
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Pediatr. , 25 April 2024
Sec. Pediatric Infectious Diseases
Volume 12 - 2024 | https://doi.org/10.3389/fped.2024.1381104
 Sophia Jan1,2,3,4*
Sophia Jan1,2,3,4* Robert Katz1,2,4
Robert Katz1,2,4 David Fagan1,2,4
David Fagan1,2,4 Telmo Santos1,2,4
Telmo Santos1,2,4 Joanna C. Beachy5
Joanna C. Beachy5 Caren Steinway1,2,4
Caren Steinway1,2,4 Jack Chen1,2
Jack Chen1,2 Alina Tsouristakis1,2
Alina Tsouristakis1,2 Briana Mancenido1,2
Briana Mancenido1,2 Christy Leung1,4
Christy Leung1,4 Emily Moore1,2
Emily Moore1,2 Estelle Wilson1,2
Estelle Wilson1,2 Lorna Lin1,2
Lorna Lin1,2 Michael Harte1,2
Michael Harte1,2 Michelle Katzow1,2,3,4
Michelle Katzow1,2,3,4 Lorry G. Rubin1,2,4,6
Lorry G. Rubin1,2,4,6
Introduction: Limited evidence exists on management recommendations for neonates born to SARS-CoV-2-positive mothers. This study looked at transmission risk of neonates presenting for primary care in a large regional health system within New York during the early months of the COVID-19 pandemic.
Methods: This was a prospective, observational study of newborns born to SARS-CoV-2-positive mothers presenting at any of the 19 Northwell Health-Cohen Children's Medical Center primary care practices who underwent another oropharyngeal/nasopharyngeal swab for detection of SARS-CoV-2 by day of life (DOL) 14.
Results: Among 293 newborns born to SARS-CoV-2-positive mothers who were negative at birth, 222 were retested at DOL 14, corresponding to times with different predominant strains. Of these, seven tested positive but had no symptoms.
Conclusion: The overall low transmission rates and absence of symptomatic infection support the safety of direct breastfeeding after hospital discharge with appropriate hand and breast hygiene.
Since the onset of the COVID-19 pandemic, continuous research into the infection of neonates born to SARS-CoV-2-positive mothers has led to updated management recommendations from both the Centers of Disease Control and Prevention and the American Academy of Pediatrics (AAP) (1, 2). While data from recent studies have shown that the highest risk of SARS-CoV-2 infection in neonates occurs when a mother is infected near the time of delivery (3), intrauterine, intrapartum, and peripartum transmission of SARS-CoV-2 from positive mothers is still rare (4–7). Results from these studies showed that the overall prevalence of babies infected immediately after birth was low, less than 3% (4–8), and few confirmed mother-to-child transmission (5–7). The objective of this study was to describe the clinical characteristics and estimate SARS-CoV-2 transmission risk to neonates presenting for primary care in a large regional health system in the New York metropolitan region in the first 5 months of the COVID-19 pandemic in the United States.
All women admitted to labor and delivery across all Northwell Health delivery hospitals were required to undergo a nasopharyngeal swab for detection of SARS-CoV-2 by nucleic acid amplification (NAA) before delivery within 24 h of admission, regardless of maternal symptoms. All mothers positive for SARS-CoV-2 were required to wear surgical masks. Infants born to asymptomatic SARS-CoV-2-positive mothers were allowed skin-to-skin contact, direct breastfeeding, and rooming with their mothers immediately after delivery and throughout the nursery course; those born to symptomatic SARS-CoV-2-positive mothers were not. Symptomatic mothers were encouraged to express breast milk while another person fed their infants. Newborns were tested for SARS-CoV-2 by NAA via a combined oropharyngeal/nasopharyngeal swab by 24 h of life. At discharge, all mothers were encouraged to feed directly at the breast after performing hand and breast hygiene, to continue wearing masks, and were shown how to properly sanitize breast pumps. This education was reinforced at primary care visits.
Study participants included newborns born to SARS-CoV-2-positive mothers presenting at any of the 19 Northwell Health-Cohen Children's Medical Center (CCMC) primary care practices who underwent another oropharyngeal/nasopharyngeal swab for detection of SARS-CoV-2 by day of life (DOL) 14. We collected maternal, newborn, and delivery characteristics, as well as emergency room and hospitalization visits in the first 14 days of life (Table 1). This study was considered exempt by the Northwell Health IRB.
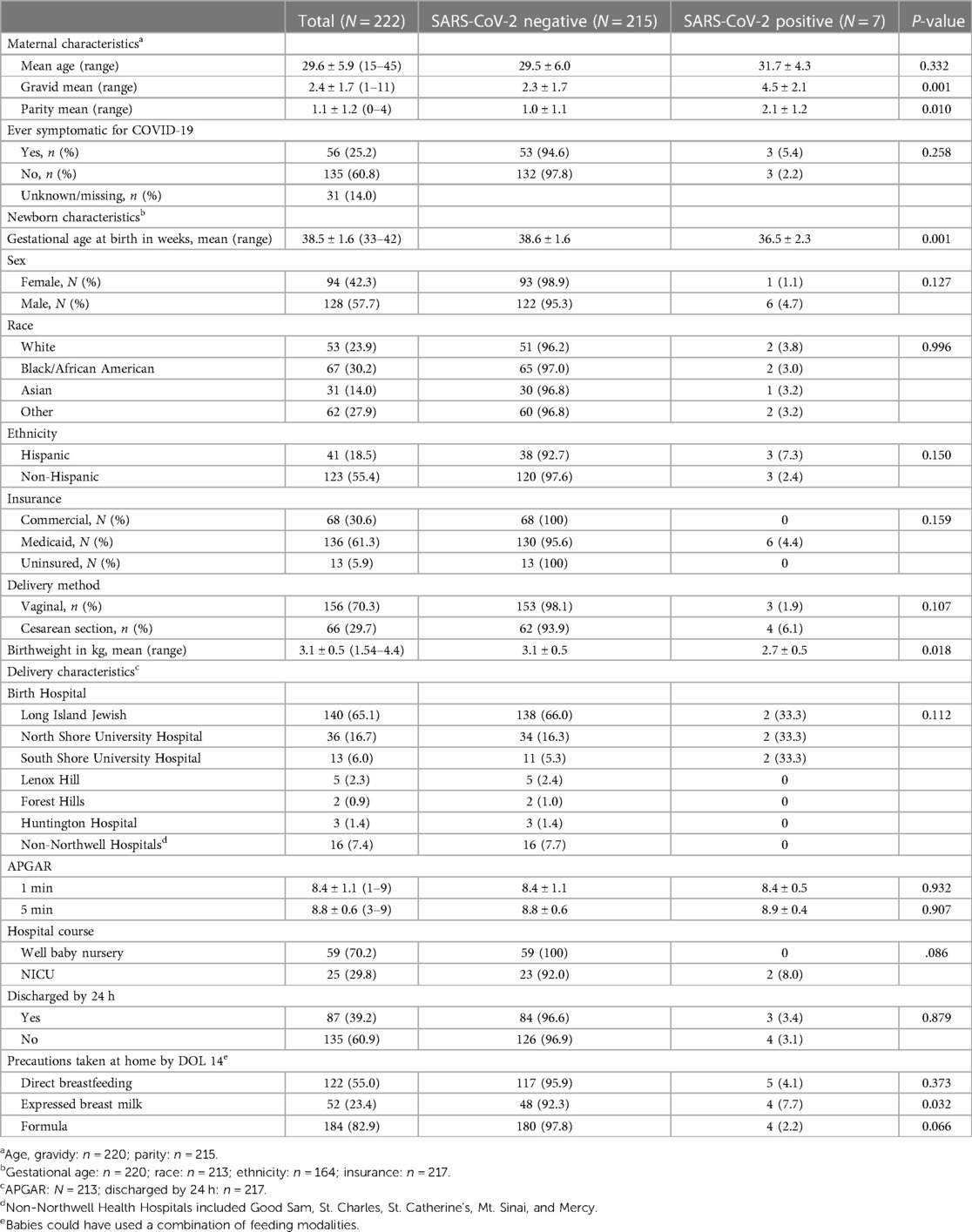
Table 1. Characteristics of newborns born to SARS-CoV-2-positive mothers: mothers, delivery circumstances, and home circumstances.
There were 293 infants born to SARS-CoV-2-positive mothers evaluated at CCMC practices between 27 March 2020 and 18 March 2022 (Figure 1). Of those, 222 newborns had repeat swab by DOL 14 and were included in the analysis (Table 1). The mean maternal age was 29.5 years; 29.3% of mothers were symptomatic for SARS-CoV-2 at delivery. The mean newborn gestational age was 38.5 weeks; 57.8% were male; 76.1% were non-White; 69.5% had Medicaid or were uninsured; and 29.8% were admitted to the NICU for reasons unrelated to maternal SARS-CoV-2 infection.
All infants tested negative for SARS-CoV-2 at DOL 0. The second SARS-CoV-2 test was obtained between DOL 2 and DOL 14 (median DOL 10). Among the second round of tests, 154 (69.4%) occurred when the alpha variant was the predominant strain, 58 (26.1%) during the delta strain, and 10 (4.5%) during the omicron strain. Of those, seven tested positive (3.2%) and none had symptoms attributable to SARS-CoV-2 infection. Details of the cases are included in Supplementary Table S1. No neonate in the cohort required emergency room care or hospital care by DOL 28.
We present the largest series of neonates born to SARS-CoV-2-positive mothers followed across a regional primary care network with many racial/ethnic minorities and Medicaid/uninsured populations. Vertical transmission is thought to occur through three primary mechanisms: in utero transmission through binding of viral spike proteins to receptors on host cell membranes; intrapartum transmission, which occurs during the process of labor and childbirth; and postnatal transmission, when the infant is exposed to maternal breast milk and/or respiratory secretions (9, 10). In this observational cohort, the rate of congenital infection as evidenced by a positive test at 24 h of age was zero; the perinatal transmission rate was 3.2% by DOL 14. These findings are similar to those in existing published cohorts: one prospective observational study found that of 177 newborns exposed to COVID-19, only 9 (5.1%) tested positive for the virus within 14 days of life via nasopharyngeal reverse transcription polymerase chain reaction (11). Similarly, previous studies have shown that the overall reported transmission rates were less than 5% (4–8, 12). Another key finding in this study is that the perinatal transmission rate persisted across multiple predominant strains in the New York metropolitan region, which mirrored that of the United States and abroad (6). Low transmission rates of similar hospital rooming-in and breastfeeding practices suggest post-hospitalization transmission mechanisms (5, 13).
The low overall transmission rates and the absence of symptomatic infection support the safety of the November 2022 AAP guidelines (3) recommending that infants born to asymptomatic mothers be allowed to room-in and directly breastfeed with appropriate masking and hand and breast hygiene. Our findings also support the safety of direct breastfeeding after hospital discharge with appropriate hand and breast hygiene. This study is limited by the short follow-up period and parent-reported adherence to hygiene and isolation practices. In addition, since the study was conducted in a single hospital system, it may not apply to other populations. However, our study represents a more regional and population-based estimate of perinatal SARS-CoV-2 transmission than prior reports.
The raw, de-identified data supporting the conclusions of this article will be made available by the authors, without undue reservation. Requests to access the datasets should be directed to SJ,c2phbjFAbm9ydGh3ZWxsLmVkdQ==.
Ethical approval was not required for the study involving humans in accordance with the local legislation and institutional requirements. Written informed consent to participate in this study was not required from the participants or the participants’ legal guardians/next of kin in accordance with the national legislation and the institutional requirements.
SJ: Conceptualization, Data curation, Formal Analysis, Funding acquisition, Investigation, Methodology, Supervision, Validation, Writing – original draft, Writing – review & editing. RK: Conceptualization, Data curation, Investigation, Validation, Writing – review & editing. DF: Conceptualization, Data curation, Writing – review & editing. TS: Investigation, Writing – review & editing. JB: Conceptualization, Data curation, Methodology, Validation, Writing – review & editing. CS: Data curation, Formal Analysis, Investigation, Project administration, Validation, Visualization, Writing – review & editing. JC: Data curation, Formal Analysis, Investigation, Project administration, Validation, Visualization, Writing – review & editing. AT: Investigation, Writing – review & editing. BM: Investigation, Writing – review & editing. CL: Investigation, Writing – review & editing. EM: Investigation, Writing – review & editing. EW: Investigation, Writing – review & editing. LL: Investigation, Writing – review & editing. MH: Investigation, Writing – review & editing. MK: Investigation, Writing – review & editing. LR: Conceptualization, Formal Analysis, Supervision, Writing – review & editing.
The authors declare that no financial support was received for the research, authorship, and/or publication of this article.
The authors thank Samantha Mickle for assisting the research team to acquire data from the pediatric service line practices.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fped.2024.1381104/full#supplementary-material
1. Dumitriu D, Emeruwa UN, Hanft E, Liao GV, Ludwig E, Walzer L, et al. Outcomes of neonates born to mothers with severe acute respiratory syndrome coronavirus 2 infection at a large medical center in New York city. JAMA Pediatr. (2021) 175(2):157–67. doi: 10.1001/jamapediatrics.2020.4298
2. Salvatore CM, Han J-Y, Acker KP, Tiwari P, Jin J, Brandler M, et al. Neonatal management and outcomes during the COVID-19 pandemic: an observation cohort study. Lancet Child Adolesc Health. (2020) 4(10):721–7. doi: 10.1016/S2352-4642(20)30235-2
3. American Academy of Pediatrics. FAQs: management of infants born to mothers with suspected or confirmed COVID-19 (2022). Available online at: https://www.aap.org/en/pages/2019-novel-coronavirus-covid-19-infections/clinical-guidance/faqs-management-of-infants-born-to-covid-19-mothers/ (accessed January 31, 2024).
4. Hudak ML, Flannery DD, Barnette K, Getzlaff T, Gautam S, Dhudasia MB, et al. Maternal and newborn hospital outcomes of perinatal SARS-CoV-2 infection: a national registry. Pediatrics. (2023) 151(2):e2022059595. doi: 10.1542/peds.2022-059595
5. Pugni L, Crippa BL, Raimondi F, Vento G, Mangili G, Coscia A, et al. SARS-CoV-2 perinatal transmission and neonatal outcomes across four different waves of COVID-19 pandemic: a nationwide prospective cohort study from the Italian society of neonatology. Int J Infect Dis. (2024) 140:17–24. doi: 10.1016/j.ijid.2023.12.011
6. Pietrasanta C, Ronchi A, Agosti M, Mangili G, Sinelli M, Ghirardello S, et al. Early postnatal infection of neonates born to mothers infected by SARS-CoV-2 omicron variant. Pediatrics. (2023) 152(5):e2023062702. doi: 10.1542/peds.2023-062702
7. Allotey J, Chatterjee S, Kew T, Gaetano A, Stallings E, Fernandez-Garcia S, et al. SARS-CoV-2 positivity in offspring and timing of mother-to-child transmission: living systematic review and meta-analysis. Br Med J. (2022) 376:e067696. doi: 10.1136/bmj-2021-067696
8. Angelidou A, Sullivan K, Melvin PR, Shui JE, Goldfarb IT, Bartolome R, et al. Association of maternal perinatal SARS-CoV-2 infection with neonatal outcomes during the COVID-19 pandemic in Massachusetts. JAMA Netw Open. (2021) 4(4):e217523. doi: 10.1001/jamanetworkopen.2021.7523
9. World Health Organization. Definition and categorization of the timing of mother-to-child transmission of SARS-CoV-2: scientific brief (2021). Available online at: https://apps.who.int/iris/handle/10665/339422 (accessed February 8, 2021).
10. Kyle MH, Hussain M, Saltz V, Mollicone I, Bence M, Dumitriu D. Vertical transmission and neonatal outcomes following maternal SARS-CoV-2 infection during pregnancy. Clin Obstet Gynecol. (2022) 65(1):195–202. doi: 10.1097/GRF.0000000000000667
11. Vigil-Vázquez S, Carrasco-García I, Hernanz-Lobo A, Manzanares A, Perez-Perez A, Toledano-Revenga J, et al. Impact of gestational COVID-19 on neonatal outcomes: is vertical infection possible? Pediatr Infect Dis J. (2022) 41(6):466–72. doi: 10.1097/INF.0000000000003518
12. Ciapponi A, Bardach A, Comandé D, Berrueta M, Argento FJ, Rodriguez Cairoli F, et al. COVID-19 and pregnancy: an umbrella review of clinical presentation, vertical transmission, and maternal and perinatal outcomes. PLoS One. (2021) 16(6):e0253974. doi: 10.1371/journal.pone.0253974
Keywords: SARS-CoV-2, newborns, COVID-19, transmission risk, pediatric medicine
Citation: Jan S, Katz R, Fagan D, Santos T, Beachy JC, Steinway C, Chen J, Tsouristakis A, Mancenido B, Leung C, Moore E, Wilson E, Lin L, Harte M, Katzow M and Rubin LG (2024) Prevalence of SARS-CoV-2 in newborns born to SARS-CoV-2-positive mothers at 2 weeks of life. Front. Pediatr. 12:1381104. doi: 10.3389/fped.2024.1381104
Received: 2 February 2024; Accepted: 2 April 2024;
Published: 25 April 2024.
Edited by:
Maurizio Aricò, Azienda Sanitaria Locale, ItalyReviewed by:
Desiree Caselli, Azienda Ospedaliero Universitaria Consorziale Policlinico di Bari, Italy© 2024 Jan, Katz, Fagan, Santos, Beachy, Steinway, Chen, Tsouristakis, Mancenido, Leung, Moore, Wilson, Lin, Harte, Katzow and Rubin. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Sophia Jan c2phbjFAbm9ydGh3ZWxsLmVkdQ==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.