
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
BRIEF RESEARCH REPORT article
Front. Pediatr., 25 August 2022
Sec. Pediatric Infectious Diseases
Volume 10 - 2022 | https://doi.org/10.3389/fped.2022.951039
This article is part of the Research TopicChildhood Vaccination and COVID-19View all 17 articles
Background: Maternal attitudes and beliefs have been shown to influence childhood vaccination coverage, resulting in under-vaccination, non-vaccination, and vaccination delay. This study aimed to investigate the mothers' attitudes and perceptions about vaccination for their children in Greece.
Methods: This was an online cross-sectional study, conducted from 4 April to 8 June 2020. A self-administered questionnaire was used to collect information about mothers' and their children's socio-demographic characteristics, previous vaccination behavior, and mothers' attitudes and perceptions about childhood vaccination. Participants included adult mothers with at least one minor child.
Results: One thousand eight hundred eighty-five mothers participated, with the majority (91.7%) believing in the usefulness of vaccines and that vaccines protect children from serious and life-threatening diseases. A larger percentage of mothers with higher educational attainment agreed/absolutely agreed that all vaccinations provided by the National Vaccination Program must be offered to their children (91.6%) (p = 0.02) and that vaccines protect children from serious and life-threatening diseases (92.9%) (p = 0.01). Significant more married/in cohabitation and not single-parent mothers agreed that vaccines are safe (53.5% and 53.4%, respectively). There were also several significant associations between maternal attitudes toward childhood vaccination and previous maternal vaccination practices [(e.g., adherence to recommended vaccination dosages (all p-values < 0.01), vaccination delays (all p-values < 0.05), and vaccination during pregnancy (all p-values < 0.01)].
Conclusion: Maternal attitudes and perceptions toward childhood vaccination are significantly influenced by sociodemographic factors and maternal vaccination practices. Revealing those is essential for public health officials in developing future strategies to improve childhood vaccination coverage and acceptance of new vaccines such as the COVID-19 vaccine.
Vaccination is undeniably a public health success story for disease eradication (1). Vaccines have been administrated since 1796, preventing millions of deaths and adverse health outcomes (2). They significantly reduced healthcare costs due to the decrease in hospitalizations and disease prevalence (3). Thus, vaccines are considered a cost-effective and life-saving tool (4, 5). More than 200 years after the first vaccine development, the ongoing public health crisis from COVID-19 also highlights the importance of investing in vaccine development, since COVID-19 vaccination contributed to the reduction of hospitalizations, death rate, and adverse health outcomes (6, 7).
The failure of current treatments for bacterial infections, due to antibiotic resistance (8–11), and the burden of infectious diseases renders vaccine development a priority to avert severe infections (12–15). The development of new vaccines is a long complex process, with several attempts to create vaccines for fatal diseases such as AIDS, malaria, and a range of parasitic infections being unsuccessful (16–18). Although vaccine development is a significant milestone for humanity, the public may delay or refuse vaccination with available vaccines: vaccine hesitancy. Vaccine hesitancy was raised during the last decades and is influenced by several determinants including ethnicity, religious, socio-economic factors, beliefs, knowledge, and safety and efficacy concerns (19–24). In addition, unfavorable vaccine incidences could reduce vaccine trust (25). Consequently, specific vaccination rates may not attain adequate coverage to prevent epidemics (26–30).
Childhood vaccination reduces the mortality rate, although some children are unvaccinated or under-vaccinated (31–33). Of note, during the COVID-19 pandemic some childhood vaccinations were delayed or missed (34–36). Specifically, after March 2020 considerably fewer children received the vaccines against diphtheria, pertussis, tetanus, and measles compared to 2019 (37, 38). Several reasons contributed to this decline including the lack of access to health services due to lockdown restrictions, and the shortage of health care staff during the COVID-19 pandemic (39). Also, there is an increasing concern that the pandemic regulations influenced health care professionals' communications with parents, hence limiting routine vaccination promotion (40).
Except for the COVID-19 pandemic, parental hesitancy toward childhood vaccination affects childhood vaccination uptake (26, 41–49). Attitudes and perceptions of parents toward vaccines may influence parental decisions to vaccinate their child/children. Parental vaccination behavior and experiences may result in childhood vaccination delays or refusal (50, 51). In addition, negative opinions toward vaccination may enhance the risk of unvaccinated children and increase the likelihood of disease outbreaks. Recently, outbreaks of vaccine-preventable disease were observed in Europe due to inadequate vaccination rates (27); hence it is essential to estimate the parental attitudes toward childhood vaccinations. Mothers seem to have a prime role in childcare (52), therefore, the present study aimed to evaluate the attitudes and perceptions of mothers in Greece concerning the vaccination of their child/children. Understanding maternal attitudes and beliefs regarding the vaccination of their children is crucial, especially during the COVID-19 pandemic.
This was an online cross-sectional study. This study reported following the Strengthening the Reporting of Observational Studies in Epidemiology (53).
This study was conducted from 4 April 2020 to 8 June 2020. The population of interest was mothers 18 years old and older with at least one minor child (<18 years old), who were living in the four geographical areas of Greece (Attica, Central Greece, North Greece, and Crete/Aegean Islands).
The sample size needed for this study was calculated using the formula, . Assuming a vaccination coverage of 90%, based on a literature review on the topic, a z equal to 1.96 under a 95% confidence interval and a precision of 2%, a sample size of ~864 individuals was required to estimate this (54).
Due to the quarantine restrictions resulting from the ongoing COVID-19 pandemic, a convenience sampling method was used, with a potential effect on sampling possibilities. The questionnaire was administered using Google Forms and dispersed using social media applications (e.g., Facebook, Instagram), instant messaging apps (e.g., WhatsApp, Viper), and social networking sites (e.g., LinkedIn), to gather a sample from all geographical areas of Greece [Attica (46.8%) of the total Greek population, Central Greece (13.0%), North Greece (29.0%) and Crete/Aegean Islands (11.2%)]. Despite the non-probabilistic sampling approach used, we have managed to recruit women of different ages among the Greek mainland and islands, ensuring a relatively representative sample of the adult female Greek population.
The self-administered questionnaire in the Greek language was specially designed after an extensive review of relevant literature and included questions regarding mothers' socio-demographic characteristics, children's characteristics, general information about vaccination practices, and attitudes and perceptions of mothers regarding childhood vaccination (Supplementary File). The survey was pilot tested by 50 mothers for face validity and comprehensibility before study commencement. The pilot study sample was not included in the sample of the study. We have also calculated the Cronbach's alpha coefficient, which it was 0.92 indicating a strong internal consistency.
The first part of the questionnaire included questions regarding maternal socio-demographic characteristics (i.e., age, employment status, educational level, and marital status) and children's characteristics (i.e., age, and gender). Age was reported in years. Geographical area was recorded as Attica, Central Greece, North Greece, and Crete/Aegean Islands while area of residence was classified as urban and rural. Marital status was recorded as never married, married/ in cohabitation, or separated/divorced/widowed. Single parent family was evaluated using a binary question (Yes vs. No). Educational level was classified into three categories: primary education (participants who completed only primary school: < 7 years of schooling), secondary education (participants who completed middle or high school: 7–12 years of schooling), and higher education (participants who have a university degree: >12 years of schooling). Employment status was recorded as unemployed, private, and state or freelance employee. Income status was described using the monthly income and was classified as (i) no income; (ii) low (<1,101 per month); (iii) middle (1,101–1,500 per month); and (iv) high (>1,500 per month). Moreover, characteristics about the children included the number of children, the age, and the gender.
This part of the questionnaire assessed maternal attitudes and perceptions toward childhood vaccination, using 14 Likert-scale questions (Q1-Q14) on a five-point rating scale (1 = absolutely disagree, 2 = disagree, 3 = neither disagree nor agree, 4 = agree, and 5 = absolutely agree).
The questionnaire also included information about previous vaccination practices, including adherence to the prescribed doses as indicated by the local recommendations (Yes vs. No) and delay of vaccination (Yes vs. No). The question used to report the reasons of possible delay of vaccination was “If you have delayed your child/children vaccination, what were the main reasons?” with possible answers being illness, lack of clear information, paediatrician's suggestion, fear of side effects of the vaccine, increased cost of vaccines, increased cost of medical visit, long distance from the vaccination site or other. Vaccination during pregnancy was reported using the question “Have you been vaccinated during your pregnancy?” (Yes vs. No). Participants' general knowledge toward vaccination was assessed using a 12-item scale, but these analyses are reported elsewhere (55).
Descriptive statistics included frequencies (n)/percentages (%) for categorical variables and mean/ standard deviation (SD) or median values/interquartile range (IQR) for continuous variables with normal or skewed distribution, respectively. The skewness of distribution was used to check the normality of numeric variables using the Shapiro–Wilk normality test. Chi-squared test, one-way analysis of variance (ANOVA), and non-parametric tests including Kruskal–Wallis were used to test significant differences between variables. Bonferroni correction test was used to address the problem of multiple comparisons. Bar charts were constructed to present the maternal attitudes and perceptions toward their children's vaccination. All statistical tests performed were two-sided, with the statistical significance level set at α = 0.05. Statistical analysis was conducted using STATA 14.0 (Stata Corp, College Station, TX, USA).
This study was conducted according to the Declaration of Helsinki guidelines and all procedures involving research study participants were approved by the Cyprus National Bioethics Committee (CNBC) (EEBK EΠ 2020.01.82). The survey was voluntary, and no incentive was offered. All the participants were informed about the study's aim and objectives before participating on the first page of the questionnaire. The respondents needed to confirm their willingness to participate voluntarily by answering a “Yes/No” question on an electronic mandatory informed consent form before being allowed to complete the online self-reporting questionnaire.
A total of 1,885 mothers, who live in the four geographical areas of Greece, completed the online questionnaire (Supplementary Figure 1). The mean age of the participants was 36.3 years old (SD = 5.0 years old) (Table 1). Almost half of the participants (46.8%) were residents of the Attica region (including Athens and its suburbs) and 87.0% were living in an urban area. The overwhelming majority were married (95.1%), while 5.1% were single parents. In addition, 73.5% of them had completed a higher education, 39.4% were private employees, and 56.6% had a high monthly salary. Participants reported 2,950 children with a median age of 42 months (IQR: 24–72 months), among whom 51.8% were boys. The majority of the mothers strictly adhered to the prescribed dosage as indicated by the local recommendations for each vaccine (94.3%), have delayed their child/children vaccination (51.5%) and have not been vaccinated during pregnancy (75.7%) (Table 1).
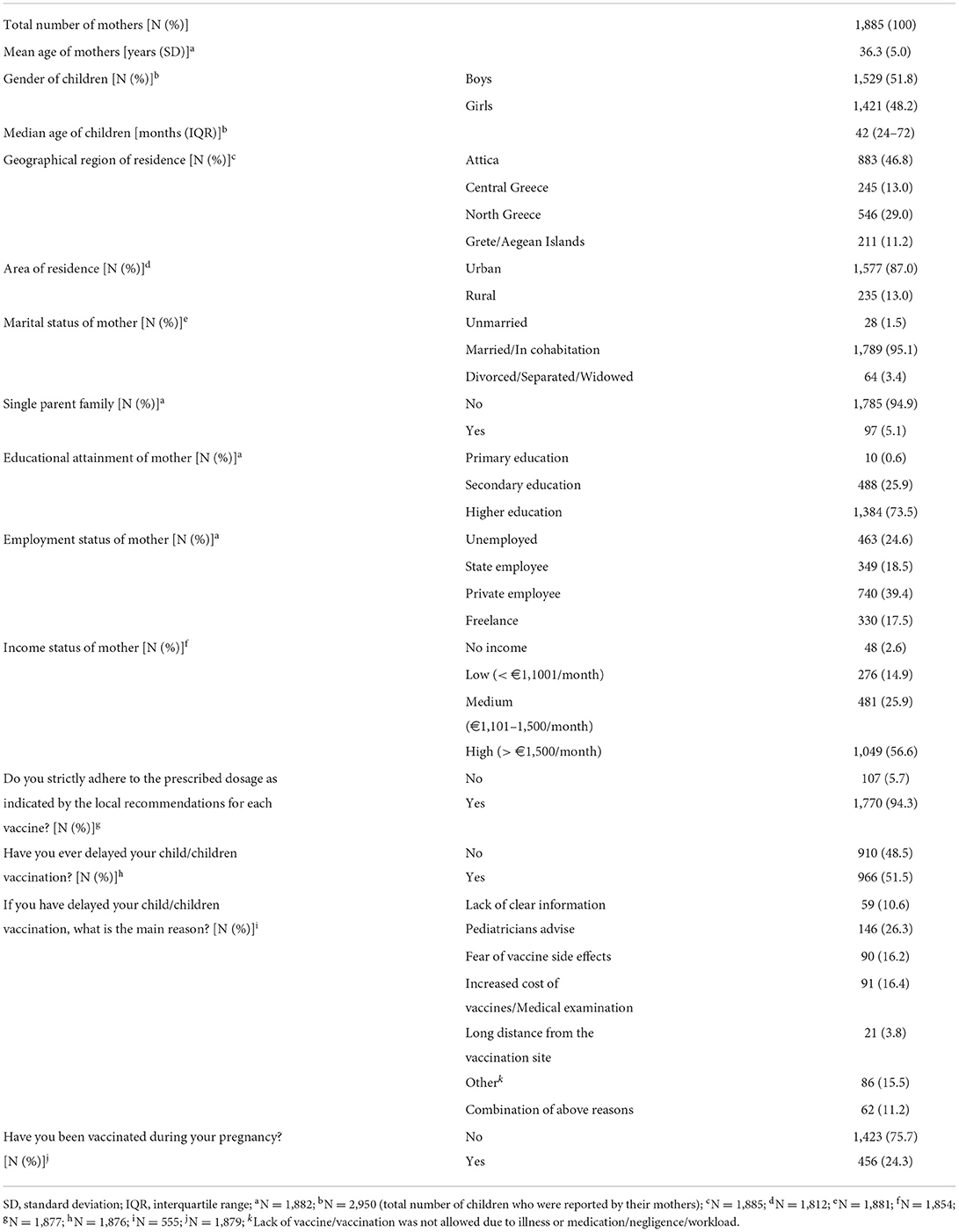
Table 1. Characteristics of the mothers and their children as well as previous vaccination behavior characteristics.
Figure 1 presents the maternal attitudes and perceptions toward their children's vaccination. Most of the participants agreed that vaccines protect children from serious and life-threatening diseases, they believe in the usefulness of vaccines (91.7% for both statements), and they also agreed that all vaccinations provided by the National Vaccination Program must be offered to their children (90.4%). Almost half of them agreed that vaccination in childhood protects for a lifetime (48.0%) and a vaccine always provides protection to a child (49.9%). On the other hand, nearly 62% of the participants, disagreed that many vaccines can adversely affect the immune system of children (61.7%) and they should be vaccinated immediately after the release of a new vaccine (61.2%). Most of the participants did not believe that natural childhood illness is better than vaccination (72.0%). Furthermore, approximately half of mothers were neutral to the question related to the safety and effectiveness of new vaccines (47.5%).
Educational level was a significant sociodemographic factor for many of the statements. Specifically, a larger percentage of mothers with higher educational attainment agreed/absolutely agreed that all vaccinations provided by the National Vaccination Program must be offered to our children (n = 1,268, 91.6%) (p = 0.02) and that vaccines protect children from serious and life-threatening diseases (n = 1,284, 92.9%) (p = 0.01). In addition, mothers with higher education were also more likely than those with other education levels, to disagree that a large number of vaccines can adversely affect the immune system of children (n = 886, 64.1%, p = 0.01). Marital status and single-parent status were significant sociodemographic predictors for one attitude. Particularly, marginally significant higher percentages of married/in cohabitation and not single-parent mothers agreed that vaccines are safe (p = 0.01) (53.5 and 53.4%, respectively). In addition, a higher percentage of married/in cohabitation mothers believed in the usefulness of vaccines compared to unmarried and divorced/separated/widowed mothers (92.1 vs. 82.1% and 84.4%, respectively) (p = 0.04) (Table 2).
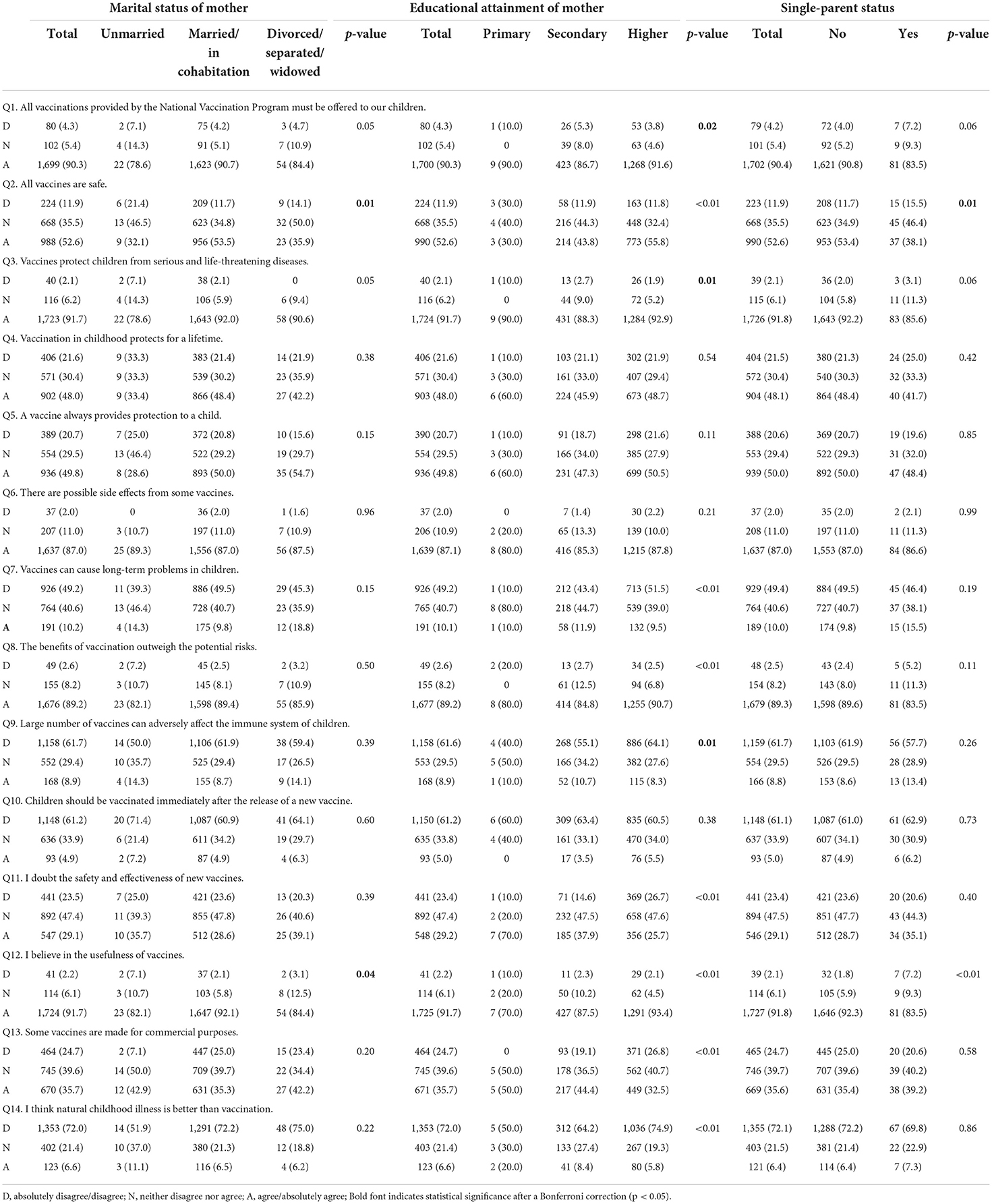
Table 2. Maternal responses to questions about vaccination attitudes by marital status, educational attainment, and single parent status.
A considerably higher proportion of mothers with high income (n = 547, 52.1%) agreed that vaccine always provides protection to a child compared to mothers without income (n = 20, 41.7%) (p = 0.03). In addition, a significant higher percentage of mothers with low, middle, or high income and employed mothers agreed that some vaccines have possible side effects compared to mothers without income (p = 0.04) and unemployed mothers (p = 0.01) (Table 3). Moreover, a significantly lower percentage of private employees (n = 56, 7.6%) (p = 0.03) and participants with a low income (n = 24, 8.7%) (p = 0.02) agreed that vaccines can cause long-term problems in children were identified compared to the other employment and income categories, respectively. A smaller percentage of unemployed mothers disagreed that some vaccines are made for commercial purposes (n = 84, 18.1%) (p = 0.02) and natural childhood illness is better than vaccination (n = 311, 67.3%) (p = 0.01) compared to employed participants. We also found that mothers without income disagreed in a significantly higher proportion, compared to the other categories, that children should be vaccinated immediately after the release of a new vaccine (n = 38, 79.2%) (p = 0.01). In the same sense, a significantly lower percentage of participants without income disagreed that large numbers of vaccines can adversely affect the immune system of children (n = 20, 41.7%) (p = 0.02). More information about the maternal responses to questions about vaccination attitudes by employment and income status of the mother is presented in Table 3.
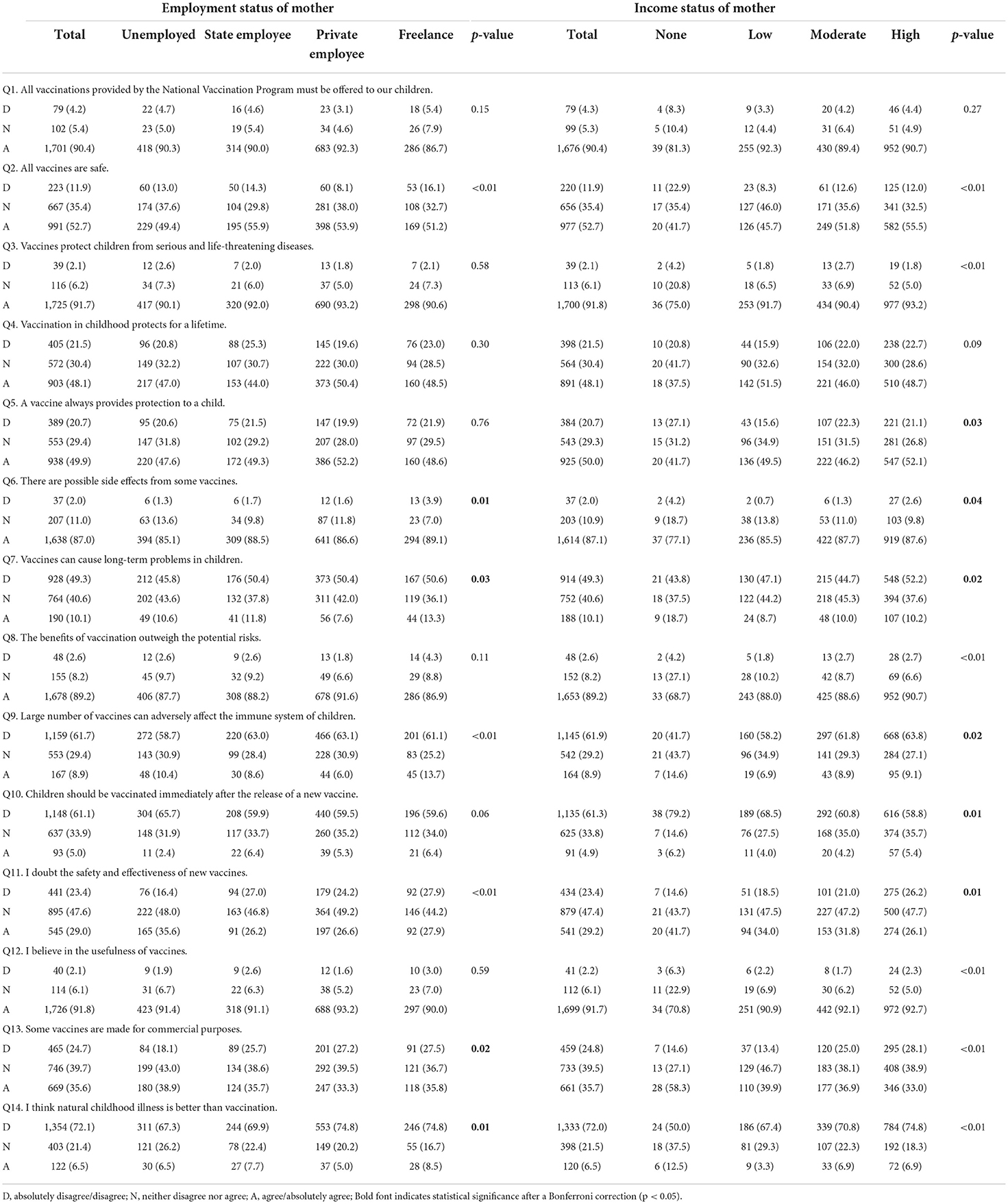
Table 3. Maternal responses to questions about vaccination attitudes by employment and income status of the mother.
Regarding mothers' age, significant differences are observed in the statements “a vaccine always provides protection to a child” (p < 0.01), “there are possible side effects from some vaccines” (p = 0.01), “I doubt the safety and effectiveness of new vaccines” (p = 0.02), and “some vaccines are made for commercial purposes” (p = 0.02). The age of the children noted significant differences only for the attitude “I doubt the safety and effectiveness of new vaccines” (p = 0.04) (Supplementary Table 1).
Region of residency was a significant sociodemographic factor for the statements “vaccines can cause long-term problems in children” and “some vaccines are made for commercial purposes” (Supplementary Table 2). More specifically, 53.7% (n = 474) of the Attica residents disagreed that vaccines could cause long-term problems, while significantly lower (p = 0.04) was the corresponding percentage for the residents of Central (n = 112, 45.7%) and North Greece (n = 247, 45.2%), as well as Crete and Aegean Islands (n = 96, 45.5%). In addition, almost half of the mothers who lived in Crete and Aegean Islands (n = 100, 47.4%), remained neutral regarding the commercial purposes of vaccines (p = 0.02). This attitude was significantly lower in the other geographical areas of Greece, while 33.6% (n = 71) of the remaining residents of Crete and Aegean Island agreed with this statement. Furthermore, in rural areas, a significantly higher proportion of participants, disagreed that children should be vaccinated immediately after the release of a new vaccine (67.2 vs. 60.4% in urban areas, p = 0.03).
Several statistically significant associations were observed between maternal attitudes toward childhood vaccination and maternal vaccination behaviors. The majority of those who adhere to the prescribed dosage as indicated by the local recommendations for each vaccine, delayed their children's vaccination, and were vaccinated during pregnancy, agreed that all the vaccinations provided by the National Vaccination Program must be offered to their children, all vaccines are safe, and vaccines protect children from serious and life-threatening diseases (all p < 0.05). In addition, most mothers who adhered to the prescribed dosage as indicated by the local recommendations for each vaccine and those who did not delay their children vaccination agreed that vaccination in childhood protects for a lifetime and a vaccine always provides protection to a child (p < 0.01). Finally, significant associations were noted between all previous maternal vaccination behaviors and attitudes toward vaccines associated with long-term problems benefits, safety and efficacy, usefulness, commercial purposes, new vaccine acceptance, and preference of natural illness compared to vaccination (Supplementary Table 3).
To the best of our knowledge, this is the first study that evaluated the attitudes and perceptions of mothers in Greece concerning the vaccination of their children during the COVID-19 pandemic. Our findings show that most of the participants agreed that vaccines protect children from serious and life-threatening diseases, and they believe in the usefulness of vaccines. In addition, most of the participants did not believe that natural childhood illness is better than vaccination and approximately half of them were neutral to the question of whether they doubt the safety and effectiveness of new vaccines. Sociodemographic factors significantly affected the maternal attitudes and perceptions toward childhood vaccination. About half of the participants with low income, secondary and higher education, reported neutral attitudes. In Aegean Islands and Crete, a significantly higher prevalence of negative and neutral vaccination perceptions was observed, while negative attitudes were reported in both rural and urban areas. The age of mothers influences their attitudes and predictions about childhood vaccination. Finally, several significant associations were observed between maternal attitudes toward childhood vaccination and previous maternal vaccination behaviors such as adherence to recommender vaccine dosages, vaccination delays, and vaccination uptake during pregnancy.
Statistically significant associations between sociodemographic and economic factors and maternal attitudes have been found in our research. The marital status and educational level are determinants of vaccine belief and attitudes in some countries. In our study, the unmarried, divorced, separated, or widowed mothers were less likely to associate with positive beliefs about vaccine usefulness. Divorced parents in the United Arab Emirates were more vaccine-hesitant (24), while married mothers in Nigeria were associated with commitment to childhood vaccination (56). In contrast, the marital status was not associated with positive attitudes in Croatia (57). The income and educational level were identified as important factors in our study, since primarily educated mothers and single parents without income have negative attitudes toward vaccination. In contrast to our findings, a study in Israel identified higher vaccination compliance among parents with low educational level and average wages (58), and highly educated mothers in Georgia were prone to complete all the childhood vaccinations (59). A previous cross-sectional study in Greece suggests an association between children's age and incomplete vaccination uptake (60). Our results show a statistically significant association only between children's and mothers' age and the safety and effectiveness of new vaccines. Different geographical areas in Greece were associated with different vaccination perceptions, which was also observed in some areas in Italy (61).
The impact of education and income on maternal attitudes and perceptions toward childhood vaccination was also observed in this study. Maternal attitudes toward vaccination protection, safety, efficacy, usefulness, and commercial purposes were linked to maternal educational attainment, income and/or marital status, and age. Our research is consistent with the worldwide literature, which identifies education and income as crucial determinants of vaccination uptake and knowledge across the world (62–65). Also, a previously published study in Greece identified parental age, educational level, and marital status as an important influence of vaccination coverage (66). The results of our study can be used for future campaign to target specific groups to enhance positive attitudes toward vaccination. It is crucial to plan and design effective campaigns which will be population specific according to the maternal socio-demographic characteristics.
Conspiracy theories around childhood vaccination have been previously reported to influence childhood vaccination uptake (67, 68). To date, there has been no detailed investigation of this topic in Greece, however, few studies are providing preliminary insights into parental belief in conspiracy theories. Among them, our study showed that the majority of mothers agreed or remained neutral on the question related to the commercial purpose of vaccines, while a prior study revealed that some mothers support the link between vaccines and autism (66). A recent study in Greece identified the fear of vaccine-related side effects as the main reason of childhood COVID-19 vaccination refusal, while conspiracy theories (vaccines have other purposes) was not a popular reason (69). To develop a full picture of the role of conspiracy theories on childhood vaccination uptake in Greece, additional studies will be needed.
Regarding the positive, negative, and neutral attitudes, we observed different attitudes depending on the vaccination question. Positive maternal attitudes were recorded to general questions such as the vaccination protection, usefulness, and supply through the national vaccination program. On the other hand, fewer positive attitudes were recorded when mothers were asked about the safety of all vaccines and lifetime protection. Mothers possessed neutral attitude toward specific vaccination questions such as the safety and efficacy of new vaccines and the commercial purposes of some vaccines. We identified a considerably high ratio of mothers with neutral attitudes concerning the long-term vaccine-related problems, the safety and efficacy of the new vaccine, and the commercial purposes of some vaccines. The prevalent neutral attitudes toward specific vaccination questions may change to positive attitudes after interventions. Prior studies have noted the importance of educational interventions in parental knowledge and attitudes toward the vaccination of their children (70, 71). We believe that population-specific educational interventions in the Greek cohort are necessary to maintain a positive attitude toward vaccination and prevent a high level of vaccination hesitancy and negative attitudes toward vaccination in the future.
There are several important differences and similarities between our research and other studies in Europe. Most of the participants in our study did not believe that natural childhood illness is better than vaccination. By contrast, many parents in Finland supported that natural illness provides longer protection compared to vaccination (72). Interestingly, we revealed that a high proportion of women in Greece have not been vaccinated during pregnancy. Similarly, only a small percentage of women in Italy and Germany have received vaccinations during pregnancy (73, 74), while the uptake in the UK was considerably higher (75). Of note, women in the UK stated that pregnancy interferes with their decision to accept the COVID-19 vaccine (76). In regard to childhood vaccination delays, those were also observed in other European countries such as France, Belgium, and Albania (77–79).
It is also important to acknowledge the role of healthcare professionals in reshaping maternal attitudes toward vaccination. Literature highlights the positive influence of parental trust toward pediatricians and vaccination uptake (80). Previous studies among mothers and pregnant women in Greece and in Cyprus identified pediatricians as the primary and trustworthy source of vaccination-related information (55, 81, 82). In addition, two of those studies revealed the influence of pediatricians on childhood vaccination delay (55, 82). Therefore, interventions through pediatricians in Greece seem to be effective. Pediatricians should inform mothers, especially those with characteristics linked to negative and neutral attitudes, about vaccination benefits. A cost-effective approach is the development of a free mobile application with videos about vaccination which will be promoted by pediatricians (83, 84).
The prevalent negative and neutral attitudes toward vaccination may lead to inadequate vaccination uptake (65), and influence new vaccine acceptance (85). Negative maternal attitudes toward new vaccines were previously shown in the Greek cohort (60). In our study, most mothers were neutral regarding the safety and efficacy of new vaccines and opposed to the immediate vaccination after a new vaccine release. The low levels of new vaccine acceptance found in our study raise concerns about the acceptability of future vaccines such as the COVID-19 vaccine. Future studies focusing on new vaccine trust among mothers in Greece are therefore recommended. Nevertheless, the majority recognized the vaccine's usefulness and disease prevention and agreed that the benefits outweigh any potential vaccination risks. These findings raise intriguing questions regarding the process of developing trust and confidence toward new vaccines.
Our study also revealed that parental vaccination behaviors are closely related to their attitudes toward childhood vaccination. Mothers who adhered to the recommended dosages for each childhood vaccine did not delay the vaccination of their children and have been vaccinated during pregnancy have shown more positive attitudes compared to those who did not adhere to the prescribed vaccine dosages, delayed vaccination, and did not receive vaccinations during pregnancy. Research in the past few years also acknowledges that parental vaccination behavior and experiences influence childhood vaccination uptake, especially that vaccination-related side effects can cause delays or vaccine refusal (51). In addition, acceptance of seasonal influenza vaccination during pregnancy was associated with maternal intention to vaccinate their infants (86).
The COVID-19 pandemic has initiated conversations around regulations to minimize the transmission of the novel coronavirus while preserving human rights and diminishing health inequalities. COVID-19 vaccine approval and availability are milestones in the history of humanity and highlighted the emergency of understanding the vaccine hesitancy. Our findings may help us to understand the parental attitudes toward the childhood COVID-19 vaccination, since reveals the maternal sociodemographic characteristics and how they influence their attitudes and perceptions toward childhood vaccination at the beginning of the pandemic. Previous studies have shown that parental confidence in the COVID-19 vaccine positively influenced the vaccine acceptance for their children (87), while positive attitudes toward childhood vaccination and belief in the importance of vaccines do not reflect their willingness to accept the COVID-19 vaccination of their children (88). Here, we identified a high level of maternal hesitancy toward new vaccines, and specific maternal characteristics were associated with negative attitudes and perceptions. Although a higher percentage of mothers who received vaccinations during pregnancy agreed that children should be vaccinated immediately after the release of new vaccines, the majority remained neutral. It is crucial to provide useful sources of vaccination-related information, with a focus on topics such as vaccine development and approval to those groups and implement strategies to minimize the parental hesitancy toward childhood vaccination and increase the acceptance of new vaccines.
Despite our major research findings, this study has some limitations. Firstly, the data collection was done using convenience sampling through an online tool that limits our study representativeness. Our sample includes a higher proportion of highly educated women compared to the general population as well as a higher proportion of women living in urban areas, which could lead to selection bias. Nevertheless, the overrepresentation of such characteristics is possible to reflect greater health awareness and interest in science, whilst the use of online methods is the best solution for data collection in periods of social distancing due to the COVID-19 pandemic. Secondly, the self-reporting nature of data collection potentially leads to misreporting and information bias and potential under-or overestimations of reported associations. However, the latter is less of an issue as it is inherent in all types of knowledge/attitude assessment research. Thirdly, this is a cross-sectional study, therefore causal relationships between mothers' knowledge and vaccination behavior cannot be inferred. Despite these limitations, our study involved a fair number of participants with different social-demographic characteristics at a national level, however, the generalizability of the findings may be limited by possible selection bias due to language barrier, unfamiliarity with online survey tools, and the oversampling of a particular network of similar groups.
The study provides knowledge about the attitudes and perceptions of mothers in Greece regarding childhood vaccination. Most of the mothers participated in the study believe in the usefulness of vaccines and that vaccines protect children from serious and life-threatening diseases. In addition, the majority of the mothers strictly adhered to the prescribed dosage as indicated by the local recommendations for each vaccine, have delayed their child/children vaccination and have not been vaccinated during pregnancy. Educational level was a significant sociodemographic factor for most many of the attitudes. In addition, maternal attitudes toward childhood vaccination and previous maternal practices (i.e., adherence to recommender vaccine dosages, vaccination delays, and vaccination uptake during pregnancy) were associated with attitudes and perceptions about vaccination. Given the fact that multiple epidemics, outbreaks, and pandemics are happening worldwide over the years, revealing the attitudes and perceptions of mothers about childhood vaccination is essential for public health planning. The neutral attitudes toward vaccination raise concerns about possible negative attitudes in the future, while the previous parental vaccination behavior affects the childhood vaccination outcome. Healthcare professionals and public health decision-makers should consider the attitudes and perceptions of mothers on the development of educational programs and campaigns, by informing and encouraging mothers about childhood vaccination. This will be critical in the coming years, as mothers' vaccination practices for their children are anticipated to become increasingly significant in the wake of the COVID-19 pandemic.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
This study was conducted according to the guidelines laid down in the Declaration of Helsinki and all procedures involving research study participants were approved by the Cyprus National Bioethics Committee (EEBK EΠ 2020.01.82). The participants provided their consent to participate in this study.
GF, MK, and KG drafted the original manuscript. GF and KG interpreted the results. AH, MK, and KG analyzed the data. ET, MK, and KG designed the survey and collected data. KG conceived and supervised this research. All authors read and approved the final manuscript.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fped.2022.951039/full#supplementary-material
1. Strassburg MA. The global eradication of smallpox. Am J Infection Cont. (1982) 10:53–9. doi: 10.1016/0196-6553(82)90003-7
2. Stewart AJ, Devlin PM. The history of the smallpox vaccine. J Infection. (2006) 52:329–34. doi: 10.1016/j.jinf.2005.07.021
3. Andre FE, Booy R, Bock HL, Clemens J, Datta SK, John TJ, et al. Vaccination greatly reduces disease, disability, death and inequity worldwide. Bull World Health Organization. (2008) 86:140–6. doi: 10.2471/BLT.07.040089
4. Orenstein WA, Ahmed R. Simply put: Vaccination saves lives. Natl Acad Sci. (2017) 114:4031–3. doi: 10.1073/pnas.1704507114
5. Abidi S, Labani S, Singh A, Asthana S, Ajmera P. Economic evaluation of human papillomavirus vaccination in the Global South: a systematic review. Int J Public Health. (2020) 2020:1–15. doi: 10.1007/s00038-020-01431-1
6. Moghadas SM, Vilches TN, Zhang K, Wells CR, Shoukat A, Singer BH, et al. The impact of vaccination on coronavirus disease 2019 (COVID-19) outbreaks in the United States. Clin Infect Dis. (2021) 73:2257–64. doi: 10.1093/cid/ciab079
7. Suthar AB, Wang J, Seffren V, Wiegand RE, Griffing S, Zell E. Public health impact of covid-19 vaccines in the US: observational study. Bmj. (2022) 377:69317. doi: 10.1136/bmj-2021-069317
8. Huijbers PM, Larsson DJ, Flach C-F. Surveillance of antibiotic resistant Escherichia coli in human populations through urban wastewater in ten European countries. Environ Pollut. (2020) 261:114200. doi: 10.1016/j.envpol.2020.114200
9. Asfaw Ali D, Tadesse B, Ebabu A. Prevalence and antibiotic resistance pattern of Salmonella isolated from caecal contents of exotic chicken in Debre Zeit and Modjo, Ethiopia. Int J Microbiol. (2020) 2020:e1910630. doi: 10.1155/2020/1910630
10. Nji E, Kazibwe J, Hambridge T, Joko CA, Larbi AA, Damptey LAO, et al. High prevalence of antibiotic resistance in commensal Escherichia coli from healthy human sources in community settings. Sci Rep. (2021) 11:1–11. doi: 10.1038/s41598-021-82693-4
11. Zhang Y, Chen M, Yu P, Yu S, Wang J, Guo H, et al. Prevalence, virulence feature, antibiotic resistance and MLST typing of Bacillus cereus isolated from retail aquatic products in China. Front Microbiol. (2020) 11:1513. doi: 10.3389/fmicb.2020.01513
12. Becker K, Hu Y, Biller-Andorno N. Infectious diseases–a global challenge. Intl J Med Microbiol. (2006) 296:179–85. doi: 10.1016/j.ijmm.2005.12.015
13. Kwong JC, Ratnasingham S, Campitelli MA, Daneman N, Deeks SL, Manuel DG, et al. The impact of infection on population health: results of the Ontario burden of infectious diseases study. PLoS ONE. (2012) 7:e44103. doi: 10.1371/journal.pone.0044103
14. Armstrong GL, Wasley A, Simard EP, McQuillan GM, Kuhnert WL, Alter MJ. The prevalence of hepatitis C virus infection in the United States, 1999 through 2002. Ann Internal Med. (2006) 144:705–14. doi: 10.7326/0003-4819-144-10-200605160-00004
15. Vos T, Lim SS, Abbafati C, Abbas KM, Abbasi M, Abbasifard M, et al. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. (2020) 396:1204–22. doi: 10.1016/S0140-6736(20)30925-9
16. Momeni AZ, Jalayer T, Emamjomeh M, Khamesipour A, Zicker F, Ghassemi RL, et al. A randomized, double-blind, controlled trial of a killed L. major vaccine plus BCG against zoonotic cutaneous leishmaniasis in Iran. Vaccine. (1999) 17:466–72. doi: 10.1016/S0264-410X(98)00220-5
17. Scorza T, D'souza S, Laloup M, Dewit J, De Braekeleer J, Verschueren H, et al. A GRA1 DNA vaccine primes cytolytic CD8+ T cells to control acute Toxoplasma gondii infection. Infect Immunity. (2003) 71:309–16. doi: 10.1128/IAI.71.1.309-316.2003
18. Group rHVS. Placebo-controlled phase 3 trial of a recombinant glycoprotein 120 vaccine to prevent HIV-1 infection. J Infect Dis. (2005) 191:654–65. doi: 10.1086/428404
19. Bertoncello C, Ferro A, Fonzo M, Zanovello S, Napoletano G, Russo F, et al. Socioeconomic determinants in vaccine hesitancy and vaccine refusal in Italy. Vaccines. (2020) 8:276. doi: 10.3390/vaccines8020276
20. Karafillakis E, Simas C, Jarrett C, Verger P, Peretti-Watel P, Dib F, et al. HPV vaccination in a context of public mistrust and uncertainty: a systematic literature review of determinants of HPV vaccine hesitancy in Europe. Human Vaccines Immunotherap. (2019) 15:1615–27. doi: 10.1080/21645515.2018.1564436
21. Marti M, de Cola M, MacDonald NE, Dumolard L, Duclos P. Assessments of global drivers of vaccine hesitancy in 2014—Looking beyond safety concerns. PLoS ONE. (2017) 12:e0172310. doi: 10.1371/journal.pone.0172310
22. Guay M, Gosselin V, Petit G, Baron G, Gagneur A. Determinants of vaccine hesitancy in Quebec: a large population-based survey. Human Vaccines Immunotherap. (2019) 15:2527–33. doi: 10.1080/21645515.2019.1603563
23. Costantino C, Caracci F, Brandi M, Bono SE, Ferro A, Sannasardo CE, et al. Determinants of vaccine hesitancy and effectiveness of vaccination counseling interventions among a sample of the general population in Palermo, Italy. Human Vaccines Immunotherap. (2020) 16:2415–21. doi: 10.1080/21645515.2020.1728157
24. Alsuwaidi AR, Elbarazi I, Al-Hamad S, Aldhaheri R, Sheek-Hussein M, Narchi H. Vaccine hesitancy and its determinants among Arab parents: a cross-sectional survey in the United Arab Emirates. Human Vaccines Immunotherap. (2020) 16:3163–9. doi: 10.1080/21645515.2020.1753439
25. Du F, Chantler T, Francis MR, Sun FY, Zhang X, Han K, et al. The determinants of vaccine hesitancy in China: A cross-sectional study following the Changchun Changsheng vaccine incident. Vaccine. (2020) 38:7464–71. doi: 10.1016/j.vaccine.2020.09.075
26. Santibanez TA, Nguyen KH, Greby SM, Fisher A, Scanlon P, Bhatt A, et al. Parental vaccine hesitancy and childhood influenza vaccination. Pediatrics. (2020) 146:e7609. doi: 10.1542/peds.2020-007609
27. Plans-Rubió P. Low percentages of measles vaccination coverage with two doses of vaccine and low herd immunity levels explain measles incidence and persistence of measles in the European Union in 2017–2018. Eur J Clin Microbiol Infect Dis. (2019) 38:1719–29. doi: 10.1007/s10096-019-03604-0
28. Papagiannis D, Rachiotis G, Mariolis A, Zafiriou E, Gourgoulianis KI. Vaccination coverage of the elderly in Greece: A cross-sectional nationwide study. Canad J Infect Dis Med Microbiol. (2020) 2020:e5459793. doi: 10.1155/2020/5459793
29. Uchida M, Kaneko M, Hidaka Y, Yamamoto H, Honda T, Takeuchi S, et al. High vaccination coverage is associated with low epidemic level of seasonal influenza in elementary schools: an observational study in Matsumoto City, Japan. BMC Infect Dis. (2018) 18:1–7. doi: 10.1186/s12879-018-3025-9
30. Papamichail D, Petraki I, Arkoudis C, Terzidis A, Smyrnakis E, Benos A, et al. Low vaccination coverage of Greek Roma children amid economic crisis: national survey using stratified cluster sampling. Eur J Public Health. (2017) 27:318–24. doi: 10.1093/eurpub/ckw179
31. Burnett E, Jonesteller CL, Tate JE, Yen C, Parashar UD. Global impact of rotavirus vaccination on childhood hospitalizations and mortality from diarrhea. J Infect Dis. (2017) 215:1666–72. doi: 10.1093/infdis/jix186
32. Jensen A, Andersen PK, Stensballe LG. Early childhood vaccination and subsequent mortality or morbidity: are observational studies hampered by residual confounding? A Danish register-based cohort study. BMJ Open. (2019) 9:e029794. doi: 10.1136/bmjopen-2019-029794
33. Kristensen I, Fine P, Aaby P, Jensen H. Routine vaccinations and child survival: follow up study in Guinea-Bissau, West AfricaCommentary: an unexpected finding that needs confirmation or rejection. BMJ. (2000) 321:1435. doi: 10.1136/bmj.321.7274.1435
34. Bimpong KA, Nuertey BD, Seidu AS, Ajinkpang S, Abdul-Mumin A. Decline in uptake of childhood vaccinations in a tertiary hospital in Northern Ghana during the COVID-19 pandemic. BioMed Res Int. (2021) 2021:e6995096. doi: 10.1155/2021/6995096
35. Chandir S, Siddiqi DA, Mehmood M, Setayesh H, Siddique M, Mirza A, et al. Impact of COVID-19 pandemic response on uptake of routine immunizations in Sindh, Pakistan: an analysis of provincial electronic immunization registry data. Vaccine. (2020) 38:7146–55. doi: 10.1016/j.vaccine.2020.08.019
36. Dong A, Meaney C, Sandhu G, De Oliveira N, Singh S, Morson N, et al. Routine childhood vaccination rates in an academic family health team before and during the first wave of the COVID-19 pandemic: a pre–post analysis of a retrospective chart review. Canad Med Assoc Open Access J. (2022) 10:E43–9. doi: 10.9778/cmajo.20210084
37. Ackerson BK, Sy LS, Glenn SC, Qian L, Park CH, Riewerts RJ, et al. Pediatric vaccination during the COVID-19 pandemic. Pediatrics. (2021) 148:e047092. doi: 10.1542/peds.2020-047092
38. MacDonald SE, Paudel YR, Kiely M, Rafferty E, Sadarangani M, Robinson JL, et al. Impact of the COVID-19 pandemic on vaccine coverage for early childhood vaccines in Alberta, Canada: a population-based retrospective cohort study. BMJ Open. (2022) 12:e055968. doi: 10.1136/bmjopen-2021-055968
39. Shet A, Carr K, Danovaro-Holliday MC, Sodha SV, Prosperi C, Wunderlich J, et al. Impact of the SARS-CoV-2 pandemic on routine immunisation services: evidence of disruption and recovery from 170 countries and territories. Lancet Global Health. (2022) 10:e186–94. doi: 10.1016/S2214-109X(21)00512-X
40. Gilkey MB, Bednarczyk RA, Gerend MA, Kornides ML, Perkins RB, Saslow D, et al. Getting human papillomavirus vaccination back on track: protecting our national investment in human papillomavirus vaccination in the COVID-19 era. J Adolesc Health. (2020) 67:633. doi: 10.1016/j.jadohealth.2020.08.013
41. Sweileh WM. Bibliometric analysis of global scientific literature on vaccine hesitancy in peer-reviewed journals (1990–2019). BMC Public Health. (2020) 20:1–15. doi: 10.1186/s12889-020-09368-z
42. Della Polla G, Pelullo CP, Napolitano F, Angelillo IF. HPV vaccine hesitancy among parents in Italy: a cross-sectional study. Human Vaccines Immunotherap. (2020) 16:2744–51. doi: 10.1080/21645515.2020.1744367
43. Kalok A, Loh SYE, Chew KT, Aziz NHA, Shah SA, Ahmad S, et al. Vaccine hesitancy towards childhood immunisation amongst urban pregnant mothers in Malaysia. Vaccine. (2020) 38:2183–9. doi: 10.1016/j.vaccine.2020.01.043
44. Wagner AL, Huang Z, Ren J, Laffoon M, Ji M, Pinckney LC, et al. Vaccine hesitancy and concerns about vaccine safety and effectiveness in Shanghai, China. Am J Prevent Med. (2021) 60:S77–86. doi: 10.1016/j.amepre.2020.09.003
45. Roberts JR, Thompson D, Rogacki B, Hale JJ, Jacobson RM, Opel DJ, et al. Vaccine hesitancy among parents of adolescents and its association with vaccine uptake. Vaccine. (2015) 33:1748–55. doi: 10.1016/j.vaccine.2015.01.068
46. Yufika A, Wagner AL, Nawawi Y, Wahyuniati N, Anwar S, Yusri F, et al. Parents' hesitancy towards vaccination in Indonesia: a cross-sectional study in Indonesia. Vaccine. (2020) 38:2592–9. doi: 10.1016/j.vaccine.2020.01.072
47. Napolitano F, D'Alessandro A, Angelillo IF. Investigating Italian parents' vaccine hesitancy: A cross-sectional survey. Human Vaccines Immunotherap. (2018) 14:1558–65. doi: 10.1080/21645515.2018.1463943
48. Giambi C, Fabiani M, D'Ancona F, Ferrara L, Fiacchini D, Gallo T, et al. Parental vaccine hesitancy in Italy–results from a national survey. Vaccine. (2018) 36:779–87. doi: 10.1016/j.vaccine.2017.12.074
49. Kempe A, Saville AW, Albertin C, Zimet G, Breck A, Helmkamp L, et al. Parental hesitancy about routine childhood and influenza vaccinations: a national survey. Pediatrics. (2020) 146:e3852. doi: 10.1542/peds.2019-3852
50. Fuchs EL. Self-reported prenatal influenza vaccination and early childhood vaccine series completion. Prevent Med. (2016) 88:8–12. doi: 10.1016/j.ypmed.2016.03.012
51. Ellithorpe ME, Adams R, Aladé F. Parents' behaviors and experiences associated with four vaccination behavior groups for childhood vaccine hesitancy. Mater Child Health J. (2022) 2022:1–9. doi: 10.1007/s10995-021-03336-8
52. Craig L, Mullan K. How mothers and fathers share childcare: A cross-national time-use comparison. Am Sociol Rev. (2011) 76:834–61. doi: 10.1177/0003122411427673
53. Von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: guidelines for reporting observational studies. Int J Surg. (2014) 12:1495–9. doi: 10.1016/j.ijsu.2014.07.013
54. Pourhoseingholi MA, Vahedi M, Rahimzadeh M. Sample size calculation in medical studies. Gastroenterol Hepatol Bed Bench. (2013) 6:14.
55. Giannakou K, Kyprianidou M, Hadjikou A, Fakonti G, Photiou G, Tzira E, et al. Knowledge of mothers regarding children's vaccinations in Greece: an online cross-sectional study. BMC Public Health. (2021) 21:1–13. doi: 10.1186/s12889-021-12179-5
56. Brown V, Oluwatosin O. Socio-demographic factors associated with childhood immunization uptake inAkinyele Local Government Area, Oyo State, Nigeria. (2012) 41:161–7.
57. Makarić ZL, Kolarić B, Tomljenović M, Posavec M. Attitudes and beliefs related to childhood vaccinations among parents of 6 years old children in Zagreb, Croatia. Vaccine. (2018) 36:7530–5. doi: 10.1016/j.vaccine.2018.10.055
58. Elran B, Yaari S, Glazer Y, Honovich M, Grotto I, Anis E. Parents' perceptions of childhood immunization in Israel: Information and concerns. Vaccine. (2018) 36:8062–8. doi: 10.1016/j.vaccine.2018.10.078
59. Verulava T, Jaiani M, Lordkipanidze A, Jorbenadze R, Dangadze B. Mothers' Knowledge and attitudes towards child immunization in georgia. Open Public Health J. (2019) 12:e10232. doi: 10.2174/1874944501912010232
60. Pavlopoulou ID, Michail KA, Samoli E, Tsiftis G, Tsoumakas K. Immunization coverage and predictive factors for complete and age-appropriate vaccination among preschoolers in Athens, Greece: a cross-sectional study. BMC Public Health. (2013) 13:1–10. doi: 10.1186/1471-2458-13-908
61. Impicciatore P, Bosetti C, Schiavio S, Pandolfini C, Bonati M. Mothers as active partners in the prevention of childhood diseases: maternal factors related to immunization status of preschool children in Italy. Prevent Med. (2000) 31:49–55. doi: 10.1006/pmed.2000.0677
62. Luman ET, McCauley MM, Shefer A, Chu SY. Maternal characteristics associated with vaccination of young children. Pediatrics. (2003) 111(Supplement 1):1215–8. doi: 10.1542/peds.111.S1.1215
63. Kose D, Erkorkmaz U, Cinar N, Altinkaynak S. Mothers' knowledge and attitudes about HPV vaccination to prevent cervical cancers. Asian Pacific J Cancer Prevent. (2014) 15:7263–6. doi: 10.7314/APJCP.2014.15.17.7263
64. Han Z, Yin Y, Zhang Y, Ehrhardt S, Thio CL, Nelson KE, et al. Knowledge of and attitudes towards hepatitis B and its transmission from mother to child among pregnant women in Guangdong Province, China. PLoS ONE. (2017) 12:e0178671. doi: 10.1371/journal.pone.0178671
65. Tabacchi G, Costantino C, Napoli G, Marchese V, Cracchiolo M, Casuccio A, et al. Determinants of European parents' decision on the vaccination of their children against measles, mumps and rubella: A systematic review and meta-analysis. Human Vaccines Immunotherap. (2016) 12:1909–23. doi: 10.1080/21645515.2016.1151990
66. Gkentzi D, Tsagri C, Kostopoulou E, Fouzas S, Vantarakis A, Dimitriou G, et al. Attitudes and beliefs of parents about routine childhood vaccination in Greece. Human Vaccines Immunotherap. (2021) 2021:1–7. doi: 10.1080/21645515.2021.1914805
67. Bradshaw AS, Treise D, Shelton SS, Cretul M, Raisa A, Bajalia A, et al. Propagandizing anti-vaccination: analysis of vaccines revealed documentary series. Vaccine. (2020) 38:2058–69. doi: 10.1016/j.vaccine.2019.12.027
68. Cobos Muñoz D, Monzón Llamas L, Bosch-Capblanch X. Exposing concerns about vaccination in low-and middle-income countries: a systematic review. Int J Public Health. (2015) 60:767–80. doi: 10.1007/s00038-015-0715-6
69. Miliordos K, Giannouchos T, Steletou E, Sanidas G, Karkania A, Vervenioti A, et al. Parental attitudes towards vaccination against COVID-19 of children 5–11 years old in Greece. J Evaluation Clin Pract. (2022) 1–5. doi: 10.1111/jep.13701
70. Tkaczyszyn K, Kuchar E, Augustynowicz E, Szenborn L. The impact of a single educational lecture on the vaccine confidence among pregnant women and young mothers. Vaccines. (2021) 9:290. doi: 10.3390/vaccines9030290
71. Awadh AI, Hassali MA, Al-Lela OQ, Bux SH, Elkalmi RM, Hadi H. Does an educational intervention improve parents' knowledge about immunization? Experience from Malaysia. BMC Pediatr. (2014) 14:1–7. doi: 10.1186/1471-2431-14-254
72. Nurmi J, Harman B. Why do parents refuse childhood vaccination? Reasons reported in Finland. Scand J Public Health. (2022) 50:490–6. doi: 10.1177/14034948211004323
73. Brixner A, Brandstetter S, Böhmer MM, Seelbach-Göbel B, Melter M, Kabesch M, et al. Prevalence of and factors associated with receipt of provider recommendation for influenza vaccination and uptake of influenza vaccination during pregnancy: cross-sectional study. BMC Pregnancy Childbirth. (2021) 21:1–12. doi: 10.1186/s12884-021-04182-w
74. Scatigna M, Appetiti A, Pasanisi M, D'Eugenio S, Fabiani L, Giuliani AR. Experience and attitudes on vaccinations recommended during pregnancy: survey on an Italian sample of women and consultant gynecologists. Human Vaccines Immunotherap. (2022) 18:1–8. doi: 10.1080/21645515.2021.1894061
75. Ralph KM, Dorey RB, Rowe R, Jones CE. Improving uptake of vaccines in pregnancy: A service evaluation of an antenatal vaccination clinic at a tertiary hospital in the UK. Midwifery. (2022) 105:103222. doi: 10.1016/j.midw.2021.103222
76. Skirrow H, Barnett S, Bell S, Riaposova L, Mounier-Jack S, Kampmann B, et al. Women's views on accepting COVID-19 vaccination during and after pregnancy, and for their babies: A multi-methods study in the UK. BMC Pregnancy Childbirth. (2022) 22:1–15. doi: 10.1186/s12884-021-04321-3
77. Mayerová D, Abbas K. Childhood immunisation timeliness and vaccine confidence by health information source, maternal, socioeconomic, and geographic characteristics in Albania. BMC Public Health. (2021) 21:1–17. doi: 10.1186/s12889-021-11724-6
78. Bailly A-C, Gras P, Lienhardt J-F, Requillart J-C, Vié-le-Sage F, Martinot A, et al. Timeliness of vaccination in infants followed by primary-care pediatricians in France. Human Vaccines Immunotherap. (2018) 14:1018–23. doi: 10.1080/21645515.2017.1409318
79. Lernout T, Theeten H, Hens N, Braeckman T, Roelants M, Hoppenbrouwers K, et al. Timeliness of infant vaccination and factors related with delay in Flanders, Belgium. Vaccine. (2014) 32:284–9. doi: 10.1016/j.vaccine.2013.10.084
80. Frawley JE, Foley H, McIntyre E. The associations between medical, allied and complementary medicine practitioner visits and childhood vaccine uptake. Vaccine. (2018) 36:866–72. doi: 10.1016/j.vaccine.2017.12.036
81. Maltezou HC, Theodora M, Lytras T, Fotiou A, Nino E, Theodoridou M, et al. Knowledge, attitudes and practices about vaccine-preventable diseases and vaccinations of children among pregnant women in Greece. Vaccine. (2020) 38:7654–8. doi: 10.1016/j.vaccine.2020.10.003
82. Kyprianidou M, Tzira E, Galanis P, Giannakou K. Knowledge of mothers regarding children's vaccinations in Cyprus: a cross-sectional study. PLoS ONE. (2021) 16:e0257590. doi: 10.1371/journal.pone.0257590
83. Salmon DA, Limaye RJ, Dudley MZ, Oloko OK, Church-Balin C, Ellingson MK, et al. MomsTalkShots: An individually tailored educational application for maternal and infant vaccines. Vaccine. (2019) 37:6478–85. doi: 10.1016/j.vaccine.2019.08.080
84. Dudley MZ, Limaye RJ, Omer SB, O'Leary ST, Ellingson MK, Spina CI, et al. Factors associated with referring close contacts to an app with individually-tailored vaccine information. Vaccine. (2020) 38:2827–32. doi: 10.1016/j.vaccine.2020.02.019
85. Skjefte M, Ngirbabul M, Akeju O, Escudero D, Hernandez-Diaz S, Wyszynski DF, et al. COVID-19 vaccine acceptance among pregnant women and mothers of young children: results of a survey in 16 countries. Eur J Epidemiol. (2021) 36:197–211. doi: 10.1007/s10654-021-00728-6
86. Frew PM, Zhang S, Saint-Victor DS, Schade AC, Benedict S, Banan M, et al. Influenza vaccination acceptance among diverse pregnant women and its impact on infant immunization. Human Vaccines Immunotherap. (2013) 9:2591–602. doi: 10.4161/hv.26993
87. Temsah M-H, Alhuzaimi AN, Aljamaan F, Bahkali F, Al-Eyadhy A, Alrabiaah A, et al. Parental attitudes and hesitancy about COVID-19 versus routine childhood vaccinations: a national survey. Front Public Health. (2021) 2021:1513. doi: 10.3389/fpubh.2021.752323
Keywords: vaccination, immunization, attitudes, mothers, children, Greece, COVID-19
Citation: Fakonti G, Hadjikou A, Tzira E, Kyprianidou M and Giannakou K (2022) Attitudes and perceptions of mothers towards childhood vaccination in Greece: lessons to improve the childhood COVID-19 vaccination acceptance. Front. Pediatr. 10:951039. doi: 10.3389/fped.2022.951039
Received: 23 May 2022; Accepted: 21 July 2022;
Published: 25 August 2022.
Edited by:
Muhammad Hammad Butt, University of Central Punjab, PakistanReviewed by:
Bart Van Den Borne, Maastricht University, NetherlandsCopyright © 2022 Fakonti, Hadjikou, Tzira, Kyprianidou and Giannakou. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Konstantinos Giannakou, Sy5HaWFubmFrb3VAZXVjLmFjLmN5
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.