
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
CASE REPORT article
Front. Pediatr. , 13 June 2024
Sec. Pediatric Rheumatology
Volume 12 - 2024 | https://doi.org/10.3389/fped.2024.1391229
 Liping Wang1
Liping Wang1 Yingying Jin1
Yingying Jin1 Hua Huang1
Hua Huang1 Zhen Yang1
Zhen Yang1 Fei Ding1
Fei Ding1 Xuemei Xu1
Xuemei Xu1 Chenxi Liu1
Chenxi Liu1 Shengfang Bao1
Shengfang Bao1 Xiqiong Han1
Xiqiong Han1 Jing Ma2
Jing Ma2 Yanliang Jin1*†
Yanliang Jin1*† Haiqing Cai3*†
Haiqing Cai3*†
Rice body synovitis (RBS) is a rare disease, especially in children. Rheumatoid disorders and tuberculosis are the first two reasons for the formation of the RB. The diagnosis is mainly based on imaging and histopathological features. Herein, we report three cases of RBS in children diagnosed with congenital synovial chondromatosis, tuberculosis (unconfirmed), and ANA -positive juvenile idiopathic arthritis. Clinical features, radiographic findings, pathophysiology, treatment process, and prognosis were reviewed and documented meticulously to enhance cognition in this population and provide some references for clinicians in diagnosing and treating the disease.
The rice body (RB) is a rice-like body with a hyaline chondroid appearance and is mainly found in the synovial fluid of joints and extra-articular tissues. Hyperplasia of the synoviocytes and thickening of the subintimal layer is the predominant pathological condition in the chronic phase (1). Inflammatory cells, nodular granulomas harboring multinucleated giant cells and capillary hyperplasia and telangiectasia can be found in the subintimal layer with the disease development. RB synovitis (RBS) was first reported by Riese in 1895; the microscopic characteristics of RBS in tuberculous arthritis were described in detail (2). RBS is an unusual lesion; data on its incidence is lacking to date. Notably, the development of RBS in adults is well known; however, it is possibly overlooked and rarely reported in children. In 1979, Wynne-Roberts described the first pediatric case of RB formation in rheumatoid arthritis (3). In his classic study, he reported the microscopic appearance of the cells in the matrix of RBS. Druschel reported two cases of children younger than three years of age with multiple RBS in the knee joint (4). RBS are always found in joints or joint-associated bursas as an accompanying manifestation of some systemic diseases. In addition to tuberculosis and rheumatoid diseases, many other diseases are associated with RBS. Identification of additional synovitis diseases is necessary before diagnosis so that patients can be treated based on etiology. In the present study, we summarize the clinical similarities and differences of RBS between three pediatric cases with different causes, including congenital synovial chondromatosis, unconfirmed tuberculosis, and ANA-positive juvenile idiopathic arthritis (JIA). We hope that these documents can enhance understanding and provide a reference for the diagnosis and treatment of RBS in children.
Here, we report RBS in three pediatric cases, whose clinical details are presented in Table 1. All the patients visited our hospital due to persistent swelling and pain in the knee joint. In Case 1, a 6-year-old girl complained of right knee swelling and pain for one month. Case 2 involved a 7-year-old boy with a three-year history of repeated and aggravated left knee swelling and pain. In Case 3, a 2-year-old girl presented with a two-month history of swelling and pain in the right knee. They had no history of recurrent or persistent fever, rash, fatigue, losing weight, and other symptoms of the three patients. And they had no significant past medical history and family history.
We detected some common clinical features in all three cases. On physical examination, the affected joint showed swelling, tenderness, and heat. However, joint function and range of motion were normal. Each case underwent imaging examinations, including ultrasound and digital radiography and magnetic resonance imaging (MRI) of the affected knee joint. Figure 1 displayed MRI finding of affected joint which significantly suggestive of arthro-synovitis. After a multidisciplinary treatment, the patients were introduced to surgical treatment; a lot of RBS were found in the affected joint (Figure 2). Intraoperative samples were collected and sent for histopathological examination. Figure 3 shows the histopathological findings of the three cases. Hyperplasia of interstitial vasculature and infiltration of inflammatory cells were easily seen microscopically.

Figure 1 Sagittal and axial MRT2 scanning of knee joint of the three RBS cases. Multiple spot-like high-density spots can be visualized around the area.
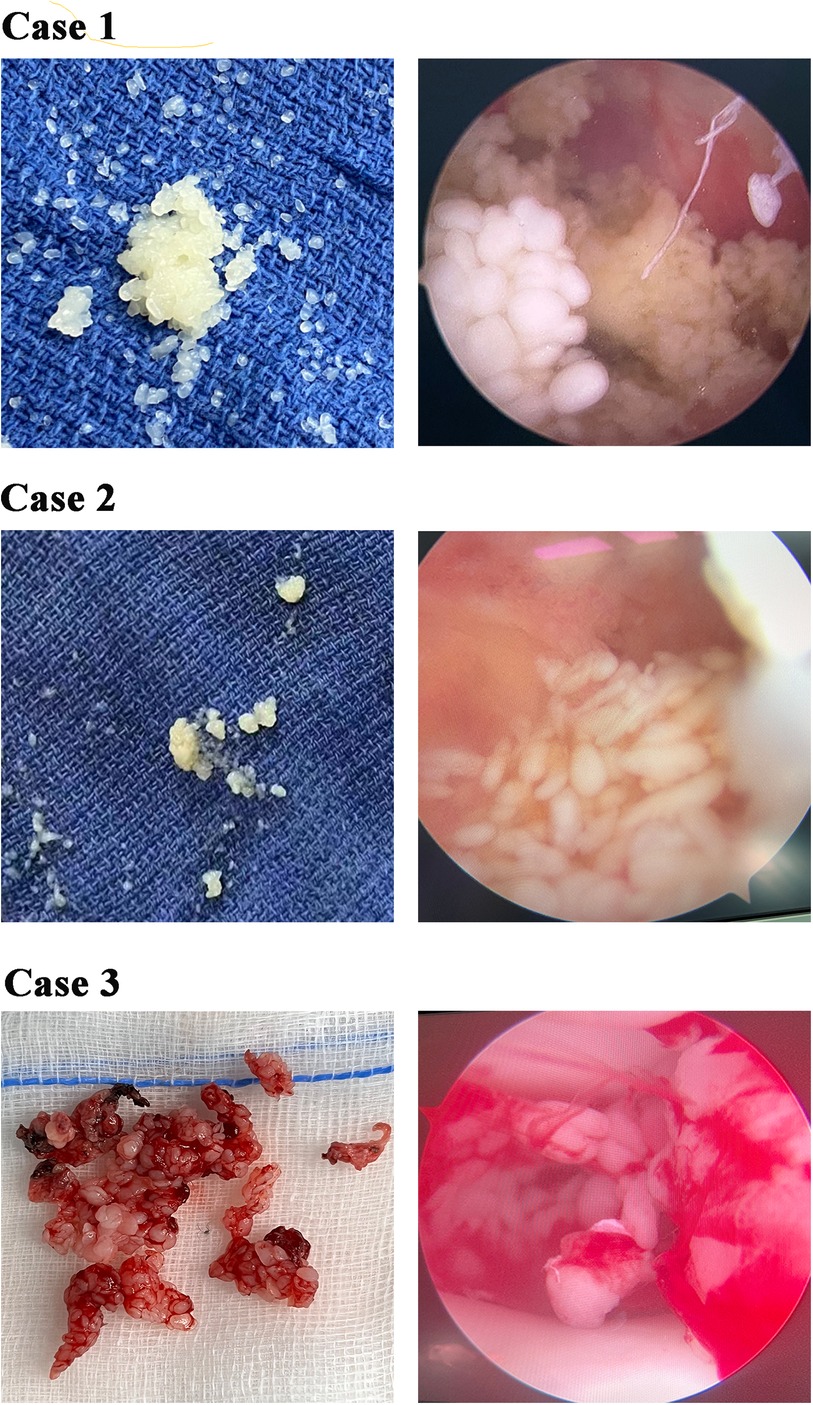
Figure 2 Photograph of multiple rice bodies (RB) that found in the affected knee joint intraoperatively. Left-side figures of every case displayed RB that taken from the affected articular cavity and right-side figures of every case showed the RB form in arthroscopy.
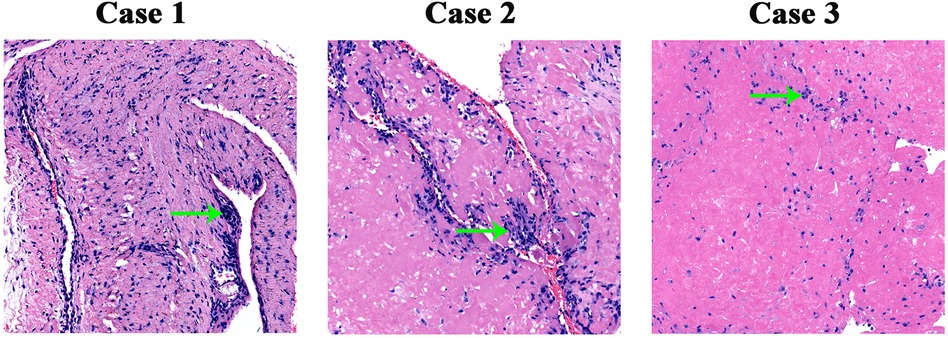
Figure 3 Pathological section of rice body. Every photomicrograph showed the hyperplasia of interstitial vascular and it was infiltrated with inflammatory cells (green arrow), H&E, ×10.
Laboratory tests including blood count, erythrocyte sedimentation rate, C-reactive protein, serum muscle enzyme, liver and renal function, electrolyte, routine urine and stool test, rheumatoid factor, HLA-B27, ANA, ENA, anti-cyclic citrullinated protein antibody, humoral and cell immunity, and pathogens especially the T-SPOT were checked. Case 1 showed a normal laboratory examination. Case 2 showed a positive T-SPOT, while ANA 1:1,000 was positive in Case 3. Other laboratory data were normal both in case 2 and case 3. After excluding other causes, the original causes of the three cases were therefore considered to be congenital synovial osteochondroma (Case 1), suspected tuberculosis (Case 2), and ANA-positive JIA (Case 3). In Case 1, the patient received no treatment after surgery; the joint symptom and sign did not show up after a three-year follow-up. In Case 2, the patient was prescribed INZ and EMB for treating tuberculosis; in Case 3, the patient was administered etanercept and methotrexate for JIA treatment. Further, Cases 2 and 3 showed no relapse after a 6-month follow-up.
Reports have shown that knee and shoulder joints are the most commonly involved sites in RBS. Recurrent pain and swelling of the affected joint are the main complaints, with no limitation in joint motion in most reported cases and the present cases. However, some researchers reported that recurrent and long-term inflammation limited articular activity (5, 6). RBS is an unusual complication of chronic bursitis rather than a disease. Multiple cases were reported in the setting of tuberculosis and rheumatoid arthritis; few cases were correlated with pigmented villonodular synovitis, gout, sarcoidosis, or infection (7–10). We searched relative references with the keywords: “rice body”, “bursitis” and “synovitis” in PubMed, yielding 39 references. Table 2 provides a detailed summary of the relative references, which may help us to better understand this disease. In the present study, we report RBS in three children diagnosed with congenital synovial chondromatosis, tuberculosis (unconfirmed), and ANA-positive JIA.
Considering the same clinical characteristics, the diagnosis and appropriate treatment are always delayed. Thus, blood tests, imaging, and histological examination need to be carried out timely. Ultrasound imaging examination can detect histological microarchitecture of synovial tissues and easily find the rice bodies that floating inside the intra-articular effusion. In clinical practice, it becomes a vital imaging modality in assessing the musculoskeletal systems, especially in pediatrics considering its large availability and the lack of ionizing radiations (11). MRI is the first priority for RBS, which usually shows hypointensity on T1-weighted imaging, hyperintensity on T2-weighted imaging, and iso- or slightly hyperintensity on T1- and T2-weighted imaging when compared to skeletal muscle (12). It appears as a soft tissue mass, debris, blood, or viscous fluid when it is small and resembles ring-enhancing loose bodies when the body is large (13). Some reports indicated that the formation of RB is just an unusual complication of chronic bursitis and is not related to the severity of the imaging findings of arthritis; however, further evidence is needed.
A variety of cells, including phagocytic cells, type C synoviocytes, chondrocytes, and inflammatory cells were found in pathological tissues of RB, which implies that it may have multiple origins, depending on their location. The mechanism of RB formation remains unclear. There are some theories (14–16): microinfarctions after intraarticular synovial inflammation and ischemia; reform and progressive enlargement by fibrin; and alteration in fluid viscosity and fibrinogen content of the synovial fluid. Synovial chondromatosis results from synovial proliferative metaplasia. It rarely evolves into synovial lined bursae and mineralized. The metaplastic cartilage is usually frond like and may produce loose bodies. There are some blue-gray cartilaginous nodules with a diameter of 1–2 cm or larger on the synovial surface of the joint, which can block joint movement in osteochondroma cases. The cartilaginous nodules are composed of synovial connective tissue and are embedded in hyaline chondrocytes under the microscope (5). If a calcified mass is detected in the clinic, the differential diagnosis of synovial chondromatosis, including pigmented villonodular synovitis and tumoral calcinosis due to scleroderma or Sjögren syndrome, must be excluded. Tuberculosis-related RBS is often accompanied by local inflammatory findings, such as local pain, lymphadenitis, and a local progression involving pulmonary tissues, skin, tendons, or bone (17). Caseous necrosis and epithelioid granulomas observed under the microscope are the most helpful findings in diagnosing tuberculosis. Pathological changes in rheumatoid synovitis include regional synovial cell necrosis and erosions covered with cellulose-like deposits. Microscopically, synovial congestion, edema, and infiltration of masses of monocytes, plasma cells, and lymphocytes are easily observed.
There is no consensus when it comes to the therapeutic options of RBS. Either surgery, open arthrotomy, or arthroscopy can be selected to remove RB. However, surgery does not aim for a radical excision and usually cannot prevent recurrence; some patients will relapse after several months or years (7, 18). The RB is a complication of chronic inflammation and other diseases. Thus, strengthening the treatment of the primary disease and enhancing the control of disease activity seem to be more essential and effective in preventing recurrence. However, no standard treatment has been established for RBS. Pharmacotherapy usually depends on the primary disease and its progression. Yamamoto (19) reported that one year of drug therapy after surgery was associated with no relapse in patients with non-tuberculous mycobacterium or fungal infections. Further, the symptoms of the present cases have been controlled over a follow-up period of six months to three years. A further study on which drug should be chosen or how long it should be administered needs to be carried out, considering the adverse drug reactions with long-term therapy. Moreover, a prolonged follow-up is necessary to fully recognize the treatment efficiency and the absence or recurrence of RBS.
In conclusion, we have reported the clinical characteristics of RBS in three pediatric cases with different primary diseases. Some local symptoms and signs, MRI findings, and pathological features are similar. Treating the primary disease is the key to preventing the recurrence of RBS because surgery only removes the already formed RB. The recurrence and prognosis are still unknown; long-term follow-up is necessary. We hope that these findings may provide a reference for physicians to develop better approaches for the diagnosis and treatment of RBS.
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding authors.
The studies involving humans were approved by Local institutional review board and regional research ethics committee of Shanghai Children's Medical Center (SCMC) Affiliated Shanghai Jiao Tong University School of Medicine. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required from the participants or the participants’ legal guardians/next of kin in accordance with the national legislation and institutional requirements. Written informed consent was obtained from the participants’ legal guardians/next of kin for the publication of any potentially identifiable images or data included in this article.
LW: Data curation, Formal Analysis, Writing – original draft. YJ: Resources, Writing – review & editing. HH: Data curation, Writing – review & editing. ZY: Writing – review & editing. FD: Writing – review & editing. XX: Conceptualization, Data curation. Writing – review & editing. CL: Writing – review & editing. SB: Writing – review & editing. XH: Writing – review & editing. JM: Formal Analysis, Resources, Writing – review & editing. YJ: Conceptualization, Resources, Writing – review & editing. HC: Conceptualization, Resources, Writing – review & editing.
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Ricci V, Ricci C, Tamborrini G, Chang KV, Mezian K, Zunica F, et al. From histology to sonography in synovitis: EURO-MUSCULUS/USPRM approach. Pathol Res Pract. (2023) 241:154273. doi: 10.1016/j.prp.2022.15427
2. Riese H. Die reiskörperchen in tuberculös erkrankten synovialsäcken. Deutsch Z Chir. (1895) 42:l–99. doi: 10.1007/BF02800232
3. Wynne-Roberts CR, Cassidy JT. Juvenile rheumatoid arthritis with rice bodies: light and electron microscopic studies. Ann Rheum Dis. (1979) 38:8–13. doi: 10.1136/ard.38.1.8
4. Druschel C, Funk JF, Kallinich T, Lieb A, Placzek RP. Development of rice bodies in 2 children younger than 3 years. J Clin Rheumatol. (2013) 19(1):35–7. doi: 10.1097/RHU.0b013e31826d6b5e
5. Haibo Z, Tianrui W, Wenlian S, Shenjie S, Chunpu L, Xia Z, et al. A case of rice body synovitis of the knee joint. Orthop Surg. (2022) 14(3):628–32. doi: 10.1111/os.13195
6. Cegarra-Escolano M, Jaloux C, Camuzard O. Rice-body formation without rheumatic disease or tuberculosis in a “sausage” ring finger. Hand Surg Rehabi. (2018) S2468–1229(18):30067–7. doi: 10.1016/j.hansur.2018.03.005
7. Fujieda Y, Ninagawa K, Matsui Y, Kono M, Kamishima T, Iwasaki N, et al. Non-tuberculosis mycobacterium tenosynovitis with rice bodies in a patient with systemic lupus erythematosus. Intern Med. (2020) 59(18):2317–20. doi: 10.2169/internalmedicine.4671-2
8. Tian Y, Hu J, Xia Q, Han D. Rice body synovitis in systemic lupus erythematosus. Rheumatol Int. (2023) 26. doi: 10.1007/s00296-023-05426
9. Mohammed Reda F, Talal G, Moncef B, Reda-Allah B, Moulay Omar L, Mohammed Saleh B. Mass of the thenar eminence hiding idiopathic massive rice bodies formation with a compression of the median nerve: case report and review of the literature. Int J Surg Case Rep. (2018) 50:28–31. doi: 10.1016/j.ijscr.2018.07.02
10. Kim DH, Lee JH, Jeong MJ, Kim SH, Kim JY, Kim SH, et al. Intra-articular masses in pediatric idiopathic arthritis: a case report. J Korean Soc Radiol. (2023) 84(3):731–5. (Korean). doi: 10.3348/jksr.2022.012
11. Pirri C, Stecco C, Güvener O, Mezian K, Ricci V, Jačisko J, et al. EURO-MUSCULUS/USPRM dynamic ultrasound protocols for knee. Am J Phys Med Rehabil. (2023) 102(5):e67–72. doi: 10.1097/PHM.0000000000002173
12. Spence LD, Adams J, Gibbons D, Mason MD, Eustace S. Rice body formation in bicipito-radial bursitis: ultrasound, CT, and MRI findings. Skeletal Radiol. (1998) 27(1):30–2. doi: 10.1007/s002560050331
13. Tan CH, Rai SB, Chandy J. MRI appearances of multiple rice body formation in chronic subacromial and subdeltoid bursitis, in association with synovial chondromatosis. Clin Radiol. (2004) 59:753–7. doi: 10.1016/j.crad.2004.03.012
14. Muirhead DE, Johnson EH, Luis C. A light and ultrastructural study of rice bodies recovered from a case of date thorn-induced extra-articular synovitis. Ultrastruct Pathol. (1998) 22(4):341–7. doi: 10.3109/0191312980910335
15. Nagasawa H, Okada K, Senma S, Chida S, Shimada Y. Tenosynovitis with rice body formation in a non-tuberculosis patient: a case report. Ups J Med Sci. (2009) 114(3):184–8. doi: 10.1080/03009730902931408
16. Kim RS, Lee JY, Jung SR, Lee KY. Tuberculous subdeltoid bursitis with rice bodies. Yonsei Med J. (2002) 43:539–42. doi: 10.3349/ymj.2002.43.4.539
17. Mir M A, Ahmad I, Yaseen M. Primary tuberculosis of hand soft tissue. World J Plast Surg. (2016) 5:313–8.27853698
18. Yamamoto D, Tada K, Suganuma S, Ikeda K, Tsuchiya H. Non-tuberculous mycobacterium or fungus induced chronic tenosynovitis with rice body of the hand. J Hand Surg Asian Pac. (2017) 22(3):337–42. doi: 10.1142/S0218810417500393
19. Iyengar K, Manickavasagar T, Nadkarni J, Mansour P, Loh W. Bilateral recurrent wrist flexor tenosynovitis and rice body formation in a patient with sero-negative rheumatoid arthritis: a case report and review of literature. Int J Surg Case Rep. (2011) 2(7):208–11. doi: 10.1016/j.ijscr.2011.07.00
Keywords: rice body, synovitis, children, imaging, histology
Citation: Wang L, Jin Y, Huang H, Yang Z, Ding F, Xu X, Liu C, Bao S, Han X, Ma J, Jin Y and Cai H (2024) Rice body synovitis in pediatrics: three different case reports. Front. Pediatr. 12:1391229. doi: 10.3389/fped.2024.1391229
Received: 19 March 2024; Accepted: 13 May 2024;
Published: 13 June 2024.
Edited by:
Giovanni Filocamo, Fondazione IRCCS Cà Granda Ospedale Maggiore Policlinico, ItalyReviewed by:
Fiammetta Zunica, Vittore Buzzi Children’s Hospital, Italy© 2024 Wang, Jin, Huang, Yang, Ding, Xu, Liu, Bao, Han, Ma, Jin and Cai. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yanliang Jin, amlueWFubGlhbmdAc2NtYy5jb20uY24=; Haiqing Cai, d3pnY2hxQDE2My5jb20=
†These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.