- 1Department of Pediatrics, Children's Hospital Los Angeles, Los Angeles, CA, United States
- 2Keck School of Medicine of University of Southern California, Los Angeles, CA, United States
- 3Department of Pediatrics, Endocrinology and Metabolism, Children's Hospital Los Angeles Center for Diabetes, Los Angeles, CA, United States
Pediatric obesity rates continue to rise steeply with significant adverse effects on health outcomes across the lifespan. Significant obesity can affect the efficacy, side effects, and ability to use certain treatment, medication, or imaging modalities needed in the evaluation and management of acute pediatric conditions. Inpatient settings are rarely used as an opportunity for weight counseling and thus there is a paucity of clinical guidelines on how to manage severe obesity in the inpatient setting. We present a literature review and three patient cases with single-center protocol for non-surgical management of severe obesity in children admitted for other acute medical reasons. We performed a PubMed review from January 2002 to February 2022 utilizing keywords: “inpatient,” “obesity,” and “intervention.” For our cases, we identified three patients with severe obesity acutely impacting their health while admitted for medical treatment who concurrently underwent acute, inpatient, weight loss regimens at a single children's hospital. The literature search yielded 33 articles describing inpatient weight loss treatments. Three patients met case criteria, all three of which demonstrated a decrease in their weight in excess percent of the 95th percentile after inpatient weight-management protocol implementation (% reduction BMIp95: 16%–30%). This highlights obesity acutely limits or impacts specific medical care required during inpatient admissions in pediatric patients. It also suggests that implementation of an inpatient weight-management protocol during admission may provide an opportune setting to support acute weight loss and overall improved health outcomes in this high-risk cohort.
Introduction
One in five children (ages 2–19 years) has obesity in the United States. Pediatric obesity is considered one of the most serious global health problems of this century, with rates projected to increase 130% over the next two decades (1, 2). Hospitals are seeing increased rates of severe pediatric obesity impacting treatment and outcomes for acute hospitalizations, regardless of presenting diagnosis (1, 3–6). Inpatient hospitalization presents an opportunity to engage in nutritional counseling, obesity-related comorbidity screening, and initiation of anti-obesity pharmacotherapy (7, 8). This is similar to screening and counseling for other conditions while inpatient, yet studies show these assessments rarely occur (7, 9, 10). There is minimal data about inpatient obesity interventions, despite the fact that severe obesity affects the acute needs, treatment, and outcomes for many medical conditions in both adult and pediatric cohorts (11). This absence of information presents major challenges to pediatric healthcare systems attempting to provide long-term, comprehensive care for youth with obesity.
Pediatric obesity independently increases morbidity and mortality across the lifespan (4, 5). Obesity has been linked to worse outcomes in hospitalized patients with prolonged length of stay, greater costs, increased infections, and increased post-operative complications (4, 5, 12–14). In pediatrics, specifically, there are significant medication safety risks for youth living with obesity, given that the majority of medications utilized inpatient have weight-based dosing. In fact, three recent reviews found that two-thirds of all prescribed medications in children with obesity were either sub-therapeutic or supra-therapeutic (1, 12, 15).
Despite negative inpatient outcomes, studies show that obesity is rarely documented or considered an important factor in inpatient care, unless it is thought to directly affect the treatment for the acute illness (6, 8). A recent study found that fewer than 40% of children's hospitals have universal policies to identify and treat patients with obesity, with BMI calculated in only 35% of pediatric inpatient encounters (12). This is particularly problematic as adult studies have found that the only factor associated with increased likelihood of treatment for obesity while inpatient was a diagnosis of obesity in the medical record (7). A pediatric study found that a documented diagnosis of obesity was associated with being 35 times more likely to receive interventions while hospitalized (9). Although there is a paucity of literature exploring weight loss counseling during acute hospitalizations, data collected in adults with obesity admitted for non-weight related conditions revealed that the majority of patients with obesity are receptive to weight loss advice while hospitalized (16).
Weight loss, even small percentages, can have long-lasting effects on health, particularly in children. BMI z-score decrease of 0.5 standard deviations has been positively correlated with improved cardiovascular risk profiles and improved lung function (17, 18). Weight loss, in the acute setting, has also been shown to have immediate positive outcomes. This is best exemplified in bariatric surgery literature, which demonstrates pre-operative weight loss is correlated with reduced operative time, blood loss, complications, liver size, and length of stay, and greater weight loss following surgery (19, 20). There is growing evidence that inpatient weight-management programs are more successful at achieving acute weight loss than outpatient treatments (17, 21, 22). In a 2011, 22-study systematic review, there was a 191% greater reduction in individuals with obesity in pediatric inpatient weight loss programs as compared to outpatient (23). In fact, even short-term inpatient weight loss treatments have been shown to be more effective than long-term outpatient intervention (24). Unfortunately, there is little data on how to incorporate weight-management strategies into inpatient encounters in youth with obesity (19).
Given research and treatment gaps for pediatric inpatient obesity management, we conducted a review of inpatient weight-management treatment in both children and adults. The objective of this article is to describe the existing literature on inpatient weight loss treatments and present examples of acute weight loss in hospitalized pediatric patients that may serve as models for future inpatient weight loss interventions. We report three cases of pediatric patients, with severe obesity affecting their immediate hospitalization, and the weight-management treatment they underwent at a single, urban, quaternary care, children's hospital.
Methods
A search was conducted through the PubMed database focused on non-surgical, inpatient, obesity weight loss treatments. The key words included: “inpatient,” “obesity,” and “intervention.” The search terms were intentionally broad to capture relevant studies while preventing omissions. The search was conducted in March 2022 and included date limits of January 2002 through February 2022. Results were screened to include articles reporting on inpatient weight loss treatments for patients with obesity. The search was not narrowed to pediatric patient populations due to the limited number of articles. Initial search of articles was conducted manually by one reviewer (VG). The database search resulted in an initial pool of 208 articles. Articles in languages other than English, and articles outside the defined time period were removed. All records were then independently reviewed by two reviewers (VG and AV) using the inclusion criteria. Given the relatively small number of search results and nuanced subject focus, all articles were evaluated for inclusion rather than having a separate screening phase. Articles that focused primarily on surgical weight loss treatment for obesity were excluded. Discrepancies were resolved through discussion between investigators. Data foci included: date, country, study design, population, duration, primary outcome(s) with results, and weight loss.
Several patient cases of pediatric, inpatient, weight loss from an urban, freestanding children's hospital caring for diverse communities were closely examined and three cases are presented as examples of this intervention. All presented cases include pediatric patients with severe obesity (120% of the 95th percentile for body mass index) for whom acute weight loss was recommended to either improve current health or better prepare for a specific therapy or treatment.
Results
The review examining inpatient weight loss treatments for patients with obesity found 208 results (Figure 1). Four articles were removed for language (n = 3) and publication date (n = 1). The remaining 204 articles were screened and 171 were secondarily excluded due to wrong primary foci including: bariatric surgery (n = 22), other surgery (n = 17), cardiovascular complications (n = 31), outpatient weight loss (n = 24), hospital costs or complications (n = 7), psychiatric/neurologic focus related to obesity (n = 13), non-specific nutrition and exercise: (n = 10), research design or conference presentation (n = 7), diabetes (n = 10), orthopedics (n = 9), hormones and weight association (n = 7), malnutrition (n = 3), and other (n = 11). 33 studies met full criteria, including 23 pediatric and 10 adult studies. Sample sizes ranged from 1 to 1,862 individuals, with four being the youngest age included. Length of interventions ranged from 7 days to 10 months. Publications included 26 clinical trials, 2 case reports, 2 review articles, 1 prospective intervention study, 1 comparative study, and 1 case series. All studies included males and females, except for 1 adult study and single-patient case reports. Results focused on weight loss, psychologic impacts of weight, quality of life, cognitive functioning, eating behaviors, and biochemical parameters associated with weight loss.
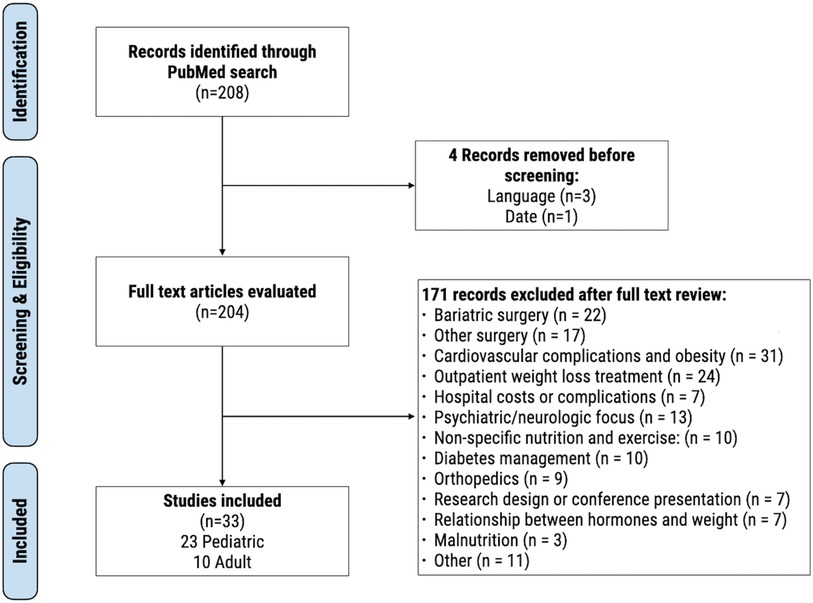
Figure 1. Modified PRISMA flow diagram for our literature search results on inpatient, non-surgical, weight loss interventions for adult and pediatric patients.
Few studies discussed the longevity of the interventions more than one year after the interventions or the recidivism rates. One study examined 3 and 5 year follow ups and demonstrated continued reduction of BMI-SDS (by 0.20 and 0.15 respectively) as well as health related behaviors (24).
Pediatric literature review
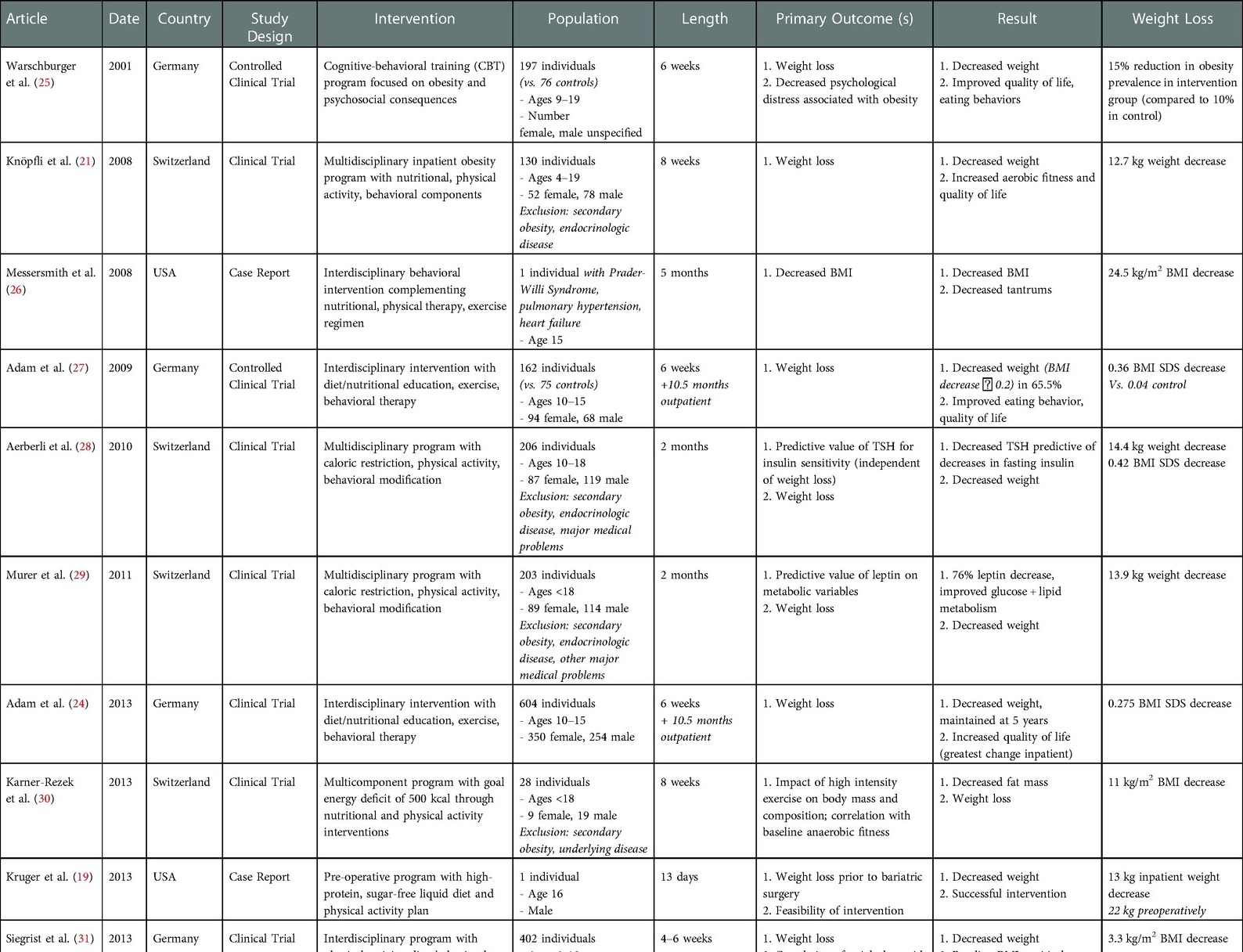
Among the 23 pediatric studies included (Table 1), the ages ranged from 4 to 19 years. There were 18 clinical trials, 2 case reports, 1 prospective intervention study, 1 comparative study, and 1 case series. All studies showed decreased weight in a portion of participants, as indicated by BMI, weight, BMI SDS, fat mass, and other measures. In addition, 5 studies also reported improved quality of life, 3 reported increased athletic fitness (i.e., athletic competence, aerobic fitness), 6 improved behavioral factors, 2 improved cognitive functioning, and 6 improved biochemical parameters.
Adult literature review
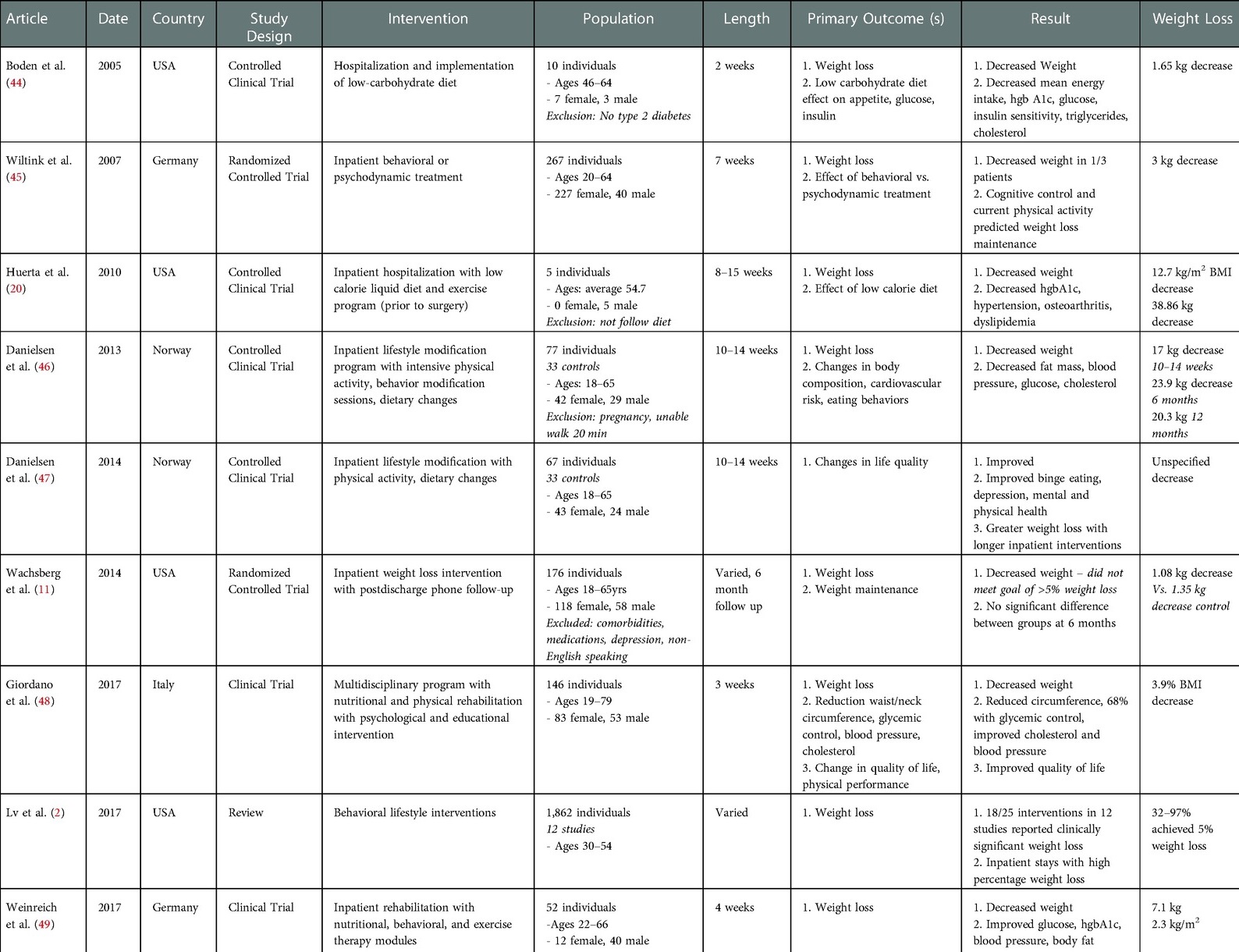
Ten adult studies (18 years and older) were also included (Table 2). There were 8 clinical trials and 2 review articles. Eight of the studies focused on individual weight loss and showed decreased weight. In addition, 5 studies reported improved biochemical parameters, 3 decreased rates of diseases associated with obesity (i.e., hypertension, dyslipidemia), 1 improved mental health, 1 increased fitness, and 2 improved quality of life.
Patient cases
We present three cases of youth with severe obesity who were hospitalized for acute medical problems while we simultaneously addressed weight-management. The severity of obesity in these youth was either impacting their present health or ability to undergo certain medical treatments. All three patients were treated following the inpatient obesity treatment roadmap developed at our institution that includes working with nutritionists, obesity medicine specialists (MD/NP), bedside nurses, and physical therapy to create an individualized nutrition, exercise, and anti-obesity medication plan for each patient (Figure 2).

Figure 2. Model of inpatient obesity treatment roadmap with collaboration of obesity medicine specialists (MD/NP), nutritionists, nurses, and physical therapists to create individualized nutrition, activity, and medical plans for pediatric patients. BMI, body mass index; CMP, comprehensive metabolic panel; MAOI, monoamine oxidase inhibitors; XR, extended release; AKI, acute kidney injury; MTC, medullary thyroid carcinoma; GI, gastrointestinal.
Case 1
Case 1 is a 16-year-old male who presented with well-controlled type 2 diabetes, obstructive sleep apnea (OSA), severe obesity, and acute onset severe back pain with limited mobility. Initial biochemical evaluation was concerning for acute lymphocytic leukemia (ALL), requiring magnetic resonance imaging (MRI) to determine staging and appropriate treatment. However, due to limitations of the MRI machine at the pediatric center, the patient was unable to obtain imaging secondary to body habitus presenting a significant diagnostic challenge. The obesity medicine team was consulted for assistance with acute weight loss to promote ability for accurate diagnosis, prognosis, and initiation of an appropriate treatment regimen for his oncologic process. The patient was admitted to inpatient rehabilitation for two weeks. On admission, his type 2 diabetes was controlled with insulin and metformin and he had a hgA1c of 6.4. However, due to worsening hepatotoxicity, his Metformin was discontinued. Given his new onset AL.L and concern for chemotherapy induced pancreatitis, the oncology team did not feel comfortable starting a glucagon-like peptide 1 (GLP-1) medication. Interventions included placing the patient on the institutional inpatient obesity protocol including: (1) intake with a registered dietitian; (2) dietary composition: 1,500 calorie per day, less than 150 grams of carbohydrates, no sugar-sweetened beverages, 35 grams of fiber, 32 ounces of water; (3) structured mealtimes (3 meals and 2 snacks); (4) daily physical therapy as tolerated; (5) initiation of weight loss medications (phentermine 15 mg daily). One week after initiation of this protocol, his weight was down trending and he was tolerating phentermine without side effect. Given lack of side effects but increasing hunger with goal of continued weight loss in efforts to obtain an MRI, his phentermine was increased to 37.5 mg daily and dietary program intensified to 1,200 calories and less than 100 grams of carbohydrates daily. At admission, his weight was at 190% BMIp95 (Figure 3). Upon discharge and after two weeks after initiation of his individualized weight-management plan, it decreased to 175%BMIp95 and his hgba1c improved to 6.0. He also reported decreased appetite and no side effects throughout his treatment. He continued his outpatient weight-management program with monthly virtual visits with obesity medicine specialists and dietitian. One month after discharge, his %BMI95 had decreased to 165% BMIp95, and by month six, to 160% BMIp95 (associated with a total BMI reduction of 4.85 kg/m2 and BMI z-score reduction of 0.12 standard deviations).
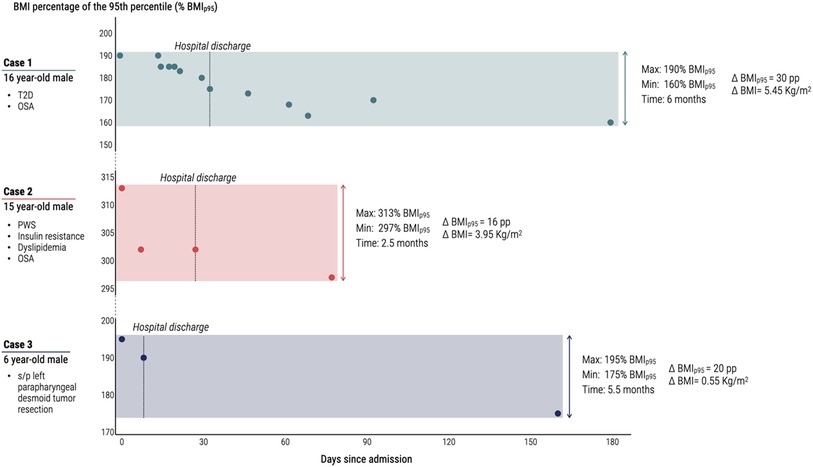
Figure 3. Change in BMI percent of the 95th percentile over time for three pediatric cases of inpatient obesity medical management. T2D, type 2 diabetes; OSA, Obstructive Sleep Apnea; PWS, Prader-Willi Syndrome; BMI, body mass index; Kg/m2, kilograms per meter squared; % BMIp95, BMI percentage of the 95th percentile; pp, percentage points; ΔBMIp95, change in BMI percentage of the 95th percentile; ΔBMI, change in absolute BMI.
Case 2
Case 2 is a 15-year-old male with Prader-Willi Syndrome, class III obesity, impaired fasting glucose, hypertriglyceridemia, and obstructive sleep apnea (OSA) controlled on continuous positive air pressure (CPAP) admitted for acute respiratory failure and placed on a ventilator. Patient had a history of excessive weight gain due to hyperphagia associated with significant anxiety exacerbated by the Covid-19 pandemic. Outpatient, he was taking Metformin 1,000 mg twice daily and Topiramate 100 mg nightly for off-label weight control. Family had completed three, intensive outpatient lifestyle modifications programs and set up a food safe zone (locked cabinets and food storage units) with limited success. Upon admission, he had a 40-pound gain since his last outpatient encounter four months prior and his respiratory function had worsened significantly in response to this weight gain with blood gases demonstrating carbon dioxide retention levels in the upper 70s. He underwent extensive evaluation for hypertension, cardiac dysfunction, and worsening obstructive sleep apnea and his acutely worsened respiratory status was thought to be largely secondarily to his weight gain. This evaluation included a normal electrocardiogram, echocardiogram and renal ultrasound. He underwent a polysomnography which was abnormal due to breath stacking, hyperventilation, and hypoxemia for which his CPAP machine was adjusted. He also had a number of screening labs during his hospitalization with normal thyroid function (TSH 2.62 uIU/ml, T4 7.5 mcg/dl), free cortisol (0.18), ACTH (21) hgbA1c (5.3%), lipid panel (triglycerides 94, total cholesterol 150). Notably he had low testosterone (Free 2.09 ng/dl, total 83 ng/dl), LH (0.31 mIU/mL), FSH (<0.66 mIU/ml), IGF-1(26 ng/ml) and IGF-BP3 and (0.8 mg/L) ultimately started on 100 mg Testosterone supplementation.
The obesity medicine team was consulted by pulmonology to address diagnostic and treatment challenges by supporting acute weight loss interventions while inpatient. This was in an effort to optimize respiratory control for ability to discharge home. The personalized intervention for this patient included placing him on the institutional inpatient obesity protocol including: (1) intake with a registered dietitian; (2) dietary composition: 800 calories daily, less than 90 grams of carbohydrates, no sugar-sweetened beverages, 35 grams of fiber, 32 ounces of water; (3) structured mealtimes (2 meals and 2 snacks); (4) daily physical therapy as tolerated; (5) optimization of weight loss medication regimen (topiramate increased to 200 mg nightly and initiation of semaglutide 0.25 mg weekly). He remained admitted to the rehabilitation unit for one month, during which, his %BMIp95 decreased from 313% to 300% BMIp95 (Figure 3). At the same time, his ventilatory needs decreased with successful transition to continuous positive airway pressure (CPAP) overnight and oxygen by nasal cannula during the day, allowing for safe discharge home. He reported no side effects from the medications during this time period. Given lack of side effects and meeting goal of decreasing respiratory support, no further medication changes were made inpatient. Upon discharge, he was enrolled in the outpatient weight-management program and attended monthly visits with obesity medicine specialists and dietitian. Two and a half months after discharge, his weight had decreased to 297% BMIp95 (associated with a total BMI reduction of 1.2 kg/m2 and BMI z-score reduction of 0.01 standard deviations). His triglycerides and hgba1c were stable at 94 and 5.3% respectively at this time and Testosterone increased with injections.
Case 3
Case 3 is a 6-year-old male with history of a parapharyngeal desmoid tumor resected in June 2019, who had subsequent weight gain of 20 kg over the next two years in association with the Covid-19 pandemic. He was getting serial MRIs with sedation for tumor monitoring, which required admission for respiratory support in the context of his obesity. The obesity medicine team was consulted by oncology and anesthesiology to support acute weight loss interventions while inpatient in an effort to minimize airway risk with his recurrent sedation needs. He was placed on the institutional inpatient obesity protocol including: (1) intake with a registered dietitian; (2) dietary composition: 1,200 calories daily, less than 100 grams of carbohydrates, no sugar-sweetened beverages, 35 grams of fiber, 32 ounces of water; (3) structured mealtimes (3 meals and 2 snacks); and (4) thirty minutes of moderate intensity physical activity daily. One challenge the obesity medicine team faced during the goal of acute weight loss was parental preference not to start anti-obesity medications. He did continue to have normal Hgb A1c (5.1–5.2%) as well as normal lipid panel (triglycerides 74, total cholesterol 161) but elevated alanine aminotransferase and aspartate aminotransferase of 62 and 48 respectively. He remained admitted to the rehabilitation unit for one week with associated weight stabilization. Upon discharge, he was enrolled in the outpatient weight-management program and met with obesity medicine specialists and a dietitian monthly. Five months after discharge, his weight had decreased from 195% BMIp95 to 175% BMIp95 (Figure 3).
Discussion
Pediatric obesity affects acute, inpatient management of non-weight related conditions by impeding efficiency of diagnostic work-ups, delaying diagnosis, limiting efficacy of medications, and contributing to longer hospital stays and higher rates of complications (4, 12, 13, 50–54). Despite severe obesity directly impacting patient care, safety, and costs, there is minimal guidance on when or how to intervene for weight-management in the inpatient settings. Overall, studies reveal that nutrition and weight-management protocols or universal counseling are limited while inpatient, even though inpatient treatments are typically most effective, which suggest there is a need and an opportunity to fill this treatment/intervention gap in research and clinical practice (10, 22, 23).
This review highlights the paucity of data available on inpatient weight-management interventions. Two categories of studies came out of this investigation: (1) inpatient admission for the purpose of weight-management (75% of studies included) and (2) weight-management as a component of an inpatient admission for another acute condition. Consistently, studies that compare inpatient vs. outpatient weight-management interventions show greater weight loss in the inpatient arm of the interventions. It is well-reported in the literature that controlled nutrition trials often have greatest success for weight-management across the lifespan, however there are challenges in incorporating those treatment strategies into real-world settings. Despite successes of inpatient weight-management interventions, the labor and cost required to implement them are significant and the disruption to an individual's daily schedule often prevents them from being enacted on a larger scale. However, even when patients are admitted for treatment of other conditions, we can learn from these studies on how to best harness successful treatment strategies and utilize hospitalization time, which creates an opportunity to start weight-management conversations and care (26, 29, 44).
With growing rates of obesity in youth, there is a pressing need to understand how to optimally address obesity within the inpatient setting. Our single center experiences highlight examples of how these needs arise and how there are rarely clear guidelines on how to consider weight-management during hospitalizations. This gap led our team to create a roadmap for addressing pediatric obesity within inpatient settings. Given growing number of multi-disciplinary, pediatric outpatient weight-management programs, there exists an opportunity to learn from these outpatient practices and design protocols supporting youth with obesity, regardless of health system setting– outpatient or inpatient. At our center, this team consists of the following: endocrinology, obesity medicine, nursing, hospital medicine, physical therapy, dietitians, and rehab specialists. To create our protocol, we referenced current clinical practice guidelines for pediatric obesity medicine, and incorporated weight loss medications, prescriptive nutrition, and activity plans focused around a structured-day approach. Each plan is individualized to the youth's medical needs and acute weight loss goals, as determined by primary team. It also incorporates transition plans from inpatient to outpatient settings. Longitudinal controlled trials are required to further investigate how inpatient protocols can be utilized and to determine the most appropriate evidenced-based strategy to support both acute weight loss and maintenance over time (55, 56).
Our case series show that multi-disciplinary execution of an inpatient obesity protocol can result in BMI reduction and support timely diagnostic work-up, safe treatment, and improved outcomes in the short term. Importantly, long term follow up is necessary to ensure continued weight loss or maintenance. All three of our cases demonstrated acute weight-loss allowing for decreased respiratory support needs and/or the ability to obtain important diagnostic imaging. No significant side effects were reported by the individuals. The adolescent patients (Case 1 and Case 2) described gratefulness for the weight loss interventions because it presented them opportunities to take control of an important aspect of their health. The patient in Case 1 reported feeling a lack of control with their new diagnosis of cancer and a relief with this achievable focus of weight loss. The parents of the patient in Case 3 reported appreciation for treating obesity as a medical disease and reducing stigma. Given the hope for longevity with these weight loss interventions, it was important to our team that the patients also felt empowered and had a realistic plan for home after their inpatient hospitalizations.
Limitations
Naturally, this review is not without limitations. First, by including “inpatient,” “obesity,” and “intervention” as our search terms, we may have excluded studies using synonyms. We only searched PubMed, so may have missed articles in other databases, but felt PubMed would be the most comprehensive source of literature relevant to inpatient pediatric obesity interventions. We also excluded non-English literature, while including literature from other countries. Second, the significant differences in methodology and reported data complicate any quantitative comparison across studies. Additionally, few studies report information on non-completers of the interventions or other potential confounding factors, so selection bias may have affected some outcomes. Limitations of our case series include only examining three patients of different ages with varied length of inpatient stays, comorbidities, and medications. Additionally, our patient follow up was confined to 6 months following hospital discharge and it is important to note that weight loss or weight maintenance requires long term follow-up and often individuals may gain weight back. Our focus was on weight loss in the acute setting to assist with specific medical needs including ability to obtain imaging or treat acute illness.
Conclusions
The prevalence of pediatric obesity continues to rise. Obesity impacts acute inpatient management of pediatric conditions by resulting in delays in diagnosis, compromised treatment plans, prolonged lengths of stay, and higher complication rates, which all contribute to increased health care costs and worse outcomes. The limited studies addressing this topic demonstrate that weight-management can and should be considered in an inpatient setting, either as the primary outcome or as an adjunct to other medical treatment. Further investigation is required to design and implement inpatient weight-management protocols for youth with obesity while hospitalized.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
Ethics statement
Verbal consent and assent from the minor(s)' legal guardian/next of kin was obtained and documented in our medical records for the publication of any potentially identifiable images or data included in this article.
Author contributions
VEG has first authorship, JCE has senior authorship, APV has last authorship. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work. All authors contributed to the article and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Kyler KE, Wagner J, Hosey-Cojocari C, Watt K, Shakhnovich V. Drug dose selection in pediatric obesity: available information for the most commonly prescribed drugs to children. Paediatr Drugs. (2019) 21(5):357–69. doi: 10.1007/s40272-019-00352-8
2. Lv N, Azar KMJ, Rosas LG, Wulfovich S, Xiao L, Ma J. Behavioral lifestyle interventions for moderate and severe obesity: a systematic review. Prev Med. (2017) 100:180–93. doi: 10.1016/j.ypmed.2017.04.022
3. Okubo Y, Handa A. The impact of obesity on pediatric inpatients with urinary tract infections in the United States. J Pediatr Urol. (2017) 13(5):455.e1–e5. doi: 10.1016/j.jpurol.2017.03.038
4. Okubo Y, Nochioka K, Testa MA. The impact of pediatric obesity on hospitalized children with lower respiratory tract infections in the United States. Clin Respir J. (2018) 12(4):1479–84. doi: 10.1111/crj.12694
5. Bechard LJ, Rothpletz-Puglia P, Touger-Decker R, Duggan C, Mehta NM. Influence of obesity on clinical outcomes in hospitalized children: a systematic review. JAMA Pediatr. (2013) 167(5):476–82. doi: 10.1001/jamapediatrics.2013.13
6. Siddiqui H, Katzow M, Homel P. Obesity among inpatient pediatrics: Prevalence and predictors of provider recognition and management. Elk grove, IL, USA: American Academy of Pediatrics Elk Grove Village (2018).
7. Salazar-Sepúlveda LL, Villarreal-Pérez JZ. Impact of diagnosis of overweight and obesity on weight management among hospitalized patients. Obes Res Clin Pract. (2019) 13(2):164–7. doi: 10.1016/j.orcp.2019.01.003
8. Rees M, Collins CE, De Vlieger N, McDonald VM. Non-Surgical interventions for hospitalized adults with class II or class III obesity: a scoping review. Diabetes Metab Syndr Obes. (2021) 14:417–29. doi: 10.2147/DMSO.S280735
9. Myers J, Werk LN, Hossain MJ, Lawless S. Quality improvement project to promote identification and treatment of children with obesity admitted to hospital. Am J Med Qual. (2020) 35(5):411–8. doi: 10.1177/1062860619898534
10. Bradford K, Kihlstrom M, Pointer I, Skinner AC, Slivka P, Perrin EM. Parental attitudes toward obesity and overweight screening and communication for hospitalized children. Hosp Pediatr. (2012) 2(3):126–32. doi: 10.1542/hpeds.2011-0036
11. Wachsberg KN, Creden A, Workman M, Lichten A, Basil A, Lee J, et al. Inpatient obesity intervention with postdischarge telephone follow-up: a randomized trial. J Hosp Med. (2014) 9(8):515–20. doi: 10.1002/jhm.2215
12. Halvorson EE, Irby MB, Skelton JA. Pediatric obesity and safety in inpatient settings: a systematic literature review. Clin Pediatr (Phila). (2014) 53(10):975–87. doi: 10.1177/0009922814533406
13. Biener AI, Cawley J, Meyerhoefer C. The medical care costs of obesity and severe obesity in youth: an instrumental variables approach. Health Econ. (2020) 29(5):624–39. doi: 10.1002/hec.4007
14. Warschburger P, Kühne D. Psychosocial determinants of quality of life in parents of obese children seeking inpatient treatment. Qual Life Res. (2014) 23(7):1985–95. doi: 10.1007/s11136-014-0659-y
15. Johnson PN, Skrepnek GH, Golding CL, Owora AH, Thomas AN, Miller JL. Relationship between rate of fentanyl infusion and time to achieve sedation in nonobese and obese critically ill children. Am J Health Syst Pharm. (2017) 74(15):1174–83. doi: 10.2146/ajhp160230
16. Harris CM, Cheskin LJ, Khaliq W, Antoine D, Landis R, Steinberg EM, et al. Hospitalists’ utilization of weight loss resources with discharge texts and primary care contact: a feasibility study. Hosp Pract (1995). (2016) 44(2):98–102. doi: 10.1080/21548331.2016.1155396
17. van der Baan-Slootweg O, Benninga MA, Beelen A, van der Palen J, Tamminga-Smeulders C, Tijssen JG, et al. Inpatient treatment of children and adolescents with severe obesity in The Netherlands: a randomized clinical trial. JAMA Pediatr. (2014) 168(9):807–14. doi: 10.1001/jamapediatrics.2014.521
18. Eslick S, Jensen ME, Collins CE, Gibson PG, Hilton J, Wood LG. Characterising a weight loss intervention in obese asthmatic children. Nutrients. (2020) 12(2):507–512. doi: 10.3390/nu12020507
19. Kruger AJ, Hrovat KB, Xanthakos SA, Inge TH. Preparation of a severely obese adolescent for significant and long-term weight loss: an illustrative case. Pediatr Surg Int. (2013) 29(8):835–9. doi: 10.1007/s00383-013-3311-y
20. Huerta S, Li Z, Anthony T, Livingston EH. Feasibility of a supervised inpatient low-calorie diet program for massive weight loss prior to RYGB in superobese patients. Obes Surg. (2010) 20(2):173–80. doi: 10.1007/s11695-009-0001-x
21. Knöpfli BH, Radtke T, Lehmann M, Schätzle B, Eisenblätter J, Gachnang A, et al. Effects of a multidisciplinary inpatient intervention on body composition, aerobic fitness, and quality of life in severely obese girls and boys. J Adolesc Health. (2008) 42(2):119–27. doi: 10.1016/j.jadohealth.2007.08.015
22. Rank M, Siegrist M, Wilks DC, Haller B, Wolfarth B, Langhof H, et al. Long-term effects of an inpatient weight-loss program in obese children and the role of genetic predisposition-rationale and design of the LOGIC-trial. BMC Pediatr. (2012) 12:30. doi: 10.1186/1471-2431-12-30
23. Kelly KP, Kirschenbaum DS. Immersion treatment of childhood and adolescent obesity: the first review of a promising intervention. Obes Rev. (2011) 12(1):37–49. doi: 10.1111/j.1467-789X.2009.00710.x
24. Adam S, Westenhoefer J, Rudolphi B, Kraaibeek HK. Three- and five-year follow-up of a combined inpatient-outpatient treatment of obese children and adolescents. Int J Pediatr. (2013) 2013:856743. doi: 10.1155/2013/856743
25. Warschburger P, Fromme C, Petermann F, Wojtalla N, Oepen J. Conceptualisation and evaluation of a cognitive-behavioural training programme for children and adolescents with obesity. Int J Obes Relat Metab Disord. (2001) 25(Suppl 1):S93–5. doi: 10.1038/sj.ijo.0801708
26. Messersmith NV, Slifer KJ, Pulbrook-Vetter V, Bellipanni K. Interdisciplinary behavioral intervention for life-threatening obesity in an adolescent with prader-willi syndrome - a case report. J Dev Behav Pediatr. (2008) 29(2):129–34. doi: 10.1097/DBP.0b013e31815f24bd
27. Adam S, Westenhofer J, Rudolphi B, Kraaibeek HK. Effects of a combined inpatient-outpatient treatment of obese children and adolescents. Obes Facts. (2009) 2(5):286–93. doi: 10.1159/000234415
28. Aeberli I, Jung A, Murer SB, Wildhaber J, Wildhaber-Brooks J, Knöpfli BH, et al. During rapid weight loss in obese children, reductions in TSH predict improvements in insulin sensitivity independent of changes in body weight or fat. J Clin Endocrinol Metab. (2010) 95(12):5412–8. doi: 10.1210/jc.2010-1169
29. Murer SB, Knöpfli BH, Aeberli I, Jung A, Wildhaber J, Wildhaber-Brooks J, et al. Baseline leptin and leptin reduction predict improvements in metabolic variables and long-term fat loss in obese children and adolescents: a prospective study of an inpatient weight-loss program. Am J Clin Nutr. (2011) 93(4):695–702. doi: 10.3945/ajcn.110.002212
30. Karner-Rezek K, Knechtle B, Fenzl M, Schlegel C, Konrad M, Rosemann T. The effects of an 8-week multicomponent inpatient treatment program on body composition and anaerobic fitness in overweight and obese children and adolescents. Int J Gen Med. (2013) 6:159–66. doi: 10.2147/IJGM.S40187
31. Siegrist M, Rank M, Wolfarth B, Langhof H, Haller B, Koenig W, et al. Leptin, adiponectin, and short-term and long-term weight loss after a lifestyle intervention in obese children. Nutrition. (2013) 29(6):851–7. doi: 10.1016/j.nut.2012.12.011
32. Verbeken S, Braet C, Goossens L, van der Oord S. Executive function training with game elements for obese children: a novel treatment to enhance self-regulatory abilities for weight-control. Behav Res Ther. (2013) 51(6):290–9. doi: 10.1016/j.brat.2013.02.006
33. Vrablík M, Dobiášová M, Zlatohlávek L, Urbanová Z, Češka R. Biomarkers of cardiometabolic risk in obese/overweight children: effect of lifestyle intervention. Physiol Res. (2014) 63(6):743–52. doi: 10.33549/physiolres.932895
34. Kokkvoll A, Grimsgaard S, Steinsbekk S, Flægstad T, Njølstad I. Health in overweight children: 2-year follow-up of finnmark activity school–a randomised trial. Arch Dis Child. (2015) 100(5):441–8. doi: 10.1136/archdischild-2014-307107
35. Halberstadt J, van Strien T, de Vet E, Eekhout I, Braet C, Seidell JC. The association of eating styles with weight change after an intensive combined lifestyle intervention for children and adolescents with severe obesity. Appetite. (2016) 99:82–90. doi: 10.1016/j.appet.2015.12.032
36. Koot BG, van der Baan-Slootweg OH, Vinke S, Bohte AE, Tamminga-Smeulders CL, Jansen PL, et al. Intensive lifestyle treatment for non-alcoholic fatty liver disease in children with severe obesity: inpatient versus ambulatory treatment. Int J Obes (Lond). (2016) 40(1):51–7. doi: 10.1038/ijo.2015.175
37. Schiel R, Kaps A, Stein G, Steveling A. Identification of predictors for weight reduction in children and adolescents with overweight and obesity (IDA-insel survey). Healthcare (Basel). (2016) 4(1):31–39. doi: 10.1016/j.zefq.2016.06.001
38. Taylor SJ, Peterson MA, Garland BH, Hastings ES. Comprehensive obesity evaluation and treatment of three adolescents: a case series. Int J Adolesc Med Health. (2016) 28(1):25–9. doi: 10.1515/ijamh-2014-0064
39. Warschburger P, Kroeller K, Haerting J, Unverzagt S, van Egmond-Fröhlich A. Empowering parents of obese children (EPOC): a randomized controlled trial on additional long-term weight effects of parent training. Appetite. (2016) 103:148–56. doi: 10.1016/j.appet.2016.04.007
40. Vantieghem S, Bautmans I, Guchtenaere A, Tanghe A, Provyn S. Improved cognitive functioning in obese adolescents after a 30-week inpatient weight loss program. Pediatr Res. (2018) 84(2):267–71. doi: 10.1038/s41390-018-0047-3
41. Miguet M, Beaulieu K, Fillon A, Khammassi M, Masurier J, Lambert C, et al. Effect of a 10-month residential multidisciplinary weight loss intervention on food reward in adolescents with obesity. Physiol Behav. (2020) 223:112996. doi: 10.1016/j.physbeh.2020.112996
42. Thivel D, Julian V, Miguet M, Pereira B, Beaulieu K, Finlayson G, et al. Introducing eccentric cycling during a multidisciplinary weight loss intervention might prevent adolescents with obesity from increasing their food intake: the TEXTOO study. Physiol Behav. (2020) 214:112744. doi: 10.1016/j.physbeh.2019.112744
43. Khammassi M, Isacco L, Pereira B, Damaso AR, Matlosz P, Maruszczak K, et al. Cardiometabolic efficacy of multidisciplinary weight loss interventions is not altered in adolescents with obesity initially diagnosed or with a persistent metabolic syndrome. Nutr Res. (2021) 86:79–87. doi: 10.1016/j.nutres.2020.12.008
44. Boden G, Sargrad K, Homko C, Mozzoli M, Stein TP. Effect of a low-carbohydrate diet on appetite, blood glucose levels, and insulin resistance in obese patients with type 2 diabetes. Ann Intern Med. (2005) 142(6):403–11. doi: 10.7326/0003-4819-142-6-200503150-00006
45. Wiltink J, Dippel A, Szczepanski M, Thiede R, Alt C, Beutel ME. Long-term weight loss maintenance after inpatient psychotherapy of severely obese patients based on a randomized study: predictors and maintaining factors of health behavior. J Psychosom Res. (2007) 62(6):691–8. doi: 10.1016/j.jpsychores.2006.12.014
46. Danielsen KK, Svendsen M, Mæhlum S, Sundgot-Borgen J. Changes in body composition, cardiovascular disease risk factors, and eating behavior after an intensive lifestyle intervention with high volume of physical activity in severely obese subjects: a prospective clinical controlled trial. J Obes. (2013) 2013:325464. doi: 10.1155/2013/325464
47. Danielsen KK, Sundgot-Borgen J, Mæhlum S, Svendsen M. Beyond weight reduction: improvements in quality of life after an intensive lifestyle intervention in subjects with severe obesity. Ann Med. (2014) 46(5):273–82. doi: 10.3109/07853890.2013.874660
48. Giordano F, Berteotti M, Budui S, Calgaro N, Franceschini L, Gilli F, et al. Multidimensional improvements induced by an intensive obesity inpatients rehabilitation programme. Eat Weight Disord. (2017) 22(2):329–38. doi: 10.1007/s40519-017-0393-x
49. Weinreich T, Filz HP, Gresser U, Richartz BM. Effectiveness of A four-week diet regimen, exercise and psychological intervention for weight loss. J Clin Diagn Res. (2017) 11(3):Lc20-lc4. doi: 10.7860/JCDR/2017/24112.9553
50. Corwin A, Aresty A, Chong S, Brunsvold M, Evans JR, Gillespie RB, et al. Will they fit? Development of a measurement device to assess body habitus compatibility with MRI bore diameter for emergency trauma imaging. Emerg Radiol. (2012) 19(2):141–8. doi: 10.1007/s10140-011-1010-3
51. Ghanem MA, Kazim NA, Elgazzar AH. Impact of obesity on nuclear medicine imaging. J Nucl Med Technol. (2011) 39(1):40–50. doi: 10.2967/jnmt.110.078881
52. Gupta N, Karol I, Kumar Y, Rapillo B, Soni N, Hayashi D. Modified technique for imaging the wrist and elbow in obese and claustrophobic patients using a non-open standard MRI scanner. Skeletal Radiol. (2019) 48(4):615–9. doi: 10.1007/s00256-018-2988-3
53. Maley N, Gebremariam A, Odetola F, Singer K. Influence of obesity diagnosis with organ dysfunction, mortality, and resource use among children hospitalized with infection in the United States. J Intensive Care Med. (2017) 32(5):339–45. doi: 10.1177/0885066616631325
54. Marcus CL, Brooks LJ, Draper KA, Gozal D, Halbower AC, Jones J, et al. Diagnosis and management of childhood obstructive sleep apnea syndrome. Pediatrics. (2012) 130(3):576–84. doi: 10.1542/peds.2012-1671
55. Barlow SE. Expert committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: summary report. Pediatrics. (2007) 120(Suppl 4):S164–92. doi: 10.1542/peds.2007-2329C
Keywords: case report, weight management, inpatient hospitalization, obesity, weight loss
Citation: Goldman VE, Espinoza JC and Vidmar AP (2023) Inpatient medical management of severe pediatric obesity: Literature review and case reports. Front. Pediatr. 11:1095144. doi: 10.3389/fped.2023.1095144
Received: 10 November 2022; Accepted: 17 January 2023;
Published: 13 February 2023.
Edited by:
Annalisa Terranegra, Sidra Medicine, QatarReviewed by:
Susma Vaidya, Children's National Hospital, United StatesInge Gies, Vrije Universiteit Brussel, Belgium
© 2023 Goldman, Espinoza and Vidmar. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Alaina P. Vidmar YXZpZG1hckBjaGxhLnVzYy5lZHU=
Specialty Section: This article was submitted to Pediatric Obesity, a section of the journal Frontiers in Pediatrics
Abbreviations BMI, Body mass index; zBMI, Body mass index Z-score; %BMIp95, Body mass index percent of the 95th percentile
 Victoria E. Goldman
Victoria E. Goldman Juan C. Espinoza
Juan C. Espinoza Alaina P. Vidmar
Alaina P. Vidmar