- 1Department of Orthopaedic Surgery, Union Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, China
- 2Department of Pediatric Orthopedic, Center for Orthopedic Surgery, The Third Affiliated Hospital of Southern Medical University, Guangzhou, China
- 3Department of Pediatric Orthopaedics, Shengjing Hospital of China Medical University, Shenyang City, China
- 4Basic Medical School, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, China
- 5Department of Orthopaedic Surgery, Children's Hospital of Nanjing Medical University, Nanjing, China
Objective: To review the radiographic manifestation and clinical appearance of children with congenital radioulnar synostosis (CRUS) retrospectively.
Study design: Retrospective cohort study of children with CRUS from multiple medical centers.
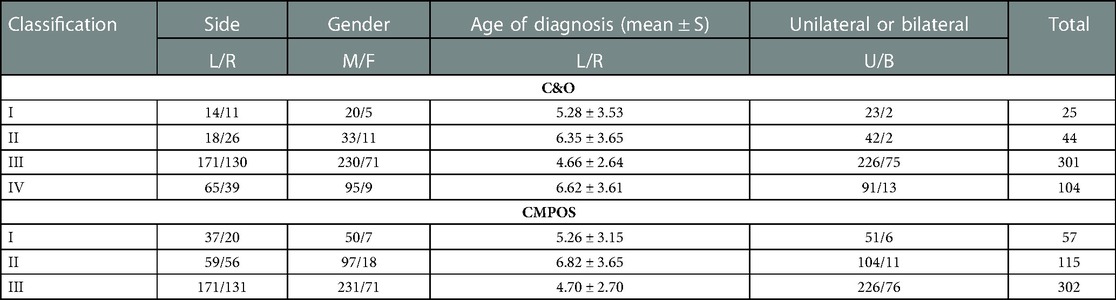
Results: A total of 329 patients (male 259, female 70) with an average age of 5.4 years (0.5–16 years old), were included in this study. In particular, 145 patients (145/329, 44.1%) demonstrated bilateral involvement, and 184 patients (left 123, right 61) demonstrated unilateral involvement. As for Clear and Omery (C&O) classification, most patients belonged to Type III, and then followed by Type IV. As for Chinese Multi-center Pediatric Orthopedic Study Group (CMPOS) classification, most patients belonged to Type III, and then followed by Type II and Type I. In C&O Type III, 92.03% patients demonstrated severe pronation. According to CMPOS classification, 92.98% Type I patients demonstrated neutral to mild pronation, 72.17% Type II patients demonstrated moderate pronation, and 92.03% Type III patients demonstrated severe pronation. The age distribution showed no significant difference between C&O Type II and IV (P = 0.96); the pronation ankylosis severity showed no significant difference between C&O Type II and IV (P = 0.387).
Conclusion: Although CRUS is a rare forearm deformity, there are certain relation between radiographic manifestation and clinical forearm functional restriction. CRUS patients of C&O or CMPOS Type III classification might suffer severe pronation deformity and warrant early intervention.
Introduction
Congenital radioulnar synostosis (CRUS) is an abnormal condition at the proximal radius and the ulna, with restricted forearm rotation as prominent features (1). The clinical characteristics of fixed forearm deformity varies across different patients, from neutral position to severe pronation (2). The functional disability depends on the fixed position of forearms, bilaterality, and social practice in different cultural backgrounds (3). Usually, x-ray of forearm should suffice for the diagnosis of this condition (1). Because of its rarity and the diversity of fixed position, there is no consensus on the treatment strategy (4, 5). So far, multiple surgical techniques and physiotherapy have been reported to be beneficial for this condition with improved life quality (6–9). However, the indication for surgery remains unclear and the postoperative outcomes remains mixed (1, 2).
Most investigations on CRUS were case reports or small cohorts. Sachar et al. reviewed the largest cohort study so far, with 350 cases in total (10). However, he merely reviewed these cases without in-depth analysis. Until present day, the literature has witnessed the publications of 616 cases in CRUS (1, 8). However, there existed no report on the correlation between radiographic manifestation and clinical function.
Nowadays, the widely adopted classification was proposed by Cleary and Omer in 1985 (11). Cleary & Omer classification (C&O classification) consists of 4 types based on the appearance of the synostosis and status of radial head on x-ray. However, because of the small cohort, the relation between C&O classification and clinical manifestation was not revealed clearly (11). In the past, supinator was thought to be absent in certain patients, which was repudiated by Li Jin et al. (12). Recently, a novel classification system based on x-ray and magnetic resonance imaging (MRI) was proposed by Chinese Multi-center Pediatric Orthopedic Study Group (CMPOS) (12). The supinator was taken into consideration in this novel anatomical classification and all patients demonstrated the presence of supinator in the MRI. However, there was still no elucidation on the relationship between radiographic classification and clinical manifestation. Therefore, a retrospective study from multiple medical centers with a large cohort of pediatric patients diagnosed as CRUS was performed.
Methods
Patients diagnosed as CRUS were reviewed retrospectively from four high-volume geographically separated medical centers. Basic information were collected anonymously and centrally with written informed consent signed by legal guardians of the patients.
The inclusion criteria were: (1) younger than 18 years old at the time of diagnosis; (2) without previous surgery or instrumentation in the affected limb; (3) without concurrent syndromic malformation or deformity of the ipsilateral upper extremity. The exclusion criteria were: (1) concomitant neuromuscular disease; (2) incomplete medical records; (3) inconsistent diagnosis between two senior attending physicians; (4) patients with complicated syndromic manifestation. This study was approved by the ethnics committee of authors’ institutes.
All the radiographic data were extracted from institutes database and reviewed by two senior attending physicians. The types of x-ray manifestations were recorded according to the C&O and CMPOS classification if their results were consistent, otherwise a third observer would check and made the final decision. Clinical manifestations were extracted from institutes database and recorded by two physicians. The observers were not involved in the authorship of this research.
C&O classification consists of four types: (I) fibrous ankylosis with normal radial head; (II) osseous synostosis with normal radial head; (III) osseous synostosis with posteriorly dislocated and hypoplastic radial head; (IV) pseudo-synostosis and anteriorly dislocated, mushroom-shaped radial head (11). CMPOS classification consists of three type: (I) fibrous pseudo-synostosis with any shape of the radial head; (II) osseous synostosis with or without dislocated radial head; (III) radiographic radial head unobservable and osseous synostosis with the ulna (12) (see Figure 1).
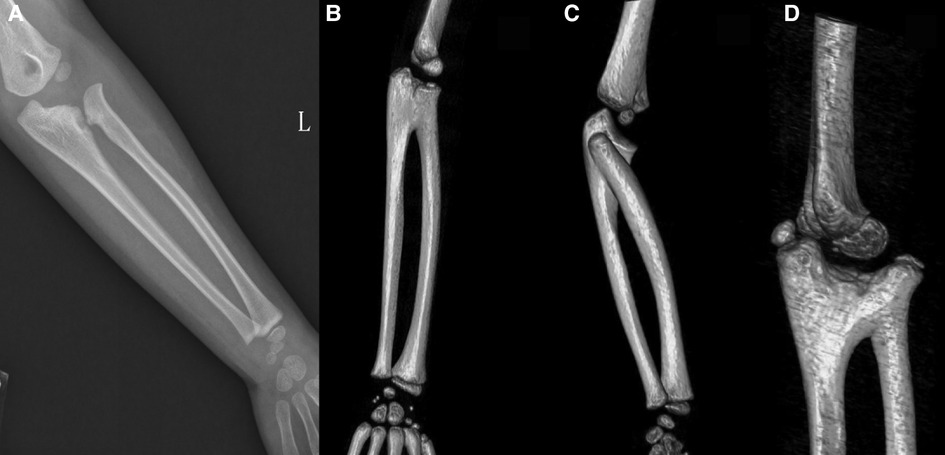
Figure 1. X-ray or CT reconstruction of forearm deformities. (A) C & O Type I; CMPOS Type I. (B) C & O Type II; CMPOS Type II. (C) C & O Type III; CMPOS Type III. (D) C & O Type IV; CMPOS Type II.
One-way ANOVA test, Student's t test and SNK-q test were conducted. Statistical analysis was performed using the IBM SPSS statistics version 20 software (SPSS Inc., Chicago, Illinois).
Results
A total of 329 patients (male 259, female 70) with an average age of 5.4 years (0.5–16 years old), were included in this study. The age was the patient firstly diagnosed as CRUS in the clinic. In particular, 145 patients (145/329, 44.1%) demonstrated bilateral involvement, and 184 patients (left 123, right 61) demonstrated unilateral involvement. Only three patients with fixed supination deformity were included, and the rest demonstrated pronation deformity. As for C&O classification, most patients belonged to Type III, and then followed by Type IV. As for CMPOS classification, most patients belonged to Type III, and then followed by Type II and Type I (see Table 1).
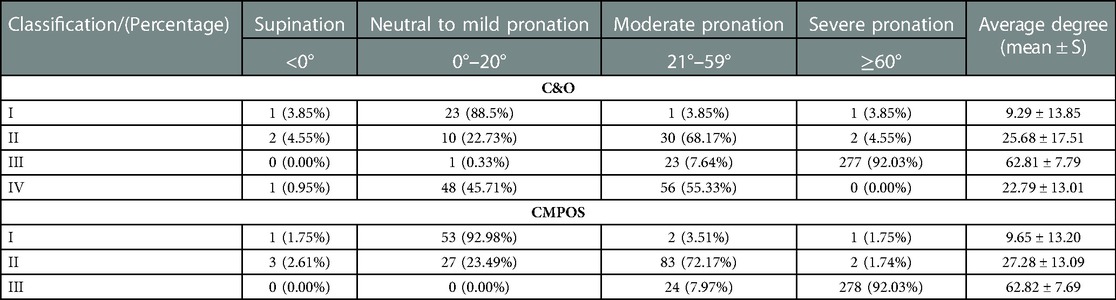
As shown in Table 2, according to C&O classification, 88.5% Type I and 45.71% Type IV patients demonstrated neutral to mild pronation. However, 68.17% Type II and 55.33% Type IV patients demonstrated moderate pronation. In C&O Type III, 92.03% patients demonstrated severe pronation. According to CMPOS classification, 92.98% Type I patients demonstrated neutral to mild pronation, 72.17% Type II patients demonstrated moderate pronation, and 92.03% Type III patients demonstrated severe pronation.
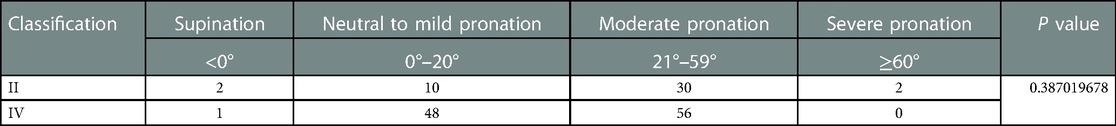
The age distribution showed no significant difference between C&O Type II and IV (P = 0.96); The pronation ankylosis severity showed no significant difference between C&O Type II and IV (P = 0.387, see Table 3).
As shown in Table 4, in the 145 patients with bilateral involvement 38.62% patients demonstrated identical pronation degrees, while 31.03% patients demonstrated more than 30 degrees difference between two arms. As for C&O classification, 92 patients (63.4%) demonstrated the same category; as for CMPOS classification, 93 (64.1%) showed the same category.
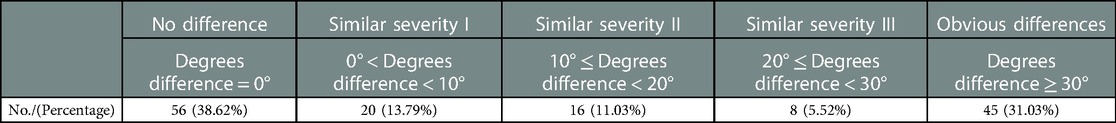
Table 4. Differences in the right and left hands pronation degree in patients with bilateral involvement.
Discussion
To the best of our knowledge, this study was the largest cohort on CRUS highlighting the association between radiographic manifestation and clinical forearm functional restriction. In this study, correlation between the pronation ankylosis and radiographic manifestation was shown in our results. Most patients in C&O and CMPOS Type III demonstrated severe pronation deformity (>60 degrees), while patients in other types demonstrated sparse distribution without normality.
Several previous studies focusing on the surgical intervention for CRUS highlighted the fixated pronation deformity as one important criterion for surgery (13–16), but the latest meta-analysis in 2022 still reached no consensus on the severity of pronation and the necessity of surgery (13). Because of its rarity, most case series did not stress on the correlation of x-ray manifestation and forearm pronation deformity.
Many surgical techniques have been reported, including derotation and mobilization surgeries (14–16). However, the optimal surgical technique remains controversial, and the reported clinical outcomes after surgery were inconsistent. Until now, there was no clinical classification guiding treatment algorithm. Besides, there was no classification reflecting clinical function of forearms. For patients with neutral or mild supination deformity, surgical intervention is not necessary. Physiotherapy seemed to be beneficial for patients with moderate rotation restriction (9). However, the criteria for surgery remains unclear. Ankylosis pronation over 60 degrees has been proposed as a criterion for operation (3–5). Patients with bilateral involvement should be carefully evaluated for daily activities restriction and necessity for surgery (1–5). Certain authors recommended surgeries for patients with bilateral pronation over 45 degrees (4, 5). Pronation severity as an important parameter has been mentioned in all publications on operative choices. However, there was no clear correlation between the pronation ankylosis and the necessity of surgery (1–7), even 20 degrees pronation was reported for surgery (14). The optimal age of surgery remains to be investigated, 1.5–9 years old have been reported in the literature (1, 2, 14).
Currently, there is no actionable classification for treatment algorithm. C&O classification is widely adopted in academic publications, but it did not reflect the severity of deformity regarding the forearm functional restriction (11). Li Jin et al. confirmed the presence of supinator in all patients with CRUS in their study (12). However, the novel CMPOS classification is still an anatomical and radiographic classification without direct reflection of the forearm functional restriction (12). Patients in type II and IV demonstrated similar pronation ankylosis degrees without chronological relevance. In this study, the manifestation of C&O II and IV was similar in age and ankylosis pronation severity, which corroborated the fusion of C&O classification II and IV as CMPOS type II (12).
The results of this study showed that most of the patients belonged to type III with prominent pronation deformity, partly because of its severity of fixed pronation leading to earlier detection. Type III are similar in C&O and CMPOS classification, as it demonstrates osseous synostosis with a hypoplastic and posteriorly dislocated radial head (11). Therefore, patients with type III deformity with severe pronation might be beneficial from early surgery. Moreover, patients with bilateral involvement did not demonstrate the same severity in both forearms, consistent with earlier publications (1, 2).
There are certain limitations in our study. Firstly, it is a retrospective study without long term follow-up. Secondly, our data did not demonstrate normal distribution because of relatively small sample size. Further investigation with longer follow-up and advanced radiological examinations including CT scan or MRI might be warranted to explore more meaningful facts about this disease.
Conclusion
Although CRUS is a rare forearm deformity, there are certain relations between radiographic manifestations and clinical forearm functional restriction. CRUS patients of C&O or CMPOS Type III classification might suffer severe pronation deformity and warrant early intervention.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by Ethics Committee of Tongji Medical College, Huazhong University of Science and Technology. Written informed consent to participate in this study was provided by the participants' legal guardian/next of kin.
Author contributions
PH, WT, W-ZZ, and YZ involved in data collection and assessments. XT and PH were responsible for literature search and study design, PH, WT and W-ZZ drafting the manuscript. PZ and XT finalized the manuscript. All authors contributed to the article and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Rutkowski PT, Samora JB. Congenital radioulnar synostosis. J Am Acad Orthop Surg. (2021) 29(13):563–70. doi: 10.5435/JAAOS-D-20-01133
2. Barik S, Farr S, Gallone G, Zarantonello P, Trisolino G, Di Gennaro GL. Results after treatment of congenital radioulnar synostosis: a systematic review and pooled data analysis. J Pediatr Orthop B. (2021) 30(6):593–600. doi: 10.1097/BPB.0000000000000841
3. Jia Y, Geng C, Song Z, Lv S, Dai B. Congenital unilateral proximal radioulnar synostosis: a surgical case report. Medicine. (2020) 99(16):e19782. doi: 10.1097/MD.0000000000019782
4. Nakasone M, Nakasone S, Kinjo M, Murase T, Kanaya F. Three-dimensional analysis of deformities of the radius and ulna in congenital proximal radioulnar synostosis. J Hand Surg Eur. (2018) 43(7):739–43. doi: 10.1177/1753193417753261
5. Kanaya K, Iba K, Yamashita T. Long-term results after a free vascularized adipofascial graft for congenital proximal radioulnar synostosis with an average follow-up of 10 years: a series of four cases. J Shoulder Elbow Surg. (2016) 25(8):1258–67. doi: 10.1016/j.jse.2016.04.009
6. Zhang ZQ, Hu XY, Yuan HJ, Zheng PF. Application of 3-dimensional printing technology in rotational osteotomy of congenital radioulnar synostosis. J Hand Surg Am. (2021) 46(10):924.e1–e6. doi: 10.1016/j.jhsa.2020.12.004
7. Tan W, Yuan Z, Lin Y, Li Y, Ji Y, Sun Y, et al. Rotational osteotomy with single incision and elastic fixation for congenital radioulnar synostosis in children: a retrospective cohort study. Transl Pediatr. (2022) 11(5):687–95. doi: 10.21037/tp-22-111
8. Martínez-Álvarez S, González-Codó S, Vara-Patudo I, Galán-Olleros M, Fraga-Collarte M, Palazón-Quevedo Á. Double-level intraperiosteal derotational osteotomy for congenital radioulnar synostosis. J Pediatr Orthop. (2022) 42(7):e756–61. doi: 10.1097/BPO.0000000000002191
9. Kepenek-Varol B, Hoşbay Z. Is short-term hand therapy effective in a child with congenital radioulnar synostosis? A case report. J Hand Ther. (2020) 33(3):435–42. doi: 10.1016/j.jht.2019.03.009
10. Sachar K, Akelman E, Ehrlich MG. Radioulnar synostosis. Hand Clin. (1994) 10(3):399–404. doi: 10.1016/S0749-0712(21)01178-1
11. Cleary JE, Omer GE Jr. Congenital proximal radio-ulnar synostosis. Natural history and functional assessment. J Bone Joint Surg Am. (1985) 67(4):539–45. doi: 10.2106/00004623-198567040-00006
12. Li J, Chen K, Wang J, Guo Y, Rai S, Tang X, et al. An anatomical classification of congenital proximal radioulnar synostosis based on retrospective MRI measurement combined with radiography. Sci Rep. (2022) 12(1):6585. doi: 10.1038/s41598-022-09411-6
13. Nema SK, Ramasubramani P, Pasupathy P, Austine J. Corrective derotation osteotomies to treat congenital radioulnar synostosis in children: results of a systematic review and meta-analysis. Indian J Orthop. (2022) 56(5):717–40. doi: 10.1007/s43465-021-00582-4
14. Bai F, Chen S, Liu L, Tong D, Li P, Rong Y, et al. Treatment of congenital radioulnar synostosis using a free vascularized fascia lata graft. Orthop Surg. (2022) 14(6):1229–34. doi: 10.1111/os.13226
15. Hamiti Y, Yushan M, Yalikun A, Lu C, Yusufu A. Derotational osteotomy and plate fixation of the radius and ulna for the treatment of congenital proximal radioulnar synostosis. Front Surg. (2022) 9:888916. doi: 10.3389/fsurg.2022.888916
Keywords: congenital radioulnar synostosis, pronation, ankylosis, classification, radiographic manifestation
Citation: Hong P, Tan W, Zhou W-Z, Zheng Y, Li J, Zheng P and Tang X (2023) The relation between radiographic manifestation and clinical characteristics of congenital radioulnar synostosis in children: A retrospective study from multiple centers. Front. Pediatr. 11:1117060. doi: 10.3389/fped.2023.1117060
Received: 6 December 2022; Accepted: 16 February 2023;
Published: 3 March 2023.
Edited by:
Giovanni Trisolino, Rizzoli Orthopedic Institute (IRCCS), Italy© 2023 Hong, Tan, Zhou, Zheng, Li, Zheng and Tang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xin Tang ZHJfeGludGFuZ0BodXN0LmVkdS5jbg== PengFei Zheng emhlbmdwZW5nZmVpQG5qbXUuZWR1LmNu
†These authors have contributed equally to this work and share first authorship
‡These authors have contributed equally to this work and share Correspondence
§ORCID Xin Tang orcid.org/0000-0002-6860-6530
Specialty Section: This article was submitted to Pediatric Orthopedics, a section of the journal Frontiers in Pediatrics
 Pan Hong
Pan Hong Wei Tan
Wei Tan Wei-Zheng Zhou3,†
Wei-Zheng Zhou3,† Yu Zheng
Yu Zheng Jin Li
Jin Li PengFei Zheng
PengFei Zheng Xin Tang
Xin Tang