- 1Department of Pediatric Orthopedic, The Second Affiliated Hospital of Jiaxing University, Jiaxing, China
- 2Department of Radiation, The Second Affiliated Hospital of Jiaxing University, Jiaxing, China
Objectives: This review evaluates the safety and efficacy of submuscular plating (SMP) vs. elastic stable intramedullary nailing (ESIN) in the treatment of pediatric femur shaft fracture.
Method: Studies comparing the efficacy and safety of SMP and ESIN in pediatric shaft fracture were retrieved from five databases (PubMed, Embase, Cochrane, OVID, and Web of Science) from inception to March 2023 using a systematic literature search strategy. A total of 13 outcome measures, such as perioperative parameters, clinical outcomes, and radiographic results, were included in the meta-analysis.
Results: Eight eligible studies involving 491 patients were included in the narrative synthesis. There were no significant differences in baseline characteristics between the two groups. Meta-analysis showed reduced radiation time (RT), soft tissue irritation and angular deformation in the SMP group than in the ESIN group. However, the SMP group had greater estimated blood loss (EBL) than the ESIN group. The duration of surgery, length of hospital stay (LOS), implant removal, complications requiring surgery, Flynn score, incidence of infection, fracture healing time, and limb length discrepancy (LLD) were similar between the two groups. Only one study reported higher incidences of fracture nonunion or delayed healing in the ESIN group.
Conclusion: SMP is an effective and safe intervention superior to ESIN in reducing soft tissue irritation, angular deformation and radiation time. Given the presence of potential bias and heterogeneity, surgeons should select the treatment that would provide the best outcomes for EBL, LOS, operation time, and bone nonunion or delayed healing based on their experience.
Systematic Review Registration: https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42023404118, Identifier PROSPERO (CRD42021228512).
Introduction
Pediatric femoral fractures are the second most common diaphyseal fracture and the most common pediatric orthopedic injury requiring hospitalization (1), representing about 2% of all pediatric fractures (2). Despite the consensus on the surgical treatment for patients over five years old (3), the selection of fixation method in skeletally immature patients remains controversial (4, 5).
An optimal surgical strategy for pediatric femoral shaft fracture depends on the age and weight of the child, characteristics of the fracture, and accompanying damage (4). In addition, an effective fixation approach should provide adequate primary stability to permit early mobilization, even early weight bearing, maintain fracture biology, minimize scaring and tissue irritation, prevent blood transfusion and serious complications, as well as reduce operation time and radiation exposure (6). The main options for surgical fixation include external fixation, open or submuscular plating fixation, rigid intramedullary nailing, and ESIN (7). External fixation is frequently associated with complications, and open reduction and internal fixation have increased risks of blood transfusion and impaired blood supply to the fracture site. Furthermore, several studies have reported avascular necrosis in rigid intramedullary nailing (8–10). On the other hand, ESIN and SMP have become the most popular fixation approaches for pediatric femoral shaft fractures in recent years (11, 12). ESIN has always been the preferred method of fixation for length stable femoral shaft fracture (13), and has recently demonstrated positive clinical outcomes with low incidences of complications in unstable femoral shaft fracture (14). SMP is an alternative option for length-unstable femoral fractures due to minimal invasion and soft tissue irritation, reliable initial stability that allows for early range of motion (ROM), and satisfactory healing rate, which increased its applicability over ESIN (15, 16).
Both approaches have been recommended in guidelines, but high-level evidence on their efficacy and safety is lacking (3, 15). As a result, neither of these techniques is considered the gold standard, and the selection of either approach remains highly debated (17). A few meta-analyses have compared ESIN with other procedures (18, 19) but not with SMP. Therefore, this study was conducted to evaluate the clinical efficacy, radiology outcomes and safety of SMP vs. ESIN in treating pediatric femoral fractures.
Methods
Search strategy
This study was performed in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) 2020 statement (20) and was registered in PROSPERO (CRD42021228512). Studies comparing the efficacy and/or safety of SMP and ESIN in pediatric femoral shaft fracture and published in English were systematically searched in PubMed, Embase, The Cochrane Library, and Web of Science from inception to March 2023 using the following terms: “Femoral Fractures”, “Femoral Fracture”, “Fracture, Femoral”, “Fractures, Femoral”, “elastic stable intramedullary nailing”, “elastic stable intramedullary nails”, “elastic stable intramedullary nail”, “elastic nailing”, “elastic nail”, “elastic nails”, “Flexible Intramedullary Nail”, “Flexible Intramedullary Nails”, “flexible intramedullary nailing”, “flexible nails”, “flexible nail”, “flexible nailing”, “Submuscular plating”, “bridge plating”, and “Submuscular bridge plating”. The detailed search strategy is shown in Supplementary Text S1. The references of all eligible studies were also manually searched. All included studies were evaluated independently by two investigators, and any disagreement was resolved by consensus.
Eligibility criteria
The inclusion criteria were as follows: (1) Randomized-controlled trial (RCT), cohort study, or case-control study; (2) Conducted in skeletally immature children aged five years or older; (3) Study included closed or Gustilo I femoral shaft fractures without other injuries that require concomitant treatment; (4) At least one perioperative measure, including operation time, EBL, LOS, incidence of complication, and radiation expose time; (5) Sufficient data for calculating odds ratio (OR) or weighted mean difference (WMD).
The exclusion criteria were: (1) Reviews, letters, editorial comments, case reports, conference abstracts, adult studies, non-clinical studies, unpublished articles, and non-English articles; (2) Outcome measures cannot be extracted completely; (3) Fewer than 20 cases in two groups (SMP and ESIN); and (4) Patients on whom more than one internal fixation method has been applied.
Postoperative plaster assisted fixation was not excluded from our analysis since it is a routine procedure performed in pediatric fracture surgery and should not have an impact on the study results.
Data extraction
Data were extracted independently by two investigators, and any discrepancy was resolved by discussion with a third investigator. Extracted data included study characteristics (first author, publication year, study period, country of study, study type, number of cases), demographics (patient age, patient weight, gender, fracture stability), perioperative parameters (duration of surgery, EBL, RT and LOS), clinical outcomes (soft tissue irritation, implant removal, complications requiring surgery, Flynn score, and infections), and radiographic outcomes (fracture healing time, angular deformation, LLD, and fracture non-union or delayed healing). Continuous variables were expressed as mean ± standard deviation using a validated mathematical method (21, 22).
Quality assessment
Quality assessment was performed using the Cochrane Collaboration's risk of bias assessment (RoB) tool for RCTs and the Newcastle–Ottawa Scale (NOS) for retrospective and prospective cohort studies. Studies with a score of 7–9 were regarded as high-quality. Discrepancies in quality assessment results were resolved through discussion between the two independent investigators.
Statistical analysis
Evidence synthesis was completed using Review Manager 5.3 (Cochrane Collaboration, Oxford, UK). Continuous and categorical variables were compared between groups using WMD and OR with confidential intervals (CIs), respectively. Heterogeneity among studies was assessed by the chi-squared (χ2) test (Cochran's Q) and inconsistency index (I2) (23). When I2 > 50%, a random-effects model was used for data analysis; otherwise, a fixed-effects model was used. Furthermore, sensitivity analyses were performed for outcomes with significant heterogeneity to evaluate the effect of the included studies. Publication bias was evaluated using funnel plots in Review Manager 5.3 (Cochrane Collaboration, Oxford, UK).
Results
Literature search and study characteristics
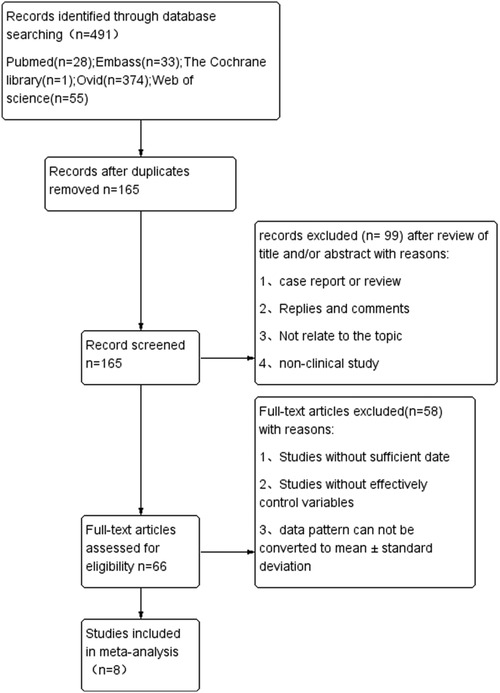
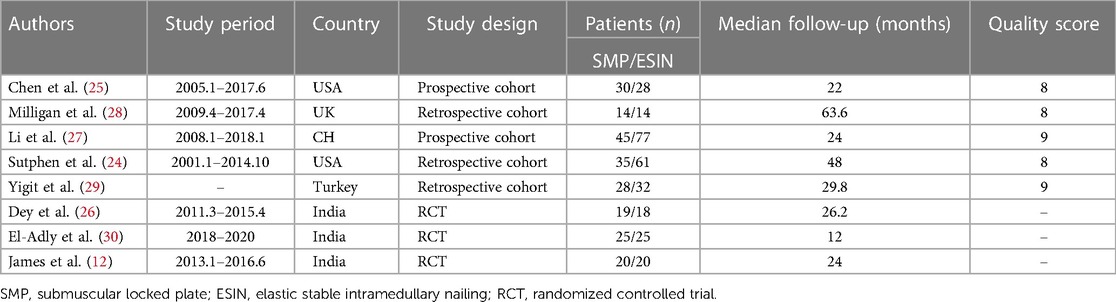
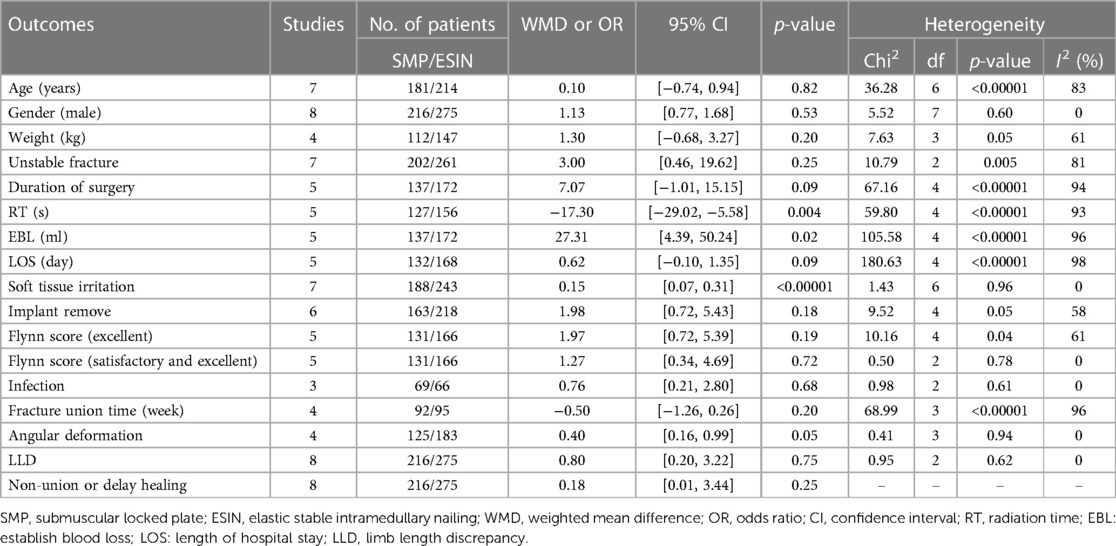
We initially identified 491 relevant publications from Pubmed (n = 28), Cochrane Library (n = 1), Embase (n = 33), OVID (n = 374), and Web of Science (n = 55). The study selection process is shown in Figure 1. After removing duplicates, the title and abstract of 165 articles were screened, and the full texts of 66 articles were assessed for eligibility. Finally, 8 studies involving 491 patients (216 in SMP group, 275 in ESIN group) were included in the meta-analysis (12, 24–30), including 2 prospective cohort studies (25, 27), 3 retrospective cohort studies (24, 28, 29), and 3 RCTs (12, 26, 30). The characteristics and quality scores of each included study are summarized in Table 1. All the included prospective and retrospective cohort studies were identified as high quality according to NOS (Supplementary Table S1). In addition, the RCTs were also of good quality with a low risk of bias according to the RoB assessment (Figure 2).
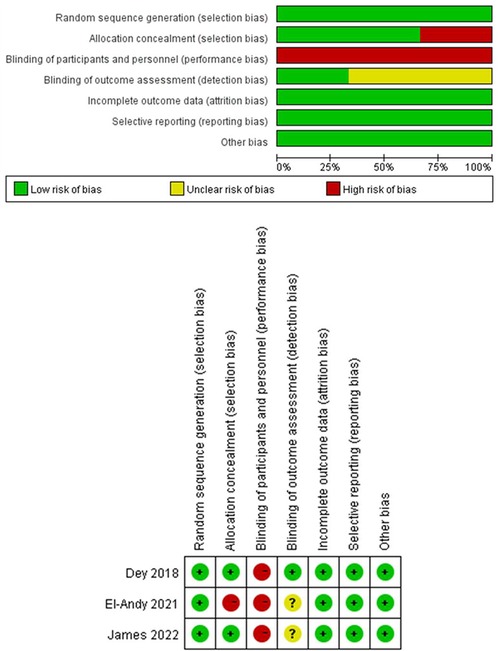
Figure 2. Publication bias in RCTs summary of the risk of bias across the 3 included RCTs; judgements regarding each risk of bias item for each included study.
Demographics
No significant differences were noted in patient age (WMD: −0.16; 95% CI: −0.73, 0.41; P = 0.58), gender (WMD: −0.16; 95% CI: −0.73, 0.41; P = 0.58), weight (WMD: −0.16; 95% CI: −0.73, 0.41; P = 0.58) and fracture stability (WMD: −0.16; 95% CI: −0.73, 0.41; P = 0.58) (Table 2).
Perioperative parameters
Duration of surgery
Duration of surgery was reported in 5 studies including 309 patients (137 in SMP and 172 in ESIN) (12, 26, 27, 29, 30). No significant difference was observed in the duration of surgery between the two groups [WMD: 7.07; 95% CI: (−1.01, 15.15); P = 0.09], but there was significant heterogeneity among the studies (I2 = 94%, P < 0.00001) (Figure 3A).

Figure 3. Forest plots of perioperative parameters: (A) duration of surgery; (B) radiological time; (C) estimated blood losing; (D) length of stay.
RT
Five studies involving 283 patients (127 in SMP and 156 in ESIN) reported radiation time (12, 24, 26, 29, 30). The pooled results showed that radiation time was significantly shorter in the SMP group than in the ESIN group [WMD, −17.3; 95% CI: (−29.02, −5.58); P = 0.004]. There was significant heterogeneity among the studies (I2 = 93%, P < 0.00001) (Figure 3B).
EBL
Five studies (12, 26, 27, 29, 30) reported EBL. The meta-analysis showed significantly greater EBL in SMP than in ESIN [WMD = 27.31, 95% CI: (4.39, 50.24), P = 0.02], with significant heterogeneity among the studies (I2 = 96%, P < 0.00001) (Figure 3C).
LOS
Five studies (n = 300) discussed LOS (132 in SMP and 168 in ESIN) (12, 27–30). Meta-analysis showed similar LOS between the two groups [WMD: 0.62; 95% CI: (−0.1, 0.35); P = 0.09], with significant heterogeneity among studies (I2 = 98%, P < 0.0001) (Figure 3D). Furthermore, funnel plots revealed a slight publication bias in all of the above four perioperative parameters (Figures 4A–D).
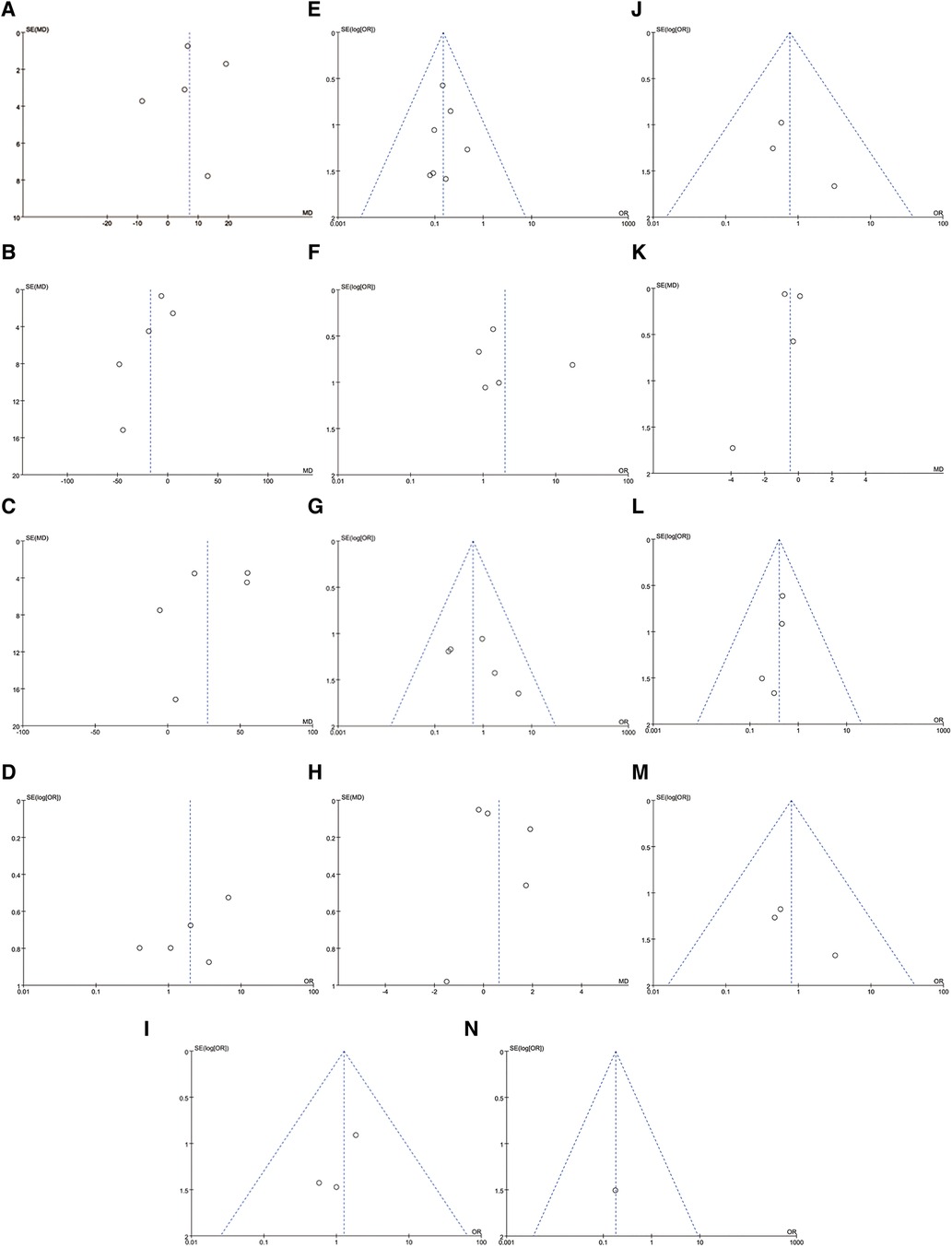
Figure 4. Funnel plots: (A) duration of surgery; (B) radiological time; (C) estimated blood losing; (D) length of stay; (E) soft tissue irritation; (F) implant remove; (G) comlication need to surgery; (H) flynn score(excellent and satisfactory); (I) flynn score(excellent); (J) infection; (K) fracture union time; (L) angular deformation; (M) limb length discrepancy; (N) non-union or delay union.
Clinical outcomes
Soft tissue irritation
Five studies reported soft tissue irritation, encompassing 431 patients (188 in SMP and 243 in ESIN) (12, 24–28, 30). The analysis results indicated significantly lower soft tissue irritation in the SMP group than in the ESIN group [OR: 0.15; 95% CI: (0.01, 0.37), P < 0.0001], with no significant heterogeneity among the studies (I2 = 0%, P = 0.96) (Figure 5A).
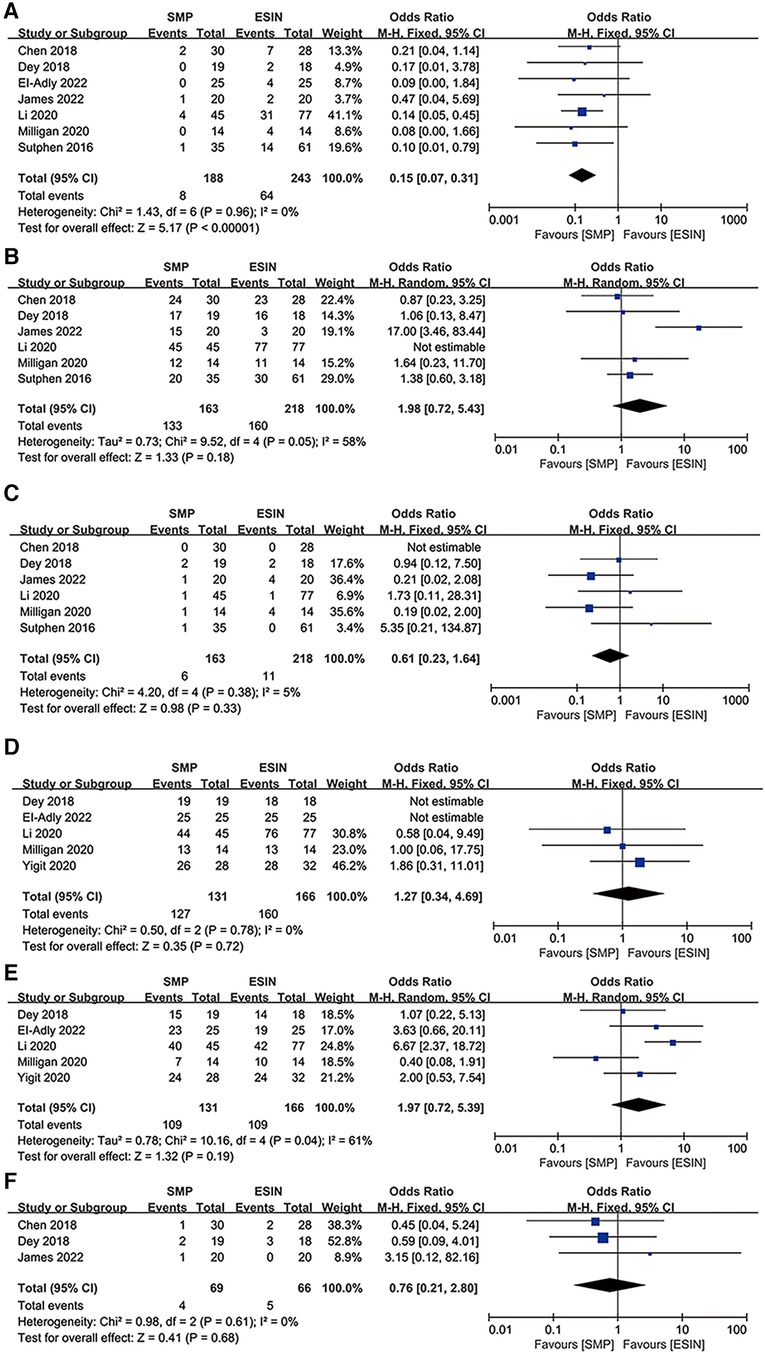
Figure 5. Forest plots of clinical outcomes: (A) soft tissue irritation; (B) implant remove; (C) comlication need to surgery; (D) flynn score(excellent and satisfactry); (E) flynn score(excellent); (F) infection.
Implant removal
Implant removal was reported in six studies with a total of 381 patients (12, 24–28), of whom 296 decided to remove their internal fixation devices (44.93% in SMP and 55.07% in ESIN). No significant difference was found in implant removal [OR: 1.98; 95% CI: (0.72, 5.43), P = 0.18]. However, there was moderate heterogeneity (I2 = 58%, P = 0.18) (Figure 5B) and slight publication bias in the studies (Figure 4F).
Complications requiring surgery
Although all 8 studies reported postoperative complications, meta-analysis was performed on only 5 studies, involving 17 cases (6 SMP vs. 11 ESIN) of complication in 323 patients (12, 24, 26–28). There was no significant difference in the incidences of complications requiring surgery between the two groups [OR: 0.61; 95% CI: (0.23, 1.64), P = 0.33] and no significant heterogeneity among the studies (I2 = 5%, P = 0.38) (Figure 5C). Reasons for secondary surgery were re-fracture, loss of reduction, deep infection, delayed union or non-union, and excessive deformity.
Flynn score
Flynn scores are rarely or poorly reported in most studies, and thus we performed subgroup analyses according to that patients have an Excellent or Satisfactory result or have an Excellent result only. We then further compared the clinical efficacy of the two interventions.
Flynn scores for child femoral shaft frame were pooled from 5 studies (26–30) involving 297 subjects (131 in SMP and 166 in ESIN). Neither the Excellent/Satisfactory [OR: 1.27; 95% CI: (0.34, 4.69), P = 0.72] nor Excellent subgroups [OR: 1.97; 95% CI: (0.72, 5.39), P = 0.19] showed a significant difference in the number of patients between the two interventions. There was significant heterogeneity in the latter subgroup (I2 = 61%, P = 0.04) (Figure 5E) but not in the former subgroup (I2 = 0%, P = 0.78) (Figure 5D). The funnel plot revealed a slight publication bias in Flynn score in the Excellent subgroup but not in the Excellent/Satisfactory subgroup.
Infections
Infections were reported in three studies (12, 25, 26), with an overall incidence of less than 7%. Infections were reported in 3 patients by Chen et al. (SMP: 1/30; ESIN: 2/28), 5 patients by Dey et al. (SMP: 2/19; ESIN: 3/18), and 1 patient by James et al. (SMP: 1/20). There was no significant difference in the incidence of infection between the two groups [OR: 0.76; 95% CI: (0.21, 2.80), P = 0.68], and there was no significant heterogeneity in the results (I2 = 0%, P = 0.61) (Figure 5F).
Radiographic results
Fracture healing time
Four studies involving 187 patients (92 in SMP and 95 in ESIN) reported fracture healing time (12, 26, 29, 30), which was defined as the first observation of cortical continuity in more than 3 directions on the anteroposterior lateral x-ray. Meta-analysis indicated no significant difference in fracture healing time between the two groups [OR: −0.5; 95% CI: (−1.26, 0.26), P = 0.20]. However, there was significant heterogeneity (I2 = 96%; P < 0.00001) (Figure 6A) and publication bias (Figure 4K).
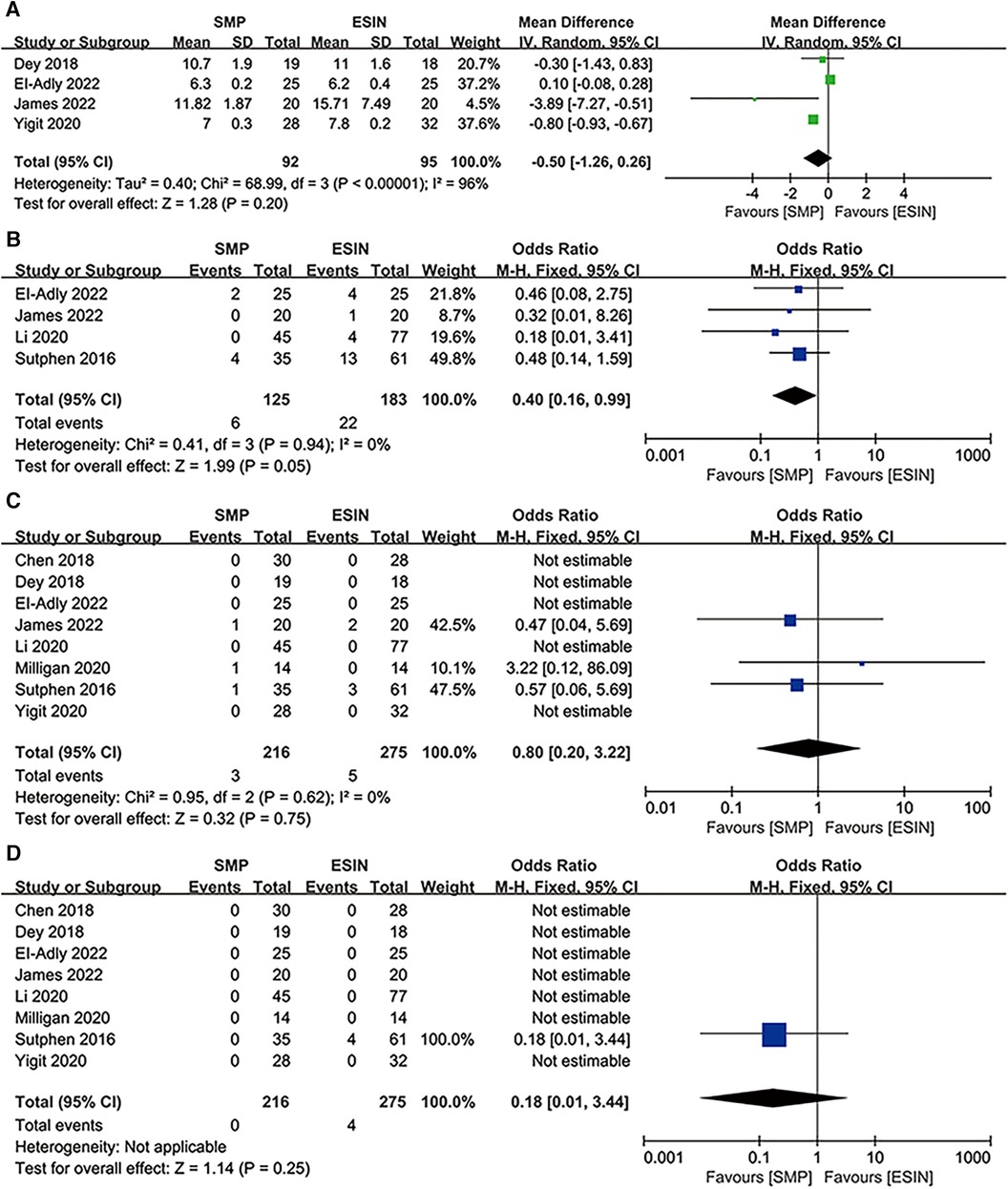
Figure 6. Forest plots of radiographic results: (A) fracture union time; (B) angular deformation; (C) limb length discrepancy; (D) non-union or delay union.
Angular deformation
Four studies involving 308 patients (125 in SMP and 183 in ESIN) (12, 24, 27, 30) discussed angular deformation. The results revealed that the SMP group had a significantly lower angular deformation rate than the ESIN group [OR: 0.4; 95% CI: (0.16, 0.99); P = 0.05] (Figure 6B), with no significant heterogeneity (I2 = 0%, P = 0.94) (Figure 4L).
LLD
The incidence of complication was reported in 8 studies with 491 patients (216 in SMP and 275 in ESIN) (12, 24–30). Meta-analysis indicated no significant difference in the incidence of complication between the two groups [OR: 0.8; 95% CI: (0.20, 3.22); P = 0.75] (Figure 6C), with no heterogeneity (I2 = 0%, P = 0.75) (Figure 4M).
Nonunion or delayed healing
Only Sutphen et al. reported 4 cases of nonunion or delayed healing, all of which were observed in the ESIN group (Figure 6D).
Sensitive analysis
To evaluate the influence of each individual study on the pooled WMD, we performed one-way sensitivity analyses on duration of surgery, RT, EBL, LOS, and fracture healing time (Figure 7). The pooled WMD for RT and fracture healing time remained unchanged after excluding each individual study. However, with the presence of heterogeneity for LOS and duration of surgery after the exclusion of Dey et al. for the former and Milligan et al. for the latter, the statistical significance of the results has changed [LOS: P = 0.009, WMD: 10.92, 95% CI: (0.07, 1.59); Duration of surgery: P = 0.009, WMD = 10.92, 95% CI: (2.71, 19.12)]. The heterogeneity in EBL also decreased (I2 = 77%, P = 0.45) when the two studies (27, 30) were excluded, and the significant difference in EBL disappeared [WMD: 7.16, 95% CI: (−11.50, 25.81), P = 0.45]. Collectively, these results indicate that the above studies were the primary sources of heterogeneity for these parameters.
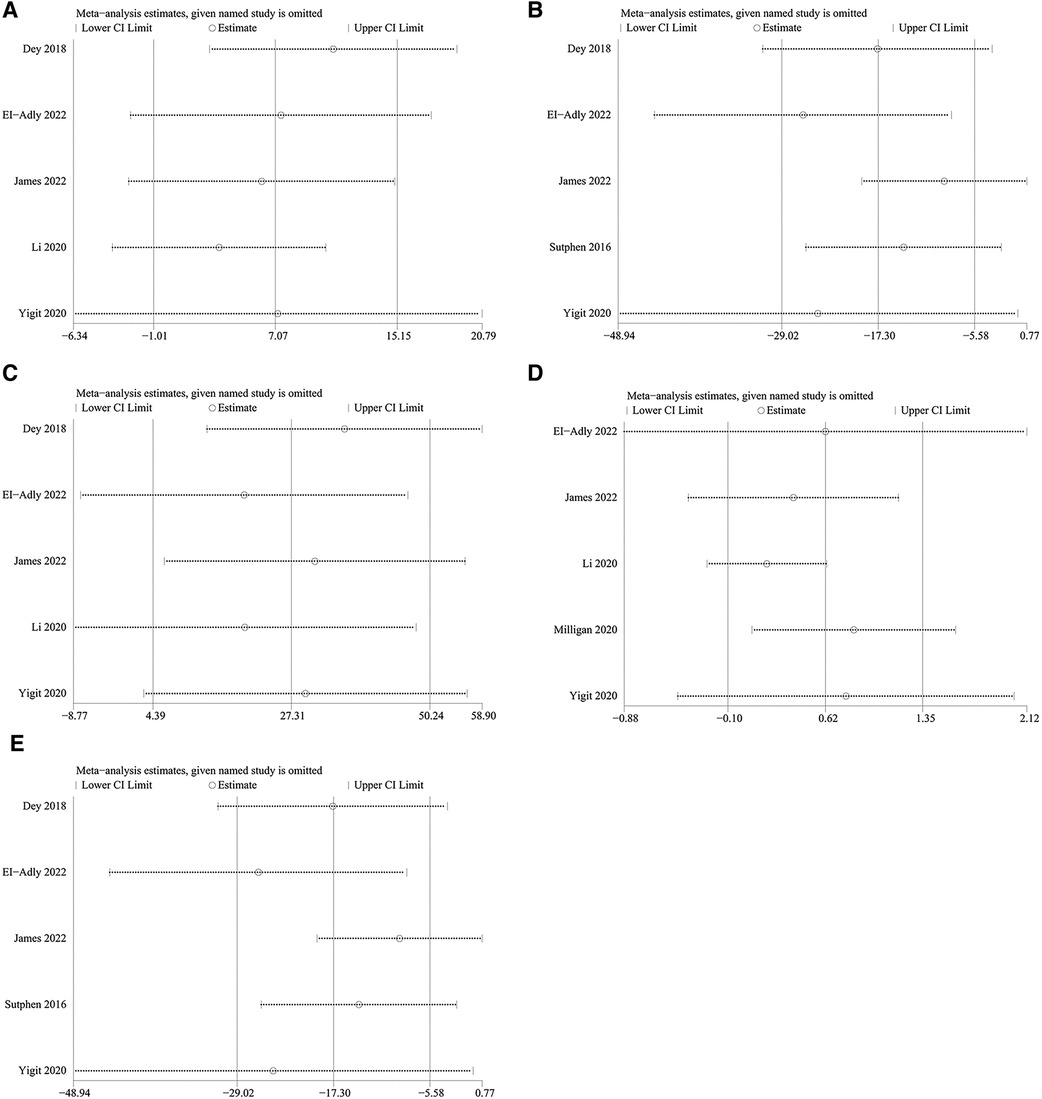
Figure 7. Sensitively analysis of: (A) duration of surgery; (B) radiological time; (C) estimated blood losing; (D) length of stay; (E) fracture union time.
Discussion
Children over the age of 5 with femoral shaft fractures have been previously shown to benefit from surgical treatment (31). However, there is currently no clear consensus on the optimal method of fixation. Commonly used fixation approaches include external fixation, rigid antegrade intramedullary nailing, common plate, SMP and ESIN. Among them, ESIN and SMP are the most widely used approaches recommended by guidelines (15). However, given potential adverse events, further research into the best treatment is warranted.
In this meta-analysis, we extracted 13 parameters from the eligible studies. Four parameters were significantly different between the two groups, while eight parameters were not. Bone nonunion or delayed healing was only reported by one study, and both occurred in the ESIN group. For perioperative parameters, the radiation exposure time was shorter in the SMP group than in the ESIN group, possibly because multiple fluoroscopies are required during ESIN fixation to achieve a more precise reduction. Studies have (32, 33) hinted that surgeons should consider the potential damages of this procedure when planning the surgical strategy. In addition, we found that the SMP group had significantly greater EBL than the ESIN group. Though, the additional bleeding in the children did not cause shock or require blood transfusions. Therefore, EBL does not have a major influence on the selection of interventions.
The ESIN group had a higher incidence of soft tissue irritation than the SMP group. These irritation symptoms partially led to early removal of internal fixation devices, wound complications, and decreased patient satisfaction. Other studies reported an equally high incidence of soft tissue irritation in ESIN (34, 35). Moreover, the ESIN group exhibited higher degrees of angularity during follow-up. It was reported that the weight of patients may influence the incidence of angular deformities after ESIN (36, 37). Therefore, the child's weight should be taken into account during ESIN. In unstable fractures, ESIN was found to be inadequate for controlling rotations whereas SMP provided good stability (38, 39). These evidence indirectly supports the reliability of this conclusion.
ESIN is associated with several surgical complications, including angular deformities, soft tissue irritation, and LLD (40), which are more common in length-unstable femoral fractures and fractures that involve the proximal or distal third of the femur (13). As a result, many researchers have shifted to SMP for pediatric femoral shaft fractures and achieved positive outcomes in children with length unstable fractures or greater body weight or fractures involving one-third of the distal and proximal ends. Nonetheless, no meta-analysis of the efficacy and safety of SMP and ESIN was conducted before. Here, we pooled the data from 8 studies published before 2023 and found that SMP results in a lower incidence of angular deformities. Body weight, fracture stability, and the thickness of ESIN may impact the results. Across the four studies reporting angular deformation, no statistical differences were found in baseline fracture stability [OR: 1.67; 95% CI: (0.08, 36.53); P = 0.74] between SMP and ESIN groups. Our results possibly indicate that SMP can provide more fixation stability. Conversely, the four study does not report the thickness of ESIN and only two of them provided body weight, so we cannot ignore the impact of ESIN thickness and body weight on the incidence of angular deformity. Due to their low incidence rates, delayed fracture healing and nonunion were reported in only one study, and all cases were observed in the ESIN group.
There were no significant differences in the incidences of postoperative infections, patient satisfaction, and postoperative complications requiring surgery between the two groups. While SMP involves a larger incision and hence greater soft tissue damage than ESIN, there was no increased risks of soft tissue complications such as exudation, infection, and wound dehiscence. Although the ESIN group has a higher incidence of angular deformities, our meta-analysis did not indicate a higher risk of LLD, which is contrary to the results of some case-control studies (34, 40, 41). In addition, while ESIN was associated with longer radiation exposure time, it did not affect fracture healing time, which may be attributed to the presence of both closed reduction and elastic fixation. Notably, the pooled results for both parameters were highly heterogeneous, and sensitivity analysis did not identify the source of heterogeneity. Hence, these findings should be interpreted with caution. The removal of studies did not abrogate the heterogeneity in LOS and surgical time but altered the statistical significance of the differences between the two groups. The new WMD indicated that SMP results in longer surgical time and LOS than ESIN. Furthermore, sensitivity analysis reduced the heterogeneity in EBL and abrogated the statistical significance between the two groups. We speculate that the stability of the results may be influenced by two studies (27, 30), and EBL is associated with the surgical skills and experience of the surgeon.
However, there are still several limitations to our study. First, the number of included studies was small and not all of them were RCTs. Due to the lack of high-quality research in this area, further RCTs are warranted to provide more reliable clinical results. Second, there is still high heterogeneity in LOS, surgical time, RT, and fracture healing time. Although we have conducted sensitivity analysis, the sources of heterogeneity could not be eliminated. Therefore, these results should be interpreted with caution. Furthermore, due to limited studies, effective conclusions cannot be drawn on the incidence of bone nonunion and delayed healing. Last, the removal of internal fixation devices was recommended in both groups, which may affect the reliability of the results. The operation time for their removal and postoperative complications are meaningful research topics, but due to insufficient data from the literature, these parameters could not be examined in this study.
Conclusion
SMP is an effective and safe intervention superior to ESIN in reducing soft tissue irritation, angular deformation, and radiation time. However, Flynn score, incidence of infection, fracture healing time, and LLD are similar between the two approaches. Given the presence of potential bias and heterogeneity, surgeons should select the treatment that would provide the best outcomes for EBL, LOS, operation time, and bone nonunion or delayed healing based on their experience.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Author contributions
DL: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Writing – original draft, Writing – review & editing. XW: Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. JL: Investigation, Methodology, Project administration, Resources, Writing – original draft, Writing – review & editing. MX: Conceptualization, Formal analysis, Supervision, Visualization, Writing – original draft, Writing – review & editing.
Funding
The authors declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fped.2023.1256630/full#supplementary-material
References
1. Loder RT, O'Donnell PW, Feinberg JR. Epidemiology and mechanisms of femur fractures in children. J Pediatr Orthop. (2006) 26(5):561–6. doi: 10.1097/01.bpo.0000230335.19029.ab
2. Sahlin Y. Occurrence of fractures in a defined population: a 1-year study. Injury. (1990) 21(3):158–60. doi: 10.1016/0020-1383(90)90085-9
3. Kocher MS, Sink EL, Blasier RD, Luhmann SJ, Mehlman CT, Scher DM, et al. American Academy of orthopaedic surgeons clinical practice guideline on treatment of pediatric diaphyseal femur fracture. J Bone Joint Surg Am. (2010) 92(8):1790–2. doi: 10.2106/JBJS.J.00137
4. Khoriati AA, Jones C, Gelfer Y, Trompeter A. The management of paediatric diaphyseal femoral fractures: a modern approach. Strategies Trauma Limb Reconstr. (2016) 11(2):87–97. doi: 10.1007/s11751-016-0258-2
5. Heideken J, Svensson T, Blomqvist P, Haglund-Akerlind Y, Janarv PM. Incidence and trends in femur shaft fractures in Swedish children between 1987 and 2005. J Pediatr Orthop. (2011) 31(5):512–9. doi: 10.1097/BPO.0b013e31821f9027
6. Park K-C, Oh C-W, Byun Y-S, Oh J-K, Lee H-J, Park K-H, et al. Intramedullary nailing versus submuscular plating in adolescent femoral fracture. Injury. (2012) 43(6):870–5. doi: 10.1016/j.injury.2011.10.032
7. Jain A, Aggarwal A, Gulati D, Singh MP. Controversies in orthopaedic trauma–management of fractures of shaft of femur in children between 6 and 12 years of age. Kathmandu Univ Med J (KUMJ). (2014) 12(45):77. doi: 10.3126/kumj.v12i1.13647
8. Flynn JM, Sarwark JF, Water PM, Bae DS, Lemke LP. The operative management of pediatric fractures of the upper extremity. J Bone Joint Surg Am. (2002) 84(12):2288–300. doi: 10.2106/00004623-200212000-00025
9. Keeler KA, Dart B, Luhmann SJ, Schoenecker PL, Ortman MR, Dobbs MB, et al. Antegrade intramedullary nailing of pediatric femoral fractures using an interlocking pediatric femoral nail and a lateral trochanteric entry point. J Pediatr Orthop. (2009) 29(4):345. doi: 10.1097/BPO.0b013e3181a53b59
10. Ramseier LE, Janicki JA, Weir S, Narayanan UG. Femoral fractures in adolescents: a comparison of four methods of fixation. J Bone Joint Surg Am. (2010) 92(5):1122–9. doi: 10.2106/JBJS.H.01735
11. Garner MR, Bhat SB, Khujanazarov I, Flynn JM, Spiegel D. Fixation of length-stable femoral shaft fractures in heavier children: flexible nails vs rigid locked nails. J Pediatr Orthop. (2011) 31(1):11. doi: 10.1097/BPO.0b013e31820321ab
12. James D, Martin D, Kumar A, Krishnan S, Gahukamble A, Madhuri V, et al. Elastic stable intramedullary nailing versus submuscular plating in pediatric diaphyseal femur fractures: a randomized controlled trial among children in south India. J Pediatr Orthop B. (2022) 31(2):e122–9. doi: 10.1097/BPB.0000000000000933
13. Sink EL, Faro F, Polousky J, Flynn K, Gralla J. Decreased complications of pediatric femur fractures with a change in management. J Pediatr Orthop. (2010) 30(7):633–7. doi: 10.1097/BPO.0b013e3181efb89d
14. Siddiqui AA, Abousamra O, Compton E, Meisel E, Illingworth KD. Titanium elastic nails are a safe and effective treatment for length unstable pediatric femur fractures. J Pediatr Orthop. (2020) 40(7):e560–5. doi: 10.1097/BPO.0000000000001474
15. Jevsevar DS, Shea KG, Murray JN, Sevarino KS. AAOS Clinical practice guideline on the treatment of pediatric diaphyseal femur fractures. J Am Acad Orthop Sur. (2015) 23(12):e101. doi: 10.5435/JAAOS-D-15-00523
16. Luo Y, Wang L, Zhao LH, Wang YC, Chen MJ, Wang S, et al. Elastic stable titanium flexible intramedullary nails versus plates in treating low grade comminuted femur shaft fractures in children. Orthop Surg. (2019) 11(4):664–70. doi: 10.1111/os.12514
17. Sanders JO, Browne RH, Mooney JF, Raney EM, Horn BD, Anderson DJ, et al. Treatment of femoral fractures in children by pediatric orthopedists: results of a 1998 survey. J Pediatr Orthop. (2001) 4:21. doi: 10.1097/01241398-200107000-00004
18. Guo YC, Feng GM, Xing GW, Yin JN, Xia B, Dong YZ, et al. A meta-analysis of flexible intramedullary nailing versus external fixation for pediatric femoral shaft fractures. J Pediatr Orthop B. (2016) 25(5):466–70. doi: 10.1097/BPB.0000000000000336
19. Imam MA, Negida AS, Elgebaly A, Hussain AS, Ernstbrunner L, Javed S, et al. Titanium elastic nails versus Spica cast in pediatric femoral shaft fractures: a systematic review and meta-analysis of 1,012 patients. Arch Bone Jt Surg. (2018) 6(3):176–88. PMID: 29911134.29911134
20. Page MJ, Mckenzie JE, Bossuyt PM, Boutron I, Moher D. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Syst Rev. (2021) 10(1):89. doi: 10.1186/s13643-021-01626-4
21. Luo D, Wan X, Liu J, Tong T. Optimally estimating the sample mean from the sample size, median, mid-range and/or mid-quartile range. Stat Methods Med Res. (2018) 27(6):1785–805. doi: 10.1177/0962280216669183
22. Wan X, Wang W, Liu J, Tong T. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol. (2014) 14:135. doi: 10.1186/1471-2288-14-135
23. Higgins J, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. (2002) 21(11):1539–58. doi: 10.1002/sim.1186
24. Sutphen SA, Mendoza JD, Mundy AC, Yang JG, Beebe AC, Samora WP, et al. Pediatric diaphyseal femur fractures: submuscular plating compared with intramedullary nailing. Orthopedics. (2016) 39(6):353–8. doi: 10.3928/01477447-20160719-03
25. Chen LK, Sullivan BT, Sponseller PD. Submuscular plates versus flexible nails in preadolescent diaphyseal femur fractures. J Child Orthop. (2018) 12(5):488–92. doi: 10.1302/1863-2548.12.180036
26. Dey S, Mishra K, Nagda TV, Dhamele J, Rathod C, Dey D. Titanium elastic nailing with temporary external fixator versus bridge plating in comminuted pediatric femoral shaft fractures: a comparative study. Indian J Orthop. (2018) 52(5):507–12. doi: 10.4103/ortho.IJOrtho_304_17
27. Li J, Rai S, Ze R, Tang X, Liu R, Hong P. The optimal choice for length unstable femoral shaft fracture in school-aged children: a comparative study of elastic stable intramedullary nail and submuscular plate. Medicine (Baltimore). (2020) 99(25):e20796. doi: 10.1097/MD.0000000000020796
28. Milligan D, Henderson L, Tucker A, Ballard J. Elastic nail fixation versus plate fixation of paediatric femoral fractures in school age patients—a retrospective observational study. J Orthop. (2020) 19:153–7. doi: 10.1016/j.jor.2019.11.033
29. Yigit S, Yıldırım A. The surgery outcomes of pediatric femoral shaft fractures and comparision of radiation risks. Acta Biomed. (2020) 91(2):326–31. doi: 10.23750/abm.v91i2.8709
30. El-Adly W, El-Gafary K, Khashaba M, Abubeih H. Flexible intramedullary nail versus submuscular locked plate with the cluster technique in pediatric femoral shaft fractures fixation. Indian J Orthop. (2022) 56(4):580–6. doi: 10.1007/s43465-021-00571-7
31. Madhuri V, Dutt V, Gahukamble AD, Tharyan P. Interventions for treating femoral shaft fractures in children and adolescents. Cochrane Database Syst Rev. (2014) (7):CD009076. doi: 10.1002/14651858.CD009076.pub2
32. Kleinerman RA. Cancer risks following diagnostic and therapeutic radiation exposure in children. Pediatr Radiol. (2006) 36(S2):121–5. doi: 10.1007/s00247-006-0191-5
33. Brenner DJ, Hall EJ. Computed tomography—an increasing source of radiation exposure. N Engl J Med. (2007) 357(22):2277–84. doi: 10.1056/NEJMra072149
34. Narayanan UG, Hyman JE, Wainwright AM, Rang M, Alman BA. Complications of elastic stable intramedullary nail fixation of pediatric femoral fractures, and how to avoid them. J Pediatr Orthop. (2004) 24(4):363. doi: 10.1097/01241398-200407000-00004
35. Kalbitz M, Fischer A, Weber B, Mayer B, Lackner I, Pressmar J. Diaphyseal femur fractures in children and adolescents-opportunities and limitations of the ESIN technique. J Clin Med. (2022) 11(24):7345. doi: 10.3390/jcm11247345
36. Madhuri V, Gahukamble A. Cochrane in context: interventions for treating femoral shaft fractures in children and adolescents. Evid Based Child Health. (2015) 9(4):827–8. doi: 10.1002/ebch.1983
37. Kayaokay K, Aktuglu K. Titanium elastic nailing in pediatric femoral diaphyseal fractures in the age group of 6–15 years mid-term and long-term outcomes. Pak J Med Sci. (2018) 34(6):1529–33. doi: 10.12669/pjms.346.16297
38. Elsayed MM, Farag HE, Zied M, Gomaa AR. Submuscular bridge plating in length-unstable pediatric femur fractures. Benha J Appl Sci. (2020) 5(6):1–6. doi: 10.21608/BJAS.2020.137138
39. Kanlic E. Advatages of submuscular bridge plating for complex pediatric femur fractures. Clin Orthop Relat Res. (2004) 426:244–51. doi: 10.1097/01.blo.0000138961.34810.af
40. Sink EL, Gralla J, Repine M. Complications of pediatric femur fractures treated with titanium elastic nails: a comparison of fracture types. J Pediatr Orthop. (2005) 25(5):577–80. doi: 10.1097/01.bpo.0000164872.44195.4f
Keywords: pediatric femoral shaft fracture, submuscular plating, elastic stable intramedullary nailing, systematic review, meta-analysis
Citation: Li D, Wang X, Lu J and Xue M (2023) Submuscular plating vs. elastic stable intramedullary nailing for diaphyseal femur fractures in children: a systematic review and meta-analysis. Front. Pediatr. 11:1256630. doi: 10.3389/fped.2023.1256630
Received: 11 July 2023; Accepted: 23 October 2023;
Published: 8 November 2023.
Edited by:
Xin Tang, Huazhong University of Science and Technology, ChinaReviewed by:
Thomas Palocaren, Christian Medical College and Hospital, IndiaYuxi Su, Children's Hospital of Chongqing Medical University, China
© 2023 Li, Wang, Lu and Xue. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Mingfeng Xue bWZ4dWVAYWxpeXVuLmNvbQ==
†These authors have contributed equally to this work and share first authorship
 Donghui Li
Donghui Li Xiangyue Wang2,†
Xiangyue Wang2,†