
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Pediatr. , 22 January 2024
Sec. Neonatology
Volume 12 - 2024 | https://doi.org/10.3389/fped.2024.1336108
 Yumeng Chen1,†
Yumeng Chen1,† Jingjie Fan2,†
Jingjie Fan2,† Xiaowei Li3,†
Xiaowei Li3,† Yufeng Ye4
Yufeng Ye4 Yanyun Lv5
Yanyun Lv5 Suijin Zheng6
Suijin Zheng6 Jianxiong Hu7
Jianxiong Hu7 Yudong Pu8*
Yudong Pu8* Tao Liu9*
Tao Liu9*
Background: During the special period of the global spread of COVID-19, pregnant women are sensitive groups to the impacts of COVID-19 epidemic. However, the effects of lockdown measures implemented in response to the COVID-19 on fetal birthweight remain unclear.
Objectives: This study investigated the associations of COVID-19 lockdown with birth weight in Chinese population.
Methods: We collected 730,153 data of participants from hospitals of five cities in the south of China, we defined the time period of level I response (1/23-2/24/2020) as level I lockdown, and women who were pregnant during level I lockdown as the exposure group. Women who were pregnant during the same calendar month from 2015 to 2019 were defined as the unexposed group. We quantitatively estimate the individual cumulative exposure dose by giving different weights to days with different emergency response levels. Generalized linear regression models were used to estimate the association between COVID-19 lockdown exposure with birth weight and risk of low birth weight (<2,500 g) and macrosomia (>4,000 g).
Results: The birth weight of the exposed group is heavier than the unexposed group (3,238.52 vs. 3,224.11 g: adjusted β = 24.39 g [95% CI: 21.88, 26.91 g]). The exposed group had a higher risk of macrosomia (2.8% vs. 2.6%; adjusted OR = 1.17 [95% CI: 1.12, 1.22]). More obvious associations were found between COVID-19 lockdown and macrosomia in women who experienced the lockdown in their early pregnancy. Women who experienced the lockdown at their 4–7 weeks of pregnancy showed statistically significant heavier birth weight than unexposed group (after adjustment): β = 1.28 (95% CI: 1.11, 1.46) g. We also observed a positive association between cumulative exposure dose of COVID-19 lockdown in all pregnant women and birth weight, after divided into four groups, Q1: β = 32.95 (95% CI: 28.16, 37.75) g; Q2: β = 18.88 (95% CI: 14.12, 23.64) g; Q3: β = 19.50 (95% CI: 14.73, 24.28) g; Q4: β = 21.82 (95% CI: 17.08, 26.56) g. However, there was no statistically significant difference in the risk of low birth weight between exposed and unexposed groups.
Conclusions: The COVID-19 lockdown measures were associated with a heavier birth weight and a higher risk of macrosomia. Early pregnancy periods may be a more susceptible exposure window for a heavier birth weight and a higher risk of macrosomia. We also observed a positive association between cumulative exposure dose of COVID-19 lockdown and birth weight. The government and health institutions should pay attention to the long-term health of the infants born during the COVID-19 lockdown period, and follow up these mothers and infants is necessary.
Since the early of 2020, the COVID-19 was reported in more than 200 countries and regions, and has become a global pandemic. As of 17 December 2023, over 772 million confirmed cases and nearly seven million deaths have been reported globally (1).The health of global population has been severely affected. During the special period of the global spread of COVID-19, pregnant women and newborns are more vulnerable as sensitive groups. On the one hand, pregnant women's concerns and fears about the epidemic have increased their psychological burden. On the other hand, during the epidemic, insufficient hospital resources have resulted in pregnant women and newborns not receiving timely medical assistance. Insufficient food and social distancing prevent pregnant women from receiving sufficient care, leading to a series of health consequences, including preterm birth, miscarriage, and fetal growth restriction (FGR).
At present, the impact of COVID-19 on newborn birth weight has not been determined. An Ireland study reported an unprecedented decrease in the number of very low birthweight (VLBW) and extremely low birthweight (ELBW) in infants born in Ireland (2). And an increase in infants' birth weight was observed in Wuhan during the COVID-19 lockdown (3). However, other studies report that there is no negative impact of COVID-19 lockdown on birthweight (4, 5).
The above researches have demonstrated possible associations between COVID-19 lockdown and birth weight, but there are still several overlooked questions. First, as the severity of the epidemic changes, COVID-19 lockdown measures are being adjusted in most of countries and regions. However, all of these previous studies did not classify the exposure (2–4), which may be underestimate the impact of COVID-19 lockdown on adverse pregnancy outcomes. Second, previous studies have shown that the birth season of newborns is associated with their birth weight (6–8), therefore the impact of different seasons should be considered in the study of associations of COVID-19 lockdown with birth weight. Third, the follow-up time in in previous studies was too short to produce an outcome. Lastly, previous studies did not consider the pregnant woman's stage of pregnancy. Studies have shown that there are significant differences in the susceptibility of pregnant women to environmental factors during different pregnancy periods (9, 10).
To address these research gaps, we calculated the cumulative exposure separately according to the lockdown period of different intensities to avoid errors caused by exposure levels, considered the effects of seasonality and extend the cohort long enough to produce an outcome, analyzed the association of the COVID-19 lockdown on birthweight in South China. This study has positive significance for the health of pregnant women and newborns during the COVID-19 lockdown.
We collected birth records of participants from hospitals of five cities in the south of China, including all hospitals in Foshan (n = 62), several hospitals in Dongguan (n = 2), Guangzhou (n = 1), Shenzhen (n = 1) and Jiangmen (n = 1). We included all birth data for all hospitals between February 1, 2015 and December 31, 2020 (N = 730,153). For this analysis, we excluding birth data with multiple births (n = 26,897), stillbirths (n = 678), or missing information on key variables (n = 88,921). In addition, 120,686 data were also excluded from this analysis because their pregnancies did not overlap with the COVID-19 lockdown in 2020 or the same calendar month from 2015 to 2019. Birth data with gestational length less than 28 weeks were also excluded (3) (n = 30,509). Overall, a sample size of 550,605 mother-infant pairs was included in the study (Figure 1). All the women were negative for the Novel Coronavirus test.
This study was approved by the Ethics Committee of Guangdong Center for Disease Control and Prevention (No. W96-027E-2020004).
Each birth data contains the following information: Infant sex, date of birth, type of delivery (vaginal or cesarean), gestational weeks (GW), number of births, parity and major adverse pregnancy outcomes such as miscarriage and stillbirth. Above information about participants' health was obtained throughout Hospital information system or birth record system. We check the quality of the source data, implausible values and outliers were either corrected or recorded as missing.
The National Emergency Response Plan for Public Emergencies by the China State Council defined 4 levels of emergency response: Level I (extremely serious), Level II (serious), Level III (relatively serious), and Level IV (common) (11). On January 23, the Guangdong Provincial Government took the lead in China in launching Level I response. The emergency response level was upgraded to level II on February 24 and upgraded to level III On May 9.We defined the time period of level I response (1/23-2/24/2020) as level I lockdown, and women who were pregnant during level I lockdown as the exposure group (N = 96,550). Our data showed significant differences in birth weight between the calendar months of pregnancy (Figure 2). To decrease the influence of seasonal effects, we defined women who became pregnant during the same calendar month from 2015 to 2019 as the unexposed group (N = 452,756).
Pregnant women and fetuses may have different sensitivities to COVID-19 lockdown at different stages of pregnancy. In order to explore the susceptible exposure window, they were further divided into 11 subgroups based on gestational age at 23 January 2020. The date of conception is calculated from gestational age and birth date. For example, women whose date of conception fell within the period of lockdown I were defined as Group I, while women whose gestational week was less than four weeks on 23 January 2020 were defined as Group II. Pregnant women whose GW less than 41 weeks were recorded as 41 weeks. The unexposed group was divided into 11 subgroups corresponding to the exposed group. For each pair of subgroups (exposed and unexposed), we evaluated the association between COVID-19 lockdown exposure and birth weight.
The lockdown measures during level II and level III response periods are not as strong as those during the level I response period, so that the different effect of different lockdown measures level should be considered. Therefore, we quantitatively estimate the cumulative exposure dose of individuals by assigning different weights to days with different emergency response levels: 1/22/2020 or earlier was the no response period, 1/23-2/24/2020 was the level I response period, 2/25-5/9/2020 was the level II response period, and 5/10-12/31/2020 was the level III response period, with weights of 0, 3, 2, and 1, respectively (12). In addition, considering the potential effects of exposure time, we estimated only the cumulative exposure dose for the first 37 GW, based on the fact that the sample was reserved for full-term delivery only (Figure 3).

Figure 3. Approach to calculating individual cumulative exposure dose to lockdown in the first 37 GWs (12). : Weeks after 37 GWs. A, B, C, D and E represent subgroups of pregnant women with different GWs during the Level I lockdown; We assigned a weighting value of 3 to the days with Level I response, 2 to the days with Level II response, 1 to the days with Level III response, and 0 to days before lockdown (no exposure). Visit this link forcreative commons licence (Available at: https://bmcpregnancychildbirth.biomedcentral.com/articles/10.1186/s12884-021-04268-5#rightslink). No changes have been made to the referenced image.
: Weeks after 37 GWs. A, B, C, D and E represent subgroups of pregnant women with different GWs during the Level I lockdown; We assigned a weighting value of 3 to the days with Level I response, 2 to the days with Level II response, 1 to the days with Level III response, and 0 to days before lockdown (no exposure). Visit this link forcreative commons licence (Available at: https://bmcpregnancychildbirth.biomedcentral.com/articles/10.1186/s12884-021-04268-5#rightslink). No changes have been made to the referenced image.
Low birth weight (LBW) was defined as a birth weight of less than 2500 g (13). Normal birth weight was defined as birth weight between 2500 and 4,000 g. Macrosomia was defined as birth weight greater than 4,000 g (14).
Considering biological rationality and literature review, we chose potential confounders such as maternal age, gestational age, parity, birth order, residential district, type of delivery and infant sex.
We used the chi-square test and t-test to compare differences of social demographic and gestational characteristics between the exposed and unexposed groups. We used the generalized linear model (GLM) to estimate the association between COVID-19 lockdown exposure and birth weight (linear regression) with adjustment for the confounders. Taking normal birth weight as reference, birth weight was further divided into low birth weight and macrosomia. We used multiple logistic regression model and we used birth weight as a classification variable in model. Similarly, GLM and multiple logistic regression models were used to estimate the association between cumulative exposure dose and birth weight. The cumulative exposure dose of the exposed group was divided into four quartiles (Q1, Q2, Q3 and Q4) to estimate the associations of each quartile of cumulative exposure (relative to unexposed) with birth weight. We did all of the analyses with R3.6.1. All tests were bilateral, and P < 0.05 was considered statistically significant.
A comparison of general characteristics between the exposed group and unexposed group is shown in Table 1. The study included 549,306 women—96,550 in the exposed group and 452,756 in the unexposed group (Table 1). There were no significant differences in infant sex between exposed group and unexposed group. The unexposed group had higher proportions of participants over the age of 30, macrosomia, multiparity, and had lower proportions of participants with natural delivery than the exposed group.
As shown in Table 2, the birth weight of the exposed group is heavier than unexposed group (3,238.52 ± 388.72 g vs. 3,224.11 ± 393.61 g). The Level I response was significantly associated with a 24.39 (95% CI: 21.88, 26.91) g increase in birth weight in the entire sample after adjusting for confounders. After dividing into 11 subgroups, the first 9 subgroups showed statistically significant heavier birth weight in the exposed group than in the unexposed group, after adjusting for confounders. As shown in Table 3, We can also find a positive correlation between cumulative exposure dose and birth weight after adjusting for confounders. Each 100 unit increase in cumulative exposure was associated with a 6.54 (95% CI: 5.66, 7.41) g increase in birth weight. After the exposure group was divided into four groups according to the cumulative exposure amount, four groups were all showed statistically significant heavier birth weight than unexposed group (after adjustment): Q1: β = 32.95 (95% CI: 28.16, 37.75) g; Q2: β = 18.88 (95% CI: 14.12, 23.64) g; Q3: β = 19.50 (95% CI: 14.73, 24.28) g; Q4: β = 21.82 (95% CI: 17.08, 26.56) g.
Table 4 shows the comparison of LBW rate and macrosomia rate between exposed and unexposed groups. Compared to the unexposed group, exposed group had a higher macrosomia rate (2.8% vs. 2.6%) in the total sample. However, there was no statistically significant difference in the risk of low birth weight between the two groups. After adjusting for confounders, the risk of macrosomia in the exposed group was statistically significantly higher than that in the unexposed group, OR = 1.17 (95% CI: 1.12, 1.22). After dividing into 11 subgroups, all of the risk of macrosomia in the exposed group was higher than that unexposed group, and the first four subgroups, subgroup 6, subgroup 8 and subgroup 9 were statistically significant. More obvious associations were found between COVID-19 lockdown and macrosomia in women who experienced the lockdown in their early pregnancy. Women who experienced the lockdown at their 4–7 weeks of pregnancy showed statistically significant heavier birth weight than unexposed group (after adjustment): β = 1.28 (95% CI: 1.11, 1.46) g. As shown in Table 5, We can also find a positive correlation between cumulative exposure dose to COVID-19 lockdown and the risk of macrosomia after adjusting for confounders. Each 100 unit increase in the COVID-19 lockdown exposure during the first 37 GWs was significantly associated with 1.04 (95% CI: 1.02, 1.06) times higher risks in macrosomia. The adjusted ORs of macrosomia for the Q1, Q2, Q3 and Q4 quartiles of cumulative exposure (vs. no exposure) were 1.31 (1.21, 1.41), 1.10 (1.02, 1.20), 1.08 (0.99, 1.17), and 1.16 (1.07, 1.26), respectively. However, there was no statistically significant difference in the risk of low birth weight between exposed and unexposed groups.
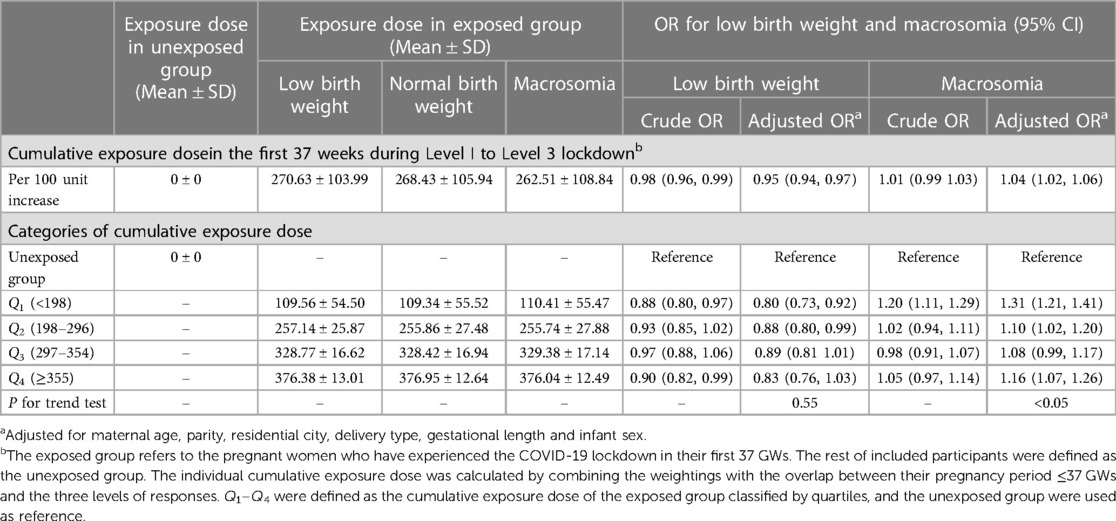
Table 5. Associations of cumulative exposure dose to the COVID-19 lockdown with low birth weight and macrosomia.
Our study of the association of COVID-19 lockdown measures and birth weight showed that COVID-19 lockdown was associated with a higher birth weight and a higher risk of macrosomia. Early and middle pregnancy might be the susceptible exposure window of the effect of COVID-19 lockdown on birth weight and macrosomia. However, no association between COVID-19 locking measures and LBW risk was observed.
There are several possible reasons for the increase in birth weight and risk of macrosomia during COVID-19 lockdown: First, dietary and nutritional status and physical activity of the pregnant women during COVID-19 lockdown period may be associated with increased weight in pregnant women, which may lead to increased birth weight in newborns (15, 16). On the one hand, during the COVID-19 lockdown, especially at the beginning of the lockdown, people stocked up on nonperishable food because of lack of supplies and panic mood. Compared with the usual, the intake of carbohydrate is higher, the intake of vitamins and dietary fiber is less, and the distribution of nutrients is very uneven (3). It can result in higher weight and a higher BMI in pregnant women. On the other hand, because of lockdown measures during the outbreak, most people were forced to work at home, and some even be unemployed. Less outdoor time and less exercise increase the risk of obesity (17). The above two causes of maternal weight increase may be the reason for the infant's birth weight increase. Secondly, pregnant women during the lockdown were facing heavier psychological pressure, including family relationships and economic issue (18). Studies have shown that pregnant women who experience high levels of psychological stress during pregnancy have an increased risk of macrosomia (19). Previous research showed that brain-derived neurotrophic factor (BDNF) are neutrophils, which are thought to play an important role in the growth and development of the placenta and fetus. One possible hypothesis to explain the relationship between maternal stress and birth weight is that changes in intrauterine concentrations of BDNF are associated with maternal stress and fetal growth and development (19). Lastly, it may also because pregnant women were unwilling or unable to go out for maternity check-ups during the epidemic, abnormal fetal weight cannot be detected in time. Our previous research also found that COVID-19lockdown increases the risk of Gestational diabetes, and Gestational diabetes is an important risk factor for macrosomia (20).
We further found that women in the early stages of pregnancy during Level I lockdown had a heavier newborn birth weight and higher risk of macrosomia. The effect of COVID-19 lockdown is more significant in the early stage of pregnancy. It may be explained that the early stage of pregnancy is a critical time for fetal development. Previous studies have suggested that the early stages of pregnancy may be a susceptible exposure window of association of fine particulate matter and risk of preterm birth (9, 10). The early pregnancy is also a critical period for the occurrence of Gestational diabetes, and Gestational diabetes is related to the increased risk of macrosomia. Gestational diabetes leads to increased insulin resistance in pregnant women, and blood sugar enters the fetal circulation through the placenta. The excess glucose in the fetal body is converted into body fat, leading to macrosomia (21). It could also be explained that women in the early stages of pregnancy during lockdown are more likely to have longer lockdown period and higher lockdown cumulative exposure, which is more likely to observe the outcome.
Our results are similar to some previous studies: some studies have shown that COVID-19 lockdown is related to increased birth weight (2, 3, 22, 23). However, our results are not completely consistent with the results of some other studies. In some studies, no statistically significant changes in birth weight were found before and after COVID-19 lockdown (4, 5). Possible reasons are as follows: 1. Studies in different regions have different economic and social backgrounds, and standards and measures for COVID-19 lockdown vary from country to country. These complex factors may lead to different research results. 2. The sample size was insufficient to explore the association between lockdown exposure and birth weight. 3. COVID-19 lockdown effects on health are likely to continue for several months. The time of observation varies in different studies. Studies with shorter observation periods may not be sufficient to produce outcomes. 4. Most previous studies did not take seasonal effects and pregnancy stages into account, which may lead to an underestimate of association between COVID-19 lockdown and birth weight.
There are some advantages in our study. First, we quantitatively evaluated the COVID-19 lockdown exposure and analyzed the exposure-response association between COVID-19 lockdown and birth weight. Second, our study has sufficient sample size and a long time span of research data. It is beneficial for us to conduct subgroup analysis and explore the susceptible exposure window of COVID-19 lockdown on the impact of birth weight. Third, previous studies have shown that birth weight of newborns is influenced by the birth season. Therefore the impact of different seasons should be considered in the study of associations of COVID-19 lockdown with birth weight. We estimated the difference in birth weight between the exposed group and newborns born in the same calendar months from 2015 to 2019.
There are also some limitations in our study. First, appropriate physical activity during pregnancy has a positive impact on the health of both the mother and fetus, including a healthy birth weight. In fact, long-term studies have shown that women who exercise regularly during pregnancy are more likely to give birth to a suitable birth weight baby (24). However, weight, BMI and physical activity intensity information of the pregnant women were not available in the study, so we can't analyze the potential impact of these variables. Second, COVID-19 lockdown measures vary greatly among different countries and regions, and their impact on birth weight may have difference. The study was conducted in only a few cities in Guangdong Province and the sample size was uneven between cities which limit the extrapolation of our results. Third, this study only selected fetal information from hospital information systems or birth record systems. However, some pregnancy losses may not be recorded in the hospital information system, which may bias the association between COVID-19 lockdown and birthweight.
As the COVID-19 lockdown may have a variety of unpredictable health impacts, it is important to disseminate relevant information on this issue for the long-term health on newborns. Parents who experience COVID-19 lockdown during pregnancy period should pay more attention to the growth and development of their infants. The public health departments should regularly follow up the newborns whose mother experienced COVID-19 lockdown during pregnancy, especially those who were overweight. At the same time, it is necessary to pay more attention to the mental health of postpartum women.
This study compared birth weights of newborns before and after the COVID-19 lockdown and showed that COVID-19 lockdown was associated with a higher birth weight and a higher risk of macrosomia. Early months of pregnancy might be the susceptible exposure window of COVID-19 lockdown. Nowadays, COVID-19 is no longer the primary health threat in people's life, but the long-term health of infants born during COVID-19 lockdown period is still well worth noticing and exploring. This study has certain significance for the public health policy and clinical treatment related to maternal and infant health in the later stage of COVID-19. The government and health institutions should pay attention to the long-term health of the infants born during the COVID-19 lockdown period, and follow up these mothers and infants is necessary.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving humans were approved by Ethics Committee of Guangdong Center for Disease Control and Prevention (No. W96-027E-2020004). The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required from the participants or the participants’ legal guardians/next of kin because Only basic information such as birth weight of the population is used, without specific personal information, and there is no intervention experiment.
YC: Conceptualization, Data curation, Formal Analysis, Investigation, Methodology, Software, Supervision, Writing – original draft, Writing – review & editing. JF: Conceptualization, Data curation, Formal Analysis, Investigation, Methodology, Software, Supervision, Writing – original draft, Writing – review & editing. XL: Conceptualization, Data curation, Formal Analysis, Investigation, Methodology, Software, Supervision, Writing – original draft, Writing – review & editing. YY: Conceptualization, Data curation, Investigation, Methodology, Software, Supervision, Writing – review & editing. YL: Conceptualization, Data curation, Investigation, Methodology, Software, Supervision, Writing – original draft, Writing – review & editing. SZ: Conceptualization, Data curation, Investigation, Methodology, Software, Supervision, Writing – original draft, Writing – review & editing. JH: Conceptualization, Data curation, Investigation, Methodology, Software, Supervision, Writing – original draft, Writing – review & editing. YP: Conceptualization, Data curation, Formal Analysis, Funding acquisition, Investigation, Methodology, Project administration, Software, Supervision, Validation, Writing – review & editing. TL: Conceptualization, Data curation, Formal Analysis, Funding acquisition, Investigation, Methodology, Project administration, Software, Supervision, Validation, Writing – review & editing, Resources.
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article.
This work was supported by the National Natural Science Foundation of China (42075173, 42175181, 42275187), National Foreign Expert Project (G2022199006L), Shenzhen Science and Technology Plan Project (JCYJ20210324125206017), Dongguan Science and Technology of Social Development Program (20221800906202), and Sanming Project of Medicine in Shenzhen (No.SZSM202211032). These funders had no role in the design of the study, data collection, and analyses, or preparation of the manuscript.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declared that they were an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. World health organization. Coronavirus disease Situation reports (2023). Available online at: Available at: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports (Updated July 2, 2023).
2. Philip RK, Purtill H, Reidy E, Daly M, Imcha M, McGrath D, et al. Unprecedented reduction in births of very low birthweight (VLBW) and extremely low birthweight (ELBW) infants during the COVID-19 lockdown in Ireland: a ‘natural experiment’ allowing analysis of data from the prior two decades. BMJ Global Health. (2020) 5(9):e003075. doi: 10.1136/bmjgh-2020-003075
3. Li M, Yin H, Jin Z, Zhang H, Leng B, Luo Y, et al. Impact of Wuhan lockdown on the indications of cesarean delivery and newborn weights during the epidemic period of COVID-19. PLoS One. (2020) 15(8):e0237420. doi: 10.1371/journal.pone.0237420
4. Kirchengast S, Hartmann B. Pregnancy outcome during the first COVID 19 lockdown in Vienna, Austria. Int J Environ Res Public Health. (2021) 18(7):3782. doi: 10.3390/ijerph18073782
5. Collins-Smith A, Prasannan L, Shan W, Dori E, Katzow M, Blitz MJ. Effect of lockdown period of COVID-19 pandemic on maternal weight gain, gestational diabetes, and newborn birth weight. Am J Perinatol. (2022). doi: 10.1055/a-1925-1347
6. Murray LJ, O'Reilly DP, Betts N, Patterson CC, Davey Smith G, Evans AE. Season and outdoor ambient temperature: effects on birth weight. Obstet Gynecol. (2000) 96(5 Pt 1):689–95. doi: 10.1016/s0029-7844(00)01022-x
7. Strand LB, Barnett AG, Tong S. The influence of season and ambient temperature on birth outcomes: a review of the epidemiological literature. Environ Res. (2011) 111(3):451–62. doi: 10.1016/j.envres.2011.01.023
8. Chodick G, Shalev V, Goren I, Inskip PD. Seasonality in birth weight in Israel: new evidence suggests several global patterns and different etiologies. Ann Epidemiol. (2007) 17(6):440–6. doi: 10.1016/j.annepidem.2006.10.013
9. Pereira G, Bell ML, Lee HJ, Koutrakis P, Belanger K. Sources of fine particulate matter and risk of preterm birth in Connecticut, 2000–2006: a longitudinal study. Environ Health Perspect. (2014) 122(10):1117–22. doi: 10.1289/ehp.1307741
10. Pereira G, Belanger K, Ebisu K, Bell ML. Fine particulate matter and risk of preterm birth in Connecticut in 2000–2006: a longitudinal study. Am J Epidemiol. (2014) 179(1):67–74. doi: 10.1093/aje/kwt216
11. Ministry of Emergency Management P. National Emergency Response Plan for Public Emergencies 2006. Available online at: http://www.gov.cn/gzdt/2006-02/28/content_213129.htm (cited July 15, 2021).
12. Dong M, Qian R, Wang J, Fan J, Ye Y, Zhou H, et al. Associations of COVID-19 lockdown with gestational length and preterm birth in China. BMC Pregnancy Childbirth. (2021) 21(1):795. doi: 10.1186/s12884-021-04268-5
13. Nakano Y. Adult-Onset diseases in low birth weight infants: association with adipose tissue maldevelopment. J Atheroscler Thromb. (2020) 27(5):397–405. doi: 10.5551/jat.RV17039
14. Boulvain M, Irion O, Dowswell T, Thornton JG. Induction of labour at or near term for suspected fetal macrosomia. Cochrane Database Syst Rev. (2016) 2016(5):Cd000938. doi: 10.1002/14651858.CD000938.pub2
15. Alberico S, Montico M, Barresi V, Monasta L, Businelli C, Soini V, et al. The role of gestational diabetes, pre-pregnancy body mass index and gestational weight gain on the risk of newborn macrosomia: results from a prospective multicentre study. BMC Pregnancy Childbirth. (2014) 14:23. doi: 10.1186/1471-2393-14-23
16. Kominiarek MA, Peaceman AM. Gestational weight gain. Am J Obstet Gynecol. (2017) 217(6):642–51. doi: 10.1016/j.ajog.2017.05.040
17. Whitaker KM, Hung P, Alberg AJ, Hair NL, Liu J. Variations in health behaviors among pregnant women during the COVID-19 pandemic. Midwifery. (2021) 95:102929. doi: 10.1016/j.midw.2021.102929
18. Moyer CA, Compton SD, Kaselitz E, Muzik M. Pregnancy-related anxiety during COVID-19: a nationwide survey of 2740 pregnant women. Arch Women’s Ment Health. (2020) 23(6):757–65. doi: 10.1007/s00737-020-01073-5
19. Mélançon J, Bernard N, Forest JC, Tessier R, Tarabulsy GM, Bouvier D, et al. Impact of maternal prenatal psychological stress on birth weight. Health psychology: official journal of the division of health psychology. Am Psychol Assoc. (2020) 39(12):1100–8. doi: 10.1037/hea0001017
20. He Z, Lv Y, Zheng S, Pu Y, Lin Q, Zhou H, et al. Association of COVID-19 lockdown with gestational diabetes Mellitus. Front Endocrinol (Lausanne). (2022) 13:824245. doi: 10.3389/fendo.2022.824245
21. Kc K, Shakya S, Zhang H. Gestational diabetes mellitus and macrosomia: a literature review. Ann Nutr Metab. (2015) 66(Suppl 2):14–20. doi: 10.1159/000371628
22. Tessier B, Annesi-Maesano I, Cambonie G, Molinari N, Kalfa N. COVID-19 lockdown related to decrease in premature birth rate and increase in birth weight in metropolitan France. Front Pediatr. (2023) 11:1223692. doi: 10.3389/fped.2023.1223692
23. Alshaikh B, Cheung PY, Soliman N, Brundler MA, Yusuf K. Impact of lockdown measures during COVID-19 pandemic on pregnancy and preterm birth. Am J Perinatol. (2022) 39(3):329–36. doi: 10.1055/s-0041-1739357
Keywords: COVID-19, lockdown, birth weight, China, pregnant woman
Citation: Chen Y, Fan J, Li X, Ye Y, Lv Y, Zheng S, Hu J, Pu Y and Liu T (2024) Associations of COVID-19 lockdown with birth weight in China. Front. Pediatr. 12:1336108. doi: 10.3389/fped.2024.1336108
Received: 10 November 2023; Accepted: 8 January 2024;
Published: 22 January 2024.
Edited by:
Jiayuan Wu, Affiliated Hospital of Guangdong Medical University, ChinaReviewed by:
Zhiqiang Nie, Guangdong Provincial People's Hospital, China© 2024 Chen, Fan, Li, Ye, Lv, Zheng, Hu, Pu and Liu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yudong Pu eGlueXVueGluMjAwMUAxNjMuY29t Tao Liu Z3p0dF8yMDAyQDE2My5jb20=
†These authors have contributed equally to this work and share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.