
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Pediatr. , 18 September 2024
Sec. Pediatric Orthopedics
Volume 12 - 2024 | https://doi.org/10.3389/fped.2024.1443447
Introduction: Although pes planus, a common deformity in children with cerebral palsy (CP), is predominantly treated through lateral column lengthening (LCL), subtalar arthroereisis (SA) has also gained popularity for this purpose. This systematic review was conducted to compare surgical outcomes between LCL and SA for pes planovalgus in children with CP.
Methods: PubMed, EMBASE, Cochrane Library, and Google Scholar were comprehensively searched for relevant articles reporting the outcomes of LCL and SA in the target population. Surgical outcomes were evaluated in terms of radiographic parameters and postoperative complications.
Results: This review included 22 studies involving patients undergoing LCL (LCL group) and 9 studies involving those undergoing SA (SA group). LCL outperformed SA in terms of corrections in the talonavicular coverage angle (8.1°–42.1° vs. 8.0°–30.7°), anteroposterior talo–first metatarsal angle (12.3°–33.7° vs. 9.8°–21.4°), and calcaneal pitch angle (2.5°–29.7° vs. 3.5°–8.0°). Furthermore, the risk of postoperative complications, such as recurrence, pain, undercorrection, and overcorrection, was higher in the LCL group than in the SA group. However, the risks of reoperation and implant-related problems were higher in the SA group than in the LCL group. A meta-analysis of two randomized studies revealed that improvement in calcaneal pitch angle was significantly greater in the LCL group than in the SA group (mean difference: 2.09°; P = 0.0488).
Conclusion: LCL outperforms SA in correcting pes planus–related radiographic parameters in patients with CP. However, postoperative complications appear to be more common after LCL than after SA.
Systematic Review Registration: https://inplasy.com/inplasy-2024-5-0126, Identifier 202450126.
Cerebral palsy (CP) is a neurological disorder that affects movement and posture, often leading to musculoskeletal deformities. Pes planovalgus, a common foot deformity in children with CP, is characterized by hindfoot valgus and longitudinal arch flattening, which can compromise gait and overall function (1). Surgical intervention is indicated when pain and dysfunction persist despite conservative treatment.
Several surgical methods are used to treat pes planovalgus (2). Although lateral column lengthening (LCL) is the predominant surgical option (2), subtalar arthroereisis (SA) has gained popularity because of its advantages, such as a low extent of invasiveness, reduced level of postoperative edema, early initiation of weight-bearing, short duration of hospitalization, and feasibility of associated soft tissue and bony procedures (3).
In a systematic review comparing clinical outcomes between LCL and SA for pediatric pes planovalgus, patients undergoing LCL achieved greater radiographic corrections and higher American Orthopaedic Foot and Ankle Society scores than did those undergoing SA. However, postoperative complications were more common after LCL than after SA (4). To the best of our knowledge, no systematic review has compared clinical outcomes between LCL and SA for pes planovalgus in children with CP. Although most studies on this topic have reported the outcomes of LCL and SA without any comparison, data synthesis can still provide valuable insights for surgeons. Therefore, this systematic review and meta-analysis was conducted to compare surgical outcomes—radiographic correction and postoperative complications—between LCL and SA for pes planovalgus in children with CP. For studies with a comparative design, a meta-analysis was also conducted.
This systematic review and meta-analysis was conducted following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines. The protocol for this review was registered in the International Platform of Registered Systematic Review and Meta-analysis Protocols (registration number: 202450126).
Relevant articles were identified by systematically searching PubMed, EMBASE, Cochrane Library, and Google Scholar on January 17, 2024 by using free-text and Medical Subject Headings terms. The following terms were used for literature search: [(“flatfoot” OR “flatfeet” OR “pes planovalgus” OR “pes planus”) AND “cerebral palsy”] AND (“arthroereisis” OR “Evans osteotomy” OR “calcaneal lengthening osteotomy” OR “lateral column lengthening”).
Two reviewers independently selected studies for inclusion in this systematic review. We included studies that reported the clinical outcomes of LCL or SA in children with CP and pes planovalgus. Protocols, case reports, reviews, comments, letters, and conference articles were excluded from the analysis. Publication date and language were not limited.
Two reviewers independently extracted the following data from the included studies: name of the first author; year of publication; level of evidence; type of surgery (LCL or SA); sample size, age, and sex of patients; duration of follow-up; outcomes of interest; flexibility of the feet; ambulatory status; Gross Motor Function Classification System (GMFCS) levels; and concomitant procedures. Surgical outcomes of interest were evaluated in terms of radiographic parameters and postoperative complications. The following radiographic parameters were assessed: talonavicular coverage, anteroposterior talo–first metatarsal, lateral talo–first metatarsal, anteroposterior talocalcaneal, lateral talocalcaneal, calcaneal pitch, and talo–horizontal angles. The following postoperative complications were assessed: recurrence, reoperation, postoperative pain, implant dislocation, implant fracture, implant-related problems, infection, temporary supination, undercorrection, overcorrection, neurovascular damage, fracture of the distal part of the calcaneus, calcaneocuboid joint subluxation, donor site morbidity, graft malposition, nonunion, and delayed union.
Two reviewers independently assessed the risk of bias in the included studies by using the methodological index for non-randomized studies tool (MINORS) for non-randomized studies and the Version 2 of the Cochrane risk-of-bias tool for randomized trials (RoB 2) (5, 6). Disagreements between the reviewers were resolved through discussion with a third reviewer until consensus was reached.
For continuous variables, we extracted mean and standard deviation values and calculated mean differences for between-group comparisons. For categorical variables, we extracted frequency and percentage values and calculated odds ratios for between-group comparisons. The included studies were divided into comparative studies and all studies. For comparative studies, a meta-analysis was performed using RevMan (version 5.4). Heterogeneity among the included studies was examined using the I2 statistic; a fixed-effects model was used when no significant heterogeneity was observed (I2 < 50%). Forest plots were generated to present the results of each study and the pooled effects of all included studies. The pooled effects were analyzed using the z-test. During the pooling of data from all included studies, the outcomes of interest were presented separately for LCL and SA.
Initially, the literature search returned 844 articles. After the removal of duplicates, 787 articles remained. After the application of the inclusion and exclusion criteria, 2 RCTs and 27 non-randomised studies (NRS) were assessed for eligibility. Among these 29 studies, 2 RCTs and 20 NRSs reported the outcomes of LCL, 2 RCTs and 7 NRSs reported the outcomes of SA, and 2 RCTs compared outcomes between LCL and SA (Figure 1).
The characteristics of the included studies are presented in Table 1. In the 29 studies, patients' mean or median age ranged from 6 to 12.1 years. The minimum follow-up duration was <12 months in 3 studies, 12–24 months in 12 studies, and ≥24 months in 14 studies. Radiographic parameters were reported in 25 studies, recurrence was reported in 11 studies with a follow-up duration of ≥12 months, and postoperative complications were reported in 24 studies. Flexibility of the feet was reported in 13 studies, and all of the feet were flexible. Ambulatory status or GMFCS levels were reported in 25 studies, and most patients were ambulatory (Table 2). Concomitant procedures are presented in Table 3. The most common concomitant procedures were Achilles lengthening and gastrocnemius recession or lengthening. The next most common procedures were peroneus brevis and longus lengthening, which were performed in both groups. The scores of MINORS are presented in Table 4. The median scores were 12.5 for LCL-focused studies (range: 6–17) and 13 for SA-focused studies (range: 7–14), indicating that LCL-focused studies and SA-focused studies were similar in terms of quality. The RoB 2 based bias risk assessment table for RCTs are presented in Table 5.
A total of 19 studies (905 feet) reported improvements in radiographic measurements for LCL and 8 (334 feet) for SA. Table 6 presents the range of mean values of seven radiographic parameters in patients undergoing LCL (LCL group) and those undergoing SA (SA group). The LCL group achieved greater corrections in the talonavicular coverage, anteroposterior talo–first metatarsal, and calcaneal pitch angles than did the SA group. In the meta-analysis of two RCTs (Figure 2) (7, 8), the pooled results revealed no significant between-group difference in improvement in the talonavicular coverage, anteroposterior talo–first metatarsal, lateral talo–first metatarsal, anteroposterior talocalcaneal, or lateral talocalcaneal angle. However, the improvement in the calcaneal pitch angle was significantly greater in the LCL group than in the SA group (mean difference: 2.09°; P = 0.0488).
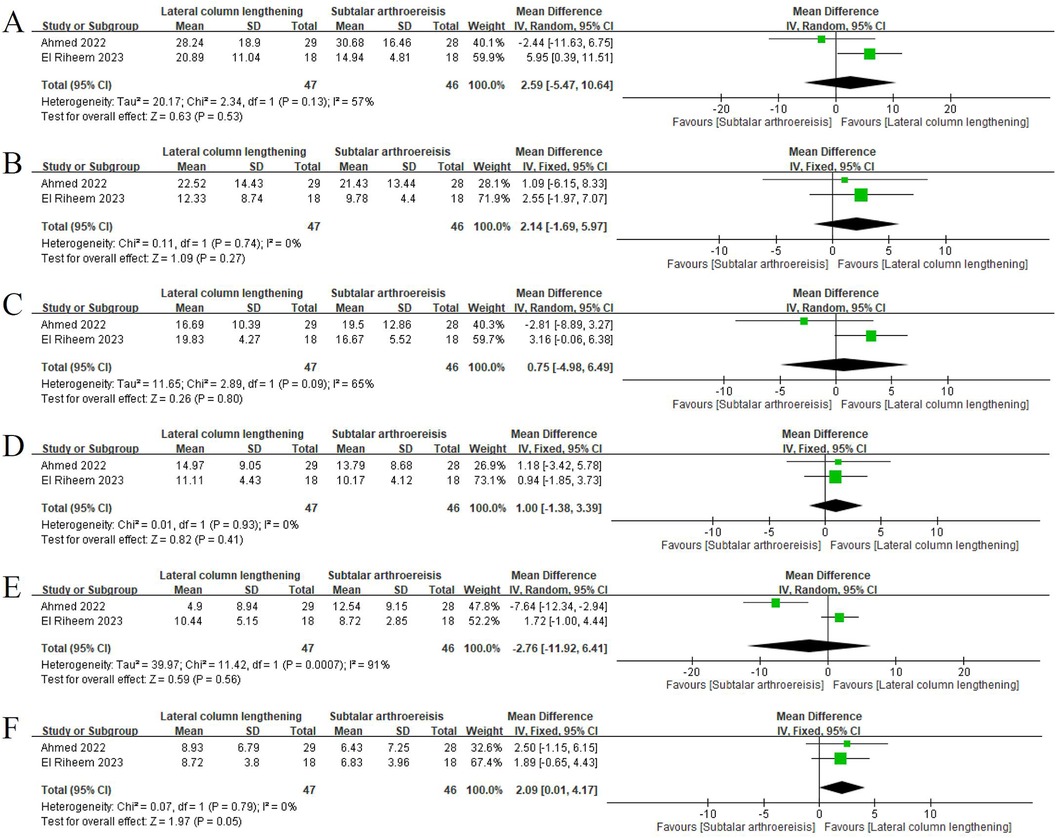
Figure 2. Forest plot for comparison between lateral column lengthening and subtalar arthroereisis. Improvements in the (A) talonavicular coverage, (B) anteroposterior talo–first metatarsal, (C) lateral talo–first metatarsal, (D) anteroposterior talocalcaneal, (E) lateral talocalcaneal, and (F) calcaneal pitch angles.
The rate of each postoperative complication was pooled (Table 7) from 19 LCL-focused studies (804 feet) and 7 SA-focused studies (324 feet). The LCL group had considerably higher risks of recurrence, postoperative pain, undercorrection, and overcorrection than did the SA group. By contrast, the SA group had substantially higher risks of reoperation and implant-related problems than did the LCL group. In the LCL group, the rates of neurovascular damage, fracture of the distal part of the calcaneus, calcaneocuboid joint subluxation, calcaneocuboid joint arthrosis, donor site morbidity, graft malposition, nonunion, and delayed union were 0.6% (1/160), 0% (0/50), 6.3% (27/431), 1.2% (1/83), 0% (0/50), 0% (0/129), 0.9% (4/451), and 0.7% (2/276), respectively. A meta-analysis of two RCTs (7, 8) revealed no significant difference in the incidence of pain, infection, and undercorrection between the LCL and SA groups (Figure 3).
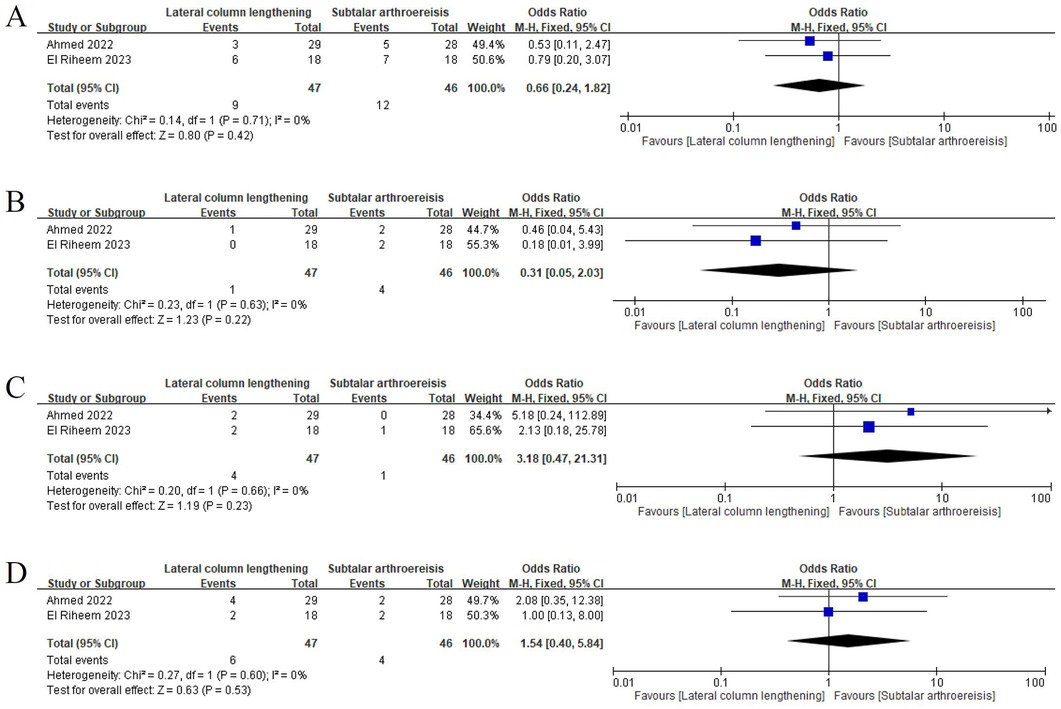
Figure 3. Forest plot for comparison between lateral column lengthening and subtalar arthroereisis. Incidence of pain (A) within the first 6 months after surgery and (B) 6 months after surgery. Incidence of (C) infection and (D) undercorrection.
To the best of our knowledge, this review included the largest number of studies reporting the outcomes of LCL and SA for pes planovalgus in children with CP. Data from these studies were pooled and analyzed to provide comprehensive information on radiographic parameters and postoperative complication risks.
Most of the included studies focused on LCL. Over the years, SA has gained popularity because of its advantages, such as a low extent of invasiveness and early initiation of weight-bearing. A systematic review of studies on pediatric pes planovalgus reported that LCL outperformed SA in terms of radiographic corrections in the anteroposterior talo–first metatarsal angle (9.5°–21.7° vs. 10.6°–12.8°) and calcaneal pitch angle (2.1°–26.53° vs. −1.3°–3.23°) (4). Our review revealed similar results, with LCL outperforming SA in correcting the anteroposterior talo–first metatarsal, talonavicular coverage, and calcaneal pitch angles, likely because LCL involves adjusting the skeletal structure of the foot. However, our meta-analysis of two comparative studies indicated a significant between-procedure difference in the mean value of the calcaneal pitch angle. The inconsistency in our findings is likely attributable to the limited number of studies available for meta-analysis and the substantial heterogeneity observed in the talonavicular coverage, lateral talo–first metatarsal, and lateral talocalcaneal angles. While treating pes planovalgus in patients with cerebral palsy, performing single-event multilevel surgery according to the symptoms is common. Therefore, although concomitant procedures are associated with outcomes, conducting subgroup analysis is challenging because previous studies did not separately report outcomes for patients undergoing different combinations of procedures.
In the systematic review of studies on pediatric pes planovalgus, postoperative complications were more common after LCL than after SA (0%–86.9% vs. 3.5%–45%). However, the rate of reoperation was similar between the LCL and SA groups (0%–27.3% vs. 0%–36.4%) (4). We did not pooled data to calculate an overall rate of postoperative complications because the definitions of these complications varied across the included studies. The rate of postoperative complications may appear higher in studies presenting more comprehensive information on these complications. Therefore, we pooled data separately for each complication.
When comparing LCL and SA, we focused on complications reported for both LCL and SA. The risks of recurrence, postoperative pain, undercorrection, and overcorrection were substantially higher in the LCL group than in the SA group. By contrast, the risk of reoperation were higher in the SA group than in the LCL group. The elevated risk of recurrence in the LCL group may be associated with additional procedures for soft tissue, graft, and fixation. The increased incidence of postoperative pain after LCL may be attributable to its the relatively invasive nature of LCL. Undercorrection in LCL can result from inadequate intraoperative lateral column lengthening or subsequent loss of correction due to graft resorption. Premature weight-bearing, inappropriate graft composition, and insufficient fixation may also contribute to undercorrection. The increased risk of overcorrection in LCL may be associated with the sequence of medializing calcaneal osteotomy and LCL. Performing the medializing calcaneal osteotomy first can lead to overcorrection of the hindfoot deformity because of additional hindfoot inversion due to LCL (36). In the subtalar arthroereisis studies we included, detailed reports on implant-related problems were provided, but other complications, such as recurrence and undercorrection, were not necessarily mentioned. Therefore, potential bias may exist due to the insufficient information, which will require the inclusion of more SA studies to address this issue.
Patients with GMFCS levels III/IV had higher risks for undercorrection following LCL than those with GMFCS levels I/II in AP talus-first metatarsal angle and lateral talus-first metatarsal angle (15). A better satisfaction rate following LCL was also reported in patients with GMFCS levels II than those with GMFCS levels III/IV (20). Based on these results, for patients with GMFCS level III/IV, additional procedures should be considered when performing LCL. The subgroup analysis for GMFCS levels was not performed in this study because most of the included studies reported outcomes without stratifying by GMFCS levels and ambulatory status. Therefore, it is not possible to assess the association between GMFCS levels and outcomes in this study.
Among the 22 studies on LCL, only 6 reported the use of staples, screws, and plates for fixating bone grafts. However, implant-related problems were clearly reported in only one of these studies. The exact number of cases involving fixation was not reported clearly. Hence, we could not determine a reliable incidence of implant-related problems after LCL involving the use of implants. Further studies are needed to verify whether implants should be used in LCL to fixate bone grafts.
The rate of reoperation was higher in the SA group than in the LCL group. Among the included studies, only that of Molayem et al. reported the rate of reoperation after SA; the causes of reoperation were implant dislocation or fracture (35). The rate of implant-related problems was higher in the study of Molayem et al. (29.6%) than in those of Aleksandrov et al. (2.3%) and Silva et al. (10.5%) (32, 34, 35). Molayem et al. indicated that the high rate of implant-related problems was associated with performing SA without Achilles tendon lengthening to balance muscle forces around the joint (35).
Pooled results from our meta-analysis of two comparative studies revealed no significant difference between LCL and SA in the incidence of pain, infection, or undercorrection. The inconsistency in findings related to pain and undercorrection may be attributable to the limited number of studies available for meta-analysis. Moreover, not all included studies provided adequate information for distinguishing postoperative complications, thereby limiting the number of cases available for data synthesis. However, by exclusively including cases with clearly reported information on postoperative complications, we minimized the risk of overestimating or underestimating the rate of each complication.
Our study has several limitations. First, most of the included studies were case-series studies, because using a comparative design or performing randomization for the between-procedure comparison of clinical outcomes in the target population is a challenging task. Therefore, only limited data could be included in the meta-analysis. Moreover, although a comparative design was used in several studies, their objective was not to compare outcomes between LCL and SA, resulting in differences in outcomes of interest. This is particularly evident in SA studies, which tend to focus more on reporting implant-related outcomes than other parameters. Therefore, when comparing LCL and SA, there may be bias due to the insufficient information of included studies. Second, for some outcomes of interest, the sample size was small because of the lack of uniformity in the outcomes reported in the included studies. Third, although some studies have longer follow-up periods and maximum follow-up time points, they did not reported outcomes separately based on the length of the follow-up time. Therefore, we can only use the minimum follow-up time as the cutoff point to present the results. However, 2 years is a relatively short time for follow-up in CP patients. Finally, we could not perform subgroup analysis by potential confounding factors such as flexibility of the feet, GMFSC levels, ambulatory status, additional procedures, LCL site, graft types for LCL, and implant types for SA. The wide intra- and interstudy variations in these factors resulted in insufficient information for the separate evaluation of outcomes. In summary, our meta-analysis included studies of limited quality. Thus, caution should be exercised when interpreting our results. Although we included studies with relatively low levels of evidence, our pooled results provide valuable insights with clinical relevance.
In conclusion, in the treatment of pes planovalgus in children with CP, LCL may outperform SA group in terms of corrections in the talonavicular coverage, anteroposterior talo–first metatarsal, and calcaneal pitch angles. However, LCL is associated with increased risks of recurrence, postoperative pain, undercorrection, and overcorrection. By contrast, SA is associated with an elevated risk of reoperation, likely because of implant-related problems. These comparisons of complications are based on a limited number of SA studies.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
C-HL: Data curation, Formal Analysis, Methodology, Writing – original draft. C-HC: Conceptualization, Data curation, Writing – review & editing. S-HY: Methodology, Writing – review & editing.
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Sees JP, Miller F. Overview of foot deformity management in children with cerebral palsy. J Child Orthop. (2013) 7(5):373–7. doi: 10.1007/s11832-013-0509-4
2. MacInnes P, Lewis TL, Griffin C, Martinuzzi M, Shepherd KL, Kokkinakis M. Surgical management of pes planus in children with cerebral palsy: a systematic review. J Child Orthop. (2022) 16(5):333–46. doi: 10.1177/18632521221112496
3. Bernasconi A, Lintz F, Sadile F. The role of arthroereisis of the subtalar joint for flatfoot in children and adults. EFORT Open Rev. (2017) 2(11):438–46. doi: 10.1302/2058-5241.2.170009
4. Suh DH, Park JH, Lee SH, Kim HJ, Park YH, Jang WY, et al. Lateral column lengthening versus subtalar arthroereisis for paediatric flatfeet: a systematic review. Int Orthop. (2019) 43(5):1179–92. doi: 10.1007/s00264-019-04303-3
5. Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J. Methodological Index for non-randomized studies (minors): development and validation of a new instrument. ANZ J Surg. (2003) 73(9):712–6. doi: 10.1046/j.1445-2197.2003.02748.x
6. Sterne JAC, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I, et al. Rob 2: a revised tool for assessing risk of bias in randomised trials. BMJ. (2019) 366:l4898. doi: 10.1136/bmj.l4898
7. Riheem YMA E, El-Barbary HM, Hegazy MM, Arafa AS. Comparative study between arthroereisis versus calcaneal lengthening in planovulgus foot in cerebral palsy children. J Pharma Negat Results. (2023) 14:51–9. doi: 10.47750/pnr.2023.14.S02.09
8. Ahmed AH, Hanna AA, Arafa AS, El-Sherbini MH, Omran AA. Prospective comparison of subtalar arthroereisis with calcaneal lengthening in the management of planovalgus feet of ambulatory children with spastic cerebral palsy? Foot Ankle Spec. (2022) 15(6):515–27. doi: 10.1177/1938640020974886
9. Erdal OA, Görgün B, Sarıkaya İA, Şeker A, Incesu M, İnan M. Treatment of planovalgus foot in cerebral palsy with lateral column lengthening using titanium cubic cage. Med Sci. (2022) 11(1):274–9. doi: 10.5455/medscience.2021.11.382
10. Rethlefsen SA, Hanson AM, Wren TAL, Kay RM. Calcaneal sliding osteotomy versus calcaneal lengthening osteotomy for valgus foot deformity correction in children with cerebral palsy. J Pediatr Orthop. (2021) 41(6):e433–8. doi: 10.1097/bpo.0000000000001790.
11. Narang A, Sud A, Chouhan D. Calcaneal lengthening osteotomy in spastic planovalgus feet. J Clin Orthop Trauma. (2021) 13:30–9. doi: 10.1016/j.jcot.2020.08.024
12. Aboelenein AM, Fahmy ML, Elbarbary HM, Mohamed AZ, Galal S. Calcaneal lengthening for the pes planovalgus foot deformity in children with cerebral palsy. J Clin Orthop Trauma. (2020) 11(2):245–50. doi: 10.1016/j.jcot.2018.07.021
13. El-Hilaly R, El-Sherbini MH, Abd-Ella MM, Omran AA. Radiological outcome of calcaneo-cuboid-cuneiform osteotomies for planovalgus feet in cerebral palsy children: relationship with pedobarography. Foot Ankle Surg. (2019) 25(4):462–8. doi: 10.1016/j.fas.2018.02.019
14. Aly AS, Abdel Rahman AF, Mahmoud S. Double calcaneal osteotomy in treatment of flexible planovalgus foot deformity in ambulatory cerebral palsy. A case series study. Foot Ankle Surg. (2019) 25(5):640–5. doi: 10.1016/j.fas.2018.07.003
15. Cho BC, Lee IH, Chung CY, Sung KH, Lee KM, Kwon SS, et al. Undercorrection of planovalgus deformity after calcaneal lengthening in patients with cerebral palsy. J Pediatr Orthop B. (2018) 27(3):206–13. doi: 10.1097/bpb.0000000000000436
16. Rhodes J, Mansour A, Frickman A, Pritchard B, Flynn K, Pan Z, et al. Comparison of allograft and bovine xenograft in calcaneal lengthening osteotomy for flatfoot deformity in cerebral palsy. J Pediatr Orthop. (2017) 37(3):e202–8. doi: 10.1097/bpo.0000000000000822
17. Luo CA, Kao HK, Lee WC, Yang WE, Chang CH. Limits of calcaneal lengthening for treating planovalgus foot deformity in children with cerebral palsy. Foot Ankle Int. (2017) 38(8):863–9. doi: 10.1177/1071100717702596
18. Kadhim M, Holmes L Jr., Miller F. Long-Term outcome of planovalgus foot surgical correction in children with cerebral palsy. J Foot Ankle Surg. (2013) 52(6):697–703. doi: 10.1053/j.jfas.2013.06.010
19. Sung KH, Chung CY, Lee KM, Lee SY, Park MS. Calcaneal lengthening for planovalgus foot deformity in patients with cerebral palsy. Clin Orthop Relat Res. (2013) 471(5):1682–90. doi: 10.1007/s11999-012-2709-5
20. Huang CN, Wu KW, Huang SC, Kuo KN, Wang TM. Medial column stabilization improves the early result of calcaneal lengthening in children with cerebral palsy. J Pediatr Orthop B. (2013) 22(3):233–9. doi: 10.1097/BPB.0b013e32835f1ede
21. Kadhim M, Holmes L Jr., Church C, Henley J, Miller F. Pes planovalgus deformity surgical correction in ambulatory children with cerebral palsy. J Child Orthop. (2012) 6(3):217–27. doi: 10.1007/s11832-012-0413-3
22. Adams SB J, Simpson AW, Pugh LI, Stasikelis PJ. Calcaneocuboid joint subluxation after calcaneal lengthening for planovalgus foot deformity in children with cerebral palsy. J Pediatr Orthop. (2009) 29(2):170–4. doi: 10.1097/BPO.0b013e3181982c33
23. Ettl V, Wollmerstedt N, Kirschner S, Morrison R, Pasold E, Raab P. Calcaneal lengthening for planovalgus deformity in children with cerebral palsy. Foot Ankle Int. (2009) 30(5):398–404. doi: 10.3113/fai-2009-0398
24. Park KB, Park HW, Lee KS, Joo SY, Kim HW. Changes in dynamic foot pressure after surgical treatment of valgus deformity of the hindfoot in cerebral palsy. J Bone Joint Surg Am. (2008) 90(8):1712–21. doi: 10.2106/jbjs.G.00792
25. Zeifang F, Breusch SJ, Döderlein L. Evans calcaneal lengthening procedure for spastic flexible flatfoot in 32 patients (46 feet) with a followup of 3–9 years. Foot Ankle Int. (2006) 27(7):500–7. doi: 10.1177/107110070602700704
26. Noritake K, Yoshihashi Y, Miyata T. Calcaneal lengthening for planovalgus foot deformity in children with spastic cerebral palsy. J Pediatr Orthop B. (2005) 14(4):274–9. doi: 10.1097/01202412-200507000-00008
27. Yoo WJ, Chung CY, Choi IH, Cho TJ, Kim DH. Calcaneal lengthening for the planovalgus foot deformity in children with cerebral palsy. J Pediatr Orthop. (2005) 25(6):781–5. doi: 10.1097/01.bpo.0000184650.26852.37
28. Andreacchio A, Orellana CA, Miller F, Bowen TR. Lateral column lengthening as treatment for planovalgus foot deformity in ambulatory children with spastic cerebral palsy. J Pediatr Orthop. (2000) 20(4):501–5.10912608
29. Danilov OA, Gorelik VV, Shulga OV. Analysis of the effectiveness of methods of correction of pronation deformities of the feet in children with cerebral palsy. Paediatr Surg Ukr. (2023) 2(79):50–7. doi: 10.15574/PS.2023.79.50
30. Elbarbary HM, Arafa AS, Said ABZ, Hegazy M, Reiad MW, Basha NY, et al. Clinical and radiological outcomes of subtalar arthroereisis for management of planovalgus foot in children with cerebral palsy: 3-year follow-up. Foot Ankle Spec. (2022) 15(6):536–44. doi: 10.1177/1938640020980911
31. Kubo H, Krauspe R, Hufeland M, Lipp C, Ruppert M, Westhoff B, et al. Radiological outcome after treatment of juvenile flatfeet with subtalar arthroereisis: a matched pair analysis of 38 cases comparing neurogenic and non-neurogenic patients. J Child Orthop. (2019) 13(4):346–52. doi: 10.1302/1863-2548.13.190046
32. Aleksandrov SA, Syundyukov AR, Yakovleva SK. X-ray evaluation of surgical treatment of the feet by using subtalar implants in patients with cerebral palsy. PTORS. (2018) 6(4):20–6. doi: 10.17816/ptors6420-26
33. Wen J, Liu H, Xiao S, Li X, Fang K, Zeng M, et al. Comparison of mid-term efficacy of spastic flatfoot in ambulant children with cerebral palsy by 2 different methods. Medicine (Baltimore). (2017) 96(22):e7044. doi: 10.1097/md.0000000000007044
34. Silva L, Fucs P. Surgical treatment of planovalgus foot in cerebral palsy by Pisani’s arthroereisis. Acta Ortop Bras. (2010) 18:162–5. doi: 10.1590/S1413-78522010000300009
35. Molayem I, Persiani P, Marcovici LL, Rost S, Calistri A, Villani C. Complications following correction of the planovalgus foot in cerebral palsy by arthroereisis. Acta Orthop Belg. (2009) 75(3):374–9.19681325
Keywords: cerebral palsy, flatfoot, pes planovalgus, lateral column lengthening, subtalar arthroereisis
Citation: Lin C-H, Chen C-H and Yao S-H (2024) Lateral column lengthening versus subtalar arthroereisis for pes planovalgus in patients with cerebral palsy: a systematic review and meta-analysis. Front. Pediatr. 12:1443447. doi: 10.3389/fped.2024.1443447
Received: 4 June 2024; Accepted: 6 September 2024;
Published: 18 September 2024.
Edited by:
Danilo Leonetti, University of Messina, ItalyReviewed by:
Soroush Baghdadi, Children's Hospital of Philadelphia, United StatesCopyright: © 2024 Lin, Chen and Yao. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Chun-Ho Chen, YmFjcml2QGdtYWlsLmNvbQ==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.