- 1Department of Thoracic and Oncological Surgery, Children’s Hospital Affiliated to Shandong University, Jinan, China
- 2Department of Thoracic and Oncological Surgery, Jinan Children’s Hospital, Jinan, China
The occurrence of simultaneous extralobar pulmonary sequestration, esophageal duplication, and bronchogenic cysts is relatively low. We report the case of a 9-month-old Chinese child who had a right lung cyst, detected in utero and was closely monitored until birth. At age 9 months, contrast-enhanced computed tomography revealed right mediastinal extralobar pulmonary sequestration and two cysts. The patient did not exhibit any abnormalities. However, the parents were concerned about the disease. Following positive psychological counseling to the parents, surgery was the strong desire. Subsequently, successful thoracoscopic surgery was performed, excising the three lesions. No postoperative complications occurred. Postoperative pathology confirmed extralobar pulmonary sequestration syndrome combined with esophageal duplication and bronchogenic cysts. The patient was followed-up at 1 and 12 months postoperatively and recovered well with no abnormal space occupation. In such cases, preoperative imaging examinations should be carefully performed, and intraoperative exploration should correspond to that before surgery to avoid lesion omission.
1 Introduction
1.1 Background
Extralobar pulmonary sequestration, esophageal duplication, and bronchogenic cysts are rarely observed in clinical practice, and all three can be managed with surgical treatment. Further, coexistence of the three conditions together is even rarer. There are cases of extralobar pulmonary sequestration complicated with bronchogenic cyst. All three have not been reported in a single case. This unique case highlights the possibility of encountering extralobar pulmonary sequestration, esophageal duplication, and bronchogenic cysts simultaneously in a single child.
2 Case presentation
A 9-month-old Chinese girl had been diagnosed with pulmonary sequestration in her right chest during a prenatal examination. However the fetus remained stable, and after birth, no obvious respiratory abnormalities, such as asthma or dyspnea, were observed. There was no family history of any related genetic diseases. The parents were anxious about mediastinal lesions; therefore, psychological counseling was provided. However, they strongly desired surgery. Consequently, we decided to operate on the patient. After hospitalization, the patient underwent all the relevant tests and examinations; she displayed normal development, and the chest examination was normal. Contrast-enhanced computed tomography (CT) of the patient's chest revealed an abnormal density indicative of a solid sac in the lower lobe of the right lung (Figure 1A, triangle, pentagram, quadrangle) (Figure 1B, triangle, arrow).
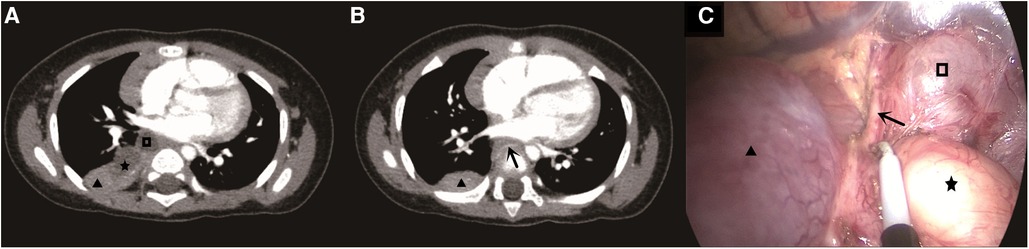
Figure 1. (A) The triangle is a extralobar pulmonary sequestration, the five-pointed star is an esophageal duplication, and the quadrilateral is a bronchogenic cyst. (B) The triangle is the outer extralobar pulmonary sequestration, and the arrow is the abnormal artery of the outer extralobar pulmonary sequestration. (C) The triangle is the outer extralobar pulmonary sequestration, the pentagram is the esophageal duplication, the quadrilateral is the bronchogenic cyst, and the arrow is the abnormal artery of the outer extralobar pulmonary sequestration.
The presence of lesions in the mediastinum was examined preoperatively. Thoracoscopic surgery was performed under general anesthesia, during which there was red, uninflated lung tissue measuring approximately 3 × 3 × 2 cm in the right mediastinum near the hilus of the lung on the farthest side (Figure 1C, triangle). Further exploration revealed a 2 × 2 × 1 cm cystic mass (Figure 1C, pentagram) and a 1.5 × 1 × 1 cm cystic mass in the intraoperative free surrounding tissue (Figure 1C, quadrangle). During thoracoscopic surgical separation, abnormal arterial supply vessels with a diameter of approximately 0.15 cm originating from the thoracic aorta were observed (Figure 1C, arrow). We successfully resected the three lesions thoracoscopically.
On the first postoperative day, the patient resumed breastfeeding. A drainage tube inserted into the patient's chest revealed 20 ml of light-bloody fluid, but no air leakage was observed.
On the second postoperative day, the child's diet returned to preoperative levels, and 18 ml of light-bloody fluid was drained; no air leakage was observed. On the third day after surgery, the children resumed their diet. The postoperative course was uneventful.
Pathological findings revealed foliar isolation of the lung (lung histological results; Figure 2A). Esophagogenic cysts (the squamous epithelium of the digestive tract is seen inside; Figure 2B) and bronchogenic cysts (respiratory epithelium dominated by pseudostratified ciliated columnar epithelium; Figure 2C) were also observed.
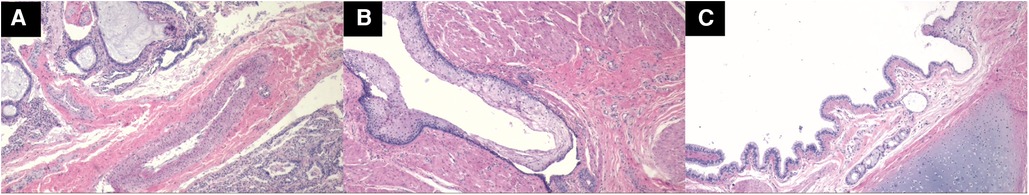
Figure 2. (A) Isolated lung HE staining magnifies pathological images by 40 times. (B) Pathological images of esophageal duplication magnified 40 times by HE staining. (C) Pathological images of bronchogenic cysts magnified 40 times by HE staining.
Postoperative review of children. The patient is asymptomatic with a normal CT scan.
3 Discussion
Pulmonary sequestration involves isolating lung tissue from the normal tracheal tree through the systemic circulation of blood. This congenital lung malformation is rare, constituting 0.15%–6.4% of all pulmonary developmental malformations (1). According to the common visceral pleural covering between the anatomical and normal lungs, there are two types of pulmonary isolation: extralobular and intralobular. Extralobar pulmonary sequestration is especially uncommon, accounting for only 15%–25% of pulmonary sequestrations (2). Approximately 60% of children with extralobar pulmonary sequestration have associated malformations, such as septal hernias, cystic adenomatoid malformations of the lungs, emphysema, and bronchogenic cysts (3). In our case, thoracoscopy revealed abnormal blood vessels in the thoracic aorta before surgery, and the solid portion exhibited extralobar pulmonary sequestration.
Esophageal duplication is a rare foregut abnormality with a very low clinical incidence (4). Bronchogenic cysts are rare congenital lung development malformations. Mampilly et al. indicated that bronchogenic cysts constitute 13%–15% of congenital intrapulmonary cyst diseases in infants. However, the pathogenesies of both esophageal duplication and bronchogenic cysts remains unclear. Esophageal duplication is often closely related to the esophagus. In our case, esophageal duplication was not closely related to the esophagus. But to those of the other two lesions. This suggests that there may be abnormalities or malformations in the development of ventral cells from the preintestinal tissues to respiratory tissues and organs during the embryonic period, possibly also leading to bronchogenic cysts. Esophageal duplication occurs when the original ventral anterior gut cells differentiate into the digestive tract tissue. This condition is rare, and our patient had pathologically confirmed esophageal duplication (5, 6). Preoperative and intraoperative diagnoses and differentiation are challenging, and postoperative pathological diagnosis is typically relied on. The duplicated esophageal wall is lined with digestive tract epithelium dominated by squamous epithelium (7), while bronchogenic cysts' inner walls consist of respiratory epithelium, characterized by pseudostratified ciliated columnar epithelium (8). In our case, although preoperative chest CT revealed two mediastinal cysts, a definitive diagnosis was not possible using preoperative imaging. Unfortunately, magnetic resonance imaging (MRI) was not performed before surgery as the parents refused the examination due to cost concerns. MRI is helpful in the diagnosis of esophageal duplication and bronchogenic cysts. However postoperative pathology confirmed the diagnosis.
Surgery is currently indicated for the treatment of exfoliar pulmonary sequestration (9, 10), esophageal duplication (11, 12), and bronchogenic cysts (13–16) in children presenting with clinical symptoms. In contrast, surgical treatment for asymptomatic cases remains controversial. Simultaneous occurrence of lobar lung isolation, esophageal duplication, and bronchogenic cysts in a single patient is exceedingly rare, and no treatment approach has been reported. In the present case, no clinical symptoms were observed. We consider the possibility of complications in particular. Thoracoscopic surgery was performed after full communication with the parents. The patient recovered well postoperatively. The operation relieved the parents' concerns and the mediastinal occupying effect on the child and was very valuable. The patient recovered well postoperatively. The operation relieved the parents' concerns. The mediastinal occupying effect on the child was relieved as well. The parents were satisfied with the surgical plan and treatment results. Thoracoscopic treatment was mainly for lobar lung isolation. We believe that the placement and positioning of the piercer is not special. Open surgery can locate the lesion in the intercostal area, similar to thoracoscopic treatment. But in this case, the advantage of thoracoscopic surgery is greater. The results were mostly good. Potential complications may include bleeding, infection, trachea injury, esophagus injury, residual cyst wall, pneumothorax, etc.
In our case, a 9-month-old Chinese child displayed extralobar pulmonary sequestration in the right mediastinum combined with an esophageal duplication and bronchogenic cyst; the three lesions were closely aligned but without duct communication. This unique case highlights the importance of raising clinical awareness among medical professionals and emphasizes the need for intraoperative exploration should to align with preoperative imaging examinations to prevent lesion omission.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by Ethics Committee/Institutional Review Committee of Jinan Children's Hospital. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants’ legal guardians/next of kin. Written informed consent was obtained from the individual(s), and minor(s)' legal guardian/next of kin, for the publication of any potentially identifiable images or data included in this article.
Author contributions
HZ: Writing – original draft, Writing – review & editing. YZ: Investigation, Methodology, Writing – original draft. RG: Investigation, Methodology, Writing – original draft. HX: Software, Supervision, Writing – original draft. SH: Software, Supervision, Writing – original draft. LL: Software, Supervision, Writing – original draft. SZ: Writing – original draft, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article.
This work was supported by 2023 science and technology plan project of Jinan Health Commission (2023-2-132) and 2023 science and technology plan project of Jinan Health Commission (2023-2-129). Shandong University Affiliated Children’s Hospital high level scientific research projects (SDFE-GCC2023005).
Acknowledgments
We would like to thank Editage (www.editage.cn) for English language editing.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Estes MEZ. Bronchopulmonary sequestration: improving practice by evaluating for a missed diagnosis. Nurse Pract. (2017) 42(6):51–5. doi: 10.1097/01.NPR.0000511775.59497.cb
2. Son SA, Do YW, Kim YE, Lee SM, Lee DH. Infarction of torsed extralobar pulmonary sequestration in adolescence. Gen Thorac Cardiovasc Surg. (2020) 68(1):77–80. doi: 10.1007/s11748-019-01105-7
3. Yamada K, Muto M, Onishi S, Machigashira S, Nishida N, Nagano A, et al. Thoracoscopic repair of neonatal left diaphragmatic hernia with sac combined with both extralobar pulmonary sequestration and congenital pulmonary airway malformation. Asian J Endosc Surg. (2023) 16(1):127–30. doi: 10.1111/ases.13120
4. Wahi JE, Safdie FM. Esophageal duplication cysts: a clinical practice review. Mediastinum. (2023) 7:1. doi: 10.21037/med-22-33
5. Kozu Y, Suzuki K, Oh S, Matsunaga T, Tsushima Y, Takamochi K. Single institutional experience with primary mediastinal cysts: clinicopathological study of 108 resected patients. Ann Thorac Cardiovasc Surg. (2014) 20(5):365–9. doi: 10.5761/atcs.oa.13-00151
6. Fievet L, Gossot D, de Lesquen H, Calabre C, Merrot T, Thomas P, et al. Resection of bronchogenic cysts in symptomatic versus asymptomatic patients: an outcome analysis. Ann Thorac Surg. (2021) 112(5):1553–8. doi: 10.1016/j.athoracsur.2020.05.031
7. McAdams HP, Kirejczyk WM, Rosado-de-Christenson ML, Matsumoto S. Bronchogenic cyst: imaging features with clinical and histopathologic correlation. Radiology. (2000) 217(2):441–6. doi: 10.1148/radiology.217.2.r00nv19441
8. Jiang JH, Yen SL, Lee SY, Chuang JH. Differences in the distribution and presentation of bronchogenic cysts between adults and children. J Pediatr Surg. (2015) 50(3):399–401. doi: 10.1016/j.jpedsurg.2014.06.008
9. Parikh DH, Rasiah SV. Congenital lung lesions: postnatal management and outcome. Semin Pediatr Surg. (2015) 24(4):160–7. doi: 10.1053/j.sempedsurg.2015.01.013
10. Baird R, Puligandla PS, Laberge JM. Congenital lung malformations: informing best practice. Semin Pediatr Surg. (2014) 23(5):270–7. doi: 10.1053/j.sempedsurg.2014.09.007
11. Fragoso AC, Casanova J, Dias JA, Estevão-Costa J. Double intercostal muscle flap to repair an extensive esophageal wall defect. Am Surg. (2023) 89(1):152–3. doi: 10.1177/0003134820952381
12. Gonzalez-Urquijo M, Hinojosa-Gonzalez DE, Padilla-Armendariz DP, Saldaña-Rodriguez JA, Leyva-Alvizo A, Rodarte-Shade M, et al. Esophageal duplication cysts in 97 adult patients: a systematic review. World J Surg. (2022) 46(1):154–62. doi: 10.1007/s00268-021-06325-8
13. Guo C, Mei J, Liu C, Deng S, Pu Q, Lin F, et al. Video-assisted thoracic surgery compared with posterolateral thoracotomy for mediastinal bronchogenic cysts in adult patients. J Thorac Dis. (2016) 8(9):2504–11. doi: 10.21037/jtd.2016.08.29
14. Fragoso AC, Fernandes S, Madureira AM, Estevão-Costa J. Acute respiratory distress due to a bronchogenic cyst submitted to percutaneous drainage followed by thoracoscopic resection. Pulmonology. (2021) 27(4):371–3. doi: 10.1016/j.pulmoe.2020.12.007
15. Ortiz RJ, Reusmann A, Boglione MM, Giuseppucci C, Ruiz J, Pérez CM, et al. Bronchogenic cyst: lessons learned in 20 years of experience at a tertiary pediatric center. J Pediatr Surg. (2023) 58(11):2156–9. doi: 10.1016/j.jpedsurg.2023.06.010
Keywords: mediastinum, extralobar pulmonary sequestration, esophageal duplication, bronchogenic cyst, Chinese children
Citation: Zhao H, Zhai Y, Guo R, Xu H, Huang S, Lv L and Zhang S (2024) Simultaneous occurrence of extralobar pulmonary sequestration, esophageal duplication, and bronchogenic cysts in a Chinese child: a rare case report. Front. Pediatr. 12:1367626. doi: 10.3389/fped.2024.1367626
Received: 9 January 2024; Accepted: 19 February 2024;
Published: 28 February 2024.
Edited by:
Francesco Morini, Meyer Children's Hospital, ItalyReviewed by:
José Estevão-Costa, University of Porto, PortugalPaul Jeziorczak, University of Illinois at Peoria, United States
© 2024 Zhao, Zhai, Guo, Xu, Huang, Lv and Zhang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Shisong Zhang zsli323@163.com
Abbreviations CT, computed tomography; MRI, magnetic resonance imaging.
 Huashan Zhao
Huashan Zhao Yunpeng Zhai1,2
Yunpeng Zhai1,2 Hongxiu Xu
Hongxiu Xu Longfei Lv
Longfei Lv Shisong Zhang
Shisong Zhang