
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Pediatr. , 26 July 2024
Sec. Pediatric Orthopedics
Volume 12 - 2024 | https://doi.org/10.3389/fped.2024.1343162
Introduction: The influence of excess weight on the development of children's feet remains a subject of debate. To further elucidate whether this relation occurs, this study compared arch morphology and flexibility in three groups of children: underweight, normal, and overweight.
Methods: In total, 1,532 children (807 boys, 725 girls; age range 7–11 years) participated in the study. The researchers measured the participants’ height and weight, calculated their body mass index, and categorized their weight status as underweight, normal weight, or overweight. A three-dimensional foot model was taken using a three-dimensional plantar scanner under non-weight-bearing and weight-bearing conditions to obtain arch morphometric indices (arch index and arch volume) and arch flexibility index (arch volume index).
Results: Analysis of the data showed that the arch index was higher in overweight children compared to underweight and normal weight children (p < 0.05), but the differences in arch volume and arch volume index in overweight children compared to underweight and normal weight children were not statistically significant (p > 0.05). All children were divided into flatfoot, normal, and pes cavus groups according to arch index, and the arch volume index was statistically significant (p < 0.01).
Conclusions: Overweight was not absolutely associated with arch structure and arch flexibility in children from a three-dimensional perspective. Arch development is a long-term process, and it is not clear whether being overweight has an effect on soft tissue or bone formation. Future studies will focus on the effects of long-term overweight on foot structure and arch flexibility in children.
There has been a global surge in obesity across various age groups (1, 2). Excess weight can lead to a range of adverse consequences, including affecting biomechanical changes in the lower limbs (e.g., alignment and structure of the hip, knee, and foot), which are associated with impaired mobility and reduced levels of physical activity (3, 4). Obesity, especially during childhood development, can lead to more serious consequences. According to the World Health Organization, approximately 10% of school-age children aged 5–17 years are overweight, of whom 3% are obese. Considering that the foot is particularly vulnerable to excess weight gain, and that children and adolescents are an important period of physical development (5), children with overweight or obesity may be at increased risk of musculoskeletal problems such as flatfeet. Therefore, the effect of excess weight on the foot structure of children should be a key concern.
To date, the effects of overweight on foot development in children remain controversial, although many studies have been published on the effects of overweight on foot structure in different age groups. Riddiford-Harland et al. found that the Chippaux-Smirak index was higher in obese children compared to their normal-weight peers, indicating a reduction in longitudinal foot arches (5). The correlation between increased body mass index (BMI), foot pain, and flatfeet were found in children and adolescents (6), as well as in adults (7). Mauch et al. (8) found significant differences in BMI and foot type. However, in contrast to all the above research, Evans (9, 10) did not find a positive correlation between increased body weight and flatfoot. As the arch is an elastic and variable three-dimensional (3D) structure, the two-dimensional metrics used in previous studies do not provide complete information, and these contradictory conclusions should be attributed to the lack of an accurate test method to fully represent its properties. On the other hand, radiographs are commonly used to diagnose foot types in adults, but applying them to children carries radiation risks, and incomplete ossification makes it difficult to obtain actual arch features in children. A more accurate indicator of morphology and flexibility is needed to reflect the relationship between body weight and arch morphology.
The arch volume (Va) formed by the projection of the arch surface onto the supporting surface is a new method to reflect the dynamic changes of medial longitudinal arch (MLA) (11–13). Zhao et al. (14) demonstrated that arch volume offers significant advantages in describing morphological alterations of the arch under varying weight-bearing conditions. Overweight may adversely affect the development of children, yet existing tests are difficult to fully characterize the arch and radiographs are not suitable for children. The three-dimensional index Va can better characterize the development of MLA in children, and thanks to Va, we can also obtain the flexibility of the foot arch. The arch volume index (AVI) can also be calculated from arch volume under the non-weight-bearing and weight-bearing arches (11). AVI can represent not only arch flexibility, but the change in mechanical energy due to arch deformation as well. Previous research indicates arch flexibility may be a meaningful description of the relationship between foot structure and foot function (15). Further understanding of arch volume and morphological changes in children with overweight is important to advance the debate on the effects of overweight on arch structure and to develop appropriate three-dimensional clinical measures. Thus, this study aims to explore the connection between excess weight and three-dimensional morphology and flexibility in children.
In this study, foot parameters, such as the arch index (AI), arch volume, and arch volume index, were compared among three groups of children: underweight, normal weight, and overweight. The primary objective of this research was to examine the association between arch morphology and overweight from a three-dimensional standpoint. In addition, the arch morphology of all children was further categorized into the flatfoot group, normal group, and pes cavus group, allowing for a comparison of the disparities in arch flexibility.
A total of 1,532 children (807 boys, 725 girls; age range 7–11 years) were included in the study. All children aged 7–11 years who had the ability to cooperate independently with the test were included in the study. Children were excluded from study participation if they had a history of lower limb deformity, trauma, surgery, neuromuscular dysfunction, or inability to stand independently. In total, 107 children were excluded from the study on the basis of these criteria. The sex and age of the children were recorded. Height and weight were measured without shoes, from which BMI was calculated. According to BMI, they were divided into three categories: underweight, normal, and overweight.
In the non-weight-bearing position, children participating in the trial were placed in a height-adjustable seat with the hip and knee joints held at 90° of flexion and the ankle joints in a neutral position. During measurement in the weight-bearing position, participants stood naturally and kept the following landmarks aligned, including the acromion, hip center, knee center, and lateral malleolus.
The “Foot Secret 3D Foot Plantar Scanner” produced by China Shanqi (Chongqing) Wisdom Medical Technology Co., Ltd., was used for 3D foot contour scanning. The scanner used active stereo 3D technology and white light mode projection. Therefore, it is safe for participants’ eyes and can be used in the absence of protective glasses. Referring to the method of Zhao et al. (14), each foot was scanned three times by the “foot Secret 3D Plantar Scanner” in both non-weight-bearing and weight-bearing positions. All scanned feet were placed with the second toe of the foot aligned with the laser axis of the platform. A three-dimensional model of the foot was obtained after scanning, and the AI and Va were obtained from the three-dimensional model. The AI calculated the ratio of the area of the middle third of the footprint to the entire footprint area (16). The Va represents that the arch plane projecting to the supporting surface then formed the volume of the foot arch (11) (Figure 1). The method proposed by Chang et al. (12) was used to calculate the AVI based on the difference in arch volume between non-weight-bearing and weight-bearing conditions, which was calculated as .
The data obtained with the 3D scanner were analyzed using SPSS Software version 19 for Windows (IBM Corp., Armonk, NY, USA), with a significance level of p < 0.05. Descriptive statistics (mean, standard deviation, frequencies) were used to analyze the demographic characteristics of the participants. All data were tested for normality using the Kolmogorov–Smirnov test. Data are presented as mean [standard deviation (SD)] or median [interquartile range (IQR)]. Children were classified according to their weight and arch type, respectively. Differences in characteristics between groups were analyzed using the Kruskal–Wallis test with Bonferroni post-hoc tests.
A total of 1,532 children (807 boys, 725 girls; age range 7–11 years) participated in this study. BMI was calculated using height and weight (BMI = weight/height2). Participants were categorized according to the method by Ma et al. (17), a BMI table based on age and sex. The statistical details of participants are given in Table 1. The proportions of children with underweight, normal weight, and overweight in this study were 8.68% (133 children), 69.26% (1,061 children), and 22.06% (338 children), respectively. There was no significant difference in age between boys (n = 807) and girls (n = 725) (p = 0.636).
Bilateral foot models obtained using three-dimensional scanning imaging were used to evaluate foot type and the calculation of “Arch Index” was consistent with the method introduced by Cavanagh and Rodgers (16). A total of 1,532 children were tested in the study and data for 3,064 feet were obtained. The prevalence of flatfoot, normal, and pes cavus in this study was 39.8% (1,218 feet), 57.1% (1,749 feet), and 3.1% (97 feet), respectively (Table 2).
Individual differences in children's developmental stages are large, and to eliminate errors in foot size, participants were divided into six groups based on foot length in the weight-bearing position and then analyzed for differences between groups with different BMI. Comparing foot parameters by weight category grouping, except for the two groups of 180–190 and 190–200, there were significant differences in AI between overweight children and normal weight children in all four groups (200–210, 210–220, 220–230, and 230–240) (p < 0.05). The data of participants' feet were measured, and the results from descriptive analysis showed that children with overweight had higher arch index in both non-weight bearing and weight bearing positions than children with normal and underweight (Table 3). Thus, overweight children have higher arch index and flatter arches.
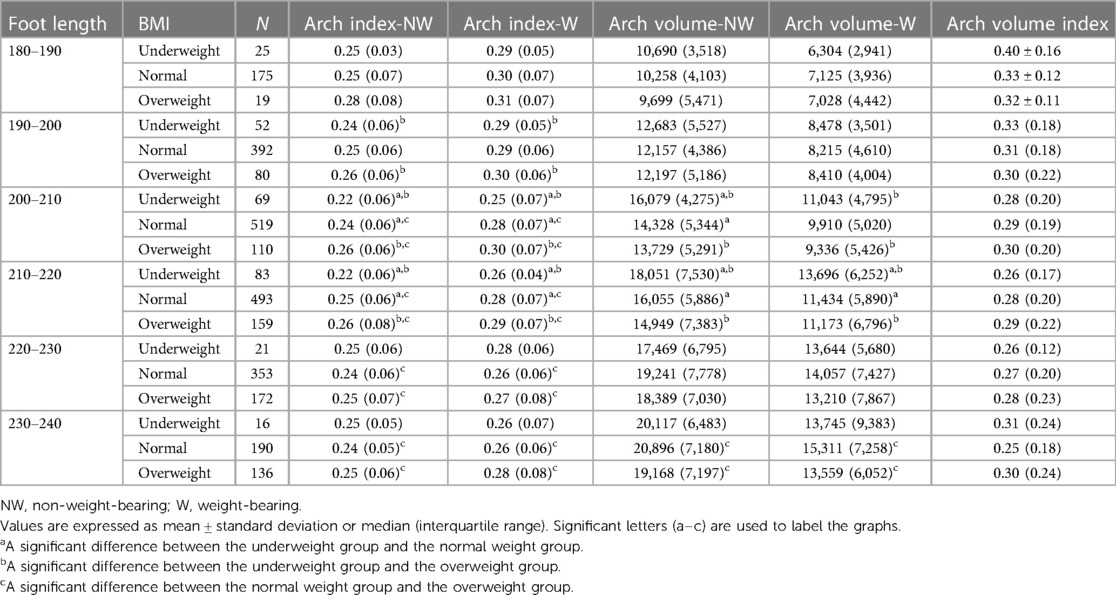
Table 3 Comparative results of foot parameters in underweight, normal weight, and overweight children in each foot length group.
Although Va showed the same trend as AI, its descriptive analysis showed that overweight children had lower Va in both the non-weight-bearing and weight-bearing positions than both normal weight and underweight children. However, with the exception of the 230–240 group, there was no statistically significant difference between the non-weight-bearing Va and weight-bearing Va of the children with overweight and normal weight in the other five groups (p > 0.05). The arch volume results reflect that the arch volume of children with overweight is not necessarily lower than that of children with underweight and normal weight. In addition, the difference in AVI between children with underweight, normal, and overweight was not statistically significant (p > 0.05), suggesting that being overweight also does not necessarily result in reduced arch flexibility in children. The numerical details of these tests can be referenced in Table 3.
Further grouping participants by foot type, there were significant differences in AVI among flatfoot, normal foot, and pes cavus (p < 0.001). The results of the descriptive analysis showed that the AVI of children with flatfeet was higher than that of children with normal and pes cavus (median = 0.39, median = 0.25, median = 0.22, respectively) (Table 4). The data show that the arch volume index increases sequentially for flatfeet, normal feet, and pes cavus, with flatfeet having higher arch flexibility (Figure 2).
The relationship between overweight and foot arch development in children is still controversial because there is no precise testing protocol for foot arches so far due to the individual differences in children's development (18). Following the property that the MLA is a three-dimensional dynamic elastic structure, this study measured, for the first time, foot parameters from two-dimensional (arch index) and three-dimensional perspectives (arch volume) in children aged 7–11 years to determine whether there are differences in the morphology of MLA in overweight children compared to normal weight and underweight children.
The study found that the AI of children with overweight was higher than that of children with normal weight and underweight, and that arch volume showed the same trend of smaller arch volume in children with overweight, which is consistent with previous studies (19, 20). Jankowicz-Szymańska et al. demonstrated that BMI was significantly associated with AI and that excess weight had a greater effect on flatfeet than age (20). Nevertheless, other research presents an ambiguous relationship between excess weight and flatfeet, with Evans failing to identify a positive association between increased body weight and flatfoot (10). On the other hand, the study showed that the prevalence of flatfeet differed from that reported in other studies, with a high prevalence of flatfeet (39.8%) obtained using AI to diagnose foot types. Xu et al. found in a meta-analysis that the detection rate of flatfoot in children in the past 20 years was 25% (21). The prevalence of AI diagnosis of foot type acquisition in children contradicts previous studies, which may be due to the fact that AI is mainly used in adults and the large individual differences in child development may lead to false-positive results in AI-diagnosed foot type. Foot development in children is based on three-dimensional structures, with a focus on the development of morphology and arch flexibility. Va as a three-dimensional index can clearly characterize the developmental trend of foot morphology, and the change of Va in non-weight-bearing and weight-bearing positions can also characterize the arch flexibility of children. The measurement of Va and arch flexibility is useful for further diagnosis and typing of the child's foot.
The relationship between overweight and changes in foot arch morphology was further determined from a three-dimensional perspective. Based on the three-dimensional characteristics of the plantar model, the Va allows visualization of the arch shape and its changes. Changes in arch morphology (i.e., differences in Va) between non-weight-bearing and weight-bearing positions can be represented by AVI. The initial findings showed no significant difference in AVI between underweight, normal, and overweight, suggesting that being overweight does not affect foot flexibility for the time being. Foot types were further classified into flatfoot, normal foot, and high arch. Among these, flatfoot is more flexible, which is consistent with the findings of Zifchock et al. (22). Williams et al. (23) found that different degrees of arch flexibility resulted in different lower limb movement patterns and weight-bearing. A clearer understanding of the relationship between flatfoot and clubfoot can help to develop appropriate clinical treatment plans for foot deformities. It also allows a better description of the foot structure, thus enhancing the predictability of the structure for foot function. Arch flexibility is an important indicator to describe the MLA, but there is no accepted method to classify arch flexibility. AVI can be used as an objective index to evaluate the arch flexibility, which can reflect not only the elasticity of the MLA, but also the mechanical energy change caused by the deformation of MLA. It is valuable to further explore arch morphology and arch flexibility through 3D scanning technology to provide an objective basis for clinical development of interventions.
In addition, although studies have shown no differences in arch volume and arch volume index in children with overweight compared to children with normal weight and underweight, there is a tendency to cause flattening of foot development, especially when children (usually at approximately 6 years of age) begin to engage in activities that place significant demands or loads on the musculoskeletal system of the lower extremities. Stovitz et al. showed that children with overweight/obese and adolescents often report foot pain, which is second only to back pain in prevalence (6). Mickle and Steele also reported that obese adults experience altered foot function and foot pain, which has a direct impact on the patient's mobility and quality of life (24). These findings support the theory that increased pressure on soft tissues and joints, which may be directly related to excess body weight, is associated with an increased incidence of foot discomfort and pain. If overweight lasted for a long time, it may lead to weight gain exceeding the tensile capacity of the plantar fascia, resulting in the formation of flatfoot (25–27). Thus, it is reasonable to hypothesize that the mechanical overload generated by the combination of excess mass and weight-bearing may be detrimental, and more specifically able to affect the structure and function of the developing musculoskeletal structures of the foot. Despite the lack of evidence on the long-term consequences of foot overload, it is noteworthy that children with overweight are less inclined to engage in physical activity (28, 29). Children with excess weight in developmental stages should be given weight control and exercise strategies to prevent the negative consequences of being overweight. It is also noteworthy that follow-up studies are needed to determine the long-term effects of overweight on the MLA. This would allow measurement of the actual evolution of foot structure in children with and without overweight. Finally, it is necessary to provide a multidimensional description of foot structure in childhood. Multidimensional description of foot structure requires a classification of arch height and arch flexibility. It will provide a more reliable basis for clinicians to intervene in overweight and arch collapse.
From a three-dimensional perspective, overweight is not unequivocally associated with the structure and flexibility of the medial longitudinal arch in children. The arch volume index as a measurement of dynamic changes in arch morphology deserves further study. Arch development is a long-term process, and it is not clear whether being overweight has an effect on soft tissue or bone formation. Future studies will focus on the effects of long-term overweight on foot structure and arch flexibility in children. Clinically, three-dimensional foot parameters can offer orthopedists and pediatricians a more comprehensive understanding of the foot, thereby enabling them to devise preventive measures and interventions with a holistic consideration of the foot.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving humans were approved by The Ethics Committee of the First Affiliated Hospital of Chongqing Medical University (batch number: 2020-102). The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants’ legal guardians/next of kin.
JC: Conceptualization, Data curation, Investigation, Writing – original draft, Writing – review & editing. LT: Conceptualization, Investigation, Writing – original draft. XY: Formal Analysis, Writing – review & editing. JT: Investigation, Methodology, Writing – review & editing. QC: Resources, Supervision, Writing – review & editing. CZ: Formal Analysis, Project administration, Writing – review & editing. HZ: Supervision, Validation, Writing – review & editing.
The authors declare that no financial support was received for the research, authorship, and/or publication of this article.
We thank all of the participants who so generously gave their time and effort for this work.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fped.2024.1343162/full#supplementary-material
1. Budnik A, Henneberg M. Worldwide increase of obesity is related to the reduced opportunity for natural selection. PLoS One. (2017) 12(1):e0170098. doi: 10.1371/journal.pone.0170098
2. Di Cesare M, Sorić M, Bovet P, Miranda JJ, Bhutta Z, Stevens GA, et al. The epidemiological burden of obesity in childhood: a worldwide epidemic requiring urgent action. BMC Med. (2019) 17(1):212. doi: 10.1186/s12916-019-1449-8
3. Wearing SC, Hennig EM, Byrne NM, Steele JR, Hills AP. The impact of childhood obesity on musculoskeletal form. Obes Rev. (2006) 7(2):209–18. doi: 10.1111/j.1467-789X.2006.00216.x
4. Shultz SP, Anner J, Hills AP. Paediatric obesity, physical activity and the musculoskeletal system. Obes Rev. (2009) 10(5):576–82. doi: 10.1111/j.1467-789X.2009.00587.x
5. Riddiford-Harland DL, Steele JR, Storlien LH. Does obesity influence foot structure in prepubescent children? Int J Obes Relat Metab Disord. (2000) 24(5):541–4. doi: 10.1038/sj.ijo.0801192
6. Stovitz SD, Pardee PE, Vazquez G, Duval S, Schwimmer JB. Musculoskeletal pain in obese children and adolescents. Acta Paediatr. (2008) 97(4):489–93. doi: 10.1111/j.1651-2227.2008.00724.x
7. Butterworth PA, Landorf KB, Gilleard W, Urquhart DM, Menz HB. The association between body composition and foot structure and function: a systematic review. Obes Rev. (2014) 15(4):348–57. doi: 10.1111/obr.12130
8. Mauch M, Grau S, Krauss I, Maiwald C, Horstmann T. Foot morphology of normal, underweight and overweight children. Int J Obes. (2008) 32(7):1068–75. doi: 10.1038/ijo.2008.52
9. Evans AM. The paediatric flat foot and general anthropometry in 140 Australian school children aged 7–10 years. J Foot Ankle Res. (2011) 4(1):12. doi: 10.1186/1757-1146-4-12
10. Evans AM, Karimi L. The relationship between paediatric foot posture and body mass index: do heavier children really have flatter feet? J Foot Ankle Res. (2015) 8:46. doi: 10.1186/s13047-015-0101-x
11. Chang HW, Chieh HF, Lin CJ, Su FC, Tsai MJ. The relationships between foot arch volumes and dynamic plantar pressure during midstance of walking in preschool children. PLoS One. (2014) 9(4):e94535. doi: 10.1371/journal.pone.0094535
12. Chang HW, Lin CJ, Kuo LC, Tsai MJ, Chieh HF, Su FC. Three-dimensional measurement of foot arch in preschool children. Biomed Eng Online. (2012) 11:76. doi: 10.1186/1475-925x-11-76
13. Meneses J, Gharbi T, Cornu JY. Three-dimensional optical high-resolution profiler with a large observation field: foot arch behavior under low static charge studies. Appl Opt. (2002) 41(25):5267–74. doi: 10.1364/ao.41.005267
14. Zhao C, Chen J, Deng Y, Huang W, Ma S, Su S, et al. Arch volume: a new method for medial longitudinal arch measurement. Foot Ankle Surg. (2022) 28(7):962–7. doi: 10.1016/j.fas.2022.01.007
15. Ker RF, Bennett MB, Bibby SR, Kester RC, Alexander RM. The spring in the arch of the human foot. Nature. (1987) 325(7000):147–9. doi: 10.1038/325147a0
16. Cavanagh PR, Rodgers MM. The arch index: a useful measure from footprints. J Biomech. (1987) 20(5):547–51. doi: 10.1016/0021-9290(87)90255-7
17. Ma J, Wang Z, Song Y, Hu P, Zhang B. BMI percentile curves for Chinese children aged 7–18 years, in comparison with the WHO and the US centers for disease control and prevention references. Public Health Nutr. (2010) 13(12):1990–6. doi: 10.1017/s1368980010000492
18. Razeghi M, Batt ME. Foot type classification: a critical review of current methods. Gait Posture. (2002) 15(3):282–91. doi: 10.1016/s0966-6362(01)00151-5
19. Adoración Villarroya M, Manuel Esquivel J, Tomás C, Buenafé A, Moreno L. Foot structure in overweight and obese children. Int J Pediatr Obes. (2008) 3(1):39–45. doi: 10.1080/17477160701520298
20. Jankowicz-Szymańska A, Wódka K, Kołpa M, Mikołajczyk E. Foot longitudinal arches in obese, overweight and normal weight females who differ in age. Homo. (2018) 69(1–2):37–42. doi: 10.1016/j.jchb.2018.03.001
21. Xu L, Gu H, Zhang Y, Sun T, Yu J. Risk factors of flatfoot in children: a systematic review and meta-analysis. Int J Environ Res Public Health. (2022) 19(14):1–13. doi: 10.3390/ijerph19148247
22. Zifchock RA, Theriot C, Hillstrom HJ, Song J, Neary M. The relationship between arch height and arch flexibility (a proposed arch flexibility classification system for the description of multidimensional foot structure). J Am Podiatr Med Assoc. (2017) 107(2):119–23. doi: 10.7547/15-051
23. Williams DS 3rd, Tierney RN, Butler RJ. Increased medial longitudinal arch mobility, lower extremity kinematics, and ground reaction forces in high-arched runners. J Athl Train. (2014) 49(3):290–6. doi: 10.4085/1062-6050-49.3.05
24. Mickle KJ, Steele JR. Obese older adults suffer foot pain and foot-related functional limitation. Gait Posture. (2015) 42(4):442–7. doi: 10.1016/j.gaitpost.2015.07.013
25. Dowling AM, Steele JR, Baur LA. Does obesity influence foot structure and plantar pressure patterns in prepubescent children? Int J Obes Relat Metab Disord. (2001) 25(6):845–52. doi: 10.1038/sj.ijo.0801598
26. Jha DK, Wongkaewpotong J, Chuckpaiwong B. Effect of age and BMI on sonographic findings of plantar fascia. J Foot Ankle Surg. (2023) 62(1):125–8. doi: 10.1053/j.jfas.2022.05.010
27. Macchi M, Spezia M, Elli S, Schiaffini G, Chisari E. Obesity increases the risk of tendinopathy, tendon tear and rupture, and postoperative complications: a systematic review of clinical studies. Clin Orthop Relat Res. (2020) 478(8):1839–47. doi: 10.1097/corr.0000000000001261
28. Riddiford-Harland DL, Steele JR, Cliff DP, Okely AD, Morgan PJ, Jones RA, et al. Lower activity levels are related to higher plantar pressures in overweight children. Med Sci Sports Exercise. (2015) 47(2):357–62. doi: 10.1249/mss.0000000000000403
Keywords: body mass index, overweight, arch index, arch volume, arch flexibility
Citation: Chen J, Tang L, Yang X, Tang J, Cheng Q, Zhao C and Zhang H (2024) A cross-sectional study of medial longitudinal arch development in children with different BMI. Front. Pediatr. 12: 1343162. doi: 10.3389/fped.2024.1343162
Received: 24 November 2023; Accepted: 11 July 2024;
Published: 26 July 2024.
Edited by:
Danilo Leonetti, University of Messina, ItalyReviewed by:
Serap Alsancak, Ankara University, Türkiye© 2024 Chen, Tang, Yang, Tang, Cheng, Zhao and Zhang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Han Zhang, Z3hybXl5emhAMTYzLmNvbQ==; Chen Zhao, bGVjcmF6QHNpbmEuY29t
†These authors have contributed equally to this work and share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.