- 1Department of Pediatrics, The First Affiliated Hospital of Nanjing Medical University, Nanjing, China
- 2Department of Pediatrics, First Affiliation Hospital of Nanjing Medical University, Nanjing, China
The coronavirus disease 2019 (COVID-19) caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has caused many significant changes to all aspects of day to day life. The disease has spread and reached pandemic proportions. The principle route of transmission is the respiratory route. Infants, pregnant women and breastfeeding mothers have all been affected. Many interventions and guidelines from important societies have been instituted in order to curb the transmission of the disease. These have involved both pharmacological and non-pharmacological methods. COVID-19 vaccines have also emerged as important methods of primary prevention of the disease. But several questions have been raised concerning the safety and efficacy of their use in pregnant and breastfeeding mothers. It has also not been clear if the vaccines are effective in generating a robust immune response in the pregnant women and breastfeeding mothers to confer passive immunity to the fetuses and infants, respectively. And they have not been tested in infants. The aspect of infant feeding has equally been affected. Although breast milk has not been known to serve as the vehicle of transmission of the virus, there is still some lack of uniformity of practice regarding breastfeeding when a mother has SARS-CoV-2 infection. This has led to infant feeding being done by the use of commercial formula feeds, pasteurized human donor breast milk, feeding on the mother's own expressed breast milk by a care giver and directly breastfeeding with skin to skin contact. This is despite breast milk being the most physiologically appropriate type of feed for infants. Therefore the pertinent question remains; should breastfeeding continue during the pandemic continue? This review also seeks to analyse the vast amount of scientific information regarding the subject and to synthesize science-based information
1. Introduction
Coronavirus disease 2019 (COVID-19) is a novel type of highly contagious infectious disease caused by a novel type of coronavirus now termed Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2). By using RNA (Ribonucleic Acid) sequencing the causative virus was found to be a previously unknown betacoronavirus (52). Because it was previously unknown, the World Health Organization (WHO) named the virus as the “novel coronavirus 2019” (2019-nCoV), and later the disease was renamed as “coronavirus disease 2019” (COVID-19) (112, 113). Coronaviruses are characterized by frequently crossing the species barrier. These events occur in circumstances that are yet to be fully understood; and can occur from animals to humans (zoonoses), or from humans to animals (reverse zoonoses) (6). The disease is believed to have originated from bats (99–107), spilling over to the human beings in which species the infection has continued, even to reach pandemic proportions. And this was not the first occurrence of such a crossing of the species barrier for beta-coronaviruses, as the phenomenon has occurred 3 times in the last 20 years leading to 3 outbreaks of zoonotic type, these being the following; SARS-CoV, MERSCoV, and SARS-CoV-2 outbreaks of 2002/3, 2012 and 2019 to date, respectively (25). Ellis et al. (29) reported that jumping the species barrier is made possible because the genomes of coronaviruses often maintain characteristic features of their wild type as well as including new characteristics.
2. Methodology
Finding reliable and authentic sources of information for citation on the topic of “breastfeeding during the COVID-19 pandemic” was a challenge for the researchers. The researchers used electronic databases using the key word searching methods to locate sources of information on the topic. A methodical search was performed in many databases, among them the Lancet, ABM, ACOG, CDC, WHO, RCOG, New England Journal of Medicine, Google Scholar, Cochrane, UpToDate, from March 2015 up to and including April, 2023. The descriptors used to perform the searches were breastfeeding, breast milk, COVID-19, Coronavirus disease 2019, SARS-CoV-2 vertical transmission, mother-to-child transmission, intrauterine transmission, in-utero transmission, immunoglobulin, COVID-19 vaccine, COVID-19 guidelines. No language restrictions were applied. Full-text articles were identified from online sources.
The credibility of each source was checked one by one so as to avoid citing false, unverifiable and unscientific information. To check for credibility of the information, the researchers found background information on each one of the authors. The researchers had the responsibility of determining that the information cited in the review was credible and valid. Therefore, a list of evaluating criteria consisting of the following was used:
i. Is this the true author of the information?
ii. Is this an authentic and reliable website?
iii. Is the information verifiable and true?
iv. Is this information from original research?
v. Are credible researchers cited by the source?
vi. Is the information concise, logical and well-organized?
2.1. Transmission of SARS-CoV-2 to the general population
From the Chinese City of Wuhan the disease spread rapidly across the whole of China, and to the rest of the world (72) leading to, on 30th January, its being declared a Public Health Emergency of International Concern, PHEIC (99–107); and as a global pandemic on March 11th, 2020, by the WHO (99–107). The pandemic continues to cause global disruption and affecting all areas of people's lives, apart from just health. It also affects other facets of human life such as the social, economic, cultural, and political and economic aspects of living globally (99–107). Therefore, there has been particular interest in the disease leading to increased publishing on the disease lately. However, some information is deficient in evidence that originates from science, which could be harmful instead of being beneficial. The need for science-based practices is very important with regard to breastfeeding in women who are suspected or confirmed to be infected with the disease (56).
In the early stages of the pandemic, it was thought that all of the patients that suffered from COVID-19 had been to the seafood market at Hunan in Wuhan. It was also thought that if they had not visited the market, then they must have consumed meat from that had originated from there. But additional investigations revealed that some of them had neither visited the food market nor consumed meat and meat product from there. Thus, the spread of the virus via aerosols or droplets was accepted (55).
The respiratory route is the principal route of transmission for SARS-COV-2, a highly contagious virus (78, 116). Spread also occurs by both direct and indirect contact between people within a distance of 2 m. But transmission over longer distances is unlikely (78). Additionally, Anastassopoulou et al. (6) reported that respiratory secretions are not only expelled during sneezing or coughing, but also during talking, singing, and laughing. The droplets so released are then inhaled. This has since formed the scientific basis for the public health advice of social distancing.
This review, meant for health care professionals, is compiled from the latest available information about Coronavirus Disease-2019 and is not intended to substitute either clinical judgement or expert opinion. It should also be noted that because of on-going research about COVID-19, new information is becoming rapidly available, and suggestions may change as such.
2.2. Characteristics of SARS-CoV-2
The SARS-CoV-2 virus is an enveloped positive sense single stranded RNA beta-coronavirus virus ranging from 27 to 33 kb in size and has a crown-like appearance from which it gets the name “corona”. Investigating the virus proved that the organization of its genome is similar to that of the other betacoronaviruses (115, 4). Its genomic sequence is 79% identical to SARS-CoV and 50% identical to Middle East Respiratory Syndrome Coronavirus (MERS-CoV), 88% identical to bat-SLCoVZC45 and bat-SL-CoVZXC21. It was also found to be 96.2% identical to CoV RaTG13 which is a bat CoV (115, 76); with structural genes whose amino acids are over 90% identical to those of SARS-CoV-2. It was also discovered that beyond the similarities in the genome, the proteins that code for genes were also similar; exhibiting 79.5% similarity to SARS-CoV-2 and 51% similarity to MERS-CoV (44, 45, 55). The SARS-CoV-2 genome contains several reading open reading frames (ORFs) whose function is to serve as a template for the production of subgenomic mRNAs and accessory proteins. It also contains putative ORFs interposed between structural genes and code for structural and accessory proteins (82, 59).
3. Breast milk dilemma during the pandemic
Even as information regarding the subject is becoming more available, we can make use of what is currently known about breastfeeding and previous outbreaks of infectious diseases to avert the deleterious effects of the COVID-19 pandemic. Additionally, we can refer to current literature in order to inform our position. Interest has also arisen regarding vaccinating the pregnant and lactating mothers against COVID-19.
Lactating women who had been recently diagnosed with COVID-19 were enrolled into a study by Pace et al. (65) in which samples of their breast milk were investigated for SARS-CoV-2 RNA, specific (Immunoglobulin A) IgA and (Immunoglobulin G) IgG. SARS-CoV-2 RNA was not found in any of the 37 breast milk samples. But they contained specific IgA and IgG, and anti-RBD IgA (anti-Receptor Binding Protein IgA). The SARS-CoV-2 Receptor Binding Domain (RBD) has the function of attaching to the Angiotensin Converting Enzyme (ACE-2) receptor before the virus can infect the cell. So, preventing this step from happening by the activity of the anti-RBD IgA may offer protection against infection. Thus, breast milk has potentially protective properties against SARS-CoV-2 to the breastfed infant (65, 16, 4, 48). In a cohort study 285 samples of breast milk collected from 110 lactating mothers were analysed. 65 (59%) of the mothers had tested positive for SARS-COV-2 by nasal or nasopharyngeal swab SARS COV-2 RT-PCR (Reverse Transcriptase Polymerase Chain Reaction) test. 9 (8%) of the mothers were symptomatic but had negative diagnostic tests and 36 (33%) were symptomatic and were not tested. Notably infectious virus was not found in any of the cultures nor was any subgenomic viral RNA a putative marker for infectivity found (47). Another study (71) enrolled 50 pregnant women all of whom were SARS-COV-2 positive. Only expressed breast milk samples from 49 mothers were analysed as one neonate who was delivered by caesarean section at term demised from severe birth asphyxia 4 days after birth. By the 4th day of the peurperium, 1 sample was collected from each mother and all of the samples tested negative for SARS COV-2 by RT PCR. At 1 day of age all the neonates were screened for SARS-CoV-2 by nasopharyngeal swab RT-PCR test. 2 (4%) of the 51 neonates tested positive during which time they were fed on formula. They remained without exhibiting any symptom of the disease. All the breast milk samples were negative for the virus. Thus breast milk is an unlikely vehicle for transmission (71). And as yet, Mother to Child Transmission (MTCT) of COVID-19 through breast milk and breastfeeding has not been known (112, 113).
3.1. Potential risk of transmission during breastfeeding, overcame by benefits
Breast milk is the most suitable and ecological feed for the infant (44, 45, 114). Breastfeeding is an important step in mother-infant interaction, and is critical in neonatal early prognosis and growth. Breast milk is indispensable because it is sufficient to nourish and meet the energy needs of children entirely during the first six months of life, with its sufficiency gradually reducing thereafter to not less than half in the next six months (i.e., up to one year), and to a third up to two years of age. Thus, it is the best source of nutrition for infants (108, 109, 110, 111, 5, 84) and should therefore be continued until the child is at least 2 years old (58, 108, 109, 110, 111). Breastfeeding also protects the neonates, infants and children against morbidity and mortality (86). Breast milk also improves survival as it confers passive immunity to the infant as it is rich in immunoglobulins which are very effective against bacterial and viral infections as well as some cancers (23, 19, 84, 67. Breast milk also plays a critical role in the development of a healthy and balanced microbiome (44, 45). Initially there was reasonable concern about the possibility of transmission COVID-19 through breastfeeding because of viral RNA and other viral particles that can be found in breast milk (60, 118). In a study of 140 breastfeeding mothers, SARS-CoV-2 RNA was isolated in 20 (14.29%) of them (68, 35). Also, literature (68) reports that the incidence of vertical transmission is not non-existent but was reported to be about 4.2% when over 800 neonates were reviewed. Another study (79) of 42 asymptomatic SARS-CoV-2 positive pregnant women and their new born infants when they were born reported that 5 out of the 42 neonates (about 11.9%) had strong evidence for possible MTCT of SARS-CoV-2. This study used the WHO criteria for classification and timing of mother-to-child transmission of SARS-CoV-2. Therefore, the risk of vertical transmission should not be overlooked. There is also lacking strong scientific evidence to the effect that there is transmission of the virus through breast milk. This has been proven because the viral materials that can be found in the breast milk of mothers with SARS-CoV-2 are unlikely to be infectious. But breast milk is a likely lasting source of the anti-Receptor Binding Domain (anti-RBD) IgA thereby conferring passive immunity against COVID-19 (4, 60, 118). Breast milk also contains lactoferrin a cationic iron-binding glycoprotein present in mucosal secretions that posses broad-spectrum activity against both DNA and RNA viruses. Both in vivo and in silico studies have shown evidence of lactoferrin activity against SARS-CoV-2 (119, 120). Therefore, important societies like the WHO, UNICEF, and Centers for Disease Control and Prevention (CDC) endorse breastfeeding even during the COVID-19 pandemic albeit with caution that preventive measures should be adhered to. Additionally, they encourage that when it is feasible, the kangaroo mother care should also be practiced (117, 96, 10, 11, 64, 60). And it is important to note that children are less likely to be infected by the disease. This has been linked to the fact that children have low expression of the main receptor for the virus, the ACE-2 receptors (39, 17). And infants have a higher chance of recovery than adults. This is due to the excellent capacity of the epithelial cells of the lungs in children to regenerate, as well as, them not having risk factors like smoking and less physical activity (54, 74).
3.2. Breastfeeding practice and promotion in nursery and at home
The critical role that breastfeeding plays is beyond providing nutrition but also conferring passive immunity to the infant, therefore, breastfed infants are less prone to infectious diseases like diarrhoea and when they do suffer from these diseases they have better prognosis (87, 75, 64). Therefore, mothers and their families should be provided with appropriate information regarding safe breastfeeding during the pandemic (84). The mothers should also be taught the “Ten Steps to Successful Breastfeeding” as part of the Baby-Friendly Hospital Initiative (BFHI) which is supported being important societies like the CDC (84). Initiation of breastfeeding should still happen within the 1st hour of birth even during the pandemic (67).
Globally, the percentages of infants being breastfed still need to be improved upon. According to the WHO between 2013 and 2018 only 43% of new born infants initiate breastfeeding within one hour of birth. Only 41% of infants under the age of six months are breastfed exclusively. And only 45% of children are breastfed at the time they are two years of age (87, 98). Due to the many benefits of breastfeeding, the practice should be encouraged and promoted among all lactating women, as well as among expectant mothers. The recommendations of the WHO and UNICEF (42), are that;
i. Breastfeeding should be initiated not more than 1 h after birth;
ii. The infant should be breastfed exclusively until 6 months of age;
iii. Beginning at 6 months of age the infant should be introduced to other foods that are safe and adequate in nutrition while breastfeeding should be continued for not less than 2 years
The above recommendations need to be emphasized because of some of the reported effects of the pandemic on lactation support and breastfeeding rates. These include keeping the mother-infant dyad separated from the rest of the family and other social support networks which reduces available lactation support. Accelerated post-delivery discharges, coupled with reduction of in-person lactation support may also lead to mothers not achieving their breastfeeding targets (24). It has been reported by another study (83) that the first time mothers were the most affected especially during the hours and days after delivery when breastfeeding had not yet been established.
3.3. Breastfeeding promotion in neonatal intensive care unit (NICU)
The importance of breastfeeding is even higher for neonates born preterm or premature. Despite that, the rates of breastfeeding are even lower in the Neonatal Intensive Care Unit (NICU) setting. Owing to the many benefits of breastfeeding to the premature neonates, breastfeeding should be encouraged in the NICU. Breastfeeding in the Neonatal Intensive Care Unit (NICU) can be promoted by among others the following ways (33, 57, 36);
i. Family-centred approach
ii. Skin-to-skin contact –kangaroo mother care
iii. Early and frequently expressing breast milk from both breasts; and
iv. Support from peers
v. Lactation counselling
vi. Involving mothers in the care of neonate admitted to the NICU
vii. Use of human donor breast milk
In the event that the milk from the mother is unavailable, human donor breast milk from milk banks can be used. Because it is pasteurized, human donor breast milk has reduced bioavailability than mother's breast milk and may therefore be used only until the mother's breast milk is available (1, 66). Despite a reduction in bioavailability, human donor breast milk is befitting substitute as it effectively inactivates the SARS-CoV-2 virus (95, 85, 64).
3.4. Breastfeeding when mother is affected
When a mother has COVID-19 she should breastfeed while adhering to COVID-19 guidelines. She can also express her own breast milk and safely feed it to the infant herself (84). But in the event that a mother is unable to breastfeed because of being very ill, she should be supported by a healthy caregiver by for example, feeding the infant with milk that has been expressed from the mother's breast. If this is not feasible, human donor breast milk sourced from milk banks can also be used. Even in such situations, safety precautions aimed at reducing the risk of transmission of the virus should be followed, among them (93, 64, 10, 11, 69, 60);
i. The caregiver should be healthy and without COVID-19, not exhibiting any of the symptoms of the disease, and preferably vaccinated.
ii. A clean breast pump (preferably a dedicated breast pump), if possible should be used.
iii. The caregiver should wash hands using soap and water prior to touching any pump, bottle parts, or the mother’s breast.
iv. The mother’s breast should also be washed before and after expressing the milk.
v. Wear a mask while administering the breast milk and whenever within 2 m of the baby.
vi. Wear a mask during expression.
vii. Proper pump cleaning after use.
Breastfeeding should be initiated and conducted normally with rooming in starting within the 1st hour of birth. The appropriate breastfeeding technique which includes mother holding the baby skin-to-skin should be encouraged. Further, uninterrupted exclusive breastfeeding for the first six months is encouraged. Thereafter breastfeeding should continue up to the age of two years or beyond, alongside other feeds (67).
4. COVID-19 in the neonate
Dhir et al. (26) reported that fewer children than adults have been infected by the disease confirmed by RT-PCR, and that they have excellent prognosis. The infection in neonates most often sets in in the postpartum period, with 2/3 being symptomatic. Because most of the neonates are reported to be well prior to the onset of symptoms of the disease implies that the symptoms are not due to non-COVID causes such as prematurity but are due to the infection itself. The occurrence of the disease in neonates is very infrequent.
But regarding severity of the disease in this age group, Dhir et al. (26) reported that it is more severe in neonates than in older children because when affected the former are more likely to require NICU admission than the latter. And according to Leung (51) neonates run a more severe clinical course with shorter time between symptom onset to death, long duration to being symptom-free and to being discharged. Whereas Kyle et al. (49) report that the course of the disease in neonates is usually mild. Similarly, in their journal article, De Bernardo et al. (21) reported that COVID-19 in neonates showed a good prognosis, with severe complications and death being rare. Further, other studies reported that infection in the neonatal period runs a mild course and that the outcome is favourable (43, 30, 31, 53). Furthermore, the WHO Scientific brief of 8th February 2021 (108–111) stated that neonatal infection of SARS-CoV-2 usually presents with non-severe symptoms.
In order to be certain about vertical transmission a neonate should be tested more than once and a positive test should be confirmed with a molecular test, RT PCR. Because maternal IgG unlike maternal IgM crosses the placenta, IgG should not be used to diagnose infection in the neonate. Instead a positive IgM test in a neonate aged at least one week old should raise suspicion for neonatal infection. Positive SARS-CoV-2 test in a neonate under the age of one week is most likely representative of maternal infection. But negative IgM at age less than one week followed by positive test after age of one week represents active infection. Because the sensitivity and specificity of a positive IgM test is variable and less reliable than that of PCR, so positive serological test (IgM) should be followed by a molecular test (PCR). However, care should be taken in interpreting a positive RT-PCR test result because it may indicate at least one of the following possibilities; active infection, contamination with viral fragments during vaginal delivery or from the environment. Therefore, a positive PCR test should be repeated and also tested on normally sterile body fluids such as cerebrospinal fluid to further confirm the diagnosis (7, 9). To date, there has been no report in literature of detection of SARS-CoV-2 in amniotic fluid and breast milk (84). And de Medeiros et al. (22) further report that the absence of evidence to support the presence of the virus in the amniotic fluid, placenta, umbilical cord and breast milk of the expectant mothers points to the unlikelihood of vertical transmission of the infection.
Therefore, the risk of vertical or horizontal transmission of SARS-CoV-2 from the mother to the neonate is low (41, 99–107, 60, 114).
5. Precautions to take during breastfeeding
Generally all children, and more specifically neonates, infants and toddlers should be handled with extra care during this period of the pandemic so as to reduce the risk of transmission. More caution should be exercised if there is risk of transmission.
A woman with COVID-19 can and should be encouraged to breastfeed, as long as necessary precautions are taken, including (99–107, 61):
i. Wearing a face mask correctly and consistently.
ii. Washing hands with soap and water or use alcohol-based hand sanitizer.
iii. Routinely cleaning and disinfecting surfaces.
Adherence to the above listed precautions is important because enhanced hygiene is a proven measure of limiting the risk for transmission. Additionally, breast hygiene is to be practiced in order to reduce the risk of transmission.
6. Breastfeeding and vaccination
COVID-19 vaccine has emerged as one of the most effective methods of primary prevention of COVID-19 (38, 97). There are several brands of the COVID-19 vaccine available on the international market (32, 27). Vaccines typically work on the same principle; stimulating the immune response to weakend or inactivated parts of a particular antigen (32, 99–107). By so doing a vaccine stimulates the immune system to produce antibodies, similar to how it would if you were infected. After invading the cell, the agent is recognised as foreign material by the immune system which develops specific immune response against it. In the event of future exposure to the natural antigen, the body produces a more robust and quick immune response that would have otherwise not been produced (37, 18). In this way, therefore, vaccines prevent diseases caused by a large number of viruses, which could even have been fatal in the absence of vaccination as the body's immune system could not have mounted an adequate immune response.
Because lactating mothers were initially excluded from clinical trials much data regarding COVID-19 vaccines and breastfeeding are lacking. Because of the same reason, data on which to base decision making in this population is also not as available (34). But it is safe to vaccinate breastfeeding women (8) and/or their infants as the non-replicating vaccines which are now authorized for use do not reproduce inside host cells. Therefore several important societies advise that lactating women can be offered the vaccine as long as they are otherwise eligible, with the American College of Obstetricians and Gynecologists (ACOG) and United Nations Children's Fund (UNICEF) among others stating that there is no need to interrupt breastfeeding after vaccination (92, 12–14, 20). Therefore, lactating women may choose to be vaccinated. And there is no contraindication to the administration of this vaccine alongside other vaccines that are otherwise routinely administered in pregnancy (70). A prospective cohort study by Gray KJ et al. (34) enrolled 131 women of reproductive age who had been vaccinated. Of the 131 women, 84 (64%) were pregnant, 31 (24%) were lactating, and 16 (12%) were non-pregnant. The study reviewed that “COVID-19 mRNA vaccines” caused a “robust humoral immunity” with comparable results in all the subjects irrespective of their pregnancy status. Furthermore, the study reviewed that the immunity arising from vaccination was of more robustness than that which was naturally occurring.
There have been no differences in the side effects arising from vaccination observed in the pregnant and the non-pregnant populations; also there have been no safety concerns from the CDC v-safe post-administration surveillance data (12–14). Furthermore, more evidence is becoming available to support the safety of COVID vaccination in pregnancy (12–14, 94). Although eligible to be vaccinated against SARS-CoV-2, pregnant women should be encouraged to minimize contact with other people. This is in order for them to reduce their chances of exposure to persons with SARS-CoV-2 infection, and to reduce their chances of contracting the infection. Despite the ACOG's (70) encouraging vaccination of pregnant women in any trimester of pregnancy, precaution should also be taken if the vaccine is to be administered during the first trimester. This is because of the likelihood of vaccine reactogenicity of which fever is the most important because it can potentially raise the risk of congenital malformations such as neural tube defects (73).
Although the COVID vaccines are a pivotal component of the COVID response globally, there is currently no basis to offer them to neonates because they were not included in clinical trials. And because neonates have both innate and adaptive immune systems that are still developing, they have poor immunogenicity and are not likely to generate adequate immune response to the vaccine (77, 96). Therefore, women who are planning to get pregnant can be encouraged to get vaccinated so that they can generate a sufficient repertoire of immunoglobulins to pass to the foetus when they get pregnant and confer passive immunity to neonate (96, 50). But this should be done with the caution already discussed above; to avoid administration of the vaccine in the first trimester. Because of their being a higher risk of potentially more severe disease and mortality from COVID-19 infection during pregnancy and that immunity from primary vaccine can wear off, the ACOG recommends that pregnant women and those in the puerperal period (≤6 weeks after delivery) should receive a bilavent mRNA booster vaccination not before 2 months after receiving their first dose or monovalent booster have elapsed (70). Significant increase in neutralizing SARS-CoV-2 specific antibodies in breast milk has been detected following COVID-19 vaccination similar to the phenomenon that occurs as after infection. It has therefore been suggested that these antibodies are passed on to the infant during breastfeeding. This is because the same antibodies have been identified in the stools of the infants 6 months after vaccination despite decrease in antibody levels (80).
Despite the foregoing evidence regarding the benefits of vaccinating both the pregnant and breastfeeding women to both the women themselves and the infants, there is vaccine hesitancy particularly against the COVID-19 vaccine than the other vaccines. Therefore, there is need for the health care providers to be aware of this and work to dispel the false information regarding COVID-19 vaccines and promote vaccination against COVID-19 (67).
7. Evolution of COVID-19 guidelines over time
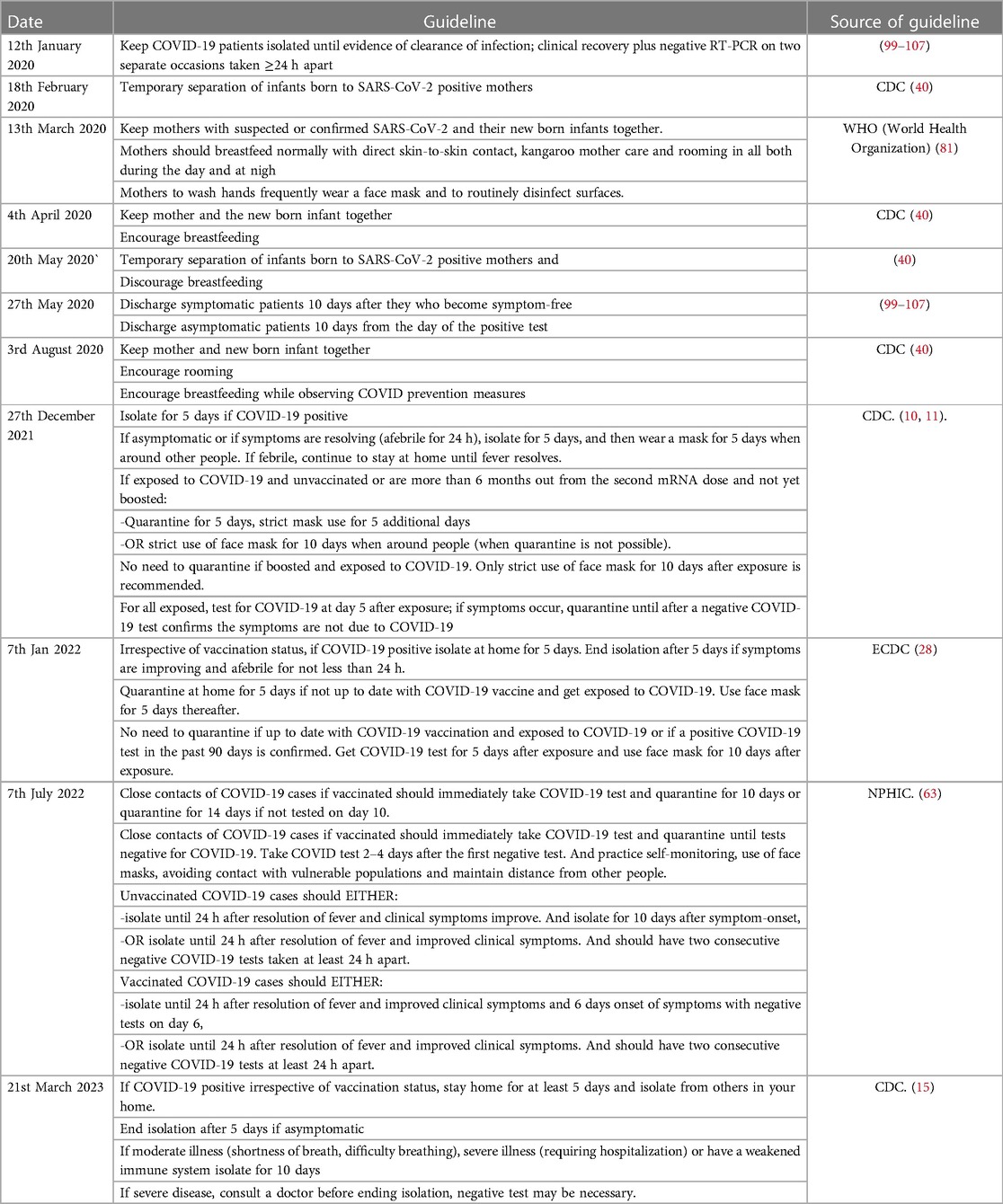
The COVID-19 guidelines in general and those particularly concerned with prevention of the disease in young children have undergone several changes over time. For example on 18th February 2020 the CDC (40) published the guidelines that recommended that infants born to COVID-19 positive mothers should be temporarily separated from their mothers until they were negative. During the period of temporary separation milk expressed from the mother's breast was to be fed to the infant by healthy caregivers. 2 months after that, on 4th April of the same year the CDC guidelines promoted keeping the mother and the new born infant together and to continue breastfeeding. But their update would on 20th May 2020 change back to discouraging keeping the COVID-19 positive mother and her new born infant together and breastfeeding. Finally, on the 3rd August 2020, their guidelines were again changed to encourage the practice of rooming in and breastfeeding while observing COVID prevention measures. The guidelines regarding isolation of COVID patients have also undergone changes. The WHO guideline published on 12th January 2020 (99–107) recommended that there was supposed to be evidence of clearance of the virus before a patient could be discharged from isolation. This was to be proven by clinical recovery and having negative RT-PCR results on two separate occasions taken not less than 24 h apart. But with new scientific evidence becoming available, the updated guidelines published on 27th May 2020 recommended that patients could be discharged from isolation if they are symptom-free for 10 days after the start of initial symptoms (for symptomatic patients) and 10 days after testing positive for SARS-CoV-2 for asymptomatic cases. The WHO (81, 99–107) has maintained the guidance given on 13th March 2020 that new born infants of mothers with suspected or confirmed COVID-19 should not be separated from their mothers. But that they should remain with their mothers, breastfed normally with direct skin-to-skin contact, kangaroo mother care and rooming in all through the day and night further encouraged. During the period that they remain COVID-19 positive, mothers are encouraged to adhere to wash hands frequently, wear a face mask and to routinely disinfect surfaces. Breastfeeding is strongly recommended given its known lifelong importance for maternal and child health.
8. Conclusion
It is more beneficial to breastfeed than not to even during the pandemic as it is unlikely that breast milk would be the vector for MTCT of COVID-19. Breast milk also offers the best innate immunity to the growing infant. Therefore, safe breastfeeding should be encouraged, with necessary precautions so that there is no transmission from the mother to the infant. Pregnant and lactating women can also choose to get vaccinated against the SARS-CoV-2. Vaccinating this group of women may even prove beneficial to their infants because passive immunity can be conferred on to the fetus in utero by trans-placental passage of the vaccine induced antibodies, and ex utero via breast milk (postpartum).
8.1. Weaknesses
The weaknesses of this review are that some issues such as the timing of vaccination of pregnant mothers that may be controversial have not been fully clarified. Additionally, most of the information is not readily available currently because the COVID-19 is a new disease. It would therefore be important for further research to study the possibility of vaccinating children, efficacy and safety of COVID-19 vaccines in children and the most appropriate timings for vaccinating pregnant and lactating mothers. It would also be important for the studies to be conducted with bigger sample sizes and in multiple sites.
Author contributions
BMC: was the main author. X-QC: reviewed the manuscript and provided mentorship. All authors contributed to the article and approved the submitted version.
Funding
The present study was supported by national natural Scientific (Grant no. 81871195) and by Jiangsu Provincial maternity and child health key talents.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. AAP. Donor Human Milk for the High-Risk Infant: Preparation, Safety, and Usage Options in the United States (2017). Available at: https://publications.aap.org/pediatrics/article/139/1/e20163440/52000/Donor-Human-Milk-for-the-High-Risk-Infant (Accessed 5 September 2022).
2. ACOG. COVID-19 Vaccines: Answers From Ob-Gyns (2022). Available at: https://www.acog.org/womens-health/faqs/covid-19-vaccines-answers-from-ob-gyns (Accessed 30 October 2022).
3. ACOG. COVID-19 Vaccination Considerations for Obstetric–Gynecologic Care (2023). Available at: https://www.acog.org/clinical/clinical-guidance/practice-advisory/articles/2020/12/covid-19-vaccination-considerations-for-obstetric-gynecologic-care (Accessed 10 January 2023).
4. Afewerky HK. Pathology and pathogenicity of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). Exp Biol Med. (2020) 245:1299–1307. doi: 10.1177/1535370220942126. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7441345/ (Accessed 4 August 2022).
5. Agne-Djigo A, Kwadjode KM, Idohou-Dossou N, Diouf A, Guiro AT, Wade S. Energy intake from human milk covers the requirement of 6-month-old Senegalese exclusively breast-fed infants. Br J Nutr. (2013) 110:1849–55. doi: 10.1017/S0007114513001074. Available at: https://www.cambridge.org/core/journals/british-journal-of-nutrition/article/energy-intake-from-human-milk-covers-the-requirement-of-6monthold-senegalese-exclusively-breastfed-infants/DA90EDDC6E820DA71EE25CAB8281F446 (Accessed 29 October 2022).23578434
6. Anastassopoulou C, Spanakis N, Tsakris A. SARS-CoV-2 transmission, the ambiguous role of children and considerations for the reopening of schools in the fall. Future Microbiol. (2020) 15:1201–1206. doi: 10.2217/fmb-2020-0195. Available at: https://www.futuremedicine.com/doi/full/10.2217/fmb-2020-0195?rfr_dat=cr_pub++0pubmed&url_ver=Z39.88-2003&rfr_id=ori%3Arid%3Acrossref.org (Accessed 11 October 2022).32878481
7. Auriti C, De Rose DU, Mondì V, Stolfi I, Tzialla C. Neonatal SARS-CoV-2 infection: practical tips. Pathogens. (2021) 10:611. doi: 10.3390/pathogens10050611. Available at: https://www.mdpi.com/2076-0817/10/5/611 (Accessed 4 July 2022).34067588
8. Bianchi DW, Kaeser L, Cernich AN. Involving pregnant individuals in clinical research on COVID-19 vaccines. JAMA. (2021) 325:1041–1042. doi: 10.1001/jama.2021.1865. Available at: https://jamanetwork.com/journals/jama/fullarticle/2776540 (Accessed 8 October 2022).33566088
9. Blumberg DA, Underwood MA, Hedriana HL, Lakshminrusimha S. Vertical transmission of SARS-CoV-2: what is the optimal definition? Am J Perinatol. (2020) 37:769–772. doi: 10.1055/s-0040-1712457. Available at: https://www.thieme-connect.com/products/ejournals/abstract/10.1055/s-0040-1712457?device=mobile&innerWidth=720&offsetWidth=412 (Accessed 20 December 2022).
10. CDC. Care for Breastfeeding People (2021). Available at: https://www.cdc.gov/coronavirus/2019-ncov/hcp/care-for-breastfeeding-women.html (Accessed 4 July 2022).
11. CDC. CDC Updates and Shortens Recommended Isolation and Quarantine Period for General Population (2021). Available at: https://www.cdc.gov/media/releases/2021/s1227-isolation-quarantine-guidance.html (Accessed 17 April 2023).
12. CDC. Care for Breastfeeding People (2022). Available at: https://www.cdc.gov/coronavirus/2019-ncov/hcp/care-for-breastfeeding-women.html (Accessed 12 October 2022).
13. CDC. COVID-19 vaccines, pregnancy and breastfeeding FAQs (2022). Available at: https://www.rcog.org.uk/guidance/coronavirus-covid-19-pregnancy-and-women-s-health/vaccination/covid-19-vaccines-pregnancy-and-breastfeeding-faqs/#:∼:text=There%20is%20no%20plausible%20mechanism,be%20vaccinated%20against%20COVID%2D19 (Accessed 30 October 2022).
14. CDC. V-safe Pregnancy Registry (2022). Available at: https://www.cdc.gov/coronavirus/2019-ncov/vaccines/safety/vsafepregnancyregistry.html (Accessed 10 January 2023).
15. CDC. Isolation and Precautions for People with COVID-19 (2023). Available at: https://www.cdc.gov/coronavirus/2019-ncov/your-health/isolation.html (Accessed 12 April 2023).
16. Chaouat AE, Achdout H, Kol I, Berhani O, Roi G, Vitner EB, et al. SARS-CoV-2 receptor binding domain fusion protein efficiently neutralizes virus infection. PLoS Pathog. (2021) 17:1–18. doi: 10.1371/journal.ppat.1010175. Available at: https://journals.plos.org/plospathogens/article?id=10.1371/journal.ppat.1010175 (Accessed 29 Dec 2022).
17. Choi JH, Choi SH, Yun KW. Risk factors for severity in children with COVID-19: a systematic review and meta-analysis. J Korean Med Sci. (2022) 37:1–14. doi: 10.3346/jkms.2022.37.e35. Available at: https://pubmed.ncbi.nlm.nih.gov/35132841/ (Accessed 3 January 2023).
18. Cromer D, Steain M, Reynaldi A, Schlub TE, Wheatley AK, Juno JA, et al. Neutralising antibody titres as predictors of protection against SARS-CoV-2 variants and the impact of boosting: a meta-analysis. Lancet Microbe. (2021) 3:e52–e61. doi: 10.1016/S2666-5247(21)00267. Available at: https://www.thelancet.com/journals/lanmic/article/PIIS2666-5247(21)00267-6/fulltext (Accessed 2 March 2022).34806056
19. Czosnykowska-Łukacka M, Lis-Kuberka J, Królak-Olejnik B, Orczyk-Pawiłowicz M. Changes in human milk immunoglobulin profile during prolonged lactation. Front Pediatr. (2020) 8:1–12. doi: 10.3389/fped.2020.00428. Available at: https://www.frontiersin.org/articles/10.3389/fped.2020.00428/full (Accessed 8 Feb 2021).
20. Davanzo R, Agosti M, Cetin I, Chiantera A, Corsello G, Ramenghi LA, et al. Breastfeeding and COVID-19 vaccination: position statement of the Italian scientific societies. Ital J Pediatr. (2021) 47:1–4. doi: 10.1186/s13052-021-00998-6. Available at: https://ijponline.biomedcentral.com/articles/10.1186/s13052-021-00998-6#citeas (Accessed 3 February 2022).33407754
21. De Bernardo G. The clinical course of SARS-CoV-2 positive neonates. J Perinatol. (2020) 40:1462–1469. doi: 10.1038/s41372-020-0715-0. Available at: https://www.nature.com/articles/s41372-020-0715-0 (Accessed 5 May 2021).32632198
22. de Medeiros KS, Sarmento ACA, Costa APF, Macêdo LTA, da Silva LAS, de Freitas CL, et al. Consequences and implications of the coronavirus disease (COVID-19) on pregnancy and newborns: a comprehensive systematic review and meta-analysis. J Perinatol. (2021) 156:394–405. doi: 10.1002/ijgo.14015. Available at: https://www.nature.com/articles/s41372-020-0715-0 (Accessed 19 January 2022).
23. Demers-Mathieu V. Comparison of Human Milk Immunoglobulin Survival during Gastric Digestion between Preterm and Term Infants (2018). ResearchGate. Available at: https://www.researchgate.net/publication/325203134_Comparison_of_Human_Milk_Immunoglobulin_Survival_during_Gastric_Digestion_between_Preterm_and_Term_Infants (Accessed 7 April 2022).
24. DeYoreo M, Kapinos K, Lawrence R, Alvarado G, Waymouth M, Demirci JR, et al. Changes in breastfeeding and lactation support experiences during COVID. J Womens Healt. (2023) 32:150–160. doi: 10.1089/jwh.2022.0146. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9940799/ (Accessed 12 April 2023).
25. Dhama K, Patel SK, Sharun K, Pathak M, Tiwari R, Yatoo MI, et al. SARS-CoV-2 jumping the species barrier: Zoonotic lessons from SARS, MERS and recent advances to combat this pandemic virus (2020). ScienceDirect. Available at: https://www.sciencedirect.com/science/article/pii/S1477893920303264 (Accessed 8 December 2021).
26. Dhir SK, Kumar J, Meena J, Kumar P. Clinical features and outcome of SARS-CoV-2 infection in neonates: a systematic review. J Trop Pediatr. (2020) 67:1–14. doi: 10.1093/tropej/fmaa059. Available at: https://academic.oup.com/tropej/article/67/3/fmaa059/5898408?login=false (Accessed 16 April 2023).
27. Earle KA, et al. Evidence for antibody as a protective correlate for COVID-19 vaccines (2021). ScienceDirect. Available at: https://www.sciencedirect.com/science/article/pii/S0264410×21006587 (Accessed 16 April 2023).
28. ECDC. Guidance on quarantine of close contacts to COVID-19 cases and isolation of COVID-19 cases (2022). Available at: https://www.ecdc.europa.eu/en/covid-19/prevention-and-control/quarantine-and-isolation (Accessed 18 April 2023).
29. Ellis P, Somogyvári F, Virok DP, Noseda M, McLean GR. Decoding Covid-19 with the SARS-CoV-2 Genome (2021). ResearchGate. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7794078/ (Accessed 17 August 2022).
30. Gabriel MAM, Vergeli RM, Carbonero CS, Sole L, Molina CT, Calle RI, et al. Maternal, perinatal and neonatal outcomes with COVID-19: a multicenter study of 242 pregnancies and their 248 infant newborns during their first month of life. Pediatr Infect Dis J. (2020) 39:e393–e397. doi: 10.1097/INF.0000000000002902. Available at: https://pubmed.ncbi.nlm.nih.gov/32947599/ (Accessed 17 August 2022).32947599
31. Gale C, Quigley MA, Placzek A, Knight M, Ladhani S, Draper ES, et al. Characteristics and outcomes of neonatal SARS-CoV-2 infection in the UK: a prospective national cohort study using active surveillance. Lancet. (2021) 5:113–121. doi: 10.1016/S2352-4642(20)30342-4. Available at: https://www.thelancet.com/journals/lanchi/article/PIIS2352-4642(20)30342-4/fulltext (Accessed 11 May 2022).
32. Gavi. VaccinesWork (2021). Available at: https://www.gavi.org/vaccineswork/there-are-four-types-covid-19-vaccines-heres-how-they-work?gclid=EAIaIQobChMIienNnPPz-gIVIoBQBh308QjGEAAYASAAEgL8xfD_BwE (Accessed 29 October 2022).
33. Gianni ML, Bezze EN, Sannino P, Baro M, Roggero P, Muscolo S, et al. Maternal views on facilitators of and barriers to breastfeeding preterm infants. ResearchGate (2018). Available at: https://www.researchgate.net/publication/327256787_Maternal_views_on_facilitators_of_and_barriers_to_breastfeeding_preterm_infants (Accessed 16 November 2022).
34. Gray KJ, Bordt EA, Atyeo C, Deriso E, Akinwunmi B, Young N, et al. Coronavirus disease 2019 vaccine response in pregnant and lactating women: a cohort study. Am J Obstet Gynecol. (2021) 225:303.e1–303.e17. doi: 10.1016/j.ajog.2021.03.023. Available at: https://pubmed.ncbi.nlm.nih.gov/33775692/ (Accessed 25 January 2022).33775692
35. Groß R, Conzelmann C, Müller JA, Stenger S, Steinhart K, Kirchhoff F, et al. Detection of SARS-CoV-2 in human breastmilk. Lancet. (2020) 395:1757–1758. doi: 10.1016/S0140-6736(20)31181-8. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7241971/ (Accessed 9 August 2022).
36. Gupta S, Parish T. Optimizing own mother’s milk supply for NICU babies. J Neonatol. (2020) 34:83–87. doi: 10.1177/0973217920922398. Available at: https://journals.sagepub.com/doi/full/10.1177/0973217920922398 (Accessed 24 November 2022).
37. Heinz FX, Stiasny K. Distinguishing features of current COVID-19 vaccines: knowns and unknowns of antigen presentation and modes of action. J Perinatol. (2021) 6:1–13. doi: 10.1038/s41541-021-00369-6. Available at: https://journals.sagepub.com/doi/full/10.1177/0973217920922398 (Accessed 22 December 2022).
38. Higdon MM, Wahl B, Jones CB, Rosen JG, Truelove SA, Baidya A, et al. A systematic review of coronavirus disease 2019 vaccine efficacy and effectiveness against severe acute respiratory syndrome coronavirus 2 infection and disease. Am J Infect Dis. (2021) 9:1–19. doi: 10.1093/ofid/ofac138. Available at: https://journals.sagepub.com/doi/full/10.1177/0973217920922398 (Accessed 14 July 2022).
39. Hoffmann M, Kleine-Weber H, Schroeder S, Krüger N, Herrler N, Erichsen S, et al. SARS-CoV-2 cell entry Depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor. Cell. (2020) 2020:271–8. doi: 10.1016/j.cell.2020.02.052
40. Hoang DV, Cashin J, Gribble K, Marinelli K, Mathisen R. Misalignment of global COVID-19 breastfeeding and newborn care guidelines with world health organization recommendations. BMJ Nutr Prev Health. (2020) 3:339–350. doi: 10.1136/bmjnph-2020-000184. Available at: https://nutrition.bmj.com/content/early/2020/12/21/bmjnph-2020-000184 (Accessed 26 July 2022).33521544
41. Ibrahim CPH, Lobko FO, Alchamat GA, Swilam WG, Wani SR, Said ST, et al. Management of infants born to mothers with SARS-CoV2 infection: a prospective observational study. BMJ Paediatr Open. (2020) 4:1–5. doi: 10.1136/bmjpo-2020-000824. Available at: https://bmjpaedsopen.bmj.com/content/4/1/e000824 (Accessed 8 June 2022).
42. Infant and young child feeding. (2021). Available at: https://www.who.int/news-room/fact-sheets/detail/infant-and-young-child-feeding (Accessed July 14, 2022).
43. Karabay M, Çınar N, Suzan ÖK, Çaka SK, Karabay O. Clinical characteristics of confirmed COVID-19 in newborns: a systematic review. J Matern Fetal Neonatal Med. (2022) 35:4386–4397. doi: 10.1080/14767058.2020.1849124. Available at: https://pubmed.ncbi.nlm.nih.gov/33213230/ (Accessed 31 December 2022).33213230
44. Kim SY, Yi DY. Analysis of the human breast milk microbiome and bacterial extracellular vesicles in healthy mothers. Exp Mol Med. (2020) 52:1288–1297. doi: 10.1038/s12276-020-0470-5. Available at: https://www.nature.com/articles/s12276-020-0470-5 (Accessed 16 April 2023).32747701
45. Kim D, Lee JY, Yang JS, Kim JW, Kim VN, Chang H, et al. The architecture of SARS-CoV-2 transcriptome. Cell. (2020) 181:914–921. doi: 10.1016/j.cell.2020.04.011. Available at: https://www.google.com/url?sa=t&source=web&rct=j&url=https://www.cell.com/cell/pdf/S0092-8674(20)30406-2.pdf&ved=2ahUKEwjBxPelv6z-AhXTNcAKHSh5BIIQFnoECA4QAQ&authuser=1&usg=AOvVaw2C1OogT82VWQj6tECxSsPm (Accessed 16 April 2023).32330414
46. Kirubananthan L, Illuri R, Rajendran R, Chandrasekaran PR. Mechanism and transmission routes of COVID-19. Elsevier Public Health Emerg Collect. (2021):65–88. doi: 10.1016/B978-0-323-85780-2.00013-5. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8237516/ (Accessed 28 April 2022).
47. Krogstad P, Contreras D, Ng H, Tobin N, Chambers CD, Bertrand K, et al. No infectious SARS-CoV-2 in breast milk from a cohort of 110 lactating women. Pediatr Res. (2021) 92:1140–1145. doi: 10.1038/s41390-021-01902-y. Available at: https://www.nature.com/articles/s41390-021-01902-y (Accessed 6 October 2022).
48. Kyle MH, Dumitriu D. Morphology, Genome Organization, Replication, and Pathogenesis of Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) (2020). Springer. Available at: https://link.springer.com/chapter/10.1007/978-981-15-4814-7_3#citeas (Accessed 24 February 2022).
49. Kyle MH, Dumitriu D. The effect of coronavirus disease 2019 on newborns. Curr Opin Pediatr. (2021) 33:618–624. doi: 10.1097/MOP.0000000000001063. Available at: https://pubmed.ncbi.nlm.nih.gov/34561359/ (Accessed 18 January 2022).34561359
50. Lechosa-Muñiz C, Paz-Zulueta M, Irure-Ventura J, Mendez-Legaza JM, González RC, Gómez-Acebo I, et al. Development of SARS-CoV-2 specific IgG and IgA antibodies in serum and milk with different SARS-CoV-2 vaccines in lactating women. Int Breastfeed J. (2023) 18:1–10. doi: 10.1186/s13006-022-00536-y. Available at: https://internationalbreastfeedingjournal.biomedcentral.com/articles/10.1186/s13006-020-00536-y (Accessed 14 April 2023).
51. Leung C. The younger the milder clinical course of COVID-19: even in newborns? Pediatr Allergy Immunol. (2020) 32:358–362. doi: 10.1111/pai.13371. Available at: https://onlinelibrary.wiley.com/doi/10.1111/pai.13371 (Accessed 2 October 2022).32931058
52. Li X, Chang J, Chen S, Wang L, Yau TO, Zhao Q, et al. Genomic feature analysis of betacoronavirus provides insights into SARS and COVID-19 pandemics. Front Microbiol. (2021) 12:1–10. doi: 10.3389/fmicb.2021.614494. Available at: https://www.frontiersin.org/articles/10.3389/fmicb.2021.614494/full (Accessed 27 August 2022).
53. Lim KH, Soong FSJ, Low YF, Goh XL, Amin Z, Ng YPM Clinical features and outcomes of neonatal COVID-19: a systematic review. J Clin Virol. (2021) 139:2–4. doi: 10.1016/j.jcv.2021.104819. Available at: https://www.sciencedirect.com/science/article/pii/S138665322100086X?via%3Dihub (Accessed 20 June 2022).
54. Lingappan K, Karmouty-Quintana H, Davies J, Akkanti B, Harting MT Understanding the age divide in COVID-19: why are children. Am J Physiol - Lung Cell Mol Physiol. (2020) 319:L39–L44. doi: 10.1152/ajplung.00183.2020. Available at: https://journals.physiology.org/doi/full/10.1152/ajplung.00183.2020 (Accessed 8 May 2021).32491949
55. Lotfi M, Hamblin MR, Rezaei N. COVID-19: transmission, prevention, and potential therapeutic opportunities. Clin Chim Acta. (2020) 508:254–266. doi: 10.1016/j.cca.2020.05.044. Available at: https://www.sciencedirect.com/science/article/pii/S0009898120302503 (Accessed 7 July 2023).32474009
56. Lubbe W, Botha E, Niela-Vilen H, Reimers P. Breastfeeding during the COVID-19. Int Breastfeed J. (2020) 15:1–9. doi: 10.1186/s13006-020-00319-3. Available at: https://internationalbreastfeedingjournal.biomedcentral.com/articles/10.1186/s13006-020-00319-3 (Accessed 1 December 2022).31921327
57. Maastrup R, Hansen BM, Kronborg H, Bojesen SN, Hallum K, Frandsen A, et al. Breastfeeding progression in preterm infants is influenced by factors in infants, mothers and clinical practice: the results of a national cohort study with high breastfeeding initiation rates. PLoS One. (2014) 9:1–14. doi: 10.1371/journal.pone.0108208. Available at: https://pubmed.ncbi.nlm.nih.gov/25251690/ (Accessed 6 April 2022).
58. Meek and Noble. Policy statement: breastfeeding and the use of human milk. Am Acad Pediatr. (2022) 150:1–15. doi: 10.1542/peds.2022-057988. Available at: https://publications.aap.org/pediatrics/article/150/1/e2022057988/188347/Policy-Statement-Breastfeeding-and-the-Use-of?autologincheck=redirected (Accessed 24 January 2023).
59. Michel CJ, Mayer C, Poch O, Thompson JD. Characterization of accessory genes in coronavirus genomes. Virol J. (2020) 17:1–13. doi: 10.1186/s12985-020-01402-1. Available at: https://virologyj.biomedcentral.com/articles/10.1186/s12985-020-01402-1 (Accessed 20 July 2022).31906972
60. Minckas N, Medvedev MM, Adejuyigbe EA, Brotherton H, Chellani H, Estifanos AS, et al. Preterm care during the COVID-19 pandemic: a comparative risk analysis of neonatal deaths averted by kangaroo mother care versus mortality due to SARS-CoV-2 infection. Lancet. (2021) 33:1–8. doi: 10.1016/j.eclinm.2021.100733. Available at: https://www.thelancet.com/journals/eclinm/article/PIIS2589-5370(21)00013-4/fulltext (Accessed 2 February 2023).
61. Narvey and Finan. Care considerations for infants born to mothers with suspected or confirmed SARS-CoV-2 infection. Can Paediatr Soc. (2023) 17:317–321, Available at: https://cps.ca/en/documents/position/infants-born-to-mothers-with-COVID (Accessed 1 March 2023).
62. Ng YPM, Low YF, Goh XL, Fok D, Amin Z Breastfeeding in COVID-19: a pragmatic approach. Am J Perinatol. (2020) 37:1377–1384. doi: 10.1055/s-0040-1716506. Available at: https://pubmed.ncbi.nlm.nih.gov/32898920/ (Accessed 1 August 2022).32898920
63. NPHIC. Test positive for COVID-19? What Is the Current Isolation Guidance from the CDC? (2022). Available at: https://www.nphic.org/blog/931-test-positive-for-covid-19-what-is-the-current-isolation-guidance-from-the-cdc (Accessed 21 April 2023).
64. Olonan-Jusi E. Human milk banks in the response to COVID-19: a statement of the regional human milk bank network for Southeast Asia and beyond. Int Breastfeed J. (2021) 16:1–6. doi: 10.1186/s13006-021-00376-2. Available at: https://internationalbreastfeedingjournal.biomedcentral.com/articles/10.1186/s13006-021-00376-2 (Accessed 22 January 2023).33397426
65. Pace RM, Williams JE, Jarvinen KM, Belfort MB, Pace CDW, Lackey KA, et al. Characterization of SARS-CoV-2 RNA, antibodies, and neutralizing capacity in milk produced by women with COVID-19. Am Soc Microbiol. (2021) 12:1–11. doi: 10.1128/mBio.03192-20. Available at: https://journals.asm.org/doi/10.1128/mBio.03192-20 (Accessed 3 December 2022).
66. Parker MG, Stellwagen LM, Noble L, Kim JH, Poindexter BB, Puopolo KM. Promoting human milk and breastfeeding for the very low birth weight infant. Am Acad Pediatr. (2021) 148:1–15. doi: 10.1542/peds.2021-054272.. Available at: https://publications.aap.org/pediatrics/article/148/5/e2021054272/181366/Promoting-Human-Milk-and-Breastfeeding-for-the (Accessed 2 February 2023).
67. Parlak ME, Öz E, Kϋçϋkkelepçe O. COVID-19 Vaccination and breastfeeding mothers in kahta district, Turkey. Vaccines. (2023) 11:1–10. doi: 10.3390/vaccines11040813. Available at: https://www.mdpi.com/2076-393X/11/4/813 (Accessed 20 February 2023).
68. Peng S, Zhu H, Yang L, Cao L, Huang X, Dynes M, et al. A study of breastfeeding practices, SARS-CoV-2 and its antibodies in the breast milk of mothers confirmed with COVID-19. Lancet Reg Health West Pac. (2020) 4:1–10. doi: 10.1016/j.lanwpc.2020.100045. Available at: https://www.thelancet.com/journals/lanwpc/article/PIIS2666-6065(20)30045-6/fulltext (Accessed 7 June 2022).
69. Poon LC, Yang H, Dumont S, Lee JCS, Copel JA, Danneels L, et al. ISUOG interim guidance on coronavirus disease 2019(COVID-19) during pregnancy and puerperium: information for healthcare professionals – an update. Ultrasound Obstet Gynecol. (2020) 55:848–862. doi: 10.1002/uog.22061. Available at: https://obgyn.onlinelibrary.wiley.com/doi/10.1002/uog.22061 (Accessed 29 December 2022).32356590
70. Prabhu M, Riley LE. Coronavirus disease 2019 (COVID-19) vaccination in pregnancy. Obstet Gynecol. (2023) 141:473–482. doi: 10.1097/AOG.0000000000005100. Available at: https://journals.lww.com/greenjournal/Fulltext/2023/03000/Coronavirus_2019_COVID_19_Vaccination_in.7.aspx (Accessed 29 March 2023).36649624
71. Prasad A, Yankappa N, Kumar P, Chaudhary BK, Pati BK, Anant M, et al. Excretion of SARS-CoV-2 in breast milk: a single-centre observational study. BMJ Paediatr Open. (2021) 5:1–5. doi: 10.1136/bmjpo-2021-001087. Available at: https://bmjpaedsopen.bmj.com/content/5/1/e001087 (Accessed 6 November 2022).
72. Qun L, Xuhua G, Peng W, Xiaoye W, Lei , Yeqing T, et al. Early transmission dynamics in Wuhan, China. N Engl J Med. (2020) 382:1199–1207. doi: 10.1056/NEJMoa2001316. Available at: https://www.nejm.org/doi/10.1056/nejmoa2001316 (Accessed 5 January 2022).31995857
73. Rasmussen SA, Kelley CF, Horton JP, Jamieson DJ. Coronavirus disease 2019 (COVID-19) vaccines and pregnancy: what obstetricians need to know. J Obstet Gynaecol. (2021) 137:408–414. doi: 10.1097/AOG.0000000000004290. Available at: https://journals.lww.com/greenjournal/Fulltext/2021/03000/Coronavirus_Disease_2019__COVID_19__Vaccines_and.4.aspx (Accessed 10 July 2022).
74. Rawat M, Chandrasekharan P, Hicar MD, Lakshminrusimha S. COVID-19 in newborns and infants—low risk of severe disease: silver lining or dark cloud? Am J Perinatol. (2020) 37:845–849. doi: 10.1055/s-0040-1710512. Available at: https://www.google.com/url?sa=t&source=web&rct=j&url=https://www.thieme-connect.com/products/ejournals/pdf/10.1055/s-0040-1710512.pdf&ved=2ahUKEwiHi_Tx4Kz-AhUzmVwKHTUwAa4QFnoECA0QAQ&usg=AOvVaw1q49VzB7WTQaHQpYFg1xrm (Accessed 1 July 2022).32380565
75. Rohmah H, Hafsah T, Rakhmilla LE. Role of exclusive breastfeeding in preventing diarrhea. Althea Med J. (2015) 2:78–81. doi: 10.15850/amj.v2n1.436. Available at: https://www.researchgate.net/publication/299385757_Role_of_Exclusive_Breastfeeding_in_Preventing_Diarrhea (Accessed 16 April 2023).
76. Sajini AA, Alkayyal AA, Mubaraki FA. The recombination potential between SARS-CoV-2 and MERS-CoV from cross-Species spill-over infections. J Epidemiol Glob Health. (2021) 11:115–159. doi: 10.2991/jegh.k.201105.001. Available at: https://pubmed.ncbi.nlm.nih.gov/33605109/ (Accessed 3 November 2022).
77. Saso A, Kampmann B. Vaccine response in newborns (2017). Springer. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5711983/ (Accessed 30 August 2022).
78. Setti L, Passarini F, De Gennaro G, Barbieri P, Perrone MG, Borelli M, et al. Airborne transmission route of COVID-19: why 2 meters/6 feet of inter-personal distance could not be enough. Int J Environ Res Public Health. (2020) 17:1–6. doi: 10.3390/ijerph17082932. Available at: https://pubmed.ncbi.nlm.nih.gov/32340347/ (Accessed 4 December 2022).
79. Sevilla-Montoya R, Hidalgo-Bravo A, Estrada-Gutiérrez G, Villavicencio-Carrisoza O, Leon-Juarez M, Villegas-Mota I, et al. Evidence of possible SARS-CoV-2 vertical transmission according to world health organization criteria in asymptomatic pregnant women. Obstet Gynecol. (2021) 58:900–908. doi: 10.1002/uog.24787. Available at: https://obgyn.onlinelibrary.wiley.com/doi/10.1002/uog.24787 (Accessed 6 July 2022).
80. Stafford LS, Valcarce V, Henry M, Neu J, Parker L, Mueller M, et al. Detection of SARS-CoV-2 IgA and IgG in human milk and breastfeeding infant stool 6 months after maternal COVID-19 vaccination. J Perinatol. (2023) :1–7. doi: 10.1038/s41372-022-01581-5. Available at: https://www.nature.com/articles/s41372-023-01660-1 (Accessed 12 April 2023).37024528
81. Stuebe A. Should infants be separated from mothers with COVID-19? First, do No harm. Breastfeed Med. (2020) 5:351–352. doi: 10.1089/bfm.2020.29153. Available at: https://pubmed.ncbi.nlm.nih.gov/32271625/ (Accessed 16 May 2022).
82. Tsai PH, Wang ML, Yang DM, Liang KH, Chou SJ, Chiou SH, et al. Genomic variance of open Reading frames (ORFs) and spike protein in severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). J Chin Med Assoc. (2020) 83:725–732. doi: 10.1097/JCMA.0000000000000387. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7493783/ (Accessed 30 July 2022).32773643
83. Turner SE, Brockway M, Azad MB, Grant A, Tomfohr-Madsen L, Brown A. Breastfeeding in the pandemic: A qualitative analysis of breastfeeding experiences among mothers from Canada and the United Kingdom. Women and Birth. (2023) 17:1–13. doi: 10.1016/j.wombi.2023.01.002. ScienceDirect. Available at: https://pubmed.ncbi.nlm.nih.gov/36669903/ (Accessed 13 November 2023).
84. Ukoli F, Leavell J, Mayo A, Moore J, Nchami N, Britt A Encouraging and reinforcing safe BreastfeedingPractices during the COVID-19 pandemic. J Environ Res Public Health. (2023) 20:1–16. doi: 10.3390/ijerph20031756. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9914864/ (Accessed 14 April 2023).
85. Unger S, Christie-Holmes N, Guvenc F, Budylowski P, Mubareka S, Scott D. Holder pasteurization of donated human milk is effective in inactivating SARS-CoV-2. Can Med Assoc J. (2020) 192:E871–E874. doi: 10.1503/cmaj.201309. Available at: https://www.google.com/url?sa=t&source=web&rct=j&url=https://www.cmaj.ca/content/cmaj/192/31/E871.full.pdf&ved=2ahUKEwjyzsH566z-AhXEnFwKHUOoArYQFnoECA0QAQ&usg=AOvVaw0lHr9U2w-3O8CQfFnVogn1 (Accessed 30 November 2022).
86. UNICEF. The Lancet: Increasing breastfeeding worldwide could prevent over 800,000 child deaths every year (2016). Available at: https://www.unicef.org.uk/babyfriendly/lancet-increasing-breastfeeding-worldwide-prevent-800000-child-deaths-every-year/ (Accessed 10 October 2022).
87. UNICEF. Breastfeeding safely during the COVID-19 pandemic (2020). Available at: https://www.unicef.org/turkiye/en/stories/breastfeeding-safely-during-covid-19-pandemic (Accessed 29 October 2022).
88. UNICEF. Global Breastfeeding Scorecard, 2019 (2020). Available at: https://www.unicef.org/southafrica/media/2606/file/Infant-and-young-child-feeding-COVID-19-joint-note.pdf (Accessed 29 September 2022).
89. UNICEF. Infant and Young Child Feeding in the Context of the COVID-19 Pandemic Eastern, Central and Southern Africa (2020). Available at: https://www.unicef.org/southafrica/media/2606/file/Infant-and-young-child-feeding-COVID-19-joint-note.pdf (Accessed 29 September 2022).
90. UNICEF. Infant and Young Child Feeding in the Context of the COVID-19 Pandemic Eastern, Central and Southern Africa (2020). Available at: https://www.unicef.org/southafrica/media/2606/file/Infant-and-young-child-feeding-COVID-19-joint-note.pdf (Accessed 9 September 2022).
91. UNICEF. Infant and Young Child Feeding in the Context of the COVID-19 Pandemic Eastern, Central and Southern Africa (2020). Available at: https://www.unicef.org/southafrica/media/2606/file/Infant-and-young-child-feeding-COVID-19-joint-note.pdf (Accessed 10 September 2022).
92. UNICEF. Frequent Asked Questions: COVID-19 vaccines and breastfeeding (2021). Available at: https://www.unicef.org/vietnam/stories/frequent-asked-questions-covid-19-vaccines-and-breastfeeding#:∼:text=stopping%20breastfeeding%20after-,vaccination.,a%20cause%20for%20its%20interruption (Accessed 30 October 2022).
93. UpToDate. COVID-19: Intrapartum and postpartum issues (2022). Available at: https://www.uptodate.com/contents/covid-19-intrapartum-and-postpartum-issues?search=covid-19-issues-&topicRef=127535&source=see_link (Accessed 12 December 2022).
94. Wainstock T, Yoles I, Sergienko R, Sheiner E. Prenatal maternal COVID-19 vaccination and pregnancy outcomes. Vaccines. (2021) 39:6037–6040. doi: 10.1016/j.vaccine.2021.09.012. Available at: https://pubmed.ncbi.nlm.nih.gov/34531079/ (Accessed 3 July 2022).
95. Walker GJ, Clifford V, Bansal N, Stella AO, Turville S, Stelzer-Braid S, et al. SARS-CoV-2 in human milk is inactivated by holder pasteurisation but not cold storage. J Paediatr Child Health. (2020) 56:1872–1874. doi: 10.1111/jpc.15065. Available at: https://pubmed.ncbi.nlm.nih.gov/32767639/ (Accessed 1 March 2022).32767639
96. Walker K, Green J, Petty J, Whiting L, Staff L, Bromley P, et al. Breastfeeding in the context of the COVID-19 pandemic: a discussion paper. J Neonatal Nurs. (2022) 28:9–15. doi: 10.1016/j.jnn.2021.08.003. Available at: https://pubmed.ncbi.nlm.nih.gov/32767639/ (Accessed 2 January 2023).34366687
97. Watson OJ, Barnsley G, Toor J, Hogan AB, Winskill P, Ghani AC. Global impact of the first year of COVID-19 vaccination: a mathematical modelling study. Lancet Infect Dis. (2022) 22:1293–1302. doi: 10.1016/S1473-3099(22)00320-6. Available at: https://www.thelancet.com/journals/laninf/article/PIIS1473-3099(22)00320-6/fulltext (Accessed 3 January 2023).35753318
98. World Health Organization. Breastfeeding within an hour after birth is critical for saving newborn lives (2018). Available at: https://www.who.int/news/item/31-07-2018-3-in-5-babies-not-breastfed-in-the-first-hour-of-life (Accessed 1 October 2022).
99. World Health Organization. Breastfeeding and COVID-19 (2020). Available at: https://www.who.int/news-room/commentaries/detail/breastfeeding-and-covid-19 (Accessed 18 October 2022).
100. World Health Organization. Clinical management of severe acute respiratory infection (SARI) when COVID-19 disease is suspected: interim guidance (2020). Available at: https://apps.who.int/iris/handle/10665/331446 (Accessed 20 January 2022).
101. World Health Organization. COVID-19 Public Health Emergency of International Concern (PHEIC) Global research and innovation forum (2020). Available at: https://www.who.int/publications/m/item/covid-19-public-health-emergency-of-international-concern-(pheic)-global-research-and-innovation-forum (Accessed 1 September 2022).
102. World Health Organization. Criteria for releasing COVID-19 patients from isolation (2020). Available at: https://www.who.int/westernpacific/publications-detail/criteria-for-releasing-covid-19-patients-from-isolation (Accessed 24 October 2022).
103. World Health Organization. Frequently asked questions (2020). Available at: https://cdn.who.int/media/docs/default-source/maternal-health/faqs-breastfeeding-and-covid-19_805d4ce8-2329-4227-9261-695afa68b32c.pdf?sfvrsn=d839e6c0_5 (Accessed 21 October 2022).
104. World Health Organization. How do vaccine work? (2020). Available at: https://www.who.int/news-room/feature-stories/detail/how-do-vaccines-work?gclid=EAIaIQobChMIudrA8oH0-gIVB7btCh2ZsQzOEAMYAiAAEgLLT_D_BwE (Accessed 5 August 2022).
105. World Health Organization. Impact of COVID-19 on people’s livelihoods, their health and our food systems (2020). Available at: https://www.who.int/news/item/13-10-2020-impact-of-covid-19-on-people’s-livelihoods-their-health-and-our-food-systems (Accessed 13 October 2022).
106. World Health Organization. Mask use in the context of COVID-19 Interim guidance (2020). Available at: https://www.who.int/publications/i/item/advice-on-the-use-of-masks-in-the-community-during-home-care-and-in-healthcare-settings-in-the-context-of-the-novel-coronavirus-(2019-ncov)-outbreak (Accessed 9 October 2022).
107. World Health Organization. Report of the WHO-China Joint Mission (2020). Available at: https://www.who.int/docs/default-source/coronaviruse/who-china-joint-mission-on-covid-19-final-report.pdf (Accessed 5 October 2022).
108. World Health Organization. Definition and categorization of timing of mother-to-child transmission of SARS-COV-2 (2021). Available at: https://who.int/publications/i/item/WHO-2019-nCoV-mother-to-child-transmission-2021 (Accessed 24 October 2022).
109. World Health Organization. Infant and young child feeding (2021). Available at: https://www.who.int/news-room/fact-sheets/detail/infant-and-young-child-feeding (Accessed 14 July 2022).
110. World Health Organization. Infant and young child feeding (2021). Available at: https://www.who.int/news-room/fact-sheets/detail/infant-and-young-child-feeding#:∼:text=Breast%2Dmilk%20is%20also%20an,between%2012%20and%2024%20months (Accessed 2 September 2022).
111. World Health Organization. Listings of WHO’s response to COVID-19 (2021). Available at: https://www.who.int/news/item/29-06-2020-covidtimeline (Accessed 2 May 2022).
112. World Health Organization. Naming the coronavirus disease (COVID-19) and the virus that causes i (2022). Available at: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/technical-guidance/naming-the-coronavirus-disease-(covid-2019)-and-the-virus-that-causes-it#:∼:text = Naming%20the%20coronavirus%20disease%20(COVID,the%20virus%20that%20causes%20it (Accessed 5 September 2022).
113. World Health Organization. Q&A on COVID-19 and Breastfeeding (2022). Available at: https://www.who.int/vietnam/news/feature-stories/detail/q-a-on-covid-19-and-breastfeeding (Accessed 29 October 2022).
114. Yang N, Che S, Zhang J, Wang X, Tang Y, Wang J. Breastfeeding of infants born to mothers with COVID-19: a rapid review. Ann Transl Med. (2020) 8:1–10. doi: 10.21037/atm-20-3299. Available at: https://atm.amegroups.com/article/view/43613/html (Accessed 3 May 2022).32055592
115. Zhang JJ, Dong X, Cao YY, Yuan YD, Yang YB, Yan YQ. Clinical characteristics of 140 patients infected with SARS-CoV-2 in Wuhan, China. Allergy. (2020) 75:1730–1741. doi: 10.1111/all.14238. Available at: https://pubmed.ncbi.nlm.nih.gov/32077115/ (Accessed 31 August 2022).32077115
116. Zhu H, Wang L, Fang C, Peng S, Zhang L, Chang G. Clinical analysis of 10 neonates born to mothers with 2019-nCoV. Transl Pediatr. (2020) 9:51–60. doi: 10.21037/tp.2020.02.06. Available at: https://tp.amegroups.com/article/view/35919/28274 (Accessed 20 November 2022).32154135
117. Zhu F, Zozaya C, Zhou Q, De Castro C, Shah PS. SARS-CoV-2 genome and antibodies in breastmilk: a systematic review and meta-analysis. Arch Dis Child Fetal Neonatal Ed. (2021) 106:514–521. doi: 10.1136/archdischild-2020-321074. Available at: https://pubmed.ncbi.nlm.nih.gov/33568494/ (Accessed 16 November 2022).33568494
118. Wei L, Jing W, Zhaoxian Z, Siying L, Zhihui R. Clinical characteristics of 19 neonates born to mothers with COVID-19. Frontiers in Medicine. (2020) 14(2):193–8. doi: 10.1007/s11684-020-0772-y
119. Hu Y, Meng X, Zhang , Xiang Y, Wang J. The in vitro antiviral activity of lactoferrin against common human coronaviruses and SARS-CoV-2 is mediated by targeting the heparan sulfate co-receptor. Emerging Microbes & Infections. (2021) 10(1):317–30. doi: 10.1080/22221751.2021.1888660
Keywords: COVID-19, breastfeeding, vertical transmission, characteristics of SARS-CoV-2, COVID-19 vaccine
Citation: Chanda BM and Chen X-Q (2023) Breastfeeding during the COVID-19 pandemic. Front. Pediatr. 11:1120763. doi: 10.3389/fped.2023.1120763
Received: 10 December 2022; Accepted: 10 May 2023;
Published: 5 June 2023.
Edited by:
MaryAnn Volpe, Tufts University, United StatesReviewed by:
Rajesh Kulkarni, Post Graduate Institute Yashwantrao Chavan Memorial Hospital, IndiaFeng Jiang, Fudan University, China
Renqiang Yu, Wuxi Maternity and Child Health Care Hospital, China
© 2023 Chanda and Chen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xiao-Qing Chen Y2hlbnhxMjAwMkBmb3htYWlsLmNvbQ==
 Bwalya Mpelwa Chanda
Bwalya Mpelwa Chanda Xiao-Qing Chen
Xiao-Qing Chen