
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Pediatr., 14 October 2022
Sec. Pediatric Urology
Volume 10 - 2022 | https://doi.org/10.3389/fped.2022.964147
This article is part of the Research TopicPyeloplasties in Challenging Scenarios as Redo Procedures, Congenital Anatomical Anomalies and Infants: Where do we Stand?View all 7 articles
 Ce Han1,2,3†
Ce Han1,2,3† Lifei Ma1,2†
Lifei Ma1,2† Pin Li1,2†
Pin Li1,2† Jia’nan Wang4
Jia’nan Wang4 Xiaoguang Zhou1,2
Xiaoguang Zhou1,2 Tian Tao1,2
Tian Tao1,2 Hualin Cao5
Hualin Cao5 Yuandong Tao1,2
Yuandong Tao1,2 Yunjie Yang6
Yunjie Yang6 Yang Zhao1,2
Yang Zhao1,2 Weiwei Zhu1,2,3
Weiwei Zhu1,2,3 Tao Guo1,2,3
Tao Guo1,2,3 Xuexue Lyu1,2,3
Xuexue Lyu1,2,3 Ran Zhuo1,2
Ran Zhuo1,2 Huixia Zhou1,2*
Huixia Zhou1,2*Objective: The objective of this study is to introduce a novel technique of robotic-assisted laparoscopic pyeloplasty (RALP) for ureteropelvic junction obstruction (UPJO) with long proximal ureteral stricture in children.
Materials and methods: Clinical information on patients who underwent a modified RALP between July 2018 and May 2019 in our center was collected retrospectively. Our surgical modifications mainly include “double-flap” tailoring of the renal pelvis and anastomosis of spatulate ureter with the double-flap. Demographic, perioperative, postoperative, and follow-up information was recorded in detail.
Results: A total of 13 patients were included in the study. All the patients underwent a modified RALP without conversion to open surgery. They were followed up with a median time of 36 months. The anteroposterior diameter of the renal pelvis was 1.19 ± 0.21 at 6 months after the surgery, which was significantly lower than that on admission (3.93 ± 0.79). The split renal function of the children was also significantly improved from 0.37 ± 0.05) to 0.46 ± 0.02 at 6 months after surgery (p < 0.05). The diuretic renography revealed that all the patients have a T1/2 time less than 20 min postoperatively. The children were in good condition during the follow-up period.
Conclusions: Modified RALP is an effective surgical treatment for children with UPJO with long proximal ureteral stricture. The success rate of this modification has been preliminarily confirmed.
Hydronephrosis, defined as dilation of the renal pelvis and/or calycesis, is a common congenital abnormality in the urological system of children (1). Ureteropelvic junction obstruction (UPJO) is the main cause of hydronephrosis (2). An untreated disease can result in renal impairment, making effective management crucial. The gold standard surgical treatment for UPJO is the Anderson-Hynes dismembered pyeloplasty technique described by Anderson and Hynes (3, 4). Owing to the potential high tension of anastomosis, conventional dismembered pyeloplasty is a relative contraindication for patients with complex conditions, especially for long proximal ureteral strictures (5).
Several surgical techniques have been adopted to address the considerable challenge of long proximal ureteral stenosis. Renal autotransplantation (6) or intestinal replacement (7) is a possible solution but always results in vascular or bowel complications. The appendix (8), oral mucosa (9), and renal pelvis (10) have also been proposed to manage the complex problem. Among them, the renal pelvis might be the best option, as it shares the same urothelium with the ureter (11). In this article, we introduced our “double-flap” technique and reported our preliminary experience.
This study included children who underwent a modified robotic-assisted laparoscopic pyeloplasty (MRALP) in our center from July 2018 to May 2019. The indication for surgery was long proximal ureteral stricture (> 2 cm), which was not suitable for traditional end-to-end anastomosis. In addition, all patients should satisfy one of the following criteria before operation: ultrasonography screening showed that the separation of the anteroposterior diameter (APD) of the renal pelvis was > 3 cm; symptomatic hydronephrosis (flank pain, recurrent urinary tract infection, fever, and hematuria), diuretic renal radionuclide scan showing obstruction, and T1/2 > 20 min. Children with vesicoureteral reflux, congenital megaureters, and posterior urethral valve or other structural anomalies were excluded from the study. All the patients underwent ultrasonography, magnetic resonance urography (Figure 1), voiding cystourethrography (VCUG), and 99 mTc-mercaptoacetyltriglycine diuretic renography before surgery. The precise stricture length was measured intraoperatively.
Postoperative complications were evaluated with the Clavien–Dindo classification system. The study was approved by the Ethics Committee of the Seventh Medical Center of the PLA General Hospital (No. 2017-036). All the patients’ parents agreed to participate in the study and signed written consent forms.
After general anesthesia, the child was placed 45–60 degrees from the horizontal direction (12). The trocar position has been described in an article previously published by our team (13). After the stricture ureter was located, we measured the length of the segment with a silk thread (Figure 2). Then we spatulated the ureter longitudinally along the lateral wall across the stricture segment of ureter. The length of spatulated ureter exceeded the stenotic ureter by 1 cm. Then, we incised the renal pelvis from the ureteropelvic junction to the lower middle third of the renal hilus. The ureter pelvis was cut into double flaps (Figures 3, 4). The inferior pelvis flap was trimmed to a tongue shape, and the first stitch was sutured between the inferior flap apex and the lowest corner of the spatulate ureter with a 6-0 monocryl suture. Then, a continuous suture was conducted between the posterior edge of the flap and the ureter. After a double-J stent was placed anterogradely, the superior pelvis flap was used to cover the defect area and anastomose continuously.
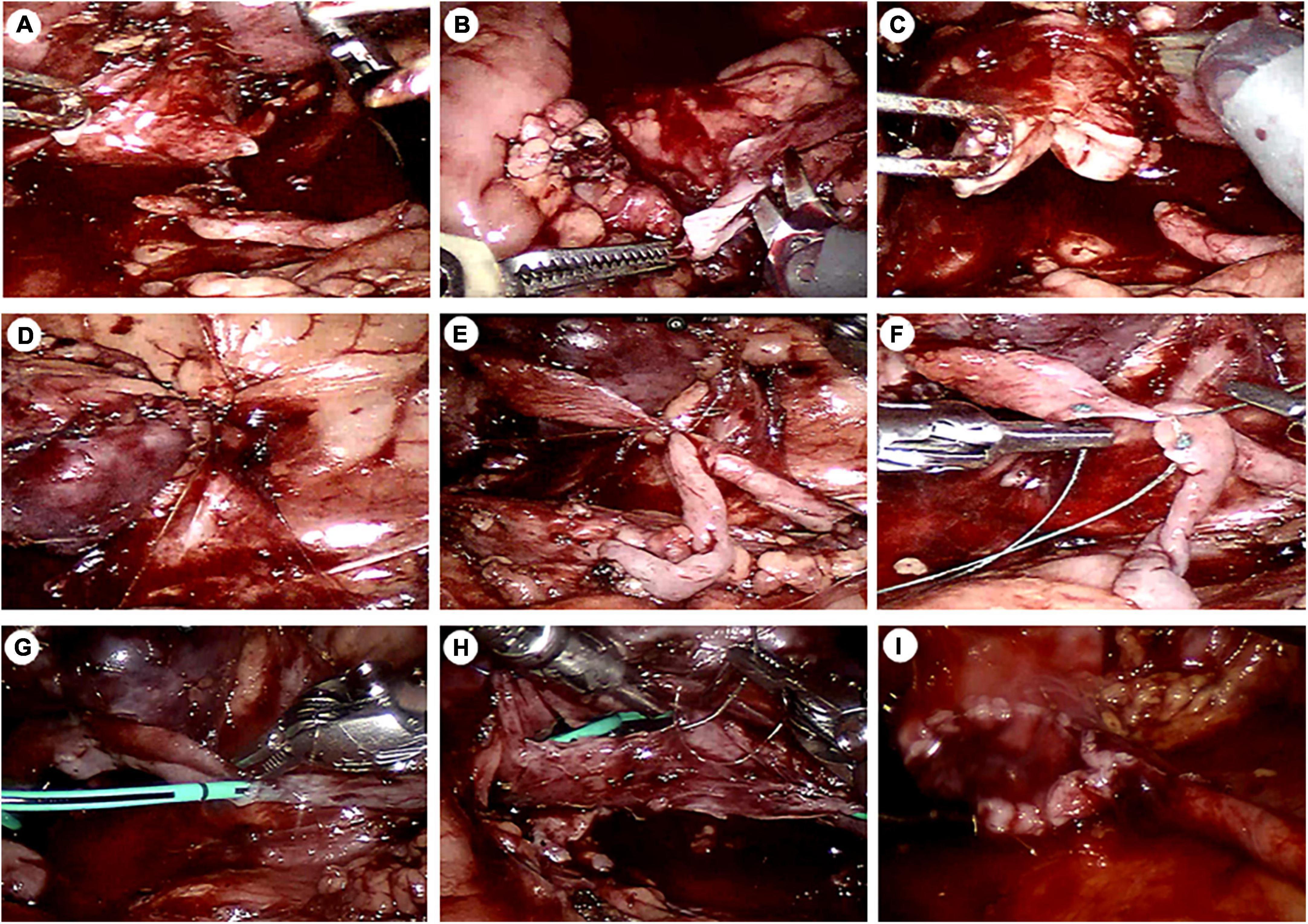
Figure 3. Intraoperative images. (A) The ureteropelvic junction was dismembered. (B) The ureter was cut longitudinally along the lateral edge of the ureter. (C) The renal pelvis was cut into double flaps. (D) The inferior pole of the kidney was fixed to the lateral abdominal wall. (E) The first stitch was placed between the lowest point of the inferior and the lowest point of the spatulate ureter. (F) The posterior wall was sutured continuously a using a traction suture. (G) A DJ stent was placed. (H) The anterior wall was anastomosed continuously. (I) The superior pelvis flap was sutured. Finally, the pelvis and the ureter together formed a “funnel.”
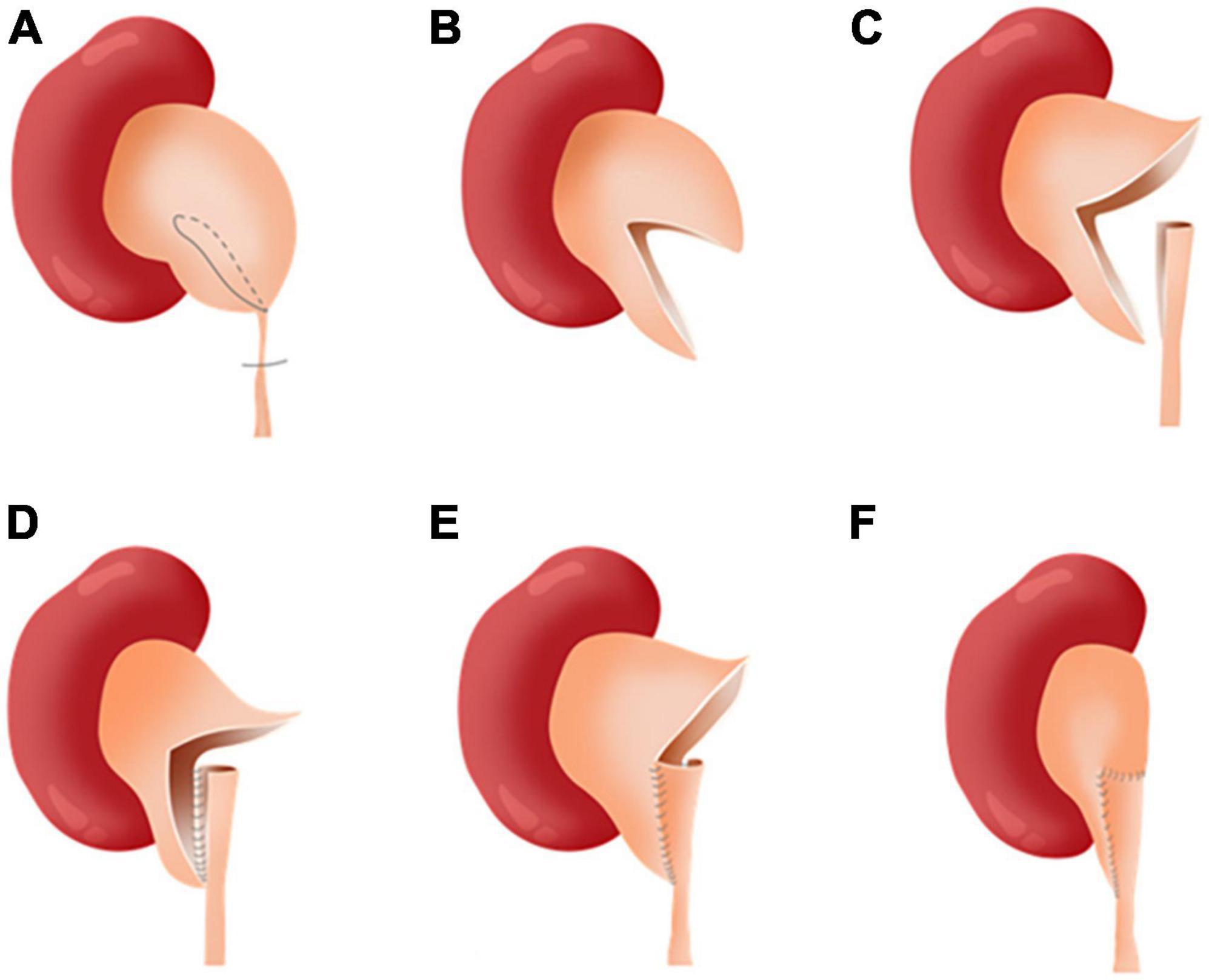
Figure 4. The “double-flap” technique. (A) Cut by line. (B) Pelvis double flaps. (C) Spatulate longitudinally along the lateral edge of the ureter. (D) Continuous posterior wall anastomosis. (E) Continuous anterior wall anastomosis. (F) Continuous superior flap anastomosis.
The double-J stent was removed under cystoscopy 6∼8 weeks after the operation. All the patients were followed up by ultrasonography 3, 6, 12, and 24 months after the operation. Six months after the operation, all the children underwent radionuclide and diuretic renography examinations.
All data were analyzed with the SPSS 26.0 statistical software. The data was expressed as median [interquartile range (IQR)] or median (range). The preoperative and postoperative data were compared by Student t-test and Fisher exact test. P < 0.05 was considered a significant difference.
A total of thirteen patients were included in this study. All the operations were successfully completed without conversion to open surgery. The baseline clinical data of all the included patients are shown in Table 1. The perioperative information and postoperative complications are summarized in Table 2. The preoperative examination indices and postoperative follow-up of the children are statistically analyzed in Table 3. In this study, eleven boys and two girls were included, with a median age of 5 years. There were nine left side hydronephrosis patients and four right side hydronephrosis patients. Seven of the children experienced flank pain. Four children were observed because of prenatal hydronephrosis, which gradually deteriorated. One child had hematuria and one had fever due to urinary tract infection. The median length of ureteral stenosis was 2.5 cm (range 2–4 cm). Two patients had Clavien-Dindo grade II complications after the operation (intravenous antibiotic treatment for fever due to infection), but none of them had Clavien-Dindo III or IV complications. The children were followed for a median of 36 months. The APD of the renal pelvis at 6 months after the operation (1.19 ± 0.21) decreased significantly compared with that before the operation (3.93 ± 0.79) (p < 0.05). The split renal function also improved from (0.37 ± 0.05) to (0.5 ± 0.02) 6 months after the operation. The diuretic renography revealed that all the patients have a T1/2 time of less than 20 min at the same time.
Treatment of UPJO with a concomitant long proximal ureteral stricture is often a dilemma for most urologists. Some experts continually explored the use of an autologous tissue to realize an alternative surgical technique, and some have achieved satisfactory results (9). Pelvic flaps, as a urothelial tissue, are one of the most preferred patch materials.
Culp and Dewierd reported the application of spiral and vertical flap technology in pyeloplasty in 1951 (14). Scardino and Prince affirmed the advantages of spiral and vertical flaps in reconstruction of proximal ureteral stenosis in 1953 (10). In 2002, Kaouk et al. reported the treatment of long ureteral stricture by laparoscopic dismembered pyeloplasty using the renal pelvis instead of the ureter. The length of the tubularized renal pelvis could be as long as 3 cm. When the pelvic tissue is adequate, adopting the pelvis to replace the ureter can be a choice (15). In 2007, Basiri et al. reported the application of a laparoscopic non-dismembered renal pelvis flap for treatment of patients with ureteral stenosis longer than 2 cm (16). In 2018, Sarihan et al. reported an open operation of reverse tubularized pelvis flap method for treatment of long ureteral stenosis. This study is the first report on patients aged 2–6 months. The study suggested that the reverse pelvic flap method is suitable for treatment of long segment UPJ obstruction in infants (17).
However, the conventional treatment has several limitations. Non-dismembered flap pyeloplasty cannot excise the obliterative, fibrotic, and non-peristaltic ureter. This situation leads to a reconstructed ureter lacking peristaltic function (18). For patients with poorly dilated renal pelvis, traditional dismembered pyeloplasty is not suitable because of lack of adequate renal pelvis tissue. The tubularized flap technique has the potential risks of restenosis and ischemia (19). Absorbing a previous experience, we modified the traditional pyeloplasty technique and developed the “double-flap” technique. This technique is quite suitable for extra renal pelvis, but it can also be used in patients with normal or small-sized renal pelvis. For intrarenal pelvis, this technique should not be applied.
This is the first study to conduct robotic-assisted laparoscopy to replace a part of the ureteral tissue with double renal pelvis flaps for treatment of UPJO with proximal ureteral stricture in children. Currently, surgical treatment has evolved from an open era to a minimally invasive era. Peters et al. first reported laparoscopic pyeloplasty in children in 1995 (20), and Gettman et al. first reported robotic pyeloplasty in 9 children in 2002 (21). Robotic and laparoscopic surgeries have achieved the same success rate as open surgery, with minimally invasive treatment, rapid postoperative recovery, and mild postoperative pain symptoms (22).
Based on our encouraging initial experience and clinical confirmation, our technical modifications proved reasonable. First, it avoids excessive pulling of the ureter. After cutting off the fibrotic and atresia ureter, the spatulated ureter can be anastomosed with pelvic flap at the horizontal level to avoid tension anastomoses caused by excessive pulling of the ureter that can result in ureteral scar formation and urinary leakage. In addition, the onlay anastomosis technique for the ureter and renal pelvis flap cannot only ensure good peristaltic function of the new ureter but also broaden the diameter of the upper ureter and form “a funnel” shape gradually tending to the normal diameter.
These key surgical procedures can help avoid postoperative restenosis. Moreover, traction sutures are used for fine operations to avoid the tissue ischemia caused by excessive clamping of the tissue (23). This method can also effectively avoid an unsmooth inner surface of the ureter lumen and excessive scar or polyp formation after surgery. In the anastomotic process, 6-0 monocryl is used for continuous suture, which can prevent the occurrence of postoperative urine leakage, and the scar reaction of anastomosis was minimal. In addition, to ensure blood supply to the ureter, the adipose tissue around the anastomotic ureter should be cleaned as much as possible to prevent the tissue from embedding into the anastomotic orifice and forming small polyps, which will adversely affect healing. Finally, we can attach the purpose that is to completely remove the diseased tissue, alleviate the patient’s symptoms, and protect the patient’s renal function.
This study had several limitations: the retrospective design has some bias when collecting the data. Moreover, this was a single-center study. Further validation of multicenter studies should be considered. This study included 13 patients, which is quite a small sample size. The effectiveness and advantages/disadvantages of this technology should be further verified by increasing the sample size.
Our modified robotic pyeloplasty could be a practical and effective treatment option with high success rate for UPJO with long proximal ureteral stricture. However, a larger sample size, longer follow-up, and further controlled prospective studies are necessary to evaluate its safety and efficacy.
The original contributions presented in this study are included in the article/supplementary material, further inquiries can be directed to the corresponding author/s.
The studies involving human participants were reviewed and approved by the Ethics Committee of the Seventh Medical Center of the PLA General Hospital (No. 2017-036). Written informed consent to participate in this study was provided by the participants’ legal guardian/next of kin. Written informed consent was obtained from the individual(s), and minor(s)’ legal guardian/next of kin, for the publication of any potentially identifiable images or data included in this article.
CH and PL: conception and design. HZ: administrative support. LM, XZ, and TT: provision of study materials or patients. WZ, YZ, and TG: collection and assembly of data. RZ and XL: data analysis and interpretation. All authors wrote the manuscript and approved the final version of the manuscript.
This study was supported by the Military Family Planning Fund (18JS001), Beijing Municipal Science and Technology Plan (No. Z181100001718008), and Capital Health Development Research Fund (No. 2016-2-5091).
We would like to thank all the colleagues in our department.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Krajewski W, Wojciechowska J, Dembowski J, Zdrojowy R, Szydełko T. Hydronephrosis in the course of ureteropelvic junction obstruction: An underestimated problem? Current opinions on the pathogenesis, diagnosis and treatment. Adv Clin Exp Med. (2017) 26:857–64. doi: 10.17219/acem/59509
2. Asl AS, Maleknejad S. Clinical outcome and follow-up of prenatal hydronephrosis. Saudi J Kidney Dis Transpl. (2012) 23:526–31.
3. Wahyudi I, Tendi W, Rahman F, Situmorang GR, Rodjani A. Minimal invasive treatment in pelvic-ureteric junction obstruction: a comprehensive review. Res Rep Urol. (2021) 13:573–80. doi: 10.2147/RRU.S268569
4. Hashim H, Woodhouse CRJ. Ureteropelvic junction obstruction. Eur Urol Suppl. (2012) 11:25–32. doi: 10.1016/j.eursup.2012.01.004
5. Wang J, Li B. Minimally invasive (laparoscopic/robotic) ureteroplasty for long segment proximal and mid ureteral strictures. Int Urol Nephrol. (2021) 53:603–5. doi: 10.1007/s11255-020-02689-3
6. Wotkowicz C, Libertino JA. Renal autotransplantation. BJU Int. (2004) 93:253–7. doi: 10.1111/j.1464-410x.2004.04596.x
7. Xiong S, Zhu W, Li X, Zhang P, Wang H, Li X. Intestinal interposition for complex ureteral reconstruction: A comprehensive review. Int J Urol. (2020) 27:377–86. doi: 10.1111/iju.14222
8. Cao, H, Zhou H, Yang F, Ma L, Zhou X, Tao T, et al. Laparoscopic inside the text. appendiceal interposition pyeloplasty for long ureteric strictures in children. J Pediatr Urol. (2018) 14:551. doi: 10.1016/j.jpurol.2018.06.017
9. Xiong S, Wang J, Zhu W, Yang K, Ding G, Li X, et al. Onlay repair technique for the management of ureteral strictures: a comprehensive review. Biomed Res Int. (2020) 2020:6178286. doi: 10.1155/2020/6178286
10. Culp OS, Deweerd JH. A pelvic flap operation for certain types of ureteropelvic obstruction; observations after two years’ experience. J Urol. (1954) 71:523–9. doi: 10.1016/s0022-5347(17)67820-0
11. Cheng S, Fan S, Wang J, Xiong S, Li X, Xu Y, et al. Laparoscopic and robotic ureteroplasty using onlay flap or graft for the management of long proximal or middle ureteral strictures: our experience and strategy. Int Urol Nephrol. (2021) 53:479–88. doi: 10.1007/s11255-020-02679-5
12. Kim SJ, Barlog JS, Akhavan A. Robotic-Assisted urologic surgery in infants: positioning, trocar placement, and physiological considerations. Front Pediatr (2019) 6:411. doi: 10.3389/fped.2018.00411
13. Li P, Zhou H, Cao H, Guo T, Zhu W, Zhao Y, et al. Early robotic-assisted laparoscopic pyeloplasty for infants under 3 months with severe ureteropelvic junction obstruction. Front Pediatr. (2021) 9:590865.
14. Scardino PL, Prince CL. Vertical flap ureteropelvioplasty. South Med J. (1953) 46:325–31. doi: 10.1097/00007611-195304000-00003
15. Kaouk JH, Kuang W, Gill IS. Laparoscopic dismembered tubularized flap pyeloplasty: a novel technique. J Urol. (2002) 167:229–31.
16. Basiri A, Behjati S, Zand S, Moghaddam SM. Laparoscopic pyeloplasty in secondary ureteropelvic junction obstruction after failed open surgery. J Endourol. (2007) 21:1045–51. doi: 10.1089/end.2006.0414
17. Sarihan H, Yalçın Comert HS, Ýmamoðlu M, Basar D. Reverse tubularized pelvis flap method for the treatment of long segment ureteropelvic junction obstruction. Med Princ Pract. (2020) 29:128–33. doi: 10.1159/000502028
18. Cheng S, Li X, Yang K, Xiong S, Li Z, Zhu H, et al. Modified laparoscopic and robotic flap pyeloplasty for recurrent ureteropelvic junction obstruction with a long proximal ureteral stricture: the “wishbone” anastomosis and the “ureteral plate” technique. Urol Int. (2021) 105:642–9. doi: 10.1159/000512994
19. Tracey AT, Eun DD, Stifelman MD, Hemal AK, Stein RJ, Mottrie A, et al. Robotic-assisted laparoscopic repair of ureteral injury: an evidence-based review of techniques and outcomes. Minerva Urol Nefrol. (2018) 70:231–41. doi: 10.23736/S0393-2249.18.03137-5
20. Peters CA, Schlussel RN, Retik AB. Pediatric laparoscopic dismembered pyeloplasty. J Urol. (1995) 153:1962–5.
21. Gettman MT, Neururer R, Bartsch G, Peschel R. Anderson-Hynes dismembered pyeloplasty performed using the da Vinci robotic system. Urology. (2002) 60:509–13. doi: 10.1016/s0090-4295(02)01761-2
22. Liu DB, Ellimoottil C, Flum AS, Casey JT, Gong EM. Contemporary national comparison of open, laparoscopic, and robotic-assisted laparoscopic pediatric pyeloplasty. J Pediatr Urol. (2014) 10:610–5. doi: 10.1016/j.jpurol.2014.06.010
Keywords: modified robotic-assisted laparoscopic pyeloplasty (MRALP), hydronephrosis, long proximal ureteral stricture, pediatrics, renal pelvic flaps
Citation: Han C, Ma L, Li P, Wang J, Zhou X, Tao T, Cao H, Tao Y, Yang Y, Zhao Y, Zhu W, Guo T, Lyu X, Zhuo R and Zhou H (2022) Modified robotic-assisted laparoscopic pyeloplasty in children for ureteropelvic junction obstruction with long proximal ureteral stricture: The “double-flap” technique. Front. Pediatr. 10:964147. doi: 10.3389/fped.2022.964147
Received: 08 June 2022; Accepted: 29 August 2022;
Published: 14 October 2022.
Edited by:
Simone Sforza, Meyer Children’s Hospital, ItalyCopyright © 2022 Han, Ma, Li, Wang, Zhou, Tao, Cao, Tao, Yang, Zhao, Zhu, Guo, Lyu, Zhuo and Zhou. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Huixia Zhou, aHVpeGlhOTk5OTlAMTYzLmNvbQ==
†These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.