- 1Department of Child Health Nursing, Graduate School of Nursing Sciences, St. Luke's International University, Tokyo, Japan
- 2Department of Nursing, School of Medicine, Yokohama City University, Yokohama, Japan
- 3Department of Regional Pediatrics and Perinatology Center for Transition to Adult Congenital Health Disease, Graduate School of Medicine, Ehime University, Ehime, Japan
Health literacy, which is the ability to find, understand, and use information as well as services to make informed health-related decisions and actions, is essential for ensuring that youths with chronic diseases adapt to and live with their illnesses. However, in Japan, an appropriate approach for measuring health literacy levels among children is yet to be developed. The Health Literacy and Resiliency Scale for Youth (HLRS-Y) was developed by Kathy Bradley-Klug and her colleagues to assess health literacy, resiliency, and self-advocacy/support among youths aged between 13 and 21 years with chronic illnesses in the United States of America (United States). In this study, we aimed to develop a Japanese version of the HLRS-Y and evaluate its content validity. After receiving approvals from the original authors, four nurse researchers with expertise in pediatric nursing translated the scale into Japanese (forward translation). Afterwards, the appropriateness of each expression was examined by a pediatrician. Next, an English native speaker translated the expressions into English (back-translation). We reported the back-translated version of the scale to the original authors to confirm its accuracy. The scale's content validity index (CVI) was evaluated by health professionals working in the fields of pediatric, transitional, and adult health care. The participants rated the items using a four-point scale. Each item was evaluated for a minimum item-level content validity index (I-CVI) value of 0.78. The scale's total and subscale validities were evaluated using a minimum scale-level content validity index based on an average (S-CVI/Ave) value of 0.90. Eleven participants responded to an online survey for evaluating content validity. Of the 36 items, 34 met the I-CVI criteria. Two items did not exceed the criteria's value, but they approximated it. The values of the S-CVI/Ave were 0.96, thereby satisfying the criteria's requirements. Based on the results, it was confirmed that the Japanese version of the HLRS-Y had good content validity. Future studies should examine the factor validity, known group validity, and reliability of this scale.
Introduction
As the number of youths with special health and medical care needs increases, it is critical for health care providers to maximize the youths' abilities and potential while providing high-quality services appropriate to their developmental stages (1). Achieving this objective requires not only enhancing medical health management but also supporting the development of various abilities, such as health literacy and resiliency.
In 1998, the World Health Organization (WHO) defined health literacy (HL) as “the achievement of a level of knowledge, personal skills, and confidence to take action to improve personal and community health by changing personal lifestyles and living conditions (2).” HL involves the capacity to make sound health decisions, and as one of the health promotion outcomes, it has been attracting attention since the 2000s. HL is a necessary skill for the twenty-first century (3).
Research on HL has developed significantly over the past two decades. Prior studies have shown an association between HL and health outcomes among healthy adults. Low levels of HL are associated with poor health knowledge, noncompliance with medical visit schedules, low rates of medication verification when taking medications, and high rates of hospitalization as well as emergency room usage (4). The acquirement and promotion of HL also results in increased access to adequate health services and health management as well as improved healthcare provider-patient relationships, health-related decisions, and lifestyle choices (5–7).
On the other hand, research on HL among children has been limited owing to the lack of appropriate measurement tools. Although several scales for assessing fundamental HL among children exist, there is no self-administered scale focusing on the independent and subjective evaluation of HL in specific conditions (8). Further research on HL scales that consider various demographic characteristics, such as age, disease patterns, family relationships, social connections, and other factors, is required to ensure that children are respected (9, 10).
In 2017, Kathy Bradley-Klug et al. developed the Health Literacy and Resiliency Scale for Youth (HLRS-Y) to assess HL, resiliency, and self-advocacy/support among 13 to 21-year-olds suffering from chronic ilnesses in the United States (11, 12). The researchers who developed the original scale determined that self-care/management, adaptive coping, and a supportive environment are essential for ensuring that children with chronic illnesses adapt and survive (11, 12). To achieve this objective, they designed the scale to focus on HL (the ability for an individual to make daily decisions regarding their health care and assert their health-related needs) and resilience (self-efficacy, self-regulation, and a sense of connectedness) as essential components aimed at helping children suffering from chronic illnesses adapt and grow (11, 12).
The target population for this scale was defined as youth aged between 13 and 21 years. The items included in the scale were designed to consider the complex and specific situations associated with prioritizing autonomy, building relationships with other individuals outside the family, and integrating identity when dealing with chronic health conditions. This scale comprised 36 items: 10 for HL, 12 for resilience, and 14 for self-advocacy/support, which were rated using a four-point scale (strongly agree, agree, disagree, and strongly disagree). The scale has been verified for factor validity and the Cronbach's alpha coefficients for each subscale were 0.87 for HL, 0.93 for resilience, and 0.79 for support and self-advocacy (11, 12). The strength of this scale is that it is self-administered, and it questions participants about independent health management factors that are necessary for them to live with chronic illnesses without giving them the feeling that they are being tested.
However, currently, in Japan, HL levels among children and adolescents suffering from chronic illnesses are not known, and an appropriate approach for measuring HL levels among such individuals is yet to be developed. Therefore, it was necessary to translate the HLRS-Y into Japanese. Referring to the consensus-based standards for the selection of health status measurement instruments (COSMIN) guidelines (13), first, permission to use and translate the scale was obtained from the authors of the original version. Second, forward translation of the scale was independently performed by four nurse researchers, fluent in English and specializing in pediatric nursing. Afterwards, the contents were reviewed and summarized through discussion. Next, the appropriateness of each expression was examined by one pediatrician. Third, the back-translation into English was performed by an English native speaker. Finally, it was verified whether the Japanese expressions were smooth and easy to understand among youths between the ages of 13 and 21 while still remaining as direct a translation as possible.
Therefore, in this study, we aimed to develop the Japanese version of the HLRS-Y and evaluate its content validity.
Material and methods
Content validity index survey
Participants
Through snowball sampling, 18 experts in the fields of pediatric, transitional, and adult health care were requested to participate in this study. The experts included physicians, nurses, university professors in the fields of nursing and education, social workers, psychologists, and independence supporters for specific pediatric chronic disease. We also recruited adult patients with congenital heart diseases as well as survivors of childhood cancer.
Survey method
The survey was conducted using a web-based self-administered questionnaire. The survey period was February 16, 2022 to February 25, 2022.
Survey contents
To obtain the professional background of the participants, we asked them about their current role, qualifications, and years of experience engaging with patients aged between 13and 21 years with childhood-onset diseases (this included the participants' years of clinical experience, education, and research).
Regarding the content validity of the Japanese version of the HLRS-Y, we asked the participants to rank the validity of the items in each domain (HL, resiliency, and self-advocacy/support) on a four-point Likert scale: 4 = highly relevant; 3 = quite relevant; 2 = somewhat relevant; and 1 = not relevant. Additionally, for each domain, we asked the participants to provide their revisions and comments regarding the items in the free-description section.
Analysis method
We relied on the item-level content validity index (I-CVI), which is calculated using the number of respondents providing a rating of three or four divided by the total number of respondents for all the items. The criterion value for I-CVI was set at 0.78 (14). We also evaluated the scale-level content validity index based on average (S-CVI/Ave), which is the average of the I-CVI. The criterion value for S-CVI/Ave was set at 0.90 (14).
Ethical considerations
In compliance with the Declaration of Helsinki, 1964, we considered the protection of human rights (15). The human rights of the individuals were defended. In this study, there was no direct intervention on the participants, and it does not contain any personal information. It was also explained to the participants that they could choose to respond and there would be no disadvantages associated with non-participation.
Result
Demographics of the participants
Eleven valid responses were received (valid response rate: 61.1%). The eleven participants were as follows: two specialist physicians (pediatric oncologist and adult cardiologist), one Certified Nurse Specialist in pediatric nursing, one social worker, one university professor of nursing, one university professor of education, one psychologist, one independence supporter for specific pediatric chronic disease, and three patients (one pediatric cancer survivor and two patients with congenital heart disease). The mean level of the years of clinical experience and years of education as well as research involving individuals suffering from chronic illnesses who are aged between 13 and 21 years was 21.0 (SD = 12.5).
CVI
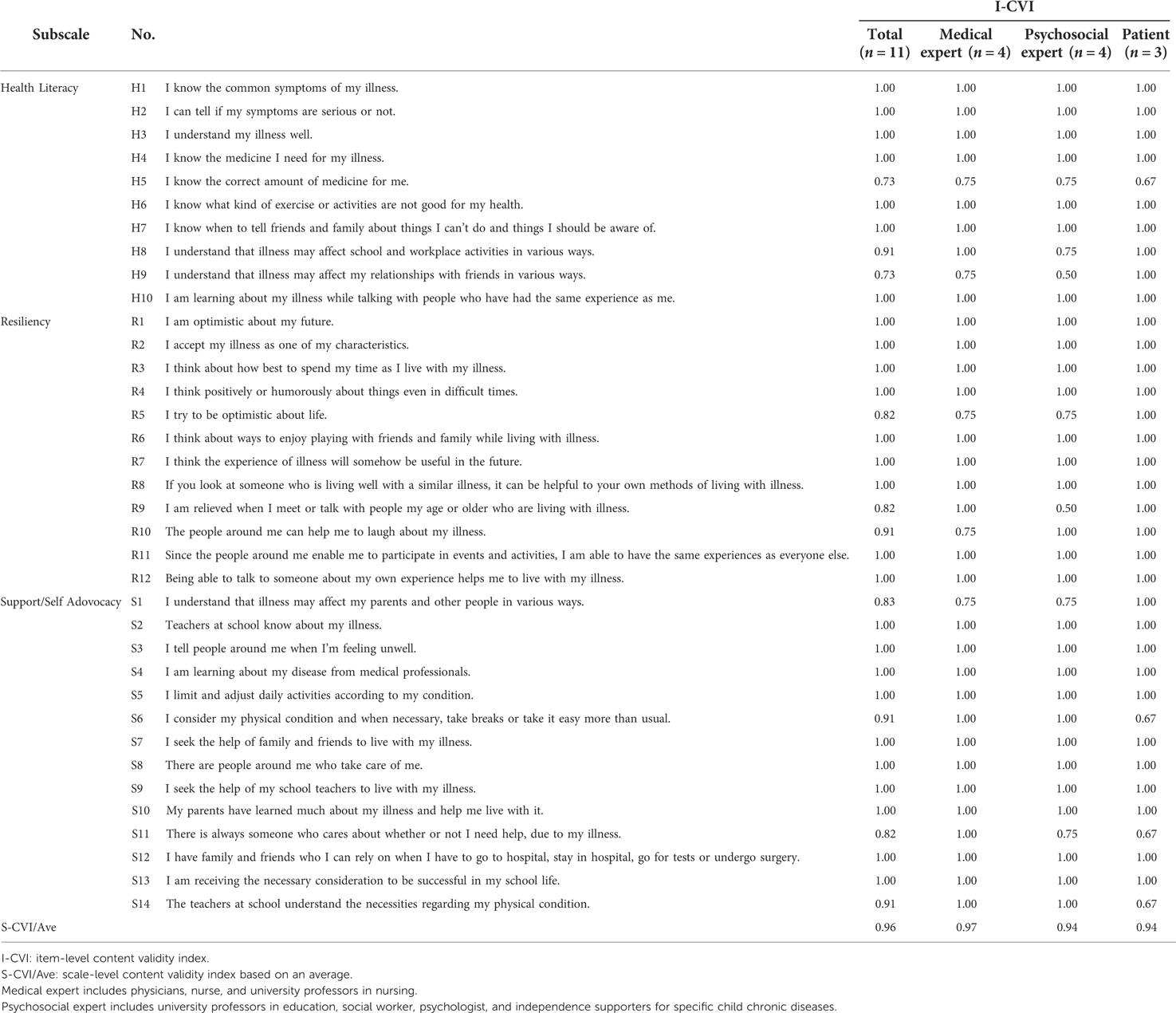
Regarding the scale's total validity, the value of the S-CVI/Ave was 0.96, which exceeded the criterion's expected levels (0.90). As shown in Table 1, 26 out of 36 items had an I-CVI of 1.00, which is the upper limit. The other four items scored 0.91, each with another four items with a score of 0.82.
There were two items for which the I-CVI values were 0.73, which was less than the criterion's expected levels (0.78). Both of these items (H5 and H9) were related to HL. Regarding H5, “I know the correct amount of medicine for me,” the participants who provided ratings of less than three or four were an adult cardiologist, an independence supporter for specific pediatric chronic disease, and a patient with congenital heart disease. The cardiologist commented that “I think the dosage for medication (s) is unnecessary knowledge.” Regarding H9, “I understand that illness may affect my relationships with friends in various ways,” the participants who provided ratings of less than three or four were a pediatric oncologist, a university professor of education, and a psychologist. The psychologist commented that “It is difficult to answer because the question is not clear.”
The I-CVI was above the criterion's expected levels. However, one patient provided a comment regarding R10: “The people around me can help me to laugh about my illness.,” stating that the phrase “laugh about my illness” might have a negative connotation in Japanese. For any other items, all the experts did not provide any comments regarding the invasive nature of the expressions to the patients involved in this study.
For some items in the self-advocacy/support criterion, there were comments pointing out that the word “school” might have resulted in difficulty in providing responses because the target population's age was up to 21 years. Additionally, a Certified Nurse Specialist commented, “Not everyone needs support. It is important to be able to ask for support if needed.”
Discussion
In this study, we developed a Japanese version of the HLRS-Y, and its content validity was assessed by eleven experts involved in supporting children with chronic illnesses, including the patients themselves. Previous studies recommend the participation of at least five experts in the CVI evaluation (16). The COSMIN Guidelines also recommend the participation of patients during content validity assessments (13). This study meets these requirements and is considered to have achieved a certain level of content validity evaluation. The results of this study were as follows: (1) The CVI of the items of HLRS-Y were above the criterion value, except for two items; (2) Experts, including the patients involved in this study confirmed that the items were not invasive; (3) Some items, such as school-related ones, might require attention in the way the questions were constructed to avoid the inclusion of situations that might not be applicable to some participants. These findings are discussed in detail as follows:
(1) The CVI of the items of HLRS-Y were above the criterion value, except for two items.
Overall, the value of the S-CVI/Ave of the HLRS-Y was 0.96, and 34 out of the 36 items met the I-CVI criteria, thereby demonstrating that the scale has good overall content validity. However, two items (H5, H9) did not meet the expected criterion's values. Regarding H5, it could be assumed that H5 did not exceed the criterion values because the experts tended to believe that the importance of medication management was in the name, timing, and effect of the medication rather than in the dosage. Several previous studies suggest that healthcare providers should consider various aspects to ensure that children suffering from chronic illnesses adhere to appropriate medication behaviors (e.g., providing information regarding the type, dosage, duration of use, and common side effects of medications, easy-to-understand medication regimens, creating self-administration plans, and regular consultations with physicians) (17–19). The Transition Readiness Assessment Questionnaire (23 items in total), which is one of the world's most used measures of transition readiness among patients with childhood-onset diseases, includes six items related to adverse medication reactions, appropriate intake, and drug names and dosages (20, 21). Because the HLRS-Y includes more items related to daily life, it has fewer items related to medical care than the TRAQ, with only two items related to medications. Because one of the items (H5) was related to medication dosage, the experts may have thought that there were other items required, such as the names and adverse reactions. On the other hand, the physician commented, “I believe specialized knowledge is unnecessary for understanding health.” Additionally, the patients stated, “I believe it depends on the individual,” and “As a patient, I believe I understand the bottom line, but it is still not as good as relying on that of the medical professionals.” We decided not to modify H5 in the Japanese version of the HLRS-Y because the scale focuses on daily life in general, and several participants commented that detailed knowledge was not always essential.
Regarding H9, the psychologist pointed out that it was difficult to understand the purpose of this question. In this item, “my health impacts” is assumed to be, for example, that the illness causes limitations in behavior, thereby making it difficult to move at the same pace as a group of friends. However, it could be difficult to understand from the first reading. Although children suffering from chronic illnesses are at a higher risk for emotional and behavioral problems (22), good friendships have been shown to have a positive impact on their psychological and physical health (23). In the Japanese version of the HLRS-Y, H9 was not modified in terms of prioritizing comparability with the original scale.
(2) Experts, including patients, confirmed that the items were not invasive.
In this study, the experts did not comment on the invasiveness of the expressions of all the items, except for R10. Regarding R10, one patient pointed out that the expression “laugh about my illness” may have a negative meaning. Therefore, we changed the expression from “humor” to “cheerful,” and we modified the item as follows: “People around me are cheerful and help me with my illness.”
(3) Some items, such as school-related ones, might require some attention in the way the questions were constructed to avoid including situations that might not be applicable to some participants.
There were items that asked about the situations in school. Because the target population for this scale was up to the age of 21 years, some participants might have already graduated from high school and were employed. The school situation was not applicable for them. In fact, patients of the age at which they are eligible for HLRS-Y may not have attended school. Specifically, severely diagnosed patients are reported to have a lower educational background (24, 25), and the more severely diagnosed patients are, the more likely for them to be out of school. However, this also suggests that severely ill patients experience some difficulties in school. Therefore, in the Japanese version of the HLRS-Y, we decided to include items related to school life. However, we shall consider adding “not applicable” as a response option.
Limitation
The expert panel included only three patients (pediatric cancer survivor and patients with congenital heart disease). When the original version of the HLRS-Y was developed, a wide range of patients was included in the study participants, including those with diabetes and juvenile rheumatoid arthritis (11). Therefore, it is necessary to increase the number of patients and the types of diseases. Guardians should also be included because they are likely to be concerned about whether the scale is invasive for their children.
In conclusion, the Japanese version of the HLRS-Y was found to have good content validity. Future studies should examine the factor validity, known group validity, and reliability of this scale.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
Author contributions
SS conceived of the present idea; SS, KK, RO and TH designed this study; SS performed the survey and analyzed the data; SS drafted the manuscript; KK, RO, and TH supervised the entire study process. All authors contributed to the article and approved the submitted version.
Funding
This study is part of the “Research into Treatment for Specific Child Chronic Diseases,” which is a project funded by the Ministry of Health, Labour and Welfare in Japan. This work was supported by the Ministry of Health, Labour and Welfare Intractable and Rare Disease Program (Grant No. JPMH21FC1017).
Acknowledgments
We would like to thank all those who participated in this survey. We also extend our deepest gratitude and appreciation to Bradley-Klug and Mercedes N. Cambric for their help in preparing the Japanese version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. American Academy of pediatrics, American academy of family physicians, American college of physicians-American society of international medicine. A consensus statement on health care transitions for young adults with special health care needs. Pediat. (2002) 110:1304–6. doi: 10.1542/peds.110.S3.1304
2. World Health Organization (1998). Division of Health Promotion, education, and communication. Health Promotion Glossary. https://apps.who.int/iris/handle/10665/64546 Accessed 26/5/2022
3. Kickbusch I. Health literacy: an essential skill for the twenty-first century. Health Educ. (2008) 108:101–4. doi: 10.1108/09654280810855559
4. Berkman ND, Sheridan SL, Donahue KE, Halpern DJ, Crotty K. Low health literacy and health outcomes: an updated systematic review. Ann Intern Med. (2011) 155:97–107. doi: 10.7326/0003-4819-155-2-201107190-00005
5. Nutbeam D. Health literacy as a public health goal: a challenge for contemporary health education and communication strategies into the 21st century. Health Promot Int. (2000) 15:259–67. doi: 10.1093/heapro/15.3.259
6. Heijmans M, Waverijn G, Rademakers J, van der Vaart R, Rijken M. Functional, communicative and critical health literacy of chronic disease patients and their importance for self-management. Patient Educ Couns Patient ed. (2015) 98:41–8. doi: 10.1016/j.pec.2014.10.006
7. Paasche-Orlow MK, Wolf MS. The causal pathways linking health literacy to health outcomes. Am J Health Behav. (2007) 31(Suppl 1):S19–26. doi: 10.5555/ajhb.2007.31.supp.S19
8. Guo S, Armstrong R, Waters E, Sathish T, Alif SM, Browne GR, et al. Quality of health literacy instruments used in children and adolescents: a systematic review. BMJ Open. (2018) 8:e020080. doi: 10.1136/bmjopen-2017-020080
9. Manganello JA. Health literacy and adolescents: a framework and agenda for future research. Health Educ Res. (2008) 23:840–7. doi: 10.1093/her/cym069
10. Bröder J, Okan O, Bauer U, Schlupp S, Pinheiro P. Advancing perspectives on health literacy in childhood and youth. Health Promot Int. (2020) 35:575–85. doi: 10.1093/heapro/daz041
11. Bradley-Klug K, Shaffer-Hudkins E, Lynn C, Jeffries DeLoatche K, Montgomery J. Initial development of the health literacy and resiliency scale: youth version. J Commun Healthc. (2017) 10:100–7. doi: 10.1080/17538068.2017.1308689
12. Cambric M. Validating the construct of resiliency in the health literacy and resiliency scale (HLRS-Y) with the child and youth resiliency measure. Tampa, Florida: University of South Florida Scholar Commons (2019).
13. Lidwine BM, Prinsen CA, Patrick DL, Alonso J, Bouter LM, de Vet HCW, et al. COSMIN Study Design checklist for patient reported outcome measurement instruments Version July 2019. https://www.cosmin.nl/wp-content/uploads/COSMIN-study-designing-checklist_final.pdf Accessed 26/5/2022
14. Polit DF, Beck CT, Owen SV. Is the CVI an acceptable indicator of content validity? Appraisal and recommendations. Res Nurs Health. (2007) 30:459–67. doi: 10.1002/nur.20199
15. Polit DF. World Medical Association Declaration of Helsinki Ethical Principles for Medical Research Involving Human Subjects. Available at DECLARATION OF HELSINKI. med.or.jpAccessed 26/5/2022.
16. Lynn MR. Determination and quantification of content validity. Nurs Res. (1986) 35(6):382–5. doi: 10.1097/00006199-198611000-00017
17. Haynes RB, McDonald H, Garg AX, Montague P. Interventions for helping patients to follow prescriptions for medications. Cochrane Database Syst Rev. (2002) 2:CD000011. doi: 10.1002/14651858.CD000011 Update in: Cochrane Database Syst Rev. 2005;(4):CD000011. PMID: 12076376
18. Gardiner P, Dvorkin L. Promoting medication adherence in children. Am Fam Physician. (2006) 74(5):793–8.16970023
19. Haynes RB, McKibbon KA, Kanani R. Systematic review of randomised trials of interventions to assist patients to follow prescriptions for medications. Lancet (London, England). (1996) 348(9024):383–6. doi: 10.1016/s0140-6736(96)01073-2
20. Wood DL, Sawicki GS, Miller MD, Smotherman C, Lukens-Bull K, Livingood WC, et al. The transition readiness assessment questionnaire (TRAQ):; its factor structure, reliability, and validity. Acad Pediatr. (2014) 14:415–22. doi: 10.1016/j.acap.2014.03.008
21. Sato Y, Ochiai R, Ishizaki Y, Nishida T, Miura K, Taki A, et al. Validation of the Japanese transition readiness assessment questionnaire (TRAQ). Pediatr Int. (2020) 62:22–8. doi: 10.1111/ped.14086
22. Hysing M, Elgen I, Gillberg C, Lundervold AJ. Emotional and behavioural problems in subgroups of children with chronic illness: results from a large-scale population study. Child Care Health Dev. (2009) 35(4):527–33. doi: 10.1111/j.1365-2214.2009.00967.x
23. Helgeson VS, Reynolds KA, Escobar O, Siminerio L, Becker D. The role of friendship in the lives of Male and female adolescents: does diabetes make a difference? J Adolesc Health. (2007) 40(1):36–43. doi: 10.1016/j.jadohealth
24. Cocomello L, Dimagli A, Biglino G, Cornish R, Caputo M, Lawlor DA, et al. Educational attainment in patients with congenital heart disease: a comprehensive systematic review and meta-analysis. BMC Cardiovasc Disord. (2021) 21(1):549. doi: 10.1186/s12872-021-02349-z
Keywords: transition to adult care, health literacy, resiliency, chronic illness, adolescents, young adults, self-advocacy
Citation: Sekine S, Kobayashi K, Ochiai R and Higaki T (2022) Content validity of the Japanese version of the health literacy and resiliency scale for youth with chronic illness. Front. Pediatr. 10:978079. doi: 10.3389/fped.2022.978079
Received: 25 June 2022; Accepted: 3 November 2022;
Published: 21 November 2022.
Edited by:
Judie Arulappan, Sultan Qaboos University, OmanReviewed by:
Péter Altorjai, European Academy of Paediatrics (EAP), BelgiumNanloh Samuel Jimam, University of Jos, Nigeria
© 2022 Sekine, Kobayashi, Ochiai and Higaki. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Saya Sekine MjFtbjAyMkBzbGNuLmFjLmpw
Specialty Section: This article was submitted to Children and Health, a section of the journal Frontiers in Pediatrics
 Saya Sekine
Saya Sekine Kyoko Kobayashi
Kyoko Kobayashi Ryota Ochiai
Ryota Ochiai Takashi Higaki
Takashi Higaki