- 1Evaluation and Research, Judi’s House/JAG Institute for Grieving Children and Families, Aurora, CO, United States
- 2Department of Family Medicine, University of Colorado School of Medicine, Aurora, CO, United States
- 3Department of Biostatistics and Informatics, Colorado School of Public Health, Aurora, CO, United States
- 4Department of Counseling Psychology, University of Denver, Denver, CO, United States
- 5Departments of Psychiatry and Pediatrics, University of Colorado School of Medicine, Aurora, CO, United States
The COVID-19 pandemic devastated public welfare worldwide, bringing excess deaths connected to causes such as homicide, substance abuse, and heart disease. In the U.S., these mortality increases disproportionally impacted communities of color and contributed to a rise in bereavement among adults and children. The death of an important person is one of the most frequently reported disruptive childhood experiences. According to 2023 Childhood Bereavement Estimation Model (CBEM) results, one in 14 U.S. children will experience the death of a parent by age 18. The current study analyzes the impact of the pandemic on childhood bereavement due to parent death by comparing CBEM results for 2021 and 2020 to the average of annual results for 2016 through 2019 for combined U.S. Census race and Hispanic origin categories. Analyses demonstrate that more than 700,000 U.S. children were newly bereaved due to a parent's death in 2020 and 2021. 2020 increases were observed for each race and Hispanic origin population, ranging from 14.9% to 72.4% compared to the 2016–2019 annual average. Hispanic Asian Pacific Islander and Hispanic Black youth experienced the largest percentage increases, while non-Hispanic white youth experienced the smallest. The results contribute to the growing evidence documenting longstanding and enduring disparities in critical U.S. health outcomes based on race and Hispanic origin. Recommendations for the scale and focus of efforts to understand and address bereavement in a way that accommodates the rising need for support in diverse populations to help all bereaved children find hope and healing are offered.
Introduction
For most of 2020, SARS-CoV-2 (COVID-19) assaulted United States (U.S.) economic and cultural practices. By late summer, the virus aggressively pushed its way into the leading causes of mortality, accounting for 1 in 8 deaths in the country (1). Simultaneously other death causes increased (2) as mental health concerns soared (3), and decreased access to health care left many uncertain about best practices in maintaining and addressing physical health. While the long-term repercussions of COVID-19 will be studied for decades, one clear effect is an increase in bereavement.
Early estimates show that for each COVID-19 death, nine close friends and family members are bereaved, including thousands of children under 18 (4). Early in the pandemic, virus-related mortality overwhelmingly impacted older adults aged 70 and over—individuals less likely to have children 0–17. As the pandemic continued, the novel coronavirus mutated, and new variants emerged. Late in 2020 and throughout 2021, despite the availability of vaccines, mortality due to the virus increased, the average age of death attributed to the virus decreased (5), and bereavement rates for children under 18 grew steadily. The pandemic's impacts on bereavement reached well beyond direct mortality due to COVID-19, as increases were noted in other leading causes of death. For example, U.S. mortality due to accidental drug overdose has risen for the past two decades, yet overdose deaths spiked more than 31% in 2020, the first year of the pandemic (6). This trend continued in 2021 when the age-adjusted rate of overdose deaths increased by 14% compared to 2020 (7). Similar findings from 2020 to 2021 demonstrate greater than expected adult mortality in all disease conditions except cancer, with the largest increases resulting from accidents, including injuries, assaults, and homicides (8).
The death of a parent during childhood is an adverse experience that increases risks for future behavioral health (9–12), academic (13), and relational problems (14), as well as suicide (15) and earlier mortality (16). Given the potential for disruptive grief reactions with significant short- and long-term consequences, the American Psychiatric Association included Prolonged Grief Disorder in a 2022 text revision of the Diagnostic and Statistical Manual 5, including developmental considerations for children and adolescents (17). The concept of grief as a “disorder” is widely debated in the childhood bereavement field. Estimates show that 10% (18) to 18% (19) of bereaved youth meet the criteria for a diagnosis. Most bereaved children look to their caregivers, peers, and community for support to navigate loss. A recent systematic literature review reflects positive outcomes for bereaved children following participation in preventative interventions aimed at promoting healthy adaptation to the death of a parent (20). Despite this evidence, there is limited access to preventive interventions that have the potential to reduce risk and promote well-being in bereaved youth and families (21). These resources are even more limited in communities with scarce financial, social, and health safety nets.
Despite the clear evidence that childhood bereavement can lead to negative outcomes, efforts to estimate childhood bereavement prevalence rates have been hampered by methodological, reporting, and data source limitations. In the absence of national bereavement tracking systems in the U.S., a statistical estimation model was developed to quantify this public health issue. The Childhood Bereavement Estimation Model (CBEM) is a theory-based probability model incorporating life-table modeling techniques. Burns et al. (22) describe how the CBEM evaluates an input dataset of age-based population, mortality, and natality data for distinct geographies to generate estimates. The CBEM uses publicly available data and incorporates a series of assumptions to derive bereavement estimates. Model results demonstrate fluctuations in childhood bereavement prevalence related to geographic location, age, population density, cause of death, and race and ethnicity. The CBEM offers social service, community support, and health professionals a tool for raising awareness about the magnitude of childhood bereavement and assessing the need for grief services within specific localities. CBEM results ultimately play a role in equipping communities to develop effective preventive bereavement interventions for children that are inclusive and accessible.
Pre-pandemic CBEM results demonstrated that Black and Indigenous children comprise a disproportionate share of bereaved youth in the U.S. (23). For example, Black youth accounted for 16.7% of the U.S. population under age 18, yet they made up 23.9% of bereaved children, a 43% overrepresentation. Analyzing CDC provisional death data from February 2020 to January 2021, Kidman and colleagues (24) estimated a 17.5%–20.2% increase in childhood bereavement due to parent death absent COVID-19. In a study aimed at quantifying COVID-19-associated orphanhood, Hillis et al. (25) demonstrated that the likelihood of experiencing parent or grandparent death due to COVID-19 was up to 4.5 times higher for children of color when compared to non-Hispanic white peers.
The current study analyzed annual childhood bereavement rates from the death of a parent from 2016 to 2021 using the CBEM and compared results from the 2 years of the pandemic (2020 and 2021) to the preceding 4 years (2016–2019) for all U.S. children 0 to 17. Further, the analyses explored the differential toll of bereavement on children based on race and Hispanic origin. Results address increases in bereavement, directly and indirectly, connected to COVID-19. Recommendations for prevention and intervention efforts are offered.
Materials and methods
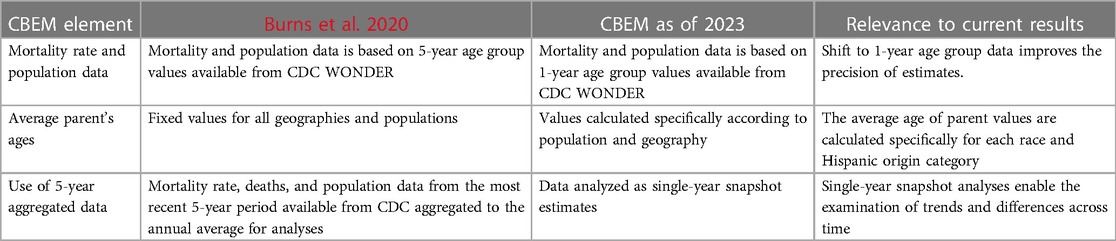
Since the initial CBEM publication (22), the model has been updated and refined to increase accuracy. An online CBEM technical appendix documents changes over time that includes quantitative techniques, information sources, and processing approaches (26). Table 1 details the changes relevant to the current analyses examining bereavement in childhood due to parent death.
In addition to the assumptions outlined by Burns et al. (22), the current analyses assume a child and their parents all identify with the same race and Hispanic origin. More than 85% of the 5.5 million first live births for the years 2016–2020, with details for both the mother's and father's race and Hispanic origin were born to a mother and father of the same race and Hispanic origin categories (27). While this assumption is restrictive, it is generally representative of most children born in the U.S.
CBEM input data
All CBEM input data came from the Center for Disease Control and Prevention's Wide-ranging Online Data for Epidemiologic Research (CDC WONDER databases; 28). Data were extracted for each year from 2016 to 2021.
All input variable data were extracted by race and Hispanic origin. Race categories for data from 2016 to 2020 included All Persons (All), American Indian or Alaska Native (AIAN), Asian or Pacific Islander (API), Black or African American (Black), and white. Hispanic origin categories included Hispanic or Latino (Hispanic) and not Hispanic or Latino (non-Hispanic). Given changes in the 2020 U.S. Census, race categories for 2021 also included More than One Race. Data were extracted by population subgroups defined by the interaction of the race and Hispanic origin categories.
Data on the size of the U.S. resident population and the number of U.S. resident deaths by single year of age for those aged 0 through 70 were extracted from CDC WONDER's Underlying Cause of Death database (29, 30). The upper limit was chosen as individuals over 70 are less likely to have children 0–17. CDC WONDER's basic natality database (31) and expanded natality database (27) were used to retrieve data on a mother's average age at first live birth.
Calculated CBEM input variables
CDC WONDER's expanded natality database (27) was used to calculate parents' age at first birth.
Father's age at first birth. The mother's average age at first live birth and the total number of births for each race and Hispanic origin category were retrieved within specified father's age group categories. Supplementary Table S1 illustrates the steps used to calculate Father's age at first live birth when data indicated the father and mother have the same race and Hispanic origin.
Supplementary Table S2 provides an example of these calculations showing how the difference in the average age of Black, non-Hispanic fathers and mothers was calculated using 2016 data. Supplementary Table S3 summarizes the mother's and father's age at first birth values incorporated in the “snapshot” analyses. The father's age at first birth variable is the only CBEM input that required calculation outside the model.
Mother's age (maFB). The average age of mothers given a child's age was calculated by adding the mother's age at first live birth to the child's age.
Father's age (daFB). The average age of fathers given the child's age is calculated by adding the calculated father's age at first live birth to the child's age.
Probability of death (ProbDeathCalc). The average annual per person probability of death is calculated by dividing the total number of deaths by the population for a given subgrouping. Supplementary Table S4 compares the crude mortality rates for adults ages 23 to 57 in each subgrouping from 2016 to 2021.
CBEM snapshot analyses
The 1-year snapshot estimates of children newly bereaved by the death of a parent are a direct reflection of the probability of a parent dying in a year. The estimated number of children of a given age newly bereaved by a parent death (Bcareca) is the product of the number of children of a given age in a year (Nca) and the probability of either parent dying in a given year [PDcare(p1p2)].
Assuming parents' deaths can be treated as statistically independent events, the probability of at least one of a child's parents dying [PDcare(p1p2)] is the sum of the independent probability of each parent's death (Pcare1pa and Pcare2pa) given a child's age, minus the product of these probabilities. In this equation, the parent's probability of death is determined by their age with one parent based on derived mother's and father's age.
Results
Figure 1 reflects the disproportionate impact of pandemic bereavement on children of color by displaying the single-year snapshot results for the percentage of the total population of children under 18 in each population category who were newly bereaved in the years 2016–2021. All categories saw increased bereavement in the first and second years of the pandemic. The 2020 U.S. Census allowed respondents to choose more than one race category. Thus, childhood bereavement results for this population are only reported in 2021. In line with previous CBEM results, non-Hispanic American Indian Alaska Native, and non-Hispanic Black youth have the highest bereavement rates across years with 10.0% and 6.4% of the total population of youth in these categories, respectively. Likewise, these two groups experienced the steepest increases in the first 2 years of the pandemic.
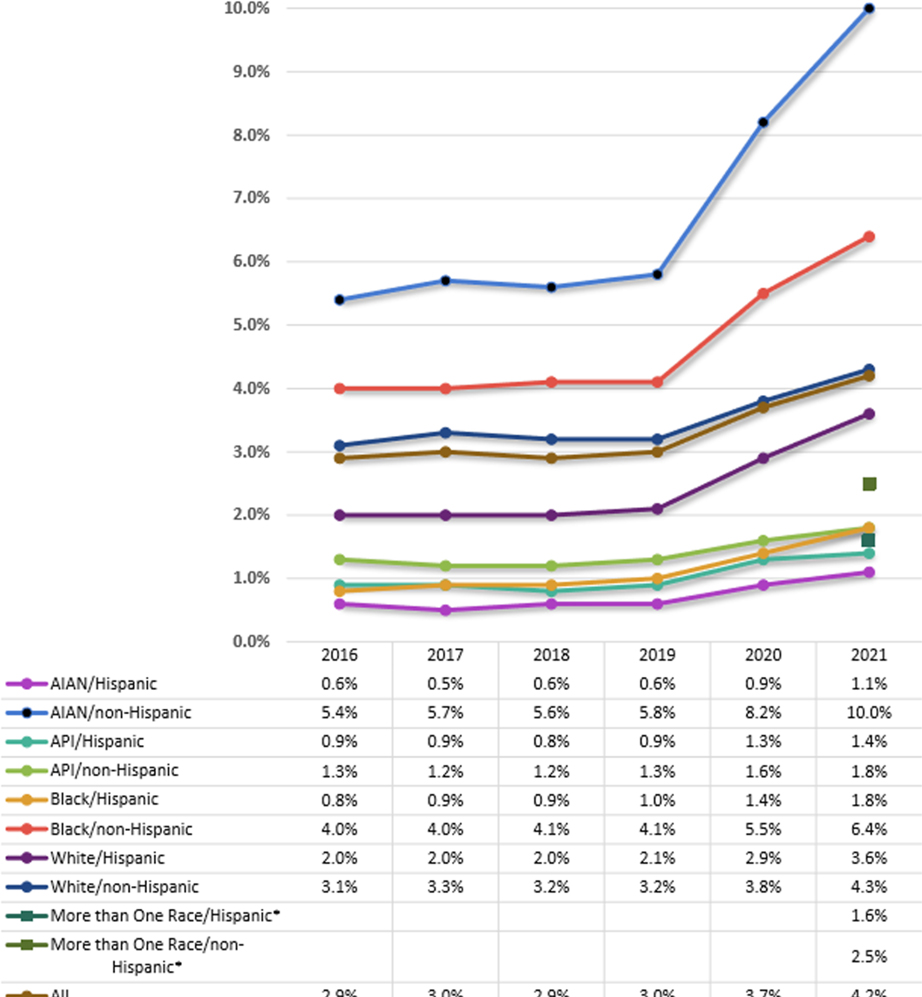
Figure 1. Percent of population under 18 newly bereaved due to parent death. *The more than one race category needs to be included for 2021 to provide a complete summary of the race by hispanic origin population subgroups addressed in the CDC WONDER mortality database.
Table 2 presents the 1-year snapshot results for newly bereaved children by population group for 2020 with more than 65,000 additional children newly bereaved compared to the annual average from 2016 to 2019, a 24.9% increase. The probability of observing 2020 counts assuming the 2016–2019 distribution is small (<5%) for all race and Hispanic origin groups. Although non-Hispanic white children saw the largest increase in newly bereaved children in 2020 (22,973), the findings are more nuanced. Non-Hispanic white youth experienced the smallest percentage increase in bereavement in 2020 (14.9%) relative to the 2016–2019 annual average. In contrast, Hispanic Asian Pacific Islander (72.0%) and Hispanic Black (72.4%) youth experienced the largest percentage increases. Table 2 also shows that these percentage increases are larger for Hispanic youth across all race groups. Given changes in the 2020 U.S. Census categorization of race, 2021 CBEM results were not analyzed compared to 2016–2020 data. Table 3 has the complete results for the number of newly bereaved children by race and Hispanic origin group for each year from 2016 to 2021.
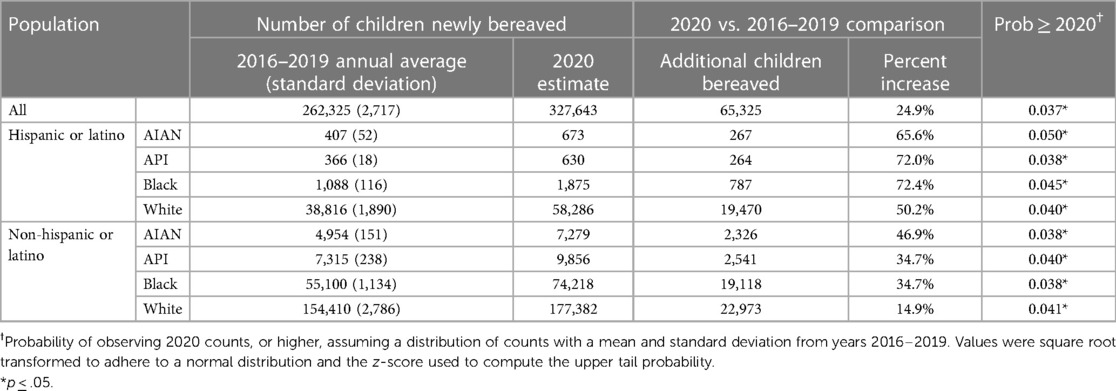
Table 2. Comparisons of CBEM parent death 2020 results with 2016–2019 average by population subgroup.

Table 3. CBEM parent death 1-year snapshot results 2016–2021 by child’s age and population subgroup.
Discussion
In a new application of the CBEM, results quantify one aspect of the COVID-19 pandemic's devastating impact on the U.S. Comparisons of CBEM results from 2020 to 2021 to results from the previous 4 years (2016–2019) clearly highlight the toll of the pandemic on childhood bereavement while also stressing the significance of the issue in the preceding years. Results demonstrate how the pandemic's initial bereavement impacts compounded existing rates of annual bereavement that averaged more than 260,000 children under age 18 being newly bereaved from the death of a parent each year. This number increased by nearly 50%, jumping to more than 383,000 by the end of 2021. The increased childhood bereavement rates were not only attributed to climbing mortality directly connected to COVID-19, but also to indirect impacts of pandemic stress and strain that resulted in rising mortality due to a range of causes such as overdose and homicide death rates. Indeed in 2020, one in five children bereaved by the death of a parent experienced an overdose loss (32). These stigmatized losses may result in increased isolation, guilt, and uncertainty for grieving families.
The nuances revealed by the current analyses show disproportionate increases in bereavement in communities of color. For example, in the first year of the pandemic, compared to the previous 4-year average, rates of childhood bereavement increased by 50% percent or more for all children identified as Hispanic or Latino, regardless of their race, yet the largest jumps were among Hispanic or Latino youth who also identified as Indigenous, Black, and Asian. As the pandemic stretched into 2021, rates of childhood bereavement continued to soar, particularly among Indigenous and Black youth. These analyses show a grim reality where roughly one in ten non-Hispanic Indigenous children under 18 experienced the death of a parent in 2021. Although the current results do not provide data on the cause of these startling differences, the cultural climate of systemic racism and historic oppression are possible contributors. For example, from the start of the pandemic, xenophobic suppositions regarding the origins of COVID-19 fueled anti-Asian sentiment nationwide that contributed to rising rates of depression and anxiety in this community (33). Systemic injustice and lack of access to quality health care contribute to stark inequities that likely resulted in disproportionate death rates for preventable death causes such as heart disease, liver disease, and homicide in communities of color (23).
The current study has important data and methodological differences from other studies of COVID-attributable bereavement or orphanhood in the U.S. (24, 25, 34). First, this study incorporates final, validated CDC WONDER data instead of preliminary estimates. Second, the CBEM results presented here are specific to children grieving the death of a parent. In contrast, prior studies investigated family characteristics or used dynamic family/community models considering bereavement for children raised by non-parent caregivers. Third, the current study's exploration of population subgroups considering race and Hispanic origin provides novel results emphasizing the context of the pandemic's impact on childhood bereavement and aiding resource allocation to provide support. The race and Hispanic origin results demonstrate how the pandemic exacerbated longstanding discrepancies in the magnitude of childhood bereavement for non-white youth.
Limitations
Although the current study considers all race and Hispanic origin combinations possible with publicly available data, options for population subgroups were constrained by the databases' content. Further, the analyses assume the child and their parents share the same race and Hispanic origin—an assumption that holds for 85% of the population. Although the availability of additional race and ethnicity options within WONDER's databases allows for CBEM expansion, changes in these subgroupings currently limit the potential scope for year-over-year comparisons. Despite using gender-based information to identify relevant annual probabilities of death for each parent, the analyses do not assume specific genders for the child's parents (i.e., the probabilities of death are not gender specific). Finally, CBEM results reflect an undercount of the childhood bereavement phenomenon as it does not include youth bereaved following the death of a parent-figure other than a mother and father. For example, the current results do not include youth bereaved by the death of a custodial grandparent, a situation more common for Black and Indigenous families (35).
Conclusion
There is a history of research documenting the potential for short- and long-term adverse effects from unaddressed childhood grief (36). The overwhelming increase in mortality created in the wake of the COVID-19 pandemic brought unprecedented attention to the longstanding issue. Without a national database tracking childhood bereavement in the U.S., the CBEM provides a sound approach to estimating prevalence. Disparities in mortality rates across race and Hispanic origin groups in the U.S. result in disproportionate youth bereavement prevalence (37). Before the pandemic, CBEM results illustrated the overrepresentation of children of color among the bereaved in the U.S. The current analyses reflect how the pandemic deepened these gaps and magnified the importance of and the need for timely and effective programming to support bereaved children and families nationwide, whether they are grieving a death due to COVID-19 or any other cause.
The pandemic acutely raised awareness and recognition of bereavement as a critical public health issue, but there is more work to be done in bringing forth culturally relevant, wide-scale, societal understanding and sensitivity. For the estimated 700,000 plus children under the age of 18 who experienced the death of a parent in 2020 and 2021, securing appropriate support may prove challenging. Although local, regional, and national organizations focused on supporting the bereaved youths exists, there are significant gaps across the country, and resources to support these efforts are scarce. Programs like the Childhood Bereavement Changemaker initiative (38) acknowledge the field's grassroots origins while bolstering the capacity to make data-informed decisions and enhance impact, but aid for this type of programming is limited. Given the longstanding nature of the issue alongside the recent increases brought on by COVID-19, the following recommendations are offered:
• Broaden public awareness and advocacy efforts that promote grief education and ensure those coping with a death loss are met with sensitivity and responsiveness.
• Assess the size and scope of the issue by creating a national system for quantifying childhood bereavement with mechanisms for annual reporting and benchmarking.
• Develop ongoing processes for screening grief reactions and offering requisite support across systems and institutions (e.g., healthcare, schools).
• Promote research that contributes to understanding the diverse needs of grieving children and translates into practical strategies and efficacious solutions in community settings where bereaved children and families live.
• Strengthen workforce and community capacity to address bereavement by developing and providing appropriate training, tools, and resources. Embed grief-informed knowledge throughout societal systems including education, health care, criminal justice, finance, and government.
• Provide and sustain an affordable continuum of comprehensive prevention and intervention services that address the broad spectrum of bereaved youth. Services should be universally accessible and culturally relevant with a focus on reducing risk and promoting well-being regardless of the acuity of grief reactions.
For the millions of U.S. children and adults bereaved in childhood, the time has come for a comprehensive approach to the development and implementation of resources, support, and services. Researchers, practitioners, educators, policymakers, and advocates must unite to invest in prevention and create social change that ensures a compassionate response to all grieving children and families nationwide.
Data availability statement
Publicly available datasets were analyzed in this study. This data can be found here: Centers for Disease Control and Prevention. Wide-ranging Online Data for Epidemiologic Research. [Internet]. Washington DC, CDC [Updated 2023 January; Cited 2023 January 30] DC 2023. CDC WONDER. Available at: https://wonder.cdc.gov/.
Author contributions
MB and LL contributed to the conception and design of the original model and the study. NC offered consultation on the statistical integrity of the model and made suggestions for improvements and refinements. DM organized the data and performed the analyses. MB wrote the first draft of the manuscript. DM, LL, and NC contributed content for the initial draft. All authors contributed to the article and approved the submitted version.
Funding
The New York Life Foundation funded the CBEM's development and continued application in support of the community working to support grieving children and better understand the scope and impact of this issue. Additional support for the CBEM comes from generous donations to Judi's House from Individuals, Corporations, and Foundations. The Center for Innovative Design and Analysis at the University of Colorado School of Public Health contributes significantly to the ongoing enhancements to the CBEM.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fped.2023.1063449/full#supplementary-material.
References
1. Shiels MS, Haque AT, de Gonzalez AB, Freedman ND. Leading cause of death in the U.S. during the COVID-19 pandemic march 2020 to October 2021. JAMA Intern Med. (2022) 182(8):883–6. doi: 10.1001/jamainternmed.2022.2476
2. Cronin CJ, Evans WN. Excess mortality from COVID and non-COVID causes in minority populations. Proc Natl Acad Sci U S A. (2021) 118(39):e2101386118. doi: 10.1073/pnas.2101386118
3. Cai C, Woolhandelr S, Himmelstein DU, Gaffney A. Trends in anxiety and depression symptoms during the COVID-19 pandemic: results from the U.S. Census Bureau's Household Pulse survey. J Gen Intern Med. (2021) 36(6):1841–3. doi: 10.1007/s11606-021-06759-9
4. Verdery AM, Smith-Greenaway E, Margolis R, Daw J. Tracking the reach of COVID-19 kin loss with a bereavement multiplier applied to the United States. Proc Natl Acad Sci U S A. (2020) 117(30):17695–701. doi: 10.1073/pnas.2007476117
5. Centers for Disease Control and Prevention, National Center for Health Statistics (NCHS). COVID-19 mortality overview. Washington DC, CDC. Available at: https://www.cdc.gov/nchs/covid19/mortality-overview.htm (Accessed August 26, 2022).
6. Hedegaard H, Miniño AM, Spencer MR, Warner M. Drug overdose deaths in the United States, 1999–2020. National center for health statistics data brief. No. 428 Hyattsville, MD. (Accessed January 28, 2023).
7. Spencer MR, Miniño AM, Warner M. Overdose deaths in the United States, 2001-2021. National center for health statistics data brief. No. 457 Hyattsville, MD. (Accessed January 28, 2023).
8. Lee WE, Park SW, Weinberger DM, Olson D, Simonsen L, Grenfell BT, et al. Direct and indirect mortality impacts of the COVID-19 pandemic in the US, March 2020-April 2021. medRxiv. (2022) 12:e77562. doi: 10.1101/2022.02.10.22270721.
9. Cerel J, Fristad MA, Verducci J, Weller RA, Weller EB. Childhood bereavement psychopathology in the 2 years postparental death. J Am Acad Child Adolesc Psychiatry. (2006) 45:681–90. doi: 10.1097/01.chi.0000215327.58799.05
10. Kaplow JB, Saunders J, Angold A, Costello EJ. Psychiatric symptoms in bereaved versus nonbereaved youth and young adults: a longitudinal epidemiological study. J Am Acad Child Adolesc Psychiatry. (2010) 49:1145–54. doi: 10.1176/appi.ajp.2014.13081132
11. Keyes KM, Pratt C, Galea S, McLaughlin KA, Koenen KC, Shear MK. The burden of loss: unexpected death of a loved one and psychiatric disorders across the life course in a national study. Am J Psychiatry. (2014) 171:864–71. doi: 10.1176/appi.ajp.2014.13081132
12. Hill RM, Kaplow JB, Oosterhoff B, Layne C. Understanding grief reactions, thwarted belongingness, and suicide ideation in bereaved adolescents: toward a unifying theory. J Clin Psychol. (2019) 75:780–93. doi: 10.1002/jclp.22731
13. Oosterhoff B, Kalpow JB, Layne CM. Links between bereavement due to sudden death and academic functioning: results from a nationally representative sample of adolescents. Sch Psychol Q. (2018) 33(3):372–80. doi: 10.1037/spq0000254
14. Brent DA, Melhem NM, Masten AS, Porta G, Walker Payne M. Longitudinal effects of parental bereavement on adolescent development. J Clin Child Adolesc Psychol. (2013) 41(6):776–91. doi: 10.1080/15374416.2012.717871
15. Guldin M, Li J, Pedersen HS, Obel C, Agerbo E, Gissler M, et al. Incidence of suicide among persons who had a parent who died during their childhood: a population-based cohort study. JAMA Psychiatry. (2015) 72(12):1227–34. doi: 10.1001/jamapsychiatry.2015.2094
16. Li J, Vestergaard M, Cnattingius S, Gissler M, Bech BH, Obel C, et al. Mortality after parent death in childhood: a nationwide cohort study from three nordic countries. PLoS Med. (2014) 11(7):e1001679. doi: 10.1371/journal.pmed.1001679
17. American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th ed. Washington, DC: American Psychiatric Association Publishing (2022).
18. Melhem NM, Porta G, Shamseddeen W, Payne MW, Brent DA. Grief in children and adolescents bereaved by sudden parental death. Arch Gen Psychiatry. (2011) 68(9):911–9. doi: 10.1001/archgenpsychiatry.2011.101
19. Kaplow JB, Layne CM, Oosterhoff B, Goldenthal H, Howell KH, Wamser-Nanney R, et al. Validation of the persistent complex bereavement disorder (PCBD) checklist: a developmentally informed assessment tool for bereaved youth. J Trauma Stress. (2018) 31(2):244–54. doi: 10.1002/jts.22277
20. Bergman AS, Axberg U, Hanson E. When a parent dies-a systemic review of the effects of support programs for parentally bereaved children and their caregivers. BMC Palliat Care. (2017) 16(1):39. doi: 10.1186/s12904-017-0223-y
21. Griese B, Burns M, Farro SA. Pathfinders: promoting healthy adjustment in bereaved children and families. Death Stud. (2017) 42(3):134–42. doi: 10.1080/07481187.2017.1370416
22. Burns M, Griese B, King S, Talmi A. Childhood bereavement: understanding prevalence and related adversity in the United States. Am J Orthopsychiatry. (2020) 90(4):391–405. doi: 10.1037/ort0000442
23. Judi’s House. CBEM childhood bereavement race and ethnicity national report. Denver, CO, USA. Judi’s House. Available at: https://judishouse.org/research-tools/cbem/cbem-race-ethnicity/cbem-race-ethnicity-reports/ (Accessed August 26, 2022).
24. Kidman R, Margolis R, Smith-Greenway E. Estimates and projections of COVID-19 and parental death in the U.S. JAMA Pediatr. (2021) 175(7):745–6. doi: 10.1001/jamapediatrics.2021.0161
25. Hillis SD, Blenkinsop A, Villaveces A, Annor FB, Liburd L, Massetti GM, et al. COVID-19 associated orphanhood and caregiver death in the United States. Pediatrics. (2021) 148(6):e2021053760. doi: 10.1542/peds.2021-053760
26. Judi’s House. CBEM technical appendix. Denver, CO USA. Judi’s House. Available at: https://judishouse.org/wp-content/uploads/2021/11/CBEM-Technical-Appendix_Nov-2021.pdf (Accessed August 26, 2022).
27. Centers for Disease Control and Prevention, National Center for Health Statistics. National vital statistics system, natality records 2016-2021 (expanded) on CDC WONDER Online Database, released in 2022. Washington DC, CDC. Available at http://wonder.cdc.gov/natality-expanded-current.html (Accessed January 30, 2023).
28. Centers for Disease Control and Prevention. Wide-ranging online data for epidemiologic research. Washington DC, CDC DC 2023. CDC WONDER. Available at: https://wonder.cdc.gov/ (Accessed January 30, 2023).
29. Centers for Disease Control and Prevention, National Center for Health Statistics. Underlying cause of death 1999-2020 on CDC WONDER online database, released in 2021. Washington DC, CDC. Available at: http://wonder.cdc.gov ucd-icd10.html (Accessed January 6, 2022).
30. Centers for Disease Control and Prevention, National Center for Health Statistics. National vital statistics system, mortality 2018-2021 on CDC WONDER online database, released in 2023. Washington DC, CDC. Available at http://wonder.cdc.gov/ucd-icd10.html (Accessed January 30, 2023).
31. Centers for Disease Control and Prevention, National Center for Health Statistics (NCHS), Division of Vital Statistics. Natality public-use data 2007-2021. Washington DC, CDC. Available at: http://wonder.cdc.gov/natality-current.html (Accessed January 30, 2023).
32. Judi’s House. CBEM COVID-19 pandemic impact report. Denver, CO, USA. Judi’s House. Available at: https://judishouse.org/research-tools/cbem/cbem-cod/cbem-pandemic-impact-report/ (Accessed January 29, 2023).
33. National Center for Health Statistics. U.S. Census Bureau, household pulse survey, 2020-2023, anxiety and depression. Washington DC, CDC. Available at: https://www.cdc.gov/nchs/covid19/pulse/mental-health.htm (Accessed January 28, 2023).
34. Treglia D, Cutuli JJ, Arasteh K, Bridgeland J, Edson JM, Phillips G, et al. Hidden pain: children who lost a parent or caregiver to COVID-19 and what the nation can do to help them. COVID collaborative. Available at: https://www.covidcollaborative.us/initiatives/hidden-pain (Accessed August 26, 2022).
35. Generations United. State of grandfamilies report 2021. Reinforcing a strong foundation: equitable supports for basic needs of grandfamilies. Available at: https://www.gu.org/resources/state-of-grandfamilies-report-2021.
36. Pham S, Porta G, Biernesser C, Payne MW, Iyengar S, Melhem N, et al. The burden of bereavement: early-onset depression and impairment in youths bereaved by sudden parental death in a 7-year prospective study. Am J Psychiatry. (2018) 175(9):887–96. doi: 10.1176/appi.ajp.2018.17070792
37. Cunningham TJ, Croft JB, Liu Y, Lu H, Eke PI, Giles WH. Vital signs: racial disparities in age-specific mortality among blacks or African Americans-United States, 1999-2015. Morb Mortal Wkly Rep. (2017) 66(17):444–56. doi: 10.15585/mmwr.mm6617e1
38. Judi's House. Childhood bereavement changemakers. Available at: https://judishouse.org/research-tools/cbc/.
Keywords: race, hispanic origin, COVID-19, grief, pandemic, childhood bereavement estimation model (CBEM), childhood bereavement, parent death
Citation: Burns M, Landry L, Mills D, Carlson N, Blueford JM and Talmi A (2023) COVID-19 pandemic’s disproportionate impact on childhood bereavement for youth of color: Reflections and recommendations. Front. Pediatr. 11:1063449. doi: 10.3389/fped.2023.1063449
Received: 7 October 2022; Accepted: 6 March 2023;
Published: 30 March 2023.
Edited by:
Nakiya Naomi Showell, Johns Hopkins Medicine, Johns Hopkins University, United StatesReviewed by:
Adam Carter, National Alliance for Children’s Grief, United StatesLydia Gimenez-Llort, Autonomous University of Barcelona, Spain
© 2023 Burns, Landry, Mills, Carlson, Blueford and Talmi. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Michaeleen Burns bWlja2liQGp1ZGlzaG91c2Uub3Jn
Specialty Section: This article was submitted to Children and Health, a section of the journal Frontiers in Pediatrics
 Michaeleen Burns
Michaeleen Burns Laura Landry1
Laura Landry1 Nichole Carlson
Nichole Carlson Jillian M. Blueford
Jillian M. Blueford