- 1Department of Neonatology, Department of Obstetrics and Gynecology, The Third Affiliated Hospital of Guangzhou Medical University, Guangzhou, China
- 2Guangdong Provincial Key Laboratory of Major Obstetric Diseases, Guangdong Pronvincial Clinical Research Center for Obstetrics and Gynecology, Guangzhou, China
- 3Department of Pediatrics, The Third Affiliated Hospital of Guangzhou Medical University, Guangzhou, China
- 4Scientific Research Center, The Second Affiliated Hospital of Guangdong Medical University, Zhanjiang, China
Neonatal genital prolapse is a rare situation. This report presents a unique case involving a pair of premature female twins who both developed vaginal wall prolapse without any neurological deficits. Multiple factors such as selective intrauterine growth restriction, feeding intolerance, extrauterine growth retardation, and elevated intra-abdominal pressure after birth may have contributed to the development of this phenomenon. Notably, the severity of prolapse was more pronounced in the twin with lower birth weight and smaller for gestational age. After a five-month follow-up period, the twins’ prolapsed vaginal wall fully retracted due to a combination of conservative treatment and enhanced nutritional support.
Introduction
Neonatal genital prolapse (NGP) is a rare disorder, which is often associated with spinal bifida, but it can also manifest in the absence of any underlying defects (1, 2). The description of NGP firstly concentrated in term infants and then sporadic cases of NGP in premature infants were reported, but all of them were singleton pregnancy (3, 4). No reports of twins about NGP have been retrieved. This is the first case reported the premature twins who experienced genital prolapse despite the absence of neurological deficits.
Case report
The monochorionic twins were delivered via cesarean section at 34 weeks of gestation due to the selective intrauterine growth restriction. This was the mother's first naturally conceived pregnancy, during which she refrained from smoking or exposure to harmful substances. Both twins are female, displayed a weight disparity of 36% at birth, with the second-born twin being smaller (1,130 g, <3rd percentile). Upon admission to the neonatal intensive care unit, no conspicuous physical anomalies were noted although the labia majora did not fully cover the labia minora, consistent with other preterm infants. The twins were treated with the continuous positive airway pressure ventilation (for less than 7 days) without needing steroids during their hospital stay.
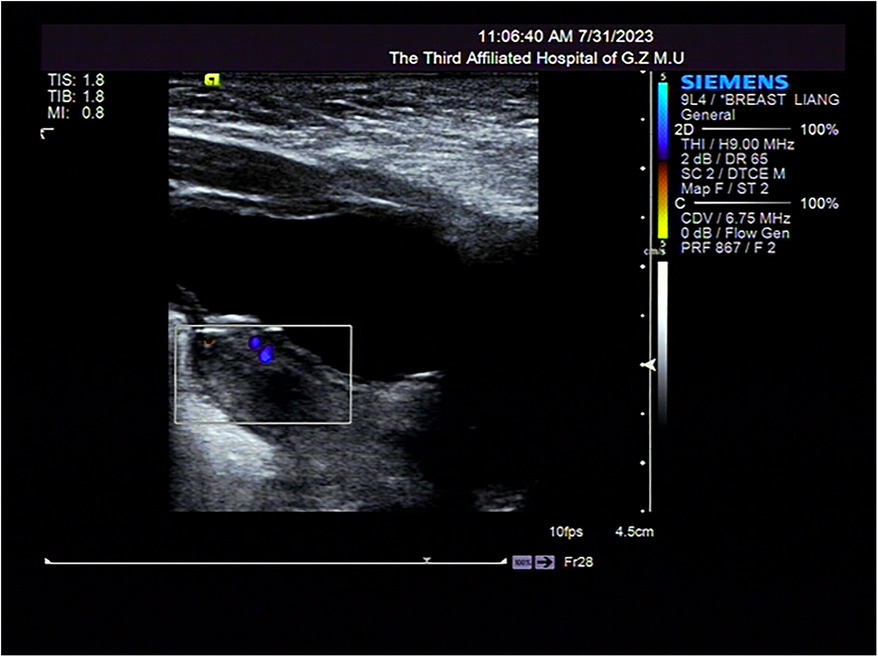
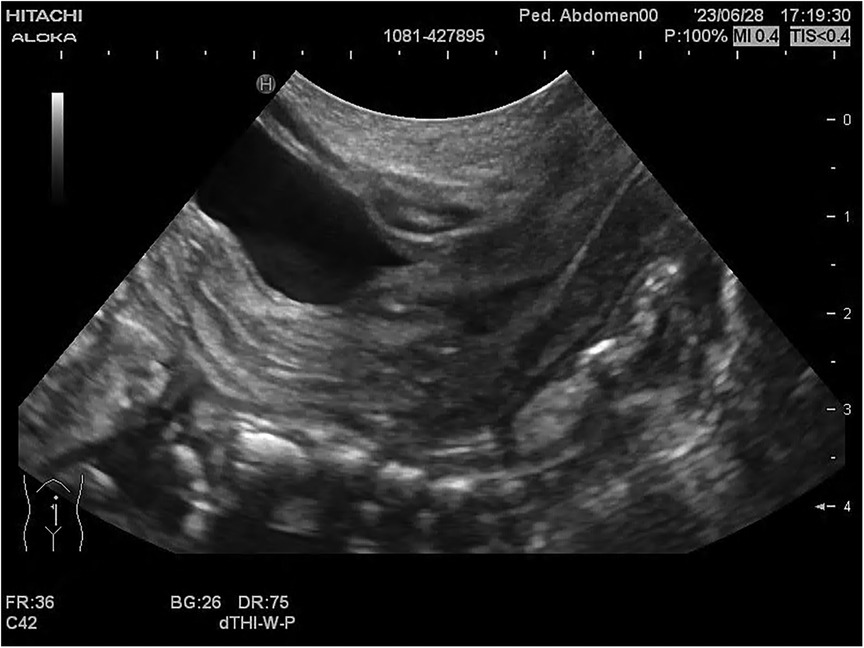
Necrotizing enterocolitis was suspected in both twins because of their inability to tolerate feed and the repeated occurrence of bloody stools. As a result, it was decided to withhold oral feeding three days before gradually resuming enteral feeds. Persistent abdominal distension persisted during this period. Moreover, the weight gain of twins is slow, less than 3rd percentile when corrected for gestational age at full term. On the 40th day after the birth of the first-born twin and the 43rd day after the second-born twin's birth, a light red, soft tissue protrusion became evident in the perineal area. The distal end of the prolapsed mass was clearly visible at the the perineal orifice (Figures 1, 3). The urethral meatus was in a normal position and the twins urinated normally. Pelvic and abdominal ultrassonography revealed no abnormalities in the position of the uterine body or cervix, and no prominent mass echoes were observed in the bilateral adnexal region. The anomalous lesions extending from the vaginal wall were diagnosed as vaginal wall prolapse (Figures 2, 4). On routine cranial ultrasound a subependymal hemorrhage was detected, a spinal x-ray, as well as an magnetic resonance imaging(MRI) under oral chloral of head, lumbar spine and thoracic spine, revealed no evidence of congenital neuromuscular conditions. Besides, neither Neonatal Behavioral Neurological Assessment score nor Test of Infant Motor Performance score showed significant abnormalities. Under the guidance of gynecologists, attempts were made for the prolapsed vaginal wall by manual reduction. However, the vaginal wall rapidly returned to its prolapsed state upon the release of pressure. The vaginal wall prolapsed became pronounced when the twins cried. The vaginal wall could not autonomously return to its original position even though the twins calmed down.
In the absence of urinary obstruction, and given the lack of increasing abdominal distension or any apparent redness or swelling at the vaginal opening of the vulva, a conservative approach was chosen for treatment. This involved daily manual reduction and intensified nursing care, which included emphasizing local cleanliness and avoiding factors that might increase abdominal pressure. Additionally, considering the twins’ slow weight gain and concurrent extrauterine growth retardation, efforts were made to enhance their daily nutrition supply with the aim of promoting weight gain.
After their hospital discharge, regular outpatient follow-up was performed for the twins. In the case of the first-born twin, after a 5-month interval, her weight retrieved to 7.2 kg (>50th percentile), accompanied by a body length of 64 cm (>50th percentile) and a head circumference of 42 cm (>50th percentile). The prolapsed vaginal wall was completely retracted. Similarly, for the second-born twin, whose prolapse was more severe, at the 5th month follow-up after discharge, her weight was 5.3 kg (>3rd percentiles), accompanied by a length of 58.5 cm (>3rd percentiles) and a head circumference of 39.5 cm (>10th percentiles). At achieving weight pursuit, the prolapsed vaginal wall was also fully retracted.
Discussion
Genital prolapse is more common in elderly women or multipara, often due to pelvic floor muscle relaxation (5). However, this disorder is rare in neonates, and there is no report of genital prolapse in twins currently. NGP usually performs as a light red, soft tissue protrusion from the perineum, ranging from mild vaginal protrusion to a complete prolapse involving the cervix and uterus. In cases of vaginal wall prolapse, the prolapsed mass is usually circumferential. Furthermore, the external opening of the cervix can often be seen at the upper end of the prolapse mass with unaffected urethral opening (6, 7).
Approximately 80% cases of NGP are related to spinal cord malformations and lack of pelvic floor muscle strength. Subsequently, the etiological factors for genital prolapse have been categorized into two subgroups. The first subgroup are cases with abnormal neurological manifestations, such as spina bifida and meningomyelocele. Another etiological subgroup is cases with normal neuroanatomy, which have diverse causes like labor injuries during delivery or increased intra-abdominal pressure (4, 8–10). In cases of mild prolapse, some reports have shown that they were not accompanied with congenital neurological abnormalities (11, 12). Other reasons such as intrauterine malnutrition, long-term feeding intolerance, prolonged hormone therapy, fluid restriction, and elevated intra-abdominal pressure also have been indicated relevant to the happening of prolapse (4, 13).
For the treatment of neonatal genital prolapse, the most common used method is manual reduction, showing favorable outcomes for cases of mild prolapse and with no relapse during follow-up (11). However, there is a tendency for recurrence constantly after manual reduction in some cases, especially in infants with moderate prolapse. In such instances, utilizing Foley silicone catheters or hypertonic saline packs to provide rudimentary uterine support may help in preventing prolapse (7, 14, 15). Nonetheless, if the capacity of conservative therapy to sustain the original genital position is limited and it potentially impeded lower limb perfusion circulation (16), we should take other alternative interventions such as uterine suspension surgery, partial labial fusion surgery, and purse string suture to rectify the prolapse (16–18). However, some experts advocate that the more aggressive surgical approaches could be executed only when the conservative treatments fail or the persistent recurrent prolapse accompanied by changes of hypertrophy and ulceration in vaginal mucosal (14).
The twins described in this case report didn't have congenital nervous system abnormalities. Although both the them suffered the selective intrauterine growth restriction during their mother's pregnancy, it is noteworthy that the second-born twin, a smaller for gestational age preterm infant, experienced a more severer form of prolapse. Morever, the twins encountered similar issues such as abdominal distension, feeding intolerance and extrauterine growth retardation after birth. As we progressively enhanced their nutritional support and facilitated weight gain, favorable outcomes were observed in the resolution of vaginal prolapse.
Remarkably, this was the first time to report the case of genital prolapse in premature twins. We speculate that multifactors including intrauterine malnutrition, being smaller for gestational age, experiencing extrauterine growth retardation and confronting elevated abdominal pressure may collectively contribute to the onset of NGP. Importantly, with removal of these risk factors, the scenario of genital prolapse can spontaneously ameliorate.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding authors.
Ethics statement
Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
JG: Writing – original draft, Writing – review & editing, Data curation, Project administration. XC: Data curation, Writing – review & editing. SL: Writing – review & editing, Data curation. WC: Writing – review & editing. XZ: Writing – review & editing, Funding acquisition, Project administration, Resources, Writing – original draft.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article.
The Natural Science Fund of Guangdong Province (NO. 2022A1515010040)
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Jijo ZW, Betele MT, Ali AS. Congenital uterovaginal prolapse in a newborn. Case Rep Obstet Gynecol. (2018) 2018:1425953. doi: 10.1155/2018/1425953
2. Adekanmbi AF, Ogunlesi TA, Fetuga MB. Rectal and genital prolapse in Nigerian newborns: case reports and review of the literature. Niger J Clin Pract. (2014) 7(1):119–21. doi: 10.4103/1119-3077.122873
3. Aykanat A, Solakoğlu E, Bilginer B, Çelik HT, Yiğit Ş. Uterovaginal prolapse in a newborn with meningomyelocele: case report. J Pediatr Adolesc Gynecol. (2020) 33(5):607–9. doi: 10.1016/j.jpag.2020.04.001
4. McGlone L, Patole S. Neonatal genital prolase. J Paediatr Child Health. (2004) 40(3):156–57. doi: 10.1111/j.1440-1754.2004.00321.x
5. Schulten SFM, Claas-Quax MJ, Weemhoff M, van Eijndhoven HW, van Leijsen SA, Vergeldt TF, et al. Risk factors for primary pelvic organ prolapse and prolapse recurrence: an updated systematic review and meta-analysis. Am J Obstet Gynecol. (2022) 227(2):192–208. doi: 10.1016/j.ajog.2022.04.046
6. Borensztajn DM, Haasnoot K, Blok GJ, Beckers GM. A newborn with a genital prolapse. BMJ Case Rep. (2010) 2010:bcr0820103280. doi: 10.1136/bcr.08.2010.3280
7. Gunasagran Y, Wahab AVA. Case report: management of a rare case of neonatal uterovaginal prolapse using a vaginal plug. J Pediatr Adolesc Gynecol. (2022) 35(1):82–4. doi: 10.1016/j.jpag.2021.09.001
8. Henn EW, Juul L, van Rensburg K. Pelvic organ prolapse in the neonate: report of two cases and review of the literature. Int Urogynecol J. (2015) 26(4):613–5. doi: 10.1007/s00192-014-2539-y
9. Pirgon O, Atabek ME, Suleymanoglu S. Genital prolapsed in a newborn following resection of saccroccugeal teratoma. J Pediatr Adolesc Gynecol. (2009) 22(5):e96–8. doi: 10.1016/j.jpag.2008.11.004
10. Yıldızdaş HY, Ece Ü, Yurdakul GB, Kolağasıgil E. Spontaneously resolved uterine prolapse in a neonate with spina bifida. Turk J Pediatr. (2019) 61(6):979–81. doi: 10.24953/turkjped.2019.06.026
11. Zhiri H, Fatih B, Harou K, Aboulfalah A, Asmouki H, Soummani A. Neonatal genital prolapse: an exceptional entity (about a case). Pan Afr Med J. (2016) 25:153. doi: 10.11604/pamj.2016.25.153.9853
12. Oumarou H, Adamou H, Amadou M, Amadou Magagi I, Omid AA, Moustapha H, et al. Neonatal uterine prolapse. Arch Pediatr. (2016) 23(3):307–8. doi: 10.1016/j.arcped.2015.11.024
13. Vega-Rich C, Sherer DM. Neonatal vaginal prolapse. Gynecol Obstet Inves. (2001) 51(3):208–10. doi: 10.1159/000052926
14. Abdelsalam SE, Desouki NM, Abd alaal NA. Use of foley catheter for management of neonatal genital prolapse: case report and review of the literature. J Pediatr Surg. (2006) 41(2):449–52. doi: 10.1016/j.jpedsurg.2005.11.031
15. Ricardo Loret de Mola J, Carpenter SE. Management of genital prolapse in neonates and young women. Obstet Gynecol Surv. (1998) 51:253–60. doi: 10.1097/00006254-199604000-00022
16. Thaker H, Jayaratna IS, Nakhoda ZK. A stepwise treatment approach to neonatal genital prolapse. Pediatr Investig. (2018) 2(1):56–8. doi: 10.1002/ped4.12026
17. Banieghbal B, Fonseca J. Surgical management of uterine prolapse in an infant. Eur J Pediatr Surg. (1998) 8(2):119–20. doi: 10.1055/s-2008-1071137
Keywords: preterm infant, twin, neonatal genital prolapse, selective intrauterine growth restriction, growth retardation
Citation: Gu J, Chen X, Li S, Chen W and Zhong X (2024) Case Report: Neonatal genital prolapse in a pair of premature Twins. Front. Pediatr. 11:1294348. doi: 10.3389/fped.2023.1294348
Received: 14 September 2023; Accepted: 18 December 2023;
Published: 9 January 2024.
Edited by:
Victoria J. Kain, Griffith Health, Griffith University, AustraliaReviewed by:
Giulia Brisighelli, University of the Witwatersrand, South AfricaClecio Picarro, Federal University of Minas Gerais, Brazil
© 2024 Gu, Chen, Li, Chen and Zhong. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xinqi Zhong emhvbmd4cTIwMTZAZ3pobXUuZWR1LmNu Wenliang Chen ZmVicmlnaHRAMTI2LmNvbQ==
 Jian Gu
Jian Gu Xiaochun Chen1,2
Xiaochun Chen1,2 Wenliang Chen
Wenliang Chen