
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Pediatr., 18 March 2024
Sec. Pediatric Infectious Diseases
Volume 12 - 2024 | https://doi.org/10.3389/fped.2024.1342493
This article is part of the Research TopicPediatric Infectious Diseases and Global Action Plan on AMRView all 8 articles
 Faris S. Alnezary1
Faris S. Alnezary1 Amira R. Alamri1
Amira R. Alamri1 Rafa D. Alrehaili1
Rafa D. Alrehaili1 Dina S. Alnizari1
Dina S. Alnizari1 Fahad Alzahrani1
Fahad Alzahrani1 Mansour Mahmoud1
Mansour Mahmoud1 Masaad S. Almutairi2*
Masaad S. Almutairi2* Amanj Kurdi3,4,5,6,†
Amanj Kurdi3,4,5,6,† Brian Godman3,4*†
Brian Godman3,4*†
Introduction: Diarrhea remains a major global health issue for children under five, contributing substantially to morbidity and mortality. Community pharmacists play a pivotal role in the management of these children; however, their competence in managing childhood diarrhea in Saudi Arabia is under-researched. This is important to ensure optimal patient care.
Method: Simulated patients (SPs) presenting with three pediatric diarrhea scenarios were used to evaluate pharmacists’ practice in terms of their counselling, history taking, over-the-counter (OTC) prescribing, medication instructions, diet/fluid advice, and/or information provision. Pharmacists’ practice was categorized into adequate, less adequate, and poor.
Results: 182 community pharmacists, primarily male and non-Saudi, participated in the study, of which 60% were in chain pharmacies. Only 5% showed adequate practice in currently managing pediatric diarrhea. Of the 182 simulated patient visits, 62% received medication in all three scenarios and 20% were referred to physicians, with 16% of pharmacists failing to provide any form of intervention. The main medications recommended were kaolin (34%), pectin (34%) and metronidazole (11%). While most pharmacists (86%) asked about the patient's identity and age, 15% provided incorrect management information, 16% failed to provide guidance on the prescribed medicines, and 18% dispensed antimicrobials without a valid prescription.
Conclusion: A high level of inadequate management of pediatric diarrhea in Saudi Arabia was observed. This highlights the need for extensive training to improve community pharmacists’ practice in service delivery including providing counselling and advice on the appropriate management of childhood diarrhea. The latter is particularly important to reduce antimicrobial resistance.
Globally, pediatric diarrhea accounts for more than 1.7 billion cases annually and is the second leading cause of mortality in children aged five and below (1). In 2017, pediatric diarrhea was responsible for an estimated 533,768 deaths globally in children under five years of age, giving an estimated mortality rate of 78.4 (70.1–87.1) per 100,000 children (2). Moreover, dehydration caused by diarrhea contributes significantly to approximately 1.5–2.5 million deaths annually among young children (1). Diarrhea is characterized by an increased frequency of defecation, with the stools being excessively soft or watery. The World Health Organization categorizes diarrhea into three clinical types, with acute watery diarrhea being the most common. This type is transient, lasting several hours to a few days, and primarily causes dehydration, along with potential symptoms including nausea, vomiting, fever, weight loss, pale complexion, malaise, and abdominal discomfort (1, 3).
Infectious agents such as viruses, bacteria, and protozoa, often encountered during travel or through contaminated food, are the primary cause of diarrhea. Sudden onset characterizes infection-induced diarrhea, with some antibiotic-associated infections, such as Clostridioides difficile, being potential causes (4, 5). Management strategies aim to identify the root cause of the diarrhea, initiate timely treatment and prevent severe dehydration, malnutrition, and death (6, 7).
Treatment primarily focuses on restoring electrolyte and fluid balance (1, 5). Antidiarrheal medications have proven effective in certain cases among adult patients and older children. Therapeutic options include oral rehydration solution (ORS) and/or zinc supplementation, as well as kaolin, loperamide, and probiotics (1, 8, 9). ORS and/or zinc supplements are widely used to manage dehydration and restore electrolyte balance, reducing the frequency of diarrhea episodes. Kaolin, often used with ORS, aids in water absorption, toxin, and germ removal in the gastrointestinal system. The U.S. Food and Drug Administration advises against using loperamide, an antimotility agent, in infants and children under two because of potential harm (10). Probiotics may also prevent antibiotic-induced diarrhea (11). Severe cases may require referral to a physician based on specific criteria, although mild cases often respond to ORS and/or zinc supplementation (1, 3). Nutrient-rich foods and adequate hydration are also beneficial (1).
Antibiotics are generally not recommended as a first-line treatment for infectious diarrhea, unless there is a specific bacterial infection causing the symptoms (12, 13). A recent study reported that rehydration is the critical treatment for children with acute diarrhea as symptoms usually resolve without antibiotics (14). However, when empirically administered especially if symptoms persist in children with acute bloody diarrhea, studies have found that antibiotic treatment can manage clinical symptoms and reduce the duration of diarrheal illness (12, 15).
Patients with diarrhea who are neglected, or receive insufficient treatment, may encounter complications including increasing morbidity, which negatively impacts on their quality of life. Community pharmacists can intervene effectively at this stage due to their increasing role in preventing and diagnosing childhood diarrhea, providing education and referral services (16). As accessible healthcare providers, they are pivotal in community health, endorsed during the recent COVID-19 pandemic (17, 18). However, there is a currently a lack of knowledge regarding community pharmacists’ management of acute childhood diarrhea in Saudi Arabia. It remains uncertain whether pharmacists are delivering appropriate management or facing challenges in this area. Identified common obstacles include insufficient patient history acquisition, inappropriate medication suggestions including antibiotics, suboptimal consultation practices, and limited public understanding of community pharmacists’ roles (16, 19). There have also been concerns with the dispensing of antibiotics without a prescription without a thorough history, rehydration and other approaches first as well as a referral to a physician if needed. The dispensing of antibiotics without a prescription has reduced appreciably in Saudi Arabia in recent years following the tightening of the regulations, greater monitoring of community pharmacy activities as well as potentially considerable financial penalties for abusing the law forbidding such practices (20). However, we are aware that inappropriate practices can return if over time there is less monitoring of community pharmacy activities coupled with continued pressure from patients to dispense antibiotics without a prescription (21–23). Such pressures were heightened during the recent COVID-19 pandemic in Saudi Arabia (24).
In view of ongoing controversies including the dispensing of antibiotics without a prescription, as well as concerns with the current management of children with diarrhea in this high priority area, we sought to ascertain current advice and management among community pharmacists in Saudi Arabia for the treatment of these children. This is particularly important due to lack of guidelines on this topic in Saudi Arabia coupled with high morbidity and mortality. Consequently, the objective of this study was to assess the practice, proficiency, and willingness of community pharmacists in Saudi Arabia in acquiring essential information and implementing appropriate interventions for managing childhood diarrhea. This includes promoting optimal management including rehydration and not dispensing any antibiotics without a referral and prescription from a physician, building on the earlier study of Merghani Ali et al. (16). Reducing inappropriate dispensing of antibiotics in ambulatory care will reduce antibiotic resistance (AMR) (12, 22).
This study employed a cross-sectional, observational design utilizing a simulated patient (SP) methodology, which is a recognized tool for evaluating community pharmacists’ (CPs) skills and practices in real-world settings (25). Specifically, we employed a covert simulated patient approach, a novel method in observational research. Using simulated patients allows the observation of practitioners’ actual responses to predetermined scenarios (26). Consequently, is seen as a more reliable method to ascertain current practices than self-administered questionnaires (27). The SPs assessed pharmacists’ practice and skills, as well as the quality of their counselling in real-life encounters using predetermined case scenarios, which is similar to the approach of Merghani et al. (16).
The study targeted a convenience sample of community pharmacies in Madinah Province, including both chain and independent pharmacies. This province was chosen for this study as it has a diverse population consisting of people from many countries who come to visit the Prophet's Mosque. In addition, to the best of our knowledge, current practices among community pharmacists towards childhood diarrhea in the province has not been studied before. No specific type of pharmacy was excluded from the study.
The study included all the districts of Madinah, utilizing a simple random selection methodology. The sample size was calculated to be 165 using the Raosoft sample size calculator, based on a 95% confidence interval, a 5% margin of error, an estimated population size of around 288 community pharmacies, and a response distribution of 50% (28). To enhance the statistical significance of the findings, an additional 17 pharmacies were included, resulting in a total sample size of 182. This increased the total number of pharmacists approached allowing for greater confidence and representativeness.
The sampling frame comprised all eligible and accessible community pharmacies in our region. To avoid duplication, any pharmacy branches or outlets belonging to the same parent company were excluded, with only the primary location selected. Each pharmacy could only be visited once across the three case scenarios to prevent re-surveying the same pharmacist.
During the visits, the simulated patients asked for “the pharmacist on duty” without specifying individual practitioners. The simulated patient exclusively interacted with the first pharmacist who they became engaged with, even if others later offered help. Only one pharmacist was assessed per pharmacy to maintain independence of the observations. Details were recorded reflecting the interaction with the pharmacist encountered rather than the whole pharmacy staff.
A team of three pharmacy students from the College of Pharmacy in Taibah University, trained as SPs, visited the community pharmacies in Madinah. The SP acted as a relative for the patient and carried out the simulated scenario. Each participant conducted a total of 60 visits, with 20 visits allocated to each scenario. The overall number of visits, including additional visits, amounted to 182. The SPs were trained to only provide information when specifically asked. The visits began in March 2023 and lasted for over three weeks.
Three hypothetical patient scenarios (Table 1) involving young children diarrhea were developed based on a thorough review of the reference guide “Symptoms in the Pharmacy” (3). The three scenarios were designed to assess different aspects of community pharmacists’ practice in managing childhood diarrhea. This included the ability of community pharmacists to identify patients requiring a physician referral (scenario 1), select appropriate OTC treatments (scenario 2), and provide counseling (scenario 3). Relevant assessment points and questions were incorporated into the scenarios by categorizing information from published literature on key considerations for triaging and advising patients with diarrhea (16, 19).
Case 1 involved an 8-month-old infant boy who had been suffering from watery stools up to 4 times per day that started suddenly yesterday. This simulated case is intended to assess whether the pharmacist makes the appropriate referral to a physician, given medical guidelines stating that all pediatric patients under 1 year of age presenting with diarrhea should be evaluated by a doctor.
Case 2 involved a 5-year-old boy with watery stools ongoing for 2 days. His sibling administered oral rehydration solution from the pharmacy, but diarrhea persisted over 4 times daily. The child exhibits concerning symptoms including paleness, lethargy, weakness, and dry mouth. The sibling returns to the pharmacy seeking additional treatment, providing details if probed. The case assesses whether the pharmacist recognizes the need for doctor referral given signs of dehydration.
Case 3 involves a 3-year-old boy with watery stools for 2 days, starting after returning from daycare. He has had over 2 loose bowel movements daily and seems fatigued, indicating likely infectious diarrhea. No medications have been tried yet. His sibling goes to the pharmacy seeking treatment. If probed, the sibling provides details—no dietary changes and no other family members affected. The case assesses the pharmacist's ability to select appropriate therapy for a young child's probable infectious diarrhea.
To minimize potential biases caused by incomplete information, every visit was thoroughly documented and later transcribed onto a designated form. The form consisted of eight sections: (i) pharmacy information [location and type (independent vs. chain pharmacy)], (ii) pharmacist information (nationality and gender), (iii) history taking, (iv) the treatment(s) dispensed, (v) type of action and advice on suggested treatments, (vi) instructions given about any medicine dispensed, (vii) advice about food and fluid intake and (viii) any additional information.
The research team, experienced in developing pharmacy assessment standards, created specific criteria to evaluate pharmacists’ willingness and attitudes toward consumers via simulated patients. The criteria measured active listening skills, nature/quantity of questions, extent of counseling, professional demeanor, and tone of voice. Active listening was assessed through eye contact, verbal acknowledgements, and clarifying questions. Open/closed-ended questions were quantified. Counseling was evaluated by word count. Pharmacists’ demeanor was subjectively rated on a 3-point scale. Their tone of voice was rated on a 5-point scale for audibility, clarity, pace and warmth.
Pharmacists’ level of interest in assisting the simulated patients was categorized as follows (3-point scale):
• High interest: displayed exceptional engagement through open-ended questions, active listening, detailed explanations, patience, and warm tone. In addition, spent considerable time interacting with the patient.
• Typical interest: addressed the patient politely with medium engagement, asked some close-ended questions, provided a straightforward response, and did not elaborate extensively.
• No/limited interest: appeared detached, impatient, or unwilling to substantially assist the patient. Interaction was brief.
Most criteria were evaluated using a binary scale: yes or no. Another author reviewed the recorded information for each visit and the associated data to add robustness to the subjective assessments.
Standardized forms were created to enable systematic documentation of relevant metrics during the simulated patient encounters. The forms allowed capture of details on history taking, pharmacist questioning, treatment or referrals advised, medication counseling, and adherence to pediatric diarrhea management guidelines.
Simulated patients underwent practice sessions to standardize their presentation and questioning of pharmacists across visits. Completed forms were subsequently reviewed by the study team for completeness, clarity, and correctness.
To minimize inter-rater variability, the same simulated patient completed all encounters for a given case scenario. Visits were scheduled across different times of day over a 3-month period to account for potential variations in pharmacist availability and to prevent detection.
The primary outcome of this study was to assess the practice of community pharmacists in acquiring necessary information and executing appropriate interventions for managing pediatric diarrhea. The practice was determined by a total score of 10 for each of the three assessed primary components: patient assessment, intervention, and professional behavior. The scores for each component were subsequently categorized into three categories: Adequate practice (7–10), Less adequate practice (4–6), and poor practice (<4) in line with previous publications (29).
Secondary outcomes included the frequency of antimicrobial dispensing without a prescription, pharmacists’ willingness to assist the patient, comparison of practices between chain and independent pharmacies, and the potential influence of the pharmacy's geographical location on its practice.
Pharmacies were broken down into chains and independent pharmacies as there can be differences in the extent of dispensing of antibiotics without a prescription depending on the nature of the pharmacy (30).
Descriptive statistics were employed to present the data, and categorical variables were reported as frequency and percentages. To assess the relationship between pharmacist's characteristics and practice categories, the Pearson Chi-Square was applied. The significance level was set at p-value <0.05. The statistical analysis was performed using IBM SPSS software version 25.
This study received ethical approval from the Institutional Research Ethics Committee at Taibah University (Ref number: COPTU-REC-55-20230224), covering all aspects of the research methodology. Throughout the investigation, the anonymity of participating community pharmacists was ensured by having the chief investigator (FSA) assign a number to each one, which was kept securely with password protection.
The majority of the participating pharmacists were male (96.2%, n = 175). In terms of their nationality, an appreciable portion were non-Saudi (85.2%, n = 155). A slightly higher percentage were chain pharmacies (59.9%, n = 109) compared to independent ones (40.1%, n = 73). Most of the pharmacies were located away from Haram (93.4%, n = 170) as opposed to those located close to Haram (6.6%, n = 12). Table 2 explains the demographic characteristics of the study population.
Across all three scenarios, the average percentage of pharmacists demonstrating adequate, less adequate, and poor practice were 5% (n = 9), 63% (n = 115), and 32% (n = 58), respectively. The third scenario had the highest rate of adequate practice at 11% (n = 7), while the first and second cases had lower rates at 2% (n = 1) and 3% (n = 2) respectively. The second scenario resulted in a high percentage of less adequate practice (82%, n = 51) compared to 44% (n = 26) in the first scenario and 62% (n = 38) in the third scenario. Regarding poor practice, the first scenario elicited the highest rate at 54% (n = 32), while the second had the lowest rate at 15% (n = 9). The third scenario exhibited an intermediate level of poor practice at 26% (n = 16) (Figure 1). In summary, the simulated cases revealed variability in pharmacists’ referral and treatment decisions based on the three differing pediatric diarrhea scenarios.
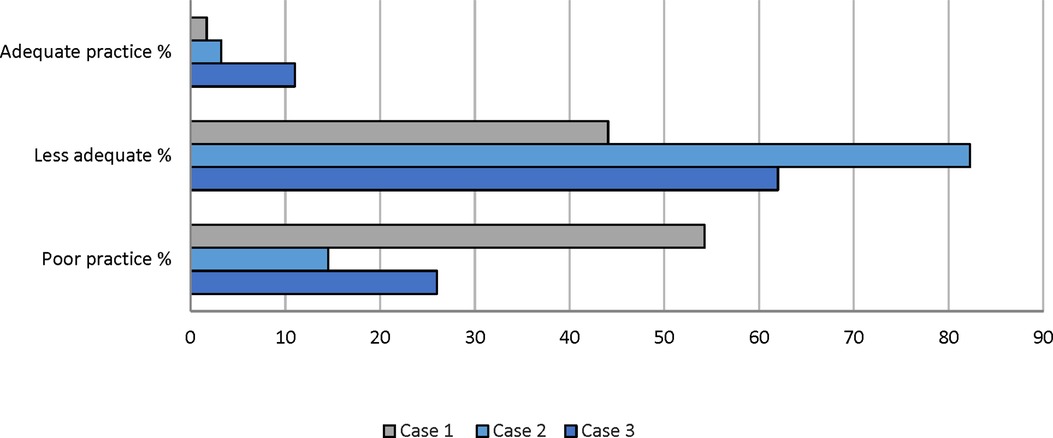
Figure 1. Percentage (%) distribution for assessment of community pharmacists’ practice across all scenarios. Scores were classified into three categories: Adequate practice (7–10), Less adequate practice (4–6), and Poor practice (<4).
Of the 182 simulated patient visits, 62% (n = 113) received medication in all three scenarios. Only 20% (n = 36) of the total cases were referred to physicians for further evaluation. In the total sample of pharmacists, 16% (n = 29) failed to provide any form of intervention such as a recommended treatment or referral, and merely stated that they were out of medication. In a small subset of cases (2%, n = 4), pharmacists recommended medicines and advised patients to seek medical consultation. Furthermore, in the first and third scenarios, only 37% (n = 22) and 8% (n = 5) of the community pharmacists, respectively, made appropriate referrals to physicians. In the second scenario, 32 out of 62 pharmacists failed to provide appropriate therapy for diarrhea (Figure 2).
The main medications recommended were kaolin and pectin (34%, n = 61) as well as metronidazole (11%, n = 20). In 6% (n = 11) of cases, both metronidazole as well as kaolin and pectin were administered along with probiotics. The recommended treatment options among participating pharmacists for all given scenarios are illustrated in Figure 3.
A majority of pharmacists (86%, n = 156) asked about the patient's identity, while 90% (n = 163) asked about the patient's age. A small number of pharmacists (8%, n = 15) provided incorrect information relating to diagnosis or treatment. Of the total sample, 49% (n = 91) did not provide guidance on any medicines dispensed, while 42% (n = 51) gave appropriate counseling. Regarding the ORS, only 37 (20%) of pharmacists recommended its use, and of these, 24 (13%) provided adequate instructions on ORS usage.
18% (n = 33) of pharmacists prescribed antimicrobials without a valid prescription, typically metronidazole (Figure 4). Regarding the pharmacists’ attitude toward customers, most pharmacists 57% (n = 104) showed a typical level of interest when interacting with simulated patients. However, 30% (n = 55) displayed a high level of interest, and 13% (n = 24) showed no interest at all.
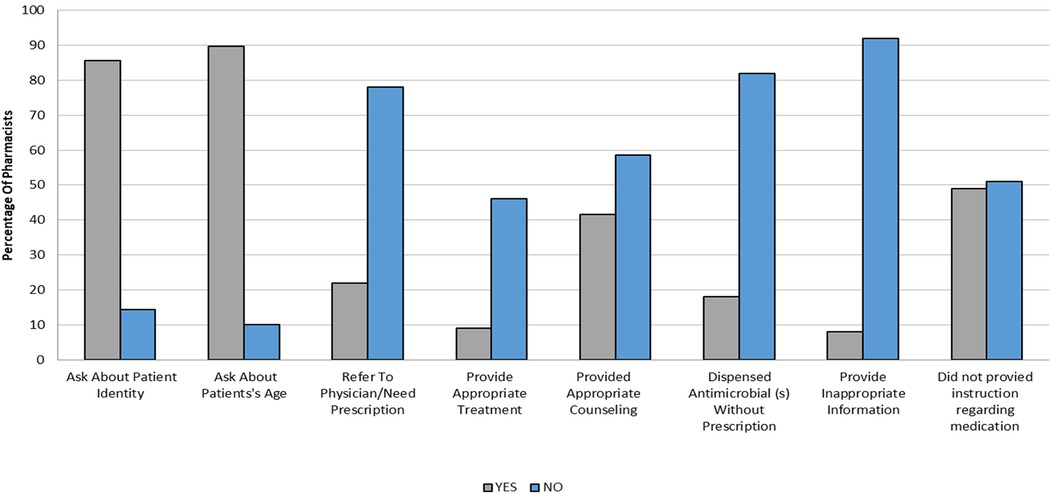
Figure 4. Percentage (%) of pharmacists who provide different types of patient assessment and treatment in all scenarios.
The analysis revealed a significant difference in pharmacists’ practices based on the time period of the visit by the simulated patients (P = 0.001). Morning visits that occurred from 8 a.m. to 12 p.m. demonstrated the highest rate of appropriate practice at 73.3% compared to other times of the day. In contrast, afternoon visits from 12 to 4 p.m. had the lowest rate of appropriate practice at only 41% and the highest rate of poor practice at 59% across all time periods. Evening visits occurring from 4 to 8 p.m. and night visits from 8 p.m. to 12 a.m. showed moderate rates of appropriate pharmacist practice at around 50%. However, night visits had the highest rate of optimal practice at 8.1% compared to other time periods.
Othe factors including gender, nationality, type of pharmacy, and pharmacy location, did not show a statistically significant relationship with practices based on their p-values (0.088, 0.229, 0.598, and 0.322, respectively). Table 3 presents a cross-tabulation of the association between pharmacists’ characteristics and practices.
We believe this is the first study to fully evaluate current practices of community pharmacy professionals in Saudi Arabia in managing children with acute diarrhea. The findings suggest that a significant proportion of pharmacists in community pharmacies display suboptimal practices in managing pediatric diarrhea. Whilst this is similar to the findings from Ethiopia, which showed that community pharmacies do not provide adequate treatment for acute diarrhea in children (31), our findings suggest an urgent need to update the curriculum for student pharmacists in Saudi Arabia and beyond as well as instigate continual professional development (CPD) activities post qualification.
A noticeable finding though was the highest rate of optimal practice occurred during night visits (8 p.m.–12 a.m.) compared to other time periods despite the limited sample size. Several factors may explain this result. These included the availability of experienced pharmacists on night shifts and lower patient volumes enabling more dedicated counseling time per case (32, 33). However, this observation warrants validation through expanded studies across more locales and with larger samples to substantiate any associations between visit time and the quality of care of pediatric diarrhea, and we will be following this up in future research projects.
It was initially hypothesized by the research team that the first scenario would yield the highest percentage of adequate practices, given the clarity of the “red flag” for referral. However, this was not the case, and the highest percentage of poor practices was observed for this scenario indicating considerable deficiencies in the pharmacists’ clinical assessment skills and judgment regarding appropriate referral. Conversely, the third scenario exhibited the highest percentage of adequate practices. The context of this scenario was intentionally broader, with more acceptable management options.
Given the appreciable differences in intervention approaches between adults and children, it is essential to obtain all relevant patient information before suggesting possible approaches to manage pediatric diarrhea. Encouragingly, a significant proportion of surveyed pharmacists in our study were engaged in this behavior, reflecting professional practice. However, the lack of a designated space for confidential patient counseling in a number of pharmacies led to some pharmacists dispensing medications without adequately seeking additional information from the patient. Overall, only 62% of pharmacists recommended one or more medications for acute diarrhea treatment, with 20% of cases referred to physicians irrespective of the case characteristics. In addition, a small number of pharmacists abstained from making any recommendations, which is a concern. Unfortunately, this could reinforce the public perception that pharmacists are mainly engaged in medicine sales and may be incapable of assessing and treating minor conditions such as diarrhea (34). This is an issue that needs to be addressed especially with community pharmacists playing a key role in many countries during the COVID-19 pandemic including giving advice on preventative measures for infectious diseases and dealing with misinformation (17, 18, 35), and they need to maintain this role and respect into the future.
In all scenarios, the majority of dispensed medications included kaolin and pectin (34%), which is similar to the findings of Merghani et al. (2022) which reported a 43% recommendation for the same medication (16). Despite the World Health Organization's statement that routine use of probiotics for severe diarrhea in children is not recommended, some pharmacists still proposed their use as a potential therapeutic intervention. However, the effectiveness of such treatments in diarrhea management remains uncertain (1, 36, 37).
Another concern is that in the present study only 20% of pharmacists recommended ORS, and none suggested the use of zinc supplements. This was very different to the findings of Merghani et al. (2022), where 90% of community pharmacists in their study in Saudi Arabia recommended the use of ORS, with 59% also suggesting the inclusion of zinc supplements (16). Similarly, Ayele et al. (2018) reported that 33.3% of pharmacists in Gondar town, Ethiopia, recommended ORS with zinc. We are not sure of the reasons behind these appreciable differences in study findings and will be exploring this further in future studies in view of the concerns raised with the findings in our study.
We have seen in the study of Khojah that during the recent COVID-19 pandemic, 15.8% of pharmacies in Saudi Arabia dispensed an antibiotic without a prescription, higher than seen in the study of Alshreedy et al. (2020) at 12.1% of patients with pharyngitis, with a similar proportion in the study of Al-Tannir et al. (20, 24, 38). However, in the current study, the percentage was slightly higher at 18%, indicating a possible lax in the current monitoring of community pharmacies. Even in the absence of evidence to support its routine use, metronidazole was often suggested for managing pediatric diarrhea, except when it was specifically caused by a Clostridioides difficile infection (14). This misuse and overuse of antibiotics is a concern as this contributes to the emergence of AMR, which poses a significant threat to public health (39). Pharmacists play a vital role in ensuring the appropriate use of antibiotics (21, 40). They have a professional responsibility to provide treatment guidance following evidence-based guidelines and considering the specific needs of their patients. By vigilance and adhering to best practices, pharmacists can help combat rising rates of AMR by not dispensing antibiotics inappropriately without a prescription. This is in line with best practice as well as the regulations in Saudi Arabia and globally, with education of patients and pharmacists key to reducing inappropriate requests and/or dispensing of antibiotics without a prescription (21).
Regarding pharmacists’ readiness to assist patients, the study findings revealed a noticeable lack of engagement and enthusiasm among pharmacists working in rural, sparsely populated areas when fulfilling their professional responsibilities. This is also a concern going forward that needs to be addressed to continue to cement their relationship with patients. As a result, direct them towards optimal management of presenting infectious diseases and away from any requests for antibiotics thereby reducing AMR.
We believe this study possesses several strengths, including its methodological approach with simulated patients. The study was also conducted among community pharmacies serving a diverse population. The simulated patients utilized in this study were students enrolled in the Doctor of Pharmacy (PharmD) program who underwent comprehensive training in multiple study situations under the principal author's supervision. Consequently, helped to ensure realistic patients. However, we are aware this study had limitations. The data collection process was restricted to a single point in time thereby limiting the evaluation of temporal variations. Pharmacies that were untraceable or temporarily closed at the time of the client visit were excluded from the study. Given that pharmacy employee behavior may vary across different time periods, and each pharmacy was only visited once by a simulated patient, certain conclusions may lack conclusiveness due to the absence of public and patient feedback. Within the context of the pseudo-patient methods, it was noted that only a limited number of pharmacists provided instructions for each medication during the payment process. However, the absence of real-world scenarios in these methods may affect the precision of determining the exact proportion of pharmacists who neglect to provide instructions. We also could not fully assess the knowledge of pharmacists regarding the management of pediatric diarrhea using the simulated patient methodology. Alongside this, we may not always be able to fully determine the pharmacy model. The study was also only conducted in one Province for the reasons stated. Additionally, some of the observations and scoring relied on subjective assessments, which may have introduced bias. Despite these limitations, we believe our findings are robust providing direction for the future.
There were concerns regarding the management of pediatric diarrhea among community pharmacists in Madinah province, and potentially across Saudi Arabia, in our study. The concerns need addressing through modification of the curriculum with undergraduate pharmacists as well as additional education post qualification to improve the management of these priority patients. Alongside this, the unauthorized sale of antibiotics without a prescription is still an issue in Saudi Arabia exacerbating AMR that also needs to be addressed. In the first instance, it is recommended to strengthen the enforcement of regulations with appreciable fines for abuse alongside conducting additional educational programs among pharmacists and parents to enhance their clinical competency and increase their awareness of the appropriate management of pediatric diarrhea. By doing so, reduce the pressures on pharmacists to dispense antibiotics inappropriately thereby helping to reduce AMR.
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding authors.
The studies involving humans were approved by Institutional Research Ethics Committee at Taibah University (Ref number: COPTU-REC-55-20230224). The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required from the participants or the participants’ legal guardians/next of kin because the research used simulated patients.
FA: Conceptualization, Data curation, Formal Analysis, Funding acquisition, Investigation, Methodology, Resources, Validation, Visualization, Writing – original draft, Writing – review & editing. AA: Data curation, Formal Analysis, Investigation, Methodology, Validation, Visualization, Writing – review & editing. RA: Data curation, Formal Analysis, Investigation, Methodology, Validation, Visualization, Writing – review & editing. DA: Conceptualization, Data curation, Formal Analysis, Methodology, Validation, Visualization, Writing – review & editing. FHA: Data curation, Formal Analysis, Investigation, Methodology, Validation, Visualization, Writing – review & editing. MM: Conceptualization, Data curation, Formal Analysis, Investigation, Methodology, Validation, Visualization, Writing – review & editing. MA: Data curation, Formal Analysis, Investigation, Methodology, Validation, Visualization, Writing – review & editing. AK: Conceptualization, Formal Analysis, Methodology, Validation, Visualization, Writing – original draft, Writing – review & editing. BG: Conceptualization, Methodology, Validation, Visualization, Writing – original draft, Writing – review & editing.
The author(s) declare financial support was received for the research, authorship, and/or publication of this article.
The APC was funded by the Deanship of Scientific Research, Qassim University.
The researchers would like to thank the Deanship of Scientific Research, Qassim University for funding publication of this project.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declared that they were an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. World Health Organization. Diarrhoeal Disease. (2017). Available online at: https://www.who.int/news-room/fact-sheets/detail/diarrhoeal-disease (Accessed August 10, 2023).
2. Troeger CE, Khalil IA, Blacker BF, Biehl MH, Albertson SB, Zimsen SR, et al. Quantifying risks and interventions that have affected the burden of diarrhoea among children younger than 5 years: an analysis of the global burden of disease study 2017. Lancet Infect Dis. (2020) 20(1):37–59. doi: 10.1016/S1473-3099(19)30401-3
3. Blenkinsopp A, Duerden M, Blenkinsopp J. Symptoms in the Pharmacy: A Guide to the Management of Common Illnesses. Hoboken: Wiley (2022).
4. Guh AY, Mu Y, Winston LG, Johnston H, Olson D, Farley MM, et al. Trends in US burden of clostridioides difficile infection and outcomes. N Engl J Med. (2020) 382(14):1320–30. doi: 10.1056/NEJMoa1910215
5. Shane AL, Mody RK, Crump JA, Tarr PI, Steiner TS, Kotloff K, et al. 2017 infectious diseases society of America clinical practice guidelines for the diagnosis and management of infectious diarrhea. Clin Infect Dis. (2017) 65(12):e45–80. doi: 10.1093/cid/cix669
6. Brandt KG, Antunes MMDC, Silva GAPD. Acute diarrhea: evidence-based management. J Pediatr (Rio J). (2015) 91:S36–43. doi: 10.1016/j.jped.2015.06.002
7. Gauchan E, Malla KK. Relationship of renal function tests and electrolyte levels with severity of dehydration in acute diarrhea. J Nepal Health Res Counc. (2015) 13(29)::84–9.26411719
8. Lamberti L, Walker C, Chan K, Jian W, Black R. Oral zinc supplementation for the treatment of acute diarrhea in children: a systematic review and meta–analysis. Nutrients. (2013) 5(11):4715–40. doi: 10.3390/nu5114715
9. Florez ID, Veroniki A-A, Al Khalifah R, Yepes-Nunez JJ, Sierra JM, Vernooij RW, et al. Comparative effectiveness and safety of interventions for acute diarrhea and gastroenteritis in children: a systematic review and network meta-analysis. PLoS One. (2018) 13(12):e0207701. doi: 10.1371/journal.pone.0207701
10. Administration, F.a.D. FDA Drug Safety Communication: FDA Warns About Serious Heart Problems with High Doses of the Antidiarrheal Medicine Loperamide (Imodium), Including from Abuse and Misuse. (2018). Available online at: https://www.fda.gov/drugs/drug-safety-and-availability/fda-drug-safety-communication-fda-warns-about-serious-heart-problems-high-doses-antidiarrheal (Accessed August 10, 2023).
11. Guo Q, Goldenberg JZ, Humphrey C, El Dib R, Johnston BC. Probiotics for the prevention of pediatric antibiotic-associated diarrhea. Cochrane Database Syst Rev. (2019) 4(4):CD004827. doi: 10.1002/14651858.CD004827.pub5
12. Zanichelli V, Sharland M, Cappello B, Moja L, Getahun H, Pessoa-Silva C, et al. The WHO AWaRe (Access, Watch, Reserve) Antibiotic Book and Prevention of Antimicrobial Resistance. (2023).
13. Sharland M, Zanichelli V, Ombajo LA, Bazira J, Cappello B, Chitatanga R, et al. The WHO essential medicines list AWaRe book: from a list to a quality improvement system. Clin Microbiol Infect. (2022) 28(12):1533–5. doi: 10.1016/j.cmi.2022.08.009
14. Bruzzese E, Giannattasio A, Guarino A. Antibiotic treatment of acute gastroenteritis in children. F1000Res. (2018) 7:193. doi: 10.12688/f1000research.12328.1
15. Diniz-Santos DR, Silva LR, Silva N. Antibiotics for the empirical treatment of acute infectious diarrhea in children. Braz J Infect Dis. (2006) 10:217–27. doi: 10.1590/S1413-86702006000300011
16. Ali EM, Alqahtani SS, Syed NK, Banji OJ, Mashragi YA, Ageel MA, et al. Self-reported and the actual involvement of community pharmacy professionals in the management of acute childhood diarrhea in Jazan Province, Saudi Arabia: simulated patient visits and survey study. Saudi Pharm J. (2022) 30(10):1497–506. doi: 10.1016/j.jsps.2022.07.012
17. Cadogan CA, Hughes CM. On the frontline against COVID-19: community pharmacists’ contribution during a public health crisis. Res Social Adm Pharm. (2021) 17(1):2032–5. doi: 10.1016/j.sapharm.2020.03.015
18. Hedima EW, Adeyemi MS, Ikunaiye NY. Community pharmacists: on the frontline of health service against COVID-19 in LMICs. Res Social Adm Pharm. (2021) 17(1):1964–6. doi: 10.1016/j.sapharm.2020.04.013
19. Ayele AA, Mekuria AB, Tegegn HG, Gebresillassie BM, Mekonnen AB, Erku DA. Management of minor ailments in a community pharmacy setting: findings from simulated visits and qualitative study in Gondar Town, Ethiopia. PLoS One. (2018) 13(1):e0190583. doi: 10.1371/journal.pone.0190583
20. Alrasheedy AA, Alsalloum MA, Almuqbil FA, Almuzaini MA, Aba Alkhayl BS, Albishri AS, et al. The impact of law enforcement on dispensing antibiotics without prescription: a multi-methods study from Saudi Arabia. Expert Rev Anti Infect Ther. (2020) 18(1):87–97. doi: 10.1080/14787210.2020.1705156
21. Sono TM, Yeika E, Cook A, Kalungia A, Opanga SA, Acolatse JEE, et al. Current rates of purchasing of antibiotics without a prescription across Sub-Saharan Africa; rationale and potential programmes to reduce inappropriate dispensing and resistance. Expert Rev Anti-Infect Ther. (2023) 21(10):1025–55. doi: 10.1080/14787210.2023.2259106
22. Godman B, Egwuenu A, Haque M, Malande OO, Schellack N, Kumar S, et al. Strategies to improve antimicrobial utilization with a special focus on developing countries. Life. (2021) 11(6):528. doi: 10.3390/life11060528
23. Jacobs TG, Robertson J, van den Ham HA, Iwamoto K, Bak Pedersen H, Mantel-Teeuwisse AK. Assessing the impact of law enforcement to reduce over-the-counter (OTC) sales of antibiotics in low-and middle-income countries; a systematic literature review. BMC Health Serv Res. (2019) 19(1):1–15. doi: 10.1186/s12913-019-4359-8
24. Khojah HMJ. Over-the-counter sale of antibiotics during COVID-19 outbreak by community pharmacies in Saudi Arabia: a simulated client study. BMC Health Serv Res. (2022) 22(1):123. doi: 10.1186/s12913-022-07553-x
25. Boura F, Al-Tabakha M, Hassan N, Darwich M. Critical appraisal of simulated patient methodology to assess the practice of community pharmacist in the Middle East and North Africa region: a systematic review. Pharm Pract (Granada). (2022) 20(3):1–21. doi: 10.18549/PharmPract.2022.3.2701
26. Collins JC, Chong WW, de Almeida Neto AC, Moles RJ, Schneider CR. The simulated patient method: design and application in health services research. Res Social Adm Pharm. (2021) 17(12):2108–15. doi: 10.1016/j.sapharm.2021.04.021
27. Edessa D, Assefa N, Dessie Y, Asefa F, Dinsa G, Oljira L. Non-prescribed antibiotic use for children at community levels in low- and middle-income countries: a systematic review and meta-analysis. J Pharm Policy Pract. (2022) 15(1):57. doi: 10.1186/s40545-022-00454-8
28. Raosoft. Sample Size Calculator. (2004). Available online at: http://www.raosoft.com/samplesize.html (Accessed March 1, 2023).
29. Akande-Sholabi W, Oyesiji E, Adebisi YA. Antimicrobial stewardship: community pharmacists’ antibiotic dispensing practices, knowledge, and perception regarding antibiotics and antibiotic resistance. J Pharm Health Serv Res. (2023) 14(4):383–91. doi: 10.1093/jphsr/rmad040
30. Mokwele RN, Schellack N, Bronkhorst E, Brink AJ, Schweickerdt L, Godman B. Using mystery shoppers to determine practices pertaining to antibiotic dispensing without a prescription among community pharmacies in South Africa—a pilot survey. JAC Antimicrob Resist. (2022) 4(1):dlab196. doi: 10.1093/jacamr/dlab196
31. Abegaz TM, Belachew SA, Abebe TB, Gebresilassie BM, Teni FS, Woldie HG. Management of children’s acute diarrhea by community pharmacies in five towns of Ethiopia: simulated client case study. Ther Clin Risk Manag. (2016) 12:515–26. doi: 10.2147/TCRM.S98474
32. Atlas KR, Forbes M, Riches J, Maina E, Lim R, Johnson T, et al. The scope of hospital medicine practice at night: a national survey of night shift hospitalists. Hosp Pract. (2021) 49(4):292–7. doi: 10.1080/21548331.2021.1932507
33. Jung YB, Lee KY. The effect of daytime surgical hospitalists on reducing night shift physicians’ workload. J Patient Saf. (2023) 19(5):346–51. doi: 10.1097/PTS.0000000000001138
34. El-Kholy AA, Abdelaal K, Alqhtani H, Abdel-Wahab BA, Abdel-Latif MMM. Publics’ perceptions of community pharmacists and satisfaction with pharmacy services in Al-Madinah City, Saudi Arabia: a cross sectional study. Medicina (Kaunas). (2022) 58(3):432. doi: 10.3390/medicina58030432
35. Kibuule D, Nambahu L, Sefah I, Kurdi A, Phuong T, Kwon H-Y, et al. Activities in Namibia to limit the prevalence and mortality from COVID-19 including community pharmacy activities and the implications. Sch Acad J Pharm. (2021) 10(5):82–92. doi: 10.36347/sajp.2021.v10i05.001
36. Pérez C. Probiotics for the treating acute diarrhea and preventing antibiotic-associated diarrhea in children. Nutr Hosp. (2015) 31(Suppl 1):64–7. doi: 10.3305/nh.2015.31.sup1.8709
37. Guarino A, Guandalini S, Lo Vecchio A. Probiotics for prevention and treatment of diarrhea. J Clin Gastroenterol. (2015) 49(Suppl 1):S37–45. doi: 10.1097/MCG.0000000000000349
38. Al-Tannir M, Altannir Y, Altannir M, AlFayyad I. Community pharmacy sales of non-prescribed antibiotics in Riyadh, Saudi Arabia: a simulated patient study. Int J Clin Pharm. (2020) 42(2):341–6. doi: 10.1007/s11096-020-01033-0
39. Murray CJ, Ikuta KS, Sharara F, Swetschinski L, Aguilar GR, Gray A, et al. Global burden of bacterial antimicrobial resistance in 2019: a systematic analysis. Lancet. (2022) 399(10325):629–55. doi: 10.1016/S0140-6736(21)02724-0
Keywords: antibiotics, appropriate care, antimicrobial resistance, pediatric diarrhea, community pharmacy, public health, Saudi Arabia
Citation: Alnezary FS, Alamri AR, Alrehaili RD, Alnizari DS, Alzahrani F, Mahmoud M, Almutairi MS, Kurdi A and Godman B (2024) Managing infectious diarrhea among young children in community pharmacies in Saudi Arabia and the implications for AMR. Front. Pediatr. 12:1342493. doi: 10.3389/fped.2024.1342493
Received: 21 November 2023; Accepted: 1 March 2024;
Published: 18 March 2024.
Edited by:
Zikria Saleem, Bahauddin Zakariya University, PakistanReviewed by:
Josette Raymond, Hôpital de Bicêtre, France© 2024 Alnezary, Alamri, Alrehaili, Alnizari, Alzahrani, Mahmoud, Almutairi, Kurdi and Godman. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Masaad S. Almutairi bWFzLmFsbXV0YWlyaUBxdS5lZHUuc2E= Brian Godman YnJpYW4uZ29kbWFuQHN0cmF0aC5hYy51aw==
†ORCID Amanj Kurdi orcid.org/0000-0001-5036-1988 Brian Godman orcid.org/0000-0001-6539-6972
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.