
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
BRIEF RESEARCH REPORT article
Front. Pediatr., 01 March 2024
Sec. Children and Health
Volume 12 - 2024 | https://doi.org/10.3389/fped.2024.1100828
This article is part of the Research TopicGlobal Excellence in Children and Health.View all 9 articles
Background: Fever is a typical symptom of many sicknesses, but for children under the age of five, fever can have devastating consequences and represents a source of worry for parents. To the best of our knowledge, no research on home management of fever in children has been conducted in Ethiopia. We aimed to assess knowledge, practices, and associated factors towards home management of childhood fever among parents visiting Gondar Town health facilities in 2022.
Method: This multicenter institutional-based cross-sectional study was conducted in Gondar public health facilities from June 1st—June 30th, 2022. Participants were fathers and mothers of children aged 0–5 years. A stratified random sampling technique was used. Data were collected through face–to–face interviews using a pretested structured questionnaire.
Results: Approximately, 40.2% (95% CI: 35.5%, 45.2%) of parents had good knowledge and only 12.8% (95% CI: 9.7–15.8) of parents practiced home fever management. Being married [Adjusted odds ratio [(AOR) = 2.1 (1.2, 3.2)], having a primary or higher level of education [AOR = 2.4 (1.17, 4.9)] [AOR = 2.0 (1.02–4.6)], respectively, and number of children [AOR = 1.8 (1.63, 2.03)] were factors associated with parental knowledge. Likewise, being married [AOR = 3.05 (2.27.50–3.83)], receiving counseling from health care providers [AOR = 2.12 (1.53–3.32)], and being male [AOR = 2.03 (1.50–3.00)] were significant predictors of practice.
Conclusion: Inadequate levels of knowledge and numerous irrational practices related to home fever management were predominant among parents, which needs to be addressed. Evidence-based health education is essential for parents to enhance their level of knowledge and practice to effectively treat fever at home.
Fever is a common symptom seen in children with various illnesses (1–5). Fevers lasting more than three days warrant visits to the emergency room, which can lead to overcrowding and higher healthcare costs (6), and about 70% of children under the age of 18 consult a doctor for fever-related illnesses (7). Fever is not a disease itself, but rather a symptom or sign of an underlying condition (8). It can be considered a threat-adaptive physiological response (9–13).
There is no doubt that parents may experience anxiety when it comes to the potential side effects of fever. Although fevers are generally regarded as a healthy response, there can be concerns about complications such as convulsions, dehydration, brain injury, and even death in rare cases (14, 15). In addition, most parents are unaware of the definition of fever, its symptoms, or how to treat it (16, 17).
It is possible to define fever or pyrexia based on its pathophysiology and clinical purpose. Pathophysiologically, exogenous pyrogens cause fever by causing host cells (mainly macrophages) to produce and release endogenous pyrogens, which are involved in some immune system functions. Endogenous pyrogens, which are substances produced by the body in response to infection or inflammation, can reach the hypothalamic thermoregulatory center. Specifically, they can target the Organum Vasculosum of the Lamina Terminalis (OVLT) in the hypothalamus. This triggers the production of prostaglandins, with prostaglandin E2 (PGE2) being the most important one. PGE2 acts on the hypothalamus to raise the body's temperature set point (10, 18–20). To start the febrile response, these raise the thermostatic set point (21). According to the World Health Organization (WHO), the Society of Critical Care Medicine, and the Infectious Disease Society of America (IDSA), among others, equivalent rectal temperatures of 38°C (100.4°F) or axillary temperatures of 37.5°C (99.5°F) in both adults and children indicate fever (22–25). Hence, a 10%–12.5% increase in metabolic rate is required for a 1°C increase in body temperature (26).
Treatment for febrile seizures (FS) is generally not advised because most occurrences are benign and self-limiting (27);that is, 80% are mild febrile convulsions with no lasting effects (28). However, parents believe that FS can cause brain damage and death, and this belief has been identified as the primary driver of parental dread of fever (15, 29, 30). In addition, numerous studies reported that 14.4%–21% of parents in Western nations such as the USA and Australia believe that fever damages the brain, and fever phobia is still common in Asian nations like Taiwan and Singapore, where 68.8%–77.7% of parents hold this belief (31–34).
In certain Sub-Saharan African nations, fever constituted more than 50% of visits to pediatric outpatient clinics (35).
According to Rajan Arora and Prashant Mahajan, fever in children is most commonly caused by infections, although it can also be caused by immune-mediated, inflammatory, or neoplastic disorders. “Fever without a source” occurs when the reason for the fever cannot be determined through history and physical examination (36).
Different cultures have different levels of knowledge regarding fever (37), appropriate antipyretic use (38, 39), level of fever phobia (40), and, in general, parental fever care (34, 37, 41). However, fever anxiety can still be found in people from all cultures, including those from Europe. In European cultures, where access to healthcare is generally widespread, individuals may still experience anxiety related to fever (40). Moreover, approximately half of all parents use antipyretics when the temperature is below 38 degrees Celsius, or use inappropriate antipyretic doses or supra-therapeutic amounts of paracetamol and ibuprofen. Four decades ago, Barton Schmitt coined the term “fever phobia” in his classic study to characterize parents' irrational anxieties about fever (29). The 2021 version of the NICE (National Institute for Health and Care Excellence) guideline regarding fever in children does not recommend tepid sponging, which involves using water to reduce body temperature. It is recommended not to over-wrap children with fever, and paracetamol or ibuprofen should be considered if the child seems distressed. Furthermore, if one medication fails to alleviate the child's distress, a switch to another agent may be considered (for example, from paracetamol to ibuprofen or vice versa), and paracetamol and ibuprofen should not be administered simultaneously (42).
Certain studies have highlighted that educational level, financial class, and cultural background were the most important factors in childhood fever knowledge and management (43–45).
In 2019, M. Kelly and his colleagues ran a randomized control trial (RCT) to determine the effectiveness of information leaflets in raising parental awareness on childhood fever. According to the findings, enhancing parental knowledge of fever and suitable management options (46). There is no recent evidence on parents' knowledge and practice of home management of fever and its contributing factors in Ethiopia. Therefore, this study aimed to assess the knowledge, practices, and associated factors toward home management of childhood fever among parents visiting Gondar town health facilities, in Amhara regional state, northwest Ethiopia, in 2022. Thus, this study can be used as a baseline by health policymakers to help design strategies.
An institutional-based cross-sectional quantitative study was conducted from June 1st, 2022—June 30th, 2022.
The research was conducted in Gondar's public health facilities. According to the Federal Democratic Republic of Ethiopia's Central Statistical Agency's (CSA) official population projection of Ethiopian cities and towns in 2015, the town has an estimated population of 323,900 people (47). Currently, one comprehensive specialty hospital and eight health centers provide health care services to the community in the municipality, totaling nine public health facilities. According to the Gondar municipal health office, 652,940 patients visit all nine governmental health institutions in the town each year, with 21,527 of them being children under the age of five (48).
All parents of children who visited the governmental health facilities in Gondar town were a population source.
Parents of children and those available during data collection at governmental health facilities in Gondar town were the study population.
All parents who have children and visit the governmental health facilities in Gondar town were considered for inclusion.
Parents of children found in Gondar metropolitan city's health institutions with serious illness conditions or with hearing loss problems (with no interpreter of sign language) were excluded from the study.
The sample size was calculated using a single population proportion formula based on the following statistical assumptions:
Because there is no previous research conducted on this topic in Ethiopia, we considered P = 50%, 95% confidence level, and a 5% margin of error.
Where:
n = the desirable sample size
Z (α/2) = the critical value at the 95% level of significance (1.96)
P = proportion of knowledge or practice.
d = margin of error
After adding a 10% non-response rate, the total sample size was 423.
To obtain a representative sample from the town's eight public health institutions and one comprehensive specialized hospital, a stratified random sampling technique was used. The study covered all healthcare facilities, and the total sample size was proportional. During the study period (one month), a 3,800 customer flow rate was predicted. To estimate the sampling interval (k), the determined sample size (n) of respondents (i.e., 3,800/423 = 8.9) was divided by the anticipated number of parents visiting the public health facilities during the study period (N). As a result, one in every nine parents was chosen using a systematic random sampling procedure until the required sample was reached (Figure 1).
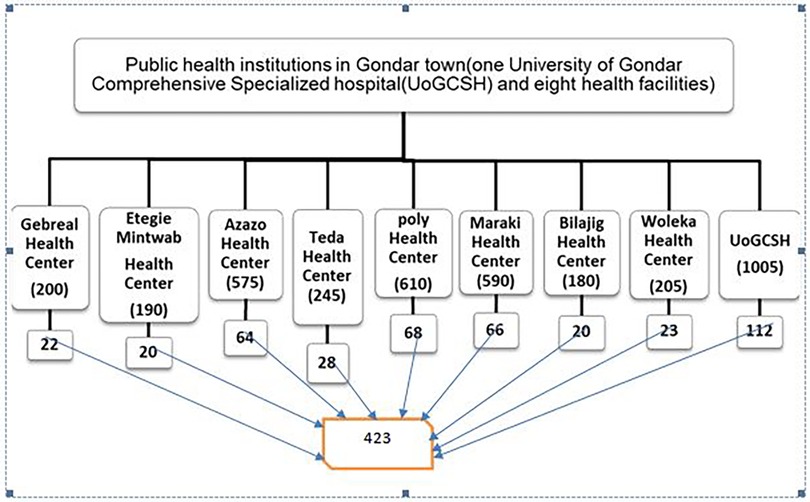
Figure 1. Schematic diagram of the sampling procedure for the study population in Gondar town governmental health facilities, Amhara regional state, Ethiopia 2022.
The data were collected using structured, pretested, and interpreted face-to-face interviewer-administered questionnaires. All questions were derived from various sources (15, 49, 50). This questionnaire broadly encompassed three sections. Section 1 comprised the characteristics of the study participants (age of the child in months, sex of the child, age of parents/guardians in years, sex of the parent, marital status, ethnicity, level of education, occupation, religion, monthly income status, relationship to the child, and number of children). Section two included 16 questions to evaluate the knowledge of parents regarding the home management of fever. Section three consisted of nine questions for an assessment of the practice of parents in the home management of childhood fever.
• Knowledge of home management of fever (good/poor)
• Practices on home management of fever (good/poor)
Sociodemographic-related factors: age of the child in months, sex of the child, age of parents/guardians in years, sex of the parent, marital status, ethnicity, level of education, occupation, religion, monthly income status, relationship to the child, and number of children.
The term “fever” is defined as “an elevation of body temperature above the normal daily variation” (51). Fever among children under 5 years of age is often defined as a temperature of 100.4°F (38°C or higher) (52). When the body's temperature exceeds 40°C, it is referred to as a high fever (53), and high fever is best treated by giving antipyretics like paracetamol or ibuprofen (54, 55).A documented oral, ear, and forehead temperature of 37.8°C or higher (also known as the “rectal equivalent”) was considered to be fever. By adding 0.2°C to the oral temperature and deducting 0.6°C from the axillary temperature, a rectal equivalent temperature was determined (56).
Parents were classified as having good knowledge if their responses to knowledge-related questions were greater than or equal to the mean, whereas parents with answers that fell below the mean were classified as having poor knowledge.
Parents who scored above or equal to the mean value on practice-related questions were considered to have good practices, whereas those who scored below the mean value on knowledge-related questions were considered to have poor practices.
The instrument was translated into the Amharic language (local language), and to check the tool's consistency, it was translated back to English to ensure data quality. For consistency of comprehension of the survey tool and modification, the structured questionnaire was pre-tested on 5% of the total sample outside the chosen health facility. Before beginning data collection, the recruited data collectors received one-day training on the purpose, confidentiality of information, relevance of the study, respondent's rights, pretest, informed consent, and interviewing techniques.
Data were coded, cleaned, and entered into Epi-Info version 7, and then exported to SPSS version 20 for statistical analysis. Sociodemographic and other study participant variables were summarized using descriptive statistics (frequencies and percentages). To show the degree of connections between the explanatory and outcome variables, binary logistic regression analysis was used. In the multivariate analysis, only factors with P < 0.25 in the bivariate analysis were considered. With a 95% confidence interval, P < 0.05 on the multivariate analysis was considered statistically significant.
Ethical clearance was issued from the school of nursing research ethical review committee on behalf of the University of Gondar. Each health facility's head or coordinator received a formal letter outlining ethics and collaboration, and the head of the health facility approved and forwarded a permission letter to the unit team leader/coordinator. The unit team leader was permitted to collect data. Participants in the study provided their informed consent after being informed of their opportunity to opt out of the study. Data were coded to maintain the confidentiality of the information for each study participant.
There were 423 participants, of which 95% (402) were female and gave a 100% response rate. The study participants' ages ranged from 26 to 35 years old, with a mean (SD) age of 30.28 ± 6.534 years. Of the children, 42.6% (180) were under the age of six months, which is the age group where the majority of them fell. More than half of the children, or 239 of them, were female, making up 56.5% of the total. Less than one-third, 33.5% (106), of the study participants had diplomas or a formal education, and the maximum percentage, 75.5% (319), of the study participants were Amharan in ethnicity. Approximately 85.8% (363) of the study participants were married.
Regarding occupational status, about 41.4% of the study participants were housewives, and 86.1% (364) were orthodox religious followers. Most study participants, 79.4% (336), earned a monthly income of 500–2,500 Ethiopian Birr. In addition, 95.7% (405) of children had a relationship with their biological father /mother and more than one-third, 32.9% (139), of the study participants had ≥3 children (Table 1).
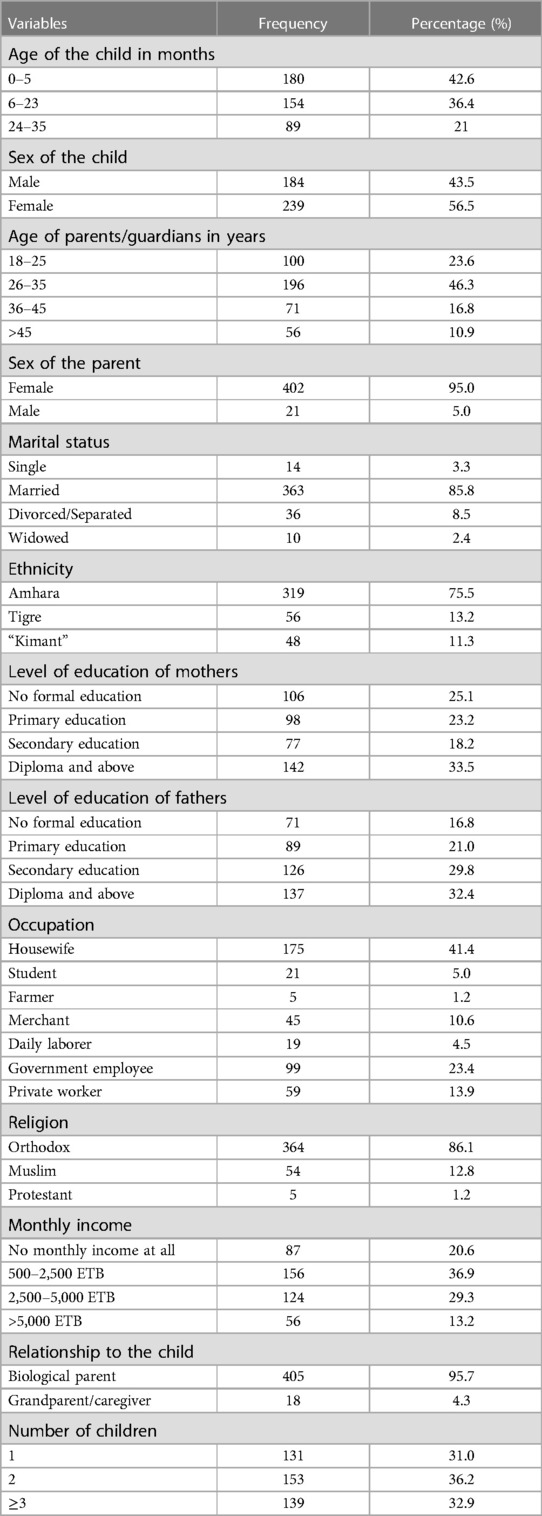
Table 1. Sociodemographic characteristics of the participants in Gondar town health facilities, 2022 (n = 423).
Parents as a whole had a knowledge level of 40.20% (95 percent confidence interval) (35.5–45.2). In a similar vein, 33.8% (143) of survey participants recognized what fever was. 18.4% (78) of the total responders who were aware of the definition of fever could recognize it. Knowledge of the appropriate temperature measurement: Of the study's participants, 27% (114) were aware of the proper normal temperature readings, while 22.7% (96) were aware of the typical range of body temperature measurements. 71.4% (302) of the study's total participants expressed concern when their child's body temperature increased.
Similarly, of the total surveyed participants, 238 (56.3%) were aware of the causes of fever, including infection (31.7%), stress (22.0%), immunization (30.5%), and seasonal allergies (13.5 percent). A total of 236 study participants—or 55.8%—knew how to measure their body temperatures. 55.1 percent of study participants were familiar with measuring their body temperatures under their arms or in their axillae at home (236).
Regarding the technique for taking temperature readings and how frequently they were taken, 64.1% (271) and 25.1% (106) of the study's participants used their hands and the intervals of 15–30 min for temperature readings and body temperatures, respectively. However, only 26.2% of the survey participants reported managing their fever at home (111). Nevertheless, most of the research participants—12.5% (53)—provided antibiotics to treat fevers, whereas 6.4% (27) gave acetaminophen. In addition, treatments include cold sponging (64.5%), using an ice pack (15.4%), and just using medications (12.3 percent). Most study participants, 72.8% (308) and 12.3% (52), utilized the precise measurement spoon or syringe that comes with the medication to administer drugs, respectively (Table 2).
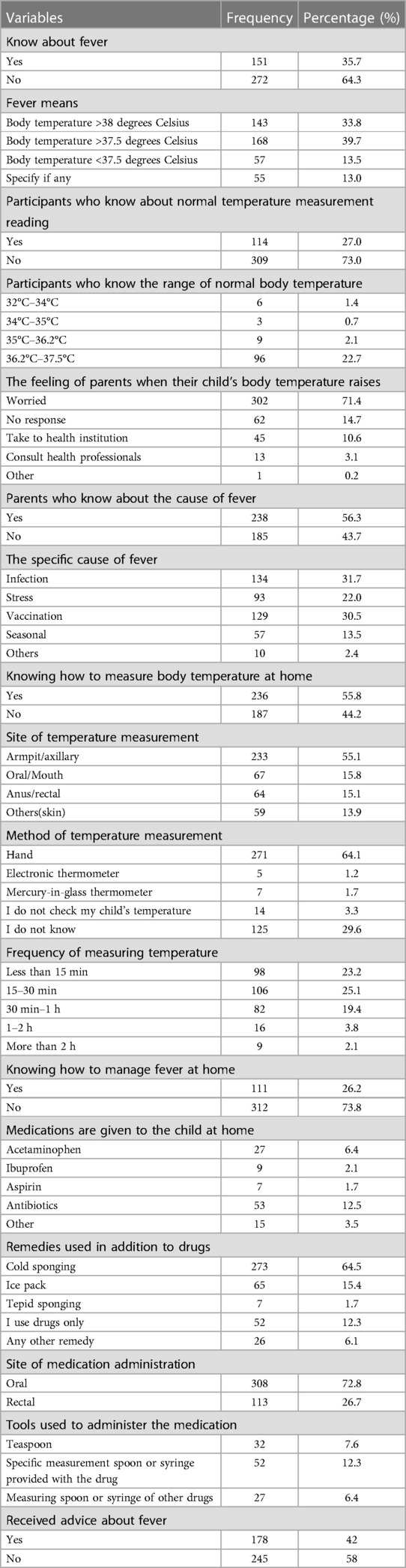
Table 2. Knowledge of parents on home-based managements of fever in Gondar town health facilities, 2022 (n = 423).
Knowledge of parents on home management of fever in Gondar City Health Institutions, Ethiopia (Figure 2).
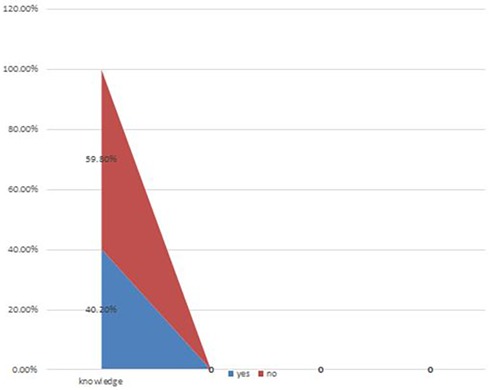
Figure 2. Knowledge of parents on home management of fever in Gondar city health institutions, Ethiopia (n = 423).
Overall, 12.8% of parents practiced managing fevers at home (95 percent confidence interval (9.7–15.8). Only 2.6% (11) of the survey participants said that they regularly measured their body temperatures at home, and 2.8% (12) reported having thermometers, both glass (1.7%) and electronic (batter, thermometer) ones (1.2 percent). Only 23.2% (98) of the participants used a proper temperature measurement technique other than a thermometer, such as using the dorsum of the hands (23.2 percent).
When a child has a fever, parents treat them immediately with wet sponging (22.5%), cold water baths (58.2%), analgesics (9.2%), antipyretic medications (3.8%), homeopathic remedies (59%), and doctor consultations (0.2 percent). More than one third, 34.3% (145), of the survey participants also phoned doctors when their body temperatures climbed to 43°C. The majority of participants, 63.6% (269), did not know when therapy should be delivered or the range of body temperatures.
Appropriate antipyretic medication was administered based on prior pediatrician advice (42.1%) and pharmacist consultation (31.4%). Additionally, 43% (182) of the trial participants calculated fever-lowering medicines based on prior pediatrician advice (Table 3).
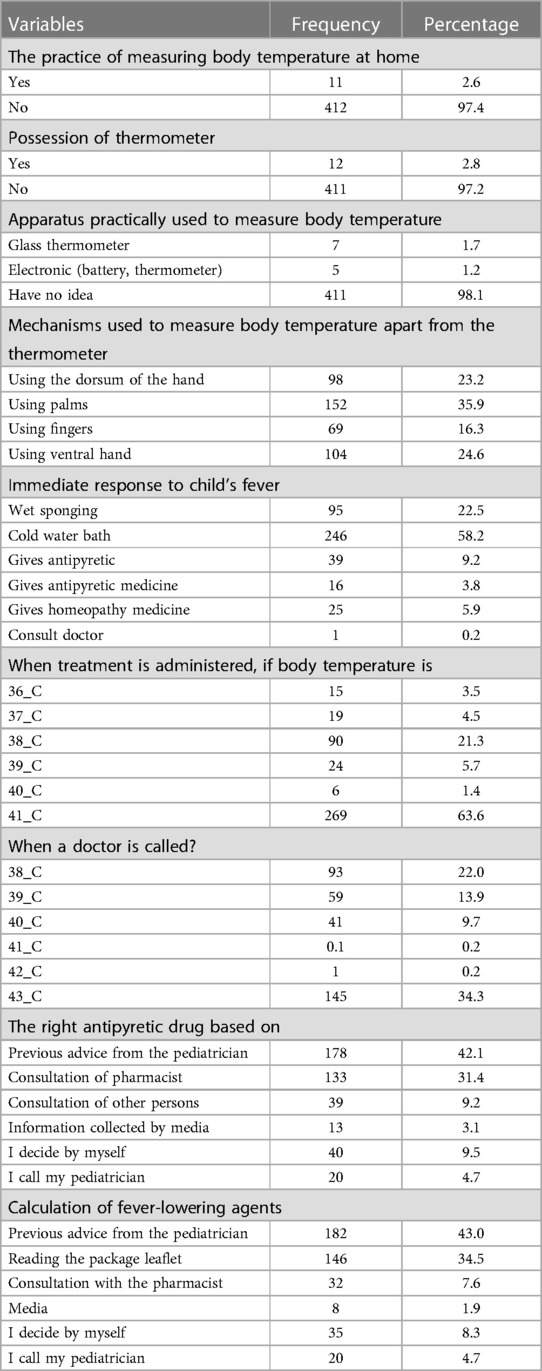
Table 3. Practice of parents on home management of fever in Gondar town health facilities, 2022 (n = 423).
Factors associated with parents' knowledge of home management of fever (Table 4).
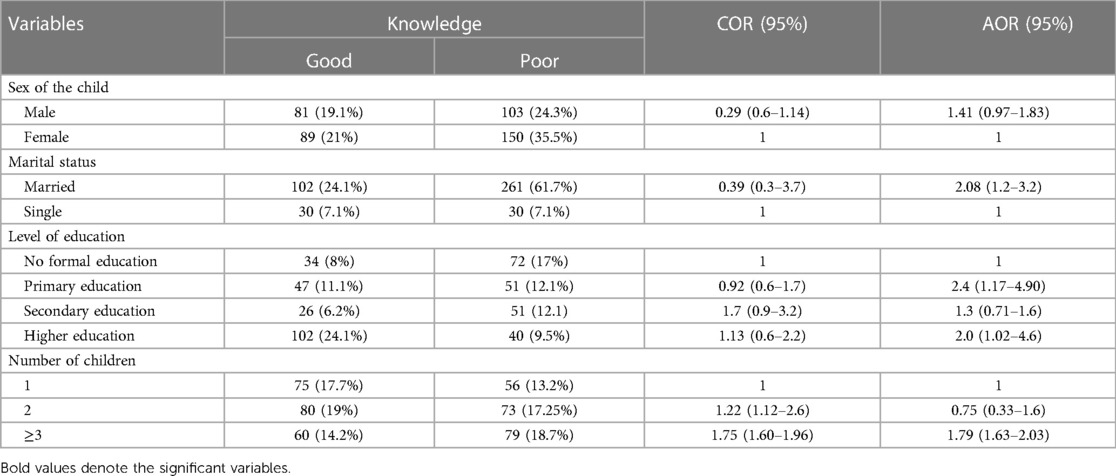
Table 4. Bivariable and multivariable analyses of factors associated with parents' knowledge on home management of child hood fever in Gondar town health facilities, 2022 (n = 423).
Factors associated with the practice of parents in the home management of fever (Table 5).
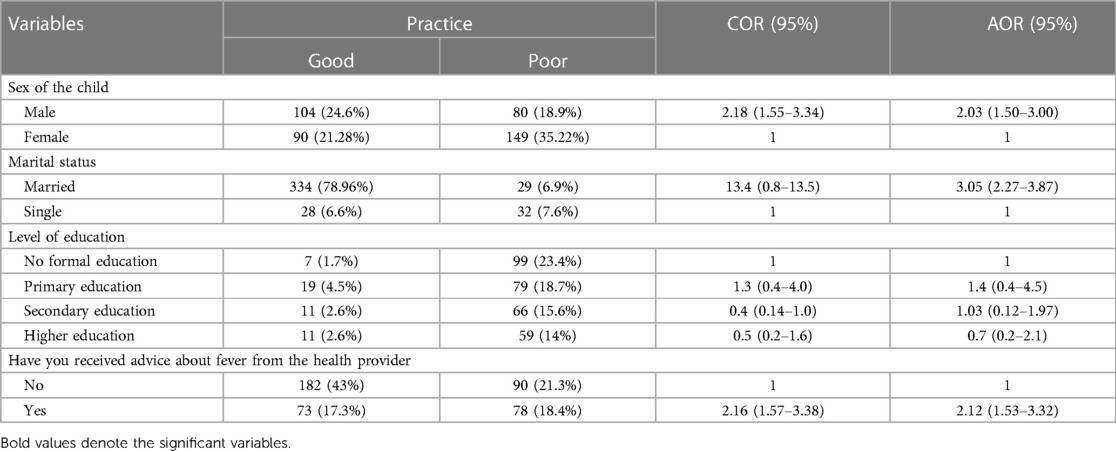
Table 5. Bivariable and multivariable analyses of factors associated with parents' practice on home management of child hood fever in Gondar town health facilities, 2022 (n = 423).
This study examined knowledge, practices, and associated factors of fever home management among parents of children under five years of age. A pervasive range of childhood diseases are accompanied by fever; most of them are managed at home before visiting a nearby health care facility. If the fever is left untreated, it can result in numerous complications such as brain damage, dehydration, seizure, and organ damage (liver and kidney), which both the life of the child and the family and community at large.
Our findings regarding the knowledge of parents about childhood fever home management revealed that less than half of the participants had good knowledge (40.20%; 95% CI, 35.5%–45.2%). This insufficient level of knowledge depicts a very high public issue that demands the stakeholders' due attention. Our finding is consistent with different studies conducted in Germany (30.6%), Saudi Arabia (38.4%), and Ghana (43%) (57–59). However, our findings show a lower level of parents' knowledge than studies conducted in different countries in India (95%), the Netherlands (88%), Korea (70.64%), Ireland (63%), and France (61%) (2, 52, 60–62). The difference in developed countries is that two thirds of the participants had higher educational levels (58, 60), but in this study, only one-third of participants had higher educational status (see Table 1), and highly educated participants are expected to have the ability to choose quality health services and seek healthcare service early for their febrile children (46). In addition, highly educated participants are expected to have enough income to afford healthcare services and different basic goods, which are needed for best survival (63). Our findings showed that parents' level of knowledge is relatively higher than studies conducted in Taiwan and Turkey, which were 19% and 18% (34, 64), respectively., The difference could be the small sample size in Turkey and the higher level of anxiety and dissatisfaction about the information given by health care providers in Taiwan.
Our results showed that only 12.8% (95% CI: 9.7%–15.8%) of parents practiced managing fevers at home, which was lower than studies conducted in different countries (Palestine 78%, Korea 75.93%, and India at 27%) (3, 60, 61). A possible reason could be the low level of socioeconomical status of our study participants compared with those countries. A low level of socioeconomical status hinders the parents from accessing quality health care services and even from homemade fever managements because they cannot afford to buy a thermometer and might not have knowledge on some home remedies such as calf wrap. This involves applying cool or cold compresses to the calf muscles. The cool or cold temperature of the compresses can cause vasoconstriction (narrowing of blood vessels) in the peripheral areas, such as the calves. This vasoconstriction can help to divert blood away from the skin's surface and reduce body heat, thus it can prevent side effects including shivering, crying, agitation, and discomfort (65) In addition, the total domestic growth per capita is much greater in India (3,173,397.59 million US$ GDP of India and 1,798,583.92 million US$ GDP of Korea) compared to Ethiopia's GDP of 111,271.11 million US$ (66). Furthermore, the survival of children in underdeveloped countries depends on the family's and community's ability to access the basic needs of life (67).
In the current study, marital status, level of education, and number of children were associated with parents' knowledge. Parents' levels of knowledge regarding fever home management was 2.1 times higher among married parents than their unmarried counterparts. Married parents are estimated to have possible support from spouses both in terms of income generation and physical support for their febrile child (68). Married parents are also more responsive to caring for their children because they are mature enough in decision-making and resources. This is not consistent with other previous studies conducted in different countries that reported that none of the parent or child variables were found to predict accurate antipyretic usage or parental antipyretic knowledge (52, 62, 69, 70).
Parents who have more than or equal to three children increase the likelihood of fever home management knowledge 1.8 times higher than parents whose number of children is less than three. This study has similar finding to a study conducted in Jordan (71, 72). A possible reason for increased knowledge in parents with more children may be their previous knowledge and experience of effective fever management. For children with older siblings, it is likely that parents use their earlier experiences with the elder child for effective management of the present child and make better-informed decisions (61, 73); these scenarios indicated a situation where the parents would be expected to have more life experience.
Moreover, the level of knowledge doubled among parents who were more educated than their counterparts. This result corresponds with studies conducted in Canada (2, 73). Enarsonet al. illustrated that parents with a high level of educational status had a lower level of apprehension and revealed less fever phobia (73) because parents who were more worried about their fever were not able to effectively treat their febrile child (34). A higher level of education plays a significant role in elucidating child health outcomes; educated personnel are estimated to have positive health-seeking behavior, acquire crucial health-related information, and enact home-based and different management modalities provided by health care providers correctly. Likewise, education is a source of income/wage that is crucial to leading a healthy life (74, 75).
Received counseling from health care provider, sex of child, and marital status were determinants of parental fever home management practice. Parents who received counseling from health care providers had better practice skills in fever home management than parents who did not receive medical advice. This agrees with a study conducted in Morocco (75), where parents who had received advice from health care professionals were more knowledgeable on how to manage their febrile children (2), how to prevent further complications, and how to seek healthcare services early when the child did not respond to home-based treatments in addition to knowing adverse medication effects (60).
The likelihood of good practice among parents whose children were male was 2,03 times more than their counterparts, which is supported by the result reported in Malaysia (76). Moreover, in our report, married parents were more knowledgeable, which is an essential predictor of successful fever home management (61). Even though married parents are expected to share their responsibility for each other, which is crucial to lead a healthy life, there are no reports supporting this suggestion (59, 62, 71).
The study was conducted in one city in the country, which limits the generalizability of the outcomes to all parents in the country. Future research on the topic must include a representative sample of parents from the whole country to overcome this limitation, which is similar to the limitation of a cross-sectional study. Despite these limitations, the study can be used with caution as a baseline for the development of interventions to raise the awareness of parents on the identification and management of childhood fever.
Marital status, number of children, and a higher level of parental education were significantly associated with parental knowledge. Likewise, receiving counseling from a health care provider and the sex of the child was a substantial predictor of good fever home management practice. Inadequate levels of knowledge and numerous irrational practices related to fever home management were predominant among parents, which needs due attention. Evidence-based health education is essential for parents to enhance their level of knowledge and practice to effectively treat fever at home.
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
On behalf of the University of Gondar, ethical approval was issued by the school of nursing research ethical review committee. Each health facility's head or coordinator received a formal letter outlining ethics and collaboration, and after that, the head of the health facility approved and forwarded a permission letter to the unit team leader/coordinator. The unit team leader was permitted to gather data. Participants in the study gave their informed permission after being informed of their opportunity to opt-out of the study. Data were coded to maintain the confidentiality of the information for each study participant.
Conceptualization: NTA, ATG, BT. Data curation: ATG, NTA. Formal analysis: NTA, AG, BT. Funding acquisition: BT. Investigation: ATG. Methodology: NTA, ATG, BT. Project administration: BT. Resources: NTA, ATG, BT. Supervision: ATG, NTA. Validation: BT. Visualization: NTA. Writing – original draft: NTA, ATG, BT. Writing – review & editing: NTA, ATG. All authors contributed to the article and approved the submitted version.
We would like to thank the data collectors.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. NICE. Feverish Illness in Children—Assessment and Initial Management in Children Younger than 5 Years. London: PLOS ONE (2007). Available online at: http://www.nice.org.uk/nicemedia/live/11010/30523/30523.pdf (accessed April 5, 2013).
2. Bertille N, Fournier-Charrière E, Pons G, Chalumeau M. Managing fever in children: a national survey of parents’ knowledge and practices in France. PLoS One. (2013) 8(12):e83469. doi: 10.1371/journal.pone.0083469
3. SeH Z, Al-Jabi SW, Sweileh WM, Nabulsi MM, Tubaila MF, Awang R, et al. Beliefs and practices regarding childhood fever among parents: a cross-sectional study from Palestine. BMC Pediatr. (2013) 13(1):1–8. doi: 10.1186/1471-2431-13-1
4. Patricia C. Evidence-based management of childhood fever: what pediatric nurses need to know. J Pediatr Nurs. (2014) 29(4):372–5. doi: 10.1016/j.pedn.2014.02.007
5. de Bont EG, Peetoom KK, Moser A, Francis NA, Dinant G-J, Cals JW. Childhood fever: a qualitative study on GPs’ experiences during out-of-hours care. Fam Pract. (2015) 32(4):449–55. doi: 10.1093/fampra/cmv029
6. Goldman RD, Kapoor A, Mehta S. Children admitted to the hospital after returning to the emergency department within 72 h. Pediatr Emerg Care. (2011) 27(9):808–11. doi: 10.1097/PEC.0b013e31822c1273
7. Nadal CF, Garía de Miguel MJ, Campderá AG, Fernández JP, Calatayud GA, Bayle MS, et al. Effectiveness and tolerability of ibuprofen-arginine versus paracetamol in children with fever of likely infectious origin. Acta Paediatr. (2002) 91(4):383–90. doi: 10.1111/j.1651-2227.2002.tb01659.x
8. Stanford Children’s Health LPcsHS. Fever in Children. Stanford, CA: Stanford Medicine Children's Health (2022).
9. Evans SS, Repasky EA, Fisher DT. Fever and the thermal regulation of immunity: the immune system feels the heat. Nat Rev Immunol. (2015) 15(6):335–49. doi: 10.1038/nri3843
10. Mackowiak PA, Borden EC, Goldblum SE, Hasday JD, Munford RS, Nasraway SA, et al. Concepts of fever: recent advances and lingering dogma. Clin Infect Dis. (1997) 25(1):119–38. doi: 10.1086/514520
11. Plaisance KI, Mackowiak PA. Antipyretic therapy: physiologic rationale, diagnostic implications, and clinical consequences. Arch Intern Med. (2000) 160(4):449–56. doi: 10.1001/archinte.160.4.449
12. Blatteis CM. Fever: pathological or physiological, injurious or beneficial? J Therm Biol. (2003) 28(1):1–13. doi: 10.1016/S0306-4565(02)00034-7
13. Tafti BF, Salmani N, Afshari S. The maternal experiences of child care with fever: a qualitative study. Int J Pediatr. (2017) 5(2):4429–37. doi: 10.22038/IJP.2017.21615.1807
14. Karwowska A, Nijssen-Jordan C, Johnson D, Davies HD. Parental and health care provider understanding of childhood fever: a Canadian perspective. Can J Emerg Med. (2002) 4(6):394–400. doi: 10.1017/S1481803500007892
15. Chiappini E, Parretti A, Becherucci P, Pierattelli M, Bonsignori F, Galli L, et al. Parental and medical knowledge and management of fever in Italian pre-school children. BMC Pediatr. (2012) 12(1):1–10. doi: 10.1186/1471-2431-12-97
16. Taveras EM, Durousseau S, Flores G. Parents’ beliefs and practices regarding childhood fever: a study of a multiethnic and socioeconomically diverse sample of parents. Pediatr Emerg Care. (2004) 20(9):579–87. doi: 10.1097/01.pec.0000139739.46591.dd
17. Krantz C. Childhood fevers: developing an evidence-based anticipatory guidance tool for parents. Pediatr Nurs. (2001) 27(6):567–74.12024528
18. El Radhi A, Carroll J, Klein N. Clinical manual of fever in children. Berlin: Springer (2009) 2.
19. Leon LR. Invited review: cytokine regulation of fever: studies using gene knockout mice. J Appl Physiol. (2002) 92(6):2648–55. doi: 10.1152/japplphysiol.01005.2001
21. El-Radhi AS, Carroll J, Klein N. Clinical Manual of Fever in Children. Berlin and Heidelberg: Springer (2009).
22. Organization WH. Integrated Management of Childhood Illness (Chart Booklet). Geneva, Switzerland: World Health Organization (2008).
23. Organization WH. Guidelines for the Treatment of Malaria. Geneva, Switzerland: World Health Organization (2015).
24. O’Grady NP, Barie PS, Bartlett JG, Bleck T, Carroll K, Kalil AC, et al. Guidelines for evaluation of new fever in critically ill adult patients: 2008 update from the American college of critical care medicine and the infectious diseases society of America. Crit Care Med. (2008) 36(4):1330–49. doi: 10.1097/CCM.0b013e318169eda9
25. d'Acremont V, Burnand B, Ambresin A-E, Genton B. Practice guidelines for evaluation of fever in returning travelers and migrants. J Travel Med. (2003) 10(2):s25–45. doi: 10.2310/7060.2003.35132
27. Baumann RJ, Duffner PK. Treatment of children with simple febrile seizures: the AAP practice parameter. Pediatr Neurol. (2000) 23(1):11–7. doi: 10.1016/S0887-8994(00)00148-X
28. Westin E, Levander MS. Parent’s experiences of their children suffering febrile seizures. J Pediatr Nurs. (2018) 38:68–73. doi: 10.1016/j.pedn.2017.11.001
29. Schmitt BD. Fever phobia: misconceptions of parents about fevers. Am J Dis Child. (1980) 134(2):176–81. doi: 10.1001/archpedi.1980.02130140050015
30. Walsh A, Edwards H. Management of childhood fever by parents: literature review. J Adv Nurs. (2006) 54(2):217–27. doi: 10.1111/j.1365-2648.2006.03802.x
31. Soon W, Cheong S, Hong C. Fever phobia in a primary healthcare setting: a Singapore perspective. Ann Acad Med Singap. (2003) 32(5 Suppl):S26–S7.14968724
32. Poirier MP, Collins EP, McGuire E. Fever phobia: a survey of caregivers of children seen in a pediatric emergency department. Clin Pediatr. (2010) 49(6):530–4. doi: 10.1177/0009922809355312
33. Walsh A, Edwards H, Fraser J. Parents’ childhood fever management: community survey and instrument development. J Adv Nurs. (2008) 63(4):376–88. doi: 10.1111/j.1365-2648.2008.04721.x
34. Chang L-C, Liu C-C, Huang M-C. Parental knowledge, concerns, and management of childhood fever in Taiwan. J Nur Res. (2013) 21(4):252–60. doi: 10.1097/jnr.0000000000000007
35. Oshikoya KA. Antimalarial prescriptions for children presenting with uncomplicated malaria to a teaching hospital in Nigeria after the change of national guidelines for malaria treatment. World J Med Sci. (2007) 2(1):49–53.
36. Arora R, Mahajan P. Evaluation of child with fever without source: review of literature and update. Pediatr Clin. (2013) 60(5):1049–62. doi: 10.1016/j.pcl.2013.06.009
37. Langer T, Pfeifer M, Soenmez A, Kalitzkus V, Wilm S, Schnepp W. Activation of the maternal caregiving system by childhood fever–a qualitative study of the experiences made by mothers with a German or a Turkish background in the care of their children. BMC Fam Pract. (2013) 14(1):1–9. doi: 10.1186/1471-2296-14-35
38. Langer T, Pfeifer M, Soenmez A, Tarhan B, Jeschke E, Ostermann T. Fearful or functional-a cross-sectional survey of the concepts of childhood fever among German and Turkish mothers in Germany. BMC Pediatr. (2011) 11(1):1–7. doi: 10.1186/1471-2431-11-41
39. Crocetti M, Sabath B, Cranmer L, Gubser S, Dooley D. Knowledge and management of fever among Latino parents. Clin Pediatr. (2009) 48(2):183–9. doi: 10.1177/0009922808324949
40. Betz MG, Grunfeld AF. ‘Fever phobia’in the emergency department: a survey of children’s caregivers. Eur J Emerg Med. (2006) 13(3):129–33. doi: 10.1097/01.mej.0000194401.15335.c7
41. Bertille N, Purssell E, Corrard F, Chiappini E, Chalumeau M. Fever Phobia 35 Years Later: Did we Fail? Oslo: Wiley Online Library (2016). p. 9–10.
42. Paul SP, Kini PK, Tibrewal SR, Heaton PA. NICE Guideline review: fever in under 5s: assessment and initial management (NG143). Arch Dis Childh Educ Pract. (2021) 107:212–6. doi: 10.1136/archdischild-2021-321718
43. Hay AD, Heron J, Ness A. The prevalence of symptoms and consultations in pre-school children in the avon longitudinal study of parents and children (ALSPAC): a prospective cohort study. Fam Pract. (2005) 22(4):367–74. doi: 10.1093/fampra/cmi035
44. Crocetti M, Moghbeli N, Serwint J. Fever phobia revisited: have parental misconceptions about fever changed in 20 years? Pediatrics. (2001) 107(6):1241–6. doi: 10.1542/peds.107.6.1241
45. Leiser D, Doitsch E, Meyer J. Mothers’ lay models of the causes and treatment of fever. Soc Sci Med. (1996) 43(3):379–87. doi: 10.1016/0277-9536(95)00400-9
46. Kelly M, Sahm L, McCarthy S, O’Sullivan R, Mc Gillicuddy A, Shiely F. Randomised controlled trial of an intervention to improve parental knowledge and management practices of fever. BMC Pediatr. (2019) 19(1):1–10. doi: 10.1186/s12887-019-1808-9
47. FDRE. Ethiopia_ Regions MCT-PS. According to Census Results and Latest Official Projections. Addis Ababa, Ethiopia: Central Statistics Agency (CSA) (2015).
49. MacMahon D, Brabyn C, Dalziel SR, McKinlay CJ, Tan E. Fever phobia in caregivers presenting to New Zealand emergency departments. Emerg Med Australas. (2021) 33(6):1074–81. doi: 10.1111/1742-6723.13804
50. AlAteeq MM, AlBader BO, Al-Howti SY, Alsharyoufi M, Abdullah JB. Parent’s knowledge and practice in home management of fever in their children in Riyadh, Saudi Arabia. J Family Med Prim Care. (2018) 7(5):1012. doi: 10.4103/jfmpc.jfmpc_18_18
51. Fields E, Chard J, Murphy MS, Richardson M. Assessment and initial management of feverish illness in children younger than 5 years: summary of updated NICE guidance. Br Med J. (2013) 346. doi: 10.1136/bmj.f2866
52. de Bont EG, Francis NA, Dinant G-J, Cals JW. Parents’ knowledge, attitudes, and practice in childhood fever: an internet-based survey. Br J Gen Pract. (2014) 64(618):e10–e6. doi: 10.3399/bjgp14X676401
53. Baxter C, Gorodzinsky FP, Leduc D, Munk P, Noonan P, Woods S. Temperature measurement in paediatrics. Paediatr Child Health. (2000) 5:273–84. doi: 10.1093/pch/5.5.273
54. Robinson JL. Body temperature measurement in paediatrics: which gadget should we believe? Paediatr Child Health. (2004) 9(7):457–9. doi: 10.1093/pch/9.7.457
55. Sullivan JE, Farrar HC. Section on clinical pharmacology and therapeutics; committee on drugs. Fever and antipyretic use in children. Pediatrics. (2011) 127(3):580–7. doi: 10.1542/peds.2010-3852
56. Parmar R, Sahu D, Bavdekar S. Knowledge, attitude and practices of parents of children with febrile convulsion. J Postgrad Med. (2001) 47(1):19.11590285
57. Kerdar SH, Himbert C, Martin DD, Jenetzky E. Cross-sectional study of parental knowledge, behaviour and anxiety in management of paediatric fever among German parents. BMJ open. (2021) 11(10):e054742. doi: 10.1136/bmjopen-2021-054742
58. Elbur A. Childhood fever and its management: differences in knowledge and practices between mothers and fathers in Taif; Saudi Arabia. World J Pharm Res. (2014) 3(4536–48):18.
59. Anokye R, Amihere R, Abbiaw P, Acheampong E, Gyamfi N, Budu-Ainooson A. Childhood fever knowledge and management: a case of mothers with children under five years. Int J Pediatr Res. (2018) 4(2):1–7. doi: 10.23937/2469-5769/1510044
60. Thota S, Ladiwala N, Sharma PK, Ganguly E. Fever awareness, management practices and their correlates among parents of under five children in urban India. Int J Contemp Pediatrics. (2018) 5(4):1368. doi: 10.18203/2349-3291.ijcp20182525
61. Park HR, Kwon IS. Knowledge and practice of fever management by mothers of preschool children at home. Child Health Nur Res. (2017) 23(2):127–36. doi: 10.4094/chnr.2017.23.2.127
62. Kelly M, Sahm LJ, Shiely F, O’Sullivan R, de Bont EG, Mc Gillicuddy A, et al. Parental knowledge, attitudes and beliefs on fever: a cross-sectional study in Ireland. BMJ Open. (2017) 7(7):e015684. doi: 10.1136/bmjopen-2016-015684
63. Ahammed B, Maniruzzaman M, Ferdausi F, Abedin MM, Hossain MT. Socioeconomic and demographic factors associated with low birth weight in Nepal: data from 2016 Nepal demographic and health survey. Soc Health Behav. (2020) 3(4):158. doi: 10.4103/SHB.SHB_46_20
64. Korkut Y. Mothers’ knowledge and management of fever in febrile children. Family Pract Palliat Care. (2018) 3(3):113–6. doi: 10.22391/fppc.370931
65. Raak C, Scharbrodt W, Berger B, Boehm K, Martin D. The use of calf compresses for gentle fever reduction-what do we know? A scoping review. Collegian. (2022) 29(5):598–611. doi: 10.1016/j.colegn.2022.01.010
66. Bank W. GDP report of different countries. (2021). Available online at: https://data.worldbank.org/indicator/NY.GDP.MKTP.CD
67. Nnebue C, Ifeadike G, Nworah N, Duru C. The effect of socio-demographic status of mother s on the management of febrile illnesses among under-fives that presented in a tertiary hospital in south-east Nigeria: a two-year review. Afrimedic J. (2010) 1(1):27–30.
68. Agushybana F. Influence of husband support on complication during pregnancy and childbirth in Indonesia. J Health Res. (2016) 30(4):249–55. doi: 10.14456/jhr.2016.34
69. Mcerlean MA, Bartfield JM, Kennedy DA, Gilman EA, Stram RL, Raccio-Robak N. Home antipyretic use in children brought to the emergency department. Pediatr Emerg Care. (2001) 17(4):249–51. doi: 10.1097/00006565-200108000-00005
70. Barrett TW, Norton VC. Parental knowledge of different acetaminophen concentrations for infants and children. Acad Emerg Med. (2000) 7(6):718–21. doi: 10.1111/j.1553-2712.2000.tb02054.x
71. Athamneh L, El-Mughrabi M, Athamneh M, Essien EJ, Abughosh S. Parents’ knowledge, attitudes and beliefs of childhood fever management in Jordan: a cross-sectional study. J Appl Res Children. (2014) 5(1):8. doi: 10.58464/2155-5834.1161
72. Chukwuocha U, Nwakwuo G, Emerole C, Dozie I, Nwuda O. Prevalent home management techniques and outcome among mothers of febrile children in Eastern Nigeria. J Public Health Epidemiol. (2014) 6(3):111–8. doi: 10.5897/JPHE2013.0591
73. Enarson MC, Ali S, Vandermeer B, Wright RB, Klassen TP, Spiers JA. Beliefs and expectations of Canadian parents who bring febrile children for medical care. Pediatrics. (2012) 130(4):e905–e12. doi: 10.1542/peds.2011-2140
74. Aslam M, Kingdon GG. Parental education and child health—understanding the pathways of impact in Pakistan. World Dev. (2012) 40(10):2014–32. doi: 10.1016/j.worlddev.2012.05.007
75. Rkain M, Rkain I, Safi M, Kabiri M, Ahid S, Benjelloun B. Knowledge and management of fever among Moroccan parents. East Mediterr Health J. (2014) 20:397–402.24960517
Keywords: fever, under-five, parents, knowledge, practice, Ethiopia
Citation: Assimamaw NT, Gonete AT and Terefe B (2024) Survey of knowledge, practice, and associated factors toward home management of childhood fever among parents visiting Gondar health facilities in 2022. Front. Pediatr. 12:1100828. doi: 10.3389/fped.2024.1100828
Received: 17 November 2022; Accepted: 9 February 2024;
Published: 1 March 2024.
Edited by:
Ihab Tewfik, University of Westminster, United KingdomReviewed by:
Gebrehiwot Berie Mekonnen, Debre Tabor University, Ethiopia© 2024 Assimamaw, Gonete and Terefe. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Almaz Tefera Gonete YWxtYXp0ZWZlcmFnM0BnbWFpbC5jb20=
Abbreviations IDSA, infectious disease society of America; OVLT, organum vasculosum of the lamina terminalis; RCT, randomized control trial; WHO, world health organization.
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.