
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
CASE REPORT article
Front. Pediatr., 18 July 2023
Sec. Pediatric Infectious Diseases
Volume 11 - 2023 | https://doi.org/10.3389/fped.2023.1198505
This article is part of the Research TopicEthnic Differences in Children in the Clinical Manifestation of Infection with SARS-Cov-2 and its VariantsView all 7 articles
 Takanori Suzuki1*
Takanori Suzuki1* Toya Kono1
Toya Kono1 Hisada Satoshi2
Hisada Satoshi2 Hidetoshi Uchida1
Hidetoshi Uchida1 Seiichiro Ota3
Seiichiro Ota3 Ichiro Tateya2
Ichiro Tateya2 Tetsushi Yoshikawa1
Tetsushi Yoshikawa1
Multisystem inflammatory syndrome in children (MIS-C) has been widely reported, mainly in Western countries. The clinical features of MIS-C and Kawasaki disease are similar. The latter is common in Asian countries, including Japan. Meanwhile, the incidence of MIS-C seems to be low in Japan. Retropharyngeal edema is relatively common in older patients with Kawasaki disease and has been reported in a few patients with MIS-C. We describe a case of severe retropharyngeal edema after coronavirus disease 2019 (COVID-19) that improved quickly with high-dose of intravenous immunoglobulin treatment. Onset of retropharyngeal edema was 3 weeks after COVID-19. The patient received appropriate intravenous antibiotics for 5 days, but his symptoms worsened. Therefore, we suspected that his retropharyngeal edema was caused by suspected MIS-C even though he did not have the typical clinical symptoms of suspected MIS-C such as gastrointestinal symptoms and shock. Retropharyngeal edema was refractory to antibiotic therapy but lessened quickly with high-dose immunoglobulin therapy, without other typical clinical manifestations of MIS-C, suggesting that early immunoglobulin therapy might prevent the progression of MIS-C.
Although coronavirus disease 2019 (COVID-19) is generally a mild disease in children, severe inflammation of multiple organ systems, a condition termed multisystem inflammatory syndrome in children (MIS-C), has been reported, mainly in Western countries (1, 2). The American College of Rheumatology has published a diagnostic algorithm for MIS-C that includes clinical features (rash, gastrointestinal symptoms, edema of the hands or feet, oral mucosal changes, conjunctivitis, lymphadenopathy, and neurologic symptoms), as well as a tiered laboratory workup (3–5). Specific treatments such as intravenous immunoglobulin and steroids are required to improve the prognosis of MIS-C. Since MIS-C and Kawasaki Disease share similar clinical features, a detailed differential diagnosis of the two diseases; this is especially necessary as Kawasaki Disease is common in Asian countries, including Japan (6, 7). Retropharyngeal edema is a characteristic finding that is relatively common in older patients with Kawasaki disease (8). Meanwhile, retropharyngeal edema has also been demonstrated in a small number of patients with MIS-C. Here we report a case of severe retropharyngeal edema that was refractory to antibiotic therapy but rapidly resolved with high-dose immunoglobulin therapy. The patient had been infected with COVID-19 three weeks before the onset of the disease and had recovered without any other clinical manifestations of MIS-C.
A previously healthy nine-year-old Japanese boy was transferred from another hospital for refractory severe retropharyngeal edema despite intensive intravenous antibiotic therapy for two days. The patient's clinical course is shown in Figure 1. He had COVID-19 three weeks prior to the onset of this disease. The antigen test for COVID-19 was positive. At that time, he had a high fever for 5 days but recovered without any complications or sequelae. Five days before admission to our hospital, he had a high fever of 39°C. Rapid antigen tests for influenza and SARS-CoV-2 performed in the local pediatric clinic were negative. Subsequently, in addition to high fever, other symptoms such as headache, neck tenderness, limitation of neck motion, muffled voice, difficulty swallowing, and severe snoring developed. Two days before admission to our hospital, he was admitted to a local hospital due to a severe inflammatory response; white blood cell count (WBC) was 25,200/μl and C-reactive protein (CRP) was 31 mg/dl. Contrast-enhanced CT(computed tomography) showed posterior pharyngeal edema. Since posterior pharyngeal abscess was suspected, ceftriaxone (1000 mg four times daily), clindamycin (300 mg four times daily), and vancomycin (500 mg four times daily) were administered. These antibiotics of the treatment started at the local hospital where the patient was first admitted. On the second day of admission to the local hospital, the patient was transferred to our hospital for surgical treatment.
On admission to our hospital, he had high fever, pharyngeal erythema, and bilateral cervical lymphadenopathy with tenderness. However, he did not have any typical symptoms of Kawasaki disease, such as ocular conjunctival hyperemia, lip redness, fingertip edema, or skin rash. He was nine-years old, which was not the preferred age for Kawasaki disease. In addition, he had no gastrointestinal symptoms. His abdomen was soft, non-tender, and non-distended. A repeat rapid antigen test for SARS-CoV-2 performed on admission to our hospital was negative. No clinical symptoms suggestive of heart failure were observed at hospital admission.
His initial workup was significant for leukocytosis (WBC count, 26,400/μl; absolute neutrophil count, 22,704/μl; absolute lymphocyte count, 1,150/μl), elevated CRP (23 mg/L) and erythrocyte sedimentation rate (104 mm/hour), and decreased sodium level (129 mEq/L). N-terminal pro-brain natriuretic peptide and Troponin I were normal (74 pg/ml, 0.0012 ng/ml). Furthermore, fibrinogen and D-dimer were elevated (881 mg/dl, 3.8 μg/ml). The patient's electrocardiogram was unremarkable, showing good cardiac contraction, no pericardial effusion, and no coronary abnormalities. This case was not vaccinated against COVID-19, and serological evaluation of COVID-19 was not been performed. Fiberoptic examination of the larynx revealed severe swelling of the palatine tonsils, mild swelling of the epiglottis, and salivary effusion. Contrast-enhanced CT showed right posterior pharyngeal edema in an area of 17 mm × 14 mm × 34 mm, a hypo-absorptive area in front of the vertebral body on C1 suggestive of edema, and bilateral tonsillar enlargement (Figures 2A,B). Although no bacteria were isolated from a throat swab or blood cultures performed at the first visit to the local hospital, the three antibiotics had been given continuously after transfer to our hospital. The patient received the three antibiotics for a total of sevens days, but his symptoms worsened.
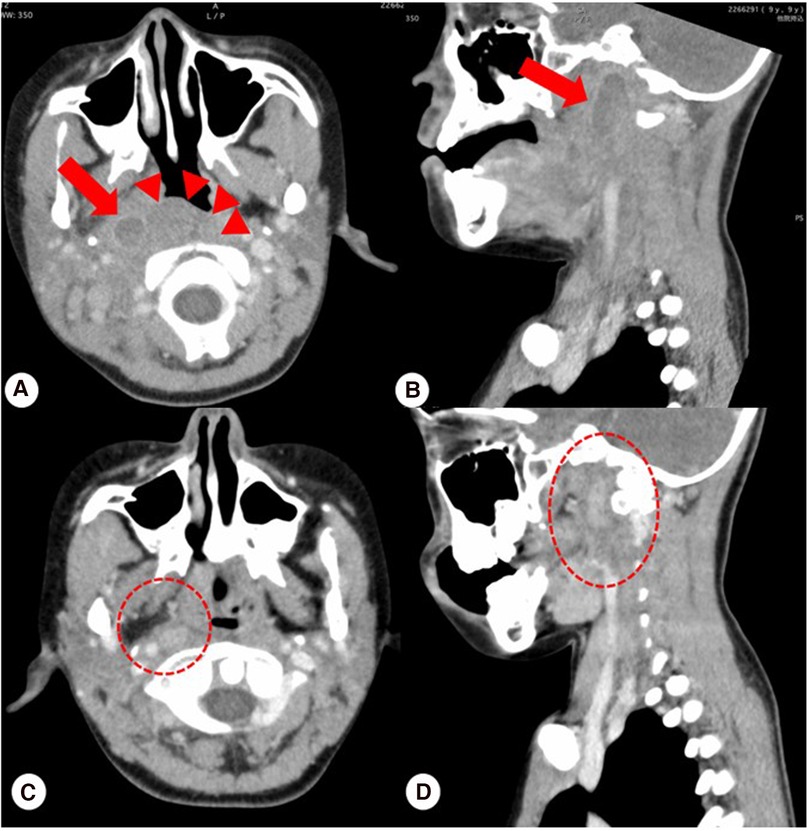
Figure 2. (A,B) Contrast-enhanced CT showed retropharyngeal edema on the right side in an area of 17 mm × 14 mm × 34 mm indicated by arrows, edema appearing as a hypo-absorptive area in front of the vertebral body on C1 indicated by arrowheads, and bilateral tonsillar enlargement. (C,D) Follow-up contrast-enhanced CT scan at 14 days after discharge confirmed complete resolution of retropharyngeal edema and no sign of edema indicated by ovals.
Due to a poor response to the three antibiotics and the previous history of COVID-19, and no bacteria were isolated from a throat swab or blood cultures performed at the local hospital and our hospital, we suspected early-stage MIS-C. In addition, it was difficult to perform surgical treatment. The patient was at high risk for upper airway obstruction due to rapidly progressive retropharyngeal edema. Thus, we diagnosed the patient with suspected MIS-C on the fifth day of admission and administered single 10% intravenous immunoglobulin (2 g/kg). Thereafter, his symptoms rapidly lessened. The patient was discharged on the 17th day of hospitalization with no findings of myocardial damage or coronary artery dilatation based on echocardiography in addition, CRP 0.13 mg/L confirmed negative. A follow-up contrast-enhanced CT scan 14 days after discharge showed complete resolution of retropharyngeal and posterior pharyngeal edema (Figures 2C,D). Consent for publication was obtained from patient and his guardians according to the institution's guidelines.
In the present case, a previously healthy nine-year-old boy developed severe retropharyngeal edema refractory to intensive antibiotic treatment. He had the typical clinical signs and symptoms of retropharyngeal edema and enhanced CT showed the typical findings of the disease. In addition to the lack of response to antimicrobial treatment for severe retropharyngeal edema, the throat swab and blood cultures performed at the first hospital visit were negative. Furthermore, he had COVID-19 three weeks prior to the onset of retropharyngeal edema. He was nine-years old, which the preferred age for MIS-C (7, 9).
There have been several case reports of MIS-C complicated by retropharyngeal edema (9–14). In one study, neck-related symptoms occurred in 39 of 137 (28.5%) patients with MIS-C; 4 of 137 (2.5%) patients with MIS-C had retropharyngeal edema (14). Since this patient did not have symptoms typical of Kawasaki disease such as skin rash, inflammation of the oral mucosa, conjunctival injection, extremity findings, gastrointestinal symptoms, and cardiac failure, the diagnosis was suspected to be early-stage retropharyngeal edema associated with MIS-C.
As a result of intravenous immunoglobulin treatment for MIS-C, his symptoms rapidly diminished and his laboratory data also rapidly returned to normal. After finishing the treatment, we monitored carefully for gastrointestinal symptoms and cardiac dysfunction, but neither gastrointestinal symptoms nor shock was observed. The previously reported cases of MIS-C with retropharyngeal edema included the typical clinical manifestations of MIS-C, including cardiac shock (10–12). In at least two patients with MIS-C, retropharyngeal edema clearly preceded the appearance of typical clinical symptoms of MIS-C, including severe gastrointestinal symptoms and shock (9, 11). These two patients were considered to have retropharyngeal abscesses and were treated with intravenous immunoglobulin and steroids after the appearance of cardiogenic shock. This case, along with the two previously reported MIS-C cases, suggests that early administration of intravenous immunoglobulin might prevent the progression of MIS-C and the development of circulatory failure. To verify our hypothesis, it is necessary to confirm in numerous cases that early administration of IVIG may prevent the exacerbation of severe conditions such as cardiogenic shock in MIS-C.suspected It is important to distinguish between retropharyngeal edema and retropharyngeal abscess for early MIS-C intervention. In addition to performing contrast-enhanced CT to confirm retropharyngeal edema, febrile children with severe neck involvement should be checked for a recent history of COVID-19 if MIS-C is suspected. Furthermore, since some of the clinical manifestations of MIS-C and Kawasaki disease overlap, biomarkers to differentiate between MIS-C and Kawasaki disease have been investigated (15). A reliable biomarker that predicts MIS-C will be useful for early intervention and improve the prognosis of patients with MIS-C.
We described a previously healthy Japanese boy with suspected MIS-C–associated retropharyngeal edema. Although he did not improve with intensive antibiotic therapy, he recovered quickly after intravenous immunoglobulin treatment and did not develop severe clinical manifestations such as cardiac shock. Therefore, retropharyngeal edema might allow for the prediction of MIS-C and early intervention might prevent disease progression.
The original contributions presented in the study are included in the article, further inquiries can be directed to the corresponding author.
Written informed consent was obtained from the participant/patient(s) for the publication of this case report.
TS, TK, and HS conceptualized and designed the study, drafted the initial manuscript, and reviewed and revised the manuscript. HU and SO collected data, carried out the initial analyses, and reviewed and revised the manuscript. IT and TY designed the data collection instruments, coordinated and supervised data collection, and critically reviewed the manuscript. All authors contributed to the article and approved the submitted version.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
COVID-19, coronavirus disease 2019; CT, computed tomography; HD, hospital day; MIS-C, multisystem inflammatory syndrome in children; WBC, white blood cell; CRP, C-reactive protein.
1. Dufort EM, Koumans EH, Chow EJ, Rosenthal EM, Muse A, Rowlands J, et al. Multisystem inflammatory syndrome in children in New York state. N Engl J Med. (2020) 383(4):347–58. doi: 10.1056/NEJMoa2021756
2. Kaushik S, Aydin SI, Derespina KR, Bansal PB, Kowalsky S, Trachtman R, et al. Multisystem inflammatory syndrome in children associated with severe acute respiratory syndrome coronavirus 2 infection (MIS-C): a multi-institutional study from New York city. J Pediatr. (2020) 224:24–9. doi: 10.1016/j.jpeds.2020.06.045
3. Henderson LA, Canna SW, Friedman KG, Gorelik M, Lapidus SK, Bassiri H, et al. American College of rheumatology clinical guidance for multisystem inflammatory syndrome in children associated with SARS-CoV-2 and hyperinflammation in pediatric COVID-19: version 2. Arthritis Rheumatol. (2021) 73(4):e13–29. doi: 10.1002/art.41616
4. Multisystem Inflammatory Syndrome in Children (MIS-C) Associated with Coronavirus Disease 2019 (COVID-19). Health Alert Network (HAN). Available at: https://emergency.cdc.gov/han/2020/han00432.asp
5. Multisystem inflammatory syndrome in children and adolescents with COVID-19. Scientific Brief. World Health Organization. Available at: https://www.who.int/news-room/commentaries/detail/multisystem-inflammatory-syndrome-in-children-and-adolescents-with-covid-19
6. Uehara R, Belay ED. Epidemiology of kawasaki disease in Asia, Europe, and the United States. J Epidemiol. (2012) 22(2):79–85. doi: 10.2188/jea.JE20110131
7. Wessels PA, Bingler MA. A comparison of kawasaki disease and multisystem inflammatory syndrome in children. Prog Pediatr Cardiol. (2022) 65:101516. doi: 10.1016/j.ppedcard.2022.101516
8. Tomomori A, Hashida Y, Sakata S. Five cases of kawasaki disease requiring differentiation from posterior pharyngeal abscess. Kawasaki disease requiring differentiation from posterior pharyngeal abscess. Syounika Rinshyo. (2014) 67:2159–64. in Japanese.
9. Zhou C, Cheng M, Hong H. A mysterious fever and retropharyngeal edema on a previously healthy 10-year-old boy without known exposure to COVID-19. Cureus. (2022) 14(5):e25373. doi: 10.7759/cureus.25373
10. Brooks R, Fisher R, Glicksman C, Pollak U, Simanovsky N, Berkun Y. Multisystem inflammatory syndrome in children associated with COVID-19 presenting as cervical inflammation. Acta Paediatr. (2023) 112:477–82. doi: 10.1111/apa.16623
11. Han P, Douillard J, Cheng J, Ramanathan A, Tieu D, Degner T. Multisystem inflammatory syndrome in children in a 15-year-old male with a retropharyngeal phlegmon. Case Rep Pediatr. (2020) 2020:6668371. doi: 10.1155/2020/6668371
12. Gupta P, Giri PP, Das D, Pal P. Pediatric inflammatory multisystem syndrome (PIMS) presenting with retropharyngeal phlegmon mimicking kawasaki disease. Clin Rheumatol. (2021) 40(5):2097–8. doi: 10.1007/s10067-020-05538-x
13. Jenkins E, Sherry W, Smith AGC, Rostad BS, Rostad CA, Jones K, et al. Retropharyngeal edema and neck pain in multisystem inflammatory syndrome in children (MIS-c). J Pediatric Infect Dis Soc. (2021) 10(9):922–5. doi: 10.1093/jpids/piab050
14. Daube A, Rickert S, Madan RP, Kahn P, Rispoli J, Dapul H. Multisystem inflammatory syndrome in children (MIS-C) and retropharyngeal edema: a case series. Int J Pediatr Otorhinolaryngol. (2021) 144:110667. doi: 10.1016/j.ijporl.2021.110667
Keywords: COVID-19, retropharyngeal edema, MIS-C, IVIG (Intravenous immunoglobulin) administration, kawasaki disease (KD)
Citation: Suzuki T, Kono T, Satoshi H, Uchida H, Ota S, Tateya I and Yoshikawa T (2023) Case report: A case of severe retropharyngeal edema after COVID-19 successfully treated with intravenous immunoglobulin. Front. Pediatr. 11:1198505. doi: 10.3389/fped.2023.1198505
Received: 1 April 2023; Accepted: 30 June 2023;
Published: 18 July 2023.
Edited by:
San-Nan Yang, E-Da Hospital, TaiwanReviewed by:
Kai-Sheng Hsieh, China Medical University, Taiwan© 2023 Suzuki, Kono, Satoshi, Uchida, Ota, Tateya and Yoshikawa. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Takanori Suzuki dGFrYW5vcmktc0BheGVsLm9jbi5uZS5qcA==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.