- 1Department of Paediatrics, Children's Hospital – London Health Sciences Centre, Schulich School of Medicine and Dentistry, Western University, London, ON, Canada
- 2Children's Health Research Institute, London, ON, Canada
- 3Lawson Health Research Institute, London, ON, Canada
- 4Division of Critical Care, Department of Medicine, London Health Sciences Centre, Schulich School of Medicine and Dentistry, Western University, London, ON, Canada
- 5Department of Ethics, London Health Sciences Centre, London, ON, Canada
- 6Department of Family Medicine, Schulich School of Medicine and Dentistry, Western University, London, ON, Canada
- 7Department of Epidemiology and Biostatistics, Schulich School of Medicine and Dentistry, Western University, London, ON, Canada
Background: Potentially inappropriate treatment in critically ill adults is associated with healthcare provider distress and burnout. Knowledge regarding perceived potentially inappropriate treatment amongst pediatric healthcare providers is limited.
Objectives: Determine the frequency and factors associated with potentially inappropriate treatment in critically ill children as perceived by providers, and describe the factors that providers report contribute to the distress they experience when providing treatment perceived as potentially inappropriate.
Methods: Prospective observational mixed-methods study in a single tertiary level PICU conducted between March 2 and September 14, 2018. Patients 0–17 years inclusive with: (1) ≥1 organ system dysfunction (2) moderate to severe mental and physical disabilities, or (3) baseline dependence on medical technology were enrolled if they remained admitted to the PICU for ≥48 h, and were not medically fit for transfer/discharge. The frequency of perceived potentially inappropriate treatment was stratified into three groups based on degree of consensus (1, 2 or 3 providers) regarding the appropriateness of ongoing active treatment per enrolled patient. Distress was self-reported using a 100-point scale.
Results: Of 374 patients admitted during the study, 133 satisfied the inclusion-exclusion criteria. Eighteen patients (unanimous - 3 patients, 2 providers - 7 patients; single provider - 8 patients) were perceived as receiving potentially inappropriate treatment; unanimous consensus was associated with 100% mortality on 3-month follow up post PICU discharge. Fifty-three percent of providers experienced distress secondary to providing treatment perceived as potentially inappropriate. Qualitative thematic analysis revealed five themes regarding factors associated with provider distress: (1) suffering including a sense of causing harm, (2) conflict, (3) quality of life, (4) resource utilization, and (5) uncertainty.
Conclusions: While treatment perceived as potentially inappropriate was infrequent, provider distress was commonly observed. By identifying specific factor(s) contributing to perceived potentially inappropriate treatment and any associated provider distress, organizations can design, implement and assess targeted interventions.
Introduction
In 2015, a multi-society (ATS/AACN/ACCP/ESICM/SCCM) policy statement defined potentially inappropriate treatment as treatment sought by a patient or surrogate decision maker that has some possibility of achieving a physiological goal (1); however, clinicians believe the treatment is non-beneficial and is “outside the boundaries of accepted practice due to other ethical considerations” (2). Futile treatment was defined as treatment “that (has) no chance of achieving the intended physiological goal” (1). Despite establishment of a formal definition, fulfillment of the criteria for potentially inappropriate is a matter of perception, and thus like non-beneficial treatment, it includes a subjective values-based judgement (3). The terms, potentially inappropriate treatment and non-beneficial are not synonymous (4). Nonbeneficial treatment emphasizes the lack of expected benefit and the imbalance between the burdens and expected benefits while potentially inappropriate treatment acknowledges that perceptions of appropriateness or benefit are influenced by the preferences, culture and values of patients and providers (4). What constitutes potentially inappropriate is open to interpretation and the associated subjectivity and ambiguity thus prevent objective measurement of potentially inappropriate treatment. To ensure patient goals and values are honored providers in the intensive care unit rely on advance directives and surrogate decision makers to assist in clarifying goals of care based on the patient's known wishes.
As children may not have formed or expressed their own values and wishes due to age or level of cognitive function (5), providers rely heavily on parents and guardians to guide medical decisions. The number of children with chronic critical illness, which is the combination of chronic complex conditions and dependence on medical technology requiring pediatric intensive care unit (PICU) admission, has increased substantially (6, 7). When patients with chronic critical illness require ongoing aggressive treatment, including initiation of invasive medical technology, PICU staff may be more likely to raise concerns about non-beneficial care (3). PICU staff may struggle to meet the needs of these children and their parents and what they believe is in child's best interests; they may perceive this treatment as potentially inappropriate and conflict and distress may result (8). Moral distress is one form of distress providers may experience in the PICU (9); it is “the anguish (experienced) in response to a situation in which the person is aware of a moral problem, acknowledges moral responsibility, and makes a moral judgement about the correct action, yet as a result of real or perceived constraints, participates in perceived moral wrongdoing” (10). Previous studies quantified futility and potentially inappropriate treatment based on definitions that are no longer utilized. These studies focused on resource utilization by patients receiving treatment perceived as potentially appropriate (6, 11). In a UK cross-sectional study of PICU patients, the frequency of futility and perceived potentially inappropriate treatment was solely determined by the unit director at a single point in time (12).
The frequency of perceived potentially inappropriate treatment in PICUs and the distress that may be associated has not been examined to our knowledge. Our primary aim was to prospectively quantify the frequency of perceived potentially inappropriate treatment over 6 months from the PICU nurses and physicians' perspective. We also aimed to describe factors associated with perceived inappropriate treatment, identify whether providing treatment perceived as potentially inappropriate is associated with provider distress and explore factors providers suggest contribute to experiencing distress when providing perceived potentially inappropriate treatment.
Materials and methods
Study design
We conducted a single-center, prospective, observational mixed-methods study approved by Western University Health Sciences Research Ethics Board (#106981) using a sample of convenience. A waiver of consent was approved for patient participants as no identifiable patient information was collected. Written informed consent was required and obtained for individual providers who chose to participate. Research procedures were conducted in accordance with established local and regional ethical standards, and with the Helsinki Declaration of 1975.
Hospital setting
The study was conducted in a medical-surgical tertiary level PICU with 800 admissions per year. The multidisciplinary team included bedside nurses, charge nurses, intensivists, a pharmacist, a dietician, a fellow, respiratory therapists (cross-cover several units in the combined adult/pediatric hospital) and residents from a variety of adult and pediatric sub-/specialties who rotated for four weeks in the PICU.
Patient selection
A research coordinator screened patients in the PICU Monday through Friday between March 2, 2018 and September 14, 2018 for study eligibility. Patients aged 0–17 years inclusive admitted to the PICU for ≥48 h and not medically fit for discharge/transfer at the time of enrollment were included if one of the following was present:
1. Any patient with ≥1 persistent organ system dysfunction
2. Moderate to severe mental and physical disabilities as defined by Baseline Pediatric Cerebral Performance Category (PCPC) (13) score of ≥3 OR baseline Pediatric Overall Performance Category (POPC) (13) score of ≥4 OR baseline Gross Motor Function Classification System (GMFCS) (14) IV or V;
3. Baseline dependence on medical technology including respiratory or feeding support, cerebrospinal fluid shunts, semi-permanent vascular access device or requirement for dialysis.
A patient was excluded from the study if at the time of enrollment, the patient had been (1) admitted to the PICU for less than 48 h, or (2) was medically fit for transfer/discharge to the ward.
Provider selection
The study was restricted to nursing and attending intensivists who were invited to participate following written informed consent. The entire PICU staff complement included 62 nurses and 6 intensivists.
Patient and provider recruitment were conducted separately.
Data collection strategy
We collected provider demographic details and assigned each individual a unique code for completion of the Ongoing Active Intervention questionnaire, herein referred to as questionnaire(s). Utilizing previously published results (15), and expert opinion (pediatric palliative care, pediatric intensive care, and health survey experts), we developed an initial questionnaire that was piloted by both PICU and non-PICU staff and refined through an iterative process. The 21-item questionnaire explored: (1) factors contributing to perceived ongoing potentially inappropriate treatment; (2) whether the provider was experiencing distress, and if so, to describe using free text, the factors to which the distress experienced was attributed (Supplementary Material).
On each study day, the bedside nurse of an eligible patient, charge nurse and intensivist on service were asked, “In your opinion, is ongoing active intervention in the critical care environment for your patient appropriate?”. The research assistant recorded the provider's answer directly into the research database via a portable electronic device. The survey question was administered privately and individually by a research assistant to ensure individual responses were kept confidential. When ongoing intervention was perceived as appropriate, the research coordinator noted the provider's response and the remainder of the questionnaire was not applicable. When ongoing intervention was perceived as potentially inappropriate (i.e., provider stated “No”), the full 21-item questionnaire was administered (See Supplemental Material). The primary objective, frequency of perceived potentially inappropriate treatment, was determined by how often “ongoing active intervention” was considered inappropriate, using three levels of agreement (1, 2, or 3 providers), on any given study day. When the research coordinator noted a difference in opinion regarding the appropriateness of ongoing active intervention between the providers, further questions were not asked of providers who believed that ongoing active intervention was appropriate in order to maintain the established survey methodology and to avoid introducing bias and potentially influencing provider responses.
We collected patient demographics and clinical data including Pediatric Risk of Mortality Score III (PRISM III) and pediatric logistic organ dysfunction (PELOD) at enrollment (marked Day 1). We collected provider questionnaire responses and PELOD scores on Days 1, 3, 5 and 7 and weekly thereafter, until patient death or discharge from PICU rather than on consecutive days to avoid questionnaire fatigue. When a study day fell on a weekend, data were collected the following Monday and subsequent study days were deferred to maintain the appropriate gap between data collection times. We collected outcome data, including disposition and survival at 3 months post PICU discharge.
Statistical Analysis
Continuous variables were summarized using medians and interquartile ranges and comparisons between groups were examined with Mann–Whitney U-tests (or Poisson loglinear regression analysis or Spearman's rank correlation coefficient, as appropriate). Categorical variables were summarized using frequencies and percentages, and comparisons between groups were examined with chi-square tests (or Fisher's exact tests, as appropriate). Patients readmitted to the PICU and perceived as receiving potentially inappropriate treatment during more than one admission were considered separate cases when analyzing patient demographics; however, given level of agreement between providers for these patients did not change over time, these patients were included only once when determining the frequency of perceived potentially inappropriate treatment. All analyses were conducted using SPSS v24 (IBM Corp., Armonk, NY, USA).
Qualitative content analysis of free text responses was conducted after closure of the questionnaire portion of the study using NVivo 12 Pro to manage and code verbatim abstractions and identify “nodes”. A detailed review of the nodes, sub-nodes and related text was independently reviewed by two coders (SC and AS) to confirm the categorization and to consolidate overlapping nodes where possible to establish subthemes. Coders subsequently met and through consensus achieved the first stage of thematic categorization. Subsequent analysis, was performed by a single coder (AS) to further consolidate subthemes into overarching themes.
Results
Potentially inappropriate treatment patient data
During the enrollment period, 420 PICU admissions among 374 unique patients were documented; 133 unique patients met the inclusion criteria (Figure 1). Three participating providers (concurrent bedside nurse, charge nurse and intensivist on duty) unanimously perceived treatment to be potentially inappropriate in 3/133 (2%) patients. One patient had a chronic complex condition, limited cognitive function and a need for medical technology; while another developed the aforementioned following severe hypoxic ischemic injury due to prolonged out of hospital cardiac arrest. The third had advanced cancer with an extremely poor prognosis. Two of the three providers concurrently perceived treatment to be potentially inappropriate in 7/133 (5%) patients and a single provider indicated they perceived potentially inappropriate treatment in 8/133 (6%) patients. The mortality rate at 3-months post PICU discharge was 3/3 (100%), 4/7 (57%) and 0/8 (0%) for the three groups, respectively. Thus, the mortality rate for patients receiving potentially inappropriate treatment as perceived by one or more providers was 7/18 (39%), while the overall PICU mortality rate in 2018 was 22/782 (2.8%) with (p < 0.001). Of the 18/133 patients (14%) perceived as receiving potentially inappropriate treatment, 2 patients required PICU readmission during the study period. Perceived potentially inappropriate treatment was associated with a higher PRISM score (p = 0.02), higher PELOD score (p = 0.03), and longer PICU length of stay (LOS; p < 0.001) but shorter overall hospital LOS (p < 0.001) Table 1.

Figure 1. Patient flow chart, study questionnaire completion and frequency of potentially inappropriate treatment as perceived by health care providers.
Provider data
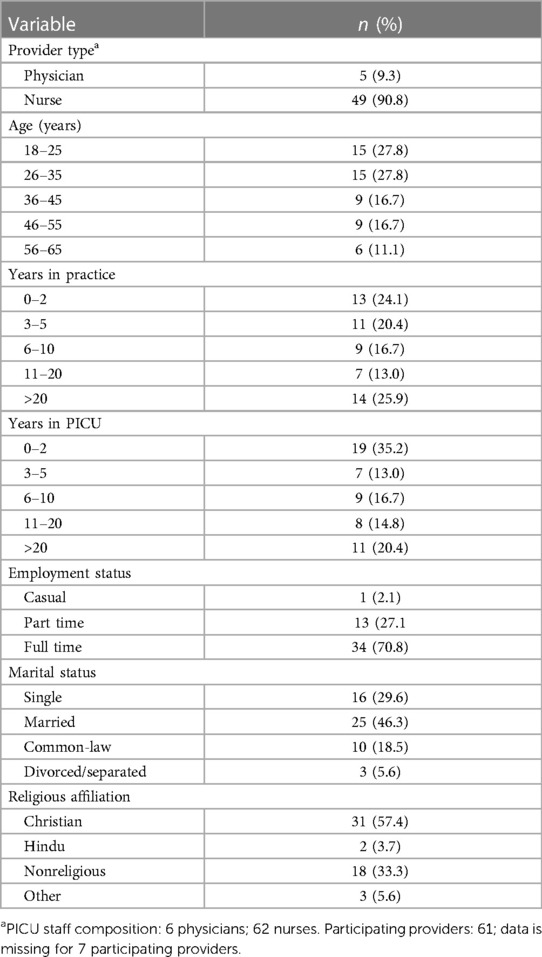
The total PICU staff complement consists of 68 providers (62 nurses and 6 physicians). Sixty-one of 68 eligible providers (56/62, 90% nurses; 5/6, 83% physicians) consented to participate in the study, and 54/61 (88.5%) provided demographic details (Table 2). Questionnaires not completed due to non-participation were marked “missing” for an overall questionnaire completion rate of 94%. Each provider was surveyed a median of 7.5 times (IQR 4.25–12.75) in 6 months. Thirty-three individual providers stated “ongoing active intervention” was not appropriate for the patient 103 times and subsequently completed the 21-item questionnaire. An individual provider completed the full 21-item questionnaire a median of 2 times (IQR 1–4).
The most common reason that providers indicated for perceiving treatment as potentially inappropriate was extremely poor current quality of life; the most common solution providers cited to resolving the situation of perceived potentially inappropriate treatment was patient discharge or demise. A surrogate decision maker's request to continue treatment was the most common reason for ongoing active intervention. In 8/18 (44%) of the patients perceived as receiving potentially inappropriate treatment, one or more providers reported not having a good sense of the patient's/family's wishes, goals and values. While very important, verifying documentation summarizing the patient's/family's goals (if known) was not included within the scope of the current study (Table 3).
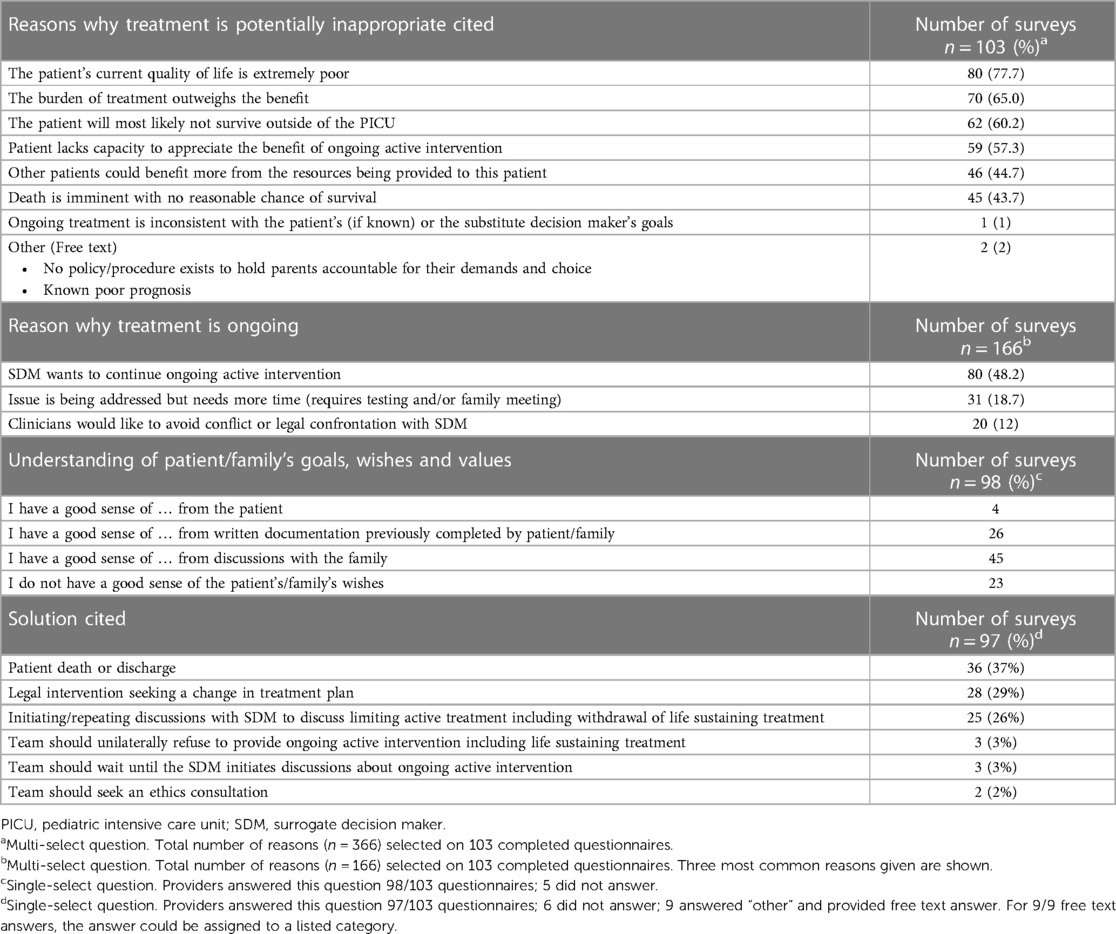
Table 3. Reasons providers cited for why ongoing active intervention was ongoing and was potentially inappropriate, their degree of understanding of patient/family wishes and potential solutions they cited to resolve the situation.
Provider distress
Providers reported experiencing distress secondary to providing treatment they perceived as potentially inappropriate in 93/103 (90%) questionnaires. Thirty-three providers (5/5, 100% participating physicians; 28/56, 50% participating nurses) reported experiencing distress at least once (median = 2, IQR = 1–4) with a median (IQR) intensity of distress measuring 65 (55–81) out of 100 during the study. Seventy-five percent (70/93) of questionnaires in which distress was reported were linked to 3 unique patients (1 required readmission). No significant relationship was found between provider type and the reported intensity or frequency of distress (p = 0.15). No significant correlation was found between frequency and average intensity of distress experienced by an individual provider (p = 0.24).
Initial coding of provider statements regarding factors to which they attributed their distress revealed more than 10 potential subthemes. Secondary analysis aimed at consolidating and collapsing the subthemes produced five overarching themes: (1) suffering including a sense of causing harm, (2) conflict, (3) quality of life, (4) resource utilization, and (5) uncertainty. Suffering was experienced as (a) existential or physical, (b) of the patient, patient's family, or others, and (c) of the provider through a sense of inflicting harm through continued ongoing treatment (Table 4). Conflict was experienced overtly through communication with families described as combative and argumentative, and through openly expressed distrust of the medical team. It was also experienced passively through lack of parental engagement and absent or challenging communication. Although infrequent (n = 4 responses), conflict within the medical team also contributed to provider distress. With prolonged ongoing treatment that was perceived as potentially inappropriate, two separate providers reported “desensitization” and cited it as a protective factor against experiencing further distress.
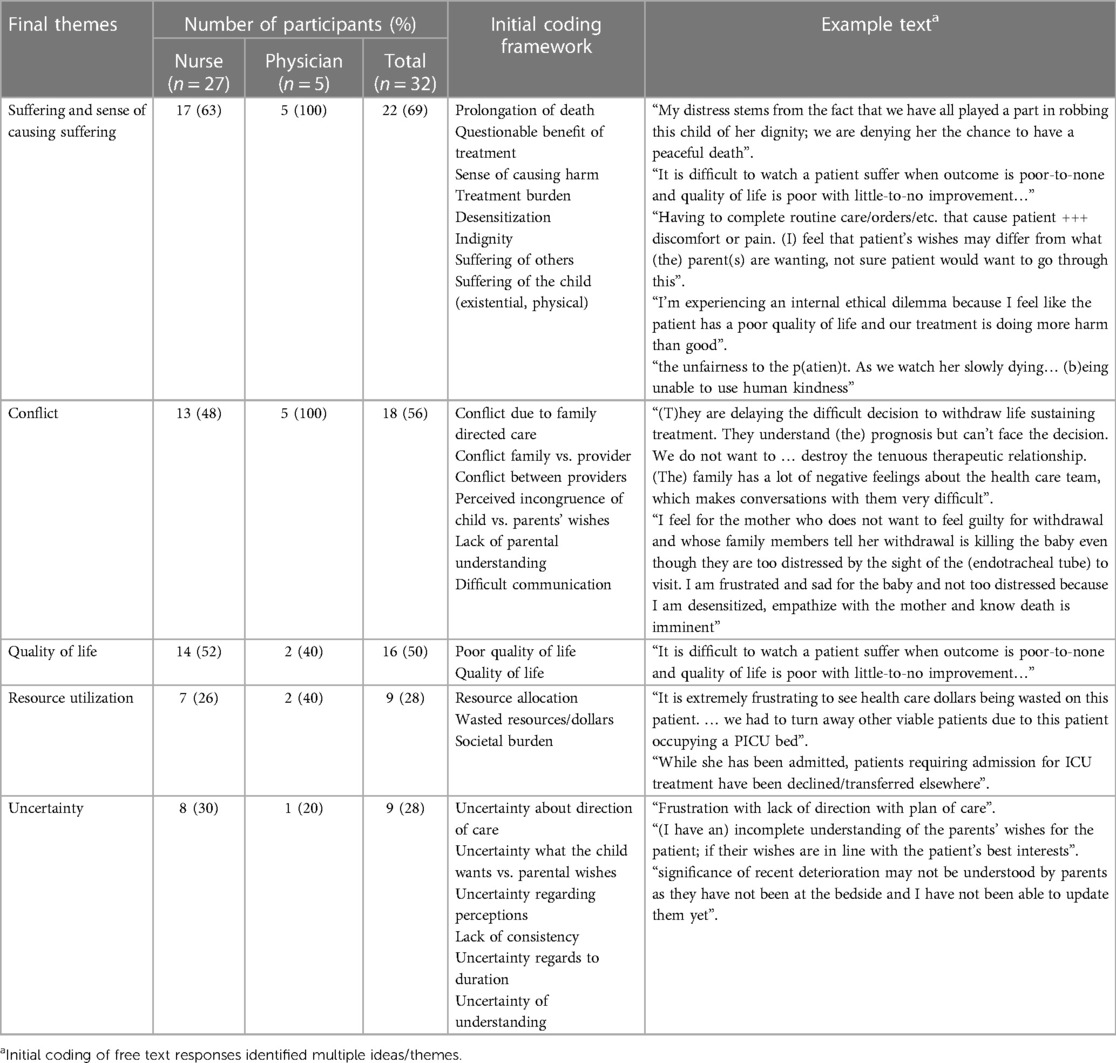
Table 4. Initial coding framework, including example text, and overarching themes providers attributed their distress to when providing potentially inappropriate treatment.
Discussion
The overall frequency of perceived potentially inappropriate treatment in the current study approached 14% based on three differing levels of agreement among providers. Greater degree of provider consensus was associated with higher mortality on follow-up 3 months post PICU discharge. Most importantly, more than one-half of providers experienced distress secondary to providing treatment they perceived as potentially inappropriate.
In a 1996 prospective cohort study including 353 children in an American PICU, 6.5% patients met the definition of futility (6): (1) Imminent demise futility (PRISM score with high risk of mortality); (2) lethal condition futility (long-term survival unlikely); or (3) qualitative futility (high morbidity). Using similar definitions, Goh and Mok reported a 5.1% futility rate in a UK PICU (11), while a cross-sectional point prevalence survey of UK PICU directors suggested 21% of all care was perceived as potentially inappropriate (13%) or futile (8%) (12). The definitions utilized in these studies differ from the current SCCM definitions; additionally, prior to 2015, the terms futility and potentially inappropriate treatment were often used interchangeably. In addition, the number of children with chronic complex conditions and chronic critical illness requiring PICU has increased substantially. Sachdeva et al. noted 89% of their children had no developmental delays; they did not specifically comment on how many of the remaining children had complex chronic conditions or were dependent on medical devices (6). In comparison, in 2010, Burns et al. reported 50% of children requiring PICU admission had a chronic complex condition (7). Variability in definitions, changes in patient demographics including the presence of chronic conditions, dependence on medical technology and differences in study methodology may explain the differing rates of perceived potentially inappropriate treatment observed. In addition, whether treatment is perceived as potentially inappropriate is a matter of opinion and thus subject to variability (4).
In cases of perceived potentially inappropriate treatment, conflict may arise due to communication issues and lack of understanding of patient/family's wishes. The importance of communication including multidisciplinary case conferences was evident based on provider responses utilizing the study questionnaire and the variable opinions regarding who was perceived as receiving potentially inappropriate treatment. Case conferences are an important means to develop rapport and trust, and establish goals of care through shared decision making (16). In a practice innovation, Wocial et al. (17) introduced weekly Pediatric Ethics and Communication Excellence (PEACE) rounds aimed at establishing realistic goals of care for PICU patients. In the pre-post intervention analysis, a statistically significant reduction in PRISM indexed length of stay, increase in a change in code status to do not resuscitate and increase in-hospital death while no change in patient 30- and 365-day mortality (17) was observed. While early and proactive communication is encouraged (1, 2) and effective (17) due to time constraints and competing demands, PICU providers may avoid case conferences thereby perpetuating the status quo and what may be perceived as potentially inappropriate treatment (18). Delays in initiating end-of-life discussions, indecision regarding perceived potentially inappropriate treatment and lack of nursing participation in case conferences (19) may contribute to distress and lead to conflict within the team. Many of our nurses did not have a good understanding of the patient's/family's wishes. Unfortunately, patient/family wishes are frequently not discussed (20), or may be poorly documented (21). Improving communication via regular multidisciplinary case discussions (17, 22), early consultation with experts in clinical ethics and palliative care (1, 2), clear documentation of patient/family wishes and goals of care, and team debriefing may reduce conflict (23), provider distress and the frequency of perceived potentially inappropriate treatment.
Half of our providers reported distress, which was primarily centered around 3 patients who required an extended PICU stay and had or developed a chronic critical illness or had an extremely poor prognosis. The PICU environment, staffing model and training programs were not developed with the needs of children with chronic critical illness in mind (3). Rapid staff turnover, gaps in continuity of care and provider discomfort in managing patients with chronic critical illness contribute to conflict (24), distress and perceived potentially inappropriate treatment. These children have a higher mortality rate (7), and use a disproportionate amount of healthcare resources compared to other PICU patients (25), leading providers to question the appropriateness of continued treatment. Providers noted their distress stemmed from observing ubiquitous suffering (patient, family, self and colleagues), conflict with family and each other, compromised quality of life, and uncertainty (e.g., direction of care). Miles et al. noted similar themes noting treatment perceived as “non-beneficial” was the most common source of provider distress (3). In a recent multicenter study, Dryden-Palmer et al. noted moral distress was common among pediatric and neonatal ICU providers (26). High scoring questions were linked to initiating and continuing life support the provider did not agree with, offers of “false hope”, and quality of care suffering due to non-continuity (26). Importantly, provider predictions regarding patient survival and functional outcome tend to pessimistic and in relation to children with medically complex conditions, inaccurate (27); providers frequently underestimate patients' quality of life (28). By proactively engaging families in regular discussions regarding the patient's condition, realistic and appropriate goals of care including resuscitation status, can be established (17). It has been postulated that witnessing prolonged potentially inappropriate treatment may lead to more intense distress or desensitization (29); interestingly, we observed the latter. Perceived potentially inappropriate treatment is independently associated with burnout, intention to quit (30, 31) and provider distress. In cases of perceived potentially inappropriate treatment, we suggest clinical staff be supported and empowered to find evidence-based solutions that consider individual and unit needs and local culture.
Strengths of the current study include its prospective and longitudinal design, and use of an interviewer-administered questionnaire with a (94%) response rate exceeding those seen in comparable adult studies (15). As a single center study, our results may reflect local unit issues rather than issues universal to PICU. However, similar themes have been identified by others lending merit to our findings. Other limitations include missing data, lack of daily surveys and not including the full multi-disciplinary team, which may have impacted study outcomes. To avoid introducing bias, follow up questions were not posed when providers differed in their opinion regarding the appropriateness of ongoing treatment; this may have resulted in the loss of potentially important data. As well, the families' voices were not included in the current study as, and as noted by Lo, families' may differ in regard to their definition of potentially inappropriate and/or non-beneficial treatment (4). Furthermore, providers may have opted to state treatment was appropriate to avoid completing the 21-item questionnaire thereby underestimating the true frequency of perceived potentially inappropriate treatment.
Conclusion
While perceived potentially inappropriate treatment may be infrequent, distress secondary to treatment perceived as potentially inappropriate is common. Interventions to address provider distress should be developed using established frameworks. Targeted interventions including: (1) strategies to improve communication with families and amongst providers, (2) clear and concise end-of-life treatment recommendations, and (3) advocacy for a congruent care plan that could alleviate conflict and uncertainty, may decrease instances of perceived potentially inappropriate treatment, and may decrease distress associated with providing perceived potentially inappropriate treatment. Future areas for research include: (1) quantification of perceived potentially inappropriate treatment and moral distress in other contexts and perhaps on a national or international scale (including the full multidisciplinary team and learners), (2) Exploring patient and families' perspectives with regards to perceived potentially inappropriate treatment, and (3) implementing strategies to reduce provider distress and perceived potentially inappropriate treatment.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Western University Health Sciences Research Ethics Board. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
AS: Conceptualization, Formal Analysis, Funding acquisition, Methodology, Resources, Supervision, Writing – original draft, Writing – review & editing. MM: Conceptualization, Formal Analysis, Methodology, Validation, Writing – review & editing, Data curation. CM: Conceptualization, Methodology, Writing – review & editing. RS: Conceptualization, Writing – review & editing. KS: Conceptualization, Methodology, Supervision, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article.
This project was supported by (IRF-49-14) Internal Research Fund grant from Lawson Health Research Institute.
Acknowledgments
Saoirse Cameron (SC), as a research coordinator, was responsible for participant enrollment, and survey administration. She assisted with thematic analysis and played a key role in this project.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fped.2024.1272648/full#supplementary-material
References
1. Bosslet GT, Pope TM, Rubenfeld GD, Lo B, Truog RD, Rushton CH, et al. An official ATS/AACN/ACCP/ESICM/SCCM policy statement: responding to requests for potentially inappropriate treatments in intensive care units. Am J Respir Crit Care Med. (2015) 191(11):1318–30. doi: 10.1164/rccm.201505-0924ST
2. Kon AA, Shepard EK, Sederstrom NO, Swoboda SM, Marshall MF, Birriel B, et al. Defining futile and potentially inappropriate interventions: a policy statement from the society of critical care medicine ethics committee. Crit Care Med. (2016) 44(9):1769–74. doi: 10.1097/CCM.0000000000001965
3. Miles AH, Rushton CH, Wise BM, Moore A, Boss RD. Pediatric chronic critical illness, prolonged ICU admissions, and clinician distress. J Pediatr Intensive Care. (2021) 11(4):275–81. doi: 10.1055/s-0041-1724098
4. Lo JJ, Graves N, Chee JH, Hildon ZJ. A systematic review defining non-beneficial and inappropriate end-of-life treatment in patients with non-cancer diagnoses: theoretical development for multi-stakeholder intervention design in acute care settings. BMC Palliat Care. (2022) 21(1):195. doi: 10.1186/s12904-022-01071-7
5. Miller-Smith L. The true abuse of futility. Perspect Biol Med. (2018) 60(3):403–7. doi: 10.1353/pbm.2018.0015
6. Sachdeva RC, Jefferson LS, Coss-Bu J, Brody BA. Resource consumption and the extent of futile care among patients in a pediatric intensive care unit setting. J Pediatr. (1996) 128(6):742–7. doi: 10.1016/s0022-3476(96)70323-2
7. Burns KH, Casey PH, Lyle RE, Bird TM, Fussell JJ, Robbins JM. Increasing prevalence of medically complex children in US hospitals. Pediatrics. (2010) 126:638–46. doi: 10.1542/peds.2009-1658
8. Hamric AB, Blackhall LJ. Nurse-physician perspectives on the care of dying patients in intensive care units: collaboration, moral distress, and ethical climate. Crit Care Med. (2007) 35(2):422–9. doi: 10.1097/01.CCM.0000254722.50608.2D
9. Boss RD, Falck A, Goloff N, Hutton N, Miles A, Shapiro M, et al. Low prevalence of palliative care and ethics consultations for children with chronic critical illness. Acta Paediatr. (2018) 107(10):1832–3. doi: 10.1111/apa.14394
10. Nathaniel AK. Moral reckoning in nursing. West J Nurs Res. (2006) 28(04):419–38, discussion 439–448. doi: 10.1177/0193945905284727
11. Goh AY, Mok Q. Identifying futility in a paediatric critical care setting: a prospective observational study. Arch Dis Child. (2001) 84(3):265–8. doi: 10.1136/adc.84.3.265
12. Vemuri G, Playfor SD. Futility and inappropriate care in pediatric intensive care: a cross-sectional survey. Pediatr Anesth. (2006) 16(3):309–13. doi: 10.1111/j.1460-9592.2005.01761.x
13. Fiser DH. Assessing the outcome of pediatric intensive care. J Pediatr. (1992) 121:68–74. doi: 10.1016/S0022-3476(05)82544-2
14. Palisano R, Rosenbaum P, Walter S, Russell D, Wood E, Galuppi B. Development and reliability of a system to classify gross motor function in children with cerebral palsy. Dev Med Child Neurol. (1997) 39(4):214–23. doi: 10.1111/j.1469-8749.1997.tb07414.x
15. Singal RK, Sibbald R, Morgan B, Quinlan M, Parry N, Radford M, et al. A prospective determination of the incidence of perceived inappropriate care in critically ill patients. Can Respir J. (2014) 21(3):165–70. doi: 10.1155/2014/429789
16. Richards CA, Starks H, O'Connor MR, Bourget E, Lindhorst T, Hays R, et al. When and why do neonatal and pediatric critical care physicians consult palliative care? Am J Hosp Palliat Care. (2018) 35(6):840–6. doi: 10.1177/1049909117739853
17. Wocial L, Ackerman V, Leland B, Benneyworth B, Patel V, Tong Y, et al. Pediatric ethics and communication excellence (PEACE) rounds: decreasing moral distress and patient length of stay in the PICU. Hec Forum. (2017) 29:75–91. doi: 10.1007/s10730-016-9313-0
18. Nelson JE, Hope AA. Integration of palliative care in chronic critical illness management. Respir Care. (2012) 57(6):1004–12. doi: 10.4187/respcare.01624
19. Flannery L, Ramjan LM, Peters K. End-of-life decisions in the intensive care unit (ICU)—exploring the experiences of ICU nurses and doctors—a critical literature review. Aust Crit Care. (2016) 29(2):97–103. doi: 10.1016/j.aucc.2015.07.004
20. Heyland DK, Barwich D, Pichora D, Dodek P, Lamontagne F, You JJ, et al. Failure to engage hospitalized elderly patients and their families in advance care planning. JAMA Intern Med. (2013) 173:778–87. doi: 10.1001/jamainternmed.2013.180
21. Ratnapalan M, Cooper AB, Scales DC, Pinto R. Documentation of best interest by intensivists: a retrospective study in an Ontario critical care unit. BMC Med Ethics. (2010) 11:1. doi: 10.1186/1472-6939-11-1
22. Curtis JR, Patrick DL, Shannon SE, Treece P, Engelberg RA, Rubenfeld GD. The family conference as a focus to improve communication about end-of-life care in the intensive care unit: opportunities for improvement. Crit Care Med. (2001) 29(2 Suppl):N26–33. doi: 10.1097/00003246-200102001-00006
23. Studdert DM, Burns JP, Mello MM, Puopolo AL, Truog RD, Brennan TA. Nature of conflict in the care of pediatric intensive care patients with prolonged stay. Pediatrics. (2003) 112(3 Pt 1):553–8. doi: 10.1542/peds.112.3.553
24. Henderson CM, Williams EP, Shapiro MC, Hahn E, Wright-Sexton L, Hutton N, et al. “Stuck in the ICU”: caring for children with chronic critical illness. Pediatr Crit Care Med. (2017) 18(11):e561–8. doi: 10.1097/PCC.0000000000001332
25. Chan T, Rodean J, Richardson T, Farris RWD, Bratton SL, Di Gennaro JL, et al. Pediatric critical care resource use by children with medical complexity. J Pediatr. (2016) 177:197–203.e1. doi: 10.1016/j.jpeds.2016.06.035
26. Dryden-Palmer K, Moore G, McNeil C, Larson CP, Tomlinson G, Roumeliotis N, et al. Moral distress of clinicians in Canadian pediatric and neonatal ICUs. Pediatr Crit Care Med. (2020 Apr) 21(4):314–23. doi: 10.1097/PCC.0000000000002189
27. Murphy SS, Graham RJ. Chronic illness in pediatric critical care. Front Pediatr. (2021) 14:9. doi: 10.3389/fped.2021.686206
28. Crocker TF, Smith JK, Skevington SM. Family and professionals underestimate quality of life across diverse cultures and health conditions: systematic review. J Clin Epidemiol. (2015) 68(5):584–95. doi: 10.1016/j.jclinepi.2014.12.007
29. Prentice T, Janvier A, Gillam L, Davis PG. Moral distress within neonatal and paediatric intensive care units: a systematic review. Arch Dis Child. (2016) 101(8):701–8. doi: 10.1136/archdischild-2015-309410
30. Piers RD, Azoulay E, Ricou B, DeKeyser Ganz F, Decruyenaere J, Max A, et al. Perceptions of appropriateness of care among European and Isaraeli intensive care unit nurses and physicians. JAMA. (2011) 306(24):2694–703. doi: 10.1001/jama.2011.1888
Keywords: death & dying, potentially inappropriate treatment, ethical conflict, medical futility, end-of-life (EOL), distress
Citation: Sarpal A, Miller MR, Martin CM, Sibbald RW and Speechley KN (2024) Perceived potentially inappropriate treatment in the PICU: frequency, contributing factors and the distress it triggers. Front. Pediatr. 12:1272648. doi: 10.3389/fped.2024.1272648
Received: 4 August 2023; Accepted: 3 January 2024;
Published: 18 January 2024.
Edited by:
Suyun Qian, Capital Medical University, ChinaReviewed by:
Gabriel Bosslet, Indiana University, United StatesSabrina Derrington, Children's Hospital of Los Angeles, United States
© 2024 Sarpal, Miller, Martin, Sibbald and Speechley. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Amrita Sarpal ZHIuYW1yaXRhLnNhcnBhbEBnbWFpbC5jb20=
†Present addresses: Amrita Sarpal, Department of Pediatrics, Sidra Medicine, Doha, Qatar; Associate Professor of Clinical Pediatrics, Weill Cornell Medicine-Qatar, Ar-Rayyan, Qatar
 Amrita Sarpal
Amrita Sarpal Michael R. Miller
Michael R. Miller Claudio M. Martin3,4
Claudio M. Martin3,4 Kathy N. Speechley
Kathy N. Speechley