
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Pediatr., 21 October 2022
Sec. Pediatric Otolaryngology
Volume 10 - 2022 | https://doi.org/10.3389/fped.2022.985375
This article is part of the Research TopicBasic and Clinical Research on Children Snoring and Obstructive Sleep Apnea SyndromeView all 11 articles
Objectives: To analyze obstructive sleep apnea (OSA)-related quality of life (QoL), the statuses of depression and anxiety, and to reveal the correlation between OSA-related QoL and two mental statuses in Chinese adolescent patients with cleft palate (CP).
Methods: The Obstructive Sleep Apnea Questionaire-18 (OSA-18), the Generalized Anxiety Disorder Scale (GAD-7) and the Patient Health Questionnaire-9 (PHQ-9) were applied to assess OSA-related QoL and the statuses of anxiety and depression in Chinese adolescent patients with CP, respectively. Non-CP adolescents were also included in the control group. OSA-related QoL and the two mental statuses were compared between the study and control groups. The correlation between the OSA-related QoL and two mental statuses was estimated in Chinese adolescent patients with CP.
Results: A total of 8.7% patients showed a moderate or high impact of OSA on QoL, while all the adolescents from the control group showed little impact. The mean total OSA-18 score of the study group (36.261 ± 13.500) was significantly higher than the control (28.435 ± 8.934). The mean PHQ-9 scores of the study group and the control group were statistically different (3.957 vs. 2.113). The GAD-7 score in the study group was slightly higher than the control group (3.043 vs. 2.194), while the proportion of moderate-severe anxiety in the study group was relatively larger than that in the control group (6.5% vs. 1.6%). Moreover, there was a positive correlation between the OSA-related QoL and the statuses of anxiety and depression respectively, and the differences in GAD-7 and PHQ-9 scores between the moderate or high impact group and the little impact group were statistically significant.
Conclusion: Chinese adolescents with CP reported a rate of moderate or high impact of OSA on QoL of 8.7%, which was significantly higher than adolescents without CP. The OSA-related QoL was worse and depression was severer in Chinese CP adolescents than in the control, while anxiety and depression in Chinese CP adolescents were associated with OSA-related QoL.
Cleft palate (CP) is one of the most common congenital abnormalities, which can lead to dysfunction of speech, breathing, and swallowing of the patients due to the abnormal anatomical structure of the palate and pharynx (1). CP might also bring nasal deformities, retrusive midface or small pharyngeal airway as the patients growing up, and herein exposes them to a high risk of obstructive sleep apnea (OSA) (2). It was found that the posterior airway space in adolescent patients after palatoplasty showed certain characteristics of OSA (3), which could affect the sleep-related breathing and related quality of life (QoL).
Sleep-disordered breathing (SDB), like OSA, could bring neuropsychiatric effects and adverse health consequences (4, 5), which could greatly affect the QoL of patients. It was reported that OSA had a correlation with mental disorders like anxiety and depression (6). Besides, it was also shown that anxiety and depression could affect sleep (7). Although sleep-related breathing problems had been found in patients with CP (8), their OSA-related QoL had not received due attention, and there was a lack of relevant study in Chinese patients with CP.
In this study, we sought to compare the OSA-related QoL, and the statuses of depression and anxiety, between patients and control adolescents, and ulteriorly demonstrate the correlation between the OSA-related QoL and these two mental statuses, anxiety and depression. The Obstructive Sleep Apnea Questionaire-18 (OSA-18) has been widely used to assess QoL in children with SDB in previous studies, in children with macroglossia and adenotonsillar hypertrophy for example (9, 10), and therefore was considered as a valid measure of health-related QoL (11). In our study, OSA-18 was applied to assess the QoL in children with CP, while the generalized anxiety disorder 7-item (GAD-7) scale and the Patient Health Questionnaire-9 (PHQ-9) were applied to assess the statuses of anxiety and depression. Based on this study, we tried to provide a theoretical basis for cleft palate care and possible psychological intervention.
Chinese Patients with a history of cleft palate hospitalized in West China Hospital of Stomatology, Sichuan University, between July 2019 and January 2021 were incorporated in the study group.
Inclusion criteria of the study group were as follows:
(1) Patients with cleft palate;
(2) Patients who had no other syndromic diseases;
(3) Patients who underwent palatoplasty at the age of 6 months to 2 years;
(4) Patients without secondary surgery of cleft palate or other types of speech surgery like posterior pharyngeal flap or orthognathic surgery at the time of data collecting;
(5) Patients aged above 10 (12) and under 17 (13).
Inclusion criteria of the control group were as follows:
(1) Individuals who had cone-beam computed tomography scan for other dental treatments;
(2) Individuals with normal speech and without significant nasal septal deviation or micromandible or other significant airway diseases;
(3) Individuals aged above 10 and under 17.
A total of 46 patients were enrolled (Mean age: 13.41 ± 2.14 years), while a total of 62 normal adolescents were enrolled (Mean age: 13.84 ± 0.91 years). Among the study group, 63.0% were males; 87.0% had cleft lip and palate, and 13.0% had cleft palate only; 26.1% were diagnosed with velopharyngeal insufficiency. In the control group, 54.8% were males.
The study was approved by the Ethics Committee of West China Hospital of Stomatology, Sichuan University (No. WCHSIRB-D-2016-084R1). All the parents of the patients enrolled in the study provided written informed consents.
The Obstructive Sleep Apnea Questionaire-18 (OSA-18) was used to assess the OSA-related QoL, which contained 18 items rated from 1 to 7 with a Likert scale. The 18 items were grouped into 5 domains: sleep disturbance, physical suffering, emotional distress, daytime problems, and caregiver concerns. A total score above 60 suggested that the sleep disorder had a moderate or high impact on QoL (14). Good reliability and validity of Chinese-version OSA-18 have been validated in patients aged 2–18 years old (15), and OSA-18 has been used in adolescent patients with cleft palate (2). The questionnaire was filled in by the patients' parents or legal guardians independently based on the situation of their children in the past 4 weeks (16).
The Generalized Anxiety Disorder 7-item (GAD-7) scale was given to adolescents themselves to assess their anxiety status over the last 2 weeks with 7 items graded on a 4-point Likert scale as 0 (not at all), 1 (several days), 2 (more than half the days), and 3 (nearly every day). The subjects were divided into normal (0–4), mild (5–9), moderate (10–14) and severe (15–21) according to the total score. Chinese-version GAD-7 has been widely used in Chinese population, notably in the cleft field (17), and has shown good reliability and validity among Chinese adolescents aged 10–17 years old (12).
The Patient Health Questionnaire-9 (PHQ-9) was applied to assess depression status in the past 2 weeks, which consisted of 9 items on a 4-point scale ranging from 0 (not at all) to 3 (nearly every day). A total score of 10 points was considered to be the dividing line between depression and non-depression. PHQ-9 has been widely used to assess depressive symptoms in patients with specific diseases (18–20), and the reliability and effectiveness of PHQ-9 have been validated in Chinese adolescents aged 11–17 years old (21), and has been applied to autistic patients aged 10–18 in Singapore (22).
In this study, all subjects received questionnaires of the Chinese version and to ensure that each item was fully understood, questionnaires were completed under the guidance of trained volunteers.
Statistical analysis was performed using SPSS 26.0 (IBM Corp., Armonk, NY, USA), and count data were expressed as the mean ± standard deviation (SD). Mann–Whitney U test was used to compare the two independent variables between groups, and categorical variables (impact on QoL) were compared between the groups using Fisher exact test, while Spearman's rank correlation was used to estimate the correlation among the OSA-related QoL, anxiety status and depression status. Shapiro-Wilk demonstrated non-normal distribution of those statistics. P-values <0.05 were statistically significant.
The mean total OSA-18 scores of the study and control groups were 36.261 and 28.435 points respectively, and differences in total OSA-18 score, domains including emotional distress, daytime problems and caregiver concern and several items of OSA-18 (OSA-18-8/10/12/15/16/17/18) were statistically significant, among which the mean score of the study group was higher than that of the control group (Table 1). 8.7% of the total OSA-18 scores were above 60 in the study group, showing moderate or high impact on QoL, while all the adolescents from the control group showed little impact, which was statistically significant (Table 2).
There was no statistically significant difference in GAD-7 total score and scores of each item between the study group and the control group. However, the mean GAD-7 total score in the study group was slightly higher than the control group (3.043 vs. 2.194) (Table 3). Besides, the proportion of moderate-severe anxiety in the study group was larger than in the control group (6.5% vs. 1.6%) (Table 4).
The mean total PHQ-9 scores of the study group and the control group were statistically different (3.957 vs. 2.113), and the mean scores of items “Poor appetite or overeating” and “Feeling bad about yourself or that you are a failure or have let yourself or your family down” showed statistical difference (Table 5).
There was a positive correlation between the OSA-related QoL and the statuses of anxiety and depression, respectively. The total OSA-18 score and domains including sleep disturbance, emotional distress and caregiver concern were all positively correlated with GAD-7 scores, while the total OSA-18 score and domains including sleep disturbance, emotional distress, daytime problems and caregiver concern were positively correlated with PHQ-9 scores (Table 6).
The differences of GAD-7 and PHQ-9 scores between the moderate or high impact group and the little impact group were statistically significant, which demonstrated the influence of OSA-related QoL on these two mental statuses (Table 7).
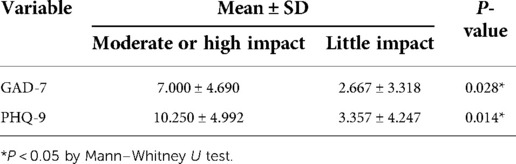
Table 7. The GAD-7 and PHQ-9 scores of different impact situations of OSA-related QoL in the study group.
Cleft palate may lead to nasal deformities, retrusive midface or small pharyngeal airway, which bring a high risk of OSA (2). OSA-related symptoms, such as snoring and noisy breathing during sleep were often reported in children with CP (3). Even after palatoplasty, upper airway dimensions were still reduced in patients with CP (23). OSA had a significant impact on quality of life, which could lead to anxiety and depression (24, 25) and result in adverse societal and individual correlates (26). In this study, we aimed to analyze OSA-related QoL and the statuses of depression and anxiety, and to further reveal the correlation between OSA-related QoL and two mental statuses in Chinese adolescent patients with CP.
According to OSA-18 results, we found that the average OSA-18 score of Chinese adolescent patients with CP was higher than the controls, which might reveal that adolescents with CP were at higher risk of OSA, consistent with the results evaluated by the Pediatric Sleep Questionnaire (PSQ) and polysomnography (PSG) in the previous studies (27, 28). The rate of moderate or high impact of OSA on QoL in children with CP (8.7%), which was approximately consistent with previous studies (9.5%) (2), was significantly higher than that of the control group (0%). As for the statistically significant domains of emotional distress, daytime problems and caregiver concern in the control group, we found that the influence of OSA on QoL in patients with CP was more manifested in emotion, behavior and the influence on caregivers than the physical symptoms, which coincided with previous studies in children with CP (29–31). Compared with non-cleft, the clinical symptoms of OSA in children with CP was similar (29). However, aggressive behavior and defiant temper were confirmed in children with CP under the influence of sleep-disordered breathing (30), and daytime functional problems such as daytime sleepiness and inattention were reported in children with CP in previous studies (31).
Our research further confirmed these conditions not only in children but also in adolescents with CP. As for the caregiver concern dimension, the sleep-disordered breathing problems of children with CP were often reported by their parents (3), and under greater pressure, the quality of life and psychology of parents of children with CP were affected simultaneously (32).
Our results showed that 6.5% of adolescent patients with CP were in moderate or severe anxiety, compared with 1.6% in the control group. However, no significant difference in total GAD-7 scores and scores of each item between the study group and the control group was found, which was consistent with the results of previous studies that there was no significant difference in life satisfaction and anxiety between patients with CP and the non-CP control group (17, 33), but the proportion of patients with CP reporting anxiety problems was higher than that of the control group (34).
In contrast to anxiety status, there were significant differences in total PHQ-9 scores screening depression between the study group and the control group. As some studies have shown, compared with healthy children, depression in children with CP was more common (35). Items that demonstrated statistically significant difference were “Poor appetite or overeating” and “Feeling bad about yourself or that you are a failure or have let yourself or your family down”. Patients with CP had difficulty chewing, especially biting hard food (36), and showed a more negative self-awareness (37), which might explain why the study group showed higher scores than the control in those items.
It used to be thought that the anxiety and depression of patients with CP mainly came from their abnormal appearance and pronunciation (38). However, our study reported that OSA-related QoL were also associated with anxiety and depression in Chinese adolescent patients with CP. Beyond this, the statuses of anxiety and depression between the moderate or high impact group and the little impact group of OSA-related QoL showed statistical significance. Previous studies have confirmed the relationship between OSA and the statuses of anxiety and depression (6, 39), and the same conclusion was drawn in Chinese adolescent patients with CP in our study.
The results showed that anxiety and depression were correlated with a number of domains of OSA-related QoL. However, there was no significant correlation between the physical suffering dimension and the statuses of anxiety and depression, which might be interpreted as, compared to the discomfort caused by sleep breathing symptoms, the psychological impact of CP was more from the mental and behavioral problems caused by it. The emotional distress dimension of OSA-18 scale was significantly correlated with GAD-7 and PHQ-9 scales, which reflected the homogeneity of the three scales in evaluating psychological status. It was also found that the caregiver concern dimension had significant correlation with GAD-7 and PHQ-9 scales. Other studies have shown that the life quality of parents of children with CP were relatively poor (32), while this study showed that this influence may be mutual. The stress and worries from parents were also related to the psychological status of children, social support and correct coping strategies being beneficial to alleviate this influence (40). Interestingly, depression symptoms were uniquely associated with daytime problems domain, which meant that children's OSA-related negative behavior during the day led to depression rather than anxiety. It might be explained that sleep may have etiologically distinct and directional associations with anxiety and depression (41).
There were some limitations in our study. The sample size should be enhanced in the future. This study was conducted only in a stomatological hospital in western China. Also, no conclusion could be drawn on the direction of causality because of the study type of cross-sectional study, and there was only scale measurement focusing on QoL, lacking objective sleep measurement. Another limitation that should be mentioned is that OSA-18 is a caregiver-administered tool based on targeted discussions with caregivers of children with OSA (16), but studies have shown discrepancies in patients vs. parents' perceptions of their conditions (42–44). Thus, further study is needed with a suitable patient-administered tool for screening OSA.
Chinese adolescents with CP reported a prevalence of rate of moderate or high impact of OSA on QoL of 8.7%, which was significantly higher than adolescents without CP. The OSA-related QoL was worse and depression was severer in Chinese CP adolescents than the control. Anxiety and depression in Chinese CP adolescents were associated with OSA-related QoL.
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding authors.
The studies involving human participants were reviewed and approved by the Ethics Committee of West China Hospital of Stomatology, Sichuan University (No. WCHSIRB-D-2016-084R1). Written informed consent to participate in this study was provided by the participants’ legal guardian/next of kin.
ZX and CY contributed equally to this work. ZX, CY, YZ, YY, WX and YZ contributed to the collection of data. ZX, CY, YZ, and TC analyzed the data. ZX, CY, BS, HH and CG contributed to writing and revising the paper. BS, HH and CG supervised the research. All authors contributed to the article and approved the submitted version.
This work was supported by the Research and Development Program, West China Hospital of Stomatology, Sichuan University (RD-02-202107), and Sichuan Province Science and Technology Support Program granted to H. Huang (2022NSFSC0743).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Massenburg BB, Hopper RA, Crowe CS, Morrison SD, Alonso N, Calis M, et al. Global burden of orofacial clefts and the world surgical workforce. Plast Reconstr Surg. (2021) 148(4):568e–80e. doi: 10.1097/prs.0000000000008334
2. Ho ACH, Savoldi F, Wong RWK, Fung SC, Li SKY, Yang Y, et al. Prevalence and risk factors for obstructive sleep apnea syndrome among children and adolescents with cleft lip and palate: a survey study in Hong Kong. Cleft Palate Craniofac J. (2021):10556656211068306. doi: 10.1177/10556656211068306. [Epub ahead of print]34939456
3. Rose E, Thissen U, Otten JE, Jonas I. Cephalometric assessment of the posterior airway space in patients with cleft palate after palatoplasty. Cleft Palate Craniofac J. (2003) 40(5):498–503. doi: 10.1597/1545-1569_2003_040_0498_caotpa_2.0.co_2
4. Shah N, Roux F, Mohsenin V. Improving health-related quality of life in patients with obstructive sleep apnea: what are the available options? Treat Respir Med. (2006) 5(4):235–44. doi: 10.2165/00151829-200605040-00002
5. Chen L, Bai C, Zheng Y, Wei L, Han C, Yuan N, et al. The association between sleep architecture, quality of life, and hypertension in patients with obstructive sleep apnea. Sleep Breath. (2022). doi: 10.1007/s11325-022-02589-z. [Epub ahead of print]
6. Garbarino S, Bardwell WA, Guglielmi O, Chiorri C, Bonanni E, Magnavita N. Association of anxiety and depression in obstructive sleep apnea patients: a systematic review and meta-analysis. Behav Sleep Med. (2020) 18(1):35–57. doi: 10.1080/15402002.2018.1545649
7. Jansson-Fröjmark M, Lindblom K. A bidirectional relationship between anxiety and depression, and insomnia? A prospective study in the general population. J Psychosom Res. (2008) 64(4):443–9. doi: 10.1016/j.jpsychores.2007.10.016
8. Muntz H, Wilson M, Park A, Smith M, Grimmer JF. Sleep disordered breathing and obstructive sleep apnea in the cleft population. Laryngoscope. (2008) 118(2):348–53. doi: 10.1097/MLG.0b013e318158195e
9. Harada T, Yamanishi T, Kurimoto T, Nishio J. Improved quality of life for children with Beckwith-Wiedemann syndrome following tongue reduction surgery. J Craniofac Surg. (2019) 30(1):163–6. doi: 10.1097/scs.0000000000004823
10. Patel D, Haszard J, Kee R, Smith L, Maessen S, Schaughency E, et al. Can sleep questionnaires predict adenotonsillectomy outcome for children with sleep disordered breathing? Int J Pediatr Otorhinolaryngol. (2022) 153:111001. doi: 10.1016/j.ijporl.2021.111001
11. Lushington K, Kennedy D, Martin J, Kohler M. Quality-of-life but not behavior improves 48-months post-adenotonsillectomy in children with SDB. Sleep Med. (2021) 81:418–29. doi: 10.1016/j.sleep.2021.02.057
12. Sun J, Liang K, Chi X, Chen S. Psychometric properties of the generalized anxiety disorder scale-7 item (GAD-7) in a large sample of Chinese adolescents. Healthcare (Basel, Switzerland). (2021) 9(12):1709. doi: 10.3390/healthcare9121709
13. Kang KT, Weng WC, Yeh TH, Lee PL, Hsu WC. Validation of the Chinese version OSA-18 quality of life questionnaire in Taiwanese children with obstructive sleep apnea. J Formos Med Assoc. (2014) 113(7):454–62. doi: 10.1016/j.jfma.2012.10.002
14. Caixeta JAS, Sampaio JCS, Costa VV, Silveira IMBD, Oliveira CRF, Caixeta LCAS, et al. Long-term impact of adenotonsillectomy on the quality of life of children with sleep-disordered breathing. Int Arch Otorhinolaryngol. (2021) 25(1):e123–8. doi: 10.1055/s-0040-1709195
15. Huang YS, Hwang FM, Lin CH, Lee LA, Huang PY, Chiu ST. Clinical manifestations of pediatric obstructive sleep apnea syndrome: clinical utility of the Chinese-version Obstructive Sleep Apnea Questionaire-18. Psychiatry Clin Neurosci. (2015) 69(12):752–62. doi: 10.1111/pcn.12331
16. Franco RA Jr., Rosenfeld RM, Rao M. First place–resident clinical science award 1999. Quality of life for children with obstructive sleep apnea. Otolaryngol Head Neck Surg. (2000) 123(1 Pt 1):9–16. doi: 10.1067/mhn.2000.105254
17. Xie Z, Yang C, Zhao Y, Yang Y, Xia W, Zong Y, et al. Anxiety in Chinese patients with cleft lip and/or palate: a preliminary study. Front Pediatr. (2022) 10:842470. doi: 10.3389/fped.2022.842470
18. Guo Q, Zheng Y, Shi J, Wang J, Li G, Li C, et al. Immediate psychological distress in quarantined patients with COVID-19 and its association with peripheral inflammation: a mixed-method study. Brain Behav Immun. (2020) 88:17–27. doi: 10.1016/j.bbi.2020.05.038
19. Dbouk N, Arguedas MR, Sheikh A. Assessment of the PHQ-9 as a screening tool for depression in patients with chronic hepatitis C. Dig Dis Sci. (2008) 53(4):1100–6. doi: 10.1007/s10620-007-9985-z
20. Richardson EJ, Richards JS. Factor structure of the PHQ-9 screen for depression across time since inkury among persons with spinal cord injury. Rehabil Psychol. (2008) 53(2):243–9. doi: 10.1037/0090-5550.53.2.243
21. Leung DYP, Mak YW, Leung SF, Chiang VCL, Loke AY. Measurement invariances of the PHQ-9 across gender and age groups in Chinese adolescents. Asia Pac Psychiatry. (2020) 12(3):e12381. doi: 10.1111/appy.12381
22. Pilunthanakul T, Goh TJ, Fung DSS, Sultana R, Allen JC, Sung M. Validity of the patient health questionnaire 9-item in autistic youths: a pilot study. BMC Psychiatry. (2021) 21(1):564. doi: 10.1186/s12888-021-03556-w
23. MacLean JE, Hayward P, Fitzgerald DA, Waters K. Cleft lip and/or palate and breathing during sleep. Sleep Med Rev. (2009) 13(5):345–54. doi: 10.1016/j.smrv.2009.03.001
24. Shapiro AL. Anxiety in middle-aged men with obstructive sleep apnea: state of the science. J Am Assoc Nurse Pract. (2014) 26(12):689–95. doi: 10.1002/2327-6924.12118
25. Comsa M, Anderson KN, Sharma A, Yadav VC, Watson S. The relationship between sleep and depression and bipolar disorder in children and young people. BJPsych Open. (2022) 8(1):e27. doi: 10.1192/bjo.2021.1076
26. Hohls JK, König HH, Quirke E, Hajek A. Anxiety, depression and quality of life-a systematic review of evidence from longitudinal observational studies. Int J Environ Res Public Health. (2021) 18(22):12022. doi: 10.3390/ijerph182212022
27. Gorucu-Coskuner H, Saglam-Aydinatay B, Aksu M, Ozgur FF, Taner T. Comparison of positive screening for obstructive sleep apnea in patients with and without cleft lip and palate. Cleft Palate Craniofac J. (2020) 57(3):364–70. doi: 10.1177/1055665619875321
28. Robison JG, Otteson TD. Increased prevalence of obstructive sleep apnea in patients with cleft palate. Arch Otolaryngol Head Neck Surg. (2011) 137(3):269–74. doi: 10.1001/archoto.2011.8
29. MacLean JE, Fitzsimons D, Fitzgerald D, Mbbs KW. Comparison of clinical symptoms and severity of sleep disordered breathing in children with and without cleft lip and/or palate. Cleft Palate Craniofac J. (2017) 54(5):523–9. doi: 10.1597/15-309
30. Moraleda-Cibrián M, Edwards SP, Kasten SJ, Warschausky SA, Buchman SR, Monasterio-Ponsa C, et al. Impact of sleep-disordered breathing on behavior and quality of life in children aged 2 to 7 years with non-syndromic cleft lip and/or palate. Pediatr Pulmonol. (2021) 56(10):3358–65. doi: 10.1002/ppul.25611
31. Moraleda-Cibrián M, Edwards S, Kasten S, Warschausky S, Buchman S, O'Brien L. Sleep-related movement disorders and growing pains: differences in daytime and bedtime behavior in 2-6 year old children with cleft palate. Sleep Med. (2021) 85:303–8. doi: 10.1016/j.sleep.2021.07.026
32. Aslan BI, Gülşen A, Tirank ŞB, Findikçioğlu K, Uzuner FD, Tutar H, et al. Family functions and life quality of parents of children with cleft lip and palate. J Craniofac Surg. (2018) 29(6):1614–8. doi: 10.1097/scs.0000000000004611
33. Cheung LK, Loh JS, Ho SM. Psychological profile of Chinese with cleft lip and palate deformities. Cleft Palate Craniofac J. (2007) 44(1):79–86. doi: 10.1597/05-053
34. Ramstad T, Ottem E, Shaw WC. Psychosocial adjustment in Norwegian adults who had undergone standardised treatment of complete cleft lip and palate. II. Self-reported problems and concerns with appearance. Scand J Plastic Reconstruct Surg Hand Surg. (1995) 29(4):329–36. doi: 10.3109/02844319509008968
35. Demir T, Karacetin G, Baghaki S, Aydin Y. Psychiatric assessment of children with nonsyndromic cleft lip and palate. Gen Hosp Psychiatry. (2011) 33(6):594–603. doi: 10.1016/j.genhosppsych.2011.06.006
36. Vaiciunaite R, Mitalauskiene A, Vasiliauskas A. The relationship between congenital cleft lip and palate malformation, skeletal and dental occlusal anomalies, and the influence of its treatment on affected patients’ oral health-related quality of life (OHRQoL). Stomatologija. (2020) 22(4):116–9. PMID: 3384728333847283
37. Tyl J, Dytrych Z, Helclová H, Schüller V, Matĕjcek Z, Beránková A. Psychological and social stress in children with cleft lip and palate. Cesk Pediatr. (1990) 45(9):532–6. PMID: 2078890 Psychický a sociální stres dĕtí s rozstĕpem rtu a patra.2078890
38. Hunt O, Burden D, Hepper P, Johnston C. The psychosocial effects of cleft lip and palate: a systematic review. Eur J Orthod. (2005) 27(3):274–85. doi: 10.1093/ejo/cji004
39. BaHammam AS, Kendzerska T, Gupta R, Ramasubramanian C, Neubauer DN, Narasimhan M, et al. Comorbid depression in obstructive sleep apnea: an under-recognized association. Sleep Breath. (2016) 20(2):447–56. doi: 10.1007/s11325-015-1223-x
40. Baker SR, Owens J, Stern M, Willmot D. Coping strategies and social support in the family impact of cleft lip and palate and parents’ adjustment and psychological distress. Cleft Palate Craniofac J. (2009) 46(3):229–36. doi: 10.1597/08-075.1
41. Johnson EO, Roth T, Breslau N. The association of insomnia with anxiety disorders and depression: exploration of the direction of risk. J Psychiatr Res. (2006) 40(8):700–8. doi: 10.1016/j.jpsychires.2006.07.008
42. Huang H, Chen N, Yin H, Skirko JR, Guo C, Ha P, et al. Validation of the Chinese velopharyngeal insufficiency effects on life outcomes instrument. Laryngoscope. (2019) 129(11):E395–E401. doi: 10.1002/lary.27792
43. Sakran KA, Al-Rokhami RK, Wu M, Chen N, Yin H, Guo C, et al. Correlation of the Chinese velopharyngeal insufficiency-related quality of life instrument and speech in subjects with cleft palate. Laryngoscope Invest Otolaryngol. (2022) 7(1):180–9. doi: 10.1002/lio2.705
44. Denadai R, Raposo-Amaral CE, Sabbag A, Ribeiro ra, Buzzo CL, Raposo-Amaral CA, et al. Measuring patient-reported health-related quality of life in velopharyngeal insufficiency: reliability and validity of the Brazilian Portuguese version of the VELO instrument. Cleft Palate Craniofac J. (2019) 56(9):1195–205. doi: 10.1177/1055665619846763
Keywords: cleft palate, OSA-related QoL, sleep-disordered breathing, anxiety, depression, OSA-18, GAD-7, PHQ-9
Citation: Zong Y, Cheng X, Xia W, Xie Z, Yang Y, Shi B, Gong C and Huang H (2022) The correlation between OSA-related quality of life and two mental statuses in adolescent Chinese patients with cleft palate: A comprehensive study. Front. Pediatr. 10:985375. doi: 10.3389/fped.2022.985375
Received: 3 July 2022; Accepted: 20 September 2022;
Published: 21 October 2022.
Edited by:
Jingying Ye, Tsinghua University, ChinaReviewed by:
Rafael Denadai, A/D DermePlastique, Brazil© 2022 Zong, Cheng, Xia, Xie, Yang, Shi, Gong and Huang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Caixia Gong Z29uZ2NhaXhpYTAxQDE2My5jb20= Hanyao Huang aHVhbmdoYW55YW9fY25Ac2N1LmVkdS5jbg==
†These authors have contributed equally to this work
Specialty Section: This article was submitted to Pediatric Otolaryngology, a section of the journal Frontiers in Pediatrics
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.