
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
BRIEF RESEARCH REPORT article
Front. Pediatr. , 26 October 2022
Sec. Pediatric Pulmonology
Volume 10 - 2022 | https://doi.org/10.3389/fped.2022.966372
Background: The current United States asthma management guidelines recommend usage of the Air Quality Index (AQI) for outdoor activity modification when air pollution is high. Little is known about parental knowledge and usage of air quality including the AQI in managing childhood asthma.
Methods: Forty parents (or legal guardians) of children with persistent asthma completed a questionnaire designed to assess 4 areas related to outdoor air pollution: awareness, perception, behavioral modification, and prior healthcare provider discussion. Descriptive statistics were obtained and Fisher's exact test was used for analysis of behavioral change by selected variables.
Results: Almost all parents reported awareness of air quality alerts or AQI, however, only 20% checked the AQI on the AirNow app or website. Most parents reported air pollution as a trigger (65%), yet few parents reported behavioral modification of their child's outdoor activity based on the perception of poor air quality (43%) or based on AQI or alerts (40%). Over half of parents reported a healthcare provider had ever discussed air pollution as a trigger, with few parents (23%) reporting recommendations for behavior change. Perception of air pollution as a trigger, healthcare provider discussion and recommendations, and usage of AirNow were associated with increased reported activity change.
Conclusion: Healthcare providers should discuss outdoor air pollution during asthma management in children and should discuss AirNow as a source for AQI information and behavioral recommendations.
Outdoor air pollution is a well-known cause of childhood asthma exacerbations (1). Current United States (US) asthma management guidelines (2) and the American Academy of Pediatrics (3) advise usage of the Air Quality Index (AQI) to reduce outdoor air pollution exposure. While recommending usage of the AQI is prudent, little is known about the usage or efficacy of personal exposure avoidance strategies, and health outcomes (4). Further, there is little data to guide parents and children with asthma on how the AQI should be used. For example, the AQI as a tool for behavioral change can be utilized in two ways: by responding to AQI alerts which are generally issued for days forecast to have air pollution above the National Ambient Air Quality Standard (NAAQS) or by checking the AQI prior to outdoor activity on the AirNow website or app as a way to learn individual susceptibility to air pollution. Despite national recommendations, it remains largely unknown if parents of children with asthma are aware of outdoor air pollution risks or the AQI, whether and how they incorporate air pollution avoidance strategies in their child's asthma management, or whether they discuss such strategies with health care professionals (5).
To date there has been one prior publication examining parents of children with asthma knowledge and response to air quality alerts (6). To our knowledge, no study has evaluated parental knowledge and usage of the AirNow app. Our objective was to characterize parental knowledge and usage of the AQI in their child's asthma management in a convenience sample of 40 parents.
An 11-item questionnaire was developed to assess parental air quality knowledge, perceptions, behavioral change, and discussion with health professionals including adapting questions used in the National Health and Nutritional Examination Survey (NHANES) (7), Behavioral Risk Factors Surveillance Survey (8), and prior AQI publications (9) (Supplementary Materials Table S1). We evaluated parental reported change in two ways: based on perception of poor air quality, which may differ from true air quality (10, 11), and based on the AQI or alerts. Parents or legal guardians (collectively referred to as “parents”) of children aged 8–17 years with physician diagnosed persistent asthma were eligible to receive the questionnaire. Parents were eligible to participate if their child was participating in a separate study (NCT: 04454125), which recruited children from a pediatric pulmonology clinic and asthma registry during July- October 2020. For the separate study, the older ages of children were selected for the ability to check the AQI and self-regulate activity. All eligible parents participated. The questionnaire was administered to the parents after written informed consent was obtained. The study was approved by the University of Pittsburgh Institutional Review Board.
Descriptive statistics were obtained for select parental and child demographics and for questionnaire data. Race and sex of both parent and child were self-reported. Questionnaire response choices of “Don”t Know/ Not Sure” and “Never thought about it” were coded as negative (9, 12). Fisher's exact test was used for comparison between groups. All analyses were conducted using SAS v 9.4 (SAS Institute Inc). Two-sided P values less than .05 were considered statistically significant.
Table 1 displays characteristics of the 40 enrolled parents: most (85%) were female and identified as mothers (78%), sixty percent self-identified as White, 38% as Black, and 63% had graduated from college or had post-graduate education. Half were married and slightly over half reported economic perception of poor, almost poor, or living check-to-check. The average age of their child was 12.5 years (± 2.7yrs) and half were female.
Table 2 displays parental responses by category: awareness, perception, behavior change, and discussion with healthcare providers. Almost all parents reported awareness of the AQI or alerts, with only 2 (5%) reporting no knowledge. Despite such awareness, only one-fifth of parents reported checking the AQI by the government-sponsored AirNow app or website. Two-thirds of parents reported outdoor air pollution as a trigger for their child's asthma, but less than one-quarter reported air pollution caused an illness or symptom in the prior year. Most parents reported they did not alter their child's outdoor activity in the last year based on perceived air quality (58%), or on the AQI or alerts (60%). Half of all parents did not instruct their child to avoid busy roads when walking, biking, or exercising to reduce exposure to air pollution, or practice these avoidance behaviors themselves. Slightly over half of parents reported ever discussing outdoor air pollution as a possible trigger for their child's asthma with healthcare providers, with only 23% of parents reporting healthcare provider instruction to reduce or change their child's activity in response to poor air quality. Most parents wanted such discussion with healthcare providers.
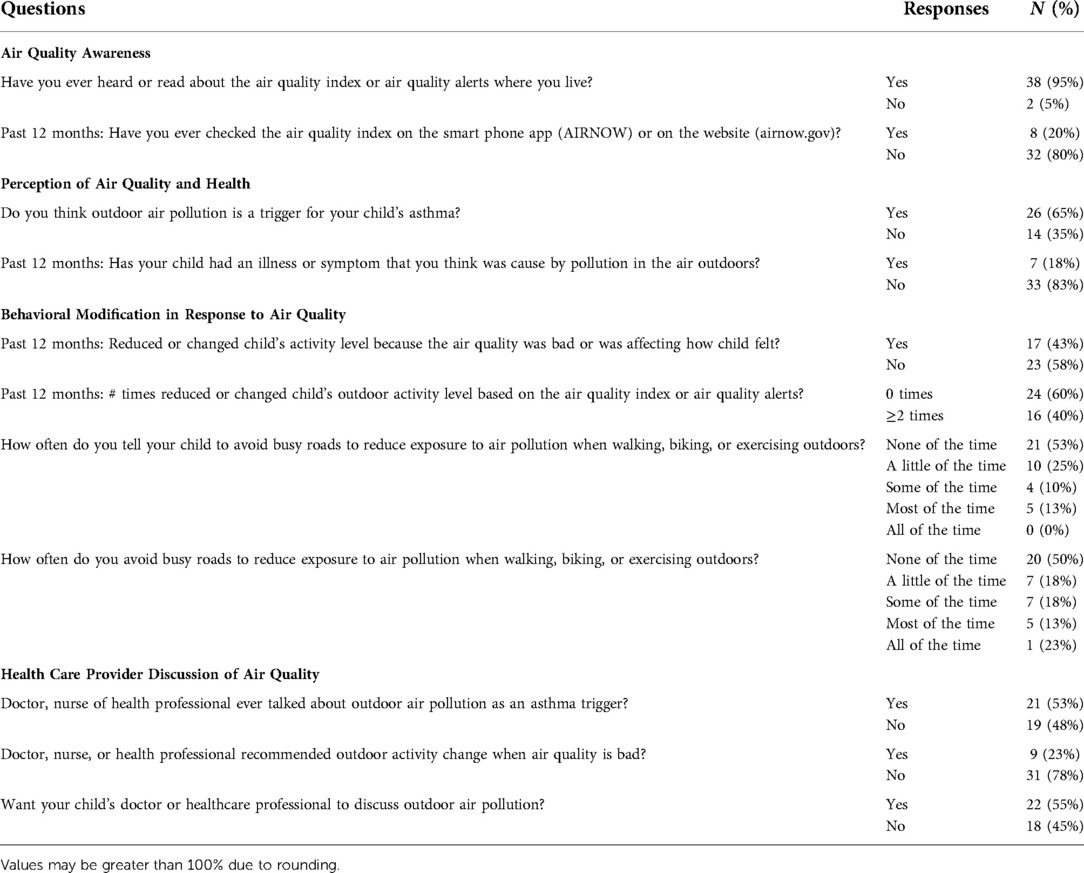
Table 2. Parental knowledge and usage of the Air Quality Index (AQI) in parents of children with persistent asthma.
Table 3 shows the results of the analysis of parental behavior change by selected variables. Parents who changed their child's behavior due to perceived air quality (i.e., thought air quality was bad or affecting their child), were more likely to perceive air pollution as an asthma trigger (88%) and report discussion of air pollution as a possible trigger with a healthcare provider (76%). For parents who did not change behavior based on perception of poor air quality, most did not endorse air pollution as an asthma trigger (52%), cause of illness or symptom in the prior 12 months (96%), report discussion with healthcare provider (65%) including recommendation for behavior change in response to poor air quality (91%), or usage of the AQI via AirNow (96%).
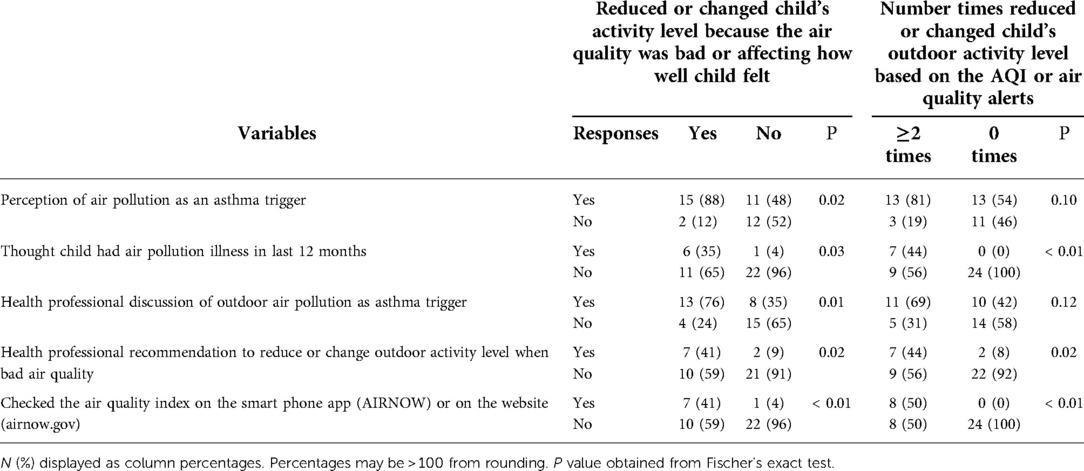
Table 3. Analysis of select variables and reported outdoor activity modifications based on air quality in children with persistent asthma.
Parents endorsing at least one behavioral change based on AQI or air quality alerts were more likely to perceive air pollution as an asthma trigger (81%) and report healthcare provider discussion of air pollution as a trigger (69%), though this was not statistically significant. Half of all parents who endorsed at least one behavioral change reported checking the AQI on AirNow. Of the parents who reported no behavior change in the last 12 months based on the AQI or air quality alerts, none of the parents thought air pollution caused an illness or symptom, most did not have healthcare provider discussions (58%) or recommendations for behavioral change (92%), and no parent reported checking the AQI on AirNow smartphone app or website. All parents who checked the AirNow app or website reported at least one behavioral change based on AQI or alert in the prior year (p < 0.01).
Behavioral changes in response to perceived air quality or based on alerts/AQI did not differ by parental or child sex, age, race, nor by parental education, economic perception, or marital status (Supplementary Materials Table S2).
Our study focuses on parental awareness of the AQI and usage of such in their child's asthma management, one of only two such studies in the US (6) and the first study to assess usage of AirNow as a source of AQI information. Awareness of the AQI or air quality alerts was nearly universal among parents of children with persistent asthma, however relatively few parents endorsed behavioral modification to reduce air pollution exposure.
Our findings are consistent with McDermott et al., who reported 88% of parents of children with and without asthma were aware of air quality alerts, although such knowledge was not associated with anticipated behavioral changes based on the number of poor air quality days (6). As a prior study of US adults found awareness of air quality alerts and behavioral change was increased in areas with more alerts (issued when AQI ≥101) (9), it is possible our findings are similar to McDermott's given both regions have poor air quality (13). Such, it is unknown if our high percentage of parents reporting knowledge of alerts translates to parents of children with asthma residing in areas with improved or differing air quality. Regardless of region, we speculate most parents of children with asthma will have greater knowledge of alerts given national studies in adults which consistently report increased air quality alert awareness in persons with asthma (8, 14) or respiratory disease (15). Our results agree with prior studies in that persons with respiratory disease more frequently report behavioral modifications in response to poor air quality, yet the overall percentages of those reporting changes are low (8, 9, 16).
We found that despite awareness of air quality alerts, only a small percentage of parents checked the AQI on the EPA's AirNow smartphone app or website. A 2014 study found that most adults received their air alerts via television (17), although it is unclear if this holds true today given the wide-spread availability of smartphones and apps. A more recent study found adolescents with asthma most often heard or read about air quality alerts on mobile apps (18). An important consideration of air alerts is that they are often issued on days when the AQI is forecast to be at the orange level and above (≥101), yet adverse childhood asthma outcomes have been reported for concentrations below that level (19, 20). Such, it is unclear how many children with asthma should follow behavioral modification advice for the AQI moderate category (51–100), which states “… pollution in this range may pose a moderate health concern for a very small number of individuals. People who are unusually sensitive to ozone or participle pollution may experience respiratory symptoms.” (21). Thus, for the AQI to be used as a tool for parents and children to learn individual susceptibilities to air pollution, the AQI must be used outside of just alerts. Therefore, parents and children must be able to find and check current AQI information (i.e., have knowledge of AirNow). Our findings of a low percentage of parents checking AirNow coupled with increased behavioral change amongst those who do, support AirNow education during clinical asthma management encounters.
Unlike other asthma triggers, air pollution's physical characteristics (e.g., colorless, odorless) and delayed onset of symptoms (i.e., lag times) may make it difficult for patients, parents, and health care providers to identify it as an asthma trigger. We found the majority of parents reported air pollution as a trigger for their child's asthma, which is higher than a prior study in which only 3% of parents reported such (22). The difference could represent selection bias or residence in a region with increased air quality awareness. Perception of air pollution as a trigger or cause of illness was higher amongst parents reporting outdoor activity modification. Future studies are needed examining if parental perception of air pollution as a trigger for their child's asthma is associated with increased outdoor air pollution susceptibility.
Consistent with prior studies in adolescents (23, 24), we found that parents of children with asthma did not endorse self nor child avoidance of activity near busy roadways. Given the known harms associated with traffic-related air pollution (TRAP) exposure for persons with asthma, the US Environmental Protection Agency advises avoidance of busy roadways (25). Our results and those of others support the need for healthcare provider discussions regarding the harms of activity near roadways. Such discussions will undoubtedly be influenced by structural and social determinants of health and should consider a child's access to safe activity areas with reduced air pollution, temporality of air pollution (i.e., TRAP highest during rush hours), and the numerous benefits of physical activity (26).
Although half of parents reported a prior healthcare provider discussion about air pollution as an asthma trigger, less than a quarter of parents reported receiving behavioral avoidance recommendations. Compared to existing studies, our results are consistent with a national study noting slightly over half (56%) of pediatricians reported patient discussions about air quality, although that study was limited by lack of specification of indoor verses outdoor pollution (27). Conversely, in studies of US adolescents only 3% overall (23) and 12% with asthma (18) reported discussion of air pollution with a healthcare provider. An important consideration is that our sample was recruited from children predominately seeking asthma management from specialists. Thus, the higher percentage of parents reporting discussion may be biased by our selection. However, if our sample is biased by parents more likely to have discussed air pollution with a healthcare provider, it is further concerning that less than a quarter of parents reported receiving outdoor activity modification recommendations in response to poor air quality. This is particularly important given our results are consistent with national studies noting associations between healthcare provider discussion and increased behavioral modification (8, 14).
Our finding that only half of parents reported a healthcare provider discussion regarding outdoor air pollution as an asthma trigger requires further investigation. The National Asthma Education and Prevention Program guidelines recommend discussion of air quality during asthma care (2) although the recommendations are less specific compared to other well-known environmental triggers. For example, the most recent update (Expert Panel Review 4) provides clear clinical recommendations regarding indoor aeroallergen management (28). The factors contributing to reduced provider discussions are unknown but could include lack of detailed national asthma guideline recommendations, inadequate knowledge of the harms of outdoor air pollution, lack of evidence demonstrating improvement in asthma outcomes when following AQI recommendations, concern for inability to change outdoor air pollution exposure for patients, and/or preferential targeting of indoor asthma triggers such as aeroallergens and tobacco smoke exposure.
Notably, there have been no large prospective studies of the association of the AQI and childhood asthma health outcomes. While our prior work demonstrated an association of the AQI and childhood asthma emergency department visits (20), primarily driven by fine particle pollution, it is unknown if the AQI is predictive of adverse childhood asthma outcomes in all regions nor if adherence to the AQI and its recommendations can prevent adverse asthma outcomes. As the AQI represents the highest individual pollutant and does not consider the effects of multiple pollutants, the health impacts associated with AQI could differ regionally and by varying pollutant concentrations. For example, a recent study in California found the AQI was associated with all cause adult respiratory emergency department visits when and where the AQI strongly correlated with fine particulate matter (29). Given the well-established link between outdoor air pollution and asthma exacerbations in children, it remains prudent to recommend usage of the AQI and speculatively, it is likely to be most beneficial when used as a tool to learn personal susceptibilities.
We acknowledge our study is limited by a small sample size, however our findings agree with results from national studies. Additionally, our study is limited by the recruitment of parents in whom most children were receiving asthma specialist care in a region with high air pollution levels. Thus, our findings may not be generalizable to all children with asthma, rural locations, or regions with improved air quality. Additionally, we did not ask about other sources of air quality information (e.g., PurpleAir, Breezometer, etc) and although mostly adapted from existing questions, our survey was not validated. Validation of our survey is needed prior to future studies. Lastly, we did not assess knowledge of indoor air quality or interventions, which can also be an important source of air pollution exposure.
When discussing behavioral interventions for outdoor air pollution, such as the Air Quality Index, it is important to note that the most equitable and impactful interventions are those at a policy level (30). Indeed, the United States (US) has experienced marked reductions in outdoor air pollution as a result of the Clean Air Act. Unfortunately, reductions are often inequitably experienced, and in general wealthier non-Hispanic White persons benefit from lower outdoor air pollutant exposure compared to other groups (31). For example, more non-US born, under-resourced, and Black and Hispanic persons live closer to major roadways compared to non-Hispanic White persons (32). Thus, personal interventions are likely to widen inequities by placing the burden of air pollution on individuals, thus a matter of environmental justice (30). However, the preponderance of evidence supports outdoor air pollution harms children with asthma and healthcare providers should discuss this as part of management. Such discussions should include assessment of potential risks, benefits, and harms (e.g., anxiety, sedentarism) of behavioral interventions (30). For example, if avoidance of exercise near a major roadway is not possible, times when pollution is likely to be lower (e.g., non-rush hours times) and the importance of physical activity for overall health could be discussed (33, 34).
In conclusion, our findings suggest that healthcare providers, as part of asthma management in children, should discuss outdoor air pollution as an asthma trigger while also recommending usage of the AirNow (app or website) to guide appropriate behavioral avoidance measures. Future studies of large cohorts of children living in different geographic regions are needed to confirm our study findings as well as assess the association and efficacy of AQI usage on improving asthma outcomes.
The original contributions presented in the study are included in the article/Supplementary materials, further inquiries can be directed to the corresponding author/s.
The studies involving human participants were reviewed and approved by University of Pittsburgh Institutional Review Board. The participants provided their written informed consent to participate in this study.
FR participated in study design and implementation; JR-A FR, Y-YH, EF, and JCC participated in data analysis; JR-A and FR wrote the initial draft of the manuscript and all co-authors participated in the review of the manuscript and approved its final version. All authors contributed to the article and approved the submitted version.
This study was supported by the American Thoracic Society Foundation (ATSF, 2019 to FR). The ATSF had no role in study design; collection, analysis nor interpretation of data; writing of the report; nor in submission decision. Contributions supported by the National Institutes of Health include KL2 TR001856 [FR; PI: Doris Rubio] and HL159333 [FR] not concurrent; MD011764 [Y-YH, JCC]; HL117191 [JCC]; HL149693 [EF]; and UL1 TR001857 [Clinical and Translational Science Institute at the University of Pittsburgh]).
We wish to thank the parents and legal guardians who participated in this study.
JCC has received research materials (inhaled corticosteroids) from Merck, to provide medications free of cost to participants in an NIH-funded study, unrelated to the current work.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fped.2022.966372/full#supplementary-material.
1. Guarnieri M, Balmes JR. Outdoor air pollution and asthma. Lancet. (2014) 383(9928):1581–92. doi: 10.1016/S0140-6736(14)60617-6
2. National Asthma Education and Prevention Program Expert Panel. Report 3 Guidelines for Diagnosis and Management of Asthma. U.S. Department of Health and Human Services, National Institutes of Health, National Heart Lung and Blood Institute; 2007.
3. Brumberg HL, Karr CJ. Council on environmental H. Ambient air pollution: health hazards to children. Pediatrics. (2021) 147(6):e2021051484. doi: 10.1542/peds.2021-051484
4. Laumbach RJ, Cromar KR, Adamkiewicz G, Carlsten C, Charpin D, Chan WR, et al. Personal interventions for reducing exposure and risk for outdoor air pollution: an official American thoracic society workshop report. Ann Am Thorac Soc. (2021) 18(9):1435–43. doi: 10.1513/AnnalsATS.202104-421ST
5. Carlsten C, Salvi S, Wong GWK, Chung KF. Personal strategies to minimise effects of air pollution on respiratory health: advice for providers, patients and the public. Eur Respir J. (2020) 55(6):1902056. doi: 10.1183/13993003.02056-2019
6. McDermott M, Srivastava R, Croskell S. Awareness of and compliance with air pollution advisories: a comparison of parents of asthmatics with other parents. J Asthma. (2006) 43(3):235–9. doi: 10.1080/02770900600567114
7. NHANES 2007-2008 and 2009-2010 Questionnaire Data. Air Quality. The Centers for Disease Control and Prevention. 2010 [cited 7/29/21]. Available at: https://wwwn.cdc.gov/Nchs/Nhanes/Search/DataPage.aspx?Component=Questionnaire/Cycle=2007-2008
8. Wen XJ, Balluz L, Mokdad A. Association between media alerts of air quality index and change of outdoor activity among adult asthma in six states, BRFSS, 2005. J Community Health. (2009) 34(1):40–6. doi: 10.1007/s10900-008-9126-4
9. Mirabelli MC, Ebelt S, Damon SA. Air quality Index and air quality awareness among adults in the United States. Environ Res. (2020) 183:109185. doi: 10.1016/j.envres.2020.109185
10. Borbet TC, Gladson LA, Cromar KR. Assessing air quality index awareness and use in Mexico city. BMC public Health. (2018) 18(1):538. doi: 10.1186/s12889-018-5418-5
11. Semenza JC, Wilson DJ, Parra J, Bontempo BD, Hart M, Sailor DJ, et al. Public perception and behavior change in relationship to hot weather and air pollution. Environ Res. (2008) 107(3):401–11. doi: 10.1016/j.envres.2008.03.005
12. Akinbami LJ, Salo PM, Cloutier MM, Wilkerson JC, Elward KS, Mazurek JM, et al. Primary care clinician adherence with asthma guidelines: the national asthma survey of physicians. J Asthma. (2020) 57(5):543–55. doi: 10.1080/02770903.2019.1579831
13. Cromar KR, Gladson LA, Ewart G. Trends in excess morbidity and mortality associated with air pollution above American thoracic society-recommended standards, 2008-2017. Ann Am Thorac Soc. (2019) 16(7):836–45. doi: 10.1513/AnnalsATS.201812-914OC
14. Mirabelli MC, Boehmer TK, Damon SA, Sircar KD, Wall HK, Yip FY, et al. Air quality awareness among U.S. Adults with respiratory and heart disease. Am J Prev Med. (2018) 54(5):679–87. doi: 10.1016/j.amepre.2018.01.037
15. Wells EM, Dearborn DG, Jackson LW. Activity change in response to bad air quality, national health and nutrition examination survey, 2007-2010. PloS one. (2012) 7(11):e50526. doi: 10.1371/journal.pone.0050526
16. Lissaker CT, Talbott EO, Kan H, Xu X. Status and determinants of individual actions to reduce health impacts of air pollution in US adults. Arch Environ Occup Health. (2016) 71(1):43–8. doi: 10.1080/19338244.2014.988673
17. Pennington AF, Sircar K, Hsu J, Zahran HS, Damon SA, Mirabelli MC. Communication channels for air quality alerts in the United States. Prev Med Rep. (2019) 14:100860. doi: 10.1016/j.pmedr.2019.100860
18. Lynch KM, Mirabelli MC. Air quality awareness and behaviors of U.S. Adolescents with and without asthma. Am J Prev Med. (2021) 61(5):724–8. doi: 10.1016/j.amepre.2021.04.030
19. Hernandez ML, Dhingra R, Burbank AJ, Todorich K, Loughlin CE, Frye M, et al. Low-level ozone has both respiratory and systemic effects in african American adolescents with asthma despite asthma controller therapy. J Allergy Clin Immunol. (2018) 142(6):1974–7. doi: 10.1016/j.jaci.2018.08.003
20. Rosser F, Han YY, Rothenberger SD, Forno E, Mair C, Celedon JC. Air quality Index and emergency department visits and hospitalizations for childhood asthma. Ann Am Thorac Soc. (2022) 19(7):1139–48. doi: 10.1513/AnnalsATS.202105-539OC
21. AQI Air Quality Index: A Guide to Air Quality and Your Health. Research Triangle Park, NC: U.S. Environmental Protection Agency, Office of Air Quality Planning and Standards, Outreach and Information Division; 2014.
22. Cabana MD, Slish KK, Lewis TC, Brown RW, Nan B, Lin X, et al. Parental management of asthma triggers within a child's Environment. J Allergy Clin Immunol. (2004) 114(2):352–7. doi: 10.1016/j.jaci.2004.04.047
23. Lynch KM, Mirabelli MC. Outdoor air quality awareness, perceptions, and behaviors among U.S. Children aged 12-17 years, 2015-2018. J Adolesc Health. (2021) 68(5):882–7. doi: 10.1016/j.jadohealth.2020.07.040
24. Lovinsky-Desir S, Jung KH, Montilla M, Quinn J, Cahill J, Sheehan D, et al. Locations of adolescent physical activity in an urban environment and their associations with air pollution and lung function. Ann Am Thorac Soc. (2021) 18(1):84–92. doi: 10.1513/AnnalsATS.201910-792OC
25. Asthma and Outdoor Air Pollution. Environmental Protection Agency, EPA-452-F-04-002. Available at: https://www.airnow.gov/sites/default/files/2018-03/asthma-flyer.pdf Accessed June, 2022.
26. Tainio M, Jovanovic Andersen Z, Nieuwenhuijsen MJ, Hu L, de Nazelle A, An R, et al. Air pollution, physical activity and health: a mapping review of the evidence. Environ Int. (2021) 147:105954. doi: 10.1016/j.envint.2020.105954
27. Mirabelli MC, Damon SA, Beavers SF, Sircar KD. Patient-Provider discussions about strategies to limit air pollution exposures. Am J Prev Med. (2018) 55(2):e49–52. doi: 10.1016/j.amepre.2018.03.018
28. U.S. Department of Health and Human Services, National Institutes of Health. 2020 Focued Updates to the Asthma Management Guidelines, Clinician's Guide. Indoor Allergen Mitigation. NIH Publication No. 20-HL-8141. Available at: https://www.nhlbi.nih.gov/resources/clinician-guide-2020-focused-updates-asthma-management-guidelines Accessed September, 2022.
29. Cromar KR, Ghazipura M, Gladson LA, Perlmutt L. Evaluating the U.S. Air quality Index as a risk communication tool: comparing associations of index values with respiratory morbidity among adults in California. PloS one. (2020) 15(11):e0242031. doi: 10.1371/journal.pone.0242031
30. Laumbach RJ, Cromar KR. Personal interventions to reduce exposure to outdoor air pollution. Annu Rev Public Health. (2022) 43:293–309. doi: 10.1146/annurev-publhealth-052120-103607
31. Jbaily A, Zhou X, Liu J, Lee TH, Kamareddine L, Verguet S, et al. Air pollution exposure disparities across US population and income groups. Nature. (2022) 601(7892):228–33. doi: 10.1038/s41586-021-04190-y
32. Boehmer TK, Foster SL, Henry JR, Woghiren-Akinnifesi EL, Yip FY. Residential proximity to major highways - United States, 2010. MMWR Surveill Summ. (2013) 62(Suppl 3):46–50. PMID: 24264489
33. Lovinsky-Desir S, Jung KH, Jezioro JR, Torrone DZ, de Planell-Saguer M, Yan B, et al. Physical activity, black carbon exposure, and DNA methylation in the FOXP3 promoter. Clin Epigenetics. (2017) 9:65. doi: 10.1186/s13148-017-0364-0
Keywords: childhood asthma, air quality index, air pollution, parental knowledge and practice, air quality index (AQI)
Citation: Reyes-Angel J, Han Y-Y, Forno E, Celedón JC and Rosser FJ (2022) Parental knowledge and usage of air quality in childhood asthma management. Front. Pediatr. 10:966372. doi: 10.3389/fped.2022.966372
Received: 10 June 2022; Accepted: 6 October 2022;
Published: 26 October 2022.
Edited by:
Malcolm King, Saskatchewan Centre for Patient-Oriented Research, CanadaReviewed by:
Jessica Rice, Children's Hospital of Philadelphia, United States© 2022 Reyes-Angel, Han, Forno, Celedón and Rosser. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Franziska Rosser RnJhbnppc2thLnJvc3NlcjJAY2hwLmVkdQ==
Specialty Section: This article was submitted to Pediatric Pulmonology, a section of the journal Frontiers in Pediatrics
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.