- Unit of Pediatric Orthopedics, Department of Women – Mother – Child’s Care, Centre Hospitalier Universitaire Vaudois, Lausanne, Switzerland
Background: The Tübingen splint was initially developed for the treatment of stable developmental hip dysplasia (DDH). Later on, some authors expanded its include for the treatment of unstable DDH, but there remain some controversies in the literature. This study aims to compare the outcome between stable and unstable DDH treated with a Tübingen splint.
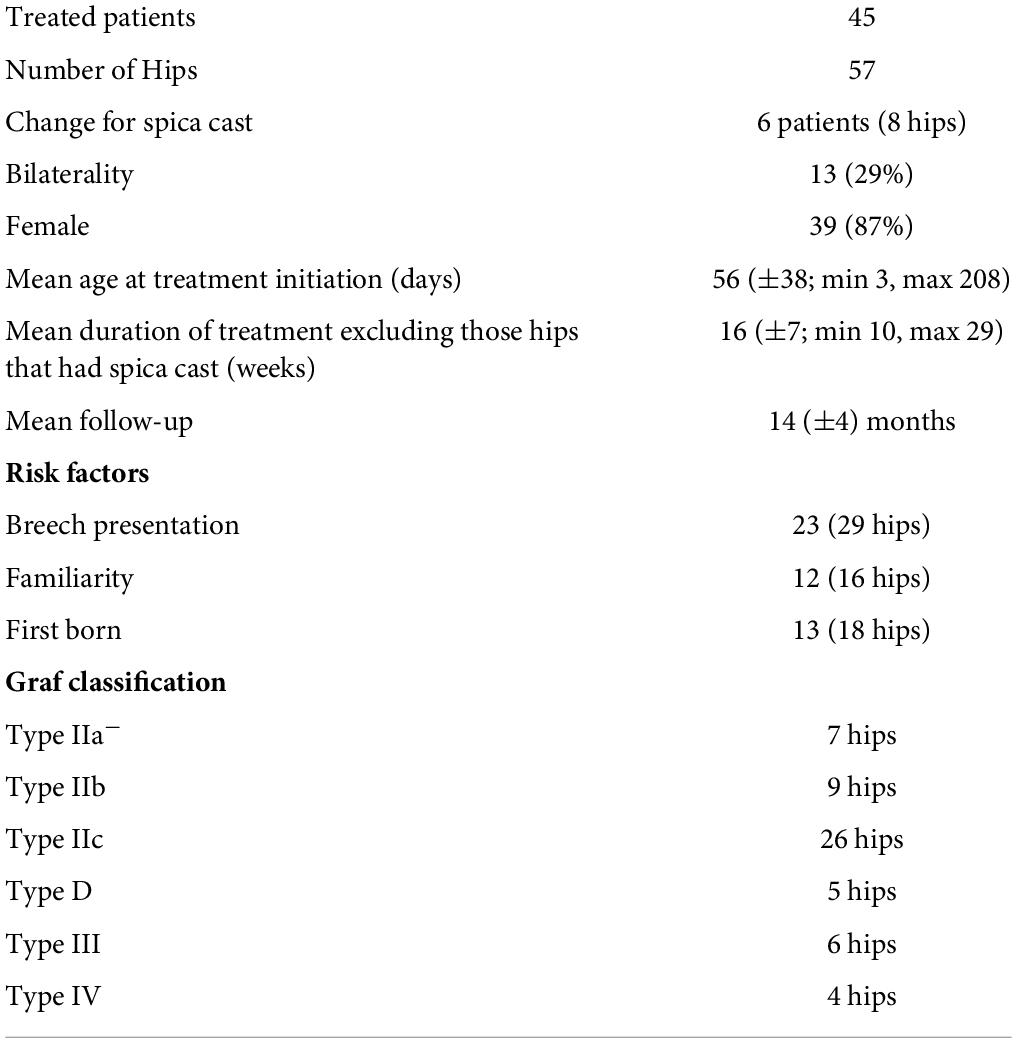
Methods: Epidemiological data and ultrasonographic data of all infants diagnosed with DDH and initially treated with a Tübingen splint at our institution between May 2017 and February 2020 were assessed retrospectively. We divided the population into stable and unstable hips using the Graf classification. Age at treatment initiation, duration of treatment, complications, and radiological outcome between 12 and 24 months were investigated.
Results: We included a total of 45 patients (57 hips) affected by DDH treated with the Tübingen splint. Treatment has been successful in 93% of stable hips and only 40% of unstable hips. Radiological outcome at 1-year follow-up significantly correlated with initial Graf classification (p < 0.001).
Conclusion: The Tübingen splint is a safe and effective treatment for stable hips, nevertheless, for unstable hips, closed reduction, and spica cast remains the gold standard.
Introduction
Developmental dysplasia of the hip (DDH) is defined as insufficient acetabular coverage of the femoral head and can range from mild dysplasia to total dislocation of the joint (1, 2). Incidence of DDH ranges between 1 and 20 per 1,000 infants per year depending on the literature and region (3). Ultrasonography according to Graf is the method of choice for diagnosis within the first months of life (4, 5). The Graf method allows us to classify DDH according to its severity into ultrasound stable (hip types I–IIc) and unstable hips (hip type D to IV) (6) (Table 1). As type IIc hip can be stable or unstable, stress examination needs to be carried out to confirm a stable or unstable joint.
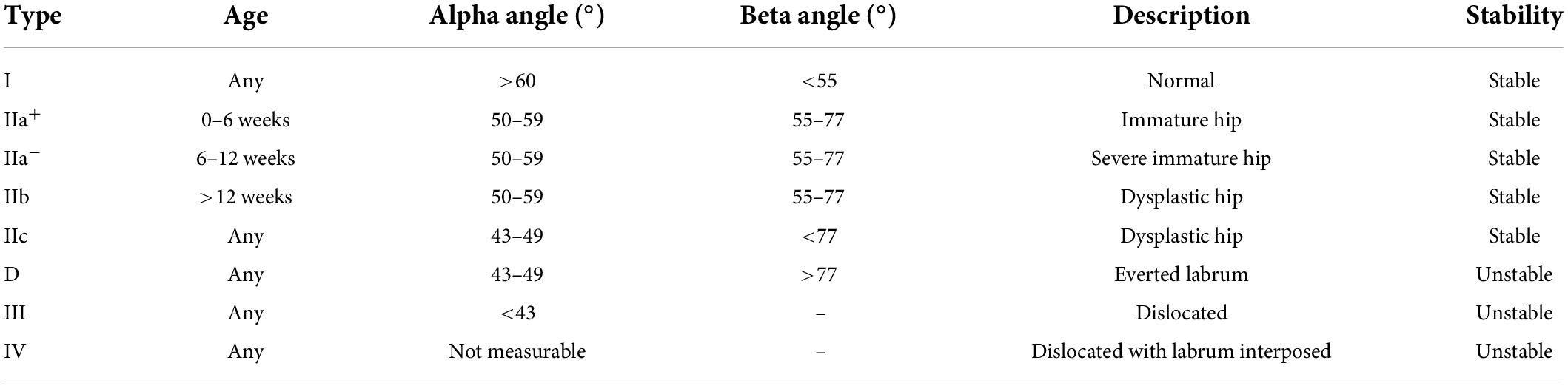
Table 1. The Graf classification system of developmental dysplasia of the hip (19).
If untreated, 20–25% of patients are at risk to developing secondary osteoarthritis and may require total hip replacement early in life (7, 8). Therefore, early diagnosis and treatment are fundamental to preventing disability later in life (4, 9, 10).
The treatment aims to achieve a concentric reposition, retention, and maturation of the hip (6, 11). In patients with an early diagnosis within the first 6 months of life, treatment is essentially functional and involves the use of dynamic harnesses and orthoses (12, 13). All of them are made to keep the hip in flexion and abduction to reduce the hip and promote hip maturation (14, 15).
The Tübingen splint, derived from the widely used Pavlik harness, is a rigid splint that maintains the flexion–position of the hip while limiting its abduction (16) (Figure 1).
Indicated harness positioning consists of 90°–110° of flexion and 45°–60° of abduction of both hips. This position is known as the safe zone to prevent tension on the capsular blood vessels and prevent avascular femoral head necrosis (AVN) (17). Initially, the device was conceived to treat DDH of types IIb and IIc designed as stable hips according to the Graf classification (Table 1) (18, 19). Later on, its use was also expanded to unstable DDH of grade D to grade IV with variable outcomes (19–22). The indication and treatment success have been confirmed by many authors for stable DDH, but there are still controversies in the literature regarding the treatment of unstable DDH with the Tübingen splint (23, 24). Some authors even recommend closed reduction and spica cast as the gold standard for unstable DDH (25).
Indeed, we believe that care should be taken when treating unstable DDH with the Tübingen splint. The aim of our study was to compare the outcome of stable and unstable DDH treated with the Tübingen splint in children aged 0–6 months.
Materials and methods
After approval by the Ethics Review Committee (ID Number 2019-01761), we performed a monocentric retrospective study. We included all patients aged between 0 and 6 months treated for primary DDH with a Tübingen splint at our tertiary pediatric orthopedic center between May 2017 and February 2020.
All patients had ultrasonographic evaluation according to the Graf method and underwent dynamic clinical evaluation by applying the Barlow and Ortolani tests for initial diagnosis (19). All the ultrasounds were done by our pediatric radiologist.
Inclusion criteria were all children aged between 0 and 6 months at the moment of diagnosis, who had no other treatment before the Tübingen splint and who underwent a pelvic x-ray around 12 months of age.
Developmental dysplasia of the hip in association with neurodevelopmental disorders and patients treated with another device before the introduction of the Tübingen splint were excluded.
The treatment indication was based on the International Interdisciplinary Consensus Meeting on the Evaluation of Developmental Dysplasia of the Hip (5).
Patients with stable DDH of grades IIa, IIb, and IIc were required the splint at least 22 h a day. Remove of the splint was allowed for bath and diaper changing. Hip ultrasonography according to the Graf method was repeated every 6 weeks until normalization of the alpha angle.
Patients of parents with unstable DDH of grades D, III, and IV were trained to use the Tübingen splint continuously 24/24 h a day, with close ultrasonographic and clinical follow-up every 2–3 weeks. The treatment was then continued as mentioned above if the ultrasound showed improvement of DDH. Conversely, in the case of worsening of the alpha angle seen on ultrasound, we proceeded to a closed reduction and application of a spica cast under general anesthesia. Hip arthrography was done at the same time.
Patients in both groups underwent radiological follow-up by a plain pelvic x-ray between 12 and 24 months of age. The radiographies were done in a supine position with extended legs.
To compare the outcomes of both groups, we recorded the following parameters: (1) the degree of DDH according to the Graf classification at initial diagnosis, (2) age at treatment initiation, (3) duration of treatment, and (4) acetabular index measured on pelvic x-ray performed at the latest follow-up between 12 and 24 months of age.
Complications, especially avascular necrosis, were also recorded. The presence of AVN was determined based on the Kalamchi and McEwan classification (26). Risk factors have been recorded for general interest.
Successful treatment by the Tübingen splint was defined as a normal acetabular index measured on pelvic x-ray at last follow-up for hips treated only by the Tübingen splint. Acetabular index values were based on the normal percentile reference curves according to Novais et al. (27).
Unstable hips requiring closed reduction due to worsening of DDH seen on follow-up ultrasound after placement of the Tübingen splint were considered as failure, as well as those hips treated with the Tübingen splint alone showing residual hip dysplasia at last follow-up.
Statistical analysis
We performed a descriptive statistical analysis to compare stable (grades IIa–IIc) and unstable hips (grades D–IV) using the Chi-Square test and Student’s t-test.
The Student’s t-test has been used to highlight the difference in treatment initiation timing between the two groups (stable vs. unstable hips). The Chi square test has been used to highlight the differences in treatment success.
Data were reported as a mean with SD.
Results
A total of 45 patients (57 hips) met our inclusion criteria. Of them 39 (87%) patients were girls. The left hip was affected in 37 cases (65%). Hips were bilaterally abnormal in 13 patients (12 girls and one boy).
Looking at patients’ demographics, 42 hips (74%) presented stable DDH of grades IIa–IIc and 15 hips (26%) presented unstable DDH of grades D–IV according to the Graf classification.
Treatment was started on average at 56 (SD ± 38) days of life. The earliest time of diagnosis was at 3 days of age and the latest at 208 days (6 months). When regarding the time at the initiation of treatment, we observed a significant difference (p < 0.003) between stable and unstable hips with an average age at the start of treatment before 6 weeks of life in only 15% (7 hips) of stable hips and in 66% (10 hips) of unstable hips. Treatment initiation after the third month of life was seen in a total of 14 hips out of 57 (25%) with 13 stable hips and only one unstable hip (p < 0.0001).
The overall average duration of treatment with the Tübingen splint, when excluding those hips that required a treatment modification by closed reduction and spica cast under general anesthesia, was 16 weeks (SD ± 7). The mean age at the last follow-up was 14 months (SD ± 4). The mean duration of follow-up was 16 months (SD ± 5).
The demographics and characteristics of our study population can be found in Table 2.
Overall treatment success was seen in 45 hips (79%) including 39 stable hips and 6 unstable or dislocated hips.
Treatment failure occurred in 12 hips (21%) including 9 unstable hips. A total of 8 hips (4 hips type D, 2 hips type III, and 2 hips type IV) underwent a closed reduction and application of a spica cast because of worsening of DDH seen on ultrasound 2–3 weeks after treatment initiation by the Tübingen splint. The 4 other hips (1 hip type IIb, 2 hips type IIc, and 1 hip type IV) treated by the Tübingen splint alone presented residual hip dysplasia at the latest follow-up. For all the 3 stable hips presenting residual hip dysplasia, initiation of treatment occurred after 3 months of life.
The mean acetabular index in these 4 cases was 30° (min 29, max 31). There was a significant difference in an acetabular index comparing hips with a successful treatment (23° ± 4) and hips presenting residual hip dysplasia (30° ± 1; p-value 0.000006). No significant difference was found concerning the age at treatment initiation. However, we observed a statistically significant difference in the duration of treatment when comparing those hips with residual hip dysplasia (13 weeks ± 1) to those hips with normal values on the latest follow-up x-ray (16 weeks ± 7; p-value 0.006).
Looking at the groups of stable and unstable hips separately, the success rate was 93% (39 hips out of 42) and 40% (6 hips out of 15), respectively. Statistical analysis confirmed a significant difference (p < 0.001) in treatment success when comparing stable and unstable DDHs (Table 3).
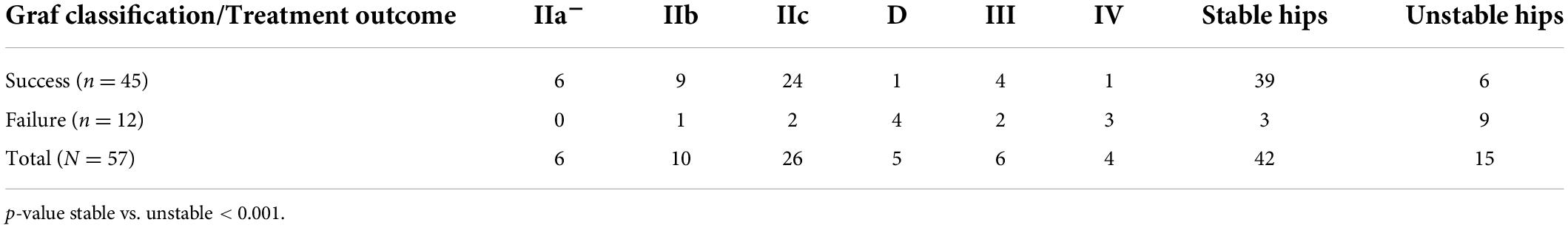
Table 3. Treatment success and failures according to severity of DDH according to Graf classification (19).
Complications were reported in 3 (5%) cases. One femoral nerve palsy (type IIc hip) occurred 5 days after treatment initiation and recovered 4 days after splint removal. The treatment could then be pursued with our standard protocol without further nerve palsy. We observed two partial femoral avascular head necrosis of type I according to the classification of Kalamchi and Mc Ewan on the pelvic x-ray at the last follow-up. Both patients presented with unstable DDH of grade D and grade III, respectively.
Regarding the 8 hips (6 patients) that underwent a treatment adaptation with closed reduction and spica cast, 2 hips needed an open reduction because of failure of treatment and irreducible hip; one hip presented residual hip dysplasia and 5 hips had normal acetabular indexes at the latest follow-up.
No statistical difference was found concerning the age at the beginning of treatment when compared to those hips treated solely by the Tübingen splint.
Discussion
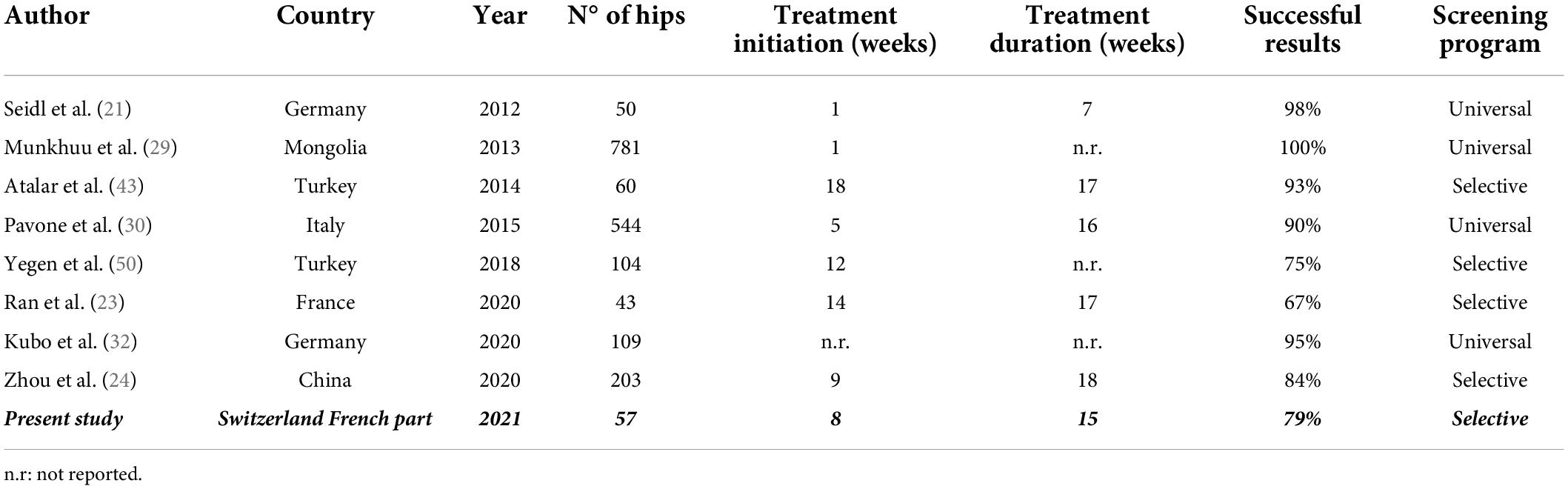
The overall treatment success rate with the Tübingen splint in our cohort was 79%. Stable and unstable DDH have a significant difference with a success rate of 93% and 40%, respectively, which is like previously published data in the literature (22, 24).
This significant difference in treatment success between stable and unstable hips has already been described by other authors. Ran et al. compared the Tübingen splint to the widely used Pavlik Harness. Successful treatment for unstable hips treated with the Tübingen splint was significantly lower than for the Pavlik Harness, especially in bilateral dislocation or in severe cases of hip dislocation as grade IV hips according to the Graf classification. Of the 43 hips treated with the Tübingen splint in their cohort, 14 hips (33%) had a poor outcome. Of them, 11 hips (79%) presented DDH of grade IV. The overall success rate was 67%, which is comparable to our results (23).
Other authors reported even failure rates as high as 78.6% for hips Graf grade IV in patients treated by a hip abduction flexion splint (28).
Our results support the treatment by closed reduction and spica casting as the gold standard for unstable hips, as already confirmed by other authors (25).
Other authors demonstrate higher success rates (29–32). Table 4 summarizes the data found in the literature.
These differences may be due to different factors; first, we could observe a different distribution of patients in some studies as seen in the cohorts from Pavone et al. and Seidl et al. They reported a 2.2% and a 2% rate of unstable hips, respectively, whereas the frequency of unstable hips was 17% in our series (30, 31).
Second, the lack of a universal screening program and the later referral of patients to our center with later treatment initiation is known as a negative predicting factor (33).
Indeed, overall initial treatment was established for an average of 56 days, which corresponds to 8 weeks of life. This is, compared to other authors, quite belated (29–31), especially if we admit that the highest post-maturation of the acetabulum after birth takes place in the first 16 weeks after birth (34).
Furthermore, failures in stable hips in our cohort concerned those patients in whom treatment was started after 3 months of life. This confirms that the earlier the treatment, the higher the success rates of treatment (29, 34, 35).
The significant difference between the start of treatment comparing stable and unstable hips in our study can be explained by the fact that stable hips are often detected late due to the absence of instability on clinical examination and therefore screening ultrasound of the hip is done later in life. This is even more evident when we look at the 14 hips in our study with treatment initiation after 3 months of life. Indeed, out of the 14 hips, which represents 25% of the hips in our series, only one hip was an unstable hip. These findings support that hip ultrasound is the only way to detect DDH, especially stable ones, with certainty (29).
It is one of the reasons why the international interdisciplinary consensus meeting on the evaluation of DDH in 2018 as well as many other authors support a universal screening program for DDH (5, 11, 36–39).
However, numerous recent studies and meta-analyses have not demonstrated the utility of universal screening in diminishing the incidence of late dysplasia (40, 41). Furthermore, Laborie et al. concluded that universal screening favors overtreatment (but not an increased rate of complications) while no significant reduction of late dysplasia was observed in comparison with selective screening (42).
We had to change the treatment in 14% (8 hips) of cases. All of them presented unstable hips according to Graf’s classification. This is in line with the results of other authors (43).
The average treatment time in our cohort was 3 months as already described in the literature (17, 30, 43).
Because the alpha angle shows a maturation of about one degree per week and the interobserver measurement error for the alpha angle at ultrasound is about 4–5 degrees, we repeated the ultrasound every 6 weeks until normalization of the alpha angle for stable hips (34, 44, 45). Regarding the unstable hips, it seemed important to us to carry out a close follow-up in order not to miss any worsening of the dysplasia which was an indication for a closed reduction and spica cast, a treatment considered as the gold standard by some authors (25).
The most frequent complication in our study was AVN of the femoral head in 5% (2 hips), which varies from 0 to 28% according to studies reported in the literature (46). However, our data may be an underestimation of the real number of AVNs given our short follow-up time of an average of 14 months.
Looking at the demographics of our study population, 87% of patients were girls. The latest epidemiological data reported that DDH is two to three times more common in females than in male infants (47, 48). A total of 77% of patients presented a positive family history or breech position. Both are known to be risk factors for DDH with a relative risk for the breech presentation of 3.8 (95% CI 2.3–6.2) and 1.39 (95% CI 1.23–1.57) for positive family history (48, 49). Nevertheless, there was no correlation between a specific risk factor and the observed failure rate.
The lack of information on whether parents removed the splint more than allowed by the caregivers, can be considered as a weak point of our study, as parental non-compliance seems to be one of the main reasons for the failure of the treatment (17).
The author also recognizes the small sample size of unstable hips (only 15 out of 57 hips) as a major limitation of the present analysis.
The strength of our study is that we were able to highlight the limitations of treatment with the Tübingen splint for unstable hips. The study supports the treatment by closed reduction and spica cast as the gold standard for unstable hips and the importance of close monitoring of unstable hips if treated with the Tübingen splint in order to be able to quickly change the treatment in the event of non-improvement.
Conclusion
Our study confirms that the Tübingen splint is a safe and effective treatment for stable hips. For unstable hips in which treatment with a Tübingen splint is initiated, very close monitoring is mandatory in order to adapt the treatment in the event of poor evolution. The treatment of choice will then be closed reduction and spica cast.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by Commission Éthique du Canton de Vaud, Switzerland. Written informed consent to participate in this study was provided by the participants’ legal guardian/next of kin. Written informed consent was obtained from the individuals’ legal guardian/next of kin for the publication of any identifiable images or data included in this article.
Author contributions
EC, C-AS, and SM: data curation. C-AS and SM: formal analysis. SM: methodology and supervision. P-YZ: project administration. ES: validation. EC: writing—original draft. ES, P-YZ, and SM: writing—review and editing. All authors contributed to the article and approved the submitted version.
Funding
Open access funding provided by University of Lausanne.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Herring J. Developmental dysplasia of the hip. 4th ed. In: JA Herring editor. Tachdijan’s Pediatric Orthopaedics. Philadelphia, PA: WB Saunders (2008).
2. Seringe R, Bonnet JC, Katti E. [Pathogeny and natural history of congenital dislocation of the hip]. Rev Chir Orthop Reparatrice Appar Mot. (1990) 76:391–402.
3. Pollet V, Percy V, Prior HJ. Relative risk and incidence for developmental dysplasia of the hip. J Pediatr. (2017) 181:202–7.
5. O’Beirne JG, Chlapoutakis K, Alshryda S, Aydingoz U, Baumann T, Casini C, et al. International interdisciplinary consensus meeting on the evaluation of developmental dysplasia of the hip. Ultraschall Med. (2019) 40:454–64. doi: 10.1055/a-0924-5491
6. Ddh RG. Diagnosis and Treatment Strategies. In: G Bentley editor. European Instructional Lectures European Federation of National Associations of Orthopaedics and Traumatology. (Vol. 9), Berlin: Springer (2009).
7. Jacobsen S, Sonne-Holm S. Hip dysplasia: a significant risk factor for the development of hip osteoarthritis. A cross-sectional survey. Rheumatology. (2005) 44:211–8.
8. Gala L, Clohisy JC, Beaule PE. Hip dysplasia in the young adult. J Bone Joint Surg Am. (2016) 98:63–73.
9. Omeroglu H, Kose N, Akceylan A. Success of pavlik harness treatment decreases in patients >/= 4 months and in ultrasonographically dislocated hips in developmental dysplasia of the hip. Clin Orthop Relat Res. (2016) 474:1146–52. doi: 10.1007/s11999-015-4388-5
10. Tschauner C, Furntrath F, Saba Y, Berghold A, Radl R. Developmental dysplasia of the hip: impact of sonographic newborn hip screening on the outcome of early treated decentered hip joints-a single center retrospective comparative cohort study based on Graf’s method of hip ultrasonography. J Child Orthop. (2011) 5:415–24. doi: 10.1007/s11832-011-0366-y
11. Agostiniani R, Atti G, Bonforte S, Casini C, Cirillo M, De Pellegrin M, et al. Recommendations for early diagnosis of developmental dysplasia of the hip (DDH): working group intersociety consensus document. Ital J Pediatr. (2020) 46:150. doi: 10.1186/s13052-020-00908-2
12. Wilkinson AG, Sherlock DA, Murray GD. The efficacy of the pavlik harness, the Craig splint and the von Rosen splint in the management of neonatal dysplasia of the hip. J Bone Joint Surg Ser B. (2002) 84:716–9.
13. Wahlen R, Zambelli PY. Treatment of the developmental dysplasia of the hip with an abduction brace in children up to 6 months old. Adv Orthop. (2015) 2015:103580.
14. Pavone V, de Cristo C, Vescio A, Lucenti L, Sapienza M, Sessa G, et al. Dynamic and static splinting for treatment of developmental dysplasia of the hip: a systematic review. Children. (2021) 8:104.
15. Merchant R, Singh A, Dala-Ali B, Sanghrajka AP, Eastwood DM. Principles of bracing in the early management of developmental dysplasia of the hip. Indian J Orthop. (2021) 55:1417–27. doi: 10.1007/s43465-021-00525-z
16. Bernau A. [The Tubingen hip flexion splint in the treatment of hip dysplasia]. Z Orthop Ihre Grenzgeb. (1990) 128:432–5.
17. Ramsey PL, Lasser S, MacEwen GD. Congenital dislocation of the hip. Use of the Pavlik harness in the child during the first six months of life. J Bone Joint Surg Am. (1976) 58:1000–4.
18. Graf R. Hip sonography: background; technique and common mistakes; results; debate and politics; challenges. Hip Int. (2017) 27:215–9. doi: 10.5301/hipint.5000514
19. Graf R. The use of ultrasonography in developmental dysplasia of the hip. Acta Orthop Traumatol Turc. (2007) 41(Suppl. 1):6–13.
20. Kubo H, Pilge H, Weimann-Stahlschmidt K, Stefanovska K, Westhoff B, Krauspe R. Use of the Tubingen splint for the initial management of severely dysplastic and unstable hips in newborns with DDH: an alternative to Fettweis plaster and Pavlik harness. Arch Orthop Trauma Surg. (2018) 138:149–53. doi: 10.1007/s00402-017-2827-3
21. Seidl T, Lohmaier J, Holker T, Funk J, Placzek R, Trouillier HH. [Reduction of unstable and dislocated hips applying the Tubingen hip flexion splint?]. Orthopade. (2012) 41:195–9. doi: 10.1007/s00132-011-1873-8
22. Yegen M, Atalar H, Gunay C, Yavuz O, Uras I. Reduction of the dislocated hips with the Tübingen hip flexion splint in infants. Int Orthop. (2019) 43: 2099–103.
23. Ran L, Chen H, Pan Y, Lin Q, Canavese F, Chen S. Comparison between the Pavlik harness and the Tubingen hip flexion splint for the early treatment of developmental dysplasia of the hip. J Pediatr Orthop B. (2020) 29:424–30.
24. Zhou Y, Li R, Li C, Zhou P, Li Y, Ke Y, et al. Tübingen hip flexion splints for developmental dysplasia of the hip in infants aged 0–6 months. BMC Pediatr. (2020) 20:280. doi: 10.1186/s12887-020-02171-0
25. Walter SG, Bornemann R, Koob S, Ossendorff R, Placzek R. Closed reduction as therapeutic gold standard for treatment of congenital hip dislocation. Z Orthop Unfall. (2020) 158:475–80.
26. Kalamchi A, MacEwen GD. Avascular necrosis following treatment of congenital dislocation of the hip. J Bone Joint Surg Am Volume. (1980) 62: 876–88.
27. Novais EN, Pan Z, Autruong PT, Meyers ML, Chang FM. Normal percentile reference curves and correlation of acetabular index and acetabular depth ratio in children. J Pediatr Orthop. (2016). 38:163–69. doi: 10.1097/BPO.0000000000000791
28. Palocaren T, Rogers K, Haumont T, Grissom L, Thacker MM. High failure rate of the Pavlik harness in dislocated hips: is it bilaterality? J Pediatr Orthop. (2013) 33:530–5. doi: 10.1097/BPO.0b013e318287ffc6
29. Munkhuu B, Essig S, Renchinnyam E, Schmid R, Wilhelm C, Bohlius J, et al. Incidence and treatment of developmental hip dysplasia in Mongolia: a prospective cohort study. PLoS One. (2013) 8:e79427. doi: 10.1371/journal.pone.0079427
30. Pavone V, Testa G, Riccioli M, Evola FR, Avondo S, Sessa G. Treatment of developmental dysplasia of hip with Tubingen hip flexion splint. J Pediatr Orthop. (2015) 35:485–9.
31. Seidl T, Lohmaier J, Hölker T, Funk J, Placzek R. Reduction of unstable and dislocated hips applying the Tübingen hip flexion splint? Orthopade. (2012) 41:195–9. doi: 10.1007/s00132-011-1873-8
32. Kubo H, Oezel L, Latz D, Hufeland M, Schiffner E, Pilge H, et al. Treatment of unstable hips with the Tubingen splint in early postnatal period: radiological mid-term results of 75 hips with mean follow-up of 5.5 years. J Child Orthop. (2020) 14:252–8. doi: 10.1302/1863-2548.14.200074
33. Bialik V. [Pavlik’s method in developmental dysplasia of the hip]. Acta Orthop Traumatol Turc. (2007) 41(Suppl. 1):19–24.
34. Graf RTC, Steindl M. Nachuntersuchungsergebnisse und Verlauf des Sogenannten Physiologisch Unreifen Hüftgelenkes (Typ Ila, nachGraf). Die Sonographie in der Orthopaedie. Wien: Springer Verlag (1988).
35. Pavone V, Testa G, Evola FR, Riccioli M, Avondo S, Sessa G. Timing in conservative management of developmental dysplasia of the hip. Hip Int. (2013) 23:598.
36. Biedermann R, Eastwood DM. Universal or selective ultrasound screening for developmental dysplasia of the hip? A discussion of the key issues. J Child Orthop. (2018) 12:296–301.
37. Thaler M, Biedermann R, Lair J, Krismer M, Landauer F. Cost-effectiveness of universal ultrasound screening compared with clinical examination alone in the diagnosis and treatment of neonatal hip dysplasia in Austria. J Bone Joint Surg Br. (2011) 93:1126–30. doi: 10.1302/0301-620X.93B8.25935
38. Biedermann R, Riccabona J, Giesinger JM, Brunner A, Liebensteiner M, Wansch J, et al. Results of universal ultrasound screening for developmental dysplasia of the hip: a prospective follow-up of 28 092 consecutive infants. Bone Joint J. (2018) 100-B:1399–404. doi: 10.1302/0301-620X.100B10.BJJ-2017-1539.R2
39. Sink EL, Ricciardi BF, Torre KD, Price CT. Selective ultrasound screening is inadequate to identify patients who present with symptomatic adult acetabular dysplasia. J Child Orthop. (2014) 8:451–5. doi: 10.1007/s11832-014-0620-1
40. Mulpuri K, Song KM, Goldberg MJ, Sevarino K. Detection and nonoperative management of pediatric developmental dysplasia of the hip in infants up to six months of age. J Am Acad Orthop Surg. (2015) 23:202–5.
41. Shorter D, Hong T, Osborn DA. Cochrane review: screening programmes for developmental dysplasia of the hip in newborn infants. Evid Based Child Health Cochr Rev J. (2013) 8:11–54.
42. Laborie LB, Markestad TJ, Davidsen H, Bruras KR, Aukland SM, Bjorlykke JA, et al. Selective ultrasound screening for developmental hip dysplasia: effect on management and late detected cases. A prospective survey during 1991-2006. Pediatr Radiol. (2014) 44:410–24. doi: 10.1007/s00247-013-2838-3
43. Atalar H, Gunay C, Komurcu M. Functional treatment of developmental hip dysplasia with the Tubingen hip flexion splint. Hip Int. (2014) 24:295–301.
44. Omeroglu H, Bicimoglu A, Koparal S, Seber S. Assessment of variations in the measurement of hip ultrasonography by the Graf method in developmental dysplasia of the hip. J Pediatr Orthop B. (2001) 10:89–95.
45. Omeroglu H. Use of ultrasonography in developmental dysplasia of the hip. J Child Orthop. (2014) 8:105–13.
46. Gulati V, Eseonu K, Sayani J, Ismail N, Uzoigwe C, Choudhury MZ, et al. Developmental dysplasia of the hip in the newborn: a systematic review. World J Orthop. (2013) 4:32–41.
47. Vafaee AR, Baghdadi T, Baghdadi A, Jamnani RK. DDH Epidemiology revisited: do we need new strategies? Arch Bone Jt Surg. (2017) 5:440–2.
48. Ortiz-Neira CL, Paolucci EO, Donnon T. A meta-analysis of common risk factors associated with the diagnosis of developmental dysplasia of the hip in newborns. Eur J Radiol. (2012) 81:e344–51.
49. Ran L, Chen H, Pan Y, Lin Q. Comparison between the Pavlik harness and the Tübingen hip flexion splint for the early treatment of developmental dysplasia of the hip. J Pediatr. (2020) 29:424–30. doi: 10.1097/BPB.0000000000000667
Keywords: DDH, Graf method, spica cast, closed reduction, Tübingen splint, hip ultrasound
Citation: Chaibi E, Saugy C-A, Samara E, Zambelli P-Y and Merckaert SR (2022) Comparison of treatment outcomes of stable and unstable developmental dysplasia of the hip with the Tübingen splint. Front. Pediatr. 10:976367. doi: 10.3389/fped.2022.976367
Received: 23 June 2022; Accepted: 19 July 2022;
Published: 25 August 2022.
Edited by:
Stefan Essig, University of Lucerne, SwitzerlandReviewed by:
Andrea Vescio, Azienda Ospedaliera Pugliese Ciaccio, ItalyVito Pavone, University of Catania, Italy
Copyright © 2022 Chaibi, Saugy, Samara, Zambelli and Merckaert. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Sophie Rosa Merckaert, U29waGllLm1lcmNrYWVydEBjaHV2LmNo
 Emmelie Chaibi
Emmelie Chaibi Eleftheria Samara
Eleftheria Samara Pierre-Yves Zambelli
Pierre-Yves Zambelli Sophie Rosa Merckaert
Sophie Rosa Merckaert