- Environment and Lifestyle Epidemiology Branch, International Agency for Research on Cancer (IARC/WHO), Lyon, France
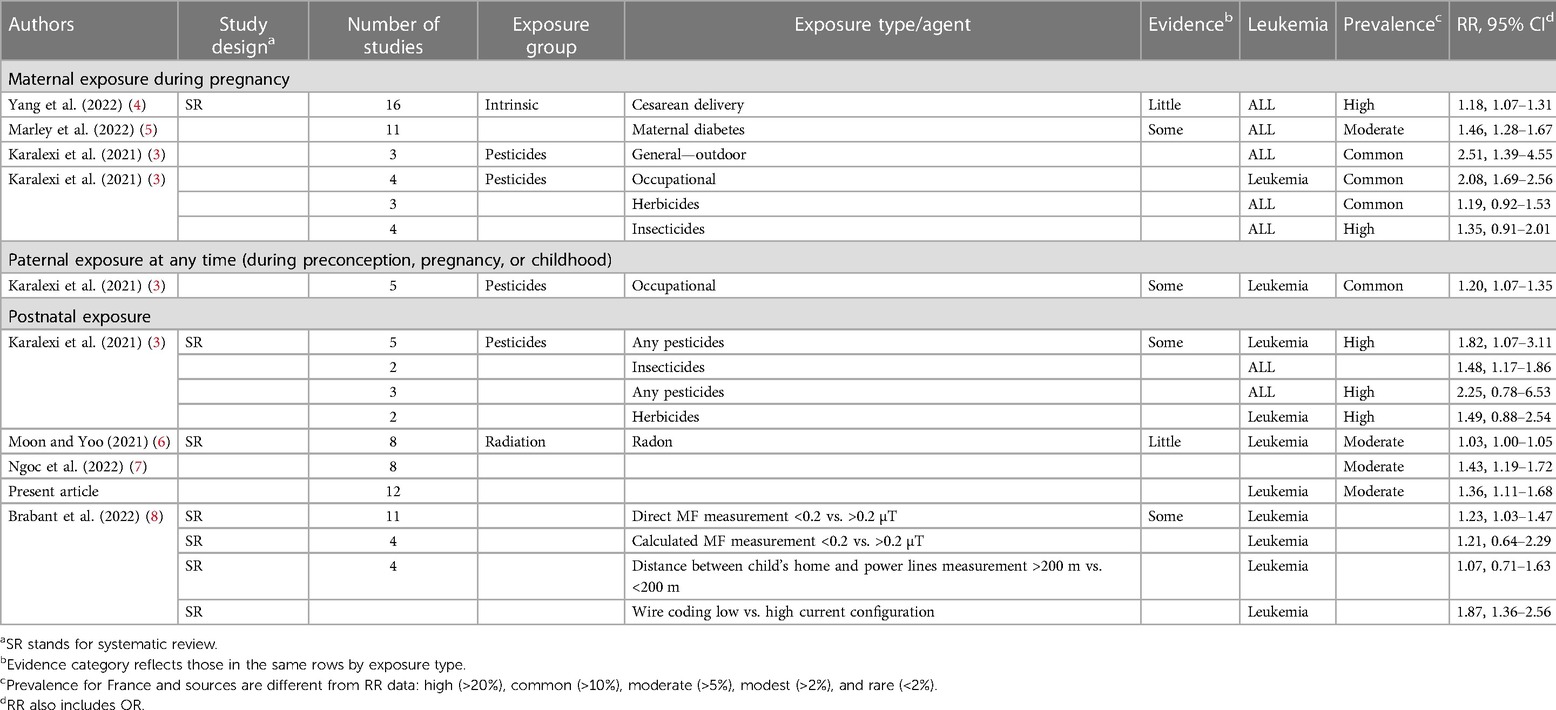
Childhood leukemia is the most common type of cancer among children globally (1). In this study, we evaluated the strength of evidence and magnitude of risk factors for childhood acute lymphoblastic leukemia (ALL) using relevant systematic reviews and pooled analyses that were not part of our previously published umbrella review (1). We also estimated the prevalence in the French population as an example of the relevance of different risk factors. The strength of the association was evaluated using the summary RR/OR values of the various meta-analyses and categorized as very strong (RR > 5), strong (RR > 2), moderate (RR > 1.5), modest (RR > 1.2), and weak (RR > 1). The strength of association, heterogeneity across studies, and number of studies were used to evaluate the strength of evidence. The evidence was categorized into “strong” (consistently strong or very strong risk estimates in quality systematic review and meta-analysis), “some” (consistently moderate risk estimates in quality systematic review and meta-analysis), “little” (consistently low risk estimates), “no” (consistently no association), and “conflicting.” The category of “conflicting” was used when systematic reviews on the same subject came to different conclusions (1). In this article, we provide an update on some of these risk factors strengthening our earlier findings and further promote the prevention of childhood ALL.
During the 70th World Health Assembly, the 2017 WHO cancer resolution adopted a global initiative for cancer prevention and control through an integrated approach (WHA70.12), which focused on reducing premature mortality from non-communicable diseases (NCDs) and achieving universal health coverage. Member states were strongly encouraged to promote the primary prevention of cancers (2). Identifying childhood ALL risk factors, especially modifiable risk factors, is crucial for the success of this campaign.
The first update is on maternal exposure to pesticides during preconception or pregnancy. A recently published systematic review (3) confirmed our previous assessment of convincing evidence of an increased ALL risk (1). In their systematic review and meta-analysis, the authors reported the strongest association in maternal outdoor exposure to pesticides during pregnancy, with more than a twofold increase in effect estimates (RR: 2.51, 95% CI: 1.39–4.55) based on three studies. The effect estimates for insecticides were 1.35 (95% CI: 0.91–2.01) based on four studies, while for herbicides, it was 1.19 (95% CI: 0.92–1.53) based on three studies. Paternal occupational exposure to pesticides at any time of the child's development was associated with childhood leukemia (OR: 1.20, 95% CI: 1.07–1.35) based on five studies. These findings were similar to the pooled summary estimates for general pesticide exposure during childhood and the risk of leukemia (OR: 1.82, 95% CI: 1.07–3.11), and for childhood exposure to insecticides and the risk of ALL (OR: 1.48, 95% CI: 1.17–1.86) based on five and two studies, respectively (Table 1). Some hypotheses suggest that childhood ALL associated with pesticide exposure may result from induced topoisomerase II inhibition leading to misrepaired DNA cleavage and further chromosomal aberrations in hematopoietic stem and/or progenitor cells (9). Greaves had earlier proposed the causal mechanism of childhood ALL to occur due to two genetic hits, with the first hit possibly being introduced by parental exposure to toxic substances during pregnancy (10).
The second update is on childhood exposure to domestic radon and the risk of leukemia. In our previous review, we concluded “conflicting evidence” based on a meta-analysis of cohort studies (two studies; OR = 0.97, 95% CI: 0.81–1.15) and of case–control studies (eight studies; OR = 1.22, 95% CI: 1.01–1.42), with somewhat conflicting results. In recent systematic reviews and meta-analyses, Moon and Yoo (6) reported a summary risk estimate of 1.03 (95% CI: 1.01–1.06) per 100 Bq/m3 radon increase based on eight case–control studies with moderate heterogeneity across studies. Ngoc et al. evaluated eight case–control studies, yielding a summary risk estimate of 1.43 (95% CI: 1.19–1.72) (7). As the case–control studies included in those meta-analyses only partly overlapped with our previous review (1), we repeated our meta-analysis with 12 case–control studies, observing an increased summary risk estimate of 1.36 (95% CI: 1.11–1.66), with a heterogeneity of 52.8%, P-value = 0.02 (Table 1). Based on this finding, we upgraded radon to “little” evidence.
Further updates are on cesarean delivery and maternal diabetes. The evidence was categorized as “little” for cesarean delivery (OR: 1.18, 95% CI: 1.07–1.31) and “some” for maternal diabetes (OR: 1.46, 95% CI: 1.28–1.67), as reported in our previous review. These findings remained unchanged even after the addition of new studies (4, 5). In addition, with regard to exposure to extremely low-frequency magnetic fields (ELF-MF), the earlier evaluation of “some” evidence remained unchanged even after the inclusion of an additional systematic review (8). The prevalence of the highlighted risk factors in France varied from “common” to “high,” except for electromagnetic field exposure, which is rare (11–16), confirming the importance of risk identification in any primary prevention.
Author contributions
FO was responsible for drafting and editing. AO, LB, and JS were involved in editing the manuscript. All authors contributed to the article and approved the submitted version.
Funding
This research was supported by the French National Cancer Institute (INCa:15670; PEDIAC Consortium).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Onyije FM, Olsson A, Baaken D, Erdmann F, Stanulla M, Wollschläger D, et al. Environmental risk factors for childhood acute lymphoblastic leukemia: an umbrella review. Cancers (Basel). (2022) 14(2). doi: 10.3390/cancers14020382
2. World Health Assembly. Cancer prevention and control in the context of an integrated approach (Wha70. 12). Available at: https://Apps.Who.Int/Gb/Ebwha/Pdf_Files/Wha70/A70_R12-En.Pdf (Accessed March 30, 2023).
3. Karalexi MA, Tagkas CF, Markozannes G, Tseretopoulou X, Hernández AF, Schüz J, et al. Exposure to pesticides and childhood leukemia risk: a systematic review and meta-analysis. Environ Pollut. (2021) 285:117376. doi: 10.1016/j.envpol.2021.117376
4. Yang Y, Yu C, Fu R, Xia S, Ni H, He Y, et al. Association of cesarean section with risk of childhood leukemia: a meta-analysis from an observational study. Hematol Oncol. (2022) 41(1):182–91. doi: 10.1002/hon.3070
5. Marley AR, Domingues A, Ghosh T, Turcotte LM, Spector LG. Maternal body mass index, diabetes, and gestational weight gain and risk for pediatric cancer in offspring: a systematic review and meta-analysis. JNCI Cancer Spectr. (2022) 6(2). doi: 10.1093/jncics/pkac020
6. Moon J, Yoo H. Residential radon exposure and leukemia: a meta-analysis and dose-response meta-analyses for ecological, case-control, and cohort studies. Environ Res. (2021) 202:111714. doi: 10.1016/j.envres.2021.111714
7. Ngoc LTN, Park D, Lee YC. Human health impacts of residential radon exposure: updated systematic review and meta-analysis of case-control studies. Int J Environ Res Public Health. (2022) 20(1). doi: 10.3390/ijerph20010097
8. Brabant C, Geerinck A, Beaudart C, Tirelli E, Geuzaine C, Bruyère O. Exposure to magnetic fields and childhood leukemia: a systematic review and meta-analysis of case-control and cohort studies. Rev Environ Health. (2022) 38(2):229–53. doi: 10.1515/reveh-2021-0112
9. Nicolella HD, de Assis S. Epigenetic inheritance: intergenerational effects of pesticides and other endocrine disruptors on cancer development. Int J Mol Sci. (2022) 23(9):4671. doi: 10.3390/ijms23094671
10. Greaves M. A causal mechanism for childhood acute lymphoblastic leukaemia. Nat Rev Cancer. (2018) 18(8):471–84. doi: 10.1038/s41568-018-0015-6
11. Glorennec P, Serrano T, Fravallo M, Warembourg C, Monfort C, Cordier S, et al. Determinants of children’s exposure to pyrethroid insecticides in western France. Environ Int. (2017) 104:76–82. doi: 10.1016/j.envint.2017.04.007
12. Ajrouche R, Roudier C, Cléro E, Ielsch G, Gay D, Guillevic J, et al. Quantitative health impact of indoor radon in France. Radiat Environ Biophys. (2018) 57(3):205–14. doi: 10.1007/s00411-018-0741-x
13. Le Ray C, Girault A, Merrer J, Bonnet C, Blondel B. Impact of national guidelines on the cesarean delivery rate in France: a 2010–2016 comparison using the Robson classification. Eur J Obstet Gynecol Reprod Biol. (2020) 252:359–65. doi: 10.1016/j.ejogrb.2020.07.012
14. Regnault N, Salanave B, Castetbon K, Cosson E, Vambergue A, Barry Y, et al. Gestational diabetes in France in 2012: screening, prevalence and management methods during pregnancy. Bulletin Épidémiologique Hebdomadaire. (2016) 9:164–73.
15. Weisskopf MG, Moisan F, Tzourio C, Rathouz PJ, Elbaz A. Pesticide exposure and depression among agricultural workers in France. Am J Epidemiol. (2013) 178(7):1051–8. doi: 10.1093/aje/kwt089
16. ANSES. Health effects associated with exposure to low-frequency electromagnetic fields. Available at: https://www.anses.fr/en/content/health-effects-associated-exposure-low-frequency-electromagnetic-fields
Keywords: childhood leukemia, risk factors, environmental exposures, pesticides, radon, cesarean delivery
Citation: Onyije FM, Olsson A, Bouaoun L and Schüz J (2023) Synthesized evidence for childhood acute lymphoblastic leukemia. Front. Pediatr. 11:1209330. doi: 10.3389/fped.2023.1209330
Received: 20 April 2023; Accepted: 4 July 2023;
Published: 24 July 2023.
Edited by:
Marta Llop, Hospital Universitario y Politécnico La Fe, SpainReviewed by:
Ruth Etzel, U.S. Environmental Protection Agency, United States© 2023 Onyije, Olsson, Bouaoun and Schüz. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Felix M. Onyije b255aWplZkBpYXJjLndoby5pbnQ=
 Felix M. Onyije
Felix M. Onyije Ann Olsson
Ann Olsson