- Department of Neonatology, Affiliated Shenzhen Maternity & Child Healthcare Hospital, Southern Medical University, Shenzhen, China
Background: Data from the China Neonatal Network currently shows that the survival rate of very preterm infants in China has improved in recent years. However, due to the unequal economic and medical development of each city in China, the national data do not completely represent the level of neonatal care in the metropolitan areas. Though many studies have published their short- or long-term survival, very few have described the care practices and the course of stay of these neonates in detail. Our objective was to examine the survival and clinical practices among preterm infants born at <24 weeks’ gestational age (GA) in a high-income city in China, from 2015 to 2021.
Methods: Retrospective study of preterm infants <24 weeks GA in a level 3 neonatal intensive care unit in China, over a period of 7 years (2015–2021). Care practices in neonatal intensive care units (NICU) and short- and long-term survival were measured.
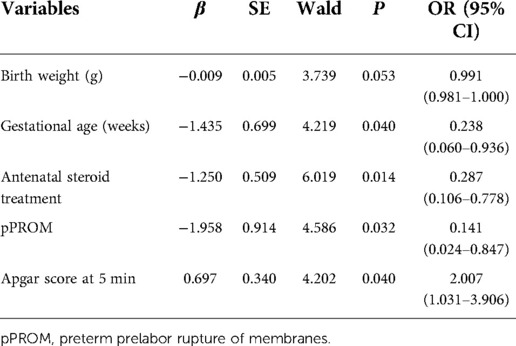
Results: A total of 32 periviable infants were included, with a median GA of 23.0 weeks and mean (SD) birth weight of 497 (94) g; 17 infants (53.1%) were female. While none of the infants born at 21 weeks of gestation survived until discharge, the survival rates were 25.0% (3 of 12) for infants born at 22 weeks and 58.8% (10 of 17) at 23 weeks. Antenatal corticosteroids were used in 56.3%, and 100% were vaginal birth. In the delivery room, surfactant was prescribed for 46.9% of the infants, and postnatal dexamethasone (≥2 courses) was prescribed to 61.5% of the infants. Logistic regression analysis showed that Apgar score at 5 minutes (OR = 2.007, 95% CI, 1.031 to 3.906, P < 0.05) increased the risk of death, while the increase in gestational age (OR = 0.238, 95% CI, 0.060–0.936, P < 0.05), antenatal use of steroids (OR = 0.287, 95% CI, 0.106–0.778, P < 0.01), and premature rupture of membranes (OR = 0.141, 95% CI, 0.024 −0.847, P = 0.032) could decrease the risk. No or mild neurodevelopmental impairment in surviving infants was 76.9% (10 of 13).
Conclusions: Although the survival rate of periviable infants was shown to be improved in our study, there is still much room for improvement, and active follow-up information should be conducted.
Introduction
According to the current definition of premature birth in China, babies who are born below 28 weeks of gestational age (GA) are defined as aborted babies, not infants (1). With advances in perinatal and neonatal care, more and more infants born at earlier GA had survived (2). The differences in perinatal management for infants <24 weeks result in wide variations in outcomes reported by countries. Although many studies have reported their short-or long-term outcomes, few have described in detail the nursing practice and hospitalization process of these infants. This study primarily aimed to evaluate mortality and short-and long-term outcomes among infants born <24 weeks gestation in Shenzhen, China, over the past 7 years. We present our single-center data together with our clinical practices to determine perinatal risk factors related to mortality.
Materials and methods
Study design and population
This retrospective cross-sectional study was carried out at the neonatal intensive care unit (NICU) of the Shenzhen Maternity & Child Healthcare Hospital. This unit has 72 incubators, serves as a level III NICU with approximately 1,500 newborn admissions per year, and is one of the largest perinatology centers in Shenzhen city, China. This is a retrospective observational study evaluating neonates of gestational ages <24 weeks born at the Shenzhen Maternity & Child Healthcare Hospital over a 7-year period from 1 January 2015–31 December 2021.Neonates who died in the delivery room were excluded from the analysis. The gestational age was determined by the best obstetric estimate based on the first obstetric ultrasound and the first day of the last normal menstrual period. Morbidity and mortality rates were retrieved from the hospital discharge records.
Ethics
The Shenzhen Maternity and Child Healthcare Hospital Institutional Ethical Committee approved the collection and usage of the clinical information for research purposes and waived the requirement for informed consent [SFYLS No. (2019)-119].
Data collection
All data related to the neonatal period, including sociodemographic characteristics and obstetric characteristics (such as maternal age, number of multiple births, mode of conception, and use of antenatal corticosteroids) were retrieved from the medical records of the NICU. The characteristics of neonates, i.e., sex, birth weight (BW), GA, surfactant treatment, ventilation mode, patent ductus arteriosus (PDA) and early onset neonatal sepsis, intraventricular hemorrhage (IVH), necrotizing enterocolitis (NEC), bronchopulmonary dysplasia (BPD), and retinopathy of prematurity (ROP) were recorded. All infants were examined by cranial magnetic resonance imaging (MRI) at post menstrual age (PMA) 37–40 weeks. All infants survived to discharge were followed up after discharge.
Definitions
Antenatal steroid treatment was considered if at least one dose of dexamethasone was given 12 h before delivery. Survivors were defined as neonates who survived to the time of discharge. BPD was defined as oxygen dependency at 36 weeks of corrected age (3). ROP and the graded standard were defined by the international classification of ROP (4). IVH were diagnosed by cranial ultrasonography or MRI. The Papile grading system was used to grade IVH (5). Sepsis was defined by clinical symptoms and positive culture from blood or cerebrospinal fluid samples (6). PDA required medical or surgical treatment.
Statistics
Continuous variables of normal distribution were expressed as the mean (±) standard deviation, and T-test was used for comparison between groups; categorical variables are expressed as number of cases and percentages. In analyses of abnormally distributed data, median (interquartile range, IQR) was used, and the Mann–Whitney U-test was applied for comparisons between two groups. Pearson's χ2 test or Fisher's exact test was applied in analyses of categorical variables. After adjustment for some possible confounding factors, the risk factors for mortality of periviable infants were evaluated using multiple logistic regression. In all analyses, P < 0.05 was taken to indicate statistical significance. The analysis was performed using SPSS statistical software version 26.0 (IBM, Corporation, NY, United States).
Results
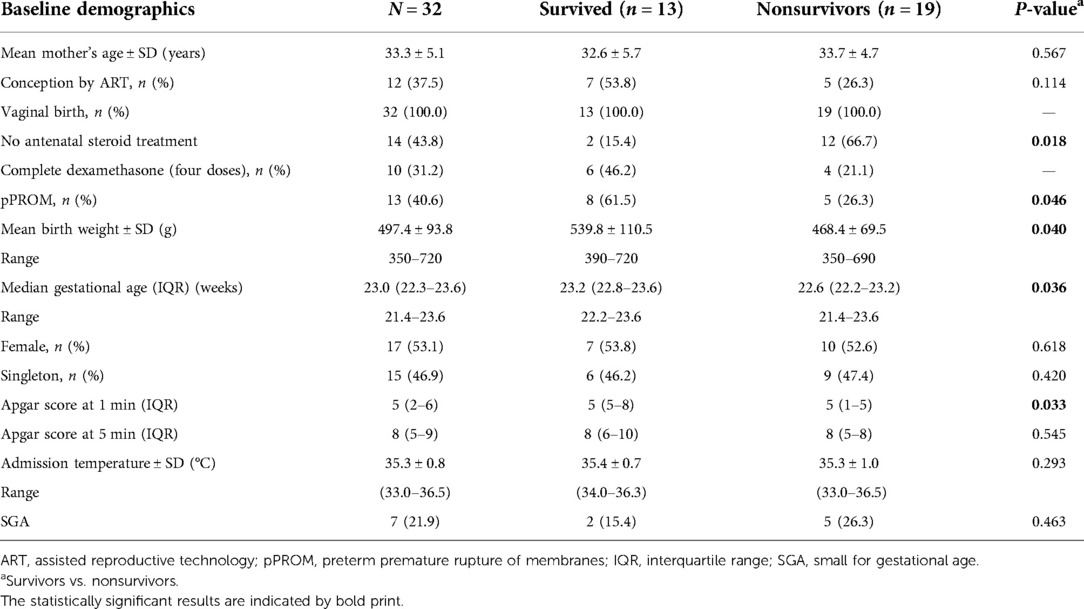
A total of 32 neonates born at 21+0–23+6 gestational age and admitted to NICU for active care were included in the study [21 weeks (n = 3), 22 weeks (n = 12), 23 weeks (n = 17)]. All infants were born by vaginal and 18 (56.3%) of the infants were exposed to antenatal corticosteroids. There was a statistically significant difference in the antenatal steroid treatment, preterm premature rupture of membrane (pPROM) rates, and Apgar score at 1 min between survivors and nonsurvivors (P < 0.05). The baseline characteristics of the enrolled neonates are summarized in Table 1.
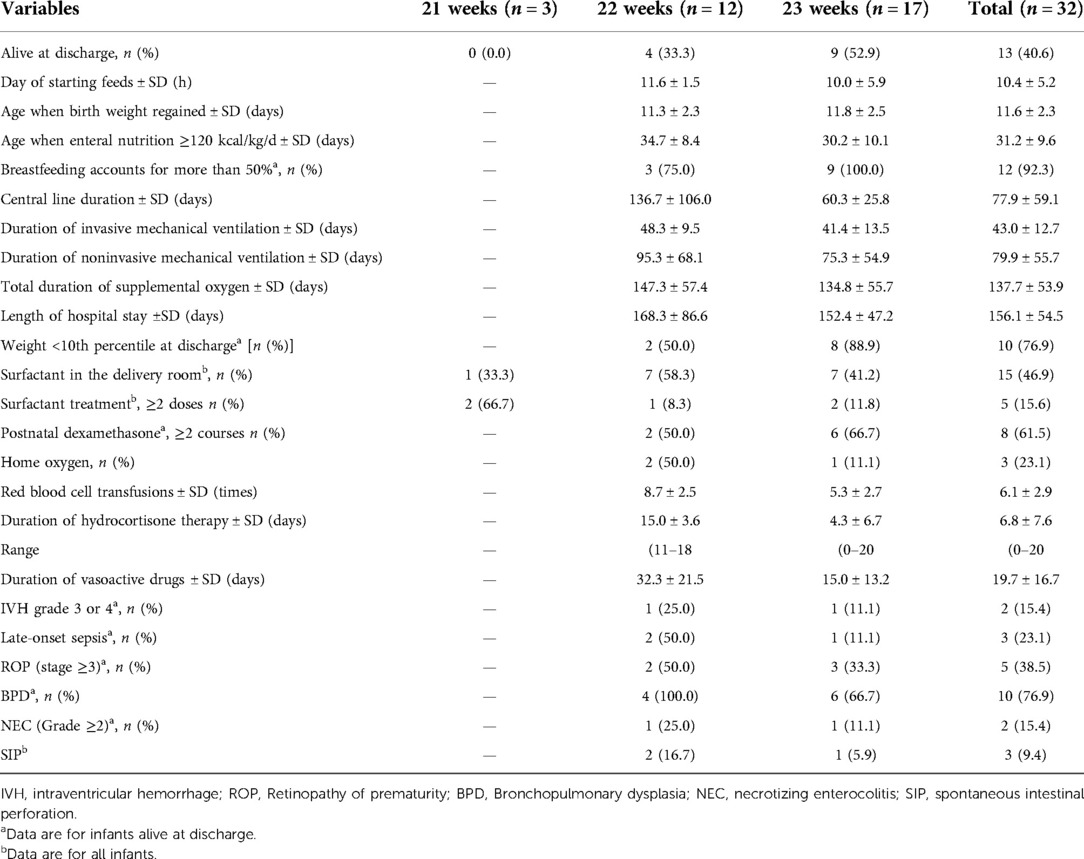
While none of the infants born at 21 weeks of gestation survived until discharge, the survival rates were 25.0% for infants born at 22 weeks and 58.8% for those born at 23 weeks. A total of 13 infants survived (40.6%), and 13 of 21 (61.9%) who received active care survived. Eight of these 32 infants died on the first day, 6 died between days 1 and 7, 2 died between days 7 and 27, and 3 died between days 28 and 65. Of the infants, 15 (46.9%) used a surfactant in the delivery room. Of the survivors, two (15.4%) were classified as having severe IVH (grade 3 or 4), five (38.4%) had ROP (stage ≥3), and 10 (76.9%) had BPD. The percentages of infants who had NEC (Grade ≥2) at 22 and 23 weeks of gestation were 25.0% and 11.1%, respectively. Three infants used oxygen after discharge in total. Care practices and morbidities for the infants according to gestational age are shown in Table 2.
Adjusting for other factors, the likelihood of dying in the NICU decreased significantly with increasing antenatal steroid treatment (OR 0.287, 95% CI, 0.106–0.778, P < 0.05). On the other hand, survival was predicted by the Apgar score after 5 min (OR 2.007, 95% CI, 1.031–3.906, P = 0.040) and preterm prelabor rupture of membranes (OR 0.141, 95% CI, 0.024–0.847, P = 0.032) (Table 3).
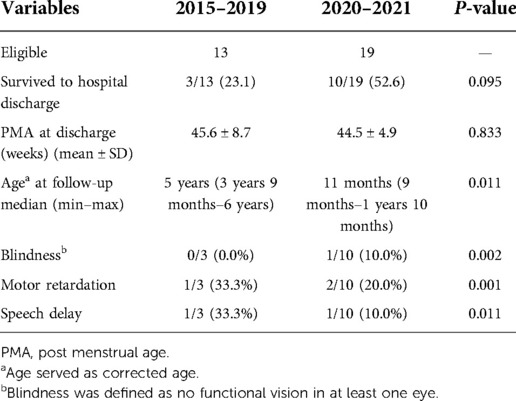
The survival rate was higher during 2020–2021 (52.6%) than during 2015–2019 (23.1%). Follow-up data with assessments at October 20, 2022, were collected for 13 infants. The proportions of motor retardation and speech delay in the evaluated infants were lower during 2020–2021 than during 2015–2019, whereas the proportion of blindness increased since one infant suffered from retinal hemorrhage (Table 4).
Discussion
In our single-center retrospective study, the survival rates of the periviable births <24 weeks was 40.6%, and considering active treatment was 61.9%. They are similar to that reported in Japan (NRNJ, 2013) (7); however, they were lower than the ones reported from the United States (single center, Iowa, 2020), Germany (single center, Cologne, 2016), and higher than that from France (EPIPAGE, 2015) and the United Kingdom (single center, Headington, 2021) (8–11).
Such variations may be associated with differences in willingness to provide active obstetrical and neonatal care for infants at the lowest GA. Infants that were born during the 22nd week of gestation had received resuscitation and active treatment after birth, so it is in the United States (12, 13). In China, parents were more worried about the poor outcomes of the infants and the economic burden, leading to withdrawal from treatment (14). Although our unit does selectively resuscitate according to the parents’ decision, our center's reputation of active treatment had attracted more parents who desired resuscitation and that broadened our experience in caring of these infants.
Differing clinical practices also contribute to the variability in survival rates.
Isayama (12) reported the unique aspects of management in Japan, which were different from ours. For example, most Japanese neonatologists performed functional echocardiography, applying ubiquitous sedation on all ventilated infants, monitoring the intracerebral venous velocity model in the acute phase to prevent IVH, and continuously measuring C-reactive protein (CRP) in the acute phase of infection. Watkins et al. (8) also reported other practices different from our center, such as taking high frequency oscillatory ventilation (HFOV) as the primary mode of respiratory support; few infants underwent tracheotomy. A series of measures had been taken to improve the prognosis of these infants for the past 2 years in our NICU, including delayed cord clamping, surfactant administration in the delivery room, incomplete “Golden Hour” practices in the first hour of postnatal life, and low-dose hydrocortisone supplementation within 9 days after birth, which had increased the survival rate in the past 2 years in the study. The Golden Hour protocol could significantly improve the stabilization of in extremely premature infants (15). Important elements of the “Golden Hour” in our NICU include insertion of umbilical catheters, blood sampling, surfactant administration, and the initiation of a glucose and amino acid infusion within 1 h of birth.
The lower rate of NEC in our center than others reported (8, 13) could be attributed to the nutrition management of periviable infants, that is characterized by (I) early minimal enteral feeding, (II) the promotion of breastfeeding, (III) probiotics administration, and (IV) routine glycerin enema after 7–10 days, which is appropriately similar to what Kanai et al. reported (16, 17). Mothers’ breastfeeding is actively practiced in our NICU, usually within 24–48 h after birth. Breastfed infants have significant benefits compared to formula fed infants, including reduced late infection, NEC, and improved neurodevelopmental outcomes (18). The reason for the lower rate of severe intraventricular hemorrhage in our study than the mean level in China was not clear (19). It might be due to the fact that neonatologists and NICU nurses try to minimize the handling of infants who are in the acute phase by keeping the head in the middle position, placing arterial lines for blood sampling, avoiding unnecessary oral or airway suctioning and physical examination, and unweighed within 1 week after birth in our NICU.
To our knowledge, hypothermia is a common problem, especially if delivered with less than 28 weeks gestation, which was associated with the increase of neonatal mortality and morbidities (20). The mean admission temperature of 32 periviable infants in this study was 35.3 ± 0.8°C, and the lowest was 33°C, owing to the parents withdrawing care in the delivery room due to economic burden. Our hospital is a level III maternity and child healthcare hospital. The delivery room is relatively well equipped with heat preservation equipment. Pediatricians receive each newborn in the delivery room, preheat all items in contact with the newborn in advance, and immediately place them on the incubator with the use of radiant warmers and plastic wraps to keep warm after birth, and send them to the NICU in an incubator immediately.
The main strength of our study is that it had reported in detail the various clinical practices related to the neonates born <24 weeks and discussed the differences between our practices and those reported, which has rarely been addressed before. In addition, it had tried to explore the various risk factors for mortality, and more importantly, it shows the short- and long-term outcomes of these neonates. However, this study has its limitations. It was a retrospective study and had not reported on the stillbirth rates and delivery room deaths. A relatively small sample size might result in imprecise estimates.
Conclusions
Survival rate and clinical practices in this study differed from other centers. The data presented here provide evidence that a series of clinical improvement measures in the early postnatal life might have helped improve the survival rate of periviable infants. Although the survival rate of periviable infants was shown to be improved in this study, there is still much room for improvement.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by Shenzhen Maternity and Child Healthcare Hospital Institutional Ethical Committee [SFYLS No. (2019)-119]. Written informed consent from the participants’ legal guardian/next of kin was not required to participate in this study in accordance with the national legislation and the institutional requirements. Written informed consent was not obtained from the minor(s)' legal guardian/next of kin for the publication of any potentially identifiable images or data included in this article.
Author contributions
CC and MW collected and analyzed data. JZ and ZH formulated the statistical tests. XX participated in writing the manuscript. CC wrote the paper. ZH and CY critically revised the manuscript. All authors contributed to the article and approved the submitted version.
Funding
This study was supported by the Shenzhen Fund for Guangdong Provincial High level Clinical Key Specialties (SZGSP009).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. General Office of the National Health and Family Planning Commission. Norms of health care for premature babies. Zhonghua Wei Chan Yi Xue Za Zhi. (2017) 20(6):401–6 (Article in Chinese). doi: 10.3760/cma.j.issn.1007-9408.2017.06.001
2. Wu F, Liu G, Feng Z, Tan X, Yang C, Ye X, et al. Short-term outcomes of extremely preterm infants at discharge: a multicenter study from Guangdong province during 2008–2017. BMC Pediatr. (2019) 19(1):405. doi: 10.1186/s12887-019-1736-8
3. Jobe AH, Bancalari E. Bronchopulmonary dysplasia. Am J Respir Crit Care Med. (2001) 163(7):1723–9. doi: 10.1164/ajrccm.163.7.2011060
4. International Committee for the Classification of Retinopathy of Prematurity. The international classification of retinopathy of prematurity revisited. Arch Ophthalmol. (2005) 123(7):991–9. doi: 10.1001/archopht.123.7.991
5. Papile LA, Munsick-Bruno G, Schaefer A. Relationship of cerebral intraventricular hemorrhage and early childhood neurologic handicaps. J Pediatr. (1983) 103(2):273–7. doi: 10.1016/s0022-3476(83)80366-7
6. Jiang S, Yang C, Yang C, Yan W, Shah V, Shah PS, et al.Epidemiology and microbiology of late-onset sepsis among preterm infants in China, 2015–2018: a cohort study. Int J Infect Dis. (2020) 96:1–9. doi: 10.1016/j.ijid.2020.03.034
7. Ishii N, Kono Y, Yonemoto N, Kusuda S, Fujimura M. Neonatal Research Network, Japan. Outcomes of infants born at 22 and 23 weeks’ gestation. Pediatrics. (2013) 132(1):62–71. doi: 10.1542/peds.2012-2857
8. Watkins PL, Dagle JM, Bell EF, Colaizy TT. Outcomes at 18 to 22 months of corrected age for infants born at 22 to 25 weeks of gestation in a center practicing active management. J Pediatr. (2020) 217:52–8. doi: 10.1016/j.jpeds.2019.08.028
9. Mehler K, Oberthuer A, Keller T, Becker I, Valter M, Roth B, et al. Survival among infants born at 22- or 23-weeks’ gestation following active prenatal and postnatal care. JAMA Pediatr. (2016) 170(7):671–7. doi: 10.1001/jamapediatrics.2016.0207
10. Ancel PY, Goffinet F, EPIPAGE-2 Writing Group, Kuhn P, Langer B, Matis J, et al. Survival and morbidity of preterm children born at 22 through 34 weeks’ gestation in France in 2011: results of the EPIPAGE-2 cohort study [published correction appears in JAMA Pediatr. 2015;169(4):323. Alberge, Catherine [Corrected to Alberge, Corine]]. JAMA Pediatr. (2015) 169(3):230–8. doi: 10.1001/jamapediatrics.2014.3351
11. Ramaswamy VV, Oommen VI, Gupta A, Weerapperuma N, Zivanovic S, Roehr CC. Care practices and outcomes of extremely preterm neonates born at 22-24 weeks-A single centre experience. J Neonatal Perinatal Med. (2021) 14(4):575–82. doi: 10.3233/NPM-200670
12. Isayama T. The clinical management and outcomes of extremely preterm infants in Japan: past, present, and future. Transl Pediatr. (2019) 8(3):199–211. doi: 10.21037/tp.2019.07.10
13. Chen Y-J, Yu W-H, Chen L-W, Huang C-C, Kang L, Lin H-S, et al. Improved survival of periviable infants after alteration of the threshold of viability by the neonatal resuscitation program 2015. Children. (2021) 8:23. doi: 10.3390/children8010023
14. Collaborative Study Group for Extremely Preterm and Extremely Low Birth Weight Infants. Short-term outcomes and their related risk factors of extremely preterm and extremely low birth weight infants in Guangdong province. Chin J Pediatr. (2019) 57(12):934–42. doi: 10.3760/cma.j.issn.0578?1310.2019.12.008
15. Croop SEW, Thoyre SM, Aliaga S, McCaffrey MJ, Wohl SP. The Golden Hour: a quality improvement initiative for extremely premature infants in the neonatal intensive care unit. J Perinatol. (2020) 40(3):530–9. doi: 10.1038/s41372-019-0545-0
16. Kulali F, Yagmur BA, Erol S, Yucel H, Guzel FI, Yalvac S, et al. Survival of periviable infants: 5-year experience at a single center. J Matern Fetal Neonatal Med. (2020) 33(22):3725–31. doi: 10.1080/14767058.2019.1583734
17. Norman M, Hallberg B, Abrahamsson T, Björklund LJ, Domellöf M, Farooqi A, et al. Association between year of birth and 1-year survival among extremely preterm infants in Sweden during 2004–2007 and 2014–2016. JAMA. (2019) 321(12):1188–99. doi: 10.1001/jama.2019.2021
18. Schanler RJ. Outcomes of human milk-fed premature infants. Semin Perinatol. (2011) 35:29–33. doi: 10.1053/j.semperi.2010.10.005
19. Cao Y, Jiang S, Sun J, Hei M, Wang L, Zhang H, et al. Assessment of neonatal intensive care unit practices, morbidity, and mortality among very preterm infants in China. JAMA Network Open. (2021) 4(8):e2118904. doi: 10.1001/jamanetworkopen.2021.18904
Keywords: survival rate, mortality, periviable infant, neonatal, extremely preterm infants, management
Citation: Chen C, Xiong X, Zhao J, Wang M, Huang Z and Yang C (2022) Survival and care practices of periviable births of <24 weeks’ gestation—a single center retrospective study in China, 2015–2021. Front. Pediatr. 10:993922. doi: 10.3389/fped.2022.993922
Received: 14 July 2022; Accepted: 14 November 2022;
Published: 7 December 2022.
Edited by:
Sascha Meyer, Saarland University Hospital, GermanyReviewed by:
Hercília Guimarães, University of Porto, PortugalHilal Özkan, Uludağ University, Turkey
© 2022 Chen, Xiong, Zhao, Wang, Huang and Yang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Chuanzhong Yang eWFuZ2N6Z2RAMTYzLmNvbQ== Zhifeng Huang c3oxOTcxaHpmQDE2My5jb20=
Specialty Section: This article was submitted to Neonatology, a section of the journal Frontiers in Pediatrics
 Chun Chen
Chun Chen Xiaoyun Xiong
Xiaoyun Xiong Jie Zhao
Jie Zhao Zhifeng Huang
Zhifeng Huang Chuanzhong Yang
Chuanzhong Yang