
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Pediatr., 06 February 2024
Sec. Children and Health
Volume 12 - 2024 | https://doi.org/10.3389/fped.2024.1287343
Objectives: The current study aimed to examine the potential transgenerational associations between maternal pain and depressiveness and childhood pain, and to explore the associations between the children's difficulties and recurrent pain (defined as pain occurring at least once a month in the previous 6 month) in healthy children aged 3–13 years.
Methods: We collected Data between 2015 and 2019 as part of the LIFE Child study in Germany and investigated associations of maternal pain and depressiveness, child age, sex, pubertal stage, emotional difficulties, conduct difficulties, hyperactivity/inattention, peer group difficulties, and prosocial skills, and family socioeconomic status with the frequency of parent-perceived headache, backache, and stomachache in a sample of 1,850 children (4,819 documented visits) using logistic and ordinal regression analyses.
Results: Overall, 10.4%, 24.4%, and 45.2% of parents reported their children had recurrent backache, headache, and stomachache, respectively, with 5.5% of children were reported to experience all three types of pain simultaneously. Higher age, female sex, puberty, emotional difficulties, low family socioeconomic status, as well as higher maternal impairment due to pain and maternal depressiveness were significantly associated with more frequent pain.
Conclusions: Our study suggests that maternal pain, maternal depressiveness, and lower family socioeconomic status as well as child's emotional difficulties are significantly associated with a higher frequency of recurrent pain in children perceived by their parents.
Recurrent pain is pain that reoccurs over time. It is a common health issue in childhood (1) that significantly impacts the health and well-being not only of the child but also of their families (2). Recurrent pain is associated with lower quality of life (3), reduced school attendance (4), decreased social participation (5) and compromised emotional functioning (6) in children. Although recurrent pain in children is not bound to a specific diagnosis (7), it can manifest as chronic pain, i.e., pain that persists or recurs for at least three months (8). Prevalence data for children and adolescents varies due to differences in definitions, pain assessments, and populations and was reported to range from 8% to 83% for headache, 4% to 53% for stomachache, and 14% to 24% for backache (1). According to the nationwide “German Health Interview and Examination Survey for Children and Adolescents” (KiGGS) in 2003–2006 (9), the 3-month prevalence of pain recurring at least once per month was 64.5% among children aged 3–10 years, while 9.9% even reported pain at least once per week.
According to Bronfenbrenner's bio-ecological model, child development is influenced by individual differences and several environmental factors acting in different systems, namely the microsystem (interpersonal relationships), the mesosystem (inter-relations between microsystems), the exosystem (e.g., a family's socio-economic position), the macrosystem (conventions in a society), and the chronosystem (development over time) (10). This theory can be applied to various areas of development, including children's perception of pain. Potential risk factors are controversially discussed in the literature. On the individual level, the experience of pain may be influenced by sociodemographic and behavioural parameters. For example, previous studies indicate that girls experience higher levels of pain than boys (11, 12). Also, higher age and an early onset of puberty have been associated with more frequent pain, especially in girls (13, 14). Regarding behavioural characteristics, recurrent pain was shown to be associated with emotional or psychological distress (15). Here, the causal direction might be bidirectional: Emotional difficulties may lead to increased sensitivity to pain (16) while recurrent pain may also lead to emotional difficulties, such as sadness and depression (15). Further, it has been observed that peer group difficulties, such as bullying, are related to recurrent pain (17). On the microsystem level, family stressors, including depressive symptoms in a parent, might affect children's experience of pain (18, 19). It has been observed that children of parents who experienced recurrent pain are more likely to develop pain themselves (20–22). Psychosocial theories suggest that mothers can transmit pain to their children (23–25). Besides genetic and epigenetic factors, family socialization also play a crucial role in shaping how to cope with pain (22). With regard to the exosystem, lower family socioeconomic status has been associated with children's poorer physical and mental health (26, 27), which in turn might increase the risk of recurrent pain (28, 29). Socioeconomic status influences several factors that can lead to recurrent pain in the context of biopsychosocial health, including the environment in which a child grows up, the family, kindergarten and school, as well as other environmental factors such as safety and well-being (27, 30). As other aspects of child development, the perception of pain changes throughout development (chronosystem) and may be subject to social norms (macrosystem).
While previous research often investigated recurrent pain in older children and adolescents (31, 32), the present study assessed recurrent pain and related factors in a sample of younger children and (young) adolescents aged 3–13 years. As the early experience of pain may influence later development (33, 34), it is important to explore which factors relate to pain in early development. Here, we explore individual (child age, sex, and puberty status, but also behavioural difficulties) familial (maternal pain and depressiveness), and socio-economic factors (socio-economic status). Based on previous research finding, we expect that girls, older children, children in puberty, children with mothers experiencing pain or depressiveness, and children with lower socioeconomic status experience higher levels of recurrent pain.
The analyses are based on data collected within the LIFE Child study, a longitudinal prospective study conducted in Leipzig, Germany. Since 2011, this study has been recruiting infants, children, and adolescents from preschools, schools, or public health centres, among others, to investigate determinants of healthy development as well as risk factors for common diseases. Follow-up visits are conducted every year. All parents gave written informed consent before their children were included in the study. The study was designed in accordance with the Declaration of Helsinki and approved by the Ethics Committee of the Medical Faculty of the University of Leipzig (Reg. No. 477/19-ek). The LIFE Child study has been described in more detail elsewhere (35, 36). Children aged 3.0–13.5 years who participated at least once in the LIFE Child study between January 2015 and December 2019 and for whom information on pain, socioeconomic status, age, and sex was available were eligible for the current analysis. A total of 1,850 children (862 (46.59%) girls and 988 (53.41%) boys) met these criteria. 1,266 of these children (68%) had participated at more than one time point, and 888 (48%) had participated more frequently than twice. The number of participants and the number of observations for each of the used questionnaires is shown in the Supplementary Table S1.
All questionnaires used in the present study were completed by children's parents on a computer screen during the visit at the LIFE Child study center.
The frequency of parent-perceived pain among children was assessed using the parent-report form of a short version of the Gießen Complaints Form (GBB-KJ) (37, 38). It assesses the frequency of eight subjective health complaints within the last six months. The frequency is rated on a 5-point Likert scale (0 = rarely or never, 1 = once a month, 2 = almost every week, 3 = several times per week, 4 = daily). In our analysis, three pain items were considered, namely headache, stomachache, and backache. The GBB-KJ has been validated in 4- to 18-year-old children (37, 38).
The parent-report version of the Strengths and Difficulties Questionnaire (39, 40) was used to assess children's behavioural difficulties. The 25 items of this screening instrument comprise the following five scales: emotional difficulties, conduct difficulties, hyperactivity/inattention, peer group difficulties, and prosocial skills. Scores on each scale range from 0 to 10, with higher scores indicating more child's difficulties or—in the case of prosocial skills—child's strengths (41). The SDQ has been validated several times for children aged 4 years and older (39), but was already used for children aged as young as three years (42). In our study, cronbach's alpha, a marker for internal consistency/reliability, was 0.65 for emotional difficulties, 0.62 for hyperactivity/inattention, 0.56 for conduct difficulties, 0.63 for peer group difficulties, and 0.62 for prosocial skills, which represents an intermediate internal reliability.
Puberty stages were assessed by trained study assistants based on Tanner's Sexual Maturity Rating (SMR). SMR is an objective classification system used to document and track the development and sequence of secondary sexual characteristics in children during puberty (43). Tanner stage 1 was defined as prepubertal, while Tanner stage >1 was defined as pubertal (44).
The mental health condition of participants' mothers was assessed using the Patient Health Questionnaire (45). The questionnaire was completed by mothers themselves. It is based on the diagnostic criteria in the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV) (46). We analysed the depressiveness scale, which comprises 9 items answered on a 4-point Likert scale (0–3 level of intensity) (47). Final scores range from 0 to 27, with higher scores indicating more depressive symptoms in the past four weeks. Cronbach's alpha in the present study for the PHQ-9 questionnaire was 0.84 which represents a good internal reliability.
Mothers' level of impairment by headache, stomachache, and backache (i.e., the same pain symptoms as assessed in children) in the past two weeks was assessed using the validated somatoform disorder scale of the Patient Health Questionnaire (45). The questionnaire was completed by mothers themselves. Each item was answered on a 3-point Likert scale, with higher scores indicate more impairment by pain (48).
The family's socioeconomic status (SES) was assessed using a parent-reported questionnaire including questions on their education, occupation, and equivalised disposable income. Information on these three parameters is combined to a composite score ranging from 3 to 21, with higher scores indicating higher SES (49, 50). We followed the categorization proposed by the KiGGS study (51) and divided our observations into three groups: low SES (3–9 points), middle SES (10–15 points), and high SES (16–21 points).
All statistical analyses were performed using R version 4.1.2 (52). In a first step, to assess the associations of child characteristics and family characteristics with child's pain (dependent variable as ordinal scale), ordinal regression analyses with one predictor (unadjusted models) were performed using the cumulative link mixed model (53), referenced as Model 1, in Tables 1, 2. In addition, to determine which predictor explained the variation in child's pain best, we used Nakagawa's R-squared to assess the proportion of variance explained by the independent variables (Supplementary Table S8) (54). In a second step, all characteristics that showed significant associations in the ordinal analyses (unadjusted models) were included in a multivariate ordinal regression analysis. One multivariate analysis was performed for child characteristics and another for family characteristics, referenced as Model 2, in Tables 3, 4. For all analyses, we also employed logistic regression models. In our logistic regression analyses we dichotomized the variable for each of the three domains of pain, and chose pain occurring at least once per month, i.e., response categories 1–4, as the threshold. Logistic regression results with one predictor (unadjusted models) are presented in the Supplements as Model 3 in Supplementary Tables S2, S3 and multivariate logistic regression results are presented in the Supplements as Model 4 in Supplementary Tables S4, S5. We additionally tested for interactions with the child's sex and age in unadjusted models, see in the Supplementary Tables S6, S7. All models were adjusted for multiple measurements per subject and multiple subjects per family by including a nested random effect. Results are presented as odds ratios, including the 95% confidence interval (CI).
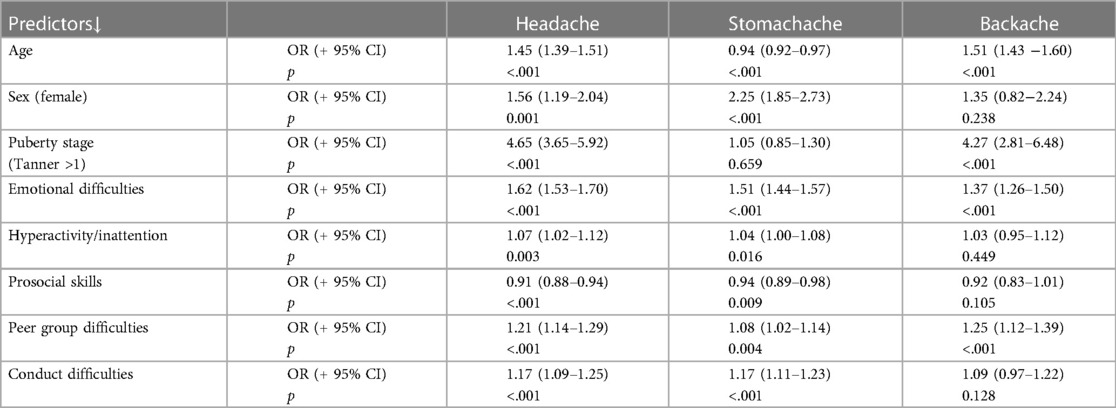
Table 1. Model 1 ordinal analyses (unadjusted models): associations between child pain and child characteristics (3–13-year-olds, in 2015–2019, observations = 4,819). OR = Odds ratio (+95% confidence interval), controlled for multiple visits, and family relationships within the sample (as random effect).
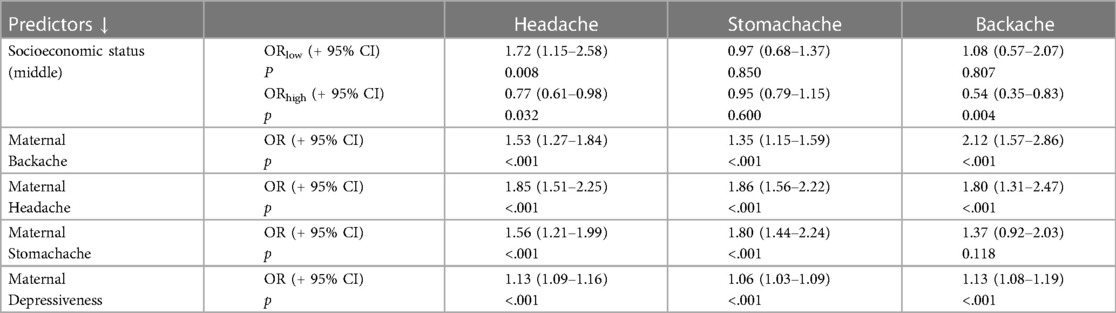
Table 2. Model 1 ordinal analyses (unadjusted models): associations between child pain and family characteristics (3–13-year-olds, in 2015–2019, observations = 4,819). OR = Odds ratio (+ 95% Confidence interval), controlled for sex, age, multiple visits, and family relationships within the sample (as random effect).
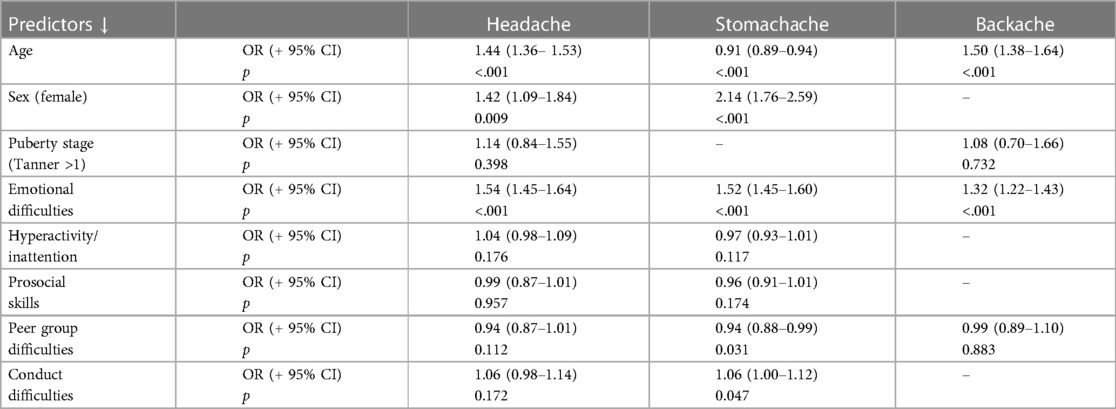
Table 3. Model 2 ordinal multivariate analyses: associations between pain and child characteristics (3–13-year-olds, in 2015–2019, observations = 4,819). OR = Odds ratio (+ 95% Confidence interval), controlled for multiple visits, and family relationships within the sample (as random effect).
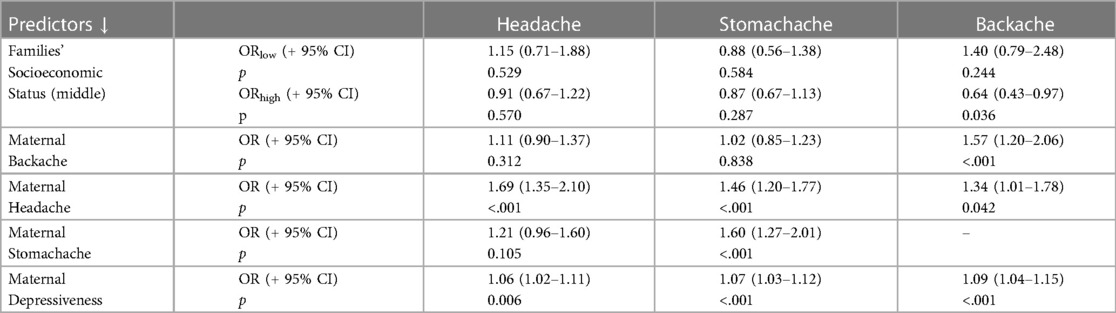
Table 4. Model 2 ordinal multivariate analyses: associations between pain and family characteristics (3–13-year-olds, in 2015–2019, observations = 4,819). OR = Odds ratio (+ 95% Confidence interval), controlled for sex, age, multiple visits, and family relationships within the sample (as random effect).
The following descriptive results are based on information from the participants' first study visit (n = 1,850). The mean age was 7.0 (SD = 3.3). Most children (38.2%) were 3–4 years old. The distribution of sex was 988 (53.4%) male to 862 (46.6%) female. Regarding SES, children from families with low SES were underrepresented (7.7%), while children from families with high SES were overrepresented (38.7%). With respect to pain, recurrent headache was reported for 25.9% of girls and 23.2% of boys. Nearly half of the children (45.3%) were reported to have recurrent stomachache (52.8% of girls, 38.8% of boys), while recurrent backache was less common, reported for only 11.5% of girls and 9.4% of boys. In total, 54.3% of all children were reported to have recurrent pain in at least one domain. 4.4% of the children were reported to have recurrent pain in all three domains simultaneously. While a relatively large group of children (26.6%) were reported to only have recurrent stomachache (in the absence of recurrent headache or backache), very few children were reported to have only recurrent headache (5.4%) or only recurrent backache (1.9%), see Figure 1.
Figure 2 shows the distribution of recurrent pain by age group and SES. Backaches tended to increase with age, with a prevalence of under 1% in 3–4 and 5–6-year-olds, 2.5% in 9–10-year-olds, and 5.8% in 11–13-year-olds. Regarding headache, the prevalence increased with growing age, especially in 11- to 13-year-olds. In contrast to backache und headache, the prevalence of stomachache was especially high in 3- to 4-year-olds and decreased with growing age. Regarding SES, recurrent pain was reported more frequently in children from families with a middle SES.
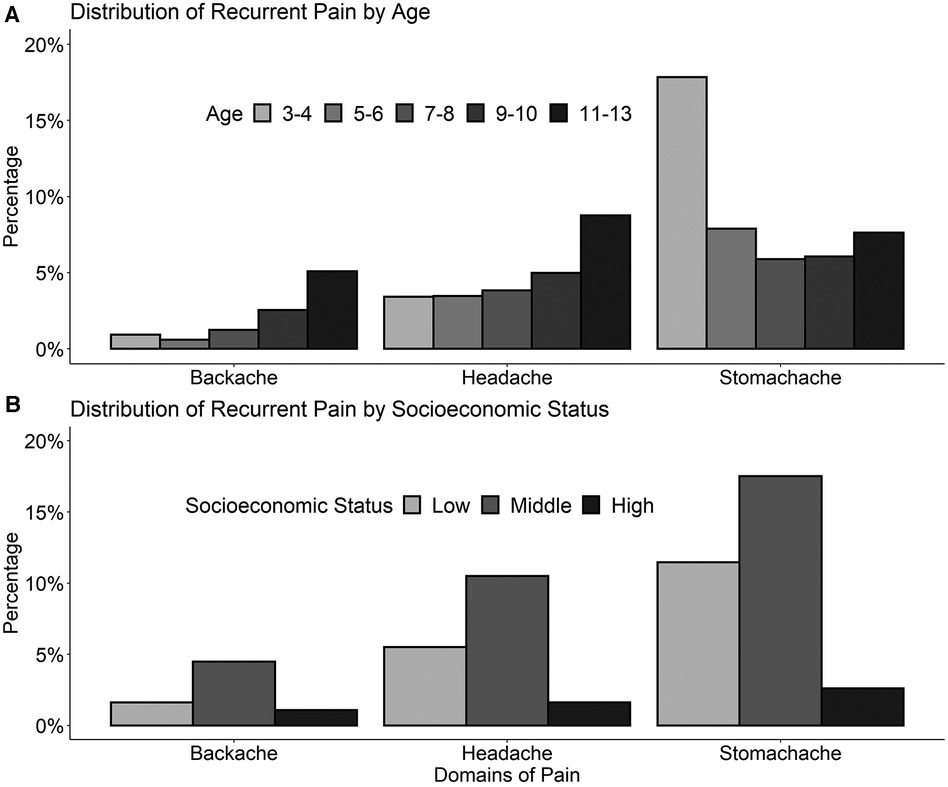
Figure 2. Frequency of recurrent stomachache, backache, and headache in 3- to-13-year-old children (n = 1,850) stratified by age (A), and socioeconomic status (B) recurrent pain was defined as pain at least once per month.
The distributions of the other variables (puberty, behavioural difficulties, maternal depressiveness, and pain) are shown in Table 5.
The following analyses were performed in the whole sample, including all follow-up visits. Odds ratios (OR) report the strengths of the association between the independent variables and the frequency of recurrent pain. In ordinal analyses (Table 1, Model 1), regarding age, we found a significant negative association with stomachache [ORstomachache = 0.94 (0.92–0.97), p < .001] and significant positive associations with headache (ORheadache = 1.45 (1.39–1.51 p < .001) and backache [ORbackache = 1.51 (1.43–1.60) p < .001]. Compared to boys, girls were reported to have significantly more headache [ORheadache = 1.56 (1.19–2.04) p < .001] and stomachache [ORstomachache = 2.25 (1.85–2.73) p < .001]. Children in puberty (Tanner >1) were reported to have headache and backache more frequently than prepubertal children (Tanner = 1) (ORheadache = 4.65 (3.65–5.92), p < .001, ORbackache = 4.27 (2.81–6.48), p < .001). The association between pubertal stage and headache was significantly stronger in girls than in boys [ORIA = 1.99 (1.23–3.22), p = 0.005], see Supplementary Table S6 for all interactions results.
Emotional and peer group difficulties were associated with a significantly increased frequency of pain reports in all three domains headache, stomachache, and backache (Table 1 Model 1). The association between backache and emotional difficulties was weaker in girls than boys [ORIA = 0.84 (0.70–0.99), p = 0.040], and became more pronounced as children's age increased [ORIA = 1.03 (1.00–1.05), p = 0.021] (Supplementary Table S6). Regarding symptoms of hyperactivity/inattention, conduct difficulties and poorer prosocial skills were associated with a significantly higher frequency of headache and stomachache (Table 1 Model 1). The results of the multivariate ordinal regression (Table 3 and Table 4 Model 2) analyses on the associations between pain and child characteristics are presented in Figure 3 (upper panel). As can be seen, associations with age, sex, and emotional difficulties remained significant, while associations with other child's difficulties did not.
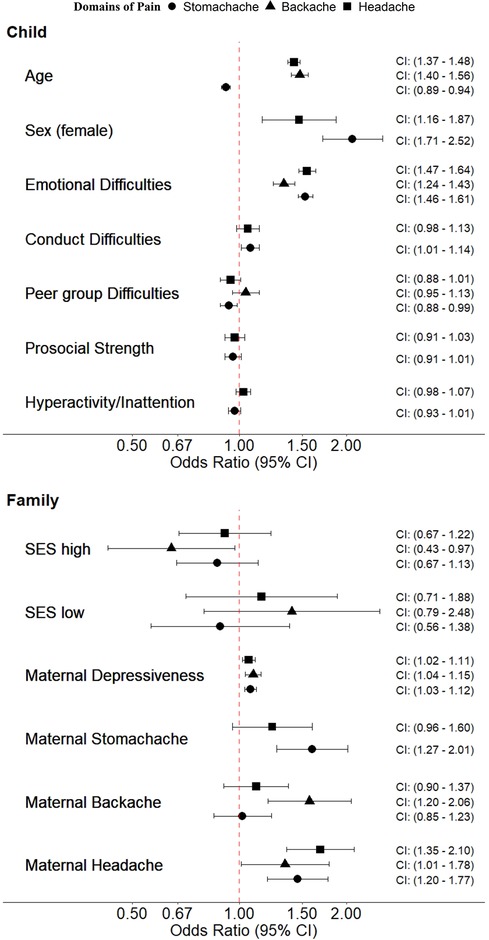
Figure 3. Associations between child and family-related characteristics with recurrent headache, stomachache, and backache. The figure visualizes the two multivariate ordinal models for the child's and family's characteristics with odds ratios including the 95% confidence intervals. Only characteristics that were significantly associated in the unadjusted models were included in the multivariate models.
Mothers' reports of their own pain impairment were associated with more frequent pain in their children in all three domains, e.g., maternal backache [ORbackache = 2.12 (1.57–2.86), p < .001], or maternal headache [ORheadache = 1.85 (1.51–2.25), p < .001] (Table 2 Model 1). The association between mothers' and children's backaches became more pronounced as children's age increased, e.g., ORIA = 1.13 (1.03–1.24), p = 0.011 (see Supplementary Table S7). Maternal depressive symptoms were associated with pain in all three domains e.g., headache ORheadache = 1.13 (1.09–1.16), p < .001 (Table 2 Model 1). The association between maternal depressiveness and stomachache in children was stronger in girls than boys: ORIA = 1.06 (1.01–1.11), p = 0.021. Compared to children from families with middle SES, children from high SES families reported back pain significantly less frequently, while children from low SES families reported headache significantly more frequently (e.g., ORheadache/SESlow = 1.72 (1.15–2.58), p = 0.008 and ORbackache/SEShigh = 0.54 (0.35–0.83), p = 0.004), (see Table 2 Model 1). In multivariate ordinal analyses, most associations, especially those between pain and maternal depressive symptoms and maternal pain in the same domain, remained significant (see Figure 3 and Tables 3, 4). In general, the results of the logistic models confirm those of the ordinal analyses.
In line with other studies (1, 4, 9, 55) our results indicate a high prevalence of recurrent pain among 3–13-year-old children growing up in an urban environment in Germany. Importantly, we found a higher prevalence of pain in childhood than the representative German KiGGS study (55). For example, in our study, the prevalence of recurrent stomachache and recurrent headaches in girls were 45.2% and 24.4%, respectively, compared to 33.7% and 20.1% in the KIGGS study. One possible explanation for these differences is that our sample was more homogeneous and basically included children from urban regions only.
In line with the bio-ecological approach of Bronfenbrenner, the findings of the present study suggest that children's experience of pain, as one facet of child development, is shaped by several individual and environmental factors. Regarding individual factors, our findings indicate that pain frequency increases with age and the onset of puberty, which is consistent with previous research (1, 4, 13, 14, 56). In contrast to another previous study, this association was more pronounced in girls than in boys (57). Potential explanations of sex differences concern hormones, as oestrogen can affect pain sensitivity and perception (58). Further, there are sex differences in pain processing, which may at least partly be socio-culturally driven, in the sense that showing or admitting to be in pain is more accepted in girls than boys (59). It is important to note that differences in frequency between sexes persist into adulthood, so there may be other contributing factors (60). However, we also found that the association between back pain and emotional difficulties was stronger in boys than in girls. This may be an indication that boys are more likely than girls to have back pain when they have emotional difficulties. As expected (61, 62), emotional difficulties were an important dependent variable associated with pain, which may be considered as the internalizing character of recurrent pain (63).
Regarding family characteristics (microsystem), our findings suggest that maternal health is also associated with pain in children. If a child's mother reported more depressive symptoms, the frequency of recurrent pain in all three domains increased. In contrast, in a meta-analysis from 2020, the non-significant pooled correlation coefficient suggested that there was no consistent association between parental depression and pain frequency in children (64). In addition, our analyses revealed a significant association between a mother's pain and her child's pain of the same type. This correlation was also observed for all three domains of recurrent pain in the current study, even in multivariate analyses. Previous studies analysing the association between parents with recurrent pain and their children's risk of reporting recurrent pain found that these children are more likely to have recurrent pain than children whose parents do not have recurrent pain (2, 31, 65, 66) and our results generally confirm this association.
On the exosystem level, we showed that lower socioeconomic status was associated with more backache and headache. This association could be due to fewer resources available in terms of education and financial or emotional assets, which could lead to lower health awareness or pain coping strategies (28–30, 67).
In summary, our findings suggest that maternal health, including impairment by pain and depressive symptoms, is associated with more frequent pain in children. These transgenerational correlations show that it is necessary to consider pain and depressiveness in mothers to understand recurrent pain in childhood. Furthermore, our results suggest that emotional and conduct difficulties, peer group interactions, and pubertal changes are key factors associated with the frequency of recurrent pain in children.
One critical limitation of the study is the lack of investigation of paternal pain/ depressiveness in contrast to maternal pain/ depressiveness, caused by the small observation size of fathers participating in the LIFE Child study. Also, the observation is relatively homogeneous considering the socioeconomic status, e.g., low SES families were underrepresented in our study, which may limit the generalisability of the findings. Our mothers' reports of their children's pain may have been influenced by their own pain impairment. Further, there is the potential of recall bias, as depressed mothers could be more likely to report higher frequency of pain in their children than others. Also, the potential influence of drug therapy on maternal factors was not examined. Another limitation of this study is that we did not include social factors, such as quality of life, among the factors influencing the development of recurrent pain in childhood. Additionally, we did not consider school attendance frequencies or other school-specific variables among school-aged older children. While the questionnaire Gießen Complaints Form (GBB-KJ) and the Strengths and Difficulties Questionnaire (SDQ), are formally validated for children aged 4 and older, it is worth noting that in our study, we also administered the questionnaire to children as young as 3 years. Finally, we performed cross-sectional analysis. Therefore, assumptions on causality are not possible.
The strengths of the study include its large observation size, controlling for multiple visits and family relationships within the observation, the investigation of interactions with sex and age and the distinction between three specific domains of pain.
In conclusion, this study provides insight into several factors associated with parent-perceived recurrent pain in children. Child characteristics such as age, sex, and emotional difficulties were significantly associated with pain frequency in several domains. In addition, family characteristics such as lower socioeconomic status, maternal pain and maternal depressive symptoms were also associated with increased pain frequency in children. The finding that a specific type of pain (e.g., back pain) in the mother was associated with the same type of pain in the child (i.e., back pain) provides additional support for the existence of a transgenerational correlation between pain of the mother and pain of the child. The findings underline the importance of a multi-dimensional assessment of pain, considering both child and family factors.
Data cannot be shared publicly because of ethical restrictions. Publishing data sets is not included in the informed consent provided by the study participants. Furthermore, the data protection concept of LIFE requests that all (external as well as internal) researchers interested in accessing the data sign a project agreement. Researchers who are interested in accessing and analysing data collected in the LIFE Child study may contact the data use and access committeeZG1AbGlmZS51bmktbGVpcHppZy5kZQ==.
The studies involving humans were approved by Ethics Committee of the Medical Faculty of the University of Leipzig (Reg. No. 477/19-ek). The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants’ legal guardians/next of kin.
LP: conceptualization, data analysis, writing – original draft. TP: data analysis, writing – review & editing. MV: data analysis, writing – review & editing. CM: data analysis, writing – review & editing. WK: supervision, writing – review & editing. AH: conceptulization, supervision, writing – review & editing.
The author(s) declare financial support was received for the research, authorship, and/or publication of this article.
This publication was supported by LIFE Child—Leipzig Research Center for Civilization Diseases, Paediatric Clinic, University of Leipzig. LIFE is funded by means for the European Union, the free state of Saxony, the European Social Fund (ESF), and the European Regional Development Fund (ERDF). Further, this publication was funded by the Open Access Publishing Fund of Leipzig University supported by the German Research Foundation within the program Open Access Publication Funding.
We would like to thank all the children and their families who took part in the LIFE child study and all the study assistants for the data collection.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fped.2024.1287343/full#supplementary-material
1. King S, Chambers CT, Huguet A, MacNevin RC, McGrath PJ, Parker L, et al. The epidemiology of chronic pain in children and adolescents revisited: a systematic review. Pain. (2011) 152:2729–38. doi: 10.1016/j.pain.2011.07.016
2. Bradshaw S, Brinkley A, Scanlan B, Hopper L. The burden and impact of recurrent abdominal pain—exploring the understanding and perception of children and their parents. Health Psychol Behav Med. (2022) 10:888–912. doi: 10.1080/21642850.2022.2121710
3. Petersen S, Hägglöf BL, Bergström EI. Impaired health-related quality of life in children with recurrent pain. Pediatrics. (2009) 124:e759–67. doi: 10.1542/peds.2008-1546
4. Roth-Isigkeit A, Thyen U, Stöven H, Schwarzenberger J, Schmucker P. Pain among children and adolescents: restrictions in daily living and triggering factors. Pediatrics. (2005) 115:e152–62. doi: 10.1542/peds.2004-0682
5. Forgeron PA, King S, Stinson JN, McGrath PJ, MacDonald AJ, Chambers CT. Social functioning and peer relationships in children and adolescents with chronic pain: a systematic review. Pain Res Manag. (2010) 15:27–41. doi: 10.1155/2010/820407
6. Lumley MA, Cohen JL, Borszcz GS, Cano A, Radcliffe AM, Porter LS, et al. Pain and emotion: a biopsychosocial review of recent research. J Clin Psychol. (2011) 67:942–68. doi: 10.1002/jclp.20816
7. Zeiter DK, Hyams JS. Recurrent abdominal pain in children. Pediatr Clin North Am. (2002) 49:53–71. doi: 10.1016/s0031-3955(03)00108-1
8. Treede R-D, Rief W, Barke A, Aziz Q, Bennett MI, Benoliel R, et al. A classification of chronic pain for ICD-11. Pain. (2015) 156:1003–7. doi: 10.1097/j.pain.0000000000000160
9. Ellert U, Neuhauser H, Roth-Isigkeit A. Schmerzen bei kindern und jugendlichen in deutschland: prävalenz und inanspruchnahme medizinischer leistungen. Ergebnisse des kinder- und jugendgesundheitssurveys (KiGGS). Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. (2007) 50:711–7. doi: 10.1007/s00103-007-0232-8
10. Bronfenbrenner U. Ecology of the family as a context for human development: research perspectives. Dev Psychol. (1986) 22:723–42. doi: 10.1037/0012-1649.22.6.723
11. Bartley EJ, Fillingim RB. Sex differences in pain: a brief review of clinical and experimental findings. Br J Anaesth. (2013) 111:52–8. doi: 10.1093/bja/aet127
12. Stevens BJ. Oxford Textbook of Pediatric Pain. Oxford: Oxford University Press Incorporated (2021). 713 p.
13. Rhee H. Relationships between physical symptoms and pubertal development. J Pediatr Health Care. (2005) 19:95–103. doi: 10.1016/j.pedhc.2004.10.004
14. Stanford EA, Chambers CT, Biesanz JC, Chen E. The frequency, trajectories and predictors of adolescent recurrent pain: a population-based approach. Pain. (2008) 138:11–21. doi: 10.1016/j.pain.2007.10.032
15. IsHak WW, Wen RY, Naghdechi L, Vanle B, Dang J, Knosp M, et al. Pain and depression: a systematic review. Harv Rev Psychiatry. (2018) 26:352–63. doi: 10.1097/HRP.0000000000000198
16. Bushnell MC, Ceko M, Low LA. Cognitive and emotional control of pain and its disruption in chronic pain. Nat Rev Neurosci. (2013) 14:502–11. doi: 10.1038/nrn3516
17. Gini G. Associations between bullying behaviour, psychosomatic complaints, emotional and behavioural problems. J Paediatr Child Health. (2008) 44:492–7. doi: 10.1111/j.1440-1754.2007.01155.x
18. Beardslee WR, Gladstone TR, O’Connor EE. Transmission and prevention of mood disorders among children of affectively ill parents: a review. J Am Acad Child Adolesc Psychiatry. (2011) 50:1098–109. doi: 10.1016/j.jaac.2011.07.020
19. Goodman SH, Gotlib IH. Risk for psychopathology in the children of depressed mothers: a developmental model for understanding mechanisms of transmission. Psychol Rev. (1999) 106:458–90. doi: 10.1037/0033-295x.106.3.458
20. Øster J. Recurrent abdominal pain, headache and limb pains in children and adolescents. Pediatrics. (1972) 50:429–36. doi: 10.1542/peds.50.3.429
21. Hotopf M. Childhood experience of illness as a risk factor for medically unexplained symptoms. Scand J Psychol. (2002) 43:139–46. doi: 10.1111/1467-9450.00279
22. Edwards PW, Zeichner A, Kuczmierczyk AR, Boczkowski J. Familial pain models: the relationship between family history of pain and current pain experience. Pain. (1985) 21:379–84. doi: 10.1016/0304-3959(85)90166-6
23. Descalzi G, Ikegami D, Ushijima T, Nestler EJ, Zachariou V, Narita M. Epigenetic mechanisms of chronic pain. Trends Neurosci. (2015) 38:237–46. doi: 10.1016/j.tins.2015.02.001
24. Main CJ. The importance of psychosocial influences on chronic pain. Pain Manag. (2013) 3:455–66. doi: 10.2217/pmt.13.49
25. Buskila D. Genetics of chronic pain states. Best Pract Res Clin Rheumatol. (2007) 21:535–47. doi: 10.1016/j.berh.2007.02.011
26. Poulain T, Vogel M, Sobek C, Hilbert A, Körner A, Kiess W. Associations between socio-economic status and child health: findings of a large German cohort study. Int J Environ Res Public Health. (2019) 16(5):677. doi: 10.3390/ijerph16050677
27. Herrmann J, Vogel M, Pietzner D, Kroll E, Wagner O, Schwarz S, et al. Factors associated with the emotional health of children: high family income as a protective factor. Eur Child Adolesc Psychiatry. (2018) 27:319–28. doi: 10.1007/s00787-017-1049-0
28. Kivimäki M, Batty GD, Pentti J, Shipley MJ, Sipilä PN, Nyberg ST, et al. Association between socioeconomic status and the development of mental and physical health conditions in adulthood: a multi-cohort study. Lancet Public Health. (2020) 5:e140–9. doi: 10.1016/S2468-2667(19)30248-8
29. Schreier HM, Chen E. Socioeconomic status and the health of youth: a multilevel, multidomain approach to conceptualizing pathways. Psychol Bull. (2013) 139:606–54. doi: 10.1037/a0029416
30. Reiss F, Meyrose A-K, Otto C, Lampert T, Klasen F, Ravens-Sieberer U. Socioeconomic status, stressful life situations and mental health problems in children and adolescents: results of the German BELLA cohort-study. PLoS One. (2019) 14:e0213700. doi: 10.1371/journal.pone.0213700
31. Grøholt E-K, Stigum H, Nordhagen R, Köhler L. Recurrent pain in children, socio-economic factors and accumulation in families. Eur J Epidemiol. (2003) 18:965–75. doi: 10.1023/a:1025889912964
32. Ragnarsson S, Myleus A, Hurtig A-K, Sjöberg G, Rosvall P-Å, Petersen S. Recurrent pain and academic achievement in school-aged children: a systematic review. J Sch Nurs. (2020) 36:61–78. doi: 10.1177/1059840519828057
33. Brattberg G. Do pain problems in young school children persist into early adulthood? A 13-year follow-up. Eur J Pain. (2004) 8:187–99. doi: 10.1016/j.ejpain.2003.08.001
34. Victoria NC, Murphy AZ. Exposure to early life pain: long term consequences and contributing mechanisms. Curr Opin Behav Sci. (2016) 7:61–8. doi: 10.1016/j.cobeha.2015.11.015
35. Poulain T, Baber R, Vogel M, Pietzner D, Kirsten T, Jurkutat A, et al. The LIFE child study: a population-based perinatal and pediatric cohort in Germany. Eur J Epidemiol. (2017) 32:145–58. doi: 10.1007/s10654-016-0216-9
36. Quante M, Hesse M, Döhnert M, Fuchs M, Hirsch C, Sergeyev E, et al. The LIFE child study: a life course approach to disease and health. BMC Public Health (2012) 12:1021. doi: 10.1186/1471-2458-12-1021
37. Barkmann C, Mack B, Brähler E, Schulte-Markwort M. Der gießener beschwerdebogen für kinder und jugendliche (GBB-KJ): faktorielle validität, reliabilität und gesamtdeutsche normierung für 4- bis 18-jährige im eltern- und selbsturteil. Diagnostica. (2008) 54:99–111. doi: 10.1026/0012-1924.54.2.99
38. Kliem S, Lohmann A, Klatt T, Mößle T, Rehbein F, Hinz A, et al. Brief assessment of subjective health complaints: development, validation and population norms of a brief form of the Giessen subjective complaints list (GBB-8). J Psychosom Res. (2017) 95:33–43. doi: 10.1016/j.jpsychores.2017.02.003
40. Hoofs H, Jansen NW, Mohren DC, Jansen MW, Kant IJ. The context dependency of the self-report version of the strength and difficulties questionnaire (SDQ): a cross-sectional study between two administration settings. PLoS One. (2015) 10:e0120930. doi: 10.1371/journal.pone.0120930
41. He J-P, Burstein M, Schmitz A, Merikangas KR. The strengths and difficulties questionnaire (SDQ): the factor structure and scale validation in U.S. adolescents. J Abnorm Child Psychol. (2013) 41:583–95. doi: 10.1007/s10802-012-9696-6
42. Maurice-Stam H, Haverman L, Splinter A, van Oers HA, Schepers SA, Grootenhuis MA. Dutch norms for the strengths and difficulties questionnaire (SDQ)—parent form for children aged 2–18 years. Health Qual Life Outcomes. (2018) 16:123. doi: 10.1186/s12955-018-0948-1
43. Marshall WA, Tanner JM. Growth and Physiological Development During Adolescence: Department of Growth and Development, Institute Of Child Health. England: University of London (1968).
44. Emmanuel M, Bokor BR. Tanner Stages. In StatPearls [Internet]. Treasure Island, FL: StatPearls Publishing (2022). PMID: 29262142.
45. Gräfe K, Zipfel S, Herzog W, Löwe B. Screening psychischer störungen mit dem “gesundheitsfragebogen für patienten (PHQ-D)”. Diagnostica. (2004) 50:171–81. doi: 10.1026/0012-1924.50.4.171
47. Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. (2001) 16:606–13. doi: 10.1046/j.1525-1497.2001.016009606.x
48. Kroenke K, Spitzer RL, Williams JB. The PHQ-15: validity of a new measure for evaluating the severity of somatic symptoms. Psychosom Med. (2002) 64:258–66. doi: 10.1097/00006842-200203000-00008
49. Lampert T, Kroll L, Müters S, Stolzenberg H. Messung des sozioökonomischen Status in der studie zur gesundheit erwachsener in deutschland (DEGS1). Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. (2013) 56:631–6. doi: 10.1007/s00103-012-1663-4
50. Winkler J, Stolzenberg H. Der sozialschichtindex im BundesGesundheitssurvey: nationaler gesundheitssurvey—sozialökonomische umstände—sozialschichtindex. Gesundheitswesen. (1999) 1999:S178–83.
51. Lampert T, Hoebel J, Kuntz B, Müters S, Kroll LE. Robert Koch-Institut, Berlin, Germany. Messung des sozioökonomischen Status und des subjektiven sozialen Status in KiGGS welle 2. Journal of Health Monitoring (2018):20. doi: 10.17886/RKI-GBE-2018-016
52. R Core Team. R: A Language and environment for statistical computing. In R-project.org [Internet]. Vienna: R Foundation for Statistical Computing (2021).
53. Christensen RHB. Cumulative link models for ordinal regression with the R package ordinal (2019).
54. Nakagawa S, Johnson PC, Schielzeth H. The coefficient of determination R2 and intra-class correlation coefficient from generalized linear mixed-effects models revisited and expanded. J R Soc Interface. (2017) 14(134). doi: 10.1098/rsif.2017.0213
55. Krause L, Sarganas G, Thamm R, Neuhauser H. Kopf-, bauch- und rückenschmerzen bei kindern und jugendlichen in deutschland ergebnisse aus KiGGS welle 2 und trends. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. (2019) 62:1184–94. doi: 10.1007/s00103-019-03007-8
56. LeResche L, Mancl LA, Drangsholt MT, Saunders K, Korff M von. Relationship of pain and symptoms to pubertal development in adolescents. Pain (2005) 118:201–9. doi: 10.1016/j.pain.2005.08.011
57. Janssens KA, Rosmalen JG, Ormel J, Verhulst FC, Hunfeld JA, Mancl LA, et al. Pubertal status predicts back pain, overtiredness, and dizziness in American and Dutch adolescents. Pediatrics. (2011) 128:553–9. doi: 10.1542/peds.2010-2364
58. Craft RM, Mogil JS, Aloisi AM. Sex differences in pain and analgesia: the role of gonadal hormones. Eur J Pain. (2004) 8:397–411. doi: 10.1016/j.ejpain.2004.01.003
59. Chaplin TM, Aldao A. Gender differences in emotion expression in children: a meta-analytic review. Psychol Bull. (2013) 139:735–65. doi: 10.1037/a0030737
60. Samulowitz A, Gremyr I, Eriksson E, Hensing G. “Brave men” and “emotional women”: a theory-guided literature review on gender bias in health care and gendered norms towards patients with chronic pain. Pain Res Manag. (2018) 2018:6358624. doi: 10.1155/2018/6358624
61. Koechlin H, Coakley R, Schechter N, Werner C, Kossowsky J. The role of emotion regulation in chronic pain: a systematic literature review. J Psychosom Res. (2018) 107:38–45. doi: 10.1016/j.jpsychores.2018.02.002
62. Strine TW, Okoro CA, McGuire LC, Balluz LS. The associations among childhood headaches, emotional and behavioral difficulties, and health care use. Pediatrics. (2006) 117:1728–35. doi: 10.1542/peds.2005-1024
63. Liu J, Chen X, Lewis G. Childhood internalizing behaviour: analysis and implications. J Psychiatr Ment Health Nurs. (2011) 18:884–94. doi: 10.1111/j.1365-2850.2011.01743.x
64. Donnelly TJ, Palermo TM, Newton-John TR. Parent cognitive, behavioural, and affective factors and their relation to child pain and functioning in pediatric chronic pain: a systematic review and meta-analysis. Pain. (2020) 161:1401–19. doi: 10.1097/j.pain.0000000000001833
65. Beveridge JK, Dobson KS, Madigan S, Yeates KO, Stone AL, Wilson AC, et al. Adverse childhood experiences in parents of youth with chronic pain: prevalence and comparison with a community-based sample. Pain Rep. (2020) 5(6):e866. doi: 10.1097/PR9.0000000000000866
66. Schulte IE, Petermann F, Noeker M. Functional abdominal pain in childhood: from etiology to maladaptation. Psychother Psychosom. (2010) 79:73–86. doi: 10.1159/000270915
67. Barkmann C, Braehler E, Schulte-Markwort M, Richterich A. Chronic somatic complaints in adolescents: prevalence, predictive validity of the parent reports, and associations with social class, health status, and psychosocial distress. Soc Psychiatry Psychiatr Epidemiol. (2011) 46:1003–11. doi: 10.1007/s00127-010-0273-4
Keywords: recurrent pain, maternal pain, maternal depressiveness, children’s behavioural difficulties, socioeconomic status, perceived pain
Citation: Petri L, Poulain T, Vogel M, Meigen C, Kiess W and Hiemisch A (2024) Parent-perceived recurrent pain in children: associations with maternal pain, depressiveness, socioeconomic status, and children's behavioural difficulties. Front. Pediatr. 12:1287343. doi: 10.3389/fped.2024.1287343
Received: 1 September 2023; Accepted: 15 January 2024;
Published: 6 February 2024.
Edited by:
Tonia C. Onyeka, University of Nigeria, NigeriaReviewed by:
Andrea Trombetta, IRCCS Local Health Authority of Reggio Emilia, Italy© 2024 Petri, Poulain, Vogel, Meigen, Kiess and Hiemisch. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Laura Petri cGV0cmkubWVkQHdlYi5kZQ==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.