
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Pediatr. , 06 December 2023
Sec. Pediatric Urology
Volume 11 - 2023 | https://doi.org/10.3389/fped.2023.1278782
 Courtney A. Stewart1
Courtney A. Stewart1 Soo Jeong Kim2
Soo Jeong Kim2 Daniel Phillips1
Daniel Phillips1 Vinaya Bhatia3
Vinaya Bhatia3 Nicolette Janzen4
Nicolette Janzen4 Jonathan A. Gerber1*
Jonathan A. Gerber1*
Objective: To evaluate the practice patterns of pediatricians as they relate to common urologic concerns.
Materials and methods: An anonymous 15-question survey was created and distributed to all pediatricians at our institution, a large multisite care center. This study was deemed exempt by the institutional review board.
Results: 55 of the 122 (45%) providers queried responded. 93% of the participants were female, and 7.3% were male. 55% recommended testicular self-examination at adolescence, while 39% did not recommend at any age. 78% stated that they were “Fairly confident” in the exam for undescended testicle (UTD). One-third referred patients with UDT to a subspecialist upon recognition at birth, 13% at 3 months of age, and 28% at 6 months of age. 10% reported obtaining a VCUG after the first febrile urinary tract infection (UTI), 26% after the second, and 36% only if there were abnormal findings on renal ultrasound. 28% of providers reported that they refer to pediatric urology after the initial febrile UTI. 19% provided antibiotics for UTI symptoms alone with negative urinalysis and urine culture.
Conclusions: Despite established guidelines, practice patterns varied among pediatricians. Pediatricians typically followed the AAP's guidelines regarding VCUGs (62%), with only a few adhering to urologic recommendations (9%). Despite the consistency between AAP and AUA guidelines regarding the age at which to refer a patient for cryptorchidism, about 70% of practitioners referred patients too early or too late. Harmonized, consolidated guidelines between pediatricians and pediatric urologists would improve patient care and efficiency of the healthcare system.
Management of surgical conditions in children by board certified pediatric surgical specialists have been associated with improved outcomes (1–3). As such, the American Academy of Pediatrics (AAP) has created referral recommendations to assist general pediatricians in determining when, and to whom, to refer their patients for pediatric surgical specialty care (4). The AAP recommends referral to a pediatric urologist for a variety of urologic conditions including undescended testes, congenital hydroceles and hernias, hypospadias, solid malignancy of a genitourinary organ, and moderate or severe vesicoureteral reflux.
Despite these guidelines, the decision to refer a child to a pediatric urologist can be complex. From the pediatrician's perspective, potential barriers can include long wait times for appointments with pediatric surgical specialties and surgical subspecialists' nonparticipation in health insurance plans (5). To further complicate matters, the AAP guidelines can differ from specialty-specific guidelines regarding the same pathology. For instance, while the most recent AAP guidelines recommends against a routine voiding cystourethrogram (VCUG) after the first febrile urinary tract infection (UTI) unless other risk factors are present (6), the Section on Urology of the AAP expressed significant concern regarding this recommendation as it could delay the diagnosis of harmful urinary tract conditions (7).
In addition, inappropriate referrals can consume a significant amount of health-system resources. A recent retrospective review showed that 19% of pediatric surgery referrals are inappropriate, and that children traveled an average of 57.4 miles for an inappropriate referral with a pediatric surgeon, with the travel burden being even more pronounced in children who lived in rural communities (8).
In this study, we sought to better understand the practice patterns for common urologic conditions of general pediatricians in our large network of community based pediatricians, including referral to pediatric urologists, in order to identify potential areas for improvement.
An online survey was developed and distributed to all pediatricians at our institution. The questions targeted pediatrician practice patterns for common urologic conditions. Topics included the frequency of performance of genitourinary (GU) exams, referral patterns for undescended testicles (UDT), recommendation for testicular self-examination, work up for urinary tract infections (UTI) including additional imaging (i.e., VCUG), and antibiotic stewardship in common UTI scenarios (Table 1). There were 15 questions in the survey; each question was multiple choice and was independent of all other questions in the survey. All responses were anonymous. The survey took respondents approximately 2 min to complete.
Responses were analyzed quantitatively and evaluated for adherence to various existing guidelines (American Urological Association [AUA], American Academy of Pediatricians [AAP]).
As the survey was anonymous and confidential (no identifying information was collected with the survey), this study posed minimal risk to the participants and was exempt from a full Institutional Review Board committee review.
55 of the 122 providers queried responded for a response rate of 45.0%. 92.7% of the respondents completed the survey in its entirety. The largest cohort of those surveyed, 36.4%, had been practicing in pediatrics for over 20 years. 21.8% have practiced less than 5 years, 21.8% have been practicing 6–10 years, 14.5% have been practicing 11–15 years, and 4.5% have been in practice for 16–20 years. 81.8% of the participants were MD/DO trained, 12.7% were nurse practitioners (NPs), and 5.5% were physician assistants (PAs). 92.7% of the participants were female, and 7.3% were male. All survey questions and answers are outlined in Table 1.
52% of participating providers reported that they perform comprehensive GU exams at each female well-child visit. 40% percent reported stopping routine GU exams once the female reached adolescence. Two providers did not perform a GU exam unless the parents reported a concern, and two providers performed GU exam and if normal, would forego future exams. 75.5% of providers performed a comprehensive GU exam for male patients at all ages and every well child visit. 17% reported that they stopped performing GU exams for males at adolescence. Three providers would perform GU exam at the initial visit and forego future exams if normal for male patients. One provider only performed GU exam for male patients if the parents mentioned a problem.
Testicular self-examination was recommended by the majority of responding providers (61.1%), but the timing of the counseling varied: 55% of providers recommended commencing testicular self-examination at adolescence, ten percent once the patients demonstrated understanding, and one percent recommended testicular self exam at any age. 39% did not recommend testicular self-examination. In addition, providers varied in their teaching method for proper testicular exam. 27% verbally told patients how to perform exam, and 21% demonstrated to patients how to perform the exam. 5.8% gave patients literature to review, and 13.5% did not provide any specific training.
The majority of respondents, 78%, stated that they were “Fairly confident” in the exam for undescended testicles. 11% stated they were “completely confident”, while seven percent said they were “somewhat confident” and four percent said they were “slightly confident”. At the time of clinical suspicion for an undescended testicle, 45.5% of providers said they would refer and 42% said they would obtain an ultrasound. 13% of providers said they would repeat the exam in six months.
Roughly one-third of respondents referred a patient to pediatric urology or pediatric surgery for undescended testis at the time of recognition at birth. Additionally, 7.4% preferred to refer at 3 months of age and 28% at 6 months of age. 11% referred the patient for surgical consultation at 9 months and 24.1% referred at one year of age. No providers reported delaying referral until puberty.
After initial febrile UTI, 10% of respondents reported ordering a VCUG while 28% report that they would directly refer to pediatric urology for all further work up. The largest group of providers (36%) ordered a VCUG only if there were abnormal findings on renal ultrasound. 26.4% preferred to order a VCUG after a second febrile UTI.
In the setting of a negative urinalysis and urine culture, 19% of respondents stated they would provide antibiotics for UTI symptoms (e.g., dysuria, frequency, urgency, suprapubic discomfort) alone. The majority of providers (81.5%) stated that they would define positive microscopic urinalysis, positive culture, and symptoms (frequency, urgency, dysuria, SP pain, etc) as a UTI. 35% of providers stated that positive urine culture alone would be a UTI. 3.7% stated they would define smelly urine as a UTI and 3.7% stated they would define positive urine dipstick alone as a UTI. In patients with new onset UTI, 83% did assess patients for concurrent constipation.
This study highlighted notable discrepancies in practice patterns by pediatricians when managing urologic conditions. Starting with the GU physical exam, the majority (75.5%) of survey participants indicated that they perform one at every visit for male children regardless of age, which is less than a previous study that reviewed GU examination documentation in well-child visits where over 95% had a documented GU exam (Figure 1) (9). Interestingly, 17% indicated they stopped GU examinations for males at adolescence, which is consistent with the United States Preventive Services Task Force (USPSTF)'s recommendation against routine testicular examinations in asymptomatic adolescents and adults for the purposes of testicular cancer screening (10). A comprehensive GU exam, however, can also identify other pathologies that present later in childhood and require surgical intervention, such as testicular ascent. A retrospective review of patients who underwent late orchiopexies, defined as at 4 years of age or later, showed that the most common reasons for late intervention were ascending testis (45%), parental delay (22%), and late referral (20%) (11). As such, an annual GU exam is recommended by the AUA (12). In addition, although the survey questions were designed to capture broad practice patterns and did not address such subtleties, a pediatric patient with a history of cryptorchidism should be monitored closely for testicular cancer given their higher risk, regardless of age (12). Also of note, providers indicated different practice patterns for females, with 52% of providers performing GU exams for female patients at all ages and 40% of providers stopping at adolescence. This discrepancy may be due to need to monitor for complications such as ascending testes or testicular masses. It could also be due to the expectation that some young women may begin visits with gynecologists at puberty; the American College of Obstetricians and Gynecologists recommends an initial reproductive health visit with an OBGYN between the ages of 13 and 15 (13).
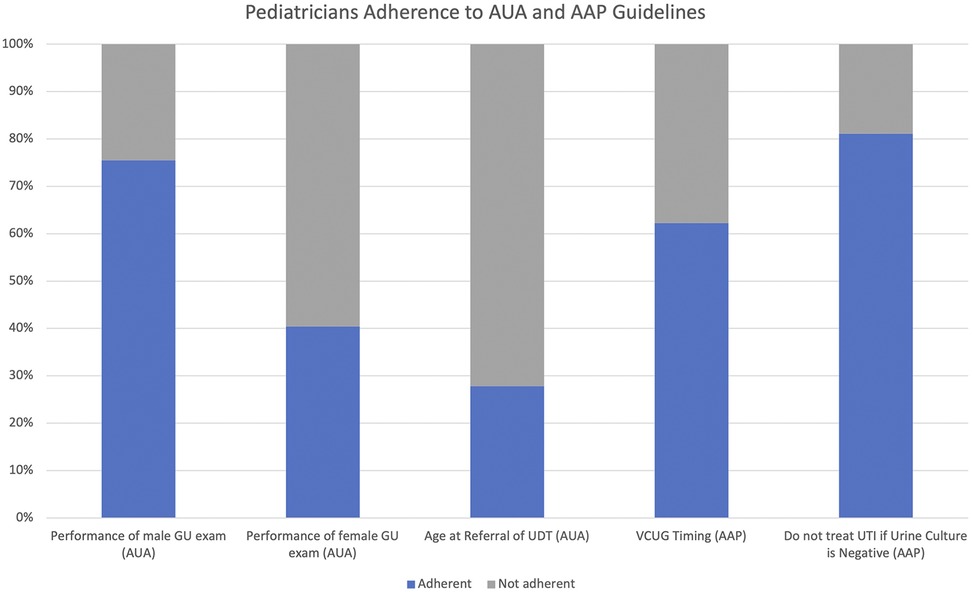
Figure 1. Pediatricians’ adherence to AUA and AAP guidelines. This figure represents the percentage of pediatricians who adhere to AUA and AAP guidelines. 75% of pediatricians adhered to AUA standards regarding the performance of GU exam. 40% of pediatricians adhered to AUA standards regarding performance of female GU exam. 28% of pediatricians adhered to AUA guidelines regarding the timing of referral for UDT. 62% of pediatricians adhered to the AAP guidelines regarding VCUG timing. 81% of pediatricians adhered to AAP guidelines regarding treating UTls with a negative urine culture.
Relatedly, approximately 60% of surveyed providers recommended testicular self-examination, with the majority (55%) having their patients initiate self-examinations beginning at adolescence. Additionally, there was great discrepancy regarding how to teach patients to perform testicular self-examination, with 27% verbally teaching and 22% demonstrating how to perform the exam. It is possible that the providers who ceased performing in-office GU examinations once patients reached adolescence were more reliant on the patients performing testicular self-examinations. This approach should be undertaken with caution; in one study from the Netherlands, it was shown that a mere 2% of teenagers routinely perform testicular self-examinations (14).
For pediatric patients with clinical suspicion for undescended testicle, 45.5% of providers stated they referred the patient to urology and 42% of providers obtained an ultrasound even though routine use of ultrasound has been specifically advised against by AUA guidance due to an estimated sensitivity and specificity of 45% and 78%, respectively (15). Furthermore, only 11% of pediatricians indicated that they were “completely confident” in their exam for undescended testicle and 78% indicated that they were “fairly confident.” Slightly lower confidence levels may lead to unnecessary referrals for UDT or in contrast, it may mean pediatricians miss an UDT on exam and fail to make the appropriate referral at six months. AUA guidelines recommend pediatric exams for undescended testicles until 6 months of age, at which time referral is required to evaluate if descent fails to occur (12).
For a pediatric patient with identified cryptorchidism, only 28% of providers referred patients to a specialist at 6 months of age, despite the similar AAP and AUA guidelines regarding timing of referral and surgical correction (Figure 1) (12, 16). Nearly a third of providers (30%) referred their patients to a surgical specialist for cryptorchidism immediately upon recognition at birth and 7.4% at 3 months of age despite previous studies showing that 35%–80% of newborn boys followed longitudinally have spontaneous descent of congenitally cryptorchid testes, usually prior to 3 months of age (15, 17, 18). In other words, almost half of the patients referred for UDT at birth could have received an unnecessary surgical subspecialist consult. On the other end of the spectrum, 11% of providers delayed referral until 9 months of age and 24% of providers delayed referral until 1 year of age which is inconsistent with known low rates of spontaneous testicular descent after 6 months of age. The AUA guidelines recommend surgical correction between 6 and 18 months of age; a delayed referral after 1 year of age, when accounting for time to schedule an evaluation with a pediatric urologist and then a surgery if necessary, could push the timing of surgical correction past this critical time frame.
The timing of obtaining a VCUG has historically been controversial and our study suggests that this continues to be an area of ongoing debate. 62% of pediatricians (36% obtained if abnormality seen in ultrasound and 26% obtained after second febrile UTI) followed the most recent guidelines put forth by the AAP, which recommends against a routine VCUG after the first febrile UTI unless abnormalities are present on the renal bladder ultrasound or there are other clinical reasons to suspect high-grade vesicoureteral reflux or obstructive uropathy (Figure 1) (6). Although the majority of pediatricians are following AAP guidelines in terms of timing of obtaining a VCUG, there is growing evidence that renal scarring may be missed by not obtaining VCUGs after the first UTI: Narchi et al. showed that following AAP guidelines would have missed 56% of children with VUR ≥ grade II, and all children with renal scarring would not have been imaged (19). In addition, when cross-sectional cohorts of patients in 2005 and 2015 were compared, patients presenting in 2015 for post-UTI VCUG had an increased likelihood of recurrent UTI and renal scarring (17). The AAP and EAU/ESPU guidelines recommend referral after first febrile UTI in part due to a study which evaluated severity of renal scarring after febrile UTIs (6, 20). The study illustrated 3% after the first UTI which then increased to 26% after the second, indicating a critical period between the first and second UTI (21). While VCUGs are an invasive imaging modality and can cause morbidity such as patient and parent distress, although perhaps less with pretest preparation and child life specialist involvement (22), future studies will be necessary to delineate risk factors for developing renal scarring in order to not improperly delay the diagnosis of symptomatic vesicoureteral reflux.
A small number (9%) of pediatricians did prefer to order a VCUG after the first febrile UTI, which is supported by the Section of Urology (7). Another interesting finding was approximately 28% of pediatricians referred patients to pediatric urology for evaluation following the first febrile UTI without further investigation, which could be an area for collaboration in order to reduce unnecessary referrals.
In regards to antibiotic use in a patient with symptoms suggestive of UTI/cystitis, the majority of providers (81%) stated that they would not prescribe antibiotics in the setting of a negative urinalysis and urine culture, which is in line with the AAP guidelines recommending both urinalysis results that suggest infection and the presence of at least 50,000 colony-forming units (CFU) per mL on a urine culture obtained in order to establish the diagnosis of UTI (Figure 1) (6). Nearly 19% of respondents stated that they would prescribe antibiotics in this clinical setting, however, which is concerning as antibiotic usage is not benign, particularly if not indicated: early exposure to antibiotics in childhood could have a negative effect on neurocognitive function, body metabolism, and increased resistance to common antimicrobial agents (23).
Although almost 82% of providers defined positive microscopic urinalysis, positive culture, and symptoms as a UTI, 35% also defined positive urine culture alone as a UTI. It is important to note that the goal of UTI therapy is renal preservation, and isolated bacteriuria without symptoms does not warrant treatment as asymptomatic bacteriuria is often self-resolving (24). Only 3% of providers defined smelly urine alone as a UTI, consistent with the current understanding that malodorous or cloudy urine has been shown to be an unreliable marker for UTI (25). In the absence of clear evidence-based protocols, it is likely that many patients are being overtreated with antibiotics.
The goal of this study was to establish broad practice and referral patterns of the general pediatricians in regards to management of urologic conditions. In order to maximize participation, the survey questions were not designed to portray the various nuances that could be present in a real-life clinical encounter, which is a limitation of this study. The providers were also asked to only select one answer choice that best represented their predominant practice preference, but they might have chosen other answers in different clinical scenarios. In addition, perhaps as a reflection of the online format (26), the overall participation rate by the pediatricians was low although in line with reported response rates for many surveys.
Pediatricians typically followed the AAP's guidelines regarding VCUGs (62%), with only a few adhering to urologic recommendations (9%). Despite the consistency between with AAP and AUA guidelines regarding the age at which to refer a patient for cryptorchidism, about 70% of practitioners referred patients too early or too late. Despite a lack of supportive guidelines, most providers did recommend testicular self-examination at some point. Most providers (81%) stated that they would not prescribe antibiotics in the setting of a negative urinalysis and culture.
Despite established guidelines, practice patterns varied greatly amongst pediatricians at our institution. Harmonized, consolidated guidelines between pediatricians and pediatric urologists would improve patient care and efficiency of the healthcare system.
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
CS: Data curation, Formal analysis, Investigation, Methodology, Project administration, Writing – original draft, Writing – review & editing. SJ: Conceptualization, Writing – original draft, Writing – review & editing. DP: Writing – review & editing. VB: Writing – review & editing. NJ: Writing – review & editing. JG: Writing – original draft, Writing – review & editing.
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
We are thankful to the pediatricians who participated in the survey that we administered.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Alexander F, Magnuson D, DiFiore J, Jirousek K, Secic M. Specialty versus generalist care of children with appendicitis: an outcome comparison. J Pediatr Surg. 2001;36(10):1510–3. doi: 10.1053/jpsu.2001.27033
2. Borenstein SH, To T, Wajja A, Langer JC. Effect of subspecialty training and volume on outcome after pediatric inguinal hernia repair. J Pediatr Surg. 2005;40(1):75–80. doi: 10.1016/j.jpedsurg.2004.09.002
3. Yohe N, Ciminero M, Solomito M, Lee MC. Impact of pediatric subspecialty training on perioperative complications in adolescent idiopathic scoliosis surgery. Orthopedics. 2020;43(5):e454–9. doi: 10.3928/01477447-20200721-11
4. Surgical Advisory Panel AAoP, Klein MD. Referral to pediatric surgical specialists. Pediatrics. 2014;133(2):350–6. doi: 10.1542/peds.2013-3820
5. Pletcher BA, Rimsza ME, Cull WL, Shipman SA, Shugerman RP, O'Connor KG. Primary care pediatricians’ satisfaction with subspecialty care, perceived supply, and barriers to care. J Pediatr. 2010;156(6):1011–1015 e1. doi: 10.1016/j.jpeds.2009.12.032
6. Subcommittee on Urinary Tract Infection SCoQI, Management, Roberts KB. Urinary tract infection: clinical practice guideline for the diagnosis and management of the initial UTI in febrile infants and children 2 to 24 months. Pediatrics. 2011;128(3):595–610. doi: 10.1542/peds.2011-1330
7. Wan J, Skoog SJ, Hulbert WC, Casale AJ, Greenfield SP, Cheng EY, et al. Section on urology response to new guidelines for the diagnosis and management of UTI. Pediatrics. 2012;129(4):e1051–3. doi: 10.1542/peds.2011-3615
8. Shinkunas LA, Klipowicz CJ, Carlisle EM. Inappropriate referrals in pediatric surgery. J Pediatr Surg. 2020;55(12):2596–601. doi: 10.1016/j.jpedsurg.2020.06.012
9. Gerber JA, Balasubramanian A, Jorgez CJ, Shukla MA, Jacob JS, Zhu H, et al. Do pediatricians routinely perform genitourinary examinations during well-child visits? A review from a large tertiary pediatric hospital. J Pediatr Urol. 2019;15(4):374 e1–e5. doi: 10.1016/j.jpurol.2019.05.007
10. U. S. Preventive Services Task Force. Screening for testicular cancer: U.S. preventive services task force reaffirmation recommendation statement. Ann Intern Med. 2011;154(7):483–6. doi: 10.7326/0003-4819-154-7-201104050-00006
11. Guven A, Kogan BA. Undescended testis in older boys: further evidence that ascending testes are common. J Pediatr Surg. 2008;43(9):1700–4. doi: 10.1016/j.jpedsurg.2008.03.029
12. Kolon TF, Herndon CD, Baker LA, Baskin LS, Baxter CG, Cheng EY, et al. Evaluation and treatment of cryptorchidism: AUA guideline. J Urol. 2014;192(2):337–45. doi: 10.1016/j.juro.2014.05.005
13. American College of Obstetricians and Gynecologists, Gynecologists’ Committee on Adolescent Health C. The initial reproductive health visit: ACOG committee opinion, number 811. Obstet Gynecol. 2020;136(4):e70–80. doi: 10.1097/AOG.0000000000004094
14. Lechner L, Oenema A, de NJ. Testicular self-examination (TSE) among Dutch young men aged 15-19: determinants of the intention to practice TSE. Health Educ Res. 2002;17(1):73–84. doi: 10.1093/her/17.1.73
15. Tasian GE, Copp HL, Baskin LS. Diagnostic imaging in cryptorchidism: utility, indications, and effectiveness. J Pediatr Surg. 2011;46(12):2406–13. doi: 10.1016/j.jpedsurg.2011.08.008
16. American Academy of Pediatrics. Timing of elective surgery on the genitalia of male children with particular reference to the risks, benefits, and psychological effects of surgery and anesthesia. Pediatrics. 1996;97(4):590–4. doi: 10.1542/peds.97.4.590
18. Hutson JM. Cryptorchidism and Hypospadias. In: Feingold KR, Anawalt B, Blackman MR, et al., editors. Endotext [Internet]. South Dartmouth, MA: MDText.com, Inc. 2000. Available from: https://www.ncbi.nlm.nih.gov/books/NBK279106/.
19. Narchi H, Marah M, Khan AA, Al-Amri A, Al-Shibli A. Renal tract abnormalities missed in a historical cohort of young children with UTI if the NICE and AAP imaging guidelines were applied. J Pediatr Urol. 2015;11(5):252 e1–7. doi: 10.1016/j.jpurol.2015.03.010
20. t Hoen LA, Bogaert G, Radmayr C, Dogan HS, Nijman RJM, Quaedackers J, et al. Update of the EAU/ESPU guidelines on urinary tract infections in children. J Pediatr Urol. 2021;17(2):200–7. doi: 10.1016/j.jpurol.2021.01.037
21. Shaikh N, Haralam MA, Kurs-Lasky M, Hoberman A. Association of renal scarring with number of febrile urinary tract infections in children. JAMA Pediatr. 2019;173(10):949–52. doi: 10.1001/jamapediatrics.2019.2504
22. Thacker PG, Collins HR, Hill J. Distress experienced during pediatric VCUGs—a granular, prospective assessment using the brief behavioral distress scale. Pediatr Radiol. 2016;46(5):660–5. doi: 10.1007/s00247-016-3540-z
23. Kutasy B, Coyle D, Fossum M. Urinary tract infection in children: management in the era of antibiotic resistance-A pediatric urologist’s view. Eur Urol Focus. 2017;3(2-3):207–11. doi: 10.1016/j.euf.2017.09.013
24. Dahiya A, Goldman RD. Management of asymptomatic bacteriuria in children. Can Fam Physician. 2018;64(11):821–4.30429177
25. Wyndaele JJ, Brauner A, Geerlings SE, Bela K, Peter T, Bjerklund-Johanson TE. Clean intermittent catheterization and urinary tract infection: review and guide for future research. BJU Int. 2012;110(11 Pt C):E910–7. doi: 10.1111/j.1464-410X.2012.11549.x
Keywords: pediatrician, vesicoureteral reflux, undescended testis, urinary tract infection, referral, practice pattern
Citation: Stewart CA, Jeong Kim S, Phillips D, Bhatia V, Janzen N and Gerber JA (2023) Urologic practice patterns of pediatricians: a survey from a large multisite pediatric care center. Front. Pediatr. 11:1278782. doi: 10.3389/fped.2023.1278782
Received: 16 August 2023; Accepted: 10 November 2023;
Published: 6 December 2023.
Edited by:
Sherry Ross, University of North Carolina at Chapel Hill, United StatesReviewed by:
Juan Ignacio Bortagaray, Royal Children's Hospital, Australia© 2023 Stewart, Jeong Kim, Phillips, Bhatia, Janzen and Gerber. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jonathan A. Gerber Sm9nZXJiZXJAdXRtYi5lZHU=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.