. Advances in the Study of Behavior. Vol. 9. New York: Academic Press (1979). p. 1–51. doi: 10.1016/S0065-3454(08)60032-7
63. Darke PR, Goldberg S. Father-infant interaction and parent stress with healthy and medically compromised infants. Infant Behavior and Development. (1994) 17(1):3–14. doi: 10.1016/0163-6383(94)90017-5
Keywords: congenital heart disease, ventricular septal defect, pediatric cardiac surgery, mother, mother-child relationship, parenting behavior, longitudinal study
Citation: Hemetsberger J, Mestermann S, Nicol H, Purbojo A, Cesnjevar RA, Kratz O, Eichler A and Gerlach J (2024) The impact of early surgical ventricular septal defect repair on parenting behavior and mother-child relationship: a prospective longitudinal study. Front. Pediatr. 12:1455310. doi: 10.3389/fped.2024.1455310
Received: 26 June 2024; Accepted: 9 October 2024;
Published: 23 October 2024.
Edited by:
Nazmi Narin, Izmir Katip Celebi University, TürkiyeReviewed by:
Nicole Sekarski, Centre Hospitalier Universitaire Vaudois (CHUV), SwitzerlandFirat Kardelen, Akdeniz University Hospital, Türkiye
Copyright: © 2024 Hemetsberger, Mestermann, Nicol, Purbojo, Cesnjevar, Kratz, Eichler and Gerlach. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jennifer Gerlach, amVubmlmZXIuZ2VybGFjaEB1ay1lcmxhbmdlbi5kZQ==
†These authors share first authorship
‡ORCID:
Ariawan Purbojo
orcid.org/0000-0002-5242-2630
Robert A. Cesnjevar
orcid.org/0000-0002-3575-6647
Oliver Kratz
orcid.org/0009-0004-7334-950X
Anna Eichler
orcid.org/0000-0001-5584-0961
Jennifer Gerlach
orcid.org/0000-0001-8439-1528
 Jonas Hemetsberger
Jonas Hemetsberger Stefan Mestermann1,†
Stefan Mestermann1,† Ariawan Purbojo
Ariawan Purbojo Oliver Kratz
Oliver Kratz Anna Eichler
Anna Eichler Jennifer Gerlach
Jennifer Gerlach