- 1Department of Midwifery, School of Nursing and Midwifery, Asrat Woldeyes Health Science Campus, Debre Berhan University, Debre Berhan, Ethiopia
- 2Department of Medicine, Obstetrician and Gynecologist, Abebech Gobena Mothers and Childrens Health Hospital, Addis Ababa, Ethiopia
- 3Department of Epidemiology, St. Peter Specialized Hospital, Addis Ababa, Ethiopia
- 4Department of Nursing, Debre Berhan Health Science College, Debre Berhan, Ethiopia
Background: Preeclampsia is a new onset of hypertension and either proteinuria or end-organ failure after 20 weeks of gestation. It is a prevalent cause of perinatal mortality, morbidity, and neonatal complications in developing nations including Ethiopia. Thus, the aimed to assess the prevalence and determinants of adverse perinatal outcomes among women with preeclampsia with severity features (PEWSF) at two selected public hospitals in Addis Ababa, Ethiopia, 2023.
Method: A cross-sectional study was carried out among 348 mothers between January 1, 2023, and July 1, 2023. A structured, pre-tested questionnaire was used to gather data from in-person interviews and a review of the patient's medical record. The statistical program Epi-Data version 4.6 was used to enter the data, and SPSS version 26.0 was used for analysis. Binary logistic regression analysis was used to find factors that were associated with unfavorable perinatal outcomes. A p-value of less than 0.05 was used to declare the significance level.
Result: The overall prevalence of unfavorable perinatal outcomes was 59.2% (95% CI: 54.0–63.8). Among the complications, low birth weight, prematurity, NICU admission, and a low fifth-minute APGAR score, encompass 48.9%, 39.4%, 20.4%, and 14.7%, respectively. No formal education [OR = 5.14, 95% CI: (1.93–13.63)], unemployment [OR = 0.42, 95% CI: (0.24–0.73)], referral cases [OR = 2.03, 95% CI: (1.08–4.06), inadequate antenatal care (ANC) contact [OR = 3.63, 95% CI: (1.22–10.71)], and family history of hypertension [OR = 1.99, 95% CI: (1.03–3.85)] have shown a statistically significant association with unfavorable perinatal outcomes.
Conclusion: In this study, the prevalence of unfavorable perinatal outcomes was high compared to other studies in Ethiopia. Level of education, occupation, mode of admission, ANC contact, and family history of hypertension were significant predictors of unfavorable perinatal outcomes. Socio-economic development, improving referral systems, and adequate antenatal care contact are needed to improve unfavorable outcomes. Additionally, antenatal screening and specialized care for high-risk mothers, e.g., those with a family history of hypertension are recommended.
Background
Preeclampsia is a new occurrence of hypertension accompanied by either end-organ failure or proteinuria following 20 weeks of gestation, during pregnancy, delivery, or the postpartum period (1). It is most likely caused by a combination of maternal and fetal/placental factors. Early in pregnancy, abnormalities in the placental vasculature may cause relative placental hypoxia, ischemia, or under-perfusion (2). This, in turn, may trigger the release of antiangiogenic factors into the mother's circulation, which modifies the function of the mother's systemic endothelium and results in hypertension as well as other disease manifestations (hematologic, neurologic, cardiac, pulmonary, renal, and hepatic dysfunction) (3). The cause of aberrant placental development and the series of events that follow, however, is yet unknown (4).
In high-income nations, preeclampsia complicates between 3% and 5% of pregnancies (5). In Africa, five to ten percent of pregnancies are affected with hypertensive disorders during pregnancy (6). According to a study conducted in Zanzibar, 26.3% of mothers had preeclampsia with severe features (PEWSF) (7). A systematic review and meta-analysis study found that the pooled prevalence of preeclampsia in Ethiopia is 11.5% (8). Furthermore, a prospective observational study conducted at Saint Paul's Hospital Millennium Medical College in Ethiopia found 19.5% of cases of preeclampsia with severe features (9).
In the USA, 12% of pregnancies complicated by preeclampsia with severe features resulted in adverse newborn outcomes (10). Besides, in Nigeria, 63.5% of preeclamptic mothers have unfavorable perinatal outcomes (11). Women in Southern Ethiopia with severe features of preeclampsia had a 46% higher risk of unfavorable perinatal outcomes (12). The proportion of adverse perinatal outcomes of severe preeclampsia in Ethiopian referral hospitals was found to be 46.6% (13). Additionally, about 66.4% of mothers with PEWSF in Addis Ababa, Ethiopia, experienced at least one neonatal complication (14).
Because of the progressive nature of the disease and the lack of a recognized medical treatment, delivery is the proven treatment, yet when to deliver is a topic of discussion for both preterm and term gestations (15). Prolonging pregnancy increases the chance of aggravating the mother's endothelial dysfunction and maintaining insufficient blood flow to the target organs, which can cause major harm to the brain, liver, kidneys, placenta/fetus, hematologic, and vascular systems (1). As a result, pregnant women with preeclampsia had a greater chance of premature birth (67.7%) (16). In the USA, preeclampsia also decreased the gestational age at delivery by nearly two weeks (17). Stillbirth, respiratory distress syndrome, intrauterine growth restriction, low birth weight, birth asphyxia, and admission to the intensive care unit are also possible consequences for neonates (14, 18). Additionally, a lifelong risk of hypertension and chronic renal disease was reported for both the mother and child (19). Children and adults born to preeclamptic women are more likely to experience mental health disorders and cognitive impairments (20). Further, hypertensive disorders of pregnancy significantly contributed to postpartum maternal deaths (21).
A study in Ethiopian Referral Hospitals identified the risk factors strongly associated with unfavorable perinatal outcomes as educational status, parity, gestational age, and time of drug given to the mother (13). The estimated gestational age at admission, mode of delivery, and severity of the disease had also a positive association with unfavorable perinatal outcomes (11). Further, educational status, maternal parity, history of ANC follow-up, having preeclampsia and eclampsia, and late provision of drugs, e.g., antihypertensive, anticonvulsant, and corticosteroid were the independent factors significantly associated with adverse perinatal outcomes (22).
Following the World Health Organization, the Ethiopian government has made efforts to curb the high burden of perinatal death by putting in place various measures at both facility and community levels. The key interventions were preventing or treating the primary causes of neonatal and child mortality, such as providing essential immunizations, treating and preventing malaria, and vitamin A supplementation, encouraging institutional delivery, offering 24-h maternity services, including ambulance access, spacing births, increasing the use of family planning, educating health extension workers, encouraging early and exclusive breastfeeding, and enhancing socioeconomic conditions (23). Moreover, Ethiopia recently switched to the new ANC eight-contact model from the outdated four-visit targeted prenatal care (ANC) approach (24). In Ethiopia, there was a notable reduction in under-5 and infant mortality (decreased from 123 to 77 per 1,000 live births in 2005 to 59 and 47, respectively, in 2019. However, there have been no significant reductions in perinatal mortality since 2016 (33 deaths per 1,000 live births in 2016 and 2019) (25). Globally, 500,000 babies dies from the preeclampsia each year (26). A prospective cohort study conducted in Southern Ethiopia also found that preeclampsia contributed to higher rates of early neonatal deaths (12). Worldwide perinatal mortality from severe preeclampsia/eclampsia continues to rise despite intense efforts to minimize pregnancy-related complications and mortalities (11, 14).
Few studies have been conducted to date on the adverse perinatal outcomes among pregnant women with preeclampsia with severe features in underdeveloped nations, such as Ethiopia. The finding could have its own slight share in achieving the target set at the local [Ethiopian Health Sector Transformation Plan-II (HSTP-II)] targeted to lower newborn mortality from 33 to 21 per 1,000 live births by 2025 (27) and global level [Sustainable Development Goal (SDG)] target plans to reduce the global neonatal mortality rate to at least as low as 12 per 1,000 live births by 2030 (28, 29). Thus, the study aimed to determine the prevalence and determinants of adverse perinatal outcomes among mothers of preeclampsia with severe features in Ethiopia.
Methods
Study design, setting, and period
A prospective cross-sectional study was carried out in Addis Ababa, the capital city of Ethiopia, from January 1, 2023, to July 30, 2023, at Abebech Gobena Mothers and Childrens Health (MCH) and St. Peter's Specialized Hospital. One of the tertiary referral hospitals directly under the Addis Ababa Health Bureau is Abebech Gobena MCH Hospital. It serves as a teaching hospital for Yekatit 12 Hospital Medical College as well. Every year, the hospital treats about 200,000 patients who were referred by roughly 18 primary hospitals, as well as catchment health clinics throughout the Oromia regional state and Addis Ababa city. On the other hand, the first tuberculosis (TB) referral hospital in the country was a government establishment called St. Peter's Specialized Hospital. In 1953, the hospital was established. presently serving as a specialist hospital overseen by the Federal Ministry of Health (FMOH), offering care to more than 100,000 patients. Serving 15 catchment health centers and 3 primary hospitals from the Oromia region and Addis Ababa city, the MCH center was founded in 2006 E.C.
Population and eligibility criteria
The source population consisted of all pregnant women diagnosed with preeclampsia severe features in the study area. The study population consisted of mothers who were selected at random and diagnosed with preeclampsia with severe features during the study period. Included were all pregnant women who underwent diagnosis, admission, and management for PEWSF. Mothers who died due to complications from PEWSF and were not giving birth at the study facilities with unclear perinatal outcomes were not included.
Sample size and sampling technique
Using the assumptions of 36% prevalence of unfavorable outcomes in Addis Ababa, Ethiopia (14), 95% confidence interval, 5% marginal error, and 5% non-response rate, the sample size was calculated using OpenEpi Version 3.03 statistical software. Taking into account the final sample size was 372. The total population sampling method was used to choose study participants.
Variables
The dependent variable was the perinatal outcome. The study included several independent variables, such as sociodemographic factors; age, marital status, residence, occupation, educational attainment, and mode of admission. Additionally, medical and reproductive history were examined, including gravidity, parity, history of abortion, and antenatal care (ANC), history of pregnancy-induced hypertension, family history of hypertension, anemia, chronic hypertension, diabetes, and renal disease. Other factors included clinical features and investigations upon admission, such as headache, dizziness, epigastric pain, visual disturbance, nausea and/or vomiting, convulsion, edema, liver function test, urea, creatinine, and urine protein. Finally, obstetric factors were considered, including onset of labor, mode of delivery, neonate's sex, and length of hospitalization.
Definition of terms
Preeclampsia with severe features
Refers to preeclampsia with one of the severity features, such as altered mental status, severe headache, altered cerebral or visual disturbance, hepatic abnormality, renal abnormality, severe blood pressure (≥160/110), thrombocytopenia (platelet count <100,000/μl), and pulmonary edema (1, 5, 14).
Severe headache
A debilitating headache that is “the worst headache I have ever had” or that worsens and doesn't go away even with analgesic treatment (1).
Hepatic abnormality
Severe, ongoing right upper quadrant or epigastric discomfort that is not relieved by medicine and cannot be explained by any other diagnosis or serum transaminase concentration ≥2 times the upper limit of the normal range, or both (1, 14).
Renal abnormality
Serum creatinine concentration doubling in the absence of other renal disease, or progressive renal insufficiency as measured by serum creatinine >1.1 mg/dl [97.2 micromol/L] (1, 14).
Unfavorable perinatal outcome
Newborns who develop at least one perinatal complication of preeclampsia with severe features, i.e., low 5th min APGAR score, need for resuscitation, neonatal intensive care unit admission, stillbirth/ intrauterine fetal death (IUFD), intrauterine growth restriction (IUGR), prematurity, low birth weight (13, 14).
Favorable perinatal outcome
Newborns who did not develop a perinatal complication of preeclampsia with severe features (13, 14).
Data collection tool, procedure, quality control
A pre-tested, structured questionnaire was used to gather data from in-person interviews and a review of the patient's medical record. The survey was modified based on comparable research (11, 13, 14, 16, 18). There were two supervisors and four data collectors on the data collection crew. The supervisors and data collectors received a one-day instruction from the lead investigators regarding the goals, protocols, techniques, and data-gathering tool. To ensure that the questions stuck to their intended purpose, they were translated back and forth between Amharic and English. At Debre Berhan Comprehensive Specialized Hospital, a pre-test was conducted on 5% of the samples, or 19 women, before the actual data collection. Based on the test results, necessary adjustments were made. The lead investigators and supervisors kept a close eye on the data's completeness, consistency, and clarity throughout the collection process.
Data management and analysis
The statistical program Epi-Data version 4.6 was used to enter the data, and SPSS version 26.0 was used for analysis. For quality control, the lead investigator chose a questionnaire at random and cross-checked it with the clinical chart and data that matched. To describe the independent and dependent variables, we used descriptive statistics. The number, frequency, percentage, and comparison of perinatal outcomes were displayed as the results. Tables showed the results of the crosstabs using chi-square testing. An independent predictive analysis of unfavorable perinatal outcomes was conducted using binary logistic regression analysis. The final multivariable logistic regression analysis model contained variables from the bivariable regression analysis that had a p-value of less than 0.25. The goodness-of-fit test developed by Hosmer and Lemeshow was used to assess the model's fitness and the value was 0.75. Additionally, the value for Nagelkerke R square during the final model was 0.36. Adjusted odds ratios (AORs) were used to interpret the strength of the link, with a two-sided 95% confidence interval (CI). A p-value of less than 0.05 was used to declare the significance level.
Ethical approval
Ethical approval was provided by Yekatit 12 Hospital Medical College's Institutional Review Board (Protocol number 128/23). A formal letter of support was sent to the hospitals under scrutiny. The participants voluntarily participated and gave their free and written informed permission. After the information was read, those who were illiterate were requested to thumbprint the consent form. No payment or special privilege was granted to the study subjects for taking part in the study. However, health education regarding the course, complications, and management options of the disease and preconceptional care for any subsequent pregnancies were provided. After data collection was finished, client records were returned to their original location while maintaining confidentiality and anonymity.
Result
Socio-demographic characteristics of participants
There were 348 responders in all, yielding a 93.5% response rate. The mean (±SD) age of participants with favorable and unfavorable perinatal outcomes was 28.15 ± 5.20 and 27.13 ± 5.14, respectively. Of the participants with unfavorable and favorable outcomes, approximately one-third, 70 (34.0%) and 64 (45.1%) had attended secondary education, respectively (p = 0.003). Additionally, 187(90.8%) of those who had unfavorable outcomes and 137 (96.5%) of those who had favorable outcomes were married (Table 1).
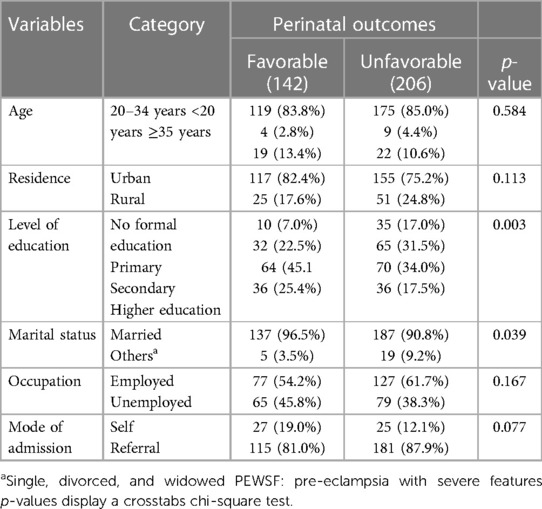
Table 1. Socio-demographic characteristics of mothers admitted with PEWSF at two selected public hospitals in Addis Ababa, Ethiopia, 2023.
Medical and reproductive history
In their most recent pregnancies, 114 (80.3%) of the women with favorable perinatal outcomes and 138 (67.0%) of the women with unfavorable outcomes received four to six antenatal care contacts (p = 0.000). The majority of women who had favorable outcomes, 138 (97.2%), and unfavorable outcomes, 188 (91.3%), gave birth to single kids (p = 0.019). Furthermore, a family history of hypertension was present in 18 (12.7%) of mothers with favorable outcomes and 52 (25.2%) with unfavorable outcomes (p = 0.004) (Table 2).
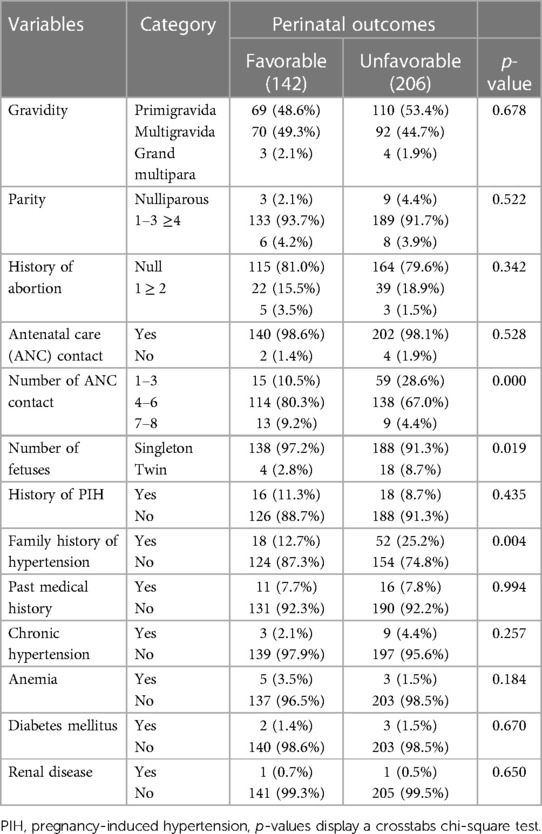
Table 2. Medical and reproductive history of mothers admitted with PEWSF at two selected public hospitals in Addis Ababa, Ethiopia, 2023.
Clinical features and investigations on admission
About 63 (44.4%) of mothers with favorable and 117 (56.8%) unfavorable outcomes were admitted with a chief complaint of headache (p = 0.023). Most mothers with favorable, 112 (78.9%), and unfavorable outcomes, 185 (89.8%), had a severe blood pressure reading at admission (p = 0.005). Additionally, labor was induced in 86 (60.6%) of mothers with favorable and 158 (76.7%) unfavorable outcomes (p = 0.001). Further, on an investigation, 34 (16.5%), 22 (10.7%), 23 (11.2%), and 152 (73.8%) of mothers with unfavorable outcomes had deranged liver function test (p = 0.000), urea (p = 0.004), creatinine (p = 0.021), and urine protein on admission (p = 0.004), respectively (Table 3).
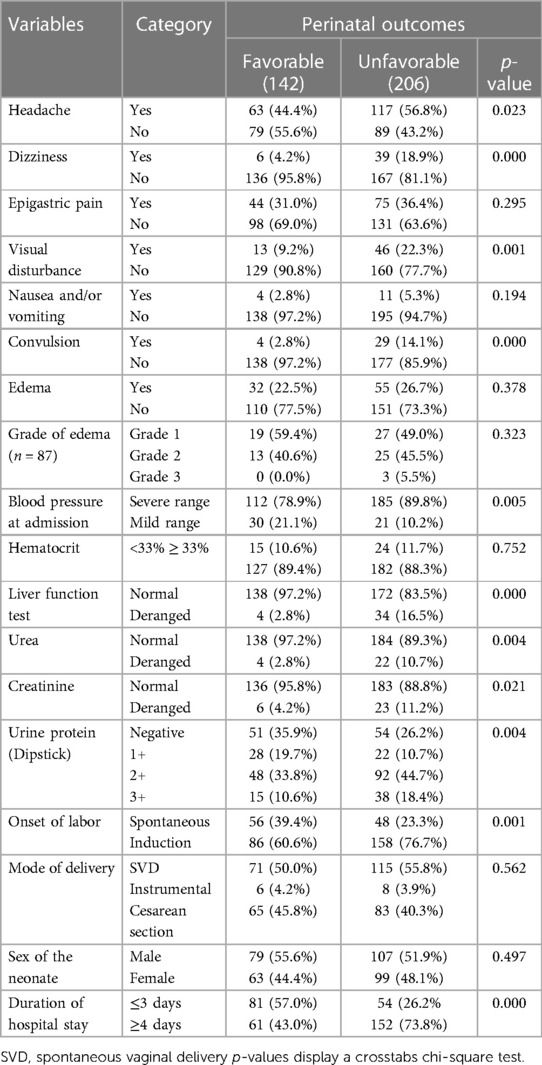
Table 3. Clinical features of mothers admitted with PEWSF at two selected public hospitals in Addis Ababa, Ethiopia, 2023.
Perinatal outcomes
The overall prevalence of unfavorable perinatal outcomes was 59.2% (N = 206) (95% CI: 54.0–63.8). Low birth weight 170/348 (48.9%), preterm 137/348 (39.4%), NICU hospitalization 71/348 (20.4%), and low fifth-min APGAR score 51/348 (14.7%) were frequently occurred unfavorable perinatal outcomes (Figure 1).
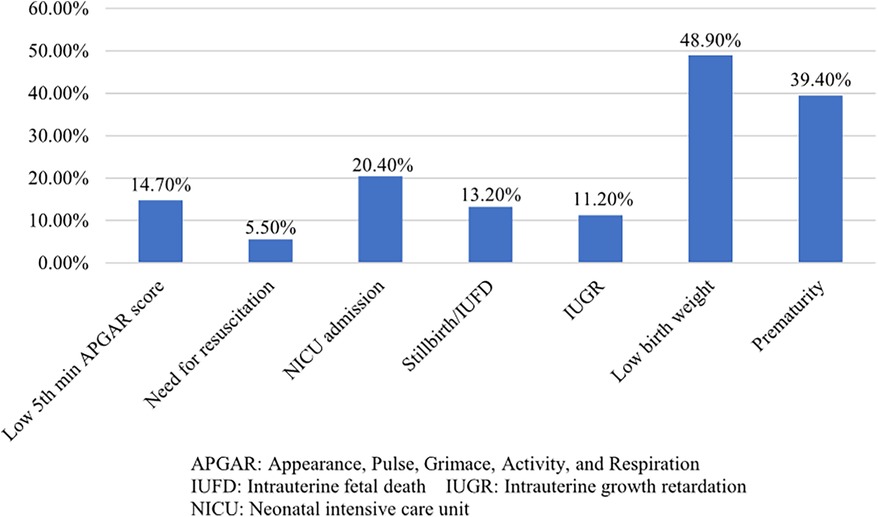
Figure 1. Adverse perinatal outcomes of mothers admitted with PEWSF at two selected public hospitals in Addis Ababa, Ethiopia, 2023.
Factors of unfavorable perinatal outcome
Bivariable logistic regression analysis was computed, and variables with a p-value of ≤0.25 were selected for the multivariable logistic regression analysis model. Accordingly, residence, level of education, marital status, occupation, mode of admission, number of ANC contacts, number of fetuses, and family history of hypertension were selected. In the final model, level of education, occupation, mode of admission, number of ANC contacts, and family history of hypertension have shown a statistically significant association with unfavorable perinatal outcomes.
Mothers who didn't attend formal education were five times more likely to develop unfavorable perinatal outcomes compared to those who attended higher education [OR = 5.14, 95% CI: (1.93–13.63)]. The odds of unfavorable perinatal outcomes were lower among unemployed mothers than the employed [OR = 0.42, 95% CI: (0.24–0.73). Unfavorable perinatal outcomes were two times more common among referred cases than self-admitted [OR = 2.03, 95% CI: (1.08–4.06)]. Mothers who have only 1–3 Antenatal care (ANC) contact were three times more likely to have unfavorable perinatal outcomes compared to those who have 7–8 contact [OR = 3.63, 95% CI: (1.22–10.71)]. Further, a family history of hypertension significantly increased the risk of unfavorable perinatal outcomes by approximately twofold [OR = 1.99, 95% CI: (1.03–3.85)] (Table 4).
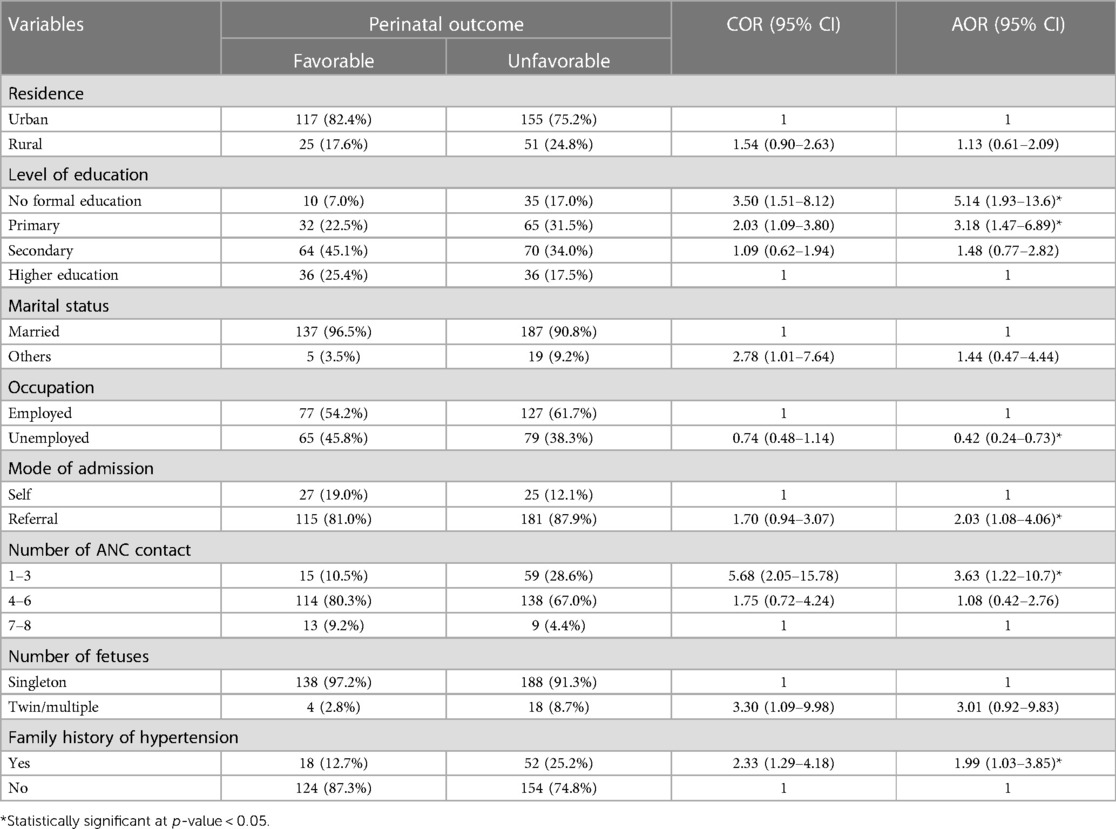
Table 4. Factors associated with unfavorable perinatal outcome among mothers admitted with PEWSF at two selected public hospitals in Addis Ababa, Ethiopia, 2023.
Discussion
The overall prevalence of unfavorable perinatal outcomes was 59.2% (95% CI: 54.0–63.8). Level of education, occupation, mode of admission, number of ANC contacts, and family history of hypertension have shown a statistically significant association with unfavorable perinatal outcomes. Low birth weight (48.9%), preterm (39.4%), NICU hospitalization (20.4%), and low fifth-minute APGAR score (14.7%) were frequently occurred unfavorable birth outcomes.
Unfavorable perinatal outcomes occurred in 59.2% of mothers with preeclampsia with severe features. This is comparable with the study findings from Nigeria, where 63.5% of preeclamptic mothers have unfavorable perinatal outcomes (11). However, it was higher than 46.6% in Ethiopian referral hospitals (13). Variations in the research population, time, setup, sample size, and the caliber and standard of care offered by modern, well-equipped maternity hospitals, together with competent prenatal and obstetric care, could account for this disparity. On the other hand, this was lower than 66.4% in Addis Ababa, Ethiopia (14). Variations in the severity of the disease, variations in clinical features (severity signs and symptoms) at admission, study period, and gestational age at diagnosis could be the cause of variations in the incidence proportion of adverse outcomes between the studies. These results suggest that women with PEWSF in particular require greater improvements in the utilization and access to maternity services. This should be used in conjunction with adequate service delivery and early case detection and management to minimize unfavorable prenatal outcomes.
Mothers who didn't attend formal education were five times more likely to develop unfavorable perinatal outcomes compared to those who attended higher education. Socioeconomic conditions have also been recognized by the national policy as a critical area for reform (30). This is consistent with a study conducted in Amhara region referral hospitals (13), which found that babies delivered to mothers with low educational attainment were more likely to experience adverse perinatal outcomes. The possible reason could be attributed to the fact that mothers with higher educational status are more likely to enhance their health care-seeking behaviors, including having adequate antenatal care, which can lead to improved perinatal outcomes. Additionally, educated mothers may also be exposed to more health education messages and campaigns, enabling them to identify potential problems and danger indicators, and take the necessary precautions during pregnancy. To overcome this challenge, Ethiopia launched a health extension program in 2003 to promote preventive health actions including health education and awareness creation straight to the homes at the local level (30, 31). But more effort needs to be made at the community level.
Compared to working mothers, unemployed mothers were less likely to have negative outcomes. In the Netherlands, the mean birth weight of children dropped by 45 g when working mothers put in more hours (≥40 h/week) (32). Similarly, employed women in South Korea (33) had greater rates of stillbirths and early miscarriages. One explanation could be that women without jobs are more likely to have the time to take care of themselves and tune in to the latest information about pregnancy-induced hypertension on the radio, television, or other media. This could perhaps mitigate the likelihood of adverse consequences for them. In general, this result suggests that setting adequate time for self-care and adhering to health recommendations is important to reduce adverse perinatal outcomes.
According to this study, a woman's admittance status significantly influenced her perinatal outcome. Referred cases were twice as likely to have unfavorable perinatal outcomes as self-admitted ones. Similarly, a prospective study conducted in Zimbabwe examined the results of pregnancy-related referrals from rural health facilities. It found that there were nine maternal deaths, a 4.4% case fatality rate, and 151 perinatal mortality rates per 1,000 live births (34). Additionally, it was found that referral systems greatly increase the risk of maternal death in Ethiopia (35, 36). Most of the referred cases might have potentially complicated cases involving the central nervous system, coma or loss of consciousness lasting 12 h or more; metabolic coma (consciousness loss and urine containing ketoacids and glucose); stroke, status epilepticus, involuntary convulsions, or complete paralysis. In most cases, these abnormalities lead to unfavorable events. It could also be due to delayed referrals, inadequate early diagnosis of potentially life-threatening complications, lack of transportation, or being too far away from referral facilities (second delay). Overall, the finding implied that coordinated effort is needed to enhance the referral system including 24-h ambulance services and availing essential drugs and supplies to improve both maternal and perinatal outcomes.
Mothers who have only 1–3 Antenatal care (ANC) contacts were three times more likely to experience unfavorable perinatal events compared to those who have 7–8 contacts. Ethiopia is tackling significant health sector issues, such as low health service utilization and a lack of human resources for health, by implementing the novel Health Extension Programme (HEP), accelerating midwifery training, Integrated Emergency Surgery and Obstetrics task shifting, and expanding family planning (30). To provide a basic package of preventive and limited curative health care, including maternity and child health services, in urban, rural, and pastoral areas, the HEP trains health extension workers (23). To improve access to necessary services, the HEP has trained and deployed about 38,000 health workers, and about 16,000 health posts and 3,000 health centers have been built (30, 37). In Southeast Ethiopia (22), a similar finding was observed: women who skipped ANC follow-up were more likely to have adverse outcomes. In northern Ethiopia, lack of ANC significantly affected perinatal outcomes (38). Furthermore, a different study conducted in Ethiopia discovered that receiving optimal prenatal care could save perinatal deaths from cardiovascular and respiratory diseases and add 1 week to intrauterine life (39). Prenatal care follow-up promotes an opportunity for early screening and treatment of hypertensive disorders of pregnancy (HDP) and access to information related to the severity features of HDP. Additionally, mothers who receive prenatal care are more likely to give birth with the assistance of a trained birth attendant, which means that their babies will have access to basic medical treatment and neonatal resuscitation. Therefore, to lower the rate of unfavorable delivery outcomes and meet sustainable development goals, more work needs to be done to improve the quality of prenatal care and mobilize pregnant women to follow the new WHO recommendations for focused ANC treatment.
Further, a family history of hypertension significantly increased the risk of unfavorable perinatal outcomes by approximately twofold. This is comparable with the study done in Zanzibar (7). It revealed that a family history of high blood pressure was a risk factor for severe preeclampsia and adverse pregnancy outcomes. Similarly in Ethiopia, the likelihood of pregnancy-induced hypertension was predicted by a family history of the condition (40, 41). These results suggest that this disease may be caused by both maternal and fetal genes. Therefore, it should be closely monitored during pregnancy as well as in the postpartum period for women with a family history of HDP.
Despite the meticulous execution of our investigation, there are certain limitations. It has the same inability to establish a causal association as cross-sectional studies. Because this study was conducted in referral hospitals, we are unsure of whether these women delayed going to the primary health facilities or if there were delays in referring them. The predictive power of the model might be low given the small Nagelkerke R square value. Additionally, because the study was conducted in a hospital, the perinatal outcome for women who were delivered at home was not evaluated. Furthermore, adverse perinatal outcomes that occur after 24 h following birth are not included in this study.
Conclusion
In this study, the prevalence of unfavorable perinatal outcomes was high compared to other studies in Ethiopia. Level of education, occupation, mode of admission, ANC contact, and family history of hypertension were significant predictors of unfavorable perinatal outcomes. Socio-economic development, improving referral systems, and adequate antenatal care contact are needed to improve unfavorable outcomes. Additionally, antenatal screening and specialized care for high-risk mothers, i.e., those with a family history of hypertension is recommended. Further long-term studies investigating the birth outcomes of women with severe pre-eclampsia symptoms are recommended.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
Ethical approval was provided by Yekatit 12 Hospital Medical College's Institutional Review Board (Protocol number 128/23). The participants provided their written informed consent to participate.
Author contributions
MT: Conceptualization, Data curation, Formal Analysis, Investigation, Methodology, Software, Supervision, Writing – review & editing. WD: Conceptualization, Data curation, Investigation, Methodology, Project administration, Software, Supervision, Validation, Visualization, Writing – original draft. GS: Conceptualization, Data curation, Investigation, Resources, Supervision, Validation, Visualization, Writing – review & editing. GW: Investigation, Methodology, Project administration, Resources, Software, Validation, Visualization, Writing – review & editing. YM: Investigation, Methodology, Resources, Software, Supervision, Visualization, Writing – review & editing. ST: Investigation, Methodology, Resources, Software, Supervision, Validation, Visualization, Writing – review & editing. AE: Conceptualization, Methodology, Project administration, Resources, Software, Supervision, Validation, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
We express our gratitude to Yekatit 12 Hospital Medical College for approving the project's ethical clearance, as well as to the supervisors, data collectors, and study participants for supplying genuine data.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. August P, Sibai BM. Preeclampsia: clinical features and diagnosis. (2017) 22. (UpToDate Accessed December).
2. Bakrania BA, Spradley FT, Drummond HA, LaMarca B, Ryan MJ, Granger JP. Preeclampsia: linking placental ischemia with maternal endothelial and vascular dysfunction. Compr Physiol. (2011) 11(1):1315–49. doi: 10.1002/cphy.c200008
3. Maynard SE, Karumanchi SA. Angiogenic factors and preeclampsia. Semin Nephrol. (2011) 31(1):33–46. doi: 10.1016/j.semnephrol.2010.10.004
4. Calvo JP, Rodríguez YP, Figueroa LQ. Update in preeclampsia. Rev Médica Sinerg. (2020) 5(01):345. doi: 10.31434/rms.v5i1.340
5. Lisonkova S, Bone JN, Muraca GM, Razaz N, Wang LQ, Sabr Y, et al. Incidence and risk factors for severe preeclampsia, hemolysis, elevated liver enzymes, and low platelet count syndrome, and eclampsia at preterm and term gestation: a population-based study. Am J Obstet Gynecol. (2021) 225(5):538–e1. doi: 10.1016/j.ajog.2021.04.261
6. Hutcheon JA, Lisonkova S, Joseph KS. Epidemiology of pre-eclampsia and the other hypertensive disorders of pregnancy. Best Pract Res Clin Obstet Gynaecol. (2011) 25(4):391–403. doi: 10.1016/j.bpobgyn.2011.01.006
7. Machano MM, Joho AA. Prevalence and risk factors associated with severe pre-eclampsia among postpartum women in Zanzibar: a cross-sectional study. BMC Public Health. (2020) 20:1–10. doi: 10.1186/s12889-020-09384-z
8. Kassa BG, Asnkew S, Ayele AD, Nigussie AA, Demilew BC, Mihirete GN. Preeclampsia and its determinants in Ethiopia: a systematic review and meta-analysis. PLoS One. (2023) 18(11):e0287038. doi: 10.1371/journal.pone.0287038
9. Tolu L B, Yigezu E, Urgie T, Feyissa GT. Maternal and perinatal outcome of preeclampsia without severe feature among pregnant women managed at a tertiary referral hospital in urban Ethiopia. PLoS One. (2020) 15(4):e0230638. doi: 10.1371/journal.pone.0230638
10. Venkatesh KK, Strauss RA, Westreich DJ, Thorp JM, Stamilio DM, Grantz KL. Adverse maternal and neonatal outcomes among women with preeclampsia with severe features <34 weeks gestation with versus without comorbidity. Pregnancy Hypertens. (2020) 20:75–82. doi: 10.1016/j.preghy.2020.03.006
11. Irowa O, Ochejele S, Ngwan SD, Ukpabi DE. Determinants of adverse perinatal outcome in preeclampsia at the federal medical centre, makurdi: a cross-sectional study. Int J Reprod Contracept Obstet Gynecol. (2023) 12(8):2349–55. doi: 10.18203/2320-1770.ijrcog20232271
12. Jikamo B, Adefris M, Azale T, Gelaye KA. Incidence of adverse perinatal outcomes and risk factors among women with pre-eclampsia, southern Ethiopia: a prospective open cohort study. BMJ Paediatr Open. (2022) 6(1):e001567. doi: 10.1136/bmjpo-2022-001567
13. Melese MF, Badi MB, Aynalem GL. Perinatal outcomes of severe preeclampsia/eclampsia and associated factors among mothers admitted in amhara region referral hospitals, north west Ethiopia, 2018. BMC Res Notes. (2019) 12:1–6. doi: 10.1186/s13104-019-4161-z
14. Wagnew M, Dessalegn M, Worku A, Nyagero J. Trends of preeclampsia/eclampsia and maternal and neonatal outcomes among women delivering in Addis Ababa selected government hospitals, Ethiopia: a retrospective cross-sectional study. Pan Afr Med J. (2016) 25(Suppl 2):1–5. doi: 10.11604/pamj.supp.2016.25.2.9716
15. Phipps EA, Thadhani R, Benzing T, Karumanchi SA. Pre-eclampsia: pathogenesis, novel diagnostics and therapies. Nat Rev Nephrol. (2019) 15(5):275–89. doi: 10.1038/s41581-019-0119-6
16. Sutan R, Aminuddin NA, Mahdy ZA. Prevalence, maternal characteristics, and birth outcomes of preeclampsia: a cross-sectional study in a single tertiary healthcare center in greater Kuala Lumpur Malaysia. Front Public Heal. (2022) 10:973271. doi: 10.3389/fpubh.2022.973271
17. Stevens W, Shih T, Incerti D, Ton TGN, Lee HC, Peneva D, et al. Short-term costs of preeclampsia to the United States health care system. Am J Obstet Gynecol. (2017) 217(3):237–48. doi: 10.1016/j.ajog.2017.04.032
18. Kongwattanakul K, Saksiriwuttho P, Chaiyarach S, Thepsuthammarat K. Incidence, characteristics, maternal complications, and perinatal outcomes associated with preeclampsia with severe features and HELLP syndrome. Int J Womens Health. (2018) 10:371–7. doi: 10.2147/IJWH.S168569
19. Turbeville HR, Sasser JM. Preeclampsia beyond pregnancy: long-term consequences for mother and child. Am J Physiol Physiol. (2020) 318(6):F1315–26. doi: 10.1152/ajprenal.00071.2020
20. Tuovinen S, Eriksson JG, Kajantie E, Räikkönen K. Maternal hypertensive pregnancy disorders and cognitive functioning of the offspring: a systematic review. J Am Soc Hypertens. (2014) 8(11):832–47. doi: 10.1016/j.jash.2014.09.005
21. Tesfay N, Tariku R, Zenebe A, Woldeyohannes F. Critical factors associated with postpartum maternal death in Ethiopia. PLoS One. (2022) 17(6):e0270495. doi: 10.1371/journal.pone.0270495
22. Amare M, Olani A, Hassen H, Jiregna B, Getachew N, Belina S. Perinatal outcomes and associated factors among women with hypertensive disorders of pregnancy delivered in Jimma zone hospitals, southwest Ethiopia. Ethiop J Health Sci. (2021) 31(6):1145–54. doi: 10.4314/ejhs.v31i6.9
24. Organization WH. Who Recommendations on Antenatal Care for a Positive Pregnancy Experience. World Health Organization (2016).
25. ICF EPHI (EPHI)[Ethiopia] and Ethiopia Mini Demographic and Health Survey 2019: Key Indicators. Rockville, Maryland, USA: EPHI ICF (2019).
26. Pre-eclampsia: new supplement on monitoring and managing the global health issue|Figo [Internet]. Available online at: https://www.figo.org/news/pre-eclampsia-new-guidelines-monitoring-and-managing-global-health-issue (Cited 2024 Jan 24).
27. (MOH) EM of H. Health Sector Transformation Plan II (HSTP II): 2020/21-2024/25 (2013 EFY-2017 EFY). Addis Ababa, Ethiopia: MOH (2021).
28. Hug L, Mishra A, Lee S, You D, Moran A, Strong KL, et al. A Neglected Tragedy the Global Burden of Stillbirths: Report of the un Inter-Agency Group for Child Mortality Estimation, 2020. London: UNICEF, WHO, UN, and World Bank Groups (2020).
29. Tefera YG, Ayele AA. Newborns and under-5 mortality in Ethiopia: the necessity to revitalize partnership in post-COVID-19 era to meet the SDG targets. J Prim Care Community Health. (2021) 12:2150132721996889. doi: 10.1177/2150132721996889
30. World Health Organization (WHO). Success Factors for Womens’s and Children’s Health. Ethiopia: World Health Organization (WHO) (2015).
31. Assefa Y, Gelaw YA, Hill PS, Taye BW, Van Damme W. Community health extension program of Ethiopia, 2003–2018: successes and challenges toward universal coverage for primary healthcare services. Global Health. (2019) 15:1–11. doi: 10.1186/s12992-018-0425-y
32. Jansen PW, Tiemeier H, Verhulst FC, Burdorf A, Jaddoe VWV, Hofman A, et al. Employment status and the risk of pregnancy complications: the generation R study. Occup Environ Med. (2010) 67(6):387–94. doi: 10.1136/oem.2009.046300
33. Kim C-B, Choe S-A, Kim T, Kim M-H, Ryu J, Oh J-W, et al. Risk of adverse pregnancy outcomes by maternal occupational status: a national population-based study in South Korea. J Occup Health. (2023) 65(1):e12380. doi: 10.1002/1348-9585.12380
34. Busumani W, Mundagowa PT. Outcomes of pregnancy-related referrals from rural health facilities to two central hospitals in Harare, Zimbabwe: a prospective descriptive study. BMC Health Serv Res. (2021) 21(1):1–11. doi: 10.1186/s12913-021-06289-4
35. Tesfay N, Tariku R, Zenebe A, Mohammed F, Woldeyohannes F. Area of focus to handle delays related to maternal death in Ethiopia. PLoS One. (2022) 17(9):e0274909.36121828
36. Teshome HN, Ayele ET, Hailemeskel S, Yimer O, Mulu GB, Tadese M. Determinants of maternal near-miss among women admitted to public hospitals in north Shewa zone, Ethiopia: a case-control study. Front Public Heal. (2022) 10:996885. doi: 10.3389/fpubh.2022.996885
37. Maternal, neonatal and child health|Ethiopia|U.S. Agency for International Development [Internet]. Available online at: https://www.usaid.gov/ethiopia/global-health/maternal-and-child-health (Cited 2021 Sep 30).
38. Tadese M, Tessema SD, Taye BT. Adverse perinatal outcomes among grand multiparous and low multiparous women and its associated factors in north Shewa zone public hospitals: the role of parity. Int J Gen Med. (2021) 14:6539. doi: 10.2147/IJGM.S333033
39. Tesfay N, Hailu G, Woldeyohannes F. Effect of optimal antenatal care on maternal and perinatal health in Ethiopia. Front Pediatr. (2023) 11:1120979. doi: 10.3389/fped.2023.1120979
40. Gudeta TA, Regassa TM. Pregnancy induced hypertension and associated factors among women attending delivery service at Mizan-Tepi university teaching hospital, Tepi general hospital and Gebretsadik Shawo hospital, southwest, Ethiopia. Ethiop J Health Sci. (2019) 29(1). doi: 10.4314/ejhs.v29i1.4
Keywords: preeclampsia, preeclampsia with severe features, perinatal outcomes, factors, Ethiopia
Citation: Tadese M, Damesa WA, Solomon GS, Fitie GW, Mitiku YM, Tessema SD and Endale A (2024) Prevalence and determinants of adverse perinatal outcomes of preeclampsia with severe features at two selected public hospitals in Addis Ababa, Ethiopia. Front. Pediatr. 12:1345055. doi: 10.3389/fped.2024.1345055
Received: 1 December 2023; Accepted: 29 January 2024;
Published: 8 February 2024.
Edited by:
David Warburton, Children’s Hospital Los Angeles, United StatesReviewed by:
Neamin Tesfay, Ethiopian Public Health Institute, EthiopiaJargalsaikhan Badarch, Mongolian National University of Medical Sciences, Mongolia
© 2024 Tadese, Damesa, Solomon, Fitie, Mitiku, Tessema and Endale. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Mesfin Tadese bWVzaXRhZDAzMUBnbWFpbC5jb20=
Abbreviations HDP, pregnancy induced hypertension; IUFD, intrauterine fetal death; IUGR, intrauterine growth retardation; MCH, maternal and child health; PEWSF, preeclampsia with severe features; PIH, pregnancy induced hypertension.
†ORCID Mesfin Tadese orcid.org/0000-0001-6288-9771
 Mesfin Tadese
Mesfin Tadese Wogene Asefa Damesa2
Wogene Asefa Damesa2 Girma Wogie Fitie
Girma Wogie Fitie Yohannes Moges Mitiku
Yohannes Moges Mitiku Saba Desta Tessema
Saba Desta Tessema Agizew Endale
Agizew Endale