- 1School of Public Health Sciences, University of Waterloo, Waterloo, ON, Canada
- 2Child Health & Exercise Medicine Program, McMaster University, Hamilton, ON, Canada
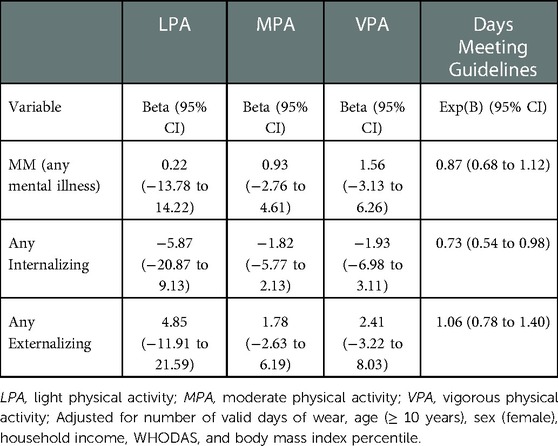
Children with physical illnesses often experience co-occurring mental illness (known as multimorbidity; MM) and it is currently unknown if MM is associated with physical activity (PA) and if the association differs between internalizing and externalizing disorders. Therefore, the aim of this study was to examine the association between MM and PA. Baseline data from the Multimorbidity in Children and Youth Across the Life Course (MY LIFE) cohort was used. MY LIFE is an ongoing prospective study that follows children ages 2 to 16 years with a chronic physical illness and measures PA using accelerometry and mental illness using the Mini International Neuropsychiatric Interview for Children and Adolescents. 140 children (53.2%) provided valid accelerometer data. Children with internalizing disorders recorded less light (B = −5.87), moderate (B = −1.82), and vigorous PA (B = −1.93) and fewer days meeting PA guidelines [Exp(B) = 0.73] and those with externalizing disorders recorded more light (B = 4.85), moderate (B = 1.78), and vigorous PA (B = 2.41) and more days meeting PA guidelines [Exp(B) = 1.06]. However, only the association between internalizing disorder and days meeting PA guidelines was statistically significant. This study provides preliminary evidence that children with MM may accumulate less PA depending on the type of mental illness they experience.
1. Introduction
Physical activity (PA) results in several positive physical and mental health benefits for both adults and children (1, 2). Evidence in children shows that PA contributes to healthy body weight, cardiovascular and muscular fitness, bone mineral density, healthy cholesterol, blood lipids, and blood pressure, as well as decreases symptoms of depression and anxiety, and can improve self-esteem (2–4). Multiple national and international organizations have evidence-informed daily PA guidelines that recommend children ages 5-to-17 years of age engage in at least 60 min of moderate -to-vigorous PA (MVPA) and children 2 to 4 years should be active at any intensity for at least 180 min (5, 6). Unfortunately, 67%–80% of children worldwide do not meet these recommendations (7, 8). This is particularly concerning given that health habits formed in childhood track consistently into adulthood, leading to prolonged exposure to the negative consequences of physical inactivity (9). Furthermore, emerging evidence suggests that PA engagement during adolescence has a lasting effect on the risk of developing multiple health concerns in middle adulthood (10). Therefore, it is critical that the patterns and correlates of PA early in life are examined to determine effective methods to promote PA to enable children to reap these positive physical and mental health benefits.
Surveillance of PA has typically excluded children and adolescents with chronic physical illness, leading to evidence on PA levels for these children to be less robust (11). However, prevalence estimates suggest that 1 in 4 children has a chronic physical illness (12), warranting specific investigation into their risk of physical inactivity. Recent estimates indicate that children with chronic physical illnesses are similarly inactive compared with healthy controls (11), but there is a gap in the literature regarding possible reasons for physical inactivity among these children. Some evidence suggests that functional limitations due to their physical illness may prohibit engagement in PA (13). Additionally, upwards of 50% of children with a physical illness experience co-occurring mental illness (known as multimorbidity, MM) (14). It is established that children with mental illnesses often experience low levels of PA (15), however, the deficit may depend on the type of mental illness. For example, children with an externalizing disorder such as attention-deficit hyperactivity disorder have been reported to show increased unorganized PA (16), whereas adolescents with internalizing disorders (e.g., depressive symptoms) have been shown to have lower levels of participation in PA (17). It is unknown if MM is associated with PA in children.
The objective of this study was to examine the association between MM and PA in children and determine whether the association differs in those with an internalizing or externalizing mental illness; it is hypothesized that children with internalizing disorders will engage in less PA and those with externalizing behaviours will engage in more PA.
2. Methods
2.1. Participants
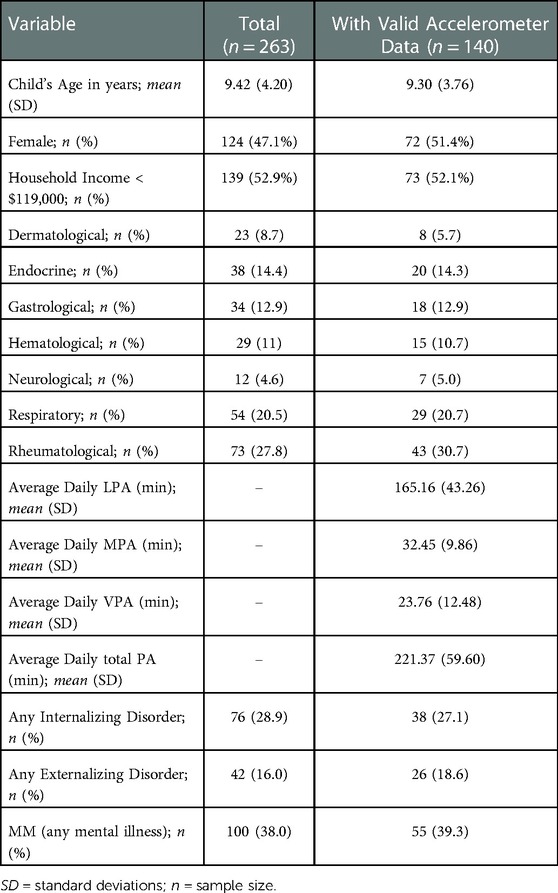
Baseline data from the Multimorbidity in Children and Youth across the Life Course (MY LIFE) study was used for this analysis. This prospective cohort study follows 263 children ages 2 to 16 years (mean age = 9.42, SD = 3.98) with a physician-diagnosed chronic physical illness (defined as a condition that has or is expected to last ≥12 months with functional limitations, dependencies, and the need for additional healthcare; including dermatological, endocrine, gastroenterological, hematological, neurological, respiratory, and rheumatological disorders). Participants were recruited from outpatient clinics at McMaster Children's Hospital and were required to be able to and have parents able to communicate in English. The sampling procedures and description of the full cohort have been previously published (18, 19).
2.2. Study participants
Eligible and consenting families were scheduled to complete baseline appointments that were approximately 60–90 min in length with subsequent follow up at 6, 12, and 24 months. Baseline assessments were conducted from August 2017 to November 2019. Computer-assisted self-report questionnaires were administered to all parents and participants over the age of 10 years. Trained research assistants also collected biological samples, anthropometric data, and fitted each participant with an accelerometer. Written consent was obtained from all parents and participants over 16 years; assent was collected from participants ages 7–15 years. Ethical approval for this study was obtained from the Hamilton Integrated Research Ethical Board and the University of Waterloo Human Research Ethics Board.
2.3. Measures
2.3.1. Mental illness
To determine the presence of multimorbidity (MM), all parents (over the telephone) and participants over 10 years of age (in-person) were asked to complete the Mini International Neuropsychiatric Interview for Children and Adolescents (MINI-KID) (20). The MINI-KID contains modules aligned with the diagnostic criteria of the DSM-5 and ICD-10 to detect internalizing disorders (i.e., major depressive episode, separation anxiety disorder, social anxiety disorder, specific phobias, and generalized anxiety disorder) and externalizing disorders (i.e., attention-deficit hyperactivity disorder, conduct disorder, and oppositional defiant disorder). The MINI-KID has excellent psychometric properties among children from clinical settings (21–24). Participants were categorized as MM if they screened positive for at least one mental illness; if they did not screen positive for any mental illness, they were categorized as not MM (physical illness only).
2.3.2. Physical activity
Participants were asked to wear an Actigraph GT3X accelerometer fitted around their waist to be worn over their right hip for 7 consecutive days (25). Participants and their parents were instructed to remove the device only during sleep and water-based activities and a logbook was provided to each family to record wear-time. Three second epochs were used to record physical activity (26). The Actilife software (Actigraph) was used to clean and process the accelerometer data. Data were considered valid if at least 10 h of wear-time were recorded on 3 days; non-wear time was defined as >60 min of consecutive zero counts or when the logbook indicated the device was removed (27, 28). The Evenson cut points were used to define PA intensity of light, moderate, and vigorous as >100, ≥2,296, ≥4,012 counts per minute, respectively (29). The number of days children met PA guidelines for their respective age categories was also computed. Guidelines for children <5 years state that average daily total PA should be at least 180 min with 3 to 4 year olds requiring at least an average daily of 60 min of MVPA (30). Guidelines for children 5 to 17 years state that they should engage in average daily 60 min of MVPA (30). Given the common guidance related to MVPA, we focused on this PA characteristic in our analyses.
2.3.3. Covariates
Parents were asked to complete the 12-item World Health Organization Disability Assessment Schedule (WHODAS) 2.0 to determine the level of physical functioning of their child (31). Self-report questionnaire for parents included items from population-based surveys conducted by Statistics Canada on various demographic information including household income before taxes, and age and sex, relating to both themselves and their child. Body mass index (BMI) was computed using participants' standing height and weight and percentiles were calculated with the World Health Organization growth reference data for children (32).
2.4. Statistical analyses
Using data only from participants with valid accelerometer data, multiple regression models were built with average daily minutes spent in each intensity of PA (light, moderate, and vigorous PA) as dependent variables. Average daily minutes of PA in each intensity were computed as the sum of the minutes of PA recorded on each valid day of wear divided by the number of valid days of wear. Three regression models were built separately using MM status (any mental illness vs. no mental illness), presence of internalizing disorder (vs. no internalizing disorder), and presence of externalizing disorder (vs. no externalizing disorder), respectively, as the independent variables. Three Poisson regression models with the number of days meeting PA guidelines as the dependent variable were also conducted. All models were adjusted for the number of valid days of accelerometer wear, age (<10 years and ≥10 years) sex, household income, WHODAS 2.0 scores, and BMI percentile. All statistical analyses were performed in SPSS (33) with α < .05. SPSS model syntax and assumption testing results are provided in a Supplementary file.
2.5. Missing data
Valid accelerometer data were obtained from 140 of the 263 total children (53.2%) enrolled in the study at baseline. Among those with valid accelerometer data there were nine children who did not have height and/or weight data available to compute BMI, and therefore were removed from the analyses. Chi-square tests showed that the proportion of missing accelerometer and BMI data was not different between males and females, between those <10 years or ≥10 years of age, or by MM status.
3. Results
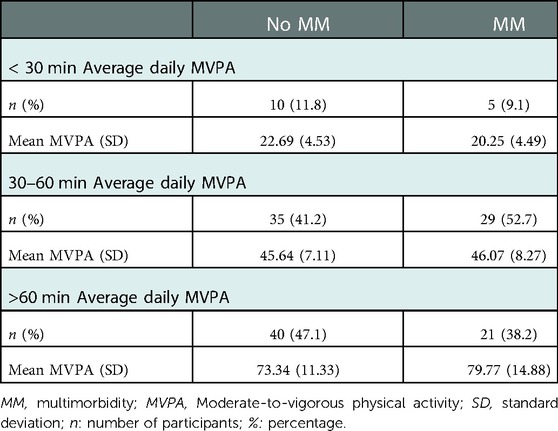
Children in the analytical sample (i.e., valid accelerometer data) were comparable to the total sample with respect to demographic and clinical characteristics (see Table 1). On average, children spent majority of their PA in light PA, with decreasing amounts of time spent in higher intensities of PA (see Table 1). Table 2 shows that of children without MM, just under half had a daily average MVPA of >1 h, averaging 73.34 min. Of children with MM, only 38% engaged in >1 h of MVPA daily, averaging 79.77 min.
The regression analyses (Table 3) show that children with MM had non-significantly fewer number of days meeting PA guidelines, and non-significantly more minutes of LPA, MPA and VPA. Children with internalizing disorders had non-significantly fewer minutes of all intensities of PA, as well as fewer days meeting PA guidelines, whereas those with externalizing disorders had non-significantly more minutes of all intensities of PA and non-significantly more days meeting PA guidelines. Only the association between internalizing disorder and days meeting PA guidelines was statistically significant.
4. Discussion
The study examined the association between the presence of MM and PA, and whether this association differed as a function of the type of mental illness, in children. While associations were not statistically significant, the pattern of results suggest that MM may be associated with fewer days meeting the recommended levels of PA. Among those engaging in >60 min of daily MVPA, there are fewer children with MM than those without; however, the former has a higher average MVPA compared to those without MM. These results suggest that children with MM may be less likely to reach daily recommended levels of MVPA, however on days they do, their activity levels are high. Moreover, when categorizing MM as the presence of either an internalizing or externalizing behaviour, the results suggest a divergent association with PA, with internalizing disorders non-significantly associated with less PA and externalizing disorders non-significantly associated with more PA. Therefore, the null positive association between any MM and minutes engaged in PA is likely obscured due to the opposite associations with internalizing and externalizing disorders.
Children with chronic physical illnesses have been reported as similarly inactive compared to their healthy peers (11), however to our knowledge there are no studies comparing the PA levels of children with physical illness to those with multimorbidity. The results of this study suggest that children with MM have similar average levels of PA, however, may accumulate these minutes in different intensities and across fewer days in the week and this may depend on the type of mental illness they experience. Reasons for children with MM meeting recommended MVPA on fewer days of the week are unclear. The complexities of their health may result in days in which children have low energy and motivation and even light PA may feel like a challenge, whereas other days a positive mood allows them to expend high amounts of energy. This may explain why children with internalizing disorder were less likely to accumulate sufficient daily PA. Evidence shows that adolescents with mood or anxiety disorders may feel tired and/or disinterested in participating in PA and may also prefer to avoid the social aspects of PA (3). Children experiencing internalizing disorders may have fewer days on which the psychopathology of their disorders does not impact their motivation and energy to engage in PA. Whereas externalizing disorders are typically characterized by hyperkinetic behaviours (e.g., running or climbing in inappropriate situations), and therefore daily PA may be higher. However, it is important to note that PA engaged in through hyperkinetic behaviours may be unorganized as it has been shown that children with externalizing disorders do not report high levels of participation in sport or intentional PA (15). Alternatively, socio-environmental factors may influence PA levels such as overprotective care environments, lack of access/opportunities for PA, or knowledge- and self-efficacy-barriers regarding safe and appropriate types of PA. It is worth noting that in a sample of 13–17 year old children, Mangerud (15) found that youth with mental illnesses (both internalizing and externalizing) were less active compared to their healthy peers. Therefore, these socio-environmental factors may operate similarly on both children with a physical illness and those with MM, such that it reduces the differential risk of inactivity. Furthermore, there are likely additional barriers known to constrain PA of children without illness that may be similarly relevant to children with MM such as motor competence, self-image, and peer and parental support for PA (15, 34, 35).
We believe that there are currently no other studies examining the association between PA and MM among children. Strengths of this study include the objective measurement of PA using accelerometery, negating the recall and social desirability biases inherent in self-report (36). MY LIFE also implemented the MINI-KID assessment to provide a reliable and valid assessment of mental illness aligned with clinical diagnoses, thereby providing a more robust determination of MM beyond symptomology. Additionally, participants were sampled across a range physical illness to increase the generalizability of the sample.
However, methodological weaknesses must also be acknowledged. Most limiting is the analytic sample size, precluding conclusions based on the model results; therefore, the analyses are exploratory and hypothesis-generating. Also, the data do not provide insight into the context or type of PA. It will be important to implement measures of qualitative assessments of PA concurrently with accelerometery to understand the types of PA children are engaging in. Finally, this study did not include a comparison of children without a physical illness, therefore it remains unclear how the presence of a mental illness is associated with PA when the child does not have a physical illness.
4.1. Conclusions and future directions
Children with and without MM have similar average levels of PA; however, may accumulate these minutes in different intensities and across fewer days in the week and this depends on the type of mental illness they experience. These results are strictly exploratory, however they provide support to further study the complex effect of MM on PA engagement to determine if these associations are robust.
Data availability statement
The datasets presented in this article are not readily available because research ethical approval for this study does not permit the public sharing of study data. However, requests to access data should be made in writing by contacting the corresponding author by email to initiate discussions regarding potential research projects.
Ethics statement
The studies involving human participants were reviewed and approved by Hamilton Integrated Research Ethical Board and the University of Waterloo Human Research Ethics Board. Written informed consent to participate in this study was obtained from all parents and participants over 16 years; assent was collected from participants ages 7–15 years.
Author contributions
CB formulated the research question, cleaned, analysed, and interpreted the data, and drafted the manuscript; BWT guided the interpretation of the results, and assisted with editing the manuscript; MAF is the Principle Investigator of the MY LIFE study, assisted with formulation of the research questions, provided the data, and assisted with interpretation the results and editing the manuscript; All authors contributed to the article and approved the submitted version.
Funding
MY LIFE was funded by the Canadian Institutes of Health Research (PJT-148602). The funding source had no role in the design of the study, collection, analysis, and interpretation of data, nor in the writing of the manuscript. Bedard is funded by a CIHR Fellowship. Timmons and Ferro are supported by the Canada Research Chairs Program.
Acknowledgments
We wish to thank the children, parents and health professionals and their staff involved in the MY LIFE as well as Jessica Zelman and Robyn Wojcicki for coordinating the study and assisting with accelerometer cleaning.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at https://www.frontiersin.org/articles/10.3389/fped.2023.920629/full#supplementary-material.
References
1. Lee I-M, Shiroma EJ, Lobelo F, Puska P, Blair SN, Katzmarzyk PT. Effect of physical inactivity on major non-communicable diseases worldwide: an analysis of burden of disease and life expectancy. Lancet. (2012) 380(9838):219–29. doi: 10.1016/S0140-6736(12)61031-9
2. Janssen I, LeBlanc AG. Systematic review of the health benefits of physical activity and fitness in school-aged children and youth. Int J Behav Nutr Phys Act. (2010) 7:40. doi: 10.1186/1479-5868-7-40
3. Biddle SJ, Asare M. Physical activity and mental health in children and adolescents: a review of reviews. Br J Sports Med. (2011) 45(11):886–95. doi: 10.1136/bjsports-2011-090185
4. Poitras VJ, Gray CE, Borghese MM, Carson V, Chaput J-P, Janssen I, et al. Systematic review of the relationships between objectively measured physical activity and health indicators in school-aged children and youth. Appl Physiol Nutr Metab. (2016) 41(6):S197–239. doi: 10.1139/apnm-2015-0663
5. Twisk JW. Physical activity guidelines for children and adolescents. Sports Med. (2001) 31(8):617–27. doi: 10.2165/00007256-200131080-00006
6. WHO W. Global recommendations on physical activity for health. Geneva World Heal Organ. (2010) 60:17–21. https://www.who.int/publications/i/item/9789241599979
7. Aubert S, Barnes JD, Abdeta C, Nader PA, Adeniyi AF, Aguilar-Farias N, et al. Global matrix 3.0 physical activity report card grades for children and youth: results and analysis from 49 countries. J Phys Act Health. (2018) 15(s2):S251–73. doi: 10.1123/jpah.2018-0472
8. Hallal PC, Andersen LB, Bull FC, Guthold R, Haskell W, Ekelund U. Global physical activity levels: surveillance progress, pitfalls, and prospects. Lancet. (2012) 380(9838):247–57. doi: 10.1016/S0140-6736(12)60646-1
9. Telama R. Tracking of physical activity from childhood to adulthood: a review. Obes Facts. (2009) 2(3):187–95. doi: 10.1159/000222244
10. Feter N, Leite JS, Umpierre D, Caputo EL, Rombaldi AJ. Multimorbidity and leisure-time physical activity over the life course: a population-based birth cohort study. BMC Public Health. (2021) 21(1):700. doi: 10.1186/s12889-021-10719-7
11. Elmesmari R, Reilly JJ, Martin A, Paton JY. Accelerometer measured levels of moderate-to-vigorous intensity physical activity and sedentary time in children and adolescents with chronic disease: a systematic review and meta-analysis. PloS One. (2017) 12(6):e0179429. doi: 10.1371/journal.pone.0179429
12. van Cleave J, Gortmaker SL, Perrin JM. Dynamics of obesity and chronic health conditions among children and youth. JAMA. (2010) 303(7):623–30. doi: 10.1001/jama.2010.104
13. Li R, Sit CH, Jane JY, Duan JZ, Fan TC, McKenzie TL, et al. Correlates of physical activity in children and adolescents with physical disabilities: a systematic review. Prev Med. (2016) 89:184–93. doi: 10.1016/j.ypmed.2016.05.029
14. Butler A, Van Lieshout RJ, Lipman EL, MacMillan HL, Gonzalez A, Gorter JW, et al. Mental disorder in children with physical conditions: a pilot study. BMJ Open. (2018) 8(1):e019011. doi: 10.1136/bmjopen-2017-019011
15. Mangerud W, Bjerkeset O, Lydersen S, Indredavik M. Physical activity in adolescents with psychiatric disorders and in the general population. Child Adolesc Psychiatry Ment Health. (2014) 8(1):2. doi: 10.1186/1753-2000-8-2
16. van Egmond-Fröhlich AWA, Weghuber D, de Zwaan M. Association of symptoms of attention-deficit/hyperactivity disorder with physical activity, Media time, and food intake in children and adolescents. PloS One. (2012) 7(11):e49781. doi: 10.1371/journal.pone.0049781
17. Sabiston CM, O’Loughlin E, Brunet J, Chaiton M, Low NC, Barnett T, et al. Linking depression symptom trajectories in adolescence to physical activity and team sports participation in young adults. Prev Med. (2013) 56(2):95–8. doi: 10.1016/j.ypmed.2012.11.013
18. Ferro MA, Lipman EL, Van Lieshout RJ, Gorter JW, Shanahan L, Boyle M, et al. Multimorbidity in children and youth across the life-course (MY LIFE): protocol of a Canadian prospective study. BMJ open. (2019) 9(11):e034544. doi: 10.1136/bmjopen-2019-034544
19. Ferro M, Lipman EL, Van Lieshout RJ, Timmons B, Shanahan L, Gorter J, et al. Cohort profile: multimorbidity in children and youth across the life-course (MY LIFE) study. J Can Acad Child Adolesc Psychiatry. (2021) 30(2):104–15.33953762
20. Sheehan DV, Shytle D, Milo K, Janavs J, Lecrubier Y. MINI international neuropsychiatric interview for children and adolescents (MINI-KID). J Clin Psychiatry. (2010) 71(3):313–26. doi: 10.4088/JCP.09m05305whi
21. Sheehan DV, Sheehan KH, Shytle RD, Janavs J, Bannon Y, Rogers JE, et al. Reliability and validity of the mini international neuropsychiatric interview for children and adolescents (MINI-KID). J Clin Psychiatry. (2010) 71(3):313–26. doi: 10.4088/JCP.09m05305whi
22. Boyle MH, Duncan L, Georgiades K, Wang L, Comeau J, Ferro MA, et al. The 2014 Ontario child health study emotional behavioural scales (OCHS-EBS) part II: psychometric adequacy for categorical measurement of selected DSM-5 disorders. Can J Psychiatry. (2019) 64(6):434–42. doi: 10.1177/0706743718808251
23. Duncan L, Georgiades K, Wang L, Van Lieshout RJ, MacMillan HL, Ferro MA, et al. Psychometric evaluation of the Mini international neuropsychiatric interview for children and adolescents (MINI-KID). Psychol Assess. (2018) 30(7):916. doi: 10.1037/pas0000541
24. McDonald E, Whitney S, Horricks L, Lipman EL, Ferro MA. Parent-child agreement on the Mini international neuropsychiatric interview for children and adolescents (MINI-KID). J Can Acad Child Adolesc Psychiatry. (2021) 4:264–72.
25. Trost SG, Pate RR, Freedson PS, Sallis JF, Taylor WC. Using objective physical activity measures with youth: how many days of monitoring are needed? Med Sci Sports Exerc. (2000) 32(2):426. doi: 10.1097/00005768-200002000-00025
26. Obeid J, Nguyen T, Gabel L, Timmons BW. Physical activity in Ontario preschoolers: prevalence and measurement issues. Appl Physiol Nutr Metab. (2011) 36(2):291–7. doi: 10.1139/h11-002
27. Colley R, Gorber SC, Tremblay MS. Quality control and data reduction procedures for accelerometry-derived measures of physical activity. Health Rep. (2010) 21(1):63.20426228
28. Troiano RP, Berrigan D, Dodd KW, Masse LC, Tilert T, McDowell M, et al. Physical activity in the United States measured by accelerometer. Med Sci Sports Exercise. (2008) 40(1):181. doi: 10.1249/mss.0b013e31815a51b3
29. Trost SG, Loprinzi PD, Moore R, Pfeiffer KA. Comparison of accelerometer cut points for predicting activity intensity in youth. Med Sci Sports Exerc. (2011) 43(7):1360–8. doi: 10.1249/MSS.0b013e318206476e
30. Tremblay MS, Carson V, Chaput J-P, Connor Gorber S, Dinh T, Duggan M, et al. Canadian 24-Hour Movement guidelines for children and youth: an integration of physical activity, sedentary behaviour, and sleep 1. Appl Physiol Nutr Metab. (2016) 41(6):S311–27. doi: 10.1139/apnm-2016-0151
31. Üstün TB, Kostanjsek N, Chatterji S, Rehm J. Measuring health and disability: manual for WHO disability assessment schedule WHODAS 2.0. World Health Organ. (2010). p. 1–89
32. de Onis M, Onyango AW, Borghi E, Siyam A, Nishida C, Siekmann J. Development of a WHO growth reference for school-aged children and adolescents. Bull W H O. (2007) 85:660–7. doi: 10.2471/BLT.07.043497
34. Sallis JF, Prochaska JJ, Taylor WC. A review of correlates of physical activity of children and adolescents. Med Sci Sports Exercise. (2000) 32(5):963–75. doi: 10.1097/00005768-200005000-00014
35. Schmutz EA, Leeger-Aschmann CS, Radtke T, Muff S, Kakebeeke TH, Zysset AE, et al. Correlates of preschool children's Objectively measured physical activity and sedentary behavior: a cross-sectional analysis of the SPLASHY study. Int J Behav Nutr Phys Act. (2017) 14(1):1. doi: 10.1186/s12966-016-0456-9
Keywords: physical activity, multimorbidity (MM), children, youth, mental illness
Citation: Bedard C, Timmons BW and Ferro MA (2023) Exploratory examination of the association between physical-mental multimorbidity and physical activity in children. Front. Pediatr. 11:920629. doi: 10.3389/fped.2023.920629
Received: 14 April 2022; Accepted: 6 January 2023;
Published: 2 February 2023.
Edited by:
Veit Roessner, University Hospital Carl Gustav Carus, GermanyReviewed by:
Shuliweeh Alenezi, King Saud University, Saudi ArabiaSrinivas Dannaram, Banner - University Medical Center Phoenix, Banner Health, United States
© 2023 Bedard, Timmons and Ferro. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Chloe Bedard YzNiZWRhcmRAdXdhdGVybG9vLmNh
Specialty Section: This article was submitted to Child and Adolescent Psychiatry, a section of the journal Frontiers in Pediatrics
 Chloe Bedard
Chloe Bedard Brian W. Timmons
Brian W. Timmons Mark A. Ferro
Mark A. Ferro