- 1The Library Unit, Shandong Sport University, Jinan, China
- 2Vanke School of Public Health, Tsinghua University, Beijing, China
- 3School of Psychology, Shenzhen University, Shenzhen, China
- 4Centre for Active Living and Learning, College of Human and Social Futures, University of Newcastle, Callaghan, NSW, Australia
- 5Active Living Research Program, Hunter Medical Research Institute, New Lambton Heights, NSW, Australia
- 6Centre for Mental Health, Shenzhen University, Guangdong, China
Background: Sleep difficulties are a common sleep-related problem among children and adolescents. However, the association between eating habits and sleep difficulties has not been extensively studied. Therefore, this study aimed to investigate the relationship between eating habits and sleep difficulties in children and adolescents.
Methods: This study utilized cross-sectional data from the 2013/2014 Health Behaviour in School-aged Children survey. A total of 213,879 young adolescents provided self-reported information on their weekday and weekend breakfast consumption, fruit and vegetable intake, sweet and soft drink consumption, and sleep difficulties. Covariates such as sex, age, family affluence, physical activity, and body mass index were also assessed. Multilevel generalized linear modelling was used to analyse the association between independent and dependent. Results were reported as odds ratios (OR) with 95% confidence intervals.
Results: Of all study participants, approximately 50% were girls. Regression models indicated that more frequent breakfast consumption was associated with fewer sleep difficulties (e.g., consuming breakfast on weekdays for 5 days: OR = 1.49, 95% CI: 1.45–1.54). Fruit and vegetable consumption once a week or more was also linked to fewer sleep difficulties (all OR > 1.08, ≥ 1.07). In addition, consuming fewer sweets and soft drinks was generally associated with fewer sleep difficulties.
Conclusion: This study provides evidence supporting the association between healthier eating habits and reduced sleep difficulties in children and adolescents. Future research using longitudinal or experimental designs is encouraged to confirm or negate these findings. Additionally, this study offers practical guidance for nutritional counselling professionals and sleep health promotion practitioners.
1. Introduction
Sleeping difficulties are increasingly prevalent among adolescents, ranging from 15% to 44% (1–3), and have become a globally recognized public health issue. The short-term and long-lasting effects of sleeping difficulties on adolescents' negative developmental outcomes have been highlighted, including a higher risk of cognitive, memory, or academic deficits, increased risk of mental health problems, poorer school performance, behavior problems, and even heart disease or a higher level of all-cause mortality (4). These adverse consequences may last into adulthood; for example, previous research shows that the level of adolescents' sleep problems predicted their adulthood sleep disturbance (5). Therefore, it has become an obligation for professionals to fully identify modifiable factors linked to sleeping difficulties among children and adolescents, which are necessary for developing tailored prevention or early intervention at an early stage.
A considerable amount of knowledge on the risk factors for sleeping difficulties has been accumulated in this field. For example, previous studies have found that lifestyle factors such as consuming excessive amounts of caffeine or prolonged use of screen media in the bedroom at night, environmental factors like excessive lighting in the bedroom, psychosocial problems such as anxiety symptoms, and even medical conditions may contribute to sleeping difficulties among adolescents (4, 6–10). However, the association between eating habits and sleeping difficulties remains understudied and lacks clear answers.
Individual eating habits, such as consuming breakfast on weekdays and weekends, consuming fruits, vegetables, sweets, and soft drinks (11), are essential for living well and can have a strong impact on adolescents' biological clock, circadian rhythm, and physiological hormones like melatonin and serotonin. These factors, in turn, can either facilitate or impair their sleep quality (12–14).
A recent exploratory study investigated the relationship between breakfast consumption and subjective sleep quality among university students. The study found that students who skipped breakfast, ate late-night snacks, or replaced meals with snacks were more likely to experience poor overall sleep quality (15). However, the study's small sample size (only 498 students) and generalization bias have raised questions about its validity. Furthermore, the underlying biological and psychological mechanisms of sleep vary from childhood to adulthood due to the developmental and maturation processes (16). Therefore, a nationally representative sample of adolescents is necessary to control the risk of false-negative or false-positive findings (17).
Although a few existing studies have found a protective role of vegetable and fruit consumption in adults' short sleep and poor sleep quality (18, 19), the influence of vegetable and fruit consumption on adolescent sleep difficulties remains unclear. For instance, only a few studies have found that adolescents with shorter sleep duration report consuming fewer fruits and vegetables than those who sleep for more than 8 h per day (20). Using 8 h of average sleep duration per day as a cut-off score for comparison may limit our understanding of the association between the frequency of vegetable and fruit intake and adolescents' general sleep difficulties.
Interestingly, the findings regarding the effects of sugar and sweet consumption on adolescent sleep difficulties are mixed. For example, a study of 287 Australian children found no association between total dietary sugar consumption and sleep problems (21). However, a study of a large sample of Korean youth found a negative association between high soft drink intake and sleep duration (22). These mixed results may be due to differences in age ranges, sample sizes, and measurement methods across studies. Therefore, additional studies with more systematic measures of eating habits during specific developmental stages are necessary to better understand these findings.
To the best of our knowledge, no studies have systematically examined the possible roles of eating habits in adolescent sleep difficulties. Additionally, the optimal frequency of these eating habits for improving adolescents' sleep quality remains unclear. Investigating these associations could provide empirical evidence for the development of dietary policies, guidelines, recommendations, or school practices for adolescents. Therefore, this study aimed to investigate the associations between adolescents' eating habits (including breakfast consumption on weekdays and weekends, fruit consumption, vegetable consumption, sweets consumption, and soft drink consumption) and sleeping difficulties using a nationally representative sample from multiple countries.
2. Method
2.1. Study design
The Health Behaviour in School-aged Children (HBSC) survey is an international, school-based study conducted in collaboration with the World Health Organization across 42 countries. This cross-sectional analysis utilized data from the 2013/2014 HBSC survey. A stratified cluster sampling method was employed to identify adolescents aged 11, 13, and 15 years, with mean ages of 11.5, 13.5, and 15.5 for each respective age group. Initially, schools were randomly selected from each participating country or region. Subsequently, the number of chosen classes depended on class size. Typically, one class was selected for each grade/year; however, additional classes were included if class sizes were smaller. Self-administered questionnaires were administered at the school level to assess health and well-being, social environments, and health behaviors among children and adolescents.
2.2. Measures
2.2.1. Independent: eating habits
The frequency of eating habits was assessed by two questions, including breakfast on weekdays and weekends, fruits, vegetables, sweets, and soft drinks. “How often do you usually have breakfast (more than a glass of milk or fruit juice)” was used to evaluate the frequency of breakfast on weekdays and weekends. Response options were never, less than once a week, two to four times a week, five to six times a week, once a day, and more than once a day. For weekdays, response options were never, only on 1 day, and on both days. The frequency of fruits, vegetables, sweets, and soft drinks was reported by adolescents in the following question: “How many times a week do you usually eat or drink fruits/vegetables/sweets (candy or chocolate)/coke or other soft drinks that contain sugar”. Response options were never, less than once a week, two to four times a week, five to six times a week, once a day, and more than once a day. For weekdays, response options were never, only on 1 day, and on both days. Eating habits were assessed by the above questions, which were based on the Food Frequency Questionnaire and showed good reliability and validity in adolescents (23).
2.2.2. Dependent: sleep difficulty
Adolescents' sleep difficulty was assessed by using a single question: “How often in the past six months did you have difficulties falling asleep?” Response options were: about every day, more than once a week, about every week, about every month, and rarely or never. There has been evidence to support this single question with good reliability and validity (24).
2.2.3. Covariates
The following covariates were adjusted in the statistical analysis, including sex, age (11/13/15 years), family well-off (very/quite/average/not very/not at all), body mass index (BMI), and physical activity. Adolescents were required to self-report their height and weight, and BMI then was calculated. In terms of physical activity, adolescents were required to answer the following question: “How many days did you participate in physical activity for at least 60 min per day in the past week?” Repose options were from 0 days to 7 days. These covariates were selected on the basis of their plausible associations with the outcome measures of interest (25).
2.3. Statistical analysis
All the statistical analysis was performed using STATA BE 17.0 (College Station, Texas, USA). Descriptive statistics were used to report sample characteristics. Multicollinearity issue was examined prior to the formal regression modelling and the results indicated no multicollinearity issues. A three-level mixed model with ordinal regression (level 3: country; level 2: school; level 1: individual; such layers were suggested according to the HBSC study protocol) was established to assess the associations of eating habits with sleeping difficulties (treated as ordinal variable), while controlling for sex, age category, family well-off, BMI and physical activity. meglm command was utilized to achieve to establish the above models. Results from the model were mainly presented as the odd ratio (OR) with a 95% confidence interval (CI), as an ordinal logistic regression model was used. A prior p-value below 0.05 was used to ascertain statistical significance.
3. Results
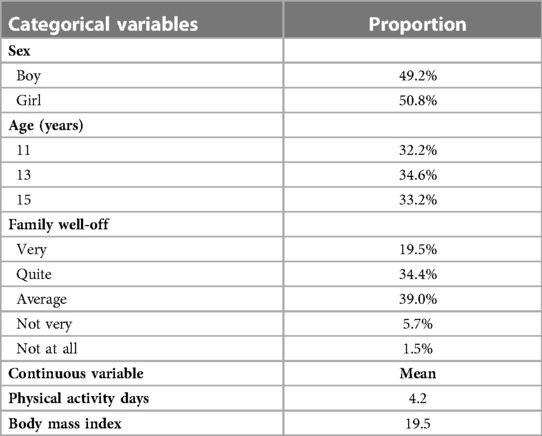
Sample characteristics are shown in Table 1. Of the 213,879 study participants aged between 11 and 15 years, 50.8% of them were girls, and the mean of BMI was 19.5. The percentage of adolescents aged 11, 13, and 15 years was 32.2%, 34.6%, and 33.2%. In total, 39.0% of the adolescents reported their family well-off as “Average”, 34.4% self-rated as “Quite”, 19.5% rated it as “Very”, 5.7% rated as “Not very”, and 1.5% rated as “Not at all”. On average, participants reported having about 4.2 days a week of physical activity.
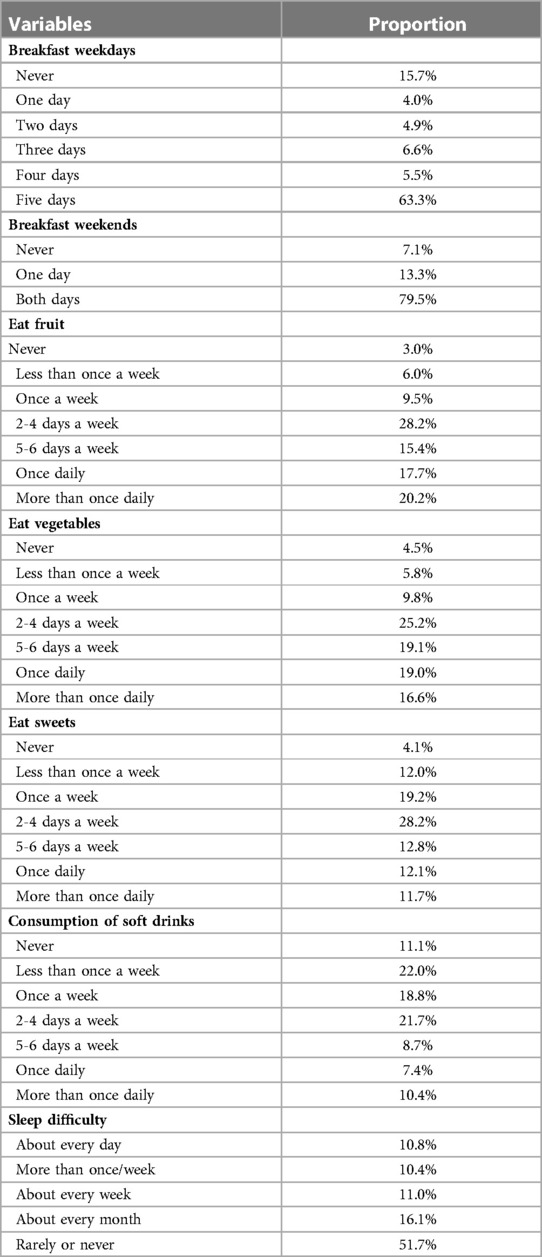
In Table 2, of the total sample, 63.3% of them reported eating breakfast for 5 days, and 15.7% never ate breakfast on weekdays. On weekends, the percentage of eating breakfast for 2 days was 79.5%, and only 7.1% of them never ate breakfast. In the total sample, 20.2% of adolescents ate fruit more than once daily, 15.4% of them reported for 5–6 days a week, 28.2% was 2–4 days a week, 9.5% was once a week, and 6.0% was less than once a week. Regarding eating vegetables, 16.6% and 19.0% of adolescents reported “more than once daily” and “once daily”, most of them ate vegetables less than once daily. Besides, the percentage of adolescents who reported eating sweets more than once daily was 11.7%, 5–6 days a week was 12.8%, 2–4 days a week was 28.2%, and once a week or less was 35.3%. There were 10.4% and 7.4% of adolescents who had soft drinks more than once daily and once daily, and more than half of adolescents reported once a week or less. In terms of sleep difficulty, 10.8% of participants reported having sleep difficulties every day, while 51.7% of them reported rarely or never with regard to sleep difficulties.
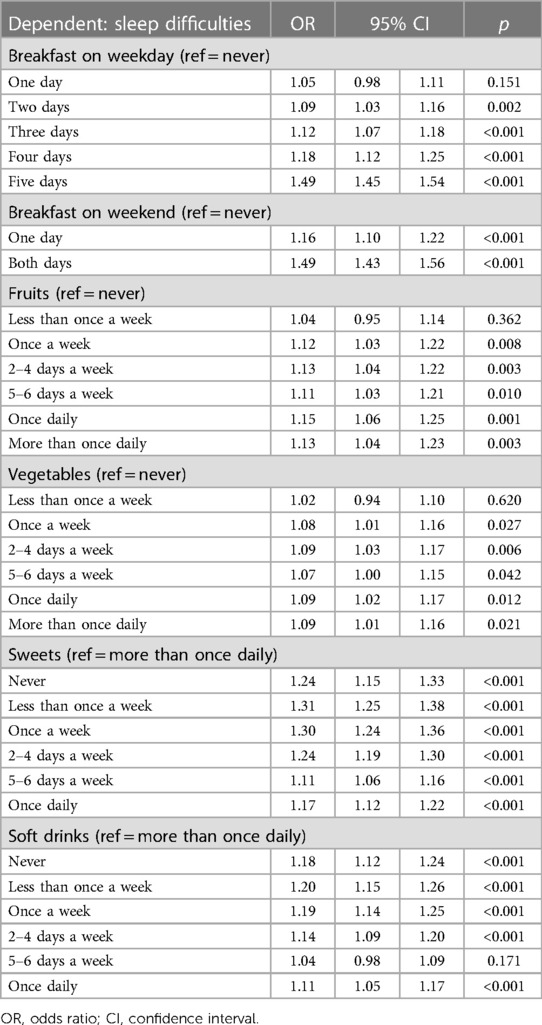
The results on the associations between independents and outcomes are shown in Table 3. Among the sample, those who ate breakfast on weekdays for two (OR = 1.09, CI = 1.03–1.16, p = 0.002), three (OR = 1.12, CI = 1.07–1.18, p < 0.001), four (OR = 1.18, CI = 1.12–1.25, p < 0.001) and 5 days (OR = 1.49, CI = 1.45–1.54, p < 0.001) were less likely to report sleep difficulties compared to those who did not eat breakfast for any day. Similarly, eating breakfast on weekends for one (OR = 1.16, CI = 1.10–1.22, p < 0.001) and 2 days (OR = 1.49, CI = 1.43–1.56, p < 0.001) were also negatively associated with sleep difficulties. In terms of fruits consumption, compared with not eating fruits, children who ate fruits once a week were at 1.12 times lower likelihood (CI = 1.03–1.22, p = 0.008), for 2–4 days a week were at 1.13 times lower likelihood (CI = 1.04–1.22, p = 0.003), for 5–6 days a week were at 1.11 times lower likelihood (CI = 1.03–1.21, p = 0.010), for once daily were at 1.15 times lower likelihood (CI = 1.06–1.25, p = 0.001), and for more than once daily were at 1.13 times lower likelihood (CI = 1.04–1.23, p = 0.003) of reporting sleep difficulties. For vegetable consumption, children who reported a higher frequency of eating vegetables were more likely to have a low level of sleep difficulties, such as once a week (OR = 1.08, CI = 1.01–1.16, p = 0.027), for 2–4 days a week (OR = 1.09, CI = 1.03–1.17, p = 0.006), for 5–6 days a week (OR = 1.07, CI = 1.00–1.15, p = 0.042), for once daily (OR = 1.09, CI = 1.02–1.17, p = 0.012) and for more than once daily (OR = 1.09, CI = 1.01–1.16, p = 0.021). However, compared with more than once daily sweets and soft drinks, fewer consumption of them were more likely associated with fewer sleep difficulties (except for 5–6 days). Pseudo R2 of the regression model was 0.012. More details can be found in Table 1.
4. Discussion
This study aims to investigate the association between eating habits and sleep difficulties in children and adolescents using a large sample based on data from the 2013/2014 round of the HBSC survey. Several interesting findings were observed. Firstly, this study found that a high frequency of breakfast consumption is associated with fewer sleep difficulties. Similarly, frequent consumption of vegetables and fruits is significantly associated with fewer sleep difficulties. Conversely, the study found that consuming more sweets and soft drinks (except for 5–6 days per week) is associated with more sleep difficulties. These findings contribute to our understanding of the relationships between eating habits and sleep health in children and adolescents. A more detailed analysis is presented below.
To the best of our knowledge, there is limited evidence regarding the associations between eating habits, particularly specific food types, and sleep difficulties among children and adolescents (26, 27). However, sleep difficulties may be regarded as clinical symptoms of overall sleep quality (25, 28). Therefore, evidence regarding eating habits and sleep quality could be useful for interpreting our research findings. Some previous studies have summarized the preliminary evidence concerning the association between eating habits and sleep quality, indicating that unhealthy eating habits were related to poor sleep quality (26, 28–30). Additionally, studies focused on workers have found that poor eating habits have a significant impact on their sleep quality (31), which is supported by later studies (32, 33). However, sleep patterns differ and change from childhood to adulthood based on various factors. Therefore, focusing on specific age-related populations is necessary. In other words, this study extends the knowledge on the relationships between healthier eating habits and better sleep quality in children and adolescents. We found that better eating habits (such as not skipping breakfast, consuming more fruits and vegetables, and limiting the intake of sweets and soft drinks) were associated with better sleep quality (i.e., fewer sleep difficulties in this study). It is worth noting that previous studies have mainly focused on the comprehensive assessment of sleep quality (28, 29, 34–36), such as using the Pittsburgh Sleep Quality Index. In this study, a single question item was used to collect children and adolescents' self-perceptions of their own sleep quality. The heterogeneity of measurements may limit our understanding of the differences between the findings of this study and other studies, which requires further verification.
Maintaining regular breakfast consumption is of great health significance for children and adolescents, as it promotes mental health (37, 38) and prevents obesity (39, 40). The results of this study indicate that a higher frequency of breakfast consumption is positively associated with better sleep quality, such as fewer sleep difficulties, which is consistent with previous studies conducted on Japanese adolescents (41). Therefore, encouraging children and adolescents to develop regular breakfast eating habits can be beneficial for promoting better sleep quality. A possible explanation for this finding is that regular breakfast consumption is associated with better mental health status, which may contribute to better sleep quality (37, 38, 41).
Synthesized evidence suggests that consuming fruits and vegetables is associated with better sleep quality (35). For example, experimental studies have shown that consuming two kiwifruits per day can significantly improve sleep quality (42). Similarly, cherries have been found to promote better sleep quality (43). In terms of vegetables, a study conducted on Korean adolescents found that consuming more vegetables was associated with better sleep quality, including fewer sleep difficulty symptoms (22), which is supported by similar studies (44, 45). Although evidence on children and adolescents is limited, this collective evidence supports our research statement that consuming more fruits and vegetables is associated with fewer sleep difficulties. Calorie restriction may be a possible mechanism for the association between eating habits and sleep difficulties, as it has been shown to promote better sleep quality (26, 29). Experimental evidence has shown that calorie restriction can be achieved through consuming most fruits and vegetables. Another possible explanation is sleep duration, which is co-dependent with better sleep quality. Appropriate sleep duration is associated with eating habits (28, 34), and healthier eating habits may be associated with better sleep quality based on appropriate sleep duration (29). Additionally, fruits and vegetables are rich in fiber, vitamins, and minerals, and high intake of these nutrients has been linked to better sleep quality (34, 44, 46).
In terms of unhealthy food items, the current study found that consuming more sweets and soft drinks was associated with more sleep difficulties, indicating poorer sleep quality. This finding is supported by some previous survey studies. For example, data from the Korean Youth Risk Behavior Surveillance indicated that poor sleep quality may be associated with higher consumption of sugar-sweetened beverages (22), which supports our finding that increased sweets consumption is related to more sleep difficulties. Many studies have confirmed the negative association between soft drink consumption and sleep quality outcomes (47–50). These previous findings partly corroborate the research findings of our study. One possible explanation for this association involves sugar, as higher sugar intake has been associated with worse sleep quality (51).
Based on the above evidence and analysis, it is reasonable to conclude that children and adolescents with healthier eating habits are more likely to experience better sleep quality. However, it is important to consider some limitations of this study. The adjusted R2 of the model is relatively small, explaining only 1.2% of the variability in sleep difficulty symptoms among young adolescents. Therefore, the findings should be interpreted with caution. Nonetheless, the model can identify potential modifiable factors that are linked to sleep difficulties among young adolescents, providing guidance for developing tailored prevention or early intervention strategies to improve sleep quality. Additionally, the cross-sectional nature of the study means that causality and directionality cannot be established from the research findings. Another limitation is that data on nutritional or food compositions, such as protein intake and carbohydrate intake, as well as some other confounding factors (e.g., developmental disorders), could not be collected due to the measurement protocol. This limitation prevents us from gaining insights into the mechanisms underlying the association between eating habits and sleep difficulties. Furthermore, the current data collected cannot reflect the dietary patterns of the study participants, inhibiting our understanding of the relationship between overall daily diet and sleep quality. It is also important to consider potential overlap between sweets and soft drinks that contain caffeine (53), such as chocolate and cola, and the effects of caffeine on sleep should be studied. Addressing these limitations is promising for generating better evidence for nutritional clinical practice and counselling.
The present study contributes to our understanding of healthy eating guidelines by providing evidence supporting the importance of increasing the frequency of breakfast consumption, as well as the intake of vegetables and fruits, among children and adolescents. Furthermore, the study highlights the need to limit sweets and soft drink consumption to no more than 5–6 days per week due to their negative association with sleep quality.
5. Conclusion
In summary, this study provides evidence on the relationships between dietary habits and sleep challenges in children and adolescents, highlighting the importance of breakfast, fruit, and vegetable consumption, as well as the negative impact of sweets and soft drinks. Prioritizing certain food items from a nutritional improvement standpoint could be highly beneficial in addressing sleep issues. However, due to the limitations of this study, further evidence from cohort and intervention studies is needed to strengthen our understanding of these associations.
Data availability statement
Publicly available datasets were analyzed in this study. This data can be found here: https://www.who.int/europe/initiatives/health-behaviour-in-school-aged-children-(hbsc)-study.
Ethics statement
Ethical review and approval were not required for the study on human participants in accordance with the local legislation and institutional requirements. Written informed consent to participate in this study was provided by the participant's legal guardian/next of kin. Written informed consent to participate in this study was provided by the participants’ legal guardian/next of kin.
Author contributions
Conceptualization, YZ, DQ; writing-original draft preparation, YZ, DQ; writing-review and editing, KL, RB, SC; supervision, DQ, SC; All authors contributed to the article and approved the submitted version.
Funding
YZ was funded by Shandong Social Science Research Project (22CTYJ15).
Acknowledgments
We appreciate the public data that can be used for research.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Jakobsson M, Josefsson K, Högberg K. Reasons for sleeping difficulties as perceived by adolescents: a content analysis. Scand J Caring Sci. (2020) 34(2):464–73. doi: 10.1111/scs.12750
2. Liang M, Guo L, Huo J, Zhou G. Prevalence of sleep disturbances in Chinese adolescents: a systematic review and meta-analysis. PLoS One. (2021) 16(3):e0247333. doi: 10.1371/journal.pone.024733
3. Kronholm E, Puusniekka R, Jokela J, Villberg J, Urrila AS, Paunio T, et al. Trends in self-reported sleep problems, tiredness and related school performance among finnish adolescents from 1984 to 2011. J Sleep Res. (2015) 24(1):3–10. doi: 10.1111/jsr.12258
4. Medic G, Wille M, Hemels ME. Short- and long-term health consequences of sleep disruption. Nat Sci Sleep. (2017) 9:151–61. doi: 10.2147/NSS.S134864
5. Dregan A, Armstrong D. Adolescence sleep disturbances as predictors of adulthood sleep disturbances–a cohort study. J Adolesc Health. (2010) 46(5):482–7. doi: 10.1016/j.jadohealth.2009.11.197
6. Aepli A, Kurth S, Tesler N, Jenni OG, Huber R. Caffeine consuming children and adolescents show altered sleep behavior and deep sleep. Brain Sci. (2015) 5(4):441–55. doi: 10.3390/brainsci5040441
7. Calamaro CJ, Yang K, Ratcliffe S, Chasens ER. Wired at a young age: the effect of caffeine and technology on sleep duration and body mass index in school-aged children. J Pediatr Health Care. (2012) 26(4):276–82. doi: 10.1016/j.pedhc.2010.12.002
8. Hale L, Kirschen GW, LeBourgeois MK, Gradisar M, Garrison MM, Montgomery-Downs H, et al. Youth screen media habits and sleep: sleep-friendly screen behavior recommendations for clinicians, educators, and parents. Child Adolesc Psychiatr Clin N Am. (2018) 27(2):229–45. doi: 10.1016/j.chc.2017.11.014
9. Willis TA, Gregory AM. Anxiety disorders and sleep in children and adolescents. Sleep Med Clin. (2015) 10(2):125–31. doi: 10.1016/j.jsmc.2015.02.002
10. Boergers J, Koinis-Mitchell D. Sleep and culture in children with medical conditions. J Pediatr Psychol. (2010) 35(9):915–26. doi: 10.1093/jpepsy/jsq016
11. Elfhag K, Tholin S, Rasmussen F. Consumption of fruit, vegetables, sweets and soft drinks are associated with psychological dimensions of eating behaviour in parents and their 12-year-old children. Public Health Nutr. (2008) 11(9):914–23. doi: 10.1017/S1368980008002371
12. Northeast RC, Vyazovskiy VV, Bechtold DA. Eat, sleep, repeat: the role of the circadian system in balancing sleep–wake control with metabolic need. Curr Opin Physiol. (2020) 15:183–91. doi: 10.1016/j.cophys.2020.02.003
13. Nakajima K. Unhealthy eating habits around sleep and sleep duration: to eat or fast? World J Diabetes. (2018) 9(11):190–4. doi: 10.4239/wjd.v9.i11.190
14. Meng X, Li Y, Li S, Zhou Y, Gan RY, Xu DP, et al. Dietary sources and bioactivities of melatonin. Nutrients. (2017) 9(4):367. doi: 10.3390/nu9040367
15. Faris ME, Vitiello MV, Abdelrahim DN, Cheikh Ismail L, Jahrami HA, Khaleel S, et al. Eating habits are associated with subjective sleep quality outcomes among university students: findings of a cross-sectional study. Sleep Breath. (2022) 26(3):1365–76. doi: 10.1007/s11325-021-02506-w
16. Bruce ES, Lunt L, McDonagh JE. Sleep in adolescents and young adults. Clin Med. (2017) 17(5):424–8. doi: 10.7861/clinmedicine.17-5-424
17. Biau DJ, Kernéis S, Porcher R. Statistics in brief: the importance of sample size in the planning and interpretation of medical research. Clin Orthop Relat Res. (2008) 466(9):2282–8. doi: 10.1007/s11999-008-0346-9
18. Pengpid S, Peltzer K. Fruit and vegetable consumption is protective from short sleep and poor sleep quality among university students from 28 countries. Nat Sci Sleep. (2020) 12:627–33. doi: 10.2147/NSS.S263922
19. Noorwali E, Hardie L, Cade J. Bridging the reciprocal gap between sleep and fruit and vegetable consumption: a review of the evidence, potential mechanisms, implications, and directions for future work. Nutrients. (2019) 11(6):1382. doi: 10.3390/nu11061382
20. Garaulet M, Ortega FB, Ruiz JR, Rey-López JP, Béghin L, Manios Y, et al. Short sleep duration is associated with increased obesity markers in European adolescents: effect of physical activity and dietary habits. The HELENA study. Int J Obes. (2011) 35(10):1308–17. doi: 10.1038/ijo.2011.149
21. Watson EJ, Coates AM, Banks S, Kohler M. Total dietary sugar consumption does not influence sleep or behaviour in Australian children. Int J Food Sci Nutr. (2018) 69(4):503–12. doi: 10.1080/09637486.2017.1386628
22. Min C, Kim H-J, Park I-S, Park B, Kim J-H, Sim S, et al. The association between sleep duration, sleep quality, and food consumption in adolescents: a cross-sectional study using the Korea youth risk behavior web-based survey. BMJ Open. (2018) 8(7):e022848. doi: 10.1136/bmjopen-2018-022848
23. Roberts C, Freeman J, Samdal O, Schnohr CW, de Looze ME, Nic Gabhainn S, et al. The health behaviour in school-aged children (HBSC) study: methodological developments and current tensions. Int J Public Health. (2009) 54(Suppl 2):140–50. doi: 10.1007/s00038-009-5405-9
24. Gariepy G, McKinnon B, Sentenac M, Elgar FJ. Validity and reliability of a brief symptom checklist to measure psychological health in school-aged children. Child Indic Res. (2016) 9(2):471–84. doi: 10.1007/s12187-015-9326-2
25. Khan A, Reyad MAH, Edwards E, Horwood S. Associations between adolescent sleep difficulties and active versus passive screen time across 38 countries. J Affect Disord. (2023) 320:298–304. doi: 10.1016/j.jad.2022.09.137
26. Binks H, Vincent GE, Gupta C, Irwin C, Khalesi S. Effects of diet on sleep: a narrative review. Nutrients. (2020) 12(4):936. doi: 10.3390/nu12040936
27. Lentjes MAH. The balance between food and dietary supplements in the general population. Proc Nutr Soc. (2019) 78(1):97–109. doi: 10.1017/S0029665118002525
28. Godos J, Grosso G, Castellano S, Galvano F, Caraci F, Ferri R. Association between diet and sleep quality: a systematic review. Sleep Med Rev. (2021) 57:101430. doi: 10.1016/j.smrv.2021.101430
29. St-Onge M-P, Mikic A, Pietrolungo CE. Effects of diet on sleep quality. Adv Nutr. (2016) 7(5):938–49. doi: 10.3945/an.116.012336
30. Zuraikat FM, Wood RA, Barragán R, St-Onge M-P. Sleep and diet: mounting evidence of a cyclical relationship. Annu Rev Nutr. (2021) 41(1):309–32. doi: 10.1146/annurev-nutr-120420-021719
31. Shimura A, Sugiura K, Inoue M, Misaki S, Tanimoto Y, Oshima A, et al. Which sleep hygiene factors are important? Comprehensive assessment of lifestyle habits and job environment on sleep among office workers. Sleep Health. (2020) 6(3):288–98. doi: 10.1016/j.sleh.2020.02.001
32. Hayashida T, Shimura A, Higashiyama M, Fujimura Y, Ono K, Inoue T. Psychosomatic stress responses and sleep disturbance mediate the effects of irregular mealtimes on presenteeism. Neuropsychiatr Dis Treat. (2021) 17:315–21. doi: 10.2147/NDT.S292249
33. Tahara Y, Makino S, Suiko T, Nagamori Y, Iwai T, Aono M, et al. Association between irregular meal timing and the mental health of Japanese workers. Nutrients. (2021) 13(8):2775. doi: 10.3390/nu13082775
34. Peuhkuri K, Sihvola N, Korpela R. Diet promotes sleep duration and quality. Nutr Res. (2012) 32(5):309–19. doi: 10.1016/j.nutres.2012.03.009
35. Wilson K, St-Onge MP, Tasali E. Diet composition and objectively assessed sleep quality: a narrative review. J Acad Nutr Diet. (2022) 122(6):1182–95. doi: 10.1016/j.jand.2022.01.007
36. Ramón-Arbués E, Granada-López J-M, Martínez-Abadía B, Echániz-Serrano E, Antón-Solanas I, Jerue BA. The association between diet and sleep quality among spanish university students. Nutrients. (2022) 14(16):3291. doi: 10.3390/nu14163291
37. Zahedi H, Djalalinia S, Sadeghi O, Zare Garizi F, Asayesh H, Payab M, et al. Breakfast consumption and mental health: a systematic review and meta-analysis of observational studies. Nutr Neurosci. (2022) 25(6):1250–64. doi: 10.1080/1028415X.2020.1853411
38. Ferrer-Cascales R, Sánchez-SanSegundo M, Ruiz-Robledillo N, Albaladejo-Blázquez N, Laguna-Pérez A, Zaragoza-Martí A. Eat or skip breakfast? The important role of breakfast quality for health-related quality of life, stress and depression in spanish adolescents. Int J Environ Res Public Health. (2018) 15(8):1781. doi: 10.3390/ijerph15081781
39. Ardeshirlarijani E, Namazi N, Jabbari M, Zeinali M, Gerami H, Jalili RB, et al. The link between breakfast skipping and overweigh/obesity in children and adolescents: a meta-analysis of observational studies. J Diabetes Metab Disord. (2019) 18(2):657–64. doi: 10.1007/s40200-019-00446-7
40. Okada C, Tabuchi T, Iso H. Association between skipping breakfast in parents and children and childhood overweight/obesity among children: a nationwide 10.5-year prospective study in Japan. Int J Obes. (2018) 42(10):1724–32. doi: 10.1038/s41366-018-0066-5
41. Otsuka Y, Kaneita Y, Itani O, Jike M, Osaki Y, Higuchi S, et al. Skipping breakfast, poor sleep quality, and internet usage and their relation with unhappiness in Japanese adolescents. PLoS One. (2020) 15(7):e0235252. doi: 10.1371/journal.pone.0235252
42. Lin HH, Tsai PS, Fang SC, Liu JF. Effect of kiwifruit consumption on sleep quality in adults with sleep problems. Asia Pac J Clin Nutr. (2011) 20(2):169–74.21669584
43. Garrido M, Paredes SD, Cubero J, Lozano M, Toribio-Delgado AF, Muñoz JL, et al. Jerte valley cherry-enriched diets improve nocturnal rest and increase 6-sulfatoxymelatonin and total antioxidant capacity in the urine of middle-aged and elderly humans. J Gerontol A Biol Sci Med Sci. (2010) 65(9):909–14. doi: 10.1093/gerona/glq099
44. Grandner MA, Jackson N, Gerstner JR, Knutson KL. Sleep symptoms associated with intake of specific dietary nutrients. J Sleep Res. (2014) 23(1):22–34. doi: 10.1111/jsr.12084
45. Ferranti R, Marventano S, Castellano S, Giogianni G, Nolfo F, Rametta S, et al. Sleep quality and duration is related with diet and obesity in young adolescent living in Sicily, Southern Italy. Sleep Sci. (2016) 9(2):117–22. doi: 10.1016/j.slsci.2016.04.003
46. Majid MS, Ahmad HS, Bizhan H, Hosein HZM, Mohammad A. The effect of vitamin D supplement on the score and quality of sleep in 20−50 year-old people with sleep disorders compared with control group. Nutr Neurosci. (2018) 21(7):511–9. doi: 10.1080/1028415X.2017.1317395
47. Galland BC, Gray AR, Penno J, Smith C, Lobb C, Taylor RW. Gender differences in sleep hygiene practices and sleep quality in New Zealand adolescents aged 15 to 17 years. Sleep Health. (2017) 3(2):77–83. doi: 10.1016/j.sleh.2017.02.001
48. Ehlers CL, Wills D, Gilder DA. A history of binge drinking during adolescence is associated with poorer sleep quality in young adult Mexican Americans and American Indians. Psychopharmacology. (2018) 235(6):1775–82. doi: 10.1007/s00213-018-4889-5
49. Ogeil RP, Cheetham A, Mooney A, Allen NB, Schwartz O, Byrne ML, et al. Early adolescent drinking and cannabis use predicts later sleep-quality problems. Psychol Addict Behav. (2019) 33(3):266–73. doi: 10.1037/adb0000453
50. Khan A, Dix C, Burton NW, Khan SR, Uddin R. Association of carbonated soft drink and fast food intake with stress-related sleep disturbance among adolescents: a global perspective from 64 countries. EClinicalMedicine. (2021) 31:100681. doi: 10.1016/j.eclinm.2020.100681
51. St-Onge M-P, Roberts A, Shechter A, Choudhury AR. Fiber and saturated fat are associated with sleep arousals and slow wave sleep. J Clin Sleep Med. (2016) 12(1):19–24. doi: 10.5664/jcsm.5384
52. Moksony F, Heged R. Small is beautiful. The use and interpretation of R2 in social research. Szociol Szle Spec Issue. (1990):130–8.
Keywords: diet, sleep quality, child, adolescent, nutrition
Citation: Zhao Y, Qu D, Liang K, Bao R and Chen S (2023) Eating habits matter for sleep difficulties in children and adolescents: A cross-sectional study. Front. Pediatr. 11:1108031. doi: 10.3389/fped.2023.1108031
Received: 25 November 2022; Accepted: 28 April 2023;
Published: 12 June 2023.
Edited by:
Akiyoshi Shimura, Tokyo Medical University, JapanReviewed by:
Taito Hayashida, Tokyo Medical University Hospital, JapanTenshi Watanabe, Ebara Hospital, Japan
© 2023 Zhao, Qu, Liang, Bao and Chen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Diyang Qu ZGl5YW5ncXVAb3V0bG9vay5jb20=
†These authors share first authorship
 Yaping Zhao
Yaping Zhao Diyang Qu
Diyang Qu Kaixin Liang
Kaixin Liang Ran Bao
Ran Bao Sitong Chen
Sitong Chen