
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
OPINION article
Front. Pediatr. , 31 March 2023
Sec. Pediatric Critical Care
Volume 11 - 2023 | https://doi.org/10.3389/fped.2023.1165301
With every school shooting, debate on firearms garners national attention. Pediatricians will have to play an important role in the practice of promoting and integrating positive changes in the environment for children. Pediatricians played an important role in the early years of motor vehicular crashes to draw national attention to the epidemic and impact on children. We provide the perspective of the financial burden due to firearm injuries, contrasting it with vehicular crashes, an additional insight for pediatricians to promote firearm safety.
Since 2013, fatal firearm injuries in children and adolescents have been increasing in United States (1). Lee et al. described a concerning trend for deaths in children, adolescents, and youth ages 1–24 years in the United States (2). In 2017, deaths due to firearm related injuries became the most common cause of death in this age group, surpassing deaths due to motor vehicle crashes. Lee and colleagues analyzed CDC's data from 2000 to 2020 and saw the number of firearm related deaths among children, adolescents and young adults increased from 7.3 per 100,000 persons to 10.28 per 100,000 persons. There is political will and a public cry to address firearm injuries as a public health problem, and research on trends, disparities, risk factors will help guide preventive efforts.
In the United States, since 2016, the economic impact of firearm related deaths, both in terms of medical costs and the statistical value of life lost to death, is consistently greater than 1 billion dollars each year. Millions of dollars are spent caring for youth in emergency departments (3), and billions of dollars are spent on inpatient care (4, 5).
CDC has ensured publicly available data through the Web-based Injury Statistics Query and Reporting System (WISQARS) (6). It is an interactive data visualization and can provide insights in trends in deaths due to various causes of injuries. WISQARS is proving to be an essential tool in identifying nature and extent of injury, fatal and non-fatal burden of such injuries, and prioritization of prevention strategies (7).
To understand the economic impact of firearm injuries from 2015 to 2020, we compared the percentage change to 2015 data for fatalities and total cost (medical and value of statistical life) for both firearm injuries and motor vehicle crashes. After obtaining the data from WISQARS, data for each type of injury for each year was tabulated and the percentage increase to the previous year was calculated. The fatality data is obtained from National Vital Statistics System (NVSS) using the death certificates. For the estimate of cost of injury data is obtained from Pacific Institute of Research and Evaluation.
We found that the percentage change in cost for firearm injuries or motor vehicle crashes corresponded to the mortality in that particular year, higher the mortality that year, higher the cost. Beginning in 2017, we found a striking trend with an increase in fatalities and total cost for firearm injuries and decrease in fatalities and total cost for motor vehicle crashes (Figure 1). It has been shown that since 2017, deaths due to firearm injuries became the leading cause of deaths for children, adolescents, and young adults. In 2020, deaths and total costs for firearm related injuries were 39.2% and 41% respectively, higher than in 2015. In 2019, we observed the largest drop in motor vehicle deaths (12.35%) and total costs (12%). These cost are only for fatal injuries either due to firearms or motor vehicular crashes.
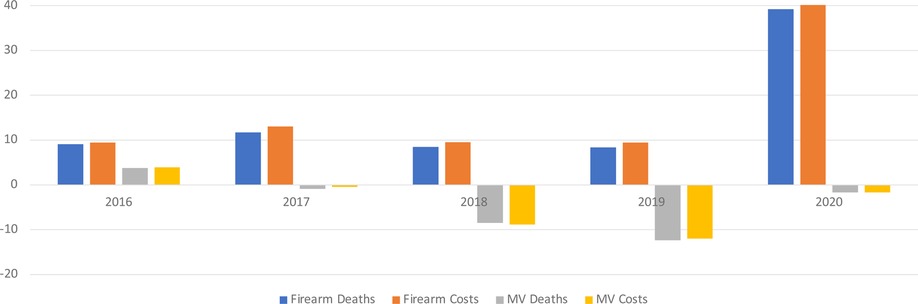
Figure 1. Percentage change in deaths and costs for firearm and motor vehicle fatalities in 1–24 years of age (compared to 2015).
During the COVID-19 pandemic there was a surge in firearm sales and in gun deaths. We have also seen an increase in the use of firearms to commit suicide. Rural children are at increasing risk for using firearms to commit suicide. Urban children are more prone to unintentional or homicidal victims of firearm injuries.
Lee and colleagues (2) present us with a comprehensive public health approach to injury reduction that has been extremely successful in preventing injury-related deaths. This should serve as a model for the public health approach to reduce firearm-related injuries and deaths. The measures implemented to prevent motor vehicle related deaths in the last 20 or more years and their efficacy in achieving that goal sit in stark contrast to the comparatively limited interventions to prevent youth firearm death and injury. Similar to the approach to motor vehicular collisions, the approach to firearm injuries can be divided into three phases to decrease the morbidity and mortality: (1) Pre-event phase (access to mental health services, child access prevention laws, licensing and permit-to-purchase requirements, extreme risk protective orders), (2) Event phase (school safety policies, “gun free zones,” magazine capacity limits, bump stock prohibitions), and (3) post event phase (medical and rehabilitation services, trauma center accreditation, EMS systems). Onus should not fall on a particular group of individuals, but each group will have to play their role if we are to decrease the mortality burden due to firearm injuries. We are seeing an increase in research funding for firearm injuries which will lead to identifying and prioritizing prevention strategies. Policy makers will have evidenced based scientific data to make informed decision for allocation of resources. One of the limitations of the study is the age group (1–24 years) arguing the higher incidence of firearm injuries in young adults and not necessarily in children. Most pediatricians are involved in the care of children and young adults up to 18 or 21 years of age. We used this age group as CDC does provide data in 5-year or 10-year age groups and data was similar to previously published study (2).
While, as pediatricians, we believe that children's lives tragically lost to violence are compelling to drive policy and research, our report also helps to highlight the economic burden of firearm-related deaths and injuries and may further strengthen the case for investment in research and in evidence-based policy initiatives to prevent firearm injuries. Pediatricians will have to harness each opportunity available or each piece of emerging data available to convince policy makers for positive changes as we amplify the voices of our patients, families, and communities that we serve.
SM and DB conceptualized and designed the study, drafted the initial manuscript and reviewed and revised the manuscript. KH critically reviewed the manuscript for important intellectual content. All authors contributed to the article and approved the submitted version.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Cunningham RM, Ranney ML, Goldstick JE, Kamat SV, Roche JS, Carter PM. Federal funding for research on the leading causes of death among children and adolescents. Health Aff (Millwood). (2019) 38(10):1653–61. doi: 10.1377/hlthaff.2019.00476
2. Lee LK, Douglas K, Hemenway D. Crossing lines—a change in the leading cause of death among U.S. Children. N Engl J Med. (2022) 386(16):1485–7. doi: 10.1056/NEJMp2200169
3. Gani F, Canner JK. Trends in the incidence of and charges associated with firearm-related injuries among pediatric patients, 2006–2014. JAMA Pediatr. (2018) 172(12):1195–6. doi: 10.1001/jamapediatrics.2018.3091
4. Lee J, Quraishi SA, Bhatnagar S, Zafonte RD, Masiakos PT. The economic cost of firearm-related injuries in the United States from 2006 to 2010. Surgery. (2014) 155(5):894–8. doi: 10.1016/j.surg.2014.02.011
5. Taylor JS, Madhavan S, Han RW, Chandler JM, Tenakoon L, Chao S. Financial burden of pediatric firearm-related injury admissions in the United States. PLoS One. (2021) 16(6):e0252821. doi: 10.1371/journal.pone.0252821
6. WISQARS (web-based injury statistics query and reporting system). Centers for Disease Control and Prevention. Available at: https://www.cdc.gov/injury/wisqars/index.html (Published December 2, 2021, Accessed July 5, 2022).
Keywords: firearm, pediatrics, etiology, motor vechicle crashes, epidemiology
Citation: Manzar S, Hoops K and Bagdure D (2023) Insight for pediatricians: Comparing economic trends for firearm related deaths and deaths from motor vehicle crashes. Front. Pediatr. 11:1165301. doi: 10.3389/fped.2023.1165301
Received: 13 February 2023; Accepted: 13 March 2023;
Published: 31 March 2023.
Edited by:
Adnan Bhutta, Riley Hospital for Children, United StatesReviewed by:
Theresa Ann Mikhailov, Medical College of Wisconsin, United States© 2023 Manzar, Hoops and Bagdure. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Dayanand Bagdure ZGF5YW5hbmQuYmFnZHVyZUBsc3Vocy5lZHU=
Specialty Section: This article was submitted to Pediatric Critical Care, a section of the journal Frontiers in Pediatrics
Abbreviations CDC, Centers for Disease Control and Prevention; WISQARS-Web-based Injury Statistics Query and Reporting System.
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.