
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Pediatr. , 19 April 2024
Sec. Pediatric Urology
Volume 12 - 2024 | https://doi.org/10.3389/fped.2024.1371028
This article is part of the Research Topic Insights in Pediatric Urology View all 7 articles
Background: Fowler–Stephens orchiopexy is commonly used for testes that cannot be brought into the scrotum in one operation. However, this surgical technique may result in a higher rate of testicular atrophy postoperatively.
Methods: During the period between 2019 and 2023, we analyzed the cases of 20 patients in whom the Shehata technique was applied for testes that could not be brought into the scrotum in one operation, and we conducted a meta-analysis to explore the incidence of testicular atrophy vis-à-vis the Shehata technique and Fowler–Stephens orchiopexy.
Results: The average age of the 20 patients was 3.78 (0.76–11.42) years. The blood supply to the testes was satisfactory, with the absence of atrophy, and the testes could be brought into the scrotum in stage II surgery. A postoperative reexamination with ultrasound revealed that the testes were securely positioned within the scrotum, with good blood supply and no atrophy, which was in contrast to their condition before the operation. The volume of the testes postoperatively was significantly greater than that of the preoperative testes (p = 0.009). There were no statistically significant differences in the growth rate of volume of the testes between the surgically treated side and the contralateral side (p = 0.25). The meta-analysis showed that the Shehata technique resulted in a lower incidence of testicular atrophy compared with Fowler–Stephens orchiopexy (p = 0.01).
Conclusions: The Shehata technique preserves the main vessels of the testes with a lower incidence of testicular atrophy, which may be a valid and safe alternative to the Fowler–Stephens technique.
Common surgical treatment techniques for an undescended testis include orchiopexy and Fowler–Stephens orchiopexy. Fowler–Stephens orchiopexy is commonly used for those testes that cannot be brought into the scrotum in one operation. However, this technique may induce a higher rate of testicular atrophy following surgery. In one study, postpubertal Wistar WU rats were used as models for Fowler–Stephens orchiopexy, which revealed significant decreases in the size of the testis, the diameter of the seminiferous tubules, and the normal sperm count. In addition, the pH levels in the tubules and interstitium also decreased, suggesting that testicular atrophy resulted from testicular ischemic injury (1). Therefore, there is still a clinical need to explore other potential surgical options for undescended testis. In another study, it has been reported that the Shehata technique can be used to treat high intra-abdominal testis without the need for vessel transection (2). This technique involves fixing the testis to a point 2.5 cm above and medial to the contralateral anterior superior iliac spine during stage I surgery (2). The authors reported that during stage II surgery, the sutures of the testis and the adhesions between the testis and the abdominal wall were removed, and then, the testis was also brought into the scrotum (2). The Shehata technique may be considered a better option for treating undescended testis that cannot be brought into the scrotum in one operation. In the context of the limited research on the Shehata technique for treating high cryptorchidism, in this study, we report a case series of 20 patients who were successfully treated with the Shehata technique for undescended testis that could not be brought into the scrotum in one operation. In addition, we conducted a meta-analysis to explore the incidence of testicular atrophy vis-à-vis the Shehata technique and Fowler–Stephens orchiopexy.
This retrospective study was conducted at the Department of Pediatric Surgery, Baoan Women's and Children's Hospital, during the period between January 2019 and August 2023. The study was approved by the local Medical Ethics Committee and conformed to the principles of the Declaration of Helsinki. It is usually the case that if the classical laparoscopically assisted orchiopexy technique fails to bring the testis to the scrotum in a single operation, the Shehata technique is performed.
The inclusion criteria were as follows: (1) patient age younger than 12 years; (2) an undescended testis that cannot be brought to the scrotum in one operation; (3) obtaining of informed consent from patients’ legal representatives.
The exclusion criteria were as follows: (1) patient age of more than 12 years; (2) an undescended testis that can be brought to the scrotum in one operation; (3) failure to obtain informed consent; (4) incomplete data.
A skin incision was made at the superior border of the umbilicus, and initial peritoneal access was achieved with a Veress needle, followed by the insertion of a 3 mm trocar. Subsequently, two 3 mm trocars were inserted into the left and right midclavicular lines at the level of the umbilicus, respectively. The testis, vas deferens, and spermatic vessels were freed (freeing the spermatic vessels as high as possible). For patients who were unable to bring the testis to the contralateral internal ring without tension and who had an obviously insufficient visualized length of the spermatic cord, the Shehata technique was performed. Otherwise, we attempted an orchiopexy. A vascular clamp was passed from the scrotal incision into the abdomen. The testis was grasped at the gubernaculum tissue with the forceps and then brought out and placed into the subdartos pouch. If the testis could not reach the ipsilateral scrotum without tension, the Shehata technique was also performed. A non-absorbable suture was passed trans-abdominally into the abdominal cavity on a curved needle, avoiding the testicular vessels and vas deferens, and fixing the testis to a point above and medial to the contralateral anterior superior iliac spine twice. However, for a small number of patients with severely insufficient spermatic vessel lengths, the testis was fixed in the area between the bladder and the contralateral anterior superior iliac spine (Figure 1).
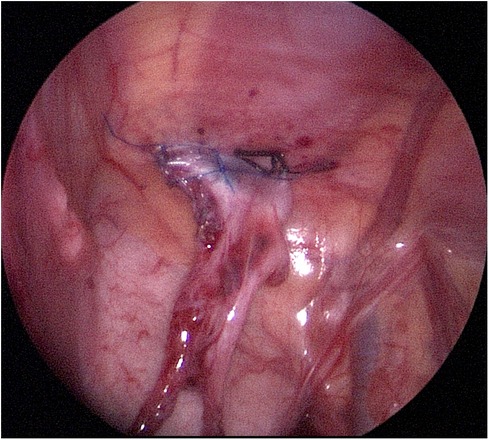
Figure 1. The affected testis was surgically fixed near the contralateral anterior superior iliac spine.
Removal of the sutures from the testis and the adhesions between the testis and the abdominal wall was performed. The affected testicular vessels and vas deferens were mobilized when their lengths were found to be insufficient. Then, the testis was brought into the scrotum without tension.
A search of the literature (up to 30 July 2023) using PubMed, Cochrane Review database, Embase, China National Knowledge Infrastructure, and Wanfang was performed to identify studies that estimated the clinical effects of the Shehata technique in treating high cryptorchidism. Searches were performed using the terms “Shehata” or “Staged laparoscopic traction-orchiopexy.” We also searched the reference lists of the relevant literature. Data were initially extracted and evaluated independently by two investigators.
The clinical data were analyzed using the R software. The formula for estimating the volume (V) of the testis, based on the measurements of length (l) and width (w) using ultrasound, is V = l × w2 × 0.52 (3). All data on testicular volume were tested for normality using the Shapiro–Wilk test. If the data followed a normal distribution pattern, a paired sample t-test was performed. If the data were not normally distributed, a Wilcoxon paired rank-sum test was conducted. A meta-analysis was performed using Review Manager Software 5.4 (Review Manager, Nordic Cochrane Centre, UK) to compare the incidence of testicular atrophy between the Shehata technique and Fowler–Stephens orchiopexy. Pooled odds ratios (ORs) and 95% confidence intervals (CIs) were calculated for the dichotomous outcomes. The I2 statistic test and Chi-squared test were performed to assess heterogeneity. A value of I2 > 50% was regarded as indicating substantial heterogeneity. The fixed-effects model was used when I2 < 50%; otherwise, the random-effects model was used. A p-value < 0.05 was considered statistically significant.
A total of 20 patients met our inclusion criteria and were included in the analysis. The average age of these patients was 3.78 years, which ranged from 0.76 to 11.42 years. The mean interval between the two stages of surgery was 6.01 months, which ranged from 3.91 to 12.65 months. In all the 20 patients, the testes did not reach the ipsilateral scrotum without tension during stage I surgery. During stage II surgery, the lengths of their testicular vessels and vas deferens were found to be longer than before surgery (Figure 2). In addition, we observed that their testes were normal and could reach the ipsilateral scrotum without tension.
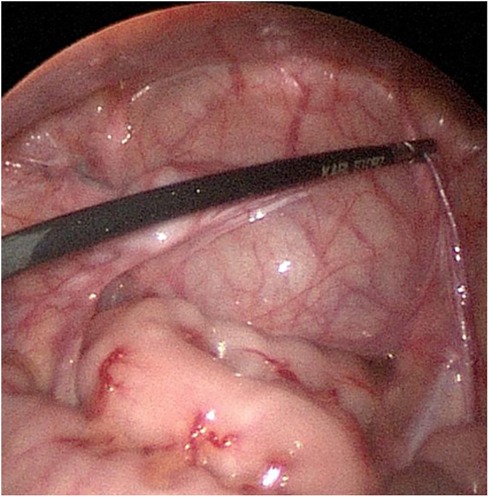
Figure 2. An elongation of the testicular vessels and the vas deferens was found during the secondary operation.
After stage I surgery and before stage II surgery, all patients were followed up for a mean period of 5.71 months (ranging from 3.19 to 12.9 months). During this time, an evaluation through color Doppler ultrasound was conducted, and the test results indicated that blood supply to the testes was good. No complications such as adhesive intestinal obstruction or internal hernia behind the testicular vessels were observed. Following stage II surgery, all patients underwent a follow-up for a mean period of 6.13 months (ranging from 3 days to 30 months). This follow-up included an evaluation of symptoms and ultrasound scan results, which confirmed that the testes were fixed in the scrotum. No testicular atrophy or other complications were observed, and blood supply to the testes remained good. The mean follow-up period for all 20 patients was 26.05 months (ranging from 2.53 to 48.59 months), and the follow-up was conducted via telephone or outpatient visits. We found no evidence of any abnormalities, aberrant locations of testes, or discomfort or pain in the testes.
The Shapiro–Wilk test indicated that the data within the study groups were not normally distributed; therefore, the Wilcoxon matched-pairs signed-rank test was performed. This test revealed that the volume of the postoperative testes was significantly greater than that of the preoperative testes (p = 0.009). There were no statistically significant differences in the growth rate of the testes’ volume between the surgical side and the contralateral side (p = 0.25).
A total of five studies involving 88 patients treated with the Shehata technique and 96 treated with Fowler–Stephens orchiopexy met the inclusion criteria (4–8). The meta-analysis showed that the Shehata technique resulted in a lower incidence of testicular atrophy compared with Fowler–Stephens orchiopexy (OR = 0.17, 95% CI 0.04, 0.67; p = 0.01), and there was no significant statistical heterogeneity (I2 = 0.0%, p = 0.99) (Figure 3).
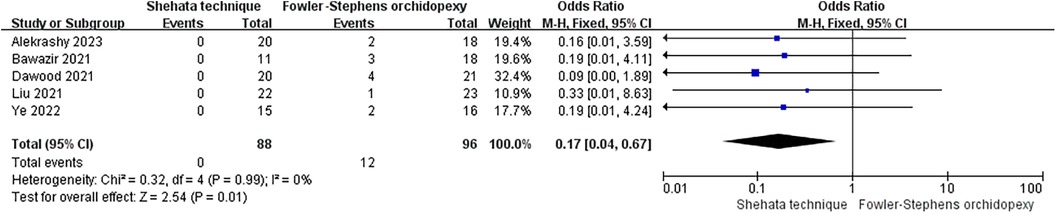
Figure 3. A comparison of the incidence of testicular atrophy between the Shehata technique group of patients and the Fowler–Stephens orchiopexy group of patients.
Undescended testis is a common congenital disorder in which unilateral or bilateral testes fail to descend into the scrotum. It may lead to complications such as testicular atrophy, infertility, testicular torsion, and malignant transformation (9). Therefore, active treatment for undescended testis is necessary. The intra-abdominal testis can be located anywhere from the lower pole of the kidney to the lower end of the internal inguinal canal. Surgical treatments for undescended testis include orchiopexy and Fowler–Stephens orchiopexy. Docimo reviewed and analyzed 8,425 cases of patients with undescended testis from 64 articles and found that the success rate for Fowler–Stephens orchiopexy was 67%, and for staged Fowler–Stephens orchiopexy, it was 77% (10). Esposito et al. performed the two-step Fowler–Stephens procedure using the laparoscopy technique on 12 patients. Among these, 16.7% experienced atrophy of the testis in the scrotum, whereas 83.3% retained a viable testis in the scrotum. Despite the good vascularization observed on echo color Doppler ultrasound, the operated testis was consistently smaller than the normal, unoperated one (11). Hvistendahl and Poulsen reported that a total of 65 patients with intra-abdominal testes underwent the laparoscopic two-stage Fowler–Stephens procedure. Of these patients, 60 required two-stage operations, while in five, the testes were removed during the second stage because of testicular atrophy or a short vas deferens. The procedure was successful in 80% of the patients (12). Yu et al. reviewed 60 studies, which included a total of 1991 operated testes. The overall success rates for one-stage and two-stage Fowler–Stephens orchiopexies were 85% and 87%, respectively. In addition, the overall atrophy rate was 10% (13). The success rates for one-stage Fowler–Stephens orchiopexies, both open and laparoscopic, were 83% and 87%, respectively, with atrophy rates of 12% and 8%. The corresponding success rates for two-stage Fowler–Stephens orchiopexies were 81% and 89%, respectively, with atrophy rates of 17% and 8% (13). When evaluating laparoscopic Fowler–Stephens orchiopexy over time, the success rates prior to the year 2000, between 2000 and 2010, and after 2010 were 85%, 89%, and 88%, respectively, with atrophy rates of 15%, 9%, and 6% (13). In 2016, it was reported that the success rate for the Shehata technique was 84% (2). The viability of the testicles relies on the presence of collateral blood supply from the vessels in the inguinal canal, hypertrophy of the artery of the vas deferens, and gubernacular vessels (14). Considering that Fowler–Stephens orchiopexy requires vessel ligation and may induce a higher rate of testicular atrophy after surgery, the Shehata technique dissociates the spermatic cord blood vessels without cutting them. This theoretically protects the blood vessels in the testicles and uses the bowel to slowly pull and lengthen the testicular vessels and vas deferens, allowing the blood vessels in the spermatic cord to extend gradually. This helps prevent testicular ischemia that may be caused by forced pulling. Therefore, the Shehata technique was performed in this study, and no testicular atrophy was found in the regular reexamination under color Doppler ultrasound. The testicular vessels and vas deferens were found to be longer than before surgery. A postoperative reexamination with color Doppler ultrasound showed good testicular blood supply without testicular atrophy. A statistical analysis showed that the volume of the postoperative testes was significantly higher than that of the preoperative testes, and there were no statistically significant differences in the growth rate of the volume of the testes between the surgical side and the contralateral side. A meta-analysis showed that the Shehata technique resulted in a lower incidence of testicular atrophy compared with Fowler–Stephens orchiopexy.
Shehata et al. included cases of patients with intra-abdominal testis occurring between the ages of 6 months and 9 years (2). However, in this study, we expanded the age range of our patients to include those between 9 and 12 years old.
Shehata et al. excluded cases of patients in whom the testis had reached the contralateral internal inguinal ring without tension (2). We adjusted the inclusion criteria for the Shehata technique to apply it only to those patients who were unable to bring the testis to the contralateral internal ring without tension and who exhibited a clearly insufficient visualized length of the spermatic cord. In such patients, the Shehata technique was employed. If the testis could not be brought down to the scrotum without tension, we performed the Shehata procedure. Conversely, if the testis could be positioned in the scrotum without tension, the Shehata procedure was deemed unnecessary, sparing the patient an additional surgery.
In this surgical technique, the majority of testicles were fixed near the contralateral anterior superior iliac spine, approximately 2.5 cm above it, with appropriate tension. However, for a small number of patients with severe deficiency of the spermatic vessels, fixing the testis near the contralateral anterior superior iliac spine was not possible. In such patients, the testis was fixed in the area between the bladder and the contralateral anterior superior iliac spine, which also yielded satisfactory results.
Shehata et al. reported 140 cases of surgery, with 16 cases of testis dropped from the fixation position (2). Dawood et al. reported 20 testes cases of surgery, with 2 cases of testis dropped from the fixation position (4). Bawazir et al. reported 11 cases of surgery, with 3 cases of testis dropped from the fixation position (7). Elsherbeny et al. reported 20 cases of surgery, with 2 cases of testis dropped from the fixation position (14). However, in our surgeries, no instances of the testis moving out of the fixation position were observed, which may be attributed to the simultaneous fixation of the testicle and the gubernaculum during stage I surgery. Another possible explanation could be the limited number of surgical cases.
This study has some limitations. Because of the difficulty patient guardians experience in fully complying with the doctor's advice, there is an obvious difference in the intervals between surgeries for different children. Furthermore, the duration of postoperative follow-up is not consistent across patients. In addition, the small proportion of children requiring staged surgery for cryptorchidism contributes to a limited clinical sample size.
The Shehata technique preserves the main vessels of the testes with a lower incidence of testicular atrophy, and may be a valid and safe alternative to the Fowler–Stephens technique.
The raw data supporting the conclusions of this article will be made available by the authors without undue reservation.
The studies involving humans were approved by Baoan Women's and Children's Hospital. The studies were conducted in accordance with the local legislation and institutional requirements. The ethics committee/institutional review board waived the requirement of written informed consent for participation from the participants or the participants’ legal guardians/next of kin because the study was approved by Baoan Women's and Children's Hospital. The data were anonymous, and the requirement for informed consent was therefore waived. Written informed consent was obtained from the individual(s), and minor(s)' legal guardian/next of kin, for the publication of any potentially identifiable images or data included in this article.
ZL: Methodology, Writing – original draft, Writing – review & editing, Data curation, Conceptualization, Visualization. ZY: Data curation, Methodology, Writing – original draft. HL: Data curation, Methodology, Writing – original draft. LW: Data curation, Writing – original draft, Supervision. BZ: Data curation, Writing – original draft, Funding acquisition, Methodology, Writing – review & editing.
The authors declare that no financial support was received for the research, authorship, and/or publication of this article.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Sperling H, Lümmen G, Schmidt C, Rübben H. Cryptorchidism: Fowler-Stephens procedure or autotransplantation—a new experimental model. Urology. (2000) 56(5):886–90. doi: 10.1016/s0090-4295(00)00771-8
2. Shehata S, Shalaby R, Ismail M, Abouheba M, Elrouby A. Staged laparoscopic traction-orchiopexy for intraabdominal testis (Shehata technique): stretching the limits for preservation of testicular vasculature. J Pediatr Surg. (2016) 51(2):211–5. doi: 10.1016/j.jpedsurg.2015.10.063
3. Hsieh ML, Huang ST, Huang HC, Chen Y, Hsu YC. The reliability of ultrasonographic measurements for testicular volume assessment: comparison of three common formulas with true testicular volume. Asian J Androl. (2009) 11(2):261–5. doi: 10.1038/aja.2008.48
4. Dawood W, Youssif M, Badawy H, Ghozlan A, Orabi S, Fahmy A. Laparoscopic staged management of high intrabdominal testis: a prospective randomized study. J Pediatr Surg. (2021) 56(12):2385–91. doi: 10.1016/j.jpedsurg.2021.02.066
5. Liu J, Tang R, Wang X, Sui B, Jin Z, Xu X, et al. Comparison of two types of staged laparoscopic orchiopexy for high intra-abdominal testes in children: a retrospective study from a single center. Front Pediatr. (2021) 9:677955. doi: 10.3389/fped.2021.677955
6. Alekrashy M, Kassem H, Elshahat W. Staged laparoscopic-traction orchiopexy versus Fowler–Stephen technique for abdominal testes: a comparative study. Egypt J Surg. (2023) 41:555–60. doi: 10.4103/ejs.ejs_29_22
7. Bawazir OA, Maghrabi AM. A comparative study between two techniques of laparoscopic orchiopexy for intra-abdominal testis. Indian J Urol. (2021) 37(3):261–6. doi: 10.4103/iju.IJU_507_20
8. Ye A, Luo JW, Liu M. Evaluation of Shehata operation in the treatment of high abdominal cryptorchidism in children. Chin Pract J Rural Doctor. (2022) 29(5):55–9. doi: 10.13201/j.issn.1001-1420.2023.03.008
9. Trussell JC, Lee PA. The relationship of cryptorchidism to fertility. Curr Urol Rep. (2004) 5(2):142–8. doi: 10.1007/s11934-004-0028-4
10. Docimo SG. The results of surgical therapy for cryptorchidism: a literature review and analysis. J Urol. (1995) 154(3):1148–52. doi: 10.1097/00005392-199509000-00082
11. Esposito C, Vallone G, Savanelli A, Settimi A. Long-term outcome of laparoscopic Fowler-Stephens orchiopexy in boys with intra-abdominal testis. J Urol. (2009) 181(4):1851–6. doi: 10.1016/j.juro.2008.12.003
12. Hvistendahl GM, Poulsen EU. Laparoscopy for the impalpable testes: experience with 80 intra-abdominal testes. J Pediatr Urol. (2009) 5(5):389–92. doi: 10.1016/j.jpurol.2009.04.004
13. Yu C, Long C, Wei Y, Tang X, Liu B, Shen L, et al. Evaluation of Fowler-Stephens orchiopexy for high-level intra-abdominal cryptorchidism: a systematic review and meta-analysis. Int J Surg. (2018) 60:74–87. doi: 10.1016/j.ijsu.2018.10.046
Keywords: Shehata technique, undescended testis, Fowler–Stephens orchiopexy, testicular atrophy, orchiopexy
Citation: Lin Z, Yu Z, Li H, Wu ri ni L and Zhang B (2024) The Shehata technique for undescended testes that cannot be brought into the scrotum in one operation—a case series and meta-analysis. Front. Pediatr. 12:1371028. doi: 10.3389/fped.2024.1371028
Received: 15 January 2024; Accepted: 3 April 2024;
Published: 19 April 2024.
Edited by:
Lisandro Ariel Piaggio, Universidad Nacional del Sur, ArgentinaReviewed by:
Adam Benjamin Hittelman, Yale University, United States© 2024 Lin, Yu, Li, Wu ri ni and Zhang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Baoxin Zhang emhhbmdieDExMjRAMTYzLmNvbQ==
†ORCID Baoxin Zhang orcid.org/0000-0001-9238-8863
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.