
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Pediatr., 16 July 2024
Sec. Children and Health
Volume 12 - 2024 | https://doi.org/10.3389/fped.2024.1376774
Objective: This study aims to establish a prediction model of foetal umbilical vein standardised blood flow volume (sQuv) on estimated foetal weight (EFW) in the third trimester.
Methods: A case-cohort study involving 200 eligible normal foetuses was conducted at the Ultrasound Department of Longquanyi District of Maternity and Child Healthcare Hospital between June 1, 2020 and December 31, 2021. Ultrasound measurements were taken at two separate intervals to assess EFW and the rate of EFW (rEFW) [first: between 28 w and 33 w6d of gestational age (GA); second: after 4–6 weeks]. Umbilical vein blood flow volume (Quv) and sQuv (normalised with EFW) were calculated only during the initial measurement. Using general linear regression, a prediction model for EFW based on GA and sQuv was developed, with the gestational week employed as a calibration scalar and validated using linear regression cross-validation.
Results: In the third trimester, EFW exhibited significant correlations with GA, abdominal circumference (AC), head circumference (HC) and Quv (all ρ > 0.6, P < 0.001). Furthermore, the rEFW showed significant correlations with Quv and sQuv (all ρ > 0.6, P < 0.001). A linear regression equation was established using a general linear regression model: rEFW = 0.32689 × sQuv. Additionally, a foetal weight prediction model (EFW = −2,554.6770 + 0.9655 × sQuv + 129.6916 × GA) was established using sQuv. The above two formulas were cross-validated by intra-group linear regression and proved to be of good efficacy.
Conclusions: In the third trimester, EFW displayed significant correlations with GA, AC, HC and Quv. Additionally, the rEFW exhibited significant correlations with Quv and sQuv. The sQuv during the third trimester has predictive value for foetal weight, serving as an early warning indicator.
Foetal weight, as the paramount indicator of intrauterine growth and development, significantly influences the condition of the foetus after birth. Birth weight is closely associated with various perinatal complications: intrauterine growth restriction may lead to foetal hypoxia, neonatal asphyxia, meconium aspiration syndrome, etc. (1). Macrosomic pregnancies may result in obstructed labour, such as prolonged labour or postpartum haemorrhage (2, 3). Additionally, research suggests that intrauterine overgrowth may be linked to long-term adverse outcomes in children, including an increased risk of hypertension and type 2 diabetes (4, 5).
Traditional methods of assessing foetal weight involve measuring maternal weight, abdominal circumference (AC) and fundal height. However, ultrasound has revolutionised this process, overcoming the limitations of traditional measurements. Foetal growth is closely related to placental circulation, with the foetal umbilical vein serving as the origin of foetal blood circulation (6–8). The umbilical vein is the sole pathway through which the foetus receives blood and nutrients from the mother. Sinkovskaya et al. (9) conducted a comprehensive observation and investigation of the foetal vein across six anatomical levels using ultrasound instruments. Initially, early studies predominantly focused on the poor prognosis of the foetus resulting from anatomical abnormalities of the umbilical vein (10). However, over time, more research turned towards foetal umbilical vein blood flow, making it a focal point of maternal–foetal medicine research.
This prospective study selected normal foetuses in the third trimester as an observational cohort. Ultrasound techniques were employed to measure and calculate foetal umbilical vein blood flow parameters to analyse the correlation between umbilical vein blood flow and foetal weight in the third trimester, as well as the distribution of blood flow. By exploring the predictive value of standardised blood flow volume on body weight, this study aims to provide obstetricians with a more effective reference index for assessing and predicting foetal body weight.
Two hundred eligible foetuses were selected from pregnant patients who underwent ultrasound examinations at the Ultrasound Department of Longquanyi District of Chengdu Maternity and Child Health Care Hospital between June 1, 2020 and December 31, 2021. This study was conducted in accordance with the Declaration of Helsinki and approved by the ethics committee of Longquanyi District of Chengdu Maternity and Child Health Care Hospital (KY-2020-04). Written informed consent was obtained from all participants.
The inclusion criteria were as follows: (1) foetuses of healthy pregnant women aged 20–34 years who voluntarily signed the Informed Consent for Research; (2) singleton pregnancies normally delivered at full term (38–42 weeks). The exclusion criteria were as follows: (1) pregnant women with hypertension, diabetes mellitus, cardiorespiratory abnormalities or history of hereditary diseases; (2) foetuses with structural malformations, chromosomal abnormalities, hydrops fetalis, oligohydramnios, umbilical artery abnormalities, right umbilical vein, portosystemic shunt, cord knots or cord entanglement; (3) foetuses clinically diagnosed as growth-restricted, small for gestational age (SGA) or large for GA (LGA).
A study cohort comprising eligible foetuses underwent two consecutive ultrasound examinations in the third trimester. The first examination was performed between GA of 28 w and 33 w6d, during which the weight and umbilical vein blood flow volume (Quv) were measured. The second examination was carried out 4–6 weeks later (GA’), during which estimated foetal weight (EFW) and the rate of EFW (rEFW) between the two intervals were calculated. Foetal GA was determined based on early gestational nuchal translucency examination (estimated GA derived from head and hip length measured by ultrasound).
A GE-E8 colour ultrasonic diagnostic instrument equipped with a transabdominal volumetric probe (model C1–5) operating at a frequency of 1–5 MHz was used (safety description: spatial peak time-averaged sound intensity <100 mW/cm2, mechanical variation of 10%). Initially, two attending physicians, each with over 5 years of experience in obstetric ultrasound examinations, underwent certification and quality assessment. Subsequently, procedures for image acquisition, data measurement and image storage were carried out (from 14:00 to 16:00 every day).
Measurements of foetal growth parameters, such as biparietal diameter, head circumference (HC), AC and femur length, were conducted thrice, and the mean value was computed. Based on the above parameters, the ultrasonic instrument's software employed Hadlock's formula to calculate ultrasound EFW in grams (11).
Umbilical vein measurements were made by deflecting the transverse section of the foetal abdominal circumference slightly towards the entrance of the abdominal wall of the umbilical cord (Figure 1). The procedure involved the following. (1) The morphology of the intra-abdominal segment of the umbilical vein was displayed using colour Doppler flow imaging mode. (2) The umbilical vein spectrum was displayed using pulsed-wave Doppler mode: a sample volume of 0.1–0.2 cm was placed approximately 1.0 cm into the abdomen within the umbilical vein, ensuring the sound velocity was parallel to blood flow and the angle correction was <30°. More than three complete waveforms were consecutively displayed, followed by mean velocity (Vuv) measurements. (3) Using the Zoom function of two-dimensional ultrasound imaging (B-Mod) mode to locally magnify the same position and measure the inner diameter of the umbilical vein (Duv). (4) Sampling was conducted during periods of foetal inactivity when the patient could suspend breathing. Measurements were repeated three times, and the mean values were recorded (12, 13).
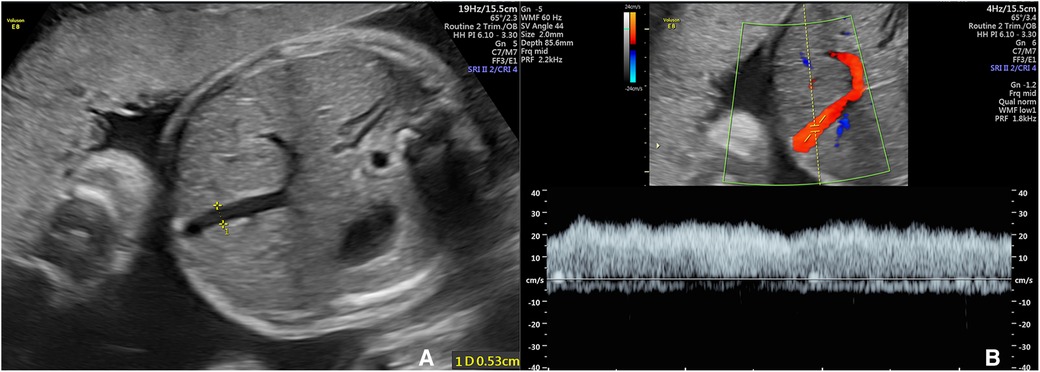
Figure 1 The ultrasonic measurment of fetal umbilical vein. (A) Velocity of umbilical venous blood flow (Vuv); (B) Diameter of umbilical venous blood flow (Duv).
The Quv was calculated using the following formula (12): Quv (ml/min) = π × [Duv (cm)/2]2 × Vuv (cm/s) × 60 (s/min).
The umbilical vein standardised blood flow volume (sQuv) was calculated using the following formula (13): sQuv (ml/min/kg) = Quv (ml/min)/EFW (g) × 1,000.
The rate of foetal weight gain was determined by two GA points and their corresponding EFW. The rEFW was calculated using the following formula: rEFW (g/w) = [EFW’ (g)−EFW (g)]/[GA’ (w)−GA (w)].
All statistical analyses were performed using SPSS software (version 27.0, IBM Corp., USA) and R 4.2.2 (R Core Foundation, Austria). This study developed a linear regression prediction model by employing the lm function in the R language and cross-validated its formula against the cv.glm function in the boot package (k = 10). Quantitative data following a normal distribution were presented as mean ± standard deviation (x ± s), and non-normally distributed quantitative data were depicted using the interquartile range (25%–75%). Count data were expressed as cases (n) and percentages (%). Pearson's (normal distribution) or Spearman's (non-normal distribution) correlation analysis was performed. Regression analysis and linear fitting were conducted for variables with significant correlation at the level of P < 0.001, and the general linear model was employed to fit the optimal curve to establish the prediction model. Furthermore, within-group cross-validation was conducted to assess the effectiveness of the model.
The umbilical vein flow and growth trajectories of 200 foetuses in the third trimester were measured and recorded using ultrasound instruments (Table 1). Concerning foetal weight, the mean value of EFW in the third trimester was obtained as 1,161 g (1,183–2,218 g), and the mean value of the rEFW in the third trimester was 185.2 g/w (110–278.4 g/w). For umbilical vein blood flow, the mean value of Quv was obtained as 288.9 ml/min (90–598 ml/min) in the third trimester. This study standardised the blood flow volume based on the foetal weight and yielded a mean value of 176 ml/min/kg (67.6–323.4 ml/min/kg) for the standardised blood flow volume (sQuv).
Spearman's correlation analysis was employed to calculate the correlation coefficient between umbilical blood flow parameters and body weight parameters. The correlation coefficients were presented using a matrix (Table 2). In the third trimester, EFW exhibited significant correlations with the GA (ρ = 0.681, P < 0.001), AC (ρ = 0.949, P < 0.001), HC (ρ = 0.792, P < 0.001) and Quv (ρ = 0.638, P < 0.001). Furthermore, the rEFW in the third trimester showed significant correlations with Quv (ρ = 0.628, P < 0.001) and sQuv (ρ = 0.641, P < 0.001).
Differential correlations of foetal Quv with HC, as well as Quv with AC, were found. This distinction was illustrated through scatterplots and regression lines (Figures 2A,B).
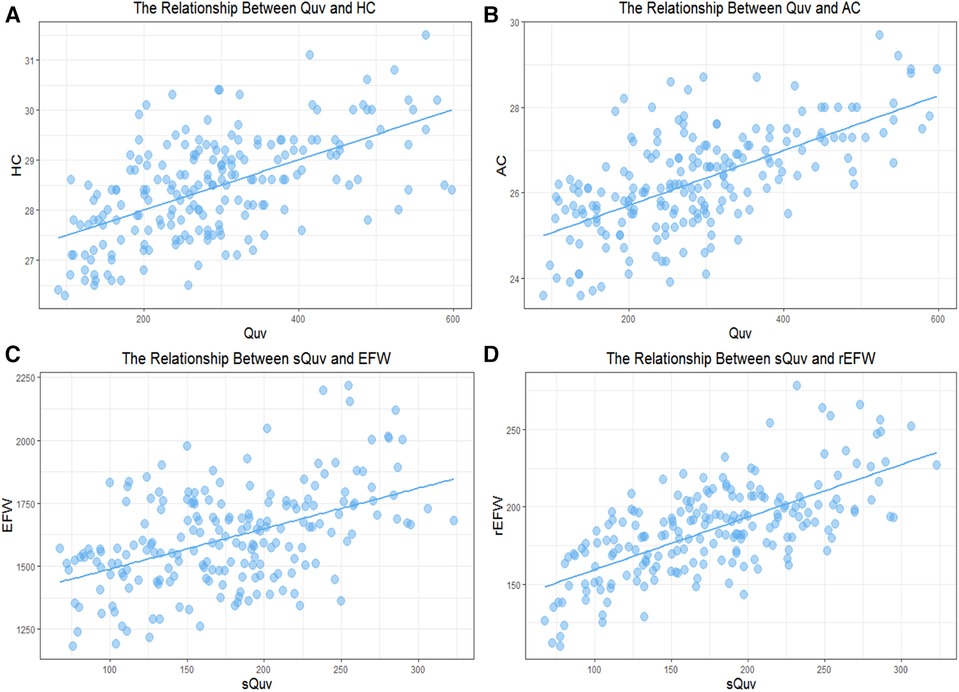
Figure 2 The relationship between fetal umbilical vein blood flow and weight parameters. (A) The relationship between Quv and HC; (B) The relationship between Quv and AC; (C) The relationship between sQuv and EFW. (D) The relationship between sQuv and rEFW.
Finally, this study standardised the Quv based on foetal weight to yield the sQuv. The correlation between the sQuv and the rEFW was demonstrated using a scatter plot and a regression line, respectively (Figure 2C). As a result, a linear regression formula was established for the sQuv and the rEFW: rEFW = 0.32689 × sQuv (Table 3), which was validated as having good efficacy through within-group cross-validation (Table 4).
Following the linear regression formula of the sQuv and the rEFW, the prediction formula of sQuv for EFW was established in the third trimester: EFW = −2,554.6770 + 0.9655 × sQuv + 129.6916 × GA (Table 5), which was validated as having good efficacy by within-group cross-validation (Table 6). Scatter plots and regression lines were used to demonstrate the high correlation between the sQuv and the rEFW, respectively (Figure 2D).
This study established a cohort of 200 patients exhibiting normal foetal weight gain in the third trimester, and ultrasound techniques were applied to measure foetal Quv. Upon confirming a significant correlation between foetal Quv and EFW, this study developed a linear regression equation incorporating a novel metric (sQuv) with the rEFW. Subsequently, a predictive model for EFW was established for foetal GA and sQuv, which demonstrated positive validation results for its efficacy. This model has the potential to serve as an early warning system for foetuses at risk of abnormal weight gain during the third trimester. The findings of this prospective study can enhance the management of foetal weight during this crucial period.
In recent years, there have been significant advancements in ultrasound instrumentation technology, which have greatly improved the visualisation and measurement of Quv, providing a more comprehensive understanding of the foetal umbilical venous system. Among the limited studies on the umbilical vein of normal foetuses, investigations into the relationship between umbilical vein diameter and GA, flow velocity and GA and flow volume and GA have been conducted (14, 15). Foetal umbilical vein diameter and flow velocity showed a significant positive correlation with GA over a longer period from 20 to 40 weeks of GA (16–18). This study opted to only include foetuses in the third trimester due to the large variation in foetal weight and rapid rate of weight gain at the same GA during this period. These findings demonstrated that the correlation between Quv and body weight was more pronounced than that between blood flow volume and GA in foetuses in late pregnancy.
Over the past two decades, advancements in early ultrasound technology have facilitated precise and consistent measurements of the fetal umbilical artery. Consequently, findings from numerous studies regarding the relationship between the fetal umbilical artery and body weight have been extensively incorporated into obstetric management (19). For example, the research conducted by Angelo Sirico et al. elegantly elucidates the correlation between the umbilical artery pulsatility index and the estimated fetal weight percentile and birthweight percentile (20–22).With recent technological improvements in ultrasound instrumentation for venous measurements, obstetricians anticipate further insights into the correlation between the foetal umbilical vein and body weight, which could significantly inform obstetric practices (23). Of the few studies that have addressed foetal umbilical vein and weight, in most cases, foetuses with abnormal weight development were selected for clinical control studies. These studies primarily explored three key areas as follows. (1) First was the diagnostic value of foetal Quv in identifying intrauterine growth restriction (24–26). Among these, a meta-analysis highlighted the umbilical vein's ability to distinguish between early-onset and late-onset foetal growth restriction (19). (2) Second, researchers such as Fatihoglu and Parra-Saavedra used umbilical vein flow to predict the occurrence of SGA (27, 28). (3) In the third trimester of pregnancy, the predictive value of foetal umbilical vein blood flow parameters for LGA has also received obstetric attention (29, 30). This study took a different perspective, focusing primarily on the relationship between Quv and foetal weight, as well as weight gain, in normally developing foetuses during late pregnancy. It is hoped that these findings will contribute to monitoring the normal growth and development of foetuses.
Measurements of foetal Quv can be interfered with by maternal respiration and intrauterine foetal activity, necessitating stringent quality control for testing personnel (31). However, blood flow volume can more directly reflect the blood supply of the foetus. In recent years, the concept of standardised blood flow rate has been introduced on top of blood flow volume to show the average distribution of blood flow per unit of body weight, making the differences in blood flow in the bodies of foetuses of different sizes more apparent (3). In this study cohort, Spearman's correlation coefficient between foetal Quv and EFW was 0.638, and that between sQuv and the rEFW was 0.641, neither of which correlated extremely well above 0.8. It is believed that this finding may better reflect the objective relationship between foetal Quv and growth in the real world. Blood flow volume represents the physical aspect of foetal blood access. However, various biochemical substances in the blood play crucial roles as biological and chemical factors for foetal blood and nutrient acquisition, including vascular growth factors and blood sugar (32, 33). Scholars from different countries have investigated the biochemical substances in foetal umbilical vein blood flow and concluded that multiple biochemical substances jointly affect foetal weight gain (34).
Nevertheless, there are still some limitations in this study. Firstly, the samples included were confined to a single hospital, whereas the predictive model would benefit from validation on foetal samples from other healthcare facilities. Secondly, as a longitudinal observation in a cohort study, the duration of this study was limited to the third trimester. In future studies, this could be extended to the second trimester to broaden the application of the model. Thirdly, this study only investigated blood flow volume in the umbilical vein, overlooking the influence of factors in the umbilical artery and significant biochemicals in the blood, potentially constraining the generalizability of the results. The correlation between foetal Quv and body weight in the real world may involve numerous factors of haemodynamics, biology and chemistry. More comprehensive research information can only be obtained through increased multidisciplinary collaboration.
In summary, this study provides valuable insights into predicting the growth trend of normal foetuses in the third trimester, emphasising its potential implications for both research and practical applications. In the third trimester, EFW displayed significant correlations with GA, AC, HC and Quv. Additionally, the rEFW exhibited significant correlations with Quv and sQuv. Using the predictive model, obstetricians can proactively identify foetal weight abnormalities during this critical development phase. Based on the findings of this study, there is significant potential for further investigation into modulating foetal Quv, thereby optimising nutrient delivery to the foetus. Innovative and efficient explorations within this field are eagerly anticipated to be embarked upon in the future.
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
The studies involving humans were approved by the ethics committee of LongQuanYi District of Chengdu Maternity and Child Health Care Hospital. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
QF: Conceptualization, Data curation, Methodology, Writing – original draft. YS: Conceptualization, Formal Analysis, Methodology, Writing – review & editing. CZ: Data curation, Methodology, Resources, Investigation, Writing – review & editing. YC: Data curation, Formal Analysis, Investigation, Software, Writing – original draft. CY: Writing – review & editing. JY: Data curation, Formal Analysis, Investigation, Writing – original draft. GH: Data curation, Supervision, Validation, Writing – review & editing.
The author(s) declare financial support was received for the research, authorship, and/or publication of this article.
Medical Research Project of Health Commission of Chengdu (2020164).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
UV, umbilical venous; Quv, quantity of umbilical venous blood flow; Vuv, velocity of umbilical venous blood flow; Duv, diameter of umbilical venous blood flow; EFW, estimated fetal weight; sQuv, standardized quantityof umbilical venous blood rate; rEFW, rate of estimated fetal weight growth; GA, gestation age; HC, head circumference; AC, abdominal circumference.
1. Burton GJ, Jauniaux E. Pathophysiology of placental-derived fetal growth restriction. Am J Obstet Gynecol. (2018) 218:S745–61. doi: 10.1016/j.ajog.2017.11.577
2. Nguyen MT, Ouzounian JG. Evaluation and management of fetal macrosomia. Obstet Gynecol Clin North Am. (2021) 48:387–99. doi: 10.1016/j.ogc.2021.02.008
3. Beta J, Khan N, Khalil A, Fiolna M, Ramadan G, Akolekar R. Maternal and neonatal complications of fetal macrosomia: systematic review and meta-analysis. Ultrasound Obstet Gynecol. (2019) 54:308–18. doi: 10.1002/uog.20279
4. Franks PW, Hanson RL, Knowler WC, Sievers ML, Bennett PH, Looker HC. Childhood obesity, other cardiovascular risk factors, and premature death. N Engl J Med. (2010) 362:485–93. doi: 10.1056/NEJMoa0904130
5. Cristian A, Tarry-Adkins JL, Aiken CE. The uterine environment and childhood obesity risk: mechanisms and predictions. Curr Nutr Rep. (2023) 12:416–25. doi: 10.1007/s13668-023-00482-z
6. Valensise H, Farsetti D, Pometti F, Vasapollo B, Novelli GP, Lees C. The cardiac-fetal-placental unit: fetal umbilical vein flow rate is linked to the maternal cardiac profile in fetal growth restriction. Am J Obstet Gynecol. (2023) 228:222.e1–.e12. doi: 10.1016/j.ajog.2022.08.004
7. Choi ES, Lee H, Lee SJ, Jung YM, Kim HY, Lee SM, et al. Ultrasonographic assessment of abnormal fetal growth related to uteroplacental-fetal biometrics and Doppler (U-AID) indices: protocol for multicenter retrospective cohort study trial. PLoS One. (2024) 19:e0298060. doi: 10.1371/journal.pone.0298060
8. Yagel S, Kivilevitch Z, Cohen SM, Valsky DV, Messing B, Shen O, et al. The fetal venous system, part II: ultrasound evaluation of the fetus with congenital venous system malformation or developing circulatory compromise. Ultrasound Obstet Gynecol. (2010) 36:93–111. doi: 10.1002/uog.7622
9. Sinkovskaya E, Klassen A, Abuhamad A. A novel systematic approach to the evaluation of the fetal venous system. Semin Fetal Neonatal Med. (2013) 18:269–78. doi: 10.1016/j.siny.2013.05.009
10. Damiani GR, Del Boca G, Biffi A. Five-vessel umbilical cord and fetal outcome: an obstetric overview. J Matern Fetal Neonatal Med. (2022) 35:6250–3. doi: 10.1080/14767058.2021.1910660
11. Hadlock FP, Harrist RB, Martinez-Poyer J. In utero analysis of fetal growth: a sonographic weight standard. Radiology. (1991) 181:129–33. doi: 10.1148/radiology.181.1.1887021
12. Ai H, Yu BL, Yin YM, Ren XP, Pan WQ, Su JL. Reference ranges of fetal ductus venous and umbilical vein flow during second and third trimester (Chinese). Chin J Umbilical Med. (2006) 11:842–5. doi: 10.3760/j.issn:1004-4477.2006.11.012
13. Xu GQ, Zhou QC, Zhou CH, Wang JQ, Long BG, Hu L, et al. Normal ranges and Z-score analysis of the normal fetal umbilical diameter, blood volume flow and normalized volume blood flow in the second and third trimesters of pregnancy. Chin J Ultrasonography. (2022) 31:386–93. doi: 10.3760/cma.j.cn131148-20211111-00824
14. DeVore GR, Epstein A. Computing Z-score equations for clinical use to measure fetal umbilical vein size and flow using six independent variables of age and size. J Ultrasound Med. (2022) 41:1949–60. doi: 10.1002/jum.15872
15. Wang L, Zhou Q, Zhou C, Wang J, Shi C, Long B, et al. Z-Score reference ranges for umbilical vein diameter and blood flow volume in normal fetuses. J Ultrasound Med. (2022) 41:907–16. doi: 10.1002/jum.15774
16. Köşüş A, Köşüş N, Turhan N. Is there any relation between umbilical artery and vein diameter and estimated fetal weight in healthy pregnant women? J Med Ultrason (2001). (2012) 39:227–34. doi: 10.1007/s10396-012-0360-0
17. Novoa V, Shazly S, Ibirogba ER, Sutton L, Tonni G, Prefumo F, et al. Perinatal outcomes of fetal intra-abdominal umbilical vein varix: a multicenter cohort study. J Matern Fetal Neonatal Med. (2021) 34:3393–6. doi: 10.1080/14767058.2019.1685969
18. Huang H, Li XY, Pang CY, Huang FX, Lai MY, Huang YF, et al. Study of the ratio of normal fetal umbilical venous blood flow rate to umbilical artery plusatility index. Chin J Ultrasonography. (2022) 31(05):394–9. doi: 10.3760/cma.j.cn131148-20211018-00745
19. Gordijn SJ, Beune IM, Thilaganathan B, Papageorghiou A, Baschat AA, Baker PN, et al. Consensus definition of fetal growth restriction: a delphi procedure. Ultrasound Obstet Gynecol. (2016) 48:333–9. doi: 10.1002/uog.15884
20. Cromi A, Ghezzi F, Di Naro E, Siesto G, Bergamini V, Raio L. Large cross-sectional area of the umbilical cord as a predictor of fetal macrosomia. Ultrasound Obstet Gynecol. (2007) 30:861–6. doi: 10.1002/uog.5183
21. Sirico A, Rizzo G, Maruotti GM, Aiello E, Morlando M, Arduini D, et al. Does fetal macrosomia affect umbilical artery Doppler velocity waveforms in pregnancies complicated by gestational diabetes? J Matern Fetal Neonatal Med. (2016) 29:3266–70. doi: 10.3109/14767058.2015.1121479
22. Sirico A, Diemert A, Glosemeyer P, Hecher K. Third trimester umbilical artery Doppler in low-risk pregnancies and its correlation to estimated fetal weight and birthweight. Ultraschall Med. (2021) 42:285–90. doi: 10.1055/a-1010-5833
23. Behery MM E, Nouh AA, Alanwar AM, Diab AE. Effect of umbilical vein blood flow on perinatal outcome of fetuses with lean and/or hypo-coiled umbilical cord. Arch Gynecol Obstet. (2011) 283:53–8. doi: 10.1007/s00404-009-1272-0
24. Rigano S, Bozzo M, Padoan A, Mustoni P, Bellotti M, Galan HL, et al. Small size-specific umbilical vein diameter in severe growth restricted fetuses that die in utero. Prenat Diagn. (2008) 28:908–13. doi: 10.1002/pd.2054
25. Hamidi OP, Driver C, Steller JG, Peek EE, Monasta L, Stampalija T, et al. Umbilical venous volume flow in late-onset fetal growth restriction. J Ultrasound Med. (2023) 42:173–83. doi: 10.1002/jum.15993
26. Rigano S, Bozzo M, Ferrazzi E, Bellotti M, Battaglia FC, Galan HL. Early and persistent reduction in umbilical vein blood flow in the growth-restricted fetus: a longitudinal study. Am J Obstet Gynecol. (2001) 185:834–8. doi: 10.1067/mob.2001.117356
27. Parra-Saavedra M, Crovetto F, Triunfo S, Savchev S, Parra G, Sanz M, et al. Added value of umbilical vein flow as a predictor of perinatal outcome in term small-for-gestational-age fetuses. Ultrasound Obstet Gynecol. (2013) 42:189–95. doi: 10.1002/uog.12380
28. Fatihoglu E, Aydin S. Diagnosing small for gestational age during second trimester routine screening: early sonographic clues. Taiwan J Obstet Gynecol. (2020) 59:287–92. doi: 10.1016/j.tjog.2020.01.019
29. Tutus S, Asal N, Uysal G, Şahin H. Is there a relationship between high birth weight and umbilical vein diameter? J Matern Fetal Neonatal Med. (2021) 34:3609–13. doi: 10.1080/14767058.2020.1814247
30. Rizzo G, Mappa I, Bitsadze V, Khizroeva J, Makatsarya A, D'Antonio F. The added value of umbilical vein flow in predicting fetal macrosomia at 36 weeks of gestation: a prospective cohort study. Acta Obstet Gynecol Scand. (2021) 100:900–7. doi: 10.1111/aogs.14047
31. Boito SM, Ursem NT, Struijk PC, Stijnen T, Wladimiroff JW. Umbilical venous volume flow and fetal behavioral states in the normally developing fetus. Ultrasound Obstet Gynecol. (2004) 23:138–42. doi: 10.1002/uog.956
32. Zhang L, Wu Q, Zhu S, Tang Y, Chen Y, Chen D, et al. Chemerin-induced down-regulation of placenta-derived exosomal miR-140-3p and miR-574-3p promotes umbilical vein endothelial cells proliferation, migration, and tube formation in gestational diabetes mellitus. Cells. (2022) 11(21):3457. doi: 10.3390/cells11213457
33. Rubin JM, Fowlkes JB, Pinter SZ, Treadwell MC, Kripfgans OD. Umbilical vein pulse wave spectral analysis: a possible method for placental assessment through evaluation of maternal and fetal flow components. J Ultrasound Med. (2022) 41:2445–57. doi: 10.1002/jum.15927
34. Lund A, Ebbing C, Rasmussen S, Qvigstad E, Kiserud T, Kessler J. Pre-gestational diabetes: maternal body mass index and gestational weight gain are associated with augmented umbilical venous flow, fetal liver perfusion, and thus birthweight. PLoS One. (2021) 16:e0256171. doi: 10.1371/journal.pone.0256171
Keywords: foetus, umbilical vein, blood flow, standardised blood flow volume, body weight
Citation: Fang Q, Shi Y, Zhang C, Cai Y, Yuan C, Yang J and He G (2024) Value of foetal umbilical vein standardised blood flow volume in predicting weight gain in the third trimester: a prospective case-cohort study. Front. Pediatr. 12: 1376774. doi: 10.3389/fped.2024.1376774
Received: 26 January 2024; Accepted: 19 June 2024;
Published: 16 July 2024.
Edited by:
Angelo Sirico, Azienda Ospedaliera di Caserta, ItalyReviewed by:
Lei Li, Shandong Provincial Hospital, China© 2024 Fang, Shi, Zhang, Cai, Yuan, Yang and He. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Qian Fang, ZmFuZ3FpYW4yMDI0ZnFAMTYzLmNvbQ==
†These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.